Abstracts
Objectives
While there is a consensus against bracing after anterior cruciate ligament (ACL) reconstruction, the question of its potential benefits, especially in cases involving meniscus repair, as well as its routine use by the majority of clinicians, remains a topic of debate. This study aims to assess the effectiveness of bracing in relation to clinical scores after ACL reconstruction, regardless of meniscus surgery.
Methods
This randomised controlled study involved patients aged 15–55 years who underwent arthroscopic ACL reconstruction surgery. All eligible patients were assigned into two groups: one group received an adjustable frame with a four-point fixation knee brace for a four-week period, while the other did not.
A single experienced surgeon performed standard anatomical single-bundle ACL reconstruction. All patients, irrespective of whether they underwent meniscus repair, followed the same rehabilitation protocol. Knee functional questionnaires, including the International Knee Documentation Committee (IKDC) score, Lysholm score, Tegner Activity Scale, Visual Analogue Scale (VAS), and examinations, were collected preoperatively, at six months, one year, and two years postoperatively. The study employed an intention-to-treat analysis and multilevel mixed-effects generalised linear models to compare continuous outcomes between the groups, adjusting for the times of follow-up.
Results
A total of 84 patients (42 patients per group) comprised of 75 males (89 %) and average age of 30 ± 9.4 years old. Patient-reported function, physical examination findings, and surgical characteristics were comparable between the two groups. (P-value >0.05) Both groups demonstrated significant improvement in IKDC and Lysholm scores at the end of the two-year follow-up period. (P-value <0.0001) In multivariate analysis, bracing was significantly associated with lower Tegner activity scale than the non-brace group after adjustment for VAS and time (coefficient −0.49, 95 % confidence interval −0.87, −0.10, P-value = 0.013). None of the graft ruptures were reported, and there was no significant difference of return to sports between the groups at the end of the follow-up.
Conclusion
The study suggests that knee bracing after ACL reconstruction, regardless of any additional meniscus procedures, fails to enhance subjective or objective outcomes and could potentially have a negative impact on the Tegner activity scale, although the difference is not clinically significant. The routine use of a postoperative brace should be discontinued.
Level of evidence
Level I, Randomised controlled trial with no negative criteria.
Keywords: ACL reconstruction, Functional outcome, Knee brace, Meniscus repair, Rehabilitation
-
●
Bracing after ACL reconstruction, irrespective of meniscus repair, fails to enhance subjective or objective outcomes.
-
●
Patients undergoing ACL reconstruction may experience a lower Tegner activity scale with brace use.
1. Introduction
Anterior cruciate ligament (ACL) injury is a common occurrence that affects many individuals worldwide. According to a study conducted in the United States, the rate of ACL reconstruction increased significantly over time in all age groups.1 Rehabilitation plays an important role in the success of ACL reconstruction. Despite many postoperative programmes are available,2,3 there is no consensus guidelines or recommendations widely accepted.
After undergoing ACL reconstruction surgery using a hamstring graft, the reconstructed knee may be at a higher risk of further injury. As a result, healthcare providers often recommend the use of a knee brace to prevent excessive movement and provide additional support and stability during the early stages of rehabilitation.4 Studies have shown that knee immobilisation can reduce excessive tibial rotation during high loading pivoting, which can partially restore normal kinematics and benefit patients recovering from ACL reconstruction with a hamstring autograft.5 However, prolonged use of a knee brace can have negative consequences, such as muscle atrophy and a decline in function and proprioception. This is because the brace limits normal joint movement, leading to disuse of the surrounding muscles.6 In addition to the potential negative effects on function, the use of a brace can also result in significant costs for the healthcare system. Meta-analyses of randomised controlled trials found that knee bracing did not significantly affect knee function or stability after ACL reconstruction. However, it may reduce pain, improve patient confidence in early rehabilitation, and protect the knee during high-risk activities. Therefore, knee braces should be used based on the individual needs, and goals of the patient.7,8
The incidence of meniscal tears associated with ACL injury is higher in chronic cases, and the number of medial meniscal tears is particularly high.9 Braces protect healing meniscus tissue by providing rotational control during early rehabilitation as most meniscus injuries occur due to combined rotational and flexion forces.10 There is a trend towards early functional start of rehabilitation after partial meniscectomy, whereas a rather restricted start is recommended after meniscus repair or replacement.10
Based on the aforementioned systematic reviews and studies, most articles recommend against bracing after ACL reconstruction,6, 7, 8 whereas the majority support the use of bracing after meniscus repair.10 Despite information from systematic reviews, the most recent survey in 2022 indicated that the majority of surgeons (54.9 %) declared using some form of brace during postoperative rehabilitation, even after primary isolated ACL reconstruction.11 Currently, the incidence of ACL reconstruction with meniscus repair is increasing, and there remains no consensus on whether bracing is beneficial after ACL reconstruction with meniscus repair.
