Abstract
Background and Objective: Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread all over the world. To assess the influence of the COVID-19 pandemic on emergency medical services (EMS) for vulnerable patients transported by ambulance. Materials and Methods: This study was a retrospective, descriptive study with a study period from 1 January 2019 to 31 December 2021 using the Osaka Emergency Information Research Intelligent Operation Network (ORION) system. We included all pediatric patients, pregnant women, and elderly patients ≥ 65 years of age transported by ambulance in Osaka Prefecture. The main outcome of this study was difficult-to-transport cases. We calculated the rate of difficult-to-transport cases under several conditions. Results: For the two year-long periods of 1 January 2019 to 31 December 2019 and 1 January 2021 to 31 December 2021, a total of 887,647 patients were transported to hospital by ambulance in Osaka Prefecture. The total number of vulnerable patients was 579,815 (304,882 in 2019 and 274,933 in 2021). Multivariate logistic regression analysis showed that difficult-to-transport cases were significantly more frequent in 2021 than in 2019. Difficult-to-transport cases were significantly less frequent in the vulnerable population than in the non-vulnerable population (adjusted odds ratio 0.81, 95% confidence interval 0.80–0.83; p < 0.001). Conclusion: During the pandemic (2021), difficult-to-transport cases were more frequent compared to before the pandemic (2019); however, vulnerable patients were not the cause of difficulties in obtaining hospital acceptance for transport.
Keywords: COVID-19, child, elderly patient, difficult-to-transport case, pregnant woman
1. Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and was first identified in Wuhan, China, in December 2019. Since then, the COVID-19 outbreak has spread all over the world [1]. The World Health Organization (WHO) declared COVID-19 a pandemic on 11 March 2020.
A previous study showed the impact of the COVID-19 pandemic on emergency medical services (EMS) systems in Osaka City, Japan [2]. Compared to 2018 or 2019, the proportion of cases experiencing difficulty in obtaining hospital acceptance in Osaka Prefecture among patients transported by ambulance due to acute disease was increased in 2020 [3,4]. However, few reports about the proportion experiencing difficulty with hospital acceptance were available in 2021, and to the best of our knowledge, no studies on the impact of the COVID-19 pandemic on EMS systems for vulnerable patients including pediatric patients, pregnant patients, and elderly patients have been reported [5].
Difficulty in obtaining hospital acceptance for the transfer of vulnerable patients (difficult-to-transport cases) has been a problem in public healthcare systems, not only in Osaka Prefecture but throughout Japan [6]. Previous studies for pediatric patients and pregnant patients revealed that there were few barriers of the healthcare system for emergency transportation before and after the COVID-19 pandemic, [3,4]. However, there were difficult-to-transport cases for elderly patients because they had a lot of comorbidities. Vulnerable populations, particularly elderly people, have made up increasingly large proportions of the global population, and transportation by ambulance has been increasing [7,8]. In addition, elderly patients are more likely to develop COVID-19 and experience more critical or mortal conditions than the general population [9,10]. Previous studies have revealed that vulnerable patients other than the elderly were not associated with difficult-to-transport cases in 2020 compared with 2018 or 2019 [3,4]. As the number of COVID-19 patients was small in the first half of 2020, comparisons between before and during the COVID-19 pandemic need to be made using 2019 and 2021 data. Three waves (the third, fourth, and fifth waves) of the COVID-19 outbreak occurred in 2021, and difficult-to-transport cases became a problem and caused a medical crisis in Osaka Prefecture in 2021.
This study aimed to assess the influence of the COVID-19 pandemic on the EMS system by comparing the pre-pandemic year of 2019 and the post-pandemic year of 2021, with a focus on vulnerable patients transported by ambulance in Osaka Prefecture.
2. Methods
2.1. Study Design and Setting
This study was a retrospective, descriptive study with a study period from 1 January 2019 to 31 December 2019 and from 1 January 2021 to 31 December 2021 using the Osaka Emergency Information Research Intelligent Operation Network (ORION) system [11]. Osaka Prefecture, the largest metropolitan community in western Japan, has a population of about 8.8 million and a total area of 1905 km2. To assess the influence of the COVID-19 pandemic on the EMS system, we focused on vulnerable patients transported by ambulance in Osaka Prefecture. Pediatric patients were divided into four age groups: infants, 0 years; toddlers, 1–4 years; children, 5–9 years; and adolescents, 10–14 years [4]. We defined “women of childbearing age” as female patients aged 15–44 years [12]. We used the presumptive diagnosis and final diagnosis for patients who were admitted, using the International Classification of Diseases, 10th revision (ICD-10) [13]. The present study defined patients with pregnancy-related issues (pregnant patients) as ICD-10 codes O00–O99 and P00–P96. We also classified elderly patients according to the Japan Gerontological Society: pre-old, 65–74 years; old, 75–89 years; and super-old, ≥90 years [14]. We collected “COVID-19” data as ICD-10 code U07.1, and “COVID-19 suspected” data (if the presence of the virus was not confirmed) as U07.2.
This study excluded patients who were not transported to a hospital. We also excluded patients who were transported in 2020, because only 92 COVID-19 patients were encountered between January and June 2020, and we wanted to examine an entire year influenced by COVID-19. Ambulance records in Osaka Prefecture are considered administrative records, so the need to obtain informed consent from participants was waived because the data were anonymous. This study was approved by the Ethics Committee of Osaka Prefectural Government (Osaka City, Japan). Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines were used to design and report the results of this study, and the Reporting of Studies Conducted using Observational Routinely Collected Health Data (RECORD) statement was also used to design and report the results of this study [15,16].
2.2. The Emergency Medical Service (EMS) System in Japan
When emergency patients call for EMS at the scene, on-scene EMS personnel assess the patient’s condition and then transport the patient to a hospital that can accept and treat the patient [4]. Only after obtaining permission from the selected hospital via a phone call can ambulances transport the patient to the hospital [4]. All expenses are covered by local governments, and there is no charge to the patient for care and transportation [4]. Recently, the number of cases of emergency patients’ transportation to a hospital by EMS has been increasing and exceeding the hospital capacity [4]. Therefore, there has been increasing cases of refusal to provide emergency transportation.
2.3. The ORION System
The Osaka prefectural government developed and introduced the ORION system as an information system for emergency patients that uses a smartphone application for hospital selection by on-scene EMS personnel. The ORION system collects all ambulance records. Medical institutions obtain information on the diagnoses and outcomes of patients transported there, and the ORION system has merged these data with ambulance records, including smartphone application data, since January 2015.
