Abstract
Background and Objectives: The assessment of coronary microcirculation may facilitate risk stratification and treatment adjustment. The aim of this study was to evaluate patients’ clinical presentation and treatment following coronary microcirculation assessment, as well as factors associated with an abnormal coronary flow reserve (CFR) and index of microcirculatory resistance (IMR) values. Materials and Results: This retrospective analysis included 223 patients gathered from the national registry of invasive coronary microvascular testing collected between 2018 and 2023. Results: The frequency of coronary microcirculatory assessments in Poland has steadily increased since 2018. Patients with impaired IMR (≥25) were less burdened with comorbidities. Patients with normal IMR underwent revascularisation attempts more frequently (11.9% vs. 29.8%, p = 0.003). After microcirculation testing, calcium channel blockers (CCBs) and angiotensin-converting enzyme inhibitors were added more often for patients with IMR and CFR abnormalities, respectively, as compared to control groups. Moreover, patients with coronary microvascular dysfunction (CMD, defined as CFR and/or IMR abnormality), regardless of treatment choice following microcirculation assessment, were provided with trimetazidine (23.2%) and dihydropyridine CCBs (26.4%) more frequently than those without CMD who were treated conservatively (6.8%) and by revascularisation (4.2% with p = 0.002 and 0% with p < 0.001, respectively). Multivariable analysis revealed no association between angina symptoms and IMR or CFR impairment. Conclusions: The frequency of coronary microcirculatory assessments in Poland has steadily increased. Angina symptoms were not associated with either IMR or CFR impairment. After microcirculation assessment, patients with impaired microcirculation, expressed as either low CFR, high IMR or both, received additional pharmacotherapy treatment more often.
Keywords: coronary flow reserve, coronary microvascular dysfunction, index of microcirculatory resistance, microcirculation
1. Introduction
Epicardial arteries larger than 400 µm in diameter constitute approximately 5% of coronary macro- and microcirculation; the remaining 95% is made up of pre-arterioles, arterioles and capillaries. The term microvascular angina was first introduced into the nomenclature in 1985 by Cannon and Epstein [1]. Structural and functional abnormality of the microvasculature system, also referred to as coronary microvascular dysfunction (CMD), is associated with multiple diseases, as well as infarct size, and overall poor clinical outcomes in many patient subgroups, e.g., those presented with myocardial infarction (MI) [2,3,4,5,6,7,8,9]. However, the largest group of patients are those with chronic coronary syndromes, persistent symptoms and clinical signs of heart ischemia, where there is no evidence of obstructive coronary artery disease based on angiography (INOCA). It is estimated that up to 40% of patients undergoing diagnostic coronary angiography fall into this group of patients [10]. Among women, this may constitute up to 2/3 of patients who have typical ischaemia symptoms without atherosclerotic lesions visible in coronary angiography [11]. Furthermore, it is estimated that up to 1/13 of these people will die within 10 years of the angiography, with the most common cause of hospitalisation being heart failure [12,13]. Additionally, approx. 70–80% of patients with chest pain and no obstructive coronary artery disease (CAD) present evidence of diffuse non-obstructive atherosclerosis, as well as coronary calcifications, in intravascular imaging [14,15]. In 2007, Camici and Crea proposed clinical and pathogenetic classifications of CMD, which, based on a clinical setting, distinguished the following four types of CMD: that which occurs in the absence of myocardial diseases and obstructive CAD, that which occurs in the presence of myocardial diseases, that which occurs in obstructive CAD, and those which are related to iatrogenic etiology [16].
As of now, two primary measures are prevalent in functional microvasculature testing: the coronary flow reserve (CFR) and the index of microcirculatory resistance (IMR). While CFR provides insight into the functions of both epicardial coronary vessels and distal vasculature, IMR offers direct assessment of the microcirculation function. Both measures are recommended by international guidelines as diagnostic methods for identifying patients with CMD, especially in the case of non-obstructive CAD, as confirmed by the normal fractional flow reserve (FFR) [17,18,19]. Cut-off values of 2.0 for CRF and 25 for IMR have been widely adopted [20,21].
In many studies, the importance of routinely assessing microcirculation is emphasised, as it may provide additional insight into a patient’s disease, and can be of additional prognostic value [9,20,22]. However, there are limited data regarding the characteristics of patients who undergo microcirculation testing.
In our study, we aimed to compare clinical characteristics and subsequent decision-making after assessing coronary microvasculature between patients with abnormal microcirculation function and those with normal IMR and CFR values. Moreover, we sought to evaluate factors associated with impaired microvasculature measurements.
2. Materials and Methods
This retrospective study is based on a national registry of invasive coronary microvascular testing (POL-MKW), in which 223 patients have been gathered to date. Data have been collected from eight catheterisation laboratories (CathLabs) in Poland between 2018 and 2023.
2.1. Coronary Angiography and Physiological Examination of Coronary Arteries
The access site, sheath and catheter size, as well as periprocedural anticoagulation use, were per operator preference. Measurements were carried out using a dedicated pressure guide (Abbott PressureWire™ X Guidewire) and the Coroventis CoroFlow Cardiovascular System. Cardiovascular medications were discontinued for 24 h prior to microcirculation assessment. A therapeutic dose of unfractionated heparin was administrated, i.e., 5000 units or 80–100 units per kg during the intervention.
Fractional Flow Reserve (FFR) was calculated as the lowest average Pd/Pa from three consecutive heartbeats during maximal hyperaemia. CFR was calculated as the ratio of mean transit time (Tmn) at rest/hyperaemic Tmn. IMR was calculated from the Pd × Tmn equation determined during hyperaemia. All the calculations mentioned above were carried out automatically by the software. IMR values ≥ 25 and CFR ≤ 2 were adopted as abnormal and defined as CMD. Patients with acute myocardial infarction (at least 72 h after diagnosis and depending on the extent of ischaemia) were excluded from the study. In cases where collateral flow should be taken into account (presence of tight stenosis in the assessed vessel or collaterals to the vessel with chronic total occlusion)—IMR was corrected according to formulas proposed by Yong et al. [23].
