Abstract
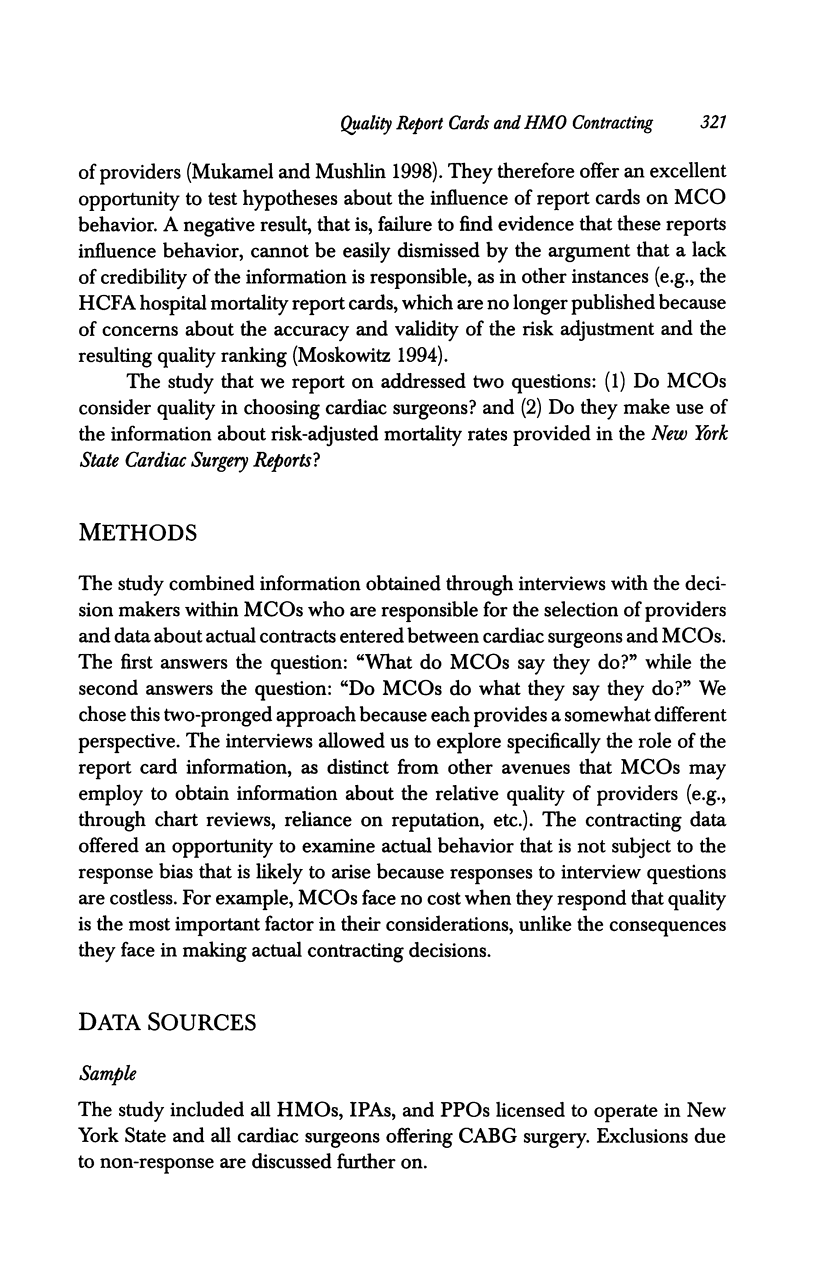
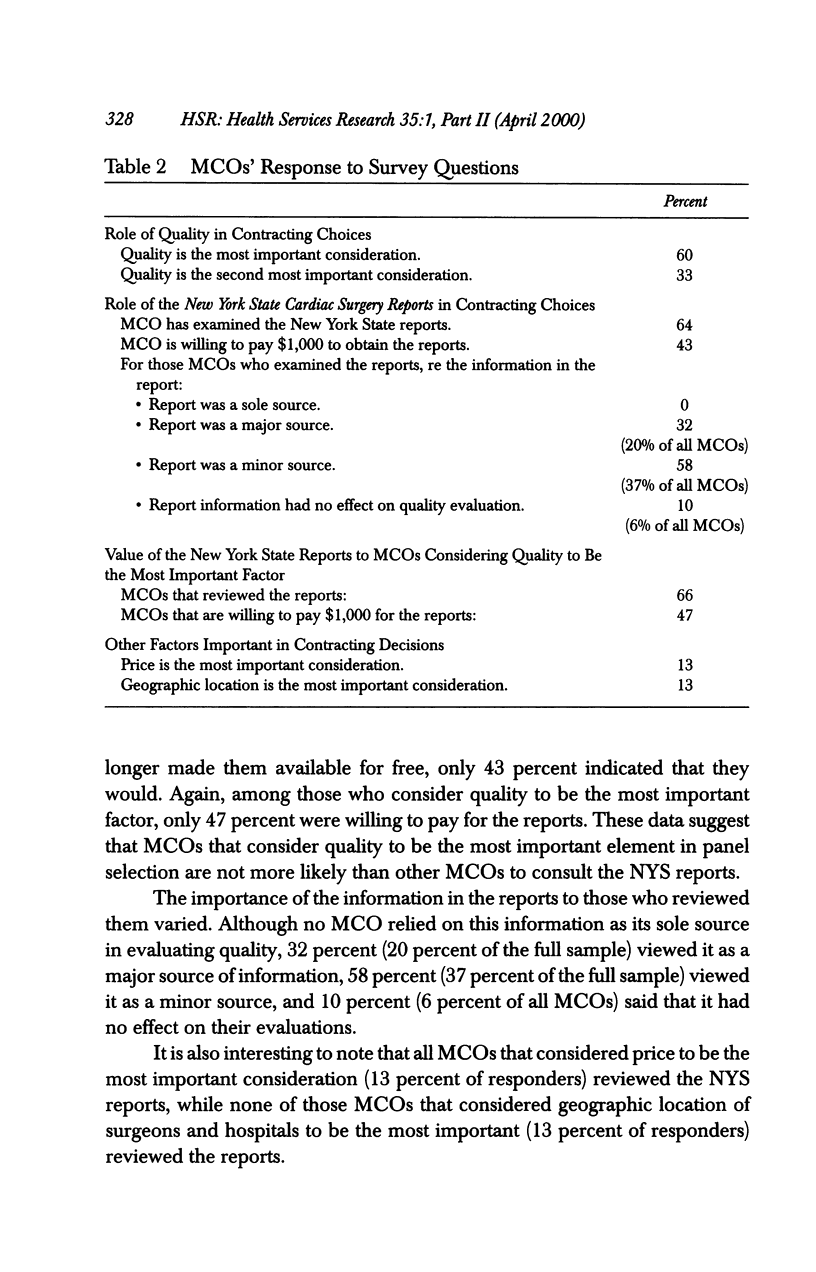
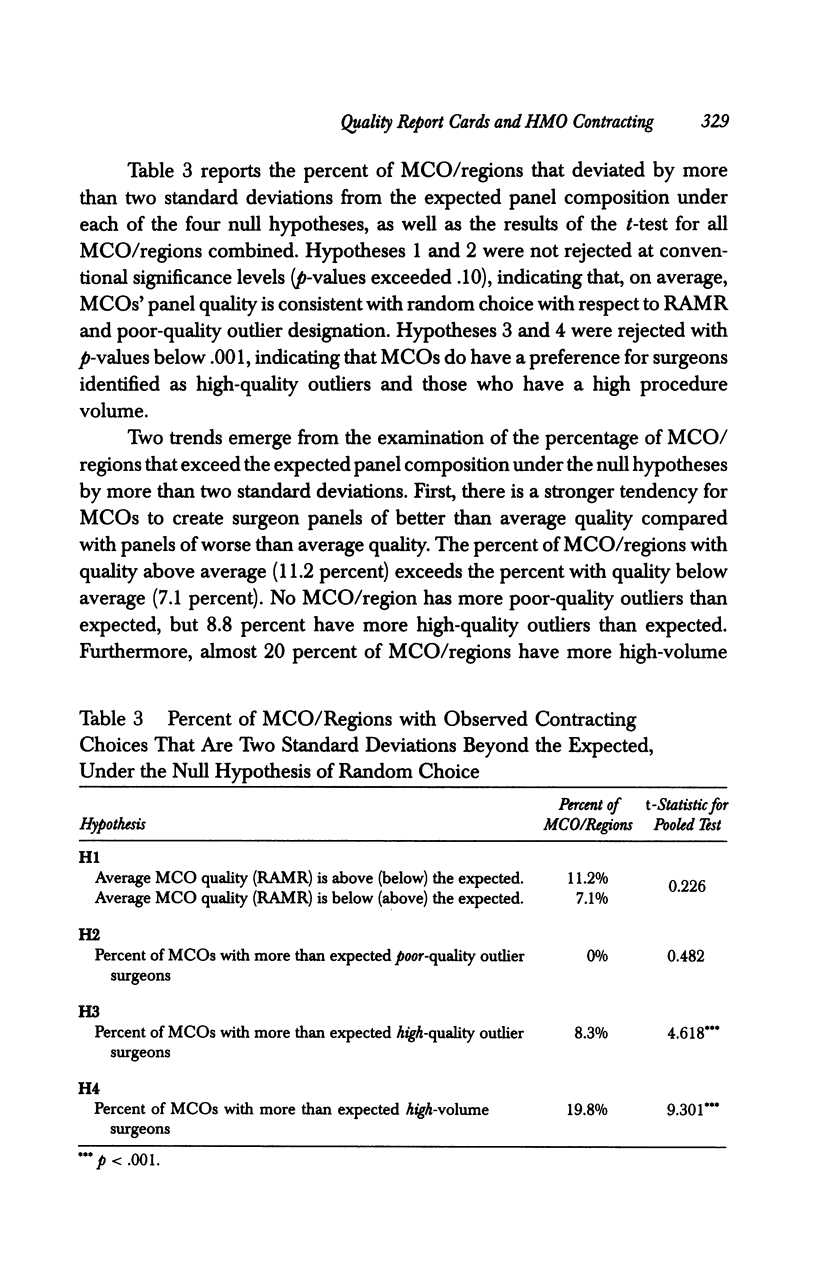
OBJECTIVE: To answer two related questions: (1) Do managed care organizations (MCOs) in New York State (NYS) consider quality when they choose cardiac surgeons? (2) Do they use information about risk-adjusted mortality rates (RAMR) provided in the New York State Cardiac Surgery Reports? DATA SOURCES: (1) Telephone interviews with and contracting data from the majority of MCOs licensed in NYS; (2) RAMR, quality outlier designation, and procedure volume for all cardiac surgeons, as reported in the Cardiac Surgery Reports. STUDY DESIGN: Interview data were analyzed in conjunction with patterns revealed by contracting data. Null hypotheses that MCOs' contracting choices were random with respect to the information published in the Cardiac Surgery Reports were tested. PRINCIPAL FINDINGS: Sixty percent of MCOs ranked the quality of surgeons as most important in their contracting considerations. Although 64 percent of MCOs indicated some knowledge of the NYS Cardiac Surgery Reports, only 20 percent indicated that the reports were a major factor in their contracting decision. Analyses of actual contracting patterns show that in aggregate, the hypothesis of random choice could be rejected with respect to high-quality outlier status and high procedure volume but not for RAMR or