This study was conducted to assess the effectiveness of bracing in terms of knee function and stability following ACL reconstruction, regardless of meniscus repair. Our hypothesis was that brace-free ACL reconstruction would yield results comparable to a brace-based approach, thus advocating for the discontinuation of routine brace use.
2. Materials and methods
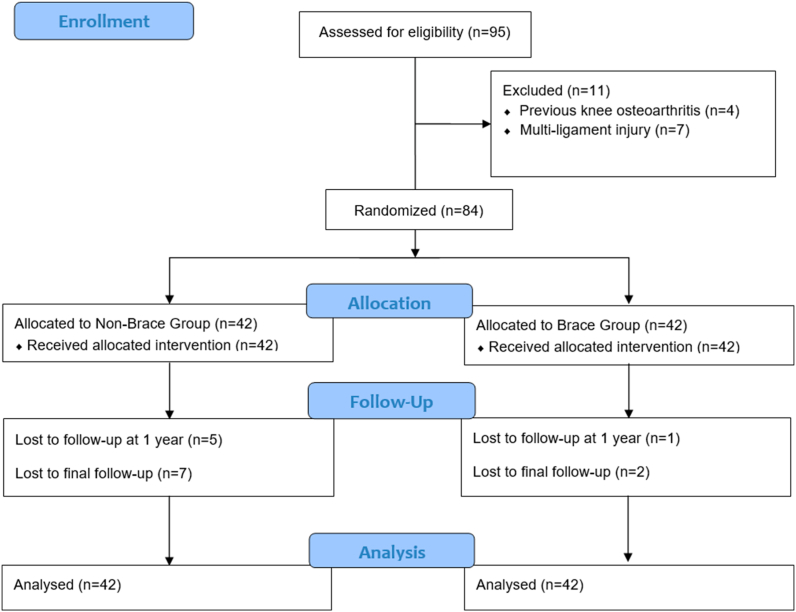
This prospective randomised controlled study was conducted at a regional hospital from June 2020 to May 2023 and was approved by the hospital ethics committee. Written informed consent was obtained from all patients participating in the study. The study has been conducted in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving human subjects. Inclusion criteria for this study are patients between the ages of 15–55 years who underwent arthroscopic ACL reconstruction surgery. However, patients with posterior instability or collateral ligament instability grade II or above, a history of ligament reconstruction, and those with previous knee osteoarthritis of Kellgren and Lawrence (KL) grade II or above were excluded from the study (Fig. 1).
Fig. 1.
CONSORT diagram.
Various blocked randomisation was generated by using STATA 16.1, StataCorp, College Station, Texas, USA. All randomisation numbers were concealed in the sealed envelopes which were opened postoperatively. Neither the subjects nor the surgeon was blinded to the randomisation in this study.
Pre-operative knee functional questionnaires were collected using the Thai version of the International Knee Documentation Committee (IKDC) score,12 the Lysholm score, and the Tegner activity scale.13 Knee examinations were performed by the same surgeon to assess knee stability and function, including range of motion, the Lachman test, the anterior drawer test, the pivot shift test, and the single leg hop test. Results were then categorised according to the IKDC classification system.14 Conventional standing knee radiographs were obtained in two planes (anteroposterior and lateral views) to evaluate the grading of osteoarthritis.
A single experienced orthopaedic surgeon performed standard anatomic single bundle ACL reconstruction on all patients. A quadruple semitendinosus tendon was used as a single graft, harvested in the standard fashion. An additional graft of the gracilis tendon was harvested in some cases if the quadruple semitendinosus tendon graft size was less than 7.5 mm in diameter. Standard anterolateral and anteromedial arthroscopic portals were created. The meniscus and cartilage procedures were carried out if necessary. The femoral tunnel was created from anteromedial portal based on the identified anatomic footprint. Its centre was pointed at the lateral bifurcate ridge and below the lateral intercondylar ridge. The tibial tunnel was approximated on between the anterior horn of the lateral meniscus and the ACL stump insertion site. The femoral fixation of the graft was achieved using a suspension device (XO button, Conmed Linvatec, FL, USA). Initial tensioning was performed manually with two-handed tensioning. The tibial site was stabilized with an interference screw (Genesys Matryx, Conmed Linvatec, FL, USA) while the knee was in full extension.
