Abstract
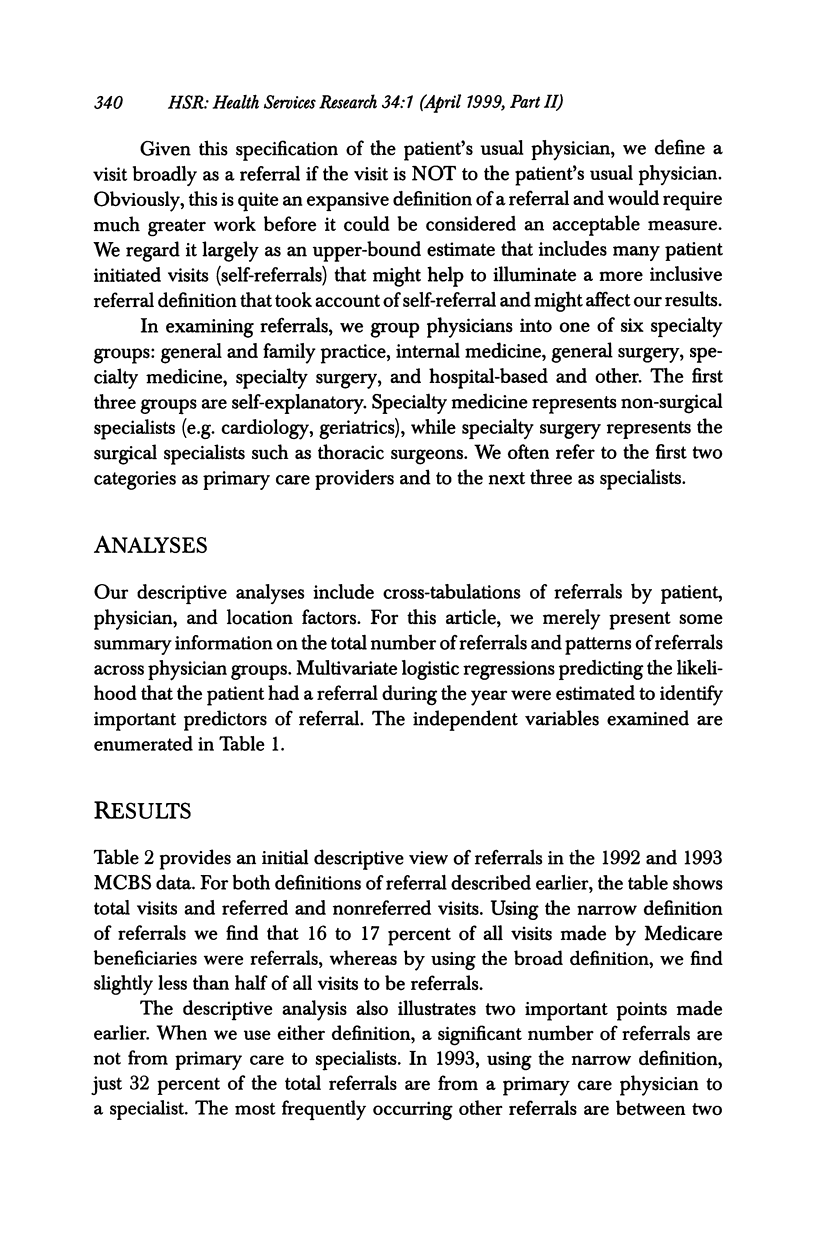
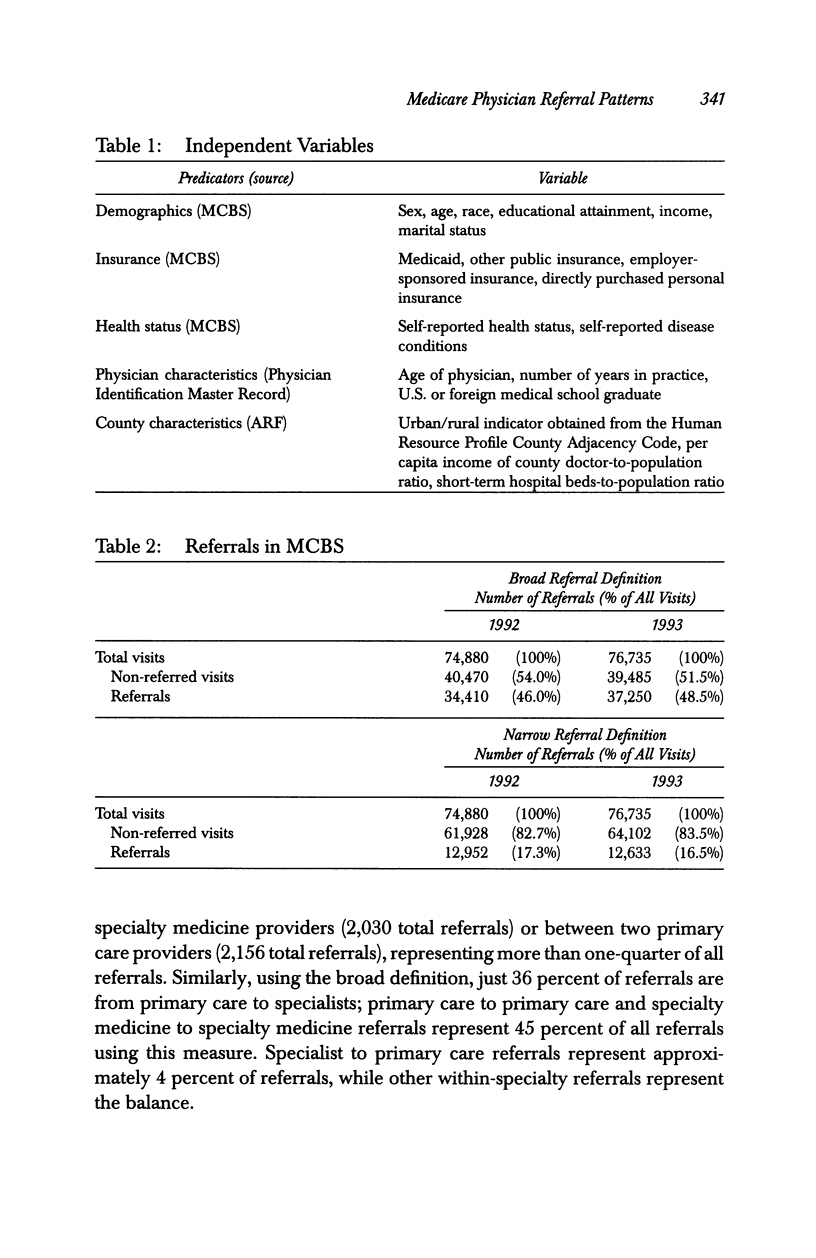
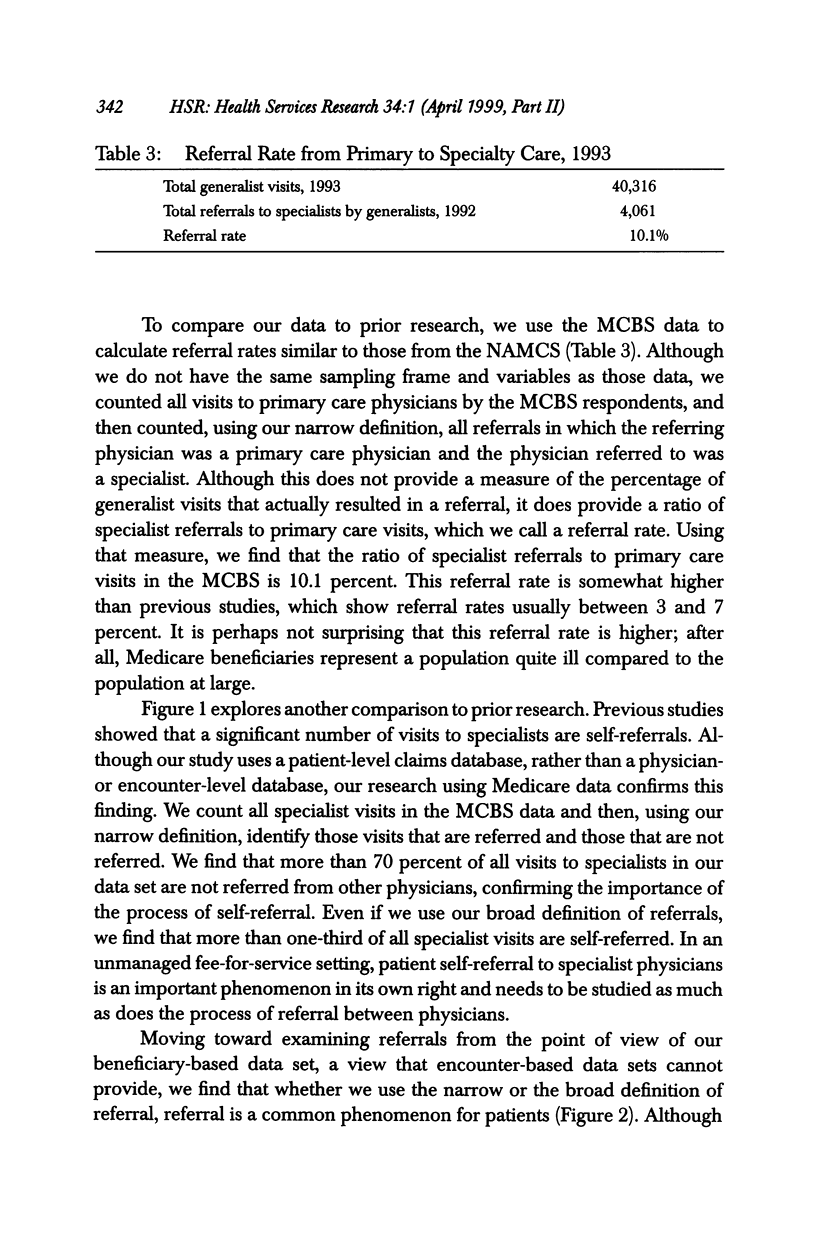
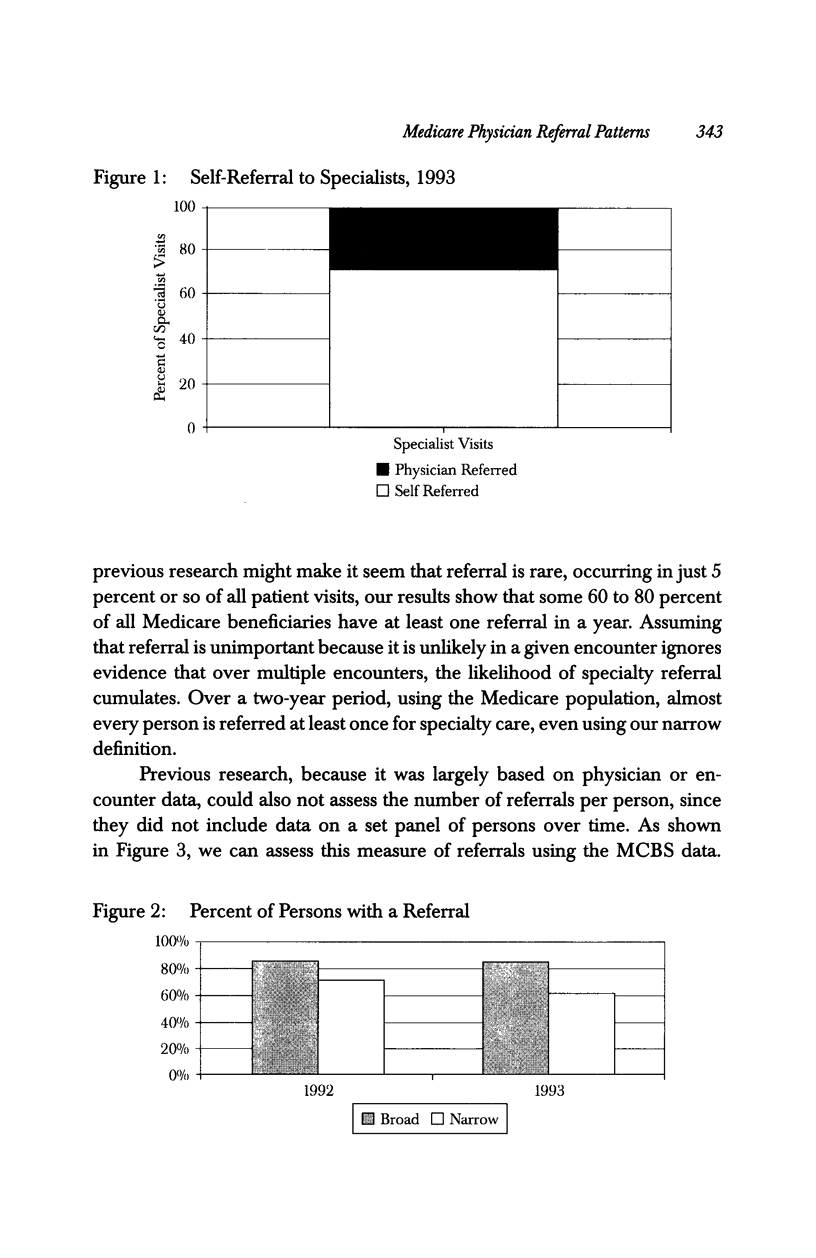
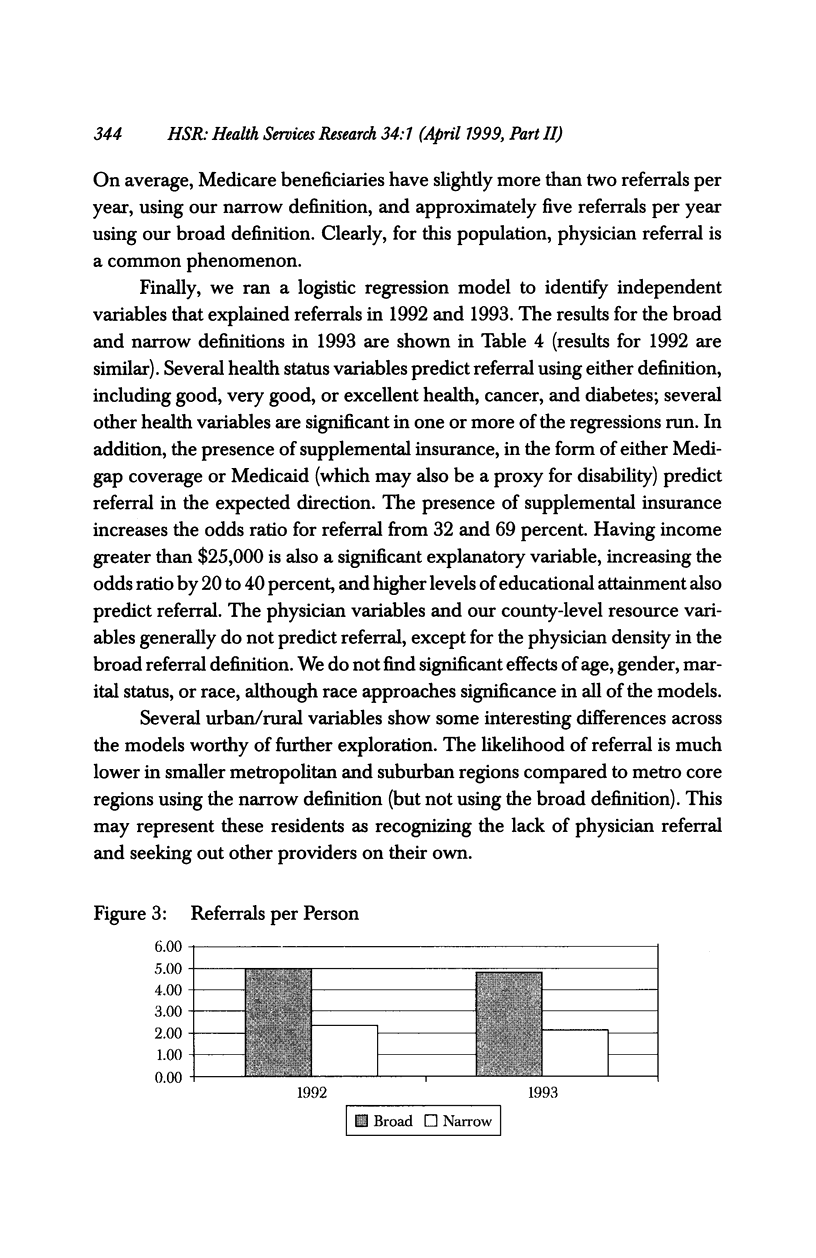
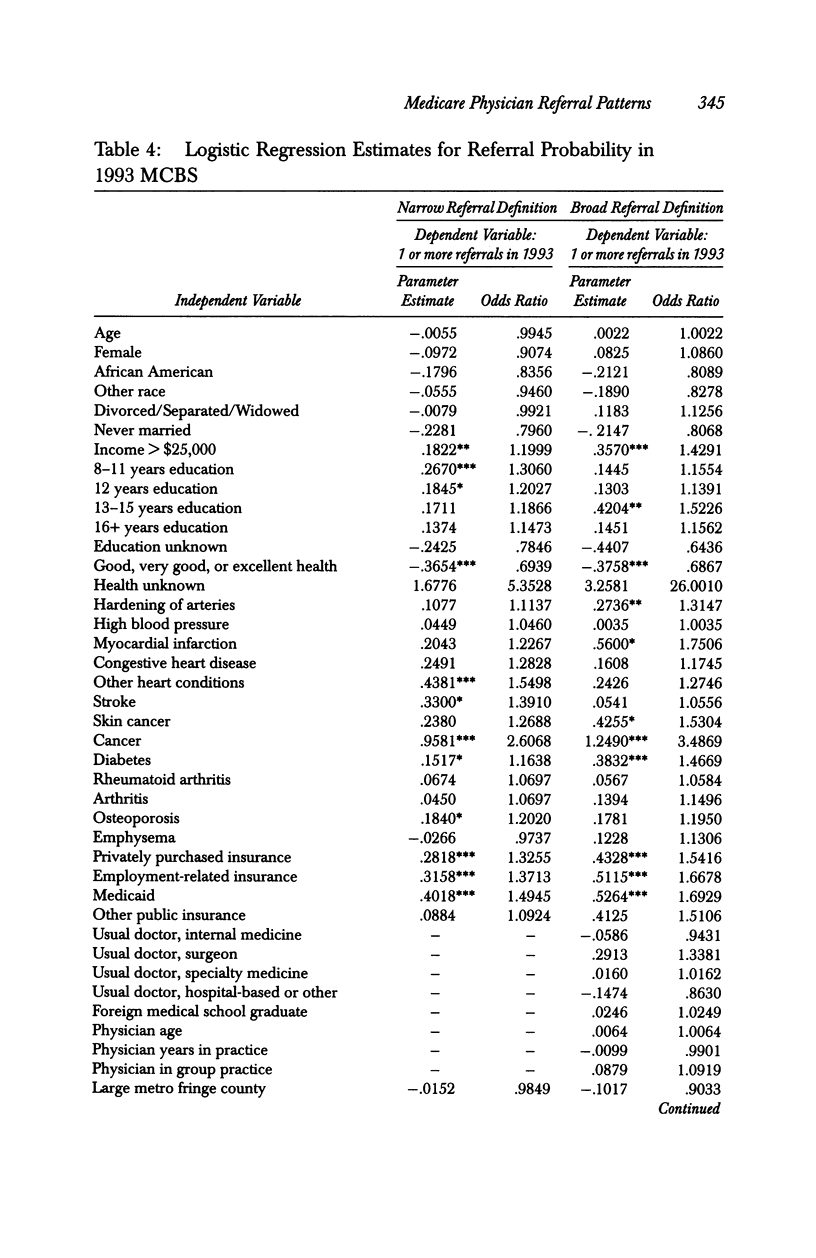
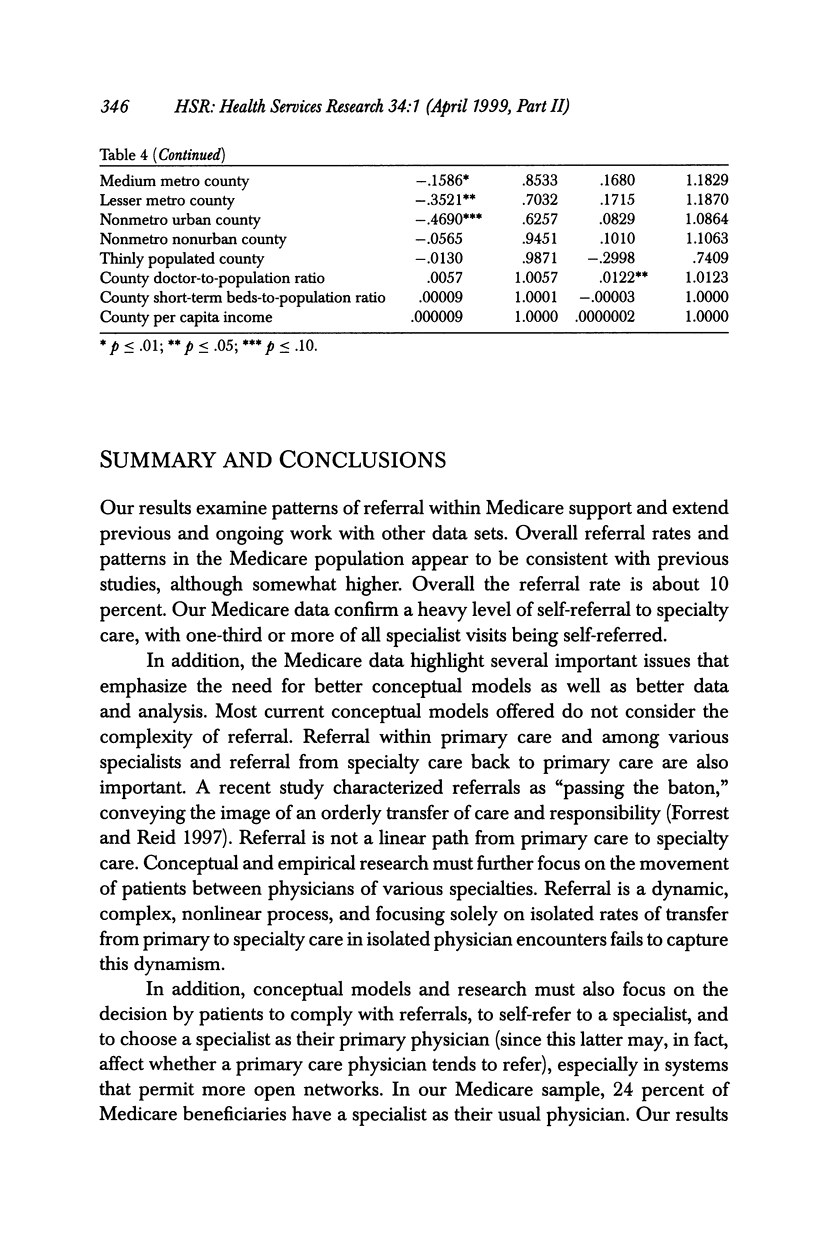
OBJECTIVE: To study patterns of referral between primary and specialty care providers among Medicare beneficiaries and to identify correlates of the probability of referral. DATA SOURCES: The 1992 and 1993 Medicare Current Beneficiary Survey (MCBS), including associated claims data. MCBS data are linked to the Area Resource File (ARF) and the Physician Identification Master Record (PIMR). STUDY DESIGN: This is a retrospective design using cross-sectional descriptive and multivariate correlational analysis. Estimates are made for two years. Key variables include two alternative