2.4. Data Collection and Quality Control
Data were uniformly collected using specific data collection forms and included the reason for the ambulance call, location of the accident, time of day, day of the week, and tools used, in addition to age, sex, and ICD-10 code. The details of the situation, including the name of the fire department, the accident type, the date of ambulance dispatch, a detailed time course before hospital arrival (time of call, ambulance dispatch, arrival at the scene, patient communication, patient’s condition in the ambulance, time of departure from the scene, and time of hospital arrival), and patient information, were recorded in text form. These data were completed by EMS personnel, then transferred to the information center in the Osaka Municipal Fire Department. To ensure the quality of the data, data sheets showing incomplete information were re-submitted to the relevant EMS personnel for correction.
2.5. Availability of Data and Materials
The datasets used in the current study are available from the corresponding author on reasonable request.
2.6. Outcomes
The primary outcome of this study was difficulty in obtaining hospital acceptance for transfer of a patient. Cases where this occurred (difficult-to-transport cases) were defined, according to the guidelines of the Fire and Disaster Management Agency [17], as those cases in which the interval from arrival at the scene to departure from the scene was longer than 30 min or cases for which ambulance crews needed to make four or more phone calls to hospitals before obtaining hospital acceptance. Disposition at the emergency department (ED), such as emergency admission, discharge to home, transfer to another hospital, or death in the ED, was also collected.
2.7. Data Analysis
We calculated the numbers of patients transported by ambulance due to any cause for the year from 1 January to 31 December 2021. For the purposes of comparison, the numbers of patients transported by ambulance for the same reasons for the year from 1 January to 31 December 2019 were also collected. In addition, we used logistic regression analysis to calculate the rate of difficulty with hospital acceptance for patients in the two year-long periods studied, then calculated the crude odds ratio (OR) for each year for difficult-to-transport cases along with the 95% confidence interval (CI), with 2019 as the reference. The OR and 95%CI of difficult-to-transport cases according to month (as compared with June), sex, weekends (as compared with weekdays), nighttime (17:00–09:00) (as compared with daytime), and each category of vulnerability were estimated using multivariate analyses. These variables were chosen based on the previous studies [3,4].
All data were statistically analyzed using SPSS version 25.0 software (IBM Corp., Armonk, NY, USA) or STATA (version 16.1; Stata Corp., College Station, TX, USA). All tests were two-tailed, with values of p < 0.05 considered statistically significant.
3. Results
Baseline Characteristics
For the two year-long periods of 1 January 2019 to 31 December 2019 and 1 January 2021 to 31 December 2021, a total of 948,248 patients were transported to hospitals by ambulance in Osaka Prefecture, Japan. Of these, 887,647 were enrolled in the present study, after excluding 60,601 patients transferred to a different hospital. Each year, 468,699 patients in 2019 and 418,950 patients in 2021 were transported to hospitals by ambulance (Table 1). The total number of pediatric patients (0–14 years old) was 65,107 (7.3%; 37,547 (8.0%) in 2019 and 27,560 (6.6%) in 2021; p < 0.001). The total number of women of childbearing age (15–44 years old) was 79,335 (8.9%; 43,105 (9.2%) in 2019 and 36,230 (8.6%) in 2021; p < 0.001). In addition, the total number of pregnant women was 1644 (0.2%; 943 (0.2%) in 2019 and 701 (0.2%) in 2021; p < 0.001). The total number of elderly patients ≥ 65 years was 513,124 (57.8%; 266,428 (56.8) in 2019 and 246,550 (59.4%) in 2021). Table 1 shows other baseline characteristics of patients transported to hospital by ambulance in Osaka Prefecture.
Table 1.
Demographic characteristics of transported patients.
| Year | 2019 | 2021 | Total | p-Value |
|---|---|---|---|---|
| Number of patients | 468,697 | 418,950 | 887,647 | <0.001 |
| Age, median (IQR) | 70.0 (38) | 72.0 (37) | <0.001 | |
| Sex (male), % | 236,661 (50.5) | 212,458 (50.7) | 449,119 (50.6) | 0.04 |
| Pediatric patients, % | 37,547 (8.0) | 27,560 (6.6) | 65,107 (7.3) | <0.001 |
| Age category of children | <0.001 | |||
| Infants (0 y), % | 3375 (9.0) | 2612 (9.5) | 5987 (9.2) | |
| Toddlers (1–4 y), % | 18,891 (50.3) | 14,081 (51.1) | 32,972 (50.6) | |
| Children (5–9 y), % | 8480 (22.6) | 5668 (20.6) | 14,148 (21.7) | |
| Adolescents (10–14 y), % | 6801 (18.1) | 5199 (18.9) | 12,000 (18.4) | |
| Adult patients (15–64 y), % | 164,722 (35.1) | 144,694 (34.5) | 309,416 (34.9) | <0.001 |
| Women of childbearing age (15–44 y), % | 43,105 (9.2) | 36,230 (8.6) | 79,335 (8.9) | <0.001 |
| Pregnant women, % | 943 (0.2) | 701 (0.2) | 1644 (0.2) | <0.001 |
| Elderly patients, % | 266,428 (56.8) | 246,550 (59.4) | 513,124 (57.8) | <0.001 |
| Age category of elderly | <0.001 | |||
| Pre-old (65–74 y), % | 73,062 (27.4) | 63,249 (25.6) | 136,311 (26.6) | |
| Old (75–89 y), % | 160,666 (60.3) | 148,448 (60.2) | 309,114 (60.2) | |
| Super-old (≥90 y), % | 32,700 (12.3) | 34,999 (14.2) | 67,699 (13.2) |
Pediatric patients, 0–14 years; adult patients, 15–64 years; elderly patients, >65 years. Statistical analyses were performed using the χ2 test for categorical variables and the Kruskal–Wallis test for continuous variables. Abbreviation: IQR, interquartile range.
