Abstract
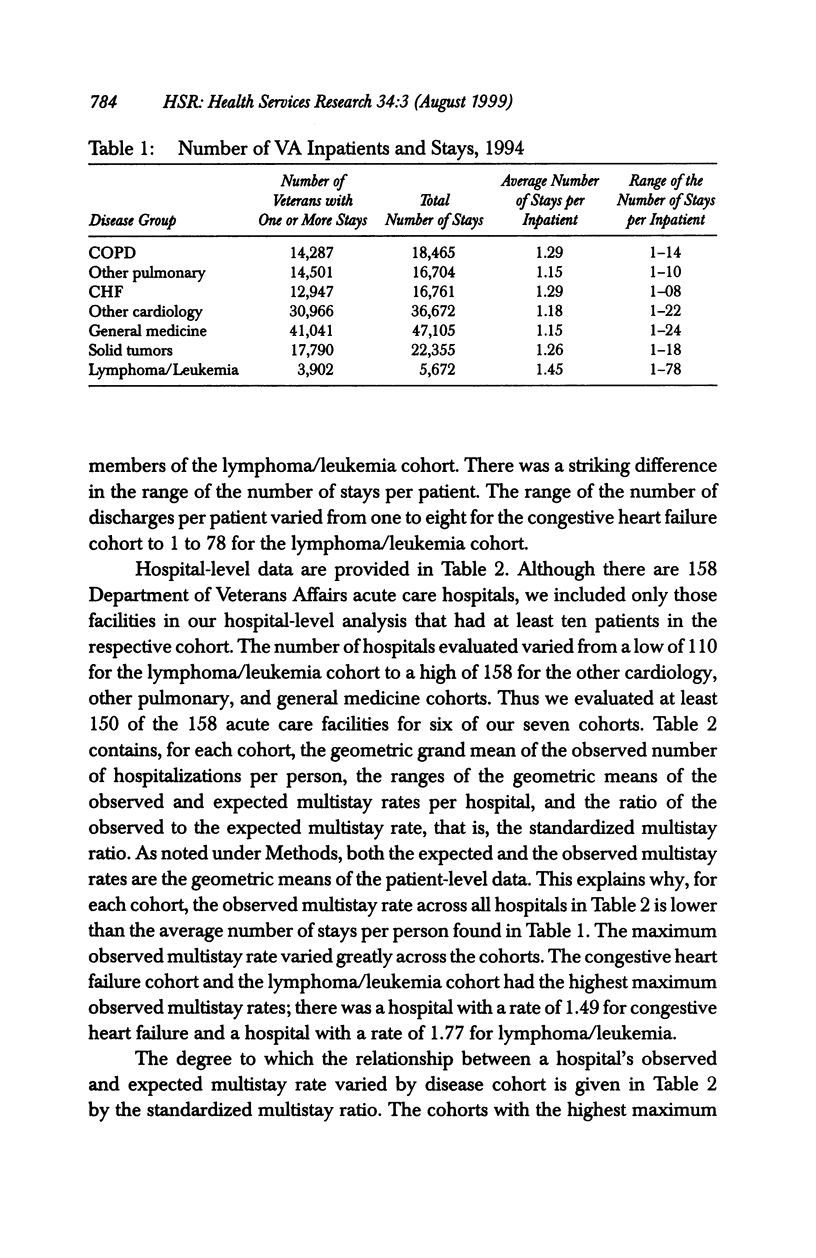
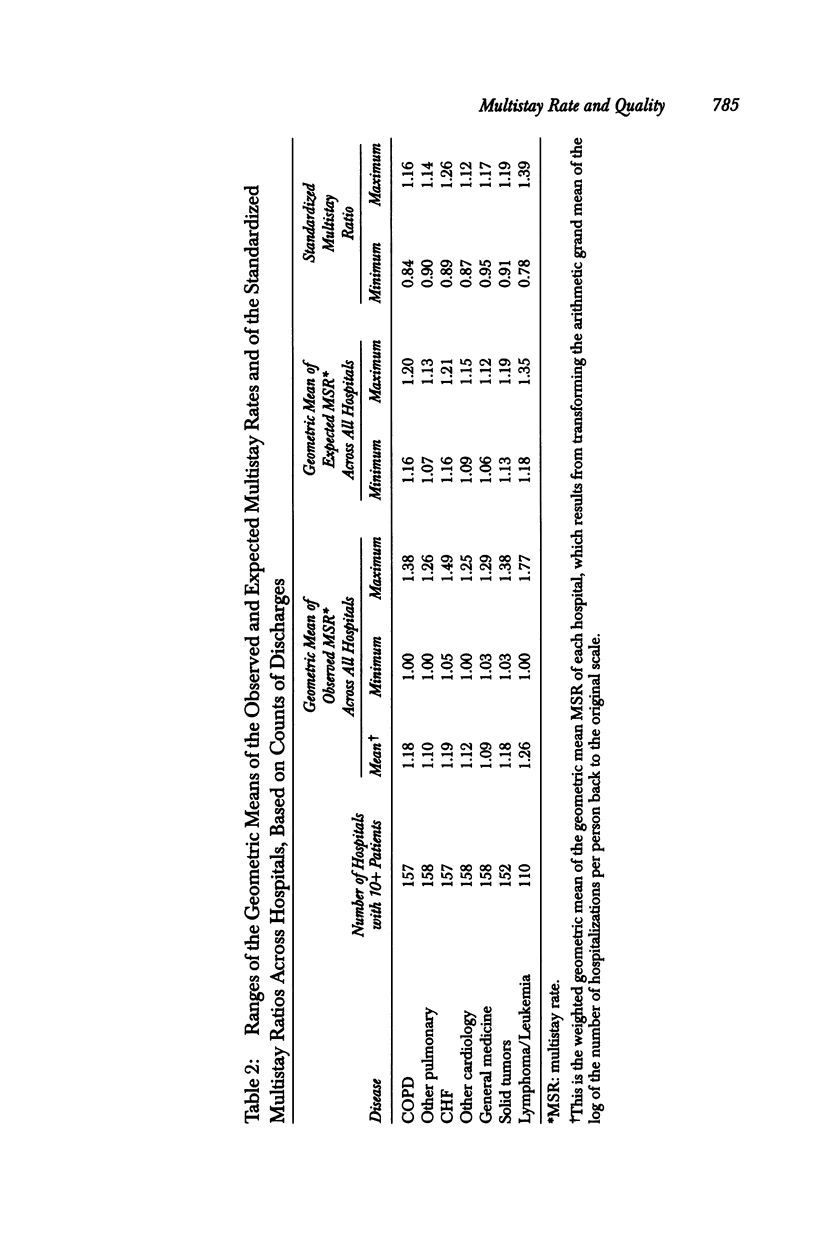
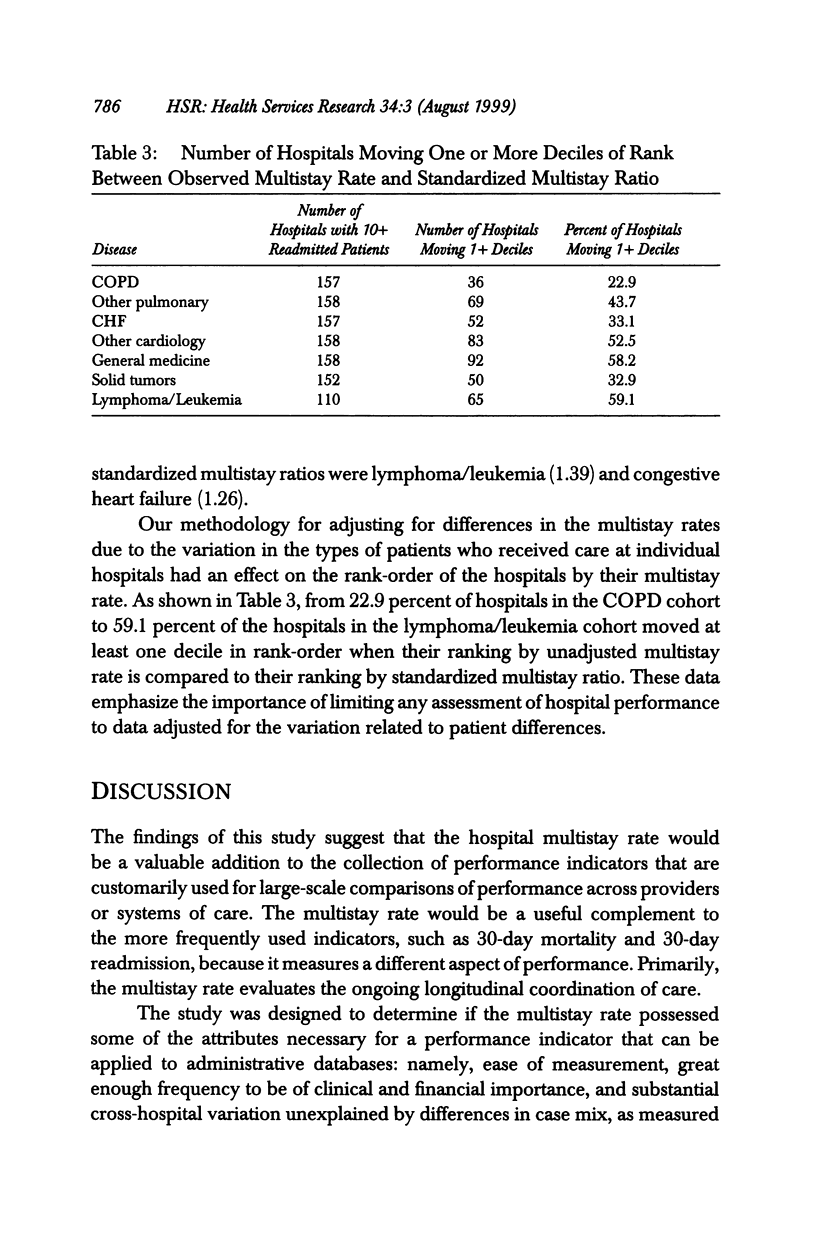
OBJECTIVES: To evaluate the hospital multistay rate to determine if it has the attributes necessary for a performance indicator that can be applied to administrative databases. DATA SOURCES/STUDY SETTING: The fiscal year 1994 Veterans Affairs Patient Treatment File (PTF), which contains discharge data on all VA inpatients. STUDY DESIGN: Using a retrospective study design, we assessed cross-hospital variation in (a) the multistay rate and (b) the standardized multistay ratio. A hospital's multistay rate is the observed average number of hospitalizations for patients with one or more hospital stays. A hospital's standardized multistay ratio is the ratio of the geometric mean of the observed number of hospitalizations per patient to the geometric mean of the expected number of hospitalizations per patient, conditional on the types of patients admitted to that hospital. DATA COLLECTION/EXTRACTION METHODS: Discharge data were extracted for the 135,434 VA patients who had one or more admissions in one of seven disease groups. PRINCIPAL FINDINGS: We found that 17.3 percent (28,300) of the admissions in the seven disease categories were readmissions. The average number of stays per person (multistay rate) for an average of seven months of follow-up ranged from 1.15 to 1.45 across the disease categories. The maximum standardized multistay ratio ranged from 1.12 to 1.39. CONCLUSIONS: This study has shown that the hospital multistay rate offers sufficient ease of measurement, frequency, and variation to potentially serve as a performance indicator.