Abstract
Soft tissue and bone defects that occur consequence of high-energy trauma are serious and challenging problems. The aim of this retrospective cohort study is to show that the artificial deformity creation (ADCr) method allows the closure of soft-tissue defects, avoids amputation, and can facilitate the reconstruction of bone defects and restore limb length.
Patients and methods
Twenty-six adult patients (age range 20–81 years) with soft tissue defects of the lower limb were treated at the Riga East University Hospital from 2018 to 2021. All patients were treated using the ADCr method which is the technique of establishing an interim deformity for resolving tissue loss. The lower extremity functional scale (LEFS) and application of methods of ilizarov (ASAMI) criteria were used for the evaluation of bone healing and lower extremity function.
Results
Complete union was achieved in all cases. The functional evaluation showed that most patients could achieve excellent and good results and return to activities of daily living. The functional result was poor in one case of a multi-fragmentary distal tibial articular fracture for which an ankle fusion was performed. Final union in this case was achieved with some residual deformity.
Conclusion
The method of ADCr is an effective surgical technique in cases of severe tibial injuries with concomitant loss of bone and soft tissues. This method could be used in cases when either a plastic or microsurgeon is not available or for instances when closing the defect with a flap is either impossible or contraindicated. Excellent and good functional results are possible without severe complications.
How to cite this article
Plotnikovs K, Kamenska J, Movcans J, et al. Artificial Deformity Creation as a Method for Limb Salvage for Patients with Massive Tibial and Soft Tissue Defects: A Report of 26 Cases. Strategies Trauma Limb Reconstr 2023;18(3):133–139.
Keywords: Artificial deformity creation, Ilizarov, Interim deformity, Limb lengthening, Limb salvage, Ortho-SUV frame
Introduction
Treatment of high-energy trauma or infection may face problems of soft tissue and bone defects, both of which are serious and challenging problems.1,2 These problems need highly skilled medical personnel, sufficient time and resources, and a high level of patient compliance. In some cases, it is not possible to advocate solving the soft tissue defect with a flap. The method of artificial deformity creation (ADCr) by shortening, rotation, and angulation of the limb facilitates primary closure of the soft tissue defect in the first instance. Once the soft tissue is healed, the interim deformity is then eliminated by techniques based on distraction histogenesis. An alternative terminology to this method is, applicable too to cases where acute shortening of the limb is performed to eliminate a bone defect (and where soft tissue closure is not the primary problem), creation of interim deformities for tissue loss (CIDTL). This method allows closure of soft-tissue defects, avoids amputation, and can facilitate reconstruction of bone defects and restore limb length.3–7 Patients are able to return to normal daily levels of activities.7–9 The aim of this report is to present a case series of successful limbs salvage by ADCr.
Patients and Methods
Twenty-six adult patients (age range 20–81 years) with soft tissue defects of the lower limb were treated at Riga East University Hospital from 2018 to 2021 (Table 1). There were 15 patients with open Gustilo–Anderson type III B tibial fractures and 11 patients with infected tibial non-unions. The fractures were also classified according to the AO/OTA system. The sizes of bone and soft tissue defects were estimated after debridement. There was bone loss in 16 cases.
Table 1.