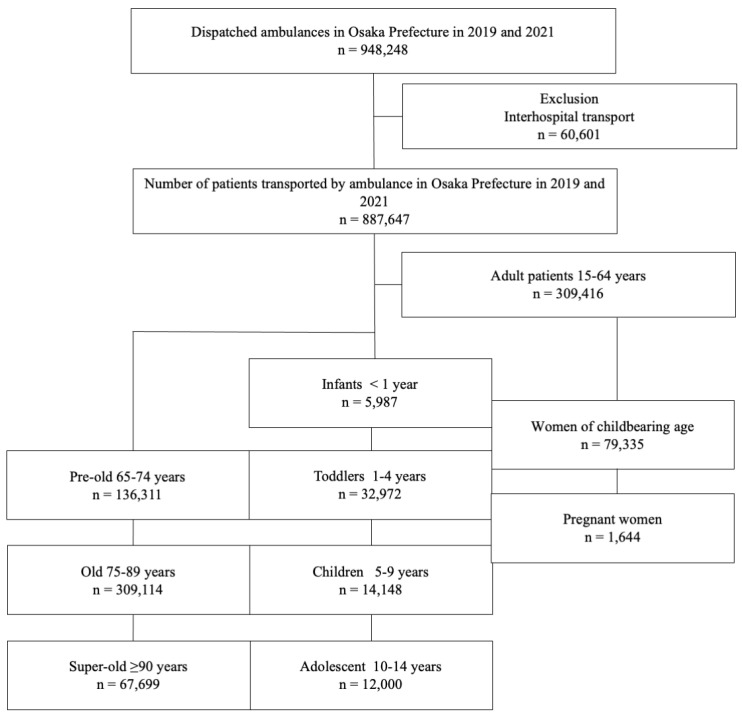
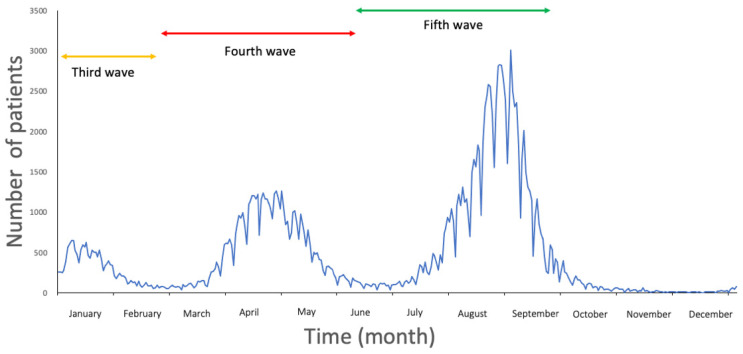
Figure 1 displays the flow diagram for this study. Figure 2 shows newly diagnosed COVID-19 cases in Osaka Prefecture, which as of the time of writing had experienced five waves of infection during the COVID-19 pandemic (the first and second waves in 2020 were omitted).
Figure 1.
Patient flow in this study. All pediatric patients <15 years of age were divided into four groups by age. All female patients 15–44 years old were divided into those of childbearing age and those who were pregnant. All elderly patients ≥ 65 years of age were divided into three groups by age.
Figure 2.
Newly diagnosed COVID-19 cases in Osaka Prefecture, Japan, in 2021. Three waves (third, fourth, and fifth waves) of the COVID-19 pandemic occurred in 2021.
Table 2 shows difficult-to-transport cases categorized according to vulnerable patients, pediatric patients, women of childbearing age, pregnant women, and elderly patients, comparing 2019 with 2021. All proportions in each category showed an increase in difficult-to-transport cases in 2021 compared with 2019. All numbers of difficult-to-transport cases except in children (5–9 y) were increased in 2021 compared with 2019.
Table 2.
Difficult-to-transport cases among pediatric patients, women of childbearing age, pregnant women, and elderly patients in 2019 and 2021.
| 2019 | Not Difficult-to-Transport Cases | Difficult-to-Transport Cases | All |
|---|---|---|---|
| Infants (0 y), % | 3349 (99.2) | 26 (0.8) | 3375 (9.0) |
| Toddlers (1–4 y), % | 18,751 (99.3) | 140 (0.7) | 18,891 (50.3) |
| Children (5–9 y), % | 8338 (98.3) | 142 (1.7) | 8,480 (22.6) |
| Adolescents (10–14 y), % | 6676 (98.2) | 125 (1.8) | 6801 (18.1) |
| Total | 37,114 (98.9) | 433 (1.2) | 37,547 |
| 2021 | Not difficult-to-transport cases | Difficult-to-transport cases | All |
| Infants (0 y), % | 2572 (98.5) | 40 (1.5) | 2612 (9.5) |
| Toddlers (1–4 y), % | 13,901 (98.7) | 180 (1.3) | 14,081 (51.1) |
| Children (5–9 y), % | 5548 (97.9) | 120 (2.1) | 5668 (20.6) |
| Adolescents (10–14 y), % | 5071 (97.5) | 128 (2.5) | 5199 (18.9) |
| Total | 27,092 (98.3) | 468 (1.7) | 27,560 |
| Women of childbearing age (15–44 y), % | 41,602 (96.5) | 1503 (3.5) | 43,105 (9.2) |
| Pregnant women, % | 931 (98.7) | 12 (1.3) | 943 (0.2) |
| 2021 | Not difficult-to-transport cases | Difficult-to-transport cases | All |
| Women of childbearing age (15–44 y), % | 34,123 (94.2) | 2107 (5.8) | 36,230 (8.6) |
| Pregnant women, % | 681 (97.2) | 20 (2.9) | 701 (0.2) |
| Pre-old (65–74 y), % | 71,158 (97.4) | 1904 (2.6) | 73,062 (27.4) |
| Old (75–89 y), % | 156,936 (97.7) | 3730 (2.3) | 160,666 (60.3) |
| Super-old (≥90 y), % | 31,806 (97.3) | 894 (2.7) | 32,700 (12.3) |
| Total | 259,900 (97.6) | 6528 (2.5) | 266,428 |
| 2021 | Not difficult-to-transport cases | Difficult-to-transport cases | All |
| Pre-old (65–74 y), % | 60,320 (95.4) | 2929 (4.6) | 63,249 (25.6) |
| Old (75–89 y), % | 140,982 (95.0) | 7466 (5.0) | 148,448 (60.2) |
| Super-old (≥90 y), % | 32,838 (93.8) | 2161 (6.2) | 34,999 (14.2) |
| Total | 234,140 (94.9) | 12,556 (5.1) | 246,696 |
Table 3 shows disposition at the ED among vulnerable patients, pediatric patients, women of childbearing age, pregnant women, and elderly patients. All proportions for admission to the hospital following initial arrival at the ED except those for children (5–9 y) and the super-old (≥90 y) were increased in 2021 compared with 2019. Both the number and proportion of deaths in the ED among women of childbearing age and elderly patients were increased in 2021 compared with 2019.
Table 3.