2.2. Statistical Analysis
Nominal variables are presented as absolute numbers and percentages. Continuous variables are expressed as means (standard deviation) and medians [first quartile; third quartile], depending on their normality, which was evaluated using the Shapiro–Wilk test. For normally distributed, continuous variables, differences were compared via the Student’s or Welch’s t-tests. In the case of non-parametrical data, the Wilcoxon test was used instead. Categorical variables were compared using Pearson’s chi-squared or Fisher’s exact test if 20% of the cells had an expected count of less than five (Monte Carlo simulation for Fisher’s test using tables of higher dimensions than 2 × 2).
All factors that may have been associated with abnormal IMR and CFR values were adopted in univariable logistic regression models. Based on their results, variables with a p-value < 0.2 were subsequently included in the multivariable model, having risk estimates presented as odds ratios (OR) with 95% confidence intervals (CI). A p-value lower than 0.05 was considered significant. The entire statistical analysis was carried out using the R test, version 4.3.1 (R Core Team (2023). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/ (accessed on: 11 July 2023)).
3. Results
3.1. Catheterisation Laboratories and Years of Study
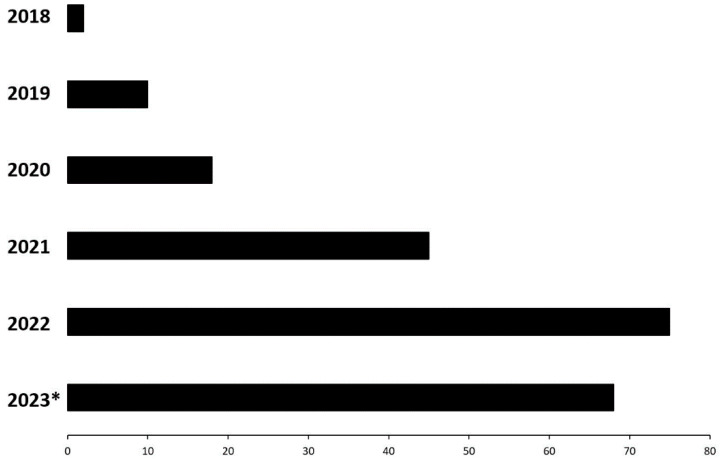
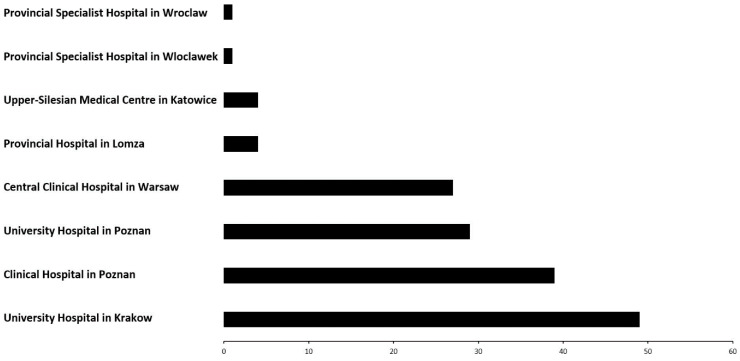
As presented in Figure 1, the frequency of performed coronary microcirculatory assessments using the Coroventis system has increased since 2018, reaching its peak in 2022 (Figure 1). These data are from July 2023; therefore, more assessments are anticipated to be conducted in 2023. Furthermore, the vast majority of assessments were performed at the four dominant centres located in Warsaw, Poznań and Kraków (Figure 2).
Figure 1.
Coronary microcirculatory assessment cases in the last five years. * Data from June 2023.
Figure 2.
Coronary microcirculatory assessment number per CathLab registries in Poland.
3.2. General Characteristics and Concomitant Diseases
We studied 223 patients with a median age of 66.2 [59.9; 71.9], most of whom were males (55%) (Table S1). Patients with abnormal IMR were less likely to have experienced a prior MI (19.3% vs. 42.1%, p < 0.001), prior percutaneous coronary intervention (PCI) (17.9% vs. 43.7%, p < 0.001), and were less often burdened with ischaemic heart disease (53.6% vs. 89.9%, p < 0.001) or thyroid problems (p = 0.04), as compared to the group with normal IMR. However, atrial fibrillation (27.4% vs. 14.9%, p = 0.03) and prior pulmonary embolism/deep venous thrombosis (PE/DVT) (13.1% vs. 3.4%, p = 0.01) were more prevalent in these patients, with the latter also being confirmed in the group with low coronary flow (12.2% vs. 3.5%, p = 0.02, Table S1).
3.3. Clinical State and Main Symptoms
Angina-related symptoms, including shortness of breath, chest pain and palpitations, were significantly more prevalent in the group with either IMR or CFR impairment (Table 1). The distribution of the CCS class differed between patients having normal and impaired IMR, with the latter group demonstrating severe symptoms (Table 1). More detailed data regarding findings from examinations, e.g., echocardiography, are shown in Table S2.
Table 1.
Clinical presentation.