Patients in study
| Case no. | Age (years) | The main problem | Fracture type (AO) | Gustilo-Anderson | Bone loss (cm) | Soft-tissue defect (cm) |
|---|---|---|---|---|---|---|
| 1 | 81 | Fracture | 42–B2 | 3B | – | 9 × 6 |
| 2 | 58 | Fracture | 43–C3 | 3B | 9,8 | 18 × 9 |
| 3 | 57 | Fracture | 42–A2 | 3B | – | 5 × 8 |
| 4 | 65 | Fracture | 42–A3 | 3B | – | 2 × 5 |
| 5 | 51 | Fracture | 43–A3 | 3B | 5 | 8 × 6 |
| 6 | 30 | Fracture | 42–C3 | 3B | – | 2 × 7 |
| 7 | 39 | Fracture | 43–A2 | 3B | – | 1.5 × 3 |
| 8 | 20 | Fracture | 42–B3 | 3B | 2 | 2 × 5 |
| 9 | 57 | Fracture | 41–A3 | 3B | 1 | 2,5 × 8 |
| 10 | 56 | Fracture | 41–C3 | 3B | 3 | 4 × 7 |
| 11 | 35 | Fracture | 43–C3 | 3B | 8 | 11 × 8 |
| 12 | 54 | Fracture | 43–A2 | 3B | – | 1,5 × 4 |
| 13 | 37 | Fracture | 42–A1 | 3B | – | 2 × 5 |
| 14 | 57 | Fracture | 41–C3 | 3B | 3 | 4 × 8 |
| 15 | 23 | Fracture | 42–A2 | 3B | – | 4 × 8 |
| 16 | 47 | Infection | 44–B3 | – | 2,5 | 5 × 9 |
| 17 | 33 | Infection | 42–B2 | 2 | – | 2 × 5 |
| 18 | 59 | Infection | 42–B2 | 2 | – | 1,5 × 4 |
| 19 | 43 | Infection | 42–B2 | 2 | 3 | 3 × 5 |
| 20 | 41 | Infection | 42–C2 | 3B | 5 | 4 × 6 |
| 21 | 68 | Infection | 41–C2 | – | 3 | 7 × 3 |
| 22 | 46 | Infection | 42–B3 | – | 5 | 6 × 2,5 |
| 23 | 21 | Infection | 41–C3 | – | 3 | 10 × 3 |
| 24 | 45 | Infection | 42–B3 | 2 | 2 | 2 × 4 |
| 25 | 62 | Infection | 42–A2 | 2 | 6 | 17 × 12 |
| 26 | 33 | Infection | 42–C3 | 3B | 7 | 9 × 5 |
All the patients were treated using the ADCr method to ensure primary soft tissue closure and subsequently underwent a gradual restoration of anatomical alignment. All details of these cases are listed in Table 2. For all cases, the initial fixation was performed with a circular external fixator. In 23 cases a hexapod circular fixator was used for multicomponent deformity correction.
Table 2.
Artificially created deformity description
| Case no. | Translation (cm) | Angulation (°) | Rotation (°) | Length reduction (cm) |
|---|---|---|---|---|
| 1 | A 1, L 3 | V 18, AP 8 | Inner 90 | TB 2 |
| 2 | P 3, M 1 | V 32, AP 45 | Inner 15 | 9,8 |
| 3 | – | – | – | TB 4 |
| 4 | – | V 13, AP 9 | – | – |
| 5 | – | V 25, AP 9 | Inner 30 | 5 |
| 6 | – | V 7, AP 8 | – | – |
| 7 | M 1 | V 10 | – | TB 1 |
| 8 | – | V 12, AP 5 | – | 2 |
| 9 | – | V 17, AP 10 | Inner 10 | 1 |
| 10 | – | V 10, AP 7 | Inner 15 | 3 |
| 11 | – | – | – | 8 |
| 12 | – | V 13 | – | TB 1 |
| 13 | – | V 5 | – | TB 2 |
| 14 | M 1,5 | V 8 | – | 3 |
| 15 | L 2,5 | V 12, AP 5 | – | TB 2 |
| 16 | – | V 29 | – | 2,5 |
| 17 | – | V 17, AP 31 | Inner 10 | – |
| 18 | – | V 21, AP 10 | – | TB 1 |
| 19 | – | – | – | 3 |
| 20 | – | AP 16 | – | 5 |
| 21 | – | AP 10 | – | 3 |
| 22 | – | AP 26 | – | 5 |
| 23 | – | AP 5 | Inner 25 | 3 |
| 24 | – | – | – | 2 |
| 25 | – | V 20 | Inner 15 | 6 |
| 26 | – | V 19, AP 3 | Inner 24 | 7 |
A, anterior; AP, apex posterior; L, lateral; M, medial; P, posterior; TB, tibial bayonet method; V, varus
The lower extremity functional scale (LEFS) was used at 6 and 12 months after frame removal and the application of methods of ilizarov (ASAMI) criteria were used for evaluating bone healing and lower extremity function. Radiologic results were evaluated on both anteroposterior and lateral X-rays.