Disposition at the emergency department among pediatric patients, women of childbearing age, pregnant women, and elderly patients.
| Pediatric Patients | |||||
|---|---|---|---|---|---|
| 2019 | Infants (0 y), % |
Toddlers (1–4 y), % |
Children (5–9 y), % |
Adolescents (10–14 y), % |
Total, % |
| Admission, % | 650 (19.3) | 3103 (16.4) | 1410 (16.6) | 1023 (15.0) | 6186 (16.5) |
| Home, % | 2682 (79.5) | 15,719 (83.2) | 7020 (82.8) | 5722 (84.1) | 31,143 (82.9) |
| Transfer, % | 21 (0.6) | 55 (0.3) | 48 (0.6) | 48 (0.7) | 172 (0.5) |
| Death, % | 21 (0.6) | 14 (0.1) | 2 (0) | 8 (0.1) | 45 (0.1) |
| No show, % | 1 (0) | 0 | 0 | 0 | 1 (0) |
| Total | 3375 | 18,891 | 8480 | 6801 | 37,547 |
| 2021 | Infants (0 y), % |
Toddlers (1–4 y), % |
Children (5–9 y), % |
Adolescents (10–14 y), % |
Total, % |
| Admission, % | 498 (19.3) | 2429 (17.3) | 929 (16.4) | 908 (17.5) | 4764 (17.3) |
| Home, % | 2074 (79.4) | 11,595 (82.4) | 4702 (83.0) | 4245 (81.7) | 22,616 (82.1) |
| Transfer, % | 27 (1.0) | 53 (0.4) | 36 (0.6) | 41 (0.8) | 157 (0.6) |
| Death, % | 12 (0.5) | 4 (0) | 1 (0) | 5 (0) | 22 (0.1) |
| No show, % | 1 (0) | 0 | 0 | 0 | 1 (0) |
| Total | 2612 | 14,081 | 5668 | 5199 | 27,560 |
| Women of childbearing age and pregnant women | |||||
| 2019 | Pregnant women, % | Women of childbearing age (15–44 y), % | |||
| Admission, % | 547 (58.0) | 6938 (16.1) | |||
| Home, % | 391 (41.5) | 35,807 (83.1) | |||
| Transfer, % | 5 (0.5) | 283 (0.7) | |||
| Death, % | 0 | 66 (0.2) | |||
| No show, % | 0 | 11 (0.0) | |||
| Total | 943 | 43,105 | |||
| 2021 | Pregnant women, % | Women of childbearing age (15–44 y), % | |||
| Admission, % | 418 (59.6) | 6086 (16.8) | |||
| Home, % | 274 (39.1) | 29,777 (82.2) | |||
| Transfer, % | 9 (1.3) | 250 (0.7) | |||
| Death, % | 0 | 111 (0.3) | |||
| No show, % | 0 | 6 (0.0) | |||
| Total | 943 | 36,230 | |||
| Elderly patients | |||||
| 2019 | Pre-old (65–74 y), % |
Old (75–89 y), % |
Super-old (≥90 y), % |
Total, % | |
| Admission, % | 31,161 (42.7) | 80,713 (50.2) | 20,128 (61.6) | 132,002 (49.6) | |
| Home, % | 39,904 (54.6) | 74,514 (46.4) | 11,162 (34.1) | 125,580 (47.1) | |
| Transfer, % | 1163 (1.6) | 2991 (1.9) | 593 (1.8) | 4747 (1.8) | |
| Death, % | 827 (1.1) | 2443 (1.5) | 816 (2.5) | 4086 (1.5) | |
| No show, % | 7 (0) | 5 (0) | 1 (0) | 13 (0) | |
| Total | 73,062 | 160,666 | 32,700 | 266,428 | |
| 2021 | Pre-old (65–74 y), % | Old (75–89 y), % | Super-old (≥90 y), % | Total, % | |
| Admission, % | 29,369 (46.4) | 77,541 (52.2) | 21,529 (61.5) | 128,439 (52.1) | |
| Home, % | 31,761 (50.2) | 64,981 (43.8) | 11,677 (33.4) | 108,419 (44.0) | |
| Transfer, % | 1163 (1.8) | 2991 (2.0) | 733 (2.1) | 4887 (2.0) | |
| Death, % | 952 (1.5) | 2927 (2.0) | 1057 (3.0) | 4936 (2.0) | |
| No show, % | 4 (0) | 8 (0) | 3 (0) | 15 (0) | |
| Total | 63,249 | 148,448 | 34,999 | 246,696 | |
Table 4 shows univariate logistic regression analysis of difficult-to-transport cases among pediatric patients, women of childbearing age, pregnant women, elderly patients, and vulnerable patients, with 2019 as the reference. The results showed that difficult-to-transport cases were significantly more frequent in 2021 than in 2019, except for children (5–9 y). Difficult-to-transport cases in 2021 among non-vulnerable patients were also significantly higher than in 2019 (adjusted OR 1.28, 95%CI 1.26–1.30; p < 0.001), but the adjusted OR was higher for vulnerable patients than for non-vulnerable patients (adjusted OR 1.46, 95%CI 1.44–1.48; p < 0.001).
Table 4.
Univariate logistic regression analysis of difficult-to-transport cases among pediatric patients, women of childbearing age, pregnant women, elderly patients, and vulnerable patients as a variable.
| 2021 vs. 2019 (Reference) | |||||
|---|---|---|---|---|---|
| Odds Ratio | 95%CI | p-Value | |||
| Infants (0 y) | 1.42 | 1.10 | – | 1.81 | 0.006 |
| Toddlers (1–4 y) | 1.32 | 1.18 | – | 1.47 | <0.001 |
| Children (5–9 y) | 1.13 | 1.00 | – | 1.27 | 0.056 |
| Adolescents (10–14 y) | 1.16 | 1.03 | – | 1.32 | 0.019 |
| Women of childbearing age (15–44 y) | 1.31 | 1.26 | – | 1.35 | <0.001 |
| Pregnant women | 1.51 | 1.05 | – | 2.17 | 0.025 |
| Pre-old (65–74 y) | 1.35 | 1.31 | – | 1.39 | <0.001 |
| Old (75–89 y) | 1.49 | 1.46 | – | 1.52 | <0.001 |
| Super-old (≥90 y) | 1.53 | 1.47 | – | 1.59 | <0.001 |
| Non-vulnerable patients | 1.28 | 1.26 | – | 1.30 | <0.001 |
| Vulnerable patients | 1.46 | 1.44 | – | 1.48 | <0.001 |
Table 5 shows multivariate logistic regression analysis of difficult-to-transport cases among all patients (pediatric patients, pregnant women, elderly patients, and vulnerable population as variables). Year, month, sex, weekends (compared with weekdays), and nighttime (17:00–09:00) (compared with daytime) were used as covariates. Adjusted ORs for difficult-to-transport cases among children (adjusted OR 0.33, 95%CI 0.31–0.35) and pregnant women (adjusted OR 0.48, 95%CI 0.34–0.69) were negative. The adjusted OR for difficult-to-transport cases of elderly patients was not significant (adjusted OR 1.01, 95%CI 0.99–1.03; p = 0.403), but elderly status represented a factor independently associated with increased risk of categorization as a difficult-to-transport case (adjusted OR 1.11, 95%CI 1.08–1.14, p < 0.001) in 2021 (Table S2). Difficult-to-transport cases showed a significantly lower frequency in the vulnerable population than in the non-vulnerable population (adjusted OR 0.81, 95%CI 0.80–0.83; p < 0.001). Supplemental tables show other results relevant to the main results. Being an adult patient (>15 and <65 years of age) was independently associated with increased risk of categorization as a difficult-to-transport case (adjusted OR 1.22, 95%CI 1.20–1.25; p < 0.001), regardless of study period (Table S1). COVID-19 (including suspected cases) was independently associated with increased risk of categorization as difficult-to-transport cases in all patients, regardless of variables. The highest adjusted OR for difficult-to-transport cases among vulnerable patients was nighttime (17:00–09:00). July and August were not associated with difficult-to-transport cases in 2019 but were significantly associated with difficult-to-transport cases in 2021 (Table S2).