All patients, whether they underwent meniscus repair or not, followed the same rehabilitation protocol. Only the treatment group were given an adjustable frame with a four-point fixation knee brace (Hinge Knee Support Large, VR Support L.P., Thailand) for a duration of four weeks (Fig. 2). The braces are offered in four sizes: S, M, L, and XL. The fitting of the braces was conducted by physiotherapists.
Fig. 2.
An adjustable frame with a four-point fixation knee brace (Hinge Knee Support Large, VR Support L.P., Thailand).
The brace allowed for a range of motion between 0 and 60° in the first two weeks and 0–90° in the following two weeks. The control group were instructed to mobilise within the same restricted ranges. All patients were initially allowed to touch down their weight for the first two weeks. After this period, partial weight bearing was permitted, and full weight bearing was encouraged after one month. Knee stability examination and patient-reported outcomes including return to sports were collected at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years post-operatively. The possible complications such as ruptured grafts were collected. All outcome measurements were assessed by a sole assessor who was unaware of the treatment modality that patients had received.
The study employed an intention-to-treat analysis. To analyse the data, the continuous variables with normal distribution were presented as mean and standard deviation and were compared between the groups using a two-sample t-test. For non-normally distributed continuous data, the median and range were used, and comparisons between the groups were conducted using the Mann-Whitney U test. Categorical data were expressed as frequency and number, and Fisher's exact test was employed to compare between the brace and non-brace groups. Repeated measures were performed for multiple time comparisons using one-way analysis of variance (ANOVA) or Kruskal-Wallis with post hoc Bonferroni tests. Regarding the possible effects of follow-up periods, the comparisons of outcomes between groups were adjusted by time using multilevel mixed-effects generalised linear models.
The study sample size was determined based on an alpha error 0.05, a power of the study 0.80, mean IKDC of bracing from the pilot study 50 (SD 15) in brace, minimal clinically important difference (MCID) of 10 on the IKDC score.15, 16, 17 This calculation yielded 36 participants for each group. To account for a potential 15 % loss to follow-up, the sample was increased to 42 participants, totally 84 participants for two groups. All statistical analysis and sample size calculation was performed using STATA 16.1, StataCorp, College Station, Texas, USA. Significant p-value was set as < 0.05.
3. Results
This study included 95 patients who underwent ACL reconstruction from June 2020 to May 2021. Four patients with previous osteoarthritis and 7 patients with multiple ligament injury were excluded. The remaining 84 patients were randomly divided into two groups, non-brace, and brace group. At the final follow-up, there were 35 patients in non-brace group and 40 patients in brace group. No reports of complications associated with bracing were received, and all patients complied well with wearing the braces.
The baseline characteristics of both groups are displayed in Table 1. The patients in both groups are similar in terms of age, sex, body mass index, causes, and time before surgery. They also had similar intraoperative meniscus findings and underwent similar meniscus surgeries. In both groups, more than 80 % of patients received only the quadruple semitendinosus tendon for their graft, while the remaining patients required both semitendinosus and gracilis tendon grafts due to sizes. The mean femoral and tibial tunnel sizes were comparable in both groups. Preoperative patient-reported function, measured using the IKDC, Lysholm score, Tegner activity scale, and Visual Analogue Scale, as well as physical examination findings, including range of motion, Lachman test, anterior drawer test, pivot shift test, and single-leg hop test, showed no statistically significant differences between the two groups.
Table 1.
Baseline characteristics.