definitions of referrals, patient socio-demographic and health status, physician characteristics, and county-level descriptors. DATA COLLECTION: The MCBS is a panel survey of a stratified random sample of Medicare beneficiaries begun in 1991. The data are linked to Medicare claims records for survey respondents. The ARF is a health resources data set that contains more than 7,000 variables at the county level, including information on health facilities, health professions, services resources and utilization, and socioeconomic and environmental characteristics. The PIMR is a record of all physicians in the United States and describes their professional characteristics. PRINCIPAL FINDINGS: The overall rate of physician referrals in the MCBS, approximately 10 percent, is higher than that found in prior research, as is the level of self-referral to specialists at about 70 percent. Depending on the dependent variable definition, between 60 and 85 percent of all Medicare beneficiaries had at least one referral, and the average number of referrals per person per year was greater than two. Referrals show a multi-directional pattern rather than a simple pattern of primary to specialty care, with referrals between primary care physicians, referrals between specialists, and referrals from specialty to primary care being not uncommon. Strong predictors of referral include patient health and patient insurance coverage and income. Physician factors do not contribute much to explaining referrals. CONCLUSIONS: Medicare referral patterns are similar to those found in other studies. Patient factors appear to be a more important factor in explaining referrals than was estimated from prior research. Additional research is needed to explain the more complex dynamics of referral patterns.