Table 5.
Multivariate logistic regression analysis of difficult-to-transport cases among all patients (pediatric patients, pregnant women, elderly patients, and vulnerable population as a variable).
| Pediatric Patients as a Variable | |||||
|---|---|---|---|---|---|
| Odds Ratio | 95%CI | p-Value | |||
| Year | |||||
| 2019 | Reference | ||||
| 2021 | 1.39 | 1.37 | – | 1.40 | <0.001 |
| Female (compared with male) | 0.91 | 0.89 | – | 0.93 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.87 | 1.78 | – | 1.98 | <0.001 |
| February | 1.52 | 1.44 | – | 1.61 | <0.001 |
| March | 1.24 | 1.17 | – | 1.32 | <0.001 |
| April | 1.64 | 1.56 | – | 1.74 | <0.001 |
| May | 1.59 | 1.50 | – | 1.68 | <0.001 |
| July | 1.00 | 0.94 | – | 1.06 | 0.963 |
| August | 1.28 | 1.21 | – | 1.35 | <0.001 |
| September | 1.27 | 1.20 | – | 1.35 | <0.001 |
| October | 1.01 | 0.95 | – | 1.07 | 0.851 |
| November | 1.01 | 0.95 | – | 1.07 | 0.773 |
| December | 1.06 | 1.00 | – | 1.13 | 0.04 |
| Weekends (compared with weekdays) | 1.19 | 1.16 | – | 1.22 | <0.001 |
| Nighttime (17:00–09:00) (compared with daytime) | 2.55 | 2.49 | – | 2.61 | <0.001 |
| Children (compared with adult > 15 y) | 0.33 | 0.31 | – | 0.35 | <0.001 |
| COVID-19 (including suspected cases) | 1.38 | 1.29 | – | 1.46 | <0.001 |
| Pregnant women as a variable | |||||
| Odds ratio | 95%CI | p-value | |||
| Year | |||||
| 2019 | Reference | ||||
| 2021 | 1.39 | 1.38 | – | 1.41 | <0.001 |
| Female (compared with male) | 0.93 | 0.91 | – | 0.95 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.91 | 1.81 | – | 2.01 | <0.001 |
| February | 1.55 | 1.47 | – | 1.65 | <0.001 |
| March | 1.27 | 1.20 | – | 1.34 | <0.001 |
| April | 1.66 | 1.57 | – | 1.75 | <0.001 |
| May | 1.60 | 1.51 | – | 1.69 | <0.001 |
| July | 1.01 | 0.95 | – | 1.07 | 0.752 |
| August | 1.31 | 1.23 | – | 1.38 | <0.001 |
| September | 1.29 | 1.22 | – | 1.37 | <0.001 |
| October | 1.02 | 0.96 | – | 1.09 | 0.448 |
| November | 1.03 | 0.97 | – | 1.09 | 0.365 |
| December | 1.08 | 1.02 | – | 1.15 | 0.008 |
| Weekends (compared with weekdays) | 1.18 | 1.16 | – | 1.21 | <0.001 |
| Nighttime (17:00–09:00) (compared with daytime) | 2.53 | 2.47 | – | 2.59 | <0.001 |
| Pregnant women | 0.48 | 0.34 | – | 0.69 | <0.001 |
| COVID-19 (including suspected cases) | 1.44 | 1.35 | – | 1.53 | <0.001 |
| Elderly patients as a variable | |||||
| Odds ratio | 95%CI | p-value | |||
| Year | |||||
| 2019 | Reference | ||||
| 2021 | 1.39 | 1.38 | – | 1.41 | <0.001 |
| Female (compared with male) | 0.93 | 0.91 | – | 0.95 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.91 | 1.81 | – | 2.01 | <0.001 |
| February | 1.55 | 1.47 | – | 1.65 | <0.001 |
| March | 1.27 | 1.20 | – | 1.34 | <0.001 |
| April | 1.66 | 1.57 | – | 1.75 | <0.001 |
| May | 1.60 | 1.51 | – | 1.69 | <0.001 |
| July | 1.01 | 0.95 | – | 1.07 | 0.755 |
| August | 1.31 | 1.23 | – | 1.38 | <0.001 |
| September | 1.29 | 1.22 | – | 1.37 | <0.001 |
| October | 1.02 | 0.96 | – | 1.09 | 0.453 |
| November | 1.03 | 0.97 | – | 1.09 | 0.373 |
| December | 1.08 | 1.02 | – | 1.15 | 0.008 |
| Weekends (compared with weekdays) | 1.18 | 1.16 | – | 1.21 | <0.001 |
| Nighttime (17:00–09:00) (compared with daytime) | 2.53 | 2.47 | – | 2.59 | <0.001 |
| Old (compared with young <65 y) | 1.01 | 0.99 | – | 1.03 | 0.403 |
| COVID-19 (including suspected cases) | 1.44 | 1.35 | – | 1.53 | <0.001 |
| Vulnerable patients as a variable | |||||
| Odds ratio | 95%CI | p-value | |||
| Year | |||||
| 2019 | Reference | ||||
| 2021 | 1.40 | 1.38 | – | 1.41 | <0.001 |
| Female (compared with male) | 0.94 | 0.92 | – | 0.96 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.93 | 1.83 | – | 2.03 | <0.001 |
| February | 1.56 | 1.48 | – | 1.65 | <0.001 |
| March | 1.27 | 1.20 | – | 1.35 | <0.001 |
| April | 1.66 | 1.57 | – | 1.75 | <0.001 |
| May | 1.60 | 1.51 | – | 1.69 | <0.001 |
| July | 1.01 | 0.95 | – | 1.07 | 0.867 |
| August | 1.29 | 1.22 | – | 1.37 | <0.001 |
| September | 1.29 | 1.22 | – | 1.37 | <0.001 |
| October | 1.02 | 0.96 | – | 1.09 | 0.457 |
| November | 1.03 | 0.97 | – | 1.10 | 0.328 |
| December | 1.09 | 1.02 | – | 1.15 | 0.006 |
| Weekends (compared with weekdays) | 1.18 | 1.16 | – | 1.21 | <0.001 |
| Nighttime (17:00–09:00) (compared with daytime) | 2.47 | 2.41 | – | 2.53 | <0.001 |
| Vulnerable patients (compared with non-vulnerable) | 0.81 | 0.80 | – | 0.83 | <0.001 |
| COVID-19 (including suspected cases) | 1.41 | 1.32 | – | 1.50 | <0.001 |
The adjusted OR for mortality in the ED among pediatric patients was negative (adjusted OR 0.08, 95%CI 0.06–0.10; p < 0.001) (Table S3). The adjusted OR for mortality in the ED was positive for elderly patients (adjusted OR 4.04, 95%CI 3.84–4.26; p < 0.001). We analyzed adjusted ORs for mortality in the ED among elderly patients separately for 2019 and 2021 (Table 6). The adjusted OR for mortality in the ED among elderly patients was also positive in 2019 (adjusted OR 4.03, 95%CI 3.74–4.35; p < 0.001) and 2021 (adjusted OR 4.05, 95%CI 3.77–4.35; p < 0.001).