| Variables | Non-brace group (N = 42) | Brace group (N = 42) | P-value |
|---|---|---|---|
| Age (year), mean (SD) | 29.1 (9.4) | 30.8 (9.6) | 0.4107 |
| Male ( %) | 40 (95.2) | 35 (83.3) | 0.156 |
| Height (cm), mean (SD) | 170.3 (6.7) | 169.3 (6.5) | 0.4595 |
| Weight (kg), mean (SD) | 72.4 (14.9) | 71.2 (12.9) | 0.7014 |
| BMI (kg/m2), mean (SD) | 24.9 (4.7) | 24.7 (3.3) | 0.8200 |
| Time to surgery (month), median (range) | 11.5 (1–120) | 9 (1–85) | 0.0887 |
| Cause ( %) | |||
| Sports | 29 (69.1) | 27 (64.3) | 0.936 |
| Traffic | 8 (19.1) | 8 (19.1) | |
| Work | 2 (4.8) | 4 (9.5) | |
| ADL | 3 (7.1) | 3 (7.1) | |
| Medial meniscus ( %) | |||
| Intact | 16 (38.1) | 18 (42.9) | 0.807 |
| Partial meniscectomy | 8 (19.0) | 6 (14.3) | |
| Repair | 18 (42.9) | 18 (42.9) | |
| Lateral meniscus ( %) | |||
| Intact | 26 (61.9) | 20 (47.6) | 0.206 |
| Partial meniscectomy | 6 (14.3) | 4 (9.5) | |
| Repair | 10 (23.8) | 18 (42.9) | |
| Graft ( %) | |||
| Semitendinosus | 36 (85.7) | 35 (83.3) | 1.000 |
| Semitendinosus + Gracilis | 6 (14.3) | 7 (16.7) | |
| Femoral size (mm), mean (SD) | 8.2 (0.4) | 8.2 (0.5) | 0.9076 |
| Tibial size (mm), mean (SD) | 8.5 (0.4) | 8.4 (0.5) | 0.5062 |
| IKDC, mean (SD) | 50.4 (10.7) | 51.0 (14.1) | 0.8279 |
| Lysholm score, mean (SD) | 69.0 (14.9) | 67.0 (17.5) | 0.5743 |
| Tegner activity scale, mean (SD) | 3.4 (1.6) | 3.1 (2.3) | 0.3247 |
| VAS, median (range) | 0 (0–8) | 0 (0–5) | 0.1662 |
| Knee extension deficit ( %) | |||
| Normal | 41 (97.6) | 42 (100) | 1.000 |
| Nearly normal | 0 | 0 | |
| Abnormal | 0 | 0 | |
| Severely abnormal | 1 (2.4) | 0 | |
| Knee flexion deficit ( %) | |||
| Normal | 41 (97.6) | 41 (97.6) | 1.000 |
| Nearly normal | 0 | 1 (2.4) | |
| Abnormal | 0 | 0 | |
| Severely abnormal | 1 (2.4) | 0 | |
| Lachman test ( %) | |||
| Nearly normal | 3 (7.2) | 2 (4.8) | 0.257 |
| Abnormal | 30 (71.4) | 36 (85.7) | |
| Severely abnormal | 9 (21.4) | 4 (9.5) | |
| Anterior drawer test ( %) | |||
| Nearly normal | 1 (2.4) | 1 (2.4) | |
| Abnormal | 30 (71.4) | 36 (85.7) | |
| Severely abnormal | 11 (26.2) | 5 (11.9) | |
| Pivot shift test ( %) | |||
| Nearly normal | 25 (59.5) | 34 (81.9) | 0.055 |
| Abnormal | 17 (40.5) | 8 (19.1) | |
| One Leg Hop test ( %) | |||
| Normal | 1 (2.4) | 0 | 0.616 |
| Nearly normal | 0 | 0 | |
| Abnormal | 1 (2.4) | 3 (7.1) | |
| Severely abnormal | 40 (95.2) | 39 (92.9) | |
Table 2 demonstrates that the IKDC score, Lysholm score, Tegner activity scale, and VAS of both groups were significantly improved over time. However, there were no statistical differences between the two groups. At the end of the 2-year follow-up period, 35 patients (83.3 %) from the non-brace group and 40 patients (95.2 %) from the brace group had completed the study and found that only the Lysholm score and Tegner activity scale were significantly different between the two groups. (with p-values of 0.0408 and 0.0402, respectively). During the specified follow-up duration, the aforementioned physical examinations were also found to be statistically comparable between the two groups.
Table 2.
Multiple comparisons according to follow-up time.