Results
The average patients’ age was 46.9 years (20–81) with 77% of patients being male. There were 15 patients with acute Gustilo-Anderson type III B open tibial fractures and 11 patients with osteomyelitis following tibial fracture treatment. Using the AO/OTA classification, five cases were in the proximal (41) tibia and five in the distal tibia. There were 15 cases in the tibial shaft (42), with the last case of a pilon-type fracture (44). There were several patients with comorbidities. Two patients with osteomyelitis had previous Gustilo type III B tibial fractures, five had Gustilo type II fractures and four had closed tibia fractures. Smokers accounted for 46.1% (n = 12) whereas 30.8% (n = 8) admitted excessive alcohol use. Seven patients had cardiovascular system pathology, two patients had diabetes mellitus, two other patients had hematopoietic system disorders, one patient had obesity, and one patient had a mental disorder.
The characteristics of tissue loss were as follows: the mean bone loss was 4.27 cm (1–9.8 cm); the soft tissue defects in both groups had a mean size of 5.5 cm × 5.98 cm (1.5 × 3–17 × 12 cm).
Wound closure was obtained primarily in 25 cases; in case no. 2 a skin graft was added. In all the cases wound closure was achieved in plastic surgery.
The average external fixation period was 333 days (range 155–563 days). The mean deformity correction period was 14.5 days (range 3–39 days). In 15 cases additional lengthening was needed and for this to be accomplished a corticotomy was performed. The mean distraction period was 57.2 days (range 20–100 days). The average index of lengthening (days in frame per cm of bone loss) was 103.71 (range 49.59–212, Table 3).
Table 3.
Deformity correction and lengthening
| Case no. | External fixation period (days) | Index of lengthening | Deformity correction period (days) | Distraction period (days) |
|---|---|---|---|---|
| 1 | 344 | – | 32 | – |
| 2 | 486 | 49, 59 | 36 | 89 |
| 3 | 236 | – | 39 | – |
| 4 | 155 | – | 7 | – |
| 5 | 479 | 95, 8 | 12 | 90 |
| 6 | 283 | – | 3 | – |
| 7 | 227 | – | 13 | – |
| 8 | 341 | 170, 5 | 3 | 20 |
| 9 | 350 | – | 7 | – |
| 10 | 563 | 187, 67 | 7 | 30 |
| 11 | 297 | 37, 125 | – | 65 |
| 12 | 178 | – | 10 | – |
| 13 | 266 | – | 15 | – |
| 14 | 232 | 77, 3 | 9 | 40 |
| 15 | 330 | – | 12 | – |
| 16 | 221 | 88, 4 | 18 | 28 |
| 17 | 252 | – | 15 | – |
| 18 | 277 | – | 28 | – |
| 19 | 305 | 101, 67 | – | 35 |
| 20 | 340 | 68 | 8 | 55 |
| 21 | 326 | 108, 67 | 6 | 40 |
| 22 | 476 | 95, 2 | 9 | 64 |
| 23 | 391 | 130, 3 | 7 | 35 |
| 24 | 424 | 212 | – | 83 |
| 25 | 372 | 62 | 19 | 85 |
| 26 | 500 | 71, 43 | 19 | 100 |
Complete bone union was achieved in all cases. Using the ASAMI bone score 88.5% (n = 23) were classed as excellent, and there were 11.5% (n = 3) good. In 88.5% (n = 23) bone union was achieved with normal alignment angles and with the absence of a limb length discrepancy. In case No. 18, the final alignment was unsatisfactory (outside the normal values) whereas, in case no. 9, bone union was achieved with correct alignment but with inequality limb lengths.
The average LEFS score was 67.7% (range 31.3–92.5%) after fixator removal. This increased to 86.7% (range 36.3–100%) at 6 months and reached 91.5% (47.5–100%) at 1 year. Using the ASAMI functional scores, 53.9% (n = 14) were classed as excellent, 23.1% (n = 6) as good, 19.2% (n = 5) as fair and 3.9% (n = 1) as poor.
Fair results using the ASAMI functional score system were achieved in cases no. 9, 10, 14, 21, and 23. In all these cases, the patients had distal tibial fractures (AO/OTA 41). Case nos. 10, 14, and 23 had articular multi-fragmentary proximal tibial fractures (41–C3); case no. 21 had a simple articular, metaphyseal multi-fragmentary proximal tibial fracture (AO/OTA 41–C2) and case no. 9 a metaphyseal multi-fragmentary proximal tibial fracture (AO/OTA 41–A3).