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ashton C. M., Ferguson J. A., Goldacre M. J. In-patient workload in medical specialties: 2. Profiles of individual diagnoses from linked statistics. QJM. 1995 Sep;88(9):661–672. [PubMed] [Google Scholar]
- Ashton C. M., Weiss T. W., Petersen N. J., Wray N. P., Menke T. J., Sickles R. C. Changes in VA hospital use 1980-1990. Med Care. 1994 May;32(5):447–458. doi: 10.1097/00005650-199405000-00004. [DOI] [PubMed] [Google Scholar]
- Ashton C. M., Wray N. P. A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med. 1996 Dec;43(11):1533–1541. doi: 10.1016/s0277-9536(96)00049-4. [DOI] [PubMed] [Google Scholar]
- Fleming C., Fisher E. S., Chang C. H., Bubolz T. A., Malenka D. J. Studying outcomes and hospital utilization in the elderly. The advantages of a merged data base for Medicare and Veterans Affairs hospitals. Med Care. 1992 May;30(5):377–391. doi: 10.1097/00005650-199205000-00001. [DOI] [PubMed] [Google Scholar]
- Goldacre M. J., Ferguson J. A. In-patient workload in medical specialties: 1. Demographic profiles and time trends from linked statistics. QJM. 1995 Sep;88(9):649–659. [PubMed] [Google Scholar]
- Hillman A. L., Pauly M. V., Kerstein J. J. How do financial incentives affect physicians' clinical decisions and the financial performance of health maintenance organizations? N Engl J Med. 1989 Jul 13;321(2):86–92. doi: 10.1056/NEJM198907133210205. [DOI] [PubMed] [Google Scholar]