| Variables | Non-brace group (N = 42) | Brace group (N = 42) | P-valueb |
|---|---|---|---|
| IKDC | |||
| Preoperative | 50.4 (10.7) | 51.0 (14.1) | 0.5743 |
| 6 months | 67.2 (10.1)c | 69.0 (12.0)c | 0.4711 |
| 1 year | 78.5 (10.3)c | 77.6 (12.2)c | 0.7473 |
| 2 years | 86.9 (8.6)c | 83.2 (10.0)c | 0.0812 |
| P-valuea | <0.0001* | <0.0001* | |
| Lysholm score | |||
| Preoperative | 69.0 (14.9) | 67.0 (17.5) | 0.5743 |
| 6 months | 85.6 (9.4)c | 84.6 (10.7)c | 0.6716 |
| 1 year | 90.3 (7.6)c | 88.7 (12.1)c | 0.4765 |
| 2 years | 95.2 (5.2)c | 92.0 (7.8)c | 0.0408* |
| P-valuec | <0.0001* | <0.0001* | |
| Tegner activity scale | |||
| Preoperative | 3.4 (1.6) | 3.1 (2.3) | 0.3247 |
| 6 months | 4.3 (1.6) | 4.1 (1.7)c | 0.6249 |
| 1 year | 5.9 (1.8)c | 5.4 (2.2)c | 0.3201 |
| 2 years | 6.7 (1.8)c | 5.8 (1.9)c | 0.0402* |
| P-valuea | <0.0001* | <0.0001* | |
| VAS | |||
| Preoperative | 0 (0–8) | 0 (0–5) | 0.1662 |
| 6 months | 0 (0–5) | 0 (0–2) | 0.8589 |
| 1 year | 0 (0–2)c | 0 (0-0)c | 0.2925 |
| 2 years | 0 (0-0)c | 0 (0-0)c | – |
| P-valuec | 0.0005* | 0.0032* | |
| Normal extension, n (%) | |||
| Preoperative | 41 (97.6) | 42 (100) | 1.000 |
| 6 months | 41 (97.6) | 41 (97.6) | 1.000 |
| 1 year | 37 (100) | 41 (100) | – |
| 2 years | 35 (100) | 39 (100) | – |
| P-value# | 1.000 | 1.000 | |
| Normal flexion, n (%) | |||
| Preoperative | 41 (97.6) | 41 (97.6) | 1.000 |
| 6 months | 42 (100) | 42 (100) | – |
| 1 year | 37 (100) | 41 (100) | – |
| 2 years | 34 (97.1) | 39 (100) | 0.473 |
| P-value# | 0.455 | 1.000 | |
| Negative Lachman test, n (%) | |||
| Preoperative | 0 | 0 | 0.257 |
| 6 months | 42 (100) | 42 (100) | – |
| 1 year | 37 (100) | 41 (100) | – |
| 2 years | 35 (100) | 39 (100) | – |
| P-value# | <0.001* | <0.001* | |
| Negative Anterior drawer test, n (%) | |||
| Preoperative | 0 | 0 | 0.216 |
| 6 months | 32 (76.2) | 24 (57.1) | 0.104 |
| 1 year | 27 (73.0) | 23 (56.1) | 0.158 |
| 2 years | 25 (71.4) | 22 (56.4) | 0.229 |
| P-value# | <0.001* | <0.001* | |
| Negative Pivot shift test, n (%) | |||
| Preoperative | 0 | 0 | 0.055 |
| 6 months | 42 (100) | 42 (100) | – |
| 1 year | 37 (100) | 41 (100) | – |
| 2 years | 35 (100) | 39 (100) | – |
| P-value# | <0.001* | <0.001* | |
| Negative One Leg Hop test, n (%) | |||
| Preoperative | 1 (2.4) | 0 | 0.616 |
| 6 months | 0 | 1 (2.4) | 1.000 |
| 1 year | 6 (16.2) | 5 (12.2) | 0.862 |
| 2 years | 14 (40.0) | 8 (20.5) | 0.054 |
| P-value# | <0.001* | <0.001* | |
VAS = visual analogue scale.
p-value according to time comparisons,
p-value comparing between non-brace and brace groups.
Significant p-value <0.05 when compared to preoperative time, *significant p-value <0.05.
Table 3 reveals that the brace group had significantly lower Tegner activity scale (−0.45, 95 % confidence interval (CI) −0.83, −0.07, p-value = 0.0022) and VAS (−0.28, 95 %CI -0.50, −0.04, p-value = 0.0023) than the non-brace group after adjustment for time. In multivariate analysis, bracing was found to be significantly associated with lower Tegner activity scale than the non-brace group after adjustment for VAS and time (−0.49, 95 %CI -0.87, 0.10, p-value = 0.013) (see Table 4).
Table 3.
Univariate analysis comparing outcomes between brace and non-brace (baseline) and adjusted by time.
| Variables | Coefficient | 95 % confidence interval | Standard error | P-value |
|---|---|---|---|---|
| IKDC | −0.47 | −2.97, 2.04 | 1.28 | 0.714 |
| Lysholm score | −1.91 | −4.53, 0.70 | 1.33 | 0.151 |
| Tegner activity scale | −0.45 | −0.83, −0.07 | 0.20 | 0.022* |
| VAS | −0.28 | −0.50, −0.04 | 0.12 | 0.023* |
Non-brace was used as a baseline group, *significant p-value <0.05.
Table 4.
The multivariate analysis parsimonious model comparing Tegner activity scale between brace and non-brace (baseline), and adjusted by time and VAS.
| Variables | Coefficient | 95 % confidence interval | Standard error | P-value |
|---|---|---|---|---|
| Tegner activity scale | −0.49 | −0.87, −0.10 | 0.20 | 0.013a |
| Time | 1.04 | 0.86, 1.22 | 0.09 | <0.001a |
| VAS | −0.08 | −0.26, −0.10 | 0.09 | 0.400 |
Significant p-value <0.05.