Table 6.
Multivariate logistic regression analysis of death in the ED for all patients in 2019 and 2021 (elderly patients as a variable).
| Odds Ratio | 95%CI | p -Value | |||
| Year | |||||
| 2019 | Reference | ||||
| 2021 | 1.17 | 1.15 | – | 1.19 | <0.001 |
| Female (compared with male) | 0.76 | 0.73 | – | 0.79 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.62 | 1.47 | – | 1.78 | <0.001 |
| February | 1.52 | 1.38 | – | 1.68 | <0.001 |
| March | 1.24 | 1.12 | – | 1.37 | <0.001 |
| April | 1.30 | 1.18 | – | 1.44 | <0.001 |
| May | 1.32 | 1.20 | – | 1.46 | <0.001 |
| July | 0.92 | 0.82 | – | 1.02 | 0.103 |
| August | 0.99 | 0.89 | – | 1.10 | 0.845 |
| September | 1.05 | 0.94 | – | 1.16 | 0.387 |
| October | 1.02 | 0.92 | – | 1.14 | 0.659 |
| November | 1.19 | 1.08 | – | 1.32 | 0.001 |
| December | 1.37 | 1.24 | – | 1.50 | <0.001 |
| Weekends (compared with weekdays) | 0.98 | 0.93 | – | 1.02 | 0.242 |
| Nighttime (17:00–09:00) (compared with daytime) | 1.60 | 1.54 | – | 1.66 | <0.001 |
| Old (compared with young <65 y) | 4.04 | 3.83 | – | 4.25 | <0.001 |
| COVID-19 (including suspected cases) | 0.25 | 0.19 | – | 0.32 | <0.001 |
| 2019 | |||||
| Odds ratio | 95% confidence interval | p-value | |||
| Female (compared with male) | 0.74 | 0.70 | – | 0.78 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.54 | 1.35 | – | 1.76 | <0.001 |
| February | 1.51 | 1.31 | – | 1.73 | <0.001 |
| March | 1.27 | 1.10 | – | 1.47 | 0.001 |
| April | 1.17 | 1.01 | – | 1.35 | 0.039 |
| May | 1.06 | 0.91 | – | 1.23 | 0.446 |
| July | 0.88 | 0.76 | – | 1.03 | 0.115 |
| August | 0.85 | 0.73 | – | 0.99 | 0.041 |
| September | 1.02 | 0.87 | – | 1.18 | 0.821 |
| October | 0.99 | 0.85 | – | 1.16 | 0.938 |
| November | 1.17 | 1.01 | – | 1.35 | 0.038 |
| December | 1.32 | 1.15 | – | 1.52 | <0.001 |
| Weekends (compared with weekdays) | 0.94 | 0.88 | – | 1.00 | 0.046 |
| Nighttime (17:00–09:00) (compared with daytime) | 1.54 | 1.46 | – | 1.64 | <0.001 |
| Old (compared with young <65 y) | 4.03 | 3.74 | – | 4.34 | <0.001 |
| COVID-19 (including suspected cases) | (omitted) | ||||
| 2021 | |||||
| Odds ratio | 95% confidence interval | p-value | |||
| Female (compared with male) | 0.78 | 0.74 | – | 0.83 | <0.001 |
| Month | |||||
| June | Reference | ||||
| January | 1.68 | 1.48 | – | 1.91 | <0.001 |
| February | 1.54 | 1.34 | – | 1.76 | <0.001 |
| March | 1.21 | 1.06 | – | 1.39 | 0.006 |
| April | 1.42 | 1.24 | – | 1.63 | <0.001 |
| May | 1.59 | 1.38 | – | 1.82 | <0.001 |
| July | 0.94 | 0.82 | – | 1.09 | 0.432 |
| August | 1.12 | 0.97 | – | 1.29 | 0.11 |
| September | 1.07 | 0.93 | – | 1.24 | 0.345 |
| October | 1.05 | 0.91 | – | 1.21 | 0.512 |
| November | 1.22 | 1.06 | – | 1.40 | 0.005 |
| December | 1.41 | 1.24 | – | 1.61 | <0.001 |
| Weekends (compared with weekdays) | 1.00 | 0.95 | – | 1.06 | 0.974 |
| Nighttime (17:00–09:00) (compared with daytime) | 1.64 | 1.56 | – | 1.73 | <0.001 |
| Old (compared with young <65 y) | 4.05 | 3.77 | – | 4.34 | <0.001 |
| COVID-19 (including suspected cases) | 0.24 | 0.19 | 0.32 | <0.001 | |
4. Discussion
This retrospective descriptive study found that difficulty in obtaining hospital acceptance for transfer of a vulnerable patient (difficult-to-transport cases) was increased in 2021 compared with 2019, at least in Osaka Prefecture. Status as a pediatric patients or pregnant woman were independent factors associated with decreased risk of difficult-to-transport cases, but elderly status of age ≥65 years was not independently associated with any decrease or increase in difficult-to-transport cases in the two year-long periods studied (2019 and 2021). However, the elderly population was independently associated with increased risk of difficult-to-transport cases during the COVID-19 pandemic in 2021.
The number of patients transported to hospital by ambulance was significantly lower in 2021 in Osaka than in 2019, although the number of patients transported by ambulance in Japan has been increasing for the past 10 years [18]. Similar reductions in ambulance callouts were seen all over the world during the pandemic in 2020 [19,20,21,22]. Two reasons may have contributed to this: first, transmission of COVID-19 is thought to occur through aerosolized droplets or direct contact, so some patients might have been reluctant to seek medical attention due to concerns about contracting COVID-19 after visiting a hospital. Second, less-urgent patients did not want to burden the healthcare system because of informational campaigns emphasizing the pressures on healthcare providers.