- Knickman J. R., Foltz A. M. A statistical analysis of reasons for East-West differences in hospital use. Inquiry. 1985 Spring;22(1):45–58. [PubMed] [Google Scholar]
- Luft H. S., Garnick D. W., Mark D. H., Peltzman D. J., Phibbs C. S., Lichtenberg E., McPhee S. J. Does quality influence choice of hospital? JAMA. 1990 Jun 6;263(21):2899–2906. [PubMed] [Google Scholar]
- Weissman J. S., Gatsonis C., Epstein A. M. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992 Nov 4;268(17):2388–2394. [PubMed] [Google Scholar]
- Wennberg J. E., Barnes B. A., Zubkoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci Med. 1982;16(7):811–824. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E., Freeman J. L., Shelton R. M., Bubolz T. A. Hospital use and mortality among Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1989 Oct 26;321(17):1168–1173. doi: 10.1056/NEJM198910263211706. [DOI] [PubMed] [Google Scholar]
- Wray N. P., Peterson N. J., Souchek J., Ashton C. M., Hollingsworth J. C. Application of an analytic model to early readmission rates within the Department of Veterans Affairs. Med Care. 1997 Aug;35(8):768–781. doi: 10.1097/00005650-199708000-00003. [DOI] [PubMed] [Google Scholar]
- Zook C. J., Moore F. D. High-cost users of medical care. N Engl J Med. 1980 May 1;302(18):996–1002. doi: 10.1056/NEJM198005013021804. [DOI] [PubMed] [Google Scholar]