| Variable | Total N = 223 |
CFR ≤ 2 N = 91 |
CFR > 2 N = 117 |
p-Value | IMR ≥ 25 N = 84 |
IMR < 25 N = 121 |
p-Value |
|---|---|---|---|---|---|---|---|
| NYHA class | |||||||
| None | 105 (47.1) | 41 (45.1) | 51 (43.6) | 0.79 | 36 (42.9) | 54 (44.6) | 0.19 |
| I | 29 (13.0) | 10 (11.0) | 19 (16.2) | 7 (8.3) | 22 (18.2) | ||
| II | 63 (28.3) | 27 (29.7) | 34 (29.1) | 27 (32.1) | 33 (27.3) | ||
| III | 21 (9.4) | 11 (12.1) | 10 (8.5) | 12 (14.3) | 9 (7.4) | ||
| IV | 5 (2.2) | 2 (2.2) | 3 (2.6) | 2 (2.4) | 3 (2.5) | ||
| Shortness of breath | 81 (37.5) | 44 (48.4) | 35 (29.9) | 0.01 | 37 (44.0) | 41 (33.9) | 0.14 |
| Chest pain | 148 (68.5) | 70 (76.9) | 71 (61.7) | 0.02 | 64 (77.1) | 75 (62.5) | 0.03 |
| Palpitation/arrhythmia | 34 (15.7) | 16 (17.6) | 17 (14.5) | 0.55 | 19 (22.6) | 13 (10.7) | 0.02 |
| Syncope | 6 (2.8) | 2 (2.2) | 4 (3.4) | 0.47 | 2 (2.4) | 4 (3.3) | 0.52 |
| Prior cardiac arrest | 5 (2.4) | 1 (1.1) | 4 (3.5) | 0.27 | 2 (2.4) | 3 (2.5) | 0.67 |
| CCS class | |||||||
| None | 61 (27.4) | 24 (26.4) | 30 (25.6) | 0.20 | 15 (17.9) | 38 (31.4) | 0.03 |
| I | 30 (13.5) | 8 (8.8) | 21 (17.9) | 8 (9.5) | 21 (17.4) | ||
| II | 94 (42.2) | 39 (42.9) | 50 (42.7) | 44 (52.4) | 43 (35.5) | ||
| III | 37 (16.6) | 19 (20.9) | 16 (13.7) | 17 (20.2) | 18 (14.9) | ||
| IV | 1 (0.5) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 1 (0.8) | ||
| Stable angina symptomatic | 100 (44.8) | 43 (47.3) | 52 (44.4) | 0.69 | 44 (52.4) | 50 (41.3) | 0.12 |
| Unstable angina symptomatic | 36 (16.1) | 20 (22.0) | 14 (12.0) | 0.052 | 17 (20.2) | 67 (79.8) | 0.24 |
Data are presented as counts (percentages). CCS: Canadian Cardiovascular Society; CFR: coronary flow reserve; IMR: index of microcirculatory resistance; NYHA: New York Heart Association.
3.4. Pharmacotherapy
As compared to the group with normal IMR, patients with abnormal IMR had less often taken P2Y12 inhibitors (p = 0.002) or calcium channel blockers (23.2% vs. 39.2%, p = 0.02, Table S3).
3.5. Coronary Angiography
The group with IMR abnormality was characterised by a lower prevalence of intermediate stenosis (30–70%) (41% vs. 73.7%, p < 0.001) and chronic total occlusions (1.2% vs. 9.1%, p = 0.02), as compared to the group with normal IMR. More detailed data are shown in Table 2.
Table 2.
Angiographic findings.
| Variable | Total N = 223 |
CFR ≤ 2 N = 91 |
CFR > 2 N = 117 |
p-Value | IMR ≥ 25 N = 84 |
IMR < 25 N = 121 |
p-Value |
|---|---|---|---|---|---|---|---|
| Angiographic image | |||||||
| - no changes | 32 (15.5) | 11 (12.4) | 20 (17.7) | 0.30 | 12 (14.6) | 19 (16.1) | 0.78 |
| - mild stenosis | 166 (79.8) | 74 (84.1) | 88 (76.5) | 0.18 | 71 (85.4) | 89 (75.4) | 0.08 |
| - intermediate stenosis | 127 (61.1) | 53 (59.6) | 70 (61.4) | 0.79 | 34 (41.0) | 87 (73.7) | <0.001 |
| - significant stenosis | 30 (13.5) | 17 (18.7) | 12 (10.3) | 0.08 | 9 (10.7) | 20 (16.5) | 0.24 |
| - CTO | 12 (5.4) | 5 (5.5) | 7 (6.0) | 0.88 | 1 (1.2) | 11 (9.1) | 0.02 |
| Intermediate stenosis location | |||||||
| - LMCA | 7 (3.1) | 4 (4.4) | 3 (2.6) | 0.70 | 25 (29.8) | 7 (5.8) | 0.04 |
| - LAD | 96 (43.0) | 39 (42.9) | 56 (47.9) | 0.47 | 8 (9.5) | 68 (56.2) | <0.001 |
| - Cx | 26 (11.7) | 15 (16.5) | 9 (7.7) | 0.049 | 8 (9.5) | 16 (13.2) | 0.42 |
| - RCA | 16 (7.2) | 8 (8.8) | 8 (6.8) | 0.60 | 6 (7.1) | 8 (6.6) | 0.45 |
| - Mg | 2 (0.9) | 7 (7.7) | 2 (1.7) | 0.50 | 3 (3.6) | 2 (1.7) | 0.51 |
| - LVB | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | - |
| - RPD | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | - |
| Significant stenosis location | |||||||
| - LMCA | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | - |
| - LAD | 12 (5.4) | 3 (3.3) | 4 (3.4) | 0.17 | 1 (1.2) | 5 (4.1) | 0.35 |
| - Cx | 9 (4.0) | 9 (9.9) | 6 (5.1) | 0.52 | 1 (1.2) | 6 (5.0) | 0.63 |
| - RCA | 12 (5.4) | 1 (1.1) | 3 (2.6) | 0.03 | 0 (0.0) | 11 (9.1) | 0.02 |
| - Mg | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | - |
| - LVB | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | - |
| - RPD | 1 (0.4) | 0 (0.0) | 0 (0.0) | 0.26 | 0 (0.0) | 1 (0.8) | 0.40 |
| CTO location | |||||||
| - LAD | 4 (1.8) | 1 (1.1) | 3 (2.7) | 0.63 | 0 (0.0) | 4 (3.3) | 0.15 |
| - Cx | 1 (0.4) | 4 (4.4) | 1 (0.9) | 1.0 | 0 (0.0) | 1 (0.8) | 1.0 |
| - RCA | 8 (3.6) | 0 (0.0) | 4 (3.4) | 0.73 | 0 (0.0) | 7 (5.8) | 0.15 |
Data are presented as counts (percentages). CFR: coronary flow reserve; CTO: chronic total occlusion; Cx: circumflex (artery); IMR: index of microcirculatory resistance; LAD: left anterior descending (artery); LMCA: left main coronary artery; LVB: left ventricular bypass; Mg: marginal (artery); RCA: right coronary artery; RPD: right posterior descending (artery).
