Abstract
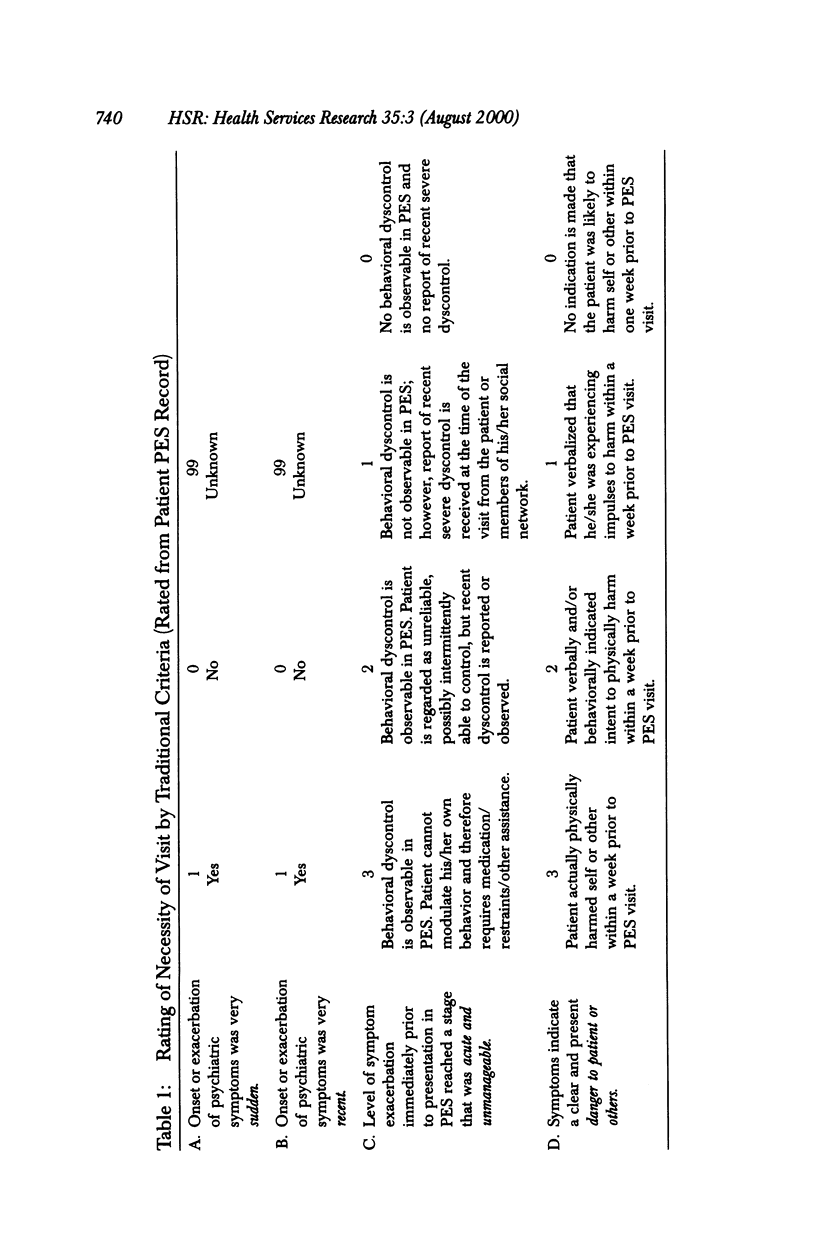