For the multivariate analysis adjusted by time and VAS, subgroup analysis was conducted based on meniscus surgery and no meniscus surgery. In cases where only meniscus surgery was performed, the brace group exhibited an insignificantly lower Tegner activity scale of −0.33 (95 % CI -0.78, 0.12, p-value = 0.150) compared to the non-brace group. However, in instances without meniscus surgery, the bracing group showed a significantly lower Tegner activity scale of −0.87 (95 % CI -1.30, −0.43, p-value <0.001). Consequently, the choice of rehabilitation approach, whether with or without a brace, did not yield significant improvements in functional outcomes in ACL reconstruction, irrespective of meniscus repair.
Throughout the follow-up period, no cases of graft rupture were observed in either group. Furthermore, at the conclusion of the follow-up, there was no significant difference in the level of return to sports between the non-brace and brace groups, as shown in Table 5.
Table 5.
The comparison of return to sports between groups.
| Variables | Non-brace group (N = 42) | Brace group (N = 42) | P-value |
|---|---|---|---|
| Return to sports ( %) | |||
| Competitive | 5 (11.9) | 4 (9.5) | 0.213 |
| Frequently | 23 (54.8) | 16 (38.1) | |
| Sometimes | 6 (14.3) | 14 (33.3) | |
| Non sporting | 8 (19.1) | 8 (19.1) | |
4. Discussion
The findings of this study confirm our hypothesis that brace-free ACL reconstruction is comparable to a brace-based approach in terms of patient-reported subjective outcomes and physically examined objective outcomes.
The increasing number of anterior cruciate ligament (ACL) reconstructions performed annually places a burden on the healthcare system, resulting in significant associated costs.18,19 Outcomes of ACL reconstruction are assessed using subjective and objective measures such as IKDC 2000 scores, Lysholm score, and Tegner activity scale. These measures offer valid and consistent documentation of the ligamentous and functional status of a knee joint.20
In terms of the IKDC score, this study observed lower scores at the preoperative stage, during the follow-ups, and at the final assessment compared to a prior study.21 However, there was a significant increase in the IKDC scores throughout the follow-up period. These observations may be attributed to variations in the population groups studied. The Lysholm score demonstrated comparability with findings from previous studies. Significantly improved scores were noted over the 2-year follow-up period in both groups.21,22
Rehabilitation is one of the important factors that affect the outcomes of ACL reconstruction. However, there is no consensus on various rehabilitation programmes.23 While bracing can provide initial support to the knee in the early stages of rehabilitation after ACL reconstruction, research has shown that knee braces have no significant clinical benefits beyond a psychological sense of security. Prolonged use of a brace may result in muscle atrophy and subsequent declines in function and proprioception. Several studies have confirmed these drawbacks.24 Choi et al. conducted a study that predicted a weakening of the vastus medialis obliquus (VMO) with long-term brace use.6 Therefore, many experts suggest that braces do not enhance long-term functional outcomes.25
The prescription of braces results in significant costs for the healthcare system.26 After studying the rehabilitation of 32 cases of ACL reconstruction, Naik concluded that rehabilitation without a knee brace can indirectly prevent re-rupture and is a cost-effective and safer approach with improved outcomes.27 Overall, while there have been several meta-analyses on bracing after ACL reconstruction, the findings have been mixed and suggest that the use of knee bracing should be individualised based on the patient's specific needs and preferences.8
In this study, the occurrence of meniscus tears revealed that 59.5 % of patients exhibited medial meniscus tears, while 45.2 % had lateral meniscus tears. These figures align with findings from previous studies.28,29 Only 42.9 % of patients underwent medial meniscus repair, while 33.3 % of patients received lateral meniscus repair. The remaining tears were treated with partial meniscectomy for minor and irreparable tears. Our study found comparable subjective and objective functional outcomes between brace-free and brace-based rehabilitation approaches following ACL reconstruction, regardless of meniscus repair.
Unlike previous findings,21,22 our study revealed a statistical finding that suggested brace use was associated with a lower Tegner activity scale at the end of the 2-year follow-up period. It is important to recognise that prolonged brace use may lead to muscle atrophy, which can subsequently affect the overall strength and function of the knee joint. This could potentially explain the lower Tegner activity scale observed in the brace group compared to the non-brace group. However, it's important to note that this difference was less than the minimal clinically important difference.