3.6. Coronary Microvascular Circulation Assessment
In the total population, the median CFR was 2.3 [1.6; 3.4], while the median IMR was 20.0 [13.0; 33.0] (Table S4). Patients with abnormal IMR had higher median values of resting full-cycle ratio (RFR) and FFR compared to the group with normal IMR (p < 0.001 and p = 0.006, Table S4). Moreover, lower CFR and higher IMR values were noted among patients with CMD (CFR ≤ 2 and/or IMR ≥ 25) when compared to the group without CMD in both the high and low FFR groups separately (Table S5).
3.7. Treatment Adjustment after Coronary Microcirculation Assessment
Every fifth patient (21.1%) underwent PCI. Patients with normal IMR were more likely to be revascularised than those with impaired IMR (29.8% vs. 11.9%, p = 0.003). We have not observed any differences in PCI rates regarding CFR and CMD (Table 3 and Table S6). Although no significant differences were noted in the conservative treatment adjustment rates, patients with CFR impairment were more often provided with additional angiotensin-converting enzyme inhibitors (ACEI) (13.2% vs. 5.1%, p = 0.04). Those with IMR abnormality were administered both dihydropyridine calcium channel blockers (DHP CCBs) and non-DHP CCBs, in comparison to patients with normal IMR (34.5% vs. 6.6%, p < 0.001 and 3.6% vs. 0%, p = 0.04, respectively, Table 3). What is more, patients with CMD, regardless of treatment choice, had trimetazidine (23.2%) and dihydropyridine CCBs (26.4%) added to pharmacotherapy more frequently than those without CMD, who were treated conservatively (6.8%) and by revascularisation (4.2% with p = 0.002 and 0% with p = 0.0001, respectively, Table S6).
Table 3.
Treatment after coronary microcirculatory assessment.
| Variable | Total N = 223 |
CFR ≤ 2 N = 91 |
CFR > 2 N = 117 |
p-Value | IMR ≥ 25 N = 84 |
IMR < 25 N = 121 |
p-Value |
|---|---|---|---|---|---|---|---|
| PCI | 47 (21.1) | 21 (23.1) | 26 (22.2) | 0.88 | 10 (11.9) | 36 (29.8) | 0.003 |
| PCI within: | |||||||
| LAD | 36 (16.1) | 16 (17.6) | 20 (17.1) | 0.93 | 8 (9.5) | 27 (22.3) | 0.02 |
| LMCA | 1 (0.5) | 1 (1.1) | 0 (0.0) | 0.44 | 0 (0.0) | 1 (0.8) | 0.59 |
| Cx | 9 (4.0) | 3 (3.3) | 6 (5.1) | 0.52 | 2 (2.4) | 7 (5.8) | 0.31 |
| RCA | 6 (2.7) | 4 (4.4) | 2 (1.7) | 0.25 | 0 (0.0) | 6 (5.0) | 0.04 |
| CABG | 5 (2.2) | 3 (3.3) | 2 (1.7) | 0.66 | 1 (1.2) | 4 (3.3) | 0.40 |
| Percutaneous valve intervention | 1 (0.5) | 1 (1.1) | 0 (0.0) | 0.45 | 1 (1.2) | 0 (0.0) | 0.43 |
| Surgical valve intervention | 1 (0.5) | 1 (1.1) | 0 (0.0) | 0.44 | 0 (0.0) | 1 (0.8) | 1.0 |
| Conservative treatment | 197 (88.3) | 78 (85.7) | 104 (88.9) | 0.49 | 78 (92.6) | 101 (83.5) | 0.047 |
| Conservative treatment adjustment | 39 (17.5) | 12 (13.2) | 26 (22.2) | 0.385 | 11 (13.1) | 26 (21.5) | 0.62 |
| Added pharmacotherapy | |||||||
| ACEI | 18 (8.1) | 12 (13.2) | 6 (5.1) | 0.04 | 10 (11.9) | 8 (6.6) | 0.19 |
| BB | 12 (5.4) | 5 (5.5) | 7 (6.0) | 0.88 | 6 (7.1) | 6 (5.0) | 0.51 |
| Nitrate | 12 (5.4) | 3 (3.3) | 9 (7.7) | 0.18 | 4 (4.8) | 8 (6.6) | 0.58 |
| Ranolazine | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | 0 (0.0) | 0 (0.0) | - |
| Ivabradine | 1 (0.4) | 1 (1.1) | 0 (0.0) | 0.26 | 1 (1.2) | 0 (0.0) | 0.23 |
| Trimetazidine | 35 (15.7) | 19 (20.9) | 16 (13.7) | 0.17 | 19 (22.6) | 15 (12.4) | 0.053 |
| CCB DHP | 38 (17.0) | 20 (22.0) | 17 (14.5) | 0.16 | 29 (34.5) | 8 (6.6) | <0.001 |
| CCB NDHP | 4 (1.8) | 3 (3.3) | 1 (0.9) | 0.20 | 3 (3.6) | 0 (0.0) | 0.04 |
Data are presented as counts (percentages). Abbreviations: see Table 2. CABG: coronary artery bypass graft; DHP: dihydropyridine; PCI: percutaneous coronary intervention; NDHP: nondihydropyridine.
3.8. Multivariable Analysis
No angina symptoms were significantly associated with either IMR or CFR impairment. However, it was revealed that intermediate stenosis in the left anterior descending (LAD) artery was connected with a 77.1% lower risk of impaired IMR, whereas intermediate stenosis within the Cx artery was related to an 85.4% decreased risk of impaired CFR. Moreover, hyperlipidaemia was noted as a factor associated with a significantly lower risk of abnormal IMR and CFR at the same time, while coronary non-invasive diagnostic testing was associated with lower risk of abnormal IMR. However, severe valvular disease and longer hospitalisations were linked with a higher risk of impaired IMR, CFR and IMR values, respectively (Table S7).