poor-quality outlier status. The panel composition of the majority of MCOs (80.2 percent) was within two standard deviations of the expected mean under the null hypothesis. CONCLUSIONS: Despite a professed preference for high-quality surgeons, the use of publicly available quality reports by MCOs is currently low, and contracting practices for the majority of MCOs do not indicate a systematic selection either for or against surgeons based on their reported mortality scores. This study suggests that policy initiatives to increase the effective use of report cards should be encouraged.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chassin M. R., Hannan E. L., DeBuono B. A. Benefits and hazards of reporting medical outcomes publicly. N Engl J Med. 1996 Feb 8;334(6):394–398. doi: 10.1056/NEJM199602083340611. [DOI] [PubMed] [Google Scholar]
- Epstein A. Performance reports on quality--prototypes, problems, and prospects. N Engl J Med. 1995 Jul 6;333(1):57–61. doi: 10.1056/NEJM199507063330114. [DOI] [PubMed] [Google Scholar]
- Hannan E. L., Kilburn H., Jr, Racz M., Shields E., Chassin M. R. Improving the outcomes of coronary artery bypass surgery in New York State. JAMA. 1994 Mar 9;271(10):761–766. [PubMed] [Google Scholar]
- Hannan E. L., Kumar D., Racz M., Siu A. L., Chassin M. R. New York State's Cardiac Surgery Reporting System: four years later. Ann Thorac Surg. 1994 Dec;58(6):1852–1857. doi: 10.1016/0003-4975(94)91726-4. [DOI] [PubMed] [Google Scholar]