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Forrest C. B., Reid R. J. Passing the baton: HMOs' influence on referrals to specialty care. Health Aff (Millwood) 1997 Nov-Dec;16(6):157–162. doi: 10.1377/hlthaff.16.6.157. [DOI] [PubMed] [Google Scholar]
- Franks P., Clancy C. M. Referrals of adult patients from primary care: demographic disparities and their relationship to HMO insurance. J Fam Pract. 1997 Jul;45(1):47–53. [PubMed] [Google Scholar]
- Glenn J. K., Lawler F. H., Hoerl M. S. Physician referrals in a competitive environment. An estimate of the economic impact of a referral. JAMA. 1987 Oct 9;258(14):1920–1923. [PubMed] [Google Scholar]
- Gonzalez M. L., Rizzo J. A. Physician referrals and the medical market place. Med Care. 1991 Oct;29(10):1017–1027. doi: 10.1097/00005650-199110000-00007. [DOI] [PubMed] [Google Scholar]
- Greenfield S., Nelson E. C., Zubkoff M., Manning W., Rogers W., Kravitz R. L., Keller A., Tarlov A. R., Ware J. E., Jr Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA. 1992 Mar 25;267(12):1624–1630. [PubMed] [Google Scholar]
- Greenfield S., Rogers W., Mangotich M., Carney M. F., Tarlov A. R. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and specialties. Results from the medical outcomes study. JAMA. 1995 Nov 8;274(18):1436–1444. [PubMed] [Google Scholar]
- Grembowski D. E., Cook K., Patrick D. L., Roussel A. E. Managed care and physician referral. Med Care Res Rev. 1998 Mar;55(1):3–31. doi: 10.1177/107755879805500101. [DOI] [PubMed] [Google Scholar]
- Grol R., Whitfield M., De Maeseneer J., Mokkink H. Attitudes to risk taking in medical decision making among British, Dutch and Belgian general practitioners. Br J Gen Pract. 1990 Apr;40(333):134–136. [PMC free article] [PubMed] [Google Scholar]