4. Discussion
In our analysis, we found that the frequency of coronary microcirculatory assessments in Poland has steadily increased. Secondly, patients with either impaired IMR or CFR were generally less burdened with comorbidities. The third major finding of this study is that patients with normal IMR underwent revascularisation attempts more frequently. Fourthly, ACEI, CBBs and DHP CCBs with trimetazidine were added to pharmacotherapy more often after microcirculation testing among patients with low CFR, high IMR and CMD presence, respectively. Last of all, multivariable analysis revealed no association between angina symptoms and IMR or CFR impairment.
In general, the clinical characteristics of patients with CMD are poorly understood, as there is a great variety of underlying pathologies, the understanding of which is limited by the paucity of available scientific evidence. It is nonetheless well-recognised that CMD is often symptomatic and may even account for up to 65% of angina symptoms in patients with normal coronary angiography [20,24,25,26]. What is more, its presence might contribute to a worse improvement of angina symptoms in patients with chronic coronary syndromes [27].
In the conducted study, patients with either impaired CFR or IMR suffered from angina symptoms more frequently; however, such an association was not confirmed in the multivariable model. This may have been driven by the broad group selection, as our research included both patients with epicardial stenoses and with non-obstructive CAD. Nevertheless, in certain studies, it has been reported that CMD does not significantly affect hard outcomes in the case of patent epicardial arteries [28]. However, in the clinical trial conducted by Ford et al. [29], it was concluded that patients with non-obstructive CAD, for whom stratified medical therapy based on invasive coronary function testing was implemented, evinced improvement in terms of angina symptom management.
In our analysis, impaired coronary flow was characterised by different clinical characteristics, including angiographic images, as compared to abnormal IMR. Since CFR is not microvascular-specific and may be affected by resting haemodynamics, some discrepancies are anticipated to emerge between IMR and CFR values. In addition, low coronary flow may enlarge RFR/FFR discrepancy [30]. It was also reported that post-procedural FFR values and coronary flow significantly vary across the IMR value range [31]. Nevertheless, that does not undermine the value of combined measurements regarding microcirculation function. Instead, it indicates the complementary characteristics of these measurements.
Importantly, we observed that patients with normal IMR underwent PCI attempts more often that those with a high IMR. This reflected the fact that, in our study, patients with normal IMR had significantly lower median values of RFR and FFR than those with abnormal IMR. It is self-evident that the angiographic evaluation determines the PCI attempt.
Interestingly, the majority of patients with abnormal IMR in our study were characterised by high FFR (>0.80), which has been a gold standard for functional epicardial coronary stenoses testing [32]. Lee et al. [7] reported that, in this group, patients with low CFR were more likely to experience patient-oriented composite outcomes (POCO; any death, MI, necessity of revascularisation) during the follow-up period, which was confirmed by other authors [33]. Furthermore, patients with the co-impairment of IMR and CFR had the highest POCO. In short, the association between microvascular impairment and a higher risk of cardiovascular events in patients with non-obstructive CAD has been confirmed in multiple studies [34,35,36,37].
In general, specific treatment options for patients with microcirculation abnormalities are limited and in contemporary clinical practice, they target symptom relief and mitigation of epicardial artery stenoses. However, in some studies, it has been suggested that patients with impaired CFR and IMR should receive more aggressive therapy [1]. We noted that, after microcirculation assessments, patients with low coronary flow or high IMR were more often provided with additional medications, i.e., ACEIs and CCBs. It could be anticipated that impaired CFR and IMR are linked to higher ACEI, CCB and statin therapies, as all of them are shown to decrease microvascular tone [26]. In fact, previously conducted clinical trials on microvascular angina were able to report improvements in coronary flow reserve following ACEI therapy as well as in angina symptom control after CCB drug implementation [38,39,40]. Moreover, we also noticed that the group with CMD (CFR ≤ 2 and/or IMR ≥ 25), regardless of treatment choice, had new DHP-CCBs and trimetazidine added to postprocedural pharmacotherapy more often than those without CMD treated conservatively or by PCI, with the latter receiving such medications least often. Trimetazidine, similarly to ranolazine, is usually given to patients as part of angina symptom management [41]. However, in a single blinded, randomised study conducted by Ilic et al. [42], it was shown that trimetazidine given to a group undergoing PCI also reduced microvascular dysfunction. This was expressed as a postprocedural IMR value. Nevertheless, it has to be emphasized that, due to the low FFR group involvement in the study and a lack of association between angina symptoms and CFR or IMR impairment, treatment choices may have been primarily driven by the presence or absence of obstructive atherosclerosis.
What is more, we noted that Cx and LAD artery location of intermediate stenosis, hyperlipidaemia and cardiac non-invasive diagnostic testing were associated with a decreased risk of microcirculation measurement abnormalities, whereas longer hospitalisation and severe valve disease increased the risk of impaired IMR and CFR. In other studies, it was reported that Killip class, delayed hospitalisation from symptom onset, peak troponin-I levels and multivessel disease were also linked to abnormal IMR [43]. Considering the risk factors, LDL-C, older age, female sex, hypertension, diabetes, previous MI and chronic renal failure were also shown to have associations with developing CMD and lower CFR [28,37,44].
In conclusion, although there is yet a great data paucity regarding targeted therapy for patients with CMD and their clinical characteristics, our analysis allows us to reveal contemporary treatment choices in clinical practice and certain associations between patients’ condition and microcirculation abnormality and, therefore, hypotheses are generated that require further investigation in prospective studies.
Limitations
This analysis, based on a national registry, has several limitations. Most importantly, it lacks a randomised design due to its retrospective characteristics. Hence, the results have to be considered solely as hypothesis-generating. Furthermore, due to the registry-based design, certain data were not available.