- Hartz A. J., Kuhn E. M., Pulido J. Prestige of training programs and experience of bypass surgeons as factors in adjusted patient mortality rates. Med Care. 1999 Jan;37(1):93–103. doi: 10.1097/00005650-199901000-00013. [DOI] [PubMed] [Google Scholar]
- Hughes R. G., Hunt S. S., Luft H. S. Effects of surgeon volume and hospital volume on quality of care in hospitals. Med Care. 1987 Jun;25(6):489–503. doi: 10.1097/00005650-198706000-00004. [DOI] [PubMed] [Google Scholar]
- Mukamel D. B., Mushlin A. I. Quality of care information makes a difference: an analysis of market share and price changes after publication of the New York State Cardiac Surgery Mortality Reports. Med Care. 1998 Jul;36(7):945–954. doi: 10.1097/00005650-199807000-00002. [DOI] [PubMed] [Google Scholar]
- Peterson E. D., DeLong E. R., Jollis J. G., Muhlbaier L. H., Mark D. B. The effects of New York's bypass surgery provider profiling on access to care and patient outcomes in the elderly. J Am Coll Cardiol. 1998 Oct;32(4):993–999. doi: 10.1016/s0735-1097(98)00332-5. [DOI] [PubMed] [Google Scholar]
- Romano P. S., Zach A., Luft H. S., Rainwater J., Remy L. L., Campa D. The California Hospital Outcomes Project: using administrative data to compare hospital performance. Jt Comm J Qual Improv. 1995 Dec;21(12):668–682. doi: 10.1016/s1070-3241(16)30195-x. [DOI] [PubMed] [Google Scholar]