A similar analysis of 2020 found that June showed the lowest number of difficult-to-transport cases that year, and cases between July and November were not significantly associated with difficult-to-transport cases in 2019 (Table S2) [3,4]. The present study showed more difficult-to-transport cases in August and September than in June 2021, which was attributed to the fifth wave of COVID-19 in Japan (Table S2; Figure 2).
The ambulance service performs triage at the scene, selects an appropriate hospital depending on the condition of the patient, and contacts the hospital to request acceptance of the patient [23] The hospital can choose not to accept the request based on treatment capabilities and bed vacancies. High burdens on emergency care resources would obviously increase the risk of a request being declined. Before the COVID-19 pandemic, the ageing of the population has made elderly patients frequent users of ambulance services, because the EMS system including the ambulance service is fully operated by the public sector under the Japanese system of universal coverage [23]. We considered the elderly population as the main age group for difficult-to-transport cases, but this group did not show increased difficulty obtaining hospital acceptance for transport compared to before the COVID-19 pandemic (Table 5 and Table S2).
One possible reason might be that this age group had primary care physicians at hospitals near their homes, representing so-called ‘hospital-centered medical care’, and thus might have been accepted within 30 min at the nearest hospitals [24].
On the other hand, patients <65 years of age were considered more likely to be healthier and might not need the services of their primary care physician in their resident area. In addition, hospitals tended not to accept patients transported by ambulance because COVID-19 spreads more in young adults than elderly patients [25]. Such patients thus might have been unable to achieve rapid acceptance by a hospital (Table S2).
Children and pregnant women were found to have a negative association with categorization as difficult-to-transport cases, but univariate logistic analysis showed greater difficulty with hospitals accepting those patients in 2021 compared to 2019, differing from previous studies [3,4]. Each COVID-19 wave in Osaka triggered a medical crisis, where non-COVID-19 medical services such as emergency medicine were temporarily halted, so populations of children and pregnant women might have encountered difficulty with transportation [26]. There were three waves in 2021 in Japan (Figure 2). In the third COVID-19 wave, there were more infections than those in the first and second COVID-19 waves in 2020 [27]. In the fourth COVID-19 wave, the Alpha variant became the main strain of the virus [27]. In the fifth COVID-19 wave, the Delta variant became the main strain, causing a medical crisis [27]. July and August were not associated with difficult-to-transport cases in 2019 but were significantly associated with difficult-to-transport cases in 2021 (Table S2). This was due to the fifth COVID-19 wave, the Delta variant, which was associated with increased susceptibility to severe disease and resulted in increasing difficult-to-transport cases.
Elderly patients (>65 years of age) were found to have an independent association with increased mortality in the ED. The adjusted OR for death in the ED for elderly patients in 2019 was similar to that in 2021. The COVID-19 pandemic caused a medical crisis in Osaka, and old age was an independent factor associated with increased risk of difficult-to-transport cases during the COVID-19 pandemic in 2021, but this did not influence the risk of mortality in the ED. One possible reason might be that patients with serious disease using ambulance services were accepted by hospitals at similar rates in both 2019 and 2021, even during medical crises. The EMS system effectively managed serious patients in Osaka during the COVID-19 pandemic.
There was a potentially altered clinical phenotype associated with some degree of preexisting immunity conferred by COVID-19 vaccination; however, children were not considered because children’s COVID-19 vaccination started in 2022 in Japan.
Several limitations to this study need to be kept in mind. First, this study was a retrospective, observational study and thus unknown confounding factors may have impacted the results. However, the ORION system has been collecting data on all emergency patients transported to critical care centers and emergency medical institutions by ambulance in Osaka Prefecture; thus, patient selection bias is small. Second, we could not include other vulnerable populations such as those with mental illness or the homeless because ORION data do not include specific patient data due to privacy concerns. Third, the final diagnosis and prognosis in hospital were unknown since this study only analyzed ambulance records.
In the future, we will use both ambulance records and hospital data to analyze the impact of the COVID-19 pandemic on the EMS system for vulnerable patients. Our study findings will be useful for the next COVID-19 or non-COVID-19 pandemic as they provide fundamental learning regarding the epidemiology of vulnerable patients in Japan.
5. Conclusions
During the COVID-19 pandemic in 2021, the frequency of difficult-to-transport cases was increased compared to 2019, but vulnerable patients were not the cause of difficulty in obtaining hospital acceptance for transfer. Each wave of COVID-19 infection influenced difficult-to-transport cases. Elderly patients ≥65 years of age had an independent association with increased mortality in the ED, but not with the COVID-19 pandemic. Our study findings will be useful for other non-COVID-19 pandemics as they provide fundamental learning regarding the epidemiology of vulnerable patients.
Acknowledgments
The authors thank the EMS providers, nurses, emergency physicians, and administrators for their cooperation with the ORION system. We thank all the members of The Working Group to Analyze the Emergency Medical Care System in Osaka Prefecture for their kind support.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/medicina60020345/s1. Table S1: Multivariate logistic regression analysis of difficult-to-transport cases among all patients (adult as a variable); Table S2: Multivariate logistic regression analysis of difficult-to-transport cases among all patients in 2019 and 2021 (pediatric patients, pregnant women, elderly patients, and vulnerable population as a variable); Table S3: Multivariate logistic regression analysis of death in the ED for all patients (pediatric patients as a variable).