5. Conclusions
The frequency of coronary microcirculatory assessments in Poland has been steadily increasing. Angina symptoms were not associated with either IMR or CFR impairment. After microcirculation assessment, patients with impaired microcirculation, expressed as either low CFR, high IMR or both, received additional pharmacotherapy treatment more often.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/medicina60020277/s1: Figure S1: Demographic and clinical characteristics Table S1: Examination findings; Table S3: Pharmacotherapy; Table S4. Coronary microcirculatory assessment: Table S5. Coronary microcirculatory assessment with regard to FFR; Table S6: Treatment after coronary microcirculatory assessment; Table S7: Factors associated with abnormal coronary microcirculation based on IMR and CFR measures—multivariable analysis.
Author Contributions
Conceptualization and Methodology, R.J. and S.B.; Formal Analysis, R.J. and W.S.; Data Curation, R.J.; Investigation, R.J., Ł.K., M.T., W.W. (Wojciech Wańha), W.W. (Wojciech Wojakowski), M.G., W.S., G.J.H., B.C., R.K., B.G., J.L., T.P., P.W., M.R., S.S.-S., M.J., T.R., M.D. and S.B.; Resources, S.B.; Supervision, and Project Administration, R.J., W.W. (Wojciech Wańha), T.P., S.B., W.W., B.G. and J.L.; Visualization: W.S. and R.J.; Writing—Original Draft Preparation, R.J., W.S., Ł.K. and M.D.; Writing—Review and Editing: R.J., Ł.K., M.T., W.W. (Wojciech Wańha), W.W. (Wojciech Wojakowski), M.G., W.S., G.J.H., B.C., R.K., B.G., J.L., T.P., P.W., M.R., S.S.-S., M.J., T.R., M.D., W.S. and S.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and UJCM Ethics Committee (protocol code 1072.6120.27.2022 and date: 23 March 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon a justified request.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding Statement
No funding was received to conduct this study. The Registry was partially founded by Abbott Poland and UJCM.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cannon R.O., Epstein S.E. ‘Microvascular angina’ as a cause of chest pain with angio-graphically normal coronary arteries. Am. J. Cardiol. 1988;61:1338–1343. doi: 10.1016/0002-9149(88)91180-0. [DOI] [PubMed] [Google Scholar]
- 2.Kelshiker M.A., Seligman H., Howard J.P., Rahman H., Foley M., Nowbar A.N., A Rajkumar C., Shun-Shin M.J., Ahmad Y., Sen S., et al. Coronary flow reserve and cardiovascular outcomes: A systematic review and meta-analysis. Eur. Heart J. 2021;43:1582–1593. doi: 10.1093/eurheartj/ehab775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Godo S., Suda A., Takahashi J., Yasuda S., Shimokawa H. Coronary Microvascular Dysfunction. Arter. Thromb. Vasc. Biol. 2021;41:1625–1637. doi: 10.1161/ATVBAHA.121.316025. [DOI] [PubMed] [Google Scholar]
- 4.Ozyurek B.A., Bozbas S.S., Eroglu S., Eyuboglu F.O. Coronary flow reserve is impaired in patients with obstructive sleep apnea. Ann. Thorac. Med. 2017;12:272–277. doi: 10.4103/atm.ATM_195_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radhakrishnan A., Pickup L.C., Price A.M., Law J.P., Edwards N.C., Steeds R.P., Ferro C.J., Townend J.N. Coronary microvascular dysfunction: A key step in the development of uraemic cardiomyopathy? Heart. 2019;105:1302–1309. doi: 10.1136/heartjnl-2019-315138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radhakrishnan A., Pickup L.C., Price A.M., Law J.P., McGee K.C., Fabritz L., Senior R., Steeds R.P., Ferro C.J., Townend J.N. Coronary microvascular dysfunction is associated with degree of anaemia in end-stage renal disease. BMC Cardiovasc. Disord. 2021;21:211. doi: 10.1186/s12872-021-02025-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee J.M., Jung J.-H., Hwang D., Park J., Fan Y., Na S.-H., Doh J.-H., Nam C.-W., Shin E.-S., Koo B.-K. Coronary Flow Reserve and Microcirculatory Resistance in Patients with Intermediate Coronary Stenosis. J. Am. Coll. Cardiol. 2016;67:1158–1169. doi: 10.1016/j.jacc.2015.12.053. [DOI] [PubMed] [Google Scholar]
- 8.De Bruyne B., Hersbach F., Pijls N.H., Bartunek J., Bech J.-W., Heyndrickx G.R., Gould K.L., Wijns W. Abnormal Epicardial Coronary Resistance in Patients with Diffuse Atherosclerosis but “Normal” Coronary Angiography. Circulation. 2001;104:2401–2406. doi: 10.1161/hc4501.099316. [DOI] [PubMed] [Google Scholar]
- 9.McGeoch R., Watkins S., Berry C., Steedman T., Davie A., Byrne J., Hillis S., Lindsay M., Robb S., Dargie H., et al. The Index of Microcirculatory Resistance Measured Acutely Predicts the Extent and Severity of Myocardial Infarction in Patients with ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc. Interv. 2010;3:715–722. doi: 10.1016/j.jcin.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Patel M.R., Peterson E.D., Dai D., Brennan J.M., Redberg R.F., Anderson H.V., Brindis R.G., Douglas P.S. Low Diagnostic Yield of Elective Coronary Angiography. N. Engl. J. Med. 2010;362:886–895. doi: 10.1056/NEJMoa0907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei J., Cheng S., Merz C.N.B. Coronary Microvascular Dysfunction Causing Cardiac Ischemia in Women. JAMA. 2019;322:2334–2335. doi: 10.1001/jama.2019.15736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bairey Merz C.N., Pepine C.J., Walsh M.N., Fleg J.L. Ischemia and No Obstructive Coronary Artery Disease (INOCA): Developing Evidence-Based Therapies and Research Agenda for the Next Decade. Circulation. 