Abstract
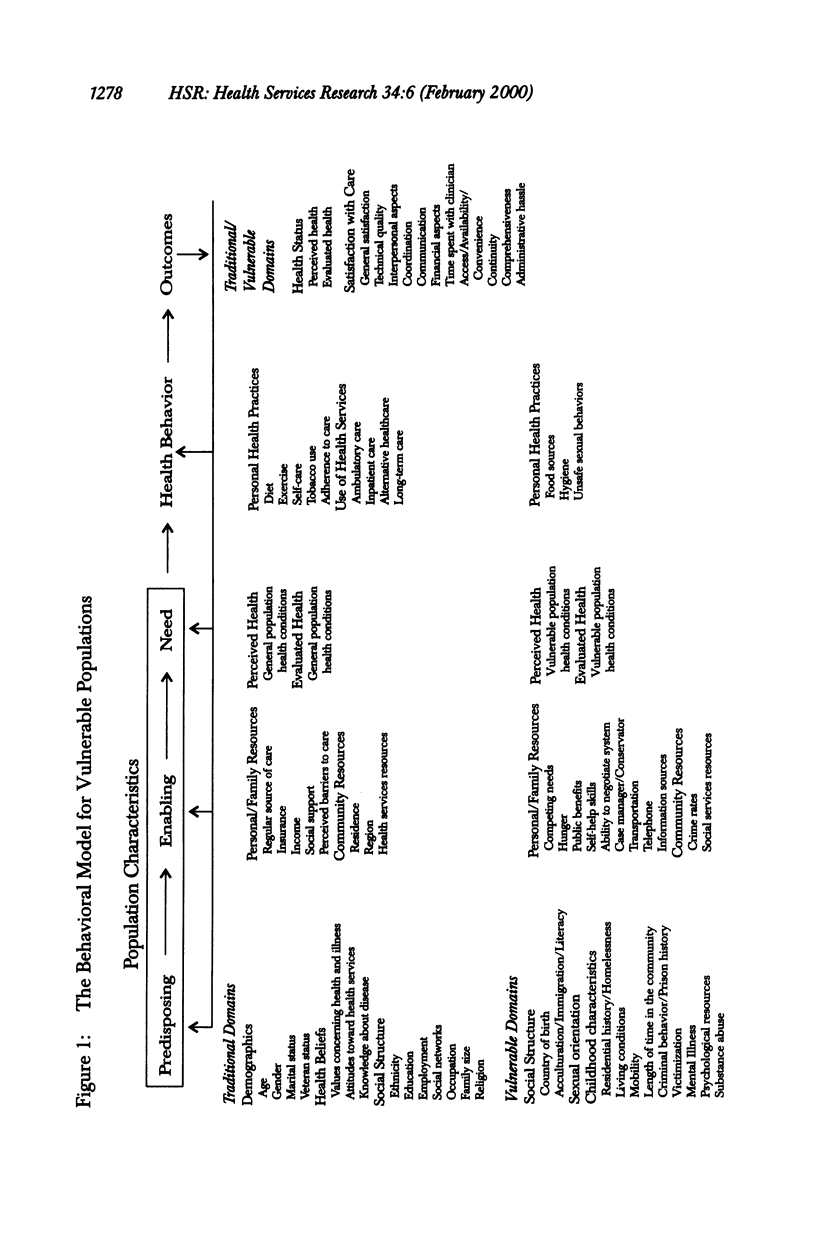
OBJECTIVES: (1) To present the Behavioral Model for Vulnerable Populations, a major revision of a leading model of access to care that is particularly applicable to vulnerable populations; and (2) to test the model in a prospective study designed to define and determine predictors of the course of health services utilization and physical health outcomes within one vulnerable population: homeless adults. We paid particular attention to the effects of mental health, substance use, residential history, competing needs, and victimization. METHODS: A community-based probability sample of 363 homeless individuals was interviewed and examined for four study conditions (high blood pressure, functional vision impairment, skin/leg/foot problems, and tuberculosis skin test positivity). Persons with at least one study condition were followed longitudinally for up to eight months. PRINCIPAL FINDINGS: Homeless adults had high rates of functional vision impairment (37 percent), skin/leg/foot problems (36 percent), and TB skin test positivity (31 percent), but a rate of high blood pressure similar to that of the general population (14 percent). Utilization was high for high blood pressure (81 percent) and TB skin test positivity (78 percent), but lower for vision impairment (33 percent) and skin/leg/foot problems (44 percent). Health status for high blood pressure, vision impairment, and skin/leg/foot problems improved over time. In general, more severe homeless status, mental health problems, and substance abuse did not deter homeless individuals from obtaining care. Better health outcomes were predicted by a variety of variables, most notably having a community clinic or private physician as a regular source of care. Generally, use of currently available services did not affect health outcomes. CONCLUSIONS: Homeless persons are willing to obtain care if they believe it is important. Our findings suggest that case identification and referral for physical health care can be successfully accomplished among homeless persons and can occur concurrently with successful efforts to help them find permanent housing, alleviate their mental illness, and abstain from substance abuse.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aday L. A. Health status of vulnerable populations. Annu Rev Public Health. 1994;15:487–509. doi: 10.1146/annurev.pu.15.050194.002415. [DOI] [PubMed] [Google Scholar]
- Alstrom C. H., Lindelius R., Salum I. Mortality among homeless men. Br J Addict Alcohol Other Drugs. 1975 Sep;70(3):245–252. doi: 10.1111/j.1360-0443.1975.tb00034.x. [DOI] [PubMed] [Google Scholar]
- Andersen R. M. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995 Mar;36(1):1–10. [PubMed] [Google Scholar]