The limitations of this study include not comparing different types of meniscus injuries and types of meniscus repair performed with ACL reconstruction, as they may affect the postoperative plan. Furthermore, this study combined all kinds of meniscus repair, ranging from simple horizontal tears to posterior meniscus root tears. Future studies may be conducted to answer these specific questions.
Nevertheless, these findings highlight the need for a comprehensive understanding of the potential drawbacks associated with brace usage in ACL reconstruction patients. While braces may provide initial stability and psychological reassurance, their prolonged use should be carefully considered to avoid potential muscle atrophy and subsequent limitations in activity levels. Further research is warranted to explore the underlying mechanisms behind these observations and to develop evidence-based recommendations regarding the appropriate duration and timing of brace use in the rehabilitation process following ACL reconstruction. By addressing these aspects, clinicians can optimise rehabilitation strategies and improve long-term functional outcomes for patients undergoing ACL reconstruction.
5. Conclusion
ACL reconstruction without a brace is as effective as a brace-based approach, irrespective of additional meniscus surgery. Therefore, the routine use of a postoperative brace should be discontinued. Additionally, brace use may result in a slightly lower Tegner activity scale in patients undergoing ACL reconstruction, although the difference is not clinically significant.
Funding/support statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Footnotes
The material contained in the manuscript has not been previously published and is not being concurrently submitted elsewhere.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.asmart.2024.01.006.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Sanders T.L., Maradit Kremers H., Bryan A.J., et al. Incidence of anterior cruciate ligament tears and reconstruction. Am J Sports Med. 2016;44(6):1502–1507. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 2.Kruse L.M., Gray B., Wright R.W. Rehabilitation after anterior cruciate ligament reconstruction. J Bone Joint Surg. 2012;94(19):1737–1748. doi: 10.2106/JBJS.K.01246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cavanaugh J.T., Killian S.E. Rehabilitation following meniscal repair. Curr Rev Musculoskelet Med. 2012;5(1):46–58. doi: 10.1007/s12178-011-9110-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marois B., Tan X.W., Pauyo T., Dodin P., Ballaz L., Nault M.L. Can a knee brace prevent ACL reinjury: a systematic review. Int J Environ Res Publ Health. 2021;18(14):7611. doi: 10.3390/ijerph18147611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giotis D., Paschos N.K., Zampeli F., Pappas E., Mitsionis G., Georgoulis A.D. Bracing can partially limit tibial rotation during stressful activities after anterior crucial ligament reconstruction with a hamstring graft. J Orthop Traumatol: Surgery & Research. 2016;102(5):601–606. doi: 10.1016/j.otsr.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Choi E.H., Kim K.K., Jun A.Y., Choi E.H., Choi S.W., Shin K.Y. Effects of the off-loading brace on the activation of femoral muscles -A preliminary study- Ann Rehabil Med. 2011;35(6):887. doi: 10.5535/arm.2011.35.6.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healy A., Farmer S., Pandyan A., Chockalingam N. A systematic review of randomised controlled trials assessing effectiveness of prosthetic and orthotic interventions. PLoS One. 2018;13(3) doi: 10.1371/journal.pone.0192094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X gang, tao Feng J., He X., Wang F., Hu Y. The effect of knee bracing on the knee function and stability following anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. J Orthop Traumatol: Surgery & Research. 2019;105(6):1107–1114. doi: 10.1016/j.otsr.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Hagino T., Ochiai S., Senga S., et al. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg. 2015;135(12):1701–1706. doi: 10.1007/s00402-015-2309-4. [DOI] [PubMed] [Google Scholar]
- 10.Koch M., Memmel C., Zeman F., et al. Early functional rehabilitation after meniscus surgery: are currently used orthopedic rehabilitation standards up to date? Rehabil Res Pract. 2020;2020:1–8. doi: 10.1155/2020/3989535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tuca M., Valderrama I., Eriksson K., Tapasvi S. Current trends in anterior cruciate ligament surgery. A worldwide benchmark study. Journal of ISAKOS. 2023;8(1):2–10. doi: 10.1016/j.jisako.2022.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Lertwanich P., Praphruetkit T., Keyurapan E., Lamsam C., Kulthanan T. Validity and reliability of Thai version of the international knee documentation committee subjective knee form. J Med Assoc Thai. 2008;91(8):1218–1225. [PubMed] [Google Scholar]