2017;135:1075–1092. doi: 10.1161/CIRCULATIONAHA.116.024534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kenkre T.S., Malhotra P., Johnson B.D., Handberg E.M., Thompson D.V., Marroquin O.C., Rogers W.J., Pepine C.J., Merz C.N.B., Kelsey S.F., et al. Ten-Year Mortality in the WISE Study (Women’s Ischemia Syndrome Evaluation) Circ. Cardiovasc. Qual. Outcomes. 2017;10:e003863. doi: 10.1161/CIRCOUTCOMES.116.003863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khuddus M.A., Pepine C.J., Handberg E.M., Merz C.N.B., Sopko G., Bavry A.A., Denardo S.J., McGORRAY S.P., Smith K.M., Sharaf B.L., et al. An Intravascular Ultrasound Analysis in Women Experiencing Chest Pain in the Absence of Obstructive Coronary Artery Disease: A Substudy from the National Heart, Lung and Blood Institute–Sponsored Women’s Ischemia Syndrome Evaluation (WISE) J. Interv. Cardiol. 2010;23:511–519. doi: 10.1111/j.1540-8183.2010.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee B.-K., Lim H.-S., Fearon W.F., Yong A.S., Yamada R., Tanaka S., Lee D.P., Yeung A.C., Tremmel J.A. Invasive Evaluation of Patients with Angina in the Absence of Obstructive Coronary Artery Disease. Circulation. 2015;131:1054–1060. doi: 10.1161/CIRCULATIONAHA.114.012636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Camici P.G., Crea F. Coronary microvascular dysfunction. N. Engl. J. Med. 2007;356:830–840. doi: 10.1056/NEJMra061889. [DOI] [PubMed] [Google Scholar]
- 17.Fearon W.F., Kobayashi Y. Invasive Assessment of the Coronary Microvasculature. Circ. Cardiovasc. Interv. 2017;10:e005361. doi: 10.1161/CIRCINTERVENTIONS.117.005361. [DOI] [PubMed] [Google Scholar]
- 18.Knuuti J., Wijns W., Saraste A., Capodanno D., Barbato E., Funck-Brentano C., Prescott E., Storey R.F., Deaton C., Cuisset T., et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 19.Fearon W.F., Balsam L.B., Farouque H.M.O., Robbins R.C., Fitzgerald P.J., Yock P.G., Yeung A.C. Novel Index for Invasively Assessing the Coronary Microcirculation. Circulation. 2003;107:3129–3132. doi: 10.1161/01.CIR.0000080700.98607.D1. [DOI] [PubMed] [Google Scholar]
- 20.Díez-Delhoyo F., Gutiérrez-Ibañes E., Loughlin G., Sanz-Ruiz R., Vázquez-Álvarez M.E., Sarnago-Cebada F., Angulo-Llanos R., Casado-Plasencia A., Elízaga J., Diáz F.F.A. Coronary physiology assessment in the catheterization laboratory. World J. Cardiol. 2015;7:525–538. doi: 10.4330/wjc.v7.i9.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kobayashi Y., Fearon W.F. Invasive Coronary Microcirculation Assessment. Circ. J. 2014;78:1021–1028. doi: 10.1253/circj.CJ-14-0364. [DOI] [PubMed] [Google Scholar]
- 22.Geng Y., Wu X., Liu H., Zheng D., Xia L. Index of microcirculatory resistance: State-of-the-art and potential applications in computational simulation of coronary artery disease. J. Zhejiang Univ. B. 2022;23:123–140. doi: 10.1631/jzus.B2100425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yong A.S., Ho M., Shah M.G., Ng M.K., Fearon W.F. Coronary Microcirculatory Resistance Is Independent of Epicardial Stenosis. Circ. Cardiovasc. Interv. 2012;5:103–108. doi: 10.1161/CIRCINTERVENTIONS.111.966556. [DOI] [PubMed] [Google Scholar]
- 24.Lanza G.A., Crea F., Kaski J.C. Clinical outcomes in patients with primary stable microvascular angina: Is the jury still out? Eur. Heart J. Qual. Care Clin. Outcomes. 2019;5:283–291. doi: 10.1093/ehjqcco/qcz029. [DOI] [PubMed] [Google Scholar]
- 25.Radico F., Zimarino M., Fulgenzi F., Ricci F., Di Nicola M., Jespersen L., Chang S.M., Humphries K.H., Marzilli M., De Caterina R. Determinants of long-term clinical outcomes in patients with angina but without obstructive coronary artery disease: A systematic review and meta-analysis. Eur. Heart J. 2018;39:2135–2146. doi: 10.1093/eurheartj/ehy185. [DOI] [PubMed] [Google Scholar]
- 26.Marinescu M.A., Löffler A.I., Ouellette M., Smith L., Kramer C.M., Bourque J.M. Coronary Microvascular Dysfunction, Microvascular Angina, and Treatment Strategies. JACC Cardiovasc. Imaging. 2015;8:210–220. doi: 10.1016/j.jcmg.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niewiara Ł., Kleczyński P., Szolc P., Guzik B., Diachyshyn M., Jelonek M., Handzlik J., Żmudka K., Legutko J. The change of angina levels in patients with chronic coronary syndromes and coronary microcirculatory dysfunc-tion—A prospective study with 24 months follow-up. Postep. Kardiol Interwencyjnej. 2023;19:318–325. doi: 10.5114/aic.2023.133806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahn J.-M., Zimmermann F.M., Johnson N.P., Shin E.-S., Koo B.-K., Lee P.H., Park D.-W., Kang S.-J., Lee S.-W., Kim Y.-H., et al. Fractional flow reserve and pressure-bounded coronary flow reserve to predict outcomes in coronary artery disease. Eur. Hearth J. 2017;38:1980–1989. doi: 10.1093/eurheartj/ehx139. [DOI] [PubMed] [Google Scholar]