- Doblin B. H., Gelberg L., Freeman H. E. Patient care and professional staffing patterns in McKinney Act clinics providing primary care to the homeless. JAMA. 1992 Feb 5;267(5):698–701. [PubMed] [Google Scholar]
- Fischer P. J., Shapiro S., Breakey W. R., Anthony J. C., Kramer M. Mental health and social characteristics of the homeless: a survey of mission users. Am J Public Health. 1986 May;76(5):519–524. doi: 10.2105/ajph.76.5.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L., Gallagher T. C., Andersen R. M., Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997 Feb;87(2):217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L., Leake B. D. Substance use among impoverished medical patients: the effect of housing status and other factors. Med Care. 1993 Sep;31(9):757–766. doi: 10.1097/00005650-199309000-00001. [DOI] [PubMed] [Google Scholar]
- Gelberg L., Linn L. S. Psychological distress among homeless adults. J Nerv Ment Dis. 1989 May;177(5):291–295. doi: 10.1097/00005053-198905000-00007. [DOI] [PubMed] [Google Scholar]
- Gelberg L., Linn L. S., Usatine R. P., Smith M. H. Health, homelessness, and poverty. A study of clinic users. Arch Intern Med. 1990 Nov;150(11):2325–2330. [PubMed] [Google Scholar]
- Gelberg L., Panarites C. J., Morgenstern H., Leake B., Andersen R. M., Koegel P. Tuberculosis skin testing among homeless adults. J Gen Intern Med. 1997 Jan;12(1):25–33. doi: 10.1046/j.1525-1497.1997.12101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L., Siecke N. Accuracy of homeless adults' self-reports. Med Care. 1997 Mar;35(3):287–290. doi: 10.1097/00005650-199703000-00008. [DOI] [PubMed] [Google Scholar]
- Hays R. D., Sherbourne C. D., Mazel R. M. The RAND 36-Item Health Survey 1.0. Health Econ. 1993 Oct;2(3):217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- Kleinman L. C., Freeman H., Perlman J., Gelberg L. Homing in on the homeless: assessing the physical health of homeless adults in Los Angeles County using an original method to obtain physical examination data in a survey. Health Serv Res. 1996 Dec;31(5):533–549. [PMC free article] [PubMed] [Google Scholar]
- Rew L. Health risks of homeless adolescents. Implications for holistic nursing. J Holist Nurs. 1996 Dec;14(4):348–359. doi: 10.1177/089801019601400407. [DOI] [PubMed] [Google Scholar]
- Robertson M. J., Cousineau M. R. Health status and access to health services among the urban homeless. Am J Public Health. 1986 May;76(5):561–563. doi: 10.2105/ajph.76.5.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins L. N., Helzer J. E., Croughan J., Ratcliff K. S. National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry. 1981 Apr;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Ropers R. H., Boyer R. Homelessness as a health risk. Alcohol Health Res World. 1987 Spring;11(3):38-41, 89. [PubMed] [Google Scholar]