The most frequent complication seen in patients was a pin-site infection which was present in 30.8% (n = 8). Four patients (15.4%) had deep infection whereas one patient (3.85%) had a superficial infection. A neurotrophic complication occurred in one (3.9%) patient (Table 4).
Table 4.
Results
| Case no. | Results at the time of dismantling* | LEFS after dismantling (%) | LEFS 6 m (%) | LEFS 12 m (%) | ASAMI functional score | ASAMI bone score | Complications |
|---|---|---|---|---|---|---|---|
| 1 | 1 | 82.5 | 97.5 | 97.5 | Excellent | Excellent | Pin–site infection |
| 2 | 1 | 61.25 | 87.5 | 90 | Good | Excellent | Pin–site infection |
| 3 | 1 | 80 | 92.5 | 100 | Excellent | Excellent | – |
| 4 | 1 | 75 | 93.75 | 100 | Excellent | Excellent | – |
| 5 | 1 | 68.75 | 90 | 97.5 | Good | Excellent | Neurotrophic complications |
| 6 | 1 | 90 | 100 | 100 | Excellent | Excellent | – |
| 7 | 1 | 65 | 90 | 97.5 | Excellent | Excellent | – |
| 8 | 1 | 92.5 | 100 | 100 | Excellent | Excellent | – |
| 9 | 3 | 46.25 | 68.75 | 78.75 | Fair | Good | Pin–site infection |
| 10 | 1 | 47.5 | 60 | 70 | Fair | Excellent | Pin–site infection |
| 11 | 4 | 31.25 | 36.25 | 47.5 | Poor | Good | Deep infection |
| 12 | 1 | 68.75 | 81.25 | 91.25 | Good | Excellent | Pin–site infection |
| 13 | 1 | 85 | 97.5 | 100 | Excellent | Excellent | – |
| 14 | 1 | 45 | 51.25 | 63.75 | Fair | Excellent | – |
| 15 | 1 | 85 | 95 | 100 | Excellent | Excellent | Pin–site infection |
| 16 | 1 | 42.5 | 77.5 | 87.5 | Good | Excellent | – |
| 17 | 1 | 80 | 97.5 | 100 | Excellent | Excellent | – |
| 18 | 2 | 50 | 81.25 | 90 | Good | Good | Pin–site infection |
| 19 | 1 | 81.25 | 92.5 | 100 | Excellent | Excellent | – |
| 20 | 1 | 63.75 | 90 | 95 | Good | Excellent | Pin–site infection |
| 21 | 1 | 48.75 | 60 | 68.75 | Fair | Excellent | – |
| 22 | 1 | 75 | 95 | 100 | Excellent | Excellent | – |
| 23 | 1 | 52.5 | 60 | 68.75 | Fair | Excellent | Deep infection |
| 24 | 1 | 77.5 | 92.5 | 97.5 | Excellent | Excellent | Deep infection |
| 25 | 1 | 78.75 | 90 | 95 | Excellent | Excellent | Superficial infection |
| 26 | 1 | 87.5 | 92.5 | 97.5 | Excellent | Excellent | Deep infection |
*1, Consolidation within the correct reference lines and angles (RLA) values and the absence of limb length discrepancy; 2, Expected consolidation at unsatisfactory (outside the normal RLA values) arrangement of fragments with/without shortening; 3, Consolidation within the correct RLA values and with inequality in the lengths of the limbs; 4, Consolidation with deformation
Case Example
The implementation of the ADCr method is presented. For the treatment of a patient who sustained a Gustilo IIIB open distal tibial fracture with an extensive bone and soft tissue defect, an acute shortening of the limb by 1 cm and angulation of 44° was performed. This procedure allowed for primary closure of the soft tissue wound without tension, without the need for further additional microsurgical tissue transfer. After subsequent correction of the interim deformity using a hexapod circular fixator, an additional docking-site procedure with autologous bone grafting was performed (Figs 1 to 7).
Fig. 1.