Author Contributions
K.O. designed the study and wrote the initial draft of the manuscript. T.K., M.N., T.M. and A.T. contributed to the analysis and interpretation of the data and assisted in the preparation of the manuscript. All authors contributed to data collection and interpretation, and all critically reviewed the manuscript. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work, including ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors meet the International Committee of Medical Journal Editors (ICMJE) authorship criteria. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ambulance records in Osaka Prefecture are considered administrative records, so the need to obtain informed consent from participants was waived because the data were anonymous. This study was approved by the Ethics Committee of Osaka Prefectural Government (Osaka City, Japan), Approval Code: 2021-006, Approval Date: 18 June 2021.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA-J. Am. Med. Assoc. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2.Katayama Y., Kiyohara K., Kitamura T., Hayashida S., Shimazu T. Influence of the COVID-19 pandemic on an emergency medical service system: A population-based, descriptive study in Osaka, Japan. Acute Med. Surg. 2020;7:e534. doi: 10.1002/ams2.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ota K., Nishioka D., Katayama Y., Kitamura T., Masui J., Ota K., Nitta M., Matsuoka T., Takasu A. Influence of the COVID-19 outbreak on transportation of pregnant women in an emergency medical service system: Population-based, ORION registry. Int. J. Gynecol. Obstet. 2022;157:366–374. doi: 10.1002/ijgo.14128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ota K., Nishioka D., Katayama Y., Kitamura T., Masui J., Ota K., Nitta M., Matsuoka T., Takasu A. Effect of the COVID-19 outbreak on emergency transport of children by an emergency medical service system: A population-based, ORION registry study. BMC Emerg. Med. 2022;22:206. doi: 10.1186/s12873-022-00765-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ageta K., Naito H., Yorifuji T., Obara T., Nojima T., Yamada T., Tsukahara K., Yakushiji H., Nakao A. Delay in Emergency Medical Service Transportation Responsiveness during the COVID-19 Pandemic in a Minimally Affected Region. Acta Med. Okayama. 2020;74:513–520. doi: 10.18926/AMO/61210. [DOI] [PubMed] [Google Scholar]
- 7.Aruga Y. Emergency medical services for the elderly: Present fact and future challenge. Nihon Rinsho. 2013;71:964–968. [PubMed] [Google Scholar]
- 8.Salvi F., Morichi V., Grilli A., Giorgi R., De Tommaso G., Dessì-Fulgheri P. The elderly in the emergency department: A critical review of problems and solutions. Intern. Emerg. Med. 2007;2:292–301. doi: 10.1007/s11739-007-0081-3. [DOI] [PubMed] [Google Scholar]
- 9.Shahid Z., Kalayanamitra R., McClafferty B., Kepko D., Ramgobin D., Patel R., Aggarwal C.S., Vunnam R., Sahu N., Bhatt D., et al. COVID-19 and Older Adults: What We Know. J. Am. Geriatr. Soc. 2020;68:926–929. doi: 10.1111/jgs.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J., Li Q., Jiang C., Zhou Y., Liu S., et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020;81:e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okamoto J., Katayama Y., Kitamura T., Sado J., Nakamura R., Kimura N., Misaki H., Yamao S., Nakao S., Nitta M., et al. Profile of the ORION (Osaka emergency information Research Intelligent Operation Network system) between 2015 and 2016 in Osaka, Japan: A population-based registry of emergency patients with both ambulance and in-hospital records. Acute Med. Surg. 2019;6:12–24. doi: 10.1002/ams2.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amyx M., Xiong X., Xie Y., Buekens P. Racial/Ethnic Differences in Sleep Disorders and Reporting of Trouble Sleeping Among Women of Childbearing Age in the United States. Matern. Child. Health J. 2017;21:306–314. doi: 10.1007/s10995-016-2115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO . International Statistical Classification of Diseases and Related Health Problems, 10th Revision ICD-10: Tabular List. Volume 1. World Health Organization; Geneva, Switzerland: 2016. [(accessed on 5 August 2023)]. pp. 332–345. Available online: http://www.who.int/classifications/icd/icdonlineversions/en/ [Google Scholar]
- 14.Difinition. [(accessed on 5 August 2023)];2017 Available online: https://www.jpn-geriat-soc.or.jp/proposal/pdf/definition_01.pdf.
- 15.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Benchimol E.I., Smeeth L., Guttmann A., Harron K., Moher D., Petersen I., Sørensen H.T., von Elm E., Langan S.M., RECORD Working Committee The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015;12:e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ministry of Health, Labour and Welfare of Japan Ambulance Service Planning Office of Fire and Service, Management Agency of Japan and Guidance of Medical Division, Health Policy Bureau, Ministry of Health L and, Disaster ASPO of F and, Service MA of J and G of M, Division HPB A Report on the Acceptance of Emergency Patients by Medical Institutions. [(accessed on 5 August 2023)];Volume 6 Available online: https://www.fdma.go.jp/disaster/coronavirus/items/coronavirus_kekka.pdf. [Google Scholar]
- 18.The Fire and Disaster Management Agency White Book on Emergency System in Japan. [(accessed on 5 August 2023)];2020 Available online: https://www.fdma.go.jp/publication/rescue/items/kkkg_r02_01_kyukyu.pdf.
- 19.Holmes J.L., Brake S., Docherty M., Lilford R., Watson S. Emergency ambulance services for heart attack and stroke during UK’s COVID-19 lockdown. Lancet. 2020;395:e93–e94. doi: 10.1016/S0140-6736(20)31031-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutherland K., Chessman J., Zhao J., Sara G., Shetty A., Smith S., Went A., Dyson S., Levesque J.F. Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Res. Pract. 2020;30:e3042030. doi: 10.17061/phrp3042030. [DOI] [PubMed] [Google Scholar]
- 21.Grunau B., Helmer J., Lee S., Acker J., Deakin J., Armour R., Tallon J., Jenneson S., Christenson J., Scheuermeyer F.X. Decrease in emergency medical services utilization during early stages of the COVID-19 pandemic in British Columbia. Can. J. Emerg. Med. 2021;23:237–241. doi: 10.1007/s43678-020-00062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ota K., Nishioka D., Katayama Y., Kitamura T., Masui J., Ota K., Nitta M., Matsuoka T., Takasu A. Epidemiology of patients with dizziness over a 3-year period, requiring utilization of the emergency medical serviced system—A Pre- and Post-COVID pandemic comparative study using the population-based ORION registry. J. Vestib. Res. 2023;33:127–136. doi: 10.3233/VES-220024. [DOI] [PubMed] [Google Scholar]
- 23.Shimizu K., Hibino S., Biros M.H., Irisawa T., Shimazu T. Emergency medicine in Japan: Past, present, and future. Int. J. Emerg. Med. 2021;14:2. doi: 10.1186/s12245-020-00316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arai H., Ouchi Y., Toba K., Endo T., Shimokado K., Tsubota K., Matsuo S., Mori H., Yumura W., Yokode M., et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr. Gerontol. Int. 2015;15:673–687. doi: 10.1111/ggi.12450. [DOI] [PubMed] [Google Scholar]
- 25.Pollard C.A., Morran M.P., Nestor-Kalinoski A.L. The COVID-19 pandemic: A global health crisis. Physiol. Genom. 2020;52:549–557. doi: 10.1152/physiolgenomics.00089.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kurahara Y., Kobayashi T., Shintani S., Matsuda Y., Tamiya A., Sugawara R., Arai T., Tachibana K., Okishio K., Matsui H., et al. Clinical characteristics of COVID-19 in Osaka, Japan: Comparison of the first–third waves with the fourth wave. Respir. Investig. 2021;59:810–818. doi: 10.1016/j.resinv.2021.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee H., Chubachi S., Namkoong H., Asakura T., Tanaka H., Otake S., Nakagawara K., Morita A., Fukushima T., Watase M., et al. Characteristics of hospitalized patients with COVID-19 during the first to fifth waves of infection: A report from the Japan COVID-19 Task Force. BMC Infect. Dis. 2022;22:935. doi: 10.1186/s12879-022-07927-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used in the current study are available from the corresponding author on reasonable request.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.