- Holtgrave D. R., Lawler F., Spann S. J. Physicians' risk attitudes, laboratory usage, and referral decisions: the case of an academic family practice center. Med Decis Making. 1991 Apr-Jun;11(2):125–130. doi: 10.1177/0272989X9101100210. [DOI] [PubMed] [Google Scholar]
- Jollis J. G., DeLong E. R., Peterson E. D., Muhlbaier L. H., Fortin D. F., Califf R. M., Mark D. B. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996 Dec 19;335(25):1880–1887. doi: 10.1056/NEJM199612193352505. [DOI] [PubMed] [Google Scholar]
- McLeod P. J., Tamblyn R. M., Gayton D., Grad R., Snell L., Berkson L., Abrahamowicz M. Use of standardized patients to assess between-physician variations in resource utilization. JAMA. 1997 Oct 8;278(14):1164–1168. [PubMed] [Google Scholar]
- Nutting P. A., Franks P., Clancy C. M. Referral and consultation in primary care: do we understand what we're doing? J Fam Pract. 1992 Jul;35(1):21–23. [PubMed] [Google Scholar]
- Reynolds G. A., Chitnis J. G., Roland M. O. General practitioner outpatient referrals: do good doctors refer more patients to hospital? BMJ. 1991 May 25;302(6787):1250–1252. doi: 10.1136/bmj.302.6787.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneeweiss R., Ellsbury K., Hart L. G., Geyman J. P. The economic impact and multiplier effect of a family practice clinic on an academic medical center. JAMA. 1989 Jul 21;262(3):370–375. [PubMed] [Google Scholar]
- Shortell S. M., Vahovich S. G. Patient referral differences among specialties. Health Serv Res. 1975 Summer;10(2):146–161. [PMC free article] [PubMed] [Google Scholar]
- Sturm R., Wells K. B. How can care for depression become more cost-effective? JAMA. 1995 Jan 4;273(1):51–58. [PubMed] [Google Scholar]