Clinical appearance of the injured limb
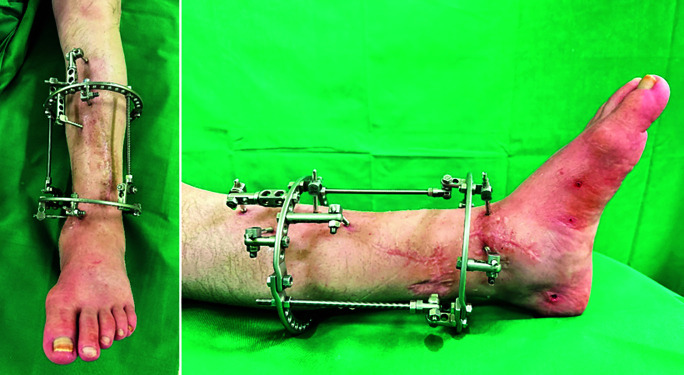
Fig. 7.
Clinical appearance of the limb after deformity correction and after hexapod and foot ring removal
Fig. 2.

Clinical appearance after surgical debridement
Fig. 3.
Clinical appearance after application of ADCr method
Fig. 4.

Digital subtraction angiography (DSA) showing vessels in the area of interim limb deformity
Fig. 5.

Tubular external fixator conversion to circular frame
Fig. 6.
Deformity correction using circular fixator hexapod ortho-SUV
Discussion
The tibia is the most common site for bone loss after a fracture and owing to the limited soft tissue cover, tibial fractures are predisposed to be open. Open fractures can be associated with large soft tissue defects (Gustilo–Anderson type III B and III C).1 Such open tibial fractures are emergencies because of a high risk of infection and further tissue devitalization.2,3,10 In addition to bone loss arising directly from trauma, bone defects can also arise from repetitive debridement in cases of osteomyelitis or of non-union. Fracture stabilization and definitive soft tissue cover should be performed at the same time as debridement or within 72 hours of injury.2 Treatment of these injuries and the consequences of such fractures are complex.1,2 The “classic” option for closure of soft tissue defects is to use a free or rotational flap.3,7,11–14 There are limitations for flap use: In single vessels in injured limbs; in patients with significant vascular comorbidities or in the absence of a microsurgeon.3–7,11 The aim of our study was to show an alternative method for limb salvage and reconstruction and to demonstrate how to manage bone and soft tissue defects simultaneously.
The literature describes the Ilizarov apparatus as the best choice for deformity correction after using the ADCr method.3,4,12,14,15 Shortening, angulation, and rotational components of the interim deformity have complex multicomponent and multi-plane characteristics. To correct each component of the deformity by using the Ilizarov device, each component of the deformity will need addressing by sequential repositioning of the correction units with partial apparatus reassembly each time.16,17 Each component of the deformity can add to a reduction in the accuracy of final correction by virtue of complexity.17,18 Through using a circular fixator hexapod, highly accurate correction is achievable without the need for the reassembly of individual correction units.16
A total of 26 patients were included in our study which may represent the largest series to date. A previous retrospective cohort study that described a similar technique for soft-tissue defect closure had 19 patients.3 The functional evaluation from this case series has shown that most patients can achieve excellent and good results and return to active daily living. An exception was in case no. 11 where the functional results were poor. This patient had a multi-fragmentary distal tibial articular fracture (AO/OTA 43–C3) for which an ankle fusion was performed. Furthermore, the final result had a residual deformity in the limb.
Conclusion
The method of ADCr is an effective surgical technique for cases of severe injuries of the tibia where there are soft tissue defects with or without bone defects. It is a method useful in cases when a microsurgeon is not available or when closing the defect with a flap is either inadvisable or contraindicated.