- 13.Briggs K.K., Lysholm J., Tegner Y., Rodkey W.G., Kocher M.S., Steadman J.R. The reliability, validity, and responsiveness of the Lysholm score and tegner activity scale for anterior cruciate ligament injuries of the knee. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 14.Irrgang J.J., Anderson A.F., Boland A.L., et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 15.Copay A.G., Eyberg B., Chung A.S., Zurcher K.S., Chutkan N., Spangehl M.J. Minimum clinically important difference: current trends in the orthopaedic literature, Part II: lower extremity. JBJS Rev. 2018;6(9) doi: 10.2106/JBJS.RVW.17.00160. e2-e2. [DOI] [PubMed] [Google Scholar]
- 16.Çelik D., Ö Çoban, Kılıçoğlu Ö. Minimal clinically important difference of commonly used hip-, knee-, foot-, and ankle-specific questionnaires: a systematic review. J Clin Epidemiol. 2019;113:44–57. doi: 10.1016/j.jclinepi.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Huang H., Nagao M., Arita H., et al. Validation and defining the minimal clinically important difference of the Japanese version of the IKDC Subjective Knee Form. J Orthop Sci. 2021;26(1):149–155. doi: 10.1016/j.jos.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 18.Deviandri R., van der Veen H.C., Lubis A.M., Utoyo G.A., van den Akker-Scheek I., Postma M.J. Burden and cost of anterior cruciate ligament reconstruction and reimbursement of its treatment in a developing country: an observational study in Indonesia. Clin Outcomes Res. 2022;14:479–486. doi: 10.2147/CEOR.S368840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carbone A.D., Wang K., Tiao J., et al. Trends in health care expenditures and patient out-of-pocket expenses in primary anterior cruciate ligament reconstruction. Am J Sports Med. 2022;50(10):2680–2687. doi: 10.1177/03635465221107082. [DOI] [PubMed] [Google Scholar]
- 20.van Meer B.L., Meuffels D.E., Vissers M.M., et al. Knee injury and osteoarthritis outcome score or international knee documentation committee subjective knee form: which questionnaire is most useful to monitor patients with an anterior cruciate ligament rupture in the short term? Arthrosc J Arthrosc Relat Surg. 2013;29(4):701–715. doi: 10.1016/j.arthro.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Mayr H.O., Stüeken P., Münch E.O., et al. Brace or no-brace after ACL graft? Four-year results of a prospective clinical trial. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1156–1162. doi: 10.1007/s00167-013-2564-2. [DOI] [PubMed] [Google Scholar]
- 22.Lowe W.R., Warth R.J., Davis E.P., Bailey L. Functional bracing after anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2017;25(3):239–249. doi: 10.5435/JAAOS-D-15-00710. [DOI] [PubMed] [Google Scholar]
- 23.Culvenor A.G., Girdwood M.A., Juhl C.B., et al. Rehabilitation after anterior cruciate ligament and meniscal injuries: a best-evidence synthesis of systematic reviews for the OPTIKNEE consensus. Br J Sports Med. 2022;56(24):1445–1453. doi: 10.1136/bjsports-2022-105495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glattke K.E., Tummala S.V., Chhabra A. Anterior cruciate ligament reconstruction recovery and rehabilitation. J Bone Joint Surg. 2022;104(8):739–754. doi: 10.2106/JBJS.21.00688. [DOI] [PubMed] [Google Scholar]
- 25.Di Miceli R., Marambio C., Zati A., Monesi R., Benedetti M. Do knee bracing and delayed weight bearing affect mid-term functional outcome after anterior cruciate ligament reconstruction? Joints. 2017;5(4):202–206. doi: 10.1055/s-0037-1606617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mayr H.O., Stüeken P., Münch E.O., et al. Brace or no-brace after ACL graft? Four-year results of a prospective clinical trial. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1156–1162. doi: 10.1007/s00167-013-2564-2. [DOI] [PubMed] [Google Scholar]
- 27.Naik A.A., Das B., Kamat Y.D. Avoid post operative bracing to reduce ACL rerupture rates. Eur J Orthop Surg Traumatol. 2019;29(8):1743–1747. doi: 10.1007/s00590-019-02521-4. [DOI] [PubMed] [Google Scholar]
- 28.Cain E., Fleisig G., Ponce B., et al. Variables associated with chondral and meniscal injuries in anterior cruciate ligament surgery. J Knee Surg. 2017;30(7):659–667. doi: 10.1055/s-0036-1593875. [DOI] [PubMed] [Google Scholar]
- 29.Michalitsis S., Vlychou M., Malizos K.N., Thriskos P., Hantes M.E. Meniscal and articular cartilage lesions in the anterior cruciate ligament-deficient knee: correlation between time from injury and knee scores. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):232–239. doi: 10.1007/s00167-013-2497-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.