- 29.Ford T.J., Stanley B., Sidik N., Good R., Rocchiccioli P., McEntegart M., Watkins S., Eteiba H., Shaukat A., Lindsay M., et al. 1-Year Outcomes of Angina Management Guided by Invasive Coronary Function Testing (CorMicA) JACC Cardiovasc. Interv. 2020;13:33–45. doi: 10.1016/j.jcin.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Legutko J., Niewiara L., Guzik B., Szolc P., Podolec J., Nosal M., Diachyshyn M., Zmudka K., Kleczynski P. The impact of coronary microvascular dysfunction on the discordance between fractional flow reserve and resting full-cycle ratio in patients with chronic coronary syndromes. Front. Cardiovasc. Med. 2022;9:1003067. doi: 10.3389/fcvm.2022.1003067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murai T., Lee T., Yonetsu T., Isobe M., Kakuta T. Influence of microvascular resistance on fractional flow reserve after successful percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 2015;85:585–592. doi: 10.1002/ccd.25499. [DOI] [PubMed] [Google Scholar]
- 32.Legutko J., Kleczyński P., Dziewierz A., Rzeszutko L., Dudek D. Adenosine intracoronary bolus dose escalation versus intravenous infusion to induce maximum coronary hypere-mia for fractional flow reserve assessment. Kardiol Pol. 2019;77:610–617. doi: 10.5603/KP.a2019.0060. [DOI] [PubMed] [Google Scholar]
- 33.Meuwissen M., Chamuleau S.A., Siebes M., de Winter R.J., Koch K.T., Dijksman L.M., Berg A.J.v.D., Tijssen J.G., Spaan J.A., Piek J.J. The prognostic value of combined intracoronary pressure and blood flow velocity measurements after deferral of percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 2008;71:291–297. doi: 10.1002/ccd.21331. [DOI] [PubMed] [Google Scholar]
- 34.Murthy V.L., Naya M., Taqueti V.R., Foster C.R., Gaber M., Hainer J., Dorbala S., Blankstein R., Rimoldi O., Camici P.G., et al. Effects of Sex on Coronary Microvascular Dysfunction and Cardiac Outcomes. Circulation. 2014;129:2518–2527. doi: 10.1161/CIRCULATIONAHA.113.008507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dhawan S.S., Corban M.T., Nanjundappa R.A., Eshtehardi P., McDaniel M.C., Kwarteng C.A., Samady H. Coronary microvascular dysfunction is associated with higher frequency of thin-cap fibroatheroma. Atherosclerosis. 2012;223:384–388. doi: 10.1016/j.atherosclerosis.2012.05.034. [DOI] [PubMed] [Google Scholar]
- 36.Taqueti V.R., Hachamovitch R., Murthy V.L., Naya M., Foster C.R., Hainer J., Dorbala S., Blankstein R., Di Carli M.F. Global Coronary Flow Reserve Is Associated with Adverse Cardiovascular Events Independently of Luminal Angiographic Severity and Modifies the Effect of Early Revascularization. Circulation. 2015;131:19–27. doi: 10.1161/CIRCULATIONAHA.114.011939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mayala H.A., Yan W., Jing H., Shuang-Ye L., Gui-Wen Y., Chun-Xia Q., Xiao-Li L., Zhao-Hui W. Clinical characteristics and biomarkers of coronary microvascular dysfunction and obstructive coronary artery disease. J. Int. Med. Res. 2019;47:6149–6159. doi: 10.1177/0300060519859134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pauly D.F., Johnson B.D., Anderson R.D., Handberg E.M., Smith K.M., Cooper-DeHoff R.M., Sopko G., Sharaf B.M., Kelsey S.F., Merz C.N.B., et al. In women with symptoms of cardiac ischemia, nonobstructive coronary arteries, and microvascular dysfunction, angiotensin-converting enzyme inhibition is associated with improved microvascular function: A double-blind randomized study from the National Heart, Lung and Blood Institute Women’s Ischemia Syndrome Evaluation (WISE) Am. Hearth J. 2011;162:678–680. doi: 10.1016/j.ahj.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Motz W., Strauer B.E., Kozàkovà M., Palombo C., Pratali L., Pittella G., Galetta F., L’Abbate A., Nunez E., Hosoya K., et al. Improvement of Coronary Flow Reserve After Long-term Therapy with Enalapril. Hypertension. 1996;27:1031–1038. doi: 10.1161/01.HYP.27.5.1031. [DOI] [PubMed] [Google Scholar]
- 40.Cannon R.O., Watson R.M., Rosing D.R., Epstein S.E. Efficacy of calcium channel blocker therapy for angina pectoris resulting from small-vessel coronary artery disease and abnormal vasodilator reserve. Am. J. Cardiol. 1985;56:242–246. doi: 10.1016/0002-9149(85)90842-2. [DOI] [PubMed] [Google Scholar]
- 41.Taqueti V.R., Di Carli M.F. Coronary Microvascular Disease Pathogenic Mechanisms and Therapeutic Options. J. Am. Coll. Cardiol. 2018;72:2625–2641. doi: 10.1016/j.jacc.2018.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ilic I., Timcic S., Milosevic M., Boskovic S., Odanovic N., Furtula M., Dobric M., Aleksandric S., Otasevic P. The imPAct of Trimetazidine on MicrOcirculation after Stenting for stable coronary artery disease (PATMOS study) Front. Cardiovasc. Med. 2023;10:1112198. doi: 10.3389/fcvm.2023.1112198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jang J.H., Lee M.J., Ko K.Y., Park J.H., Baek Y.S., Sung-Woo K., Shin S.-H., Woo S.-I., Kim D.-H., Suh Y.-J., et al. Mechanical and Pharmacological Revascularization Strategies for Prevention of Microvascular Dysfunction in ST-Segment Elevation Myocardial Infarction: Analysis from Index of Microcirculatory Resistance Registry Data. J. Interv. Cardiol. 2020;2020:5036396. doi: 10.1155/2020/5036396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Niewiara L., Kleczyński P., Guzik B., Szolc P., Baran J., Podolec J., Diachyshyn M., Żmudka K., Legutko J. Impaired coronary flow reserve in patients with poor type 2 diabetes control: Preliminary results from prospective microvascular dysfunction registry. Cardiol J. 2022 doi: 10.5603/CJ.a2022.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon a justified request.