Orcid
Konstantins Plotnikovs https://orcid.org/0000-0002-6631-9343
Jekaterina Kamenska https://orcid.org/0000-0002-6998-5835
Jevgenijs Movcans https://orcid.org/0000-0003-0561-4696
Leonid Solomin https://orcid.org/0000-0003-3705-3280
Haralds Plaudis https://orcid.org/0000-0002-3951-5437
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Adamczyk A, Meulenkamp B, Wilken G, et al. Managing bone loss in open fractures. OTA Int. 2020;3(1):e059. doi: 10.1097/OI9.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.British Orthopaedic Association; British Association of Plastic Reconstructive and Aesthetic Surgeons. 2017. Audit Standards for Trauma: OPEN FRACTURES.https://www.nice.org.uk/guidance/NG37/chapter/recommendations Available from: [Google Scholar]
- 3.Hernández-Irizarry R, Quinnan SM, Reid JS, et al. Intentional temporary limb deformation for closure of soft-tissue defects in open tibial fractures. J Orthop Trauma. 2021;35(6):e189–e94. doi: 10.1097/BOT.0000000000001988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lerner A, Fodor L, Soudry M, et al. Acute shortening Modular treatment modality for severe combined bone and soft tissue loss of the extremities. J Trauma. 2004;57(3):603–608. doi: 10.1097/01.ta.0000087888.01738.35. [DOI] [PubMed] [Google Scholar]
- 5.Plotnikovs K, Ribakovs O, Movcans J, et al. A 52-Year-Old Man with a Gustilo-Anderson IIIB open tibial shaft fracture with extensive soft-tissue defect requiring limb salvage with artificial deformity-creating technique. Am J Case Rep. 2022;23:e934788. doi: 10.12659/AJCR.934788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sen C, Kocaoglu M, Eralp L, et al. Bifocal compression-distraction in the acute treatment of grade III open tibia fractures with bone and soft-tissue loss: A report of 24 cases. J Orthop Trauma. 2004;18(3):150–157. doi: 10.1097/00005131-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Plotnikovs K, Movcans J, Solomin L. Acute shortening for open tibial fractures with bone and soft tissue defects: Systematic review of literature. Strategies Trauma Limb Reconstr. 2022;17(1):44–54. doi: 10.5005/jp-journals-10080-1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu YQ, Fan XY, He XQ, et al. Reconstruction of massive tibial bone and soft tissue defects by trifocal bone transport combined with soft tissue distraction experience from 31 cases. BMC Musculoskelet Disord. 2021;22(1):34. doi: 10.1186/s12891-020-03894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yushan M, Ren P, Abula A, et al. Bifocal or trifocal (double-level) bone transport using unilateral rail system in the treatment of large tibial defects caused by infection A retrospective study. Orthop Surg. 2020;12(1):184–193. doi: 10.1111/os.12604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poletti FL, Macmull S, Mushtaq N, et al. Current concepts and principles in open tibial fractures–part II management. MOJ Orthop Rheumatol. 2017;8(2):00305. doi: 10.15406/mojor.2017.08.00305. [DOI] [Google Scholar]
- 11.Catagni MA, Azzam W, Guerreschi F, et al. Trifocal versus bifocal bone transport in treatment of long segmental tibial bone defects. Bone Joint J. 2019;101-B(2):162–169. doi: 10.1302/0301-620X.101B2.BJJ-2018-0340.R2. [DOI] [PubMed] [Google Scholar]
- 12.Chan J, Harry L, Williams G, et al. Soft tissue reconstruction of open fractures of the lower limb muscle versus fasciocutaneous flaps. Plast Reconstr Surg. 2012;130(2):284e–295e. doi: 10.1097/PRS.0b013e3182589e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gopal S, Majumder S, Batchelor AG, et al. Fix and flap The radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82(7):959–966. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 14.Mullen JE, Rozbruch SR, Blyakher A, et al. Ilizarov method for wound closure and bony union of an open grade IIIB tibia fracture. Case Rep Clin Pr Rev. 2004;5(1):1–6. http://www.crcpr-online.com/pub/vol_5/no_1/3389.pdf Available from: [Google Scholar]
- 15.Salih S, Mills E, McGregor-Riley J, et al. Transverse debridement and acute shortening followed by distraction histogenesis in the treatment of open tibial fractures with bone and soft tissue loss. Strategies Trauma Limb Reconstr. 2018;13(3):129–135. doi: 10.1007/s11751-018-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Solomin LN. 2nd edition. Springer, Springer-Verlag; 2012. The basic principles of external skeletal fixation using the Ilizarov and other devices, pp. 705–708. [DOI] [Google Scholar]
- 17.Manner HM, Huebl M, Radler C, et al. Accuracy of complex lower- limb deformity correction with external fixation: A comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J Child Orthop. 2007;1(1):55–61. doi: 10.1007/s11832-006-0005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eren I, Eralp L, Kocaoglu M. Comparative clinical study on deformity correction accuracy of different external fixators. Int Orthop. 2013;37(11):2247–2252. doi: 10.1007/s00264-013-2116-x. [DOI] [PMC free article] [PubMed] [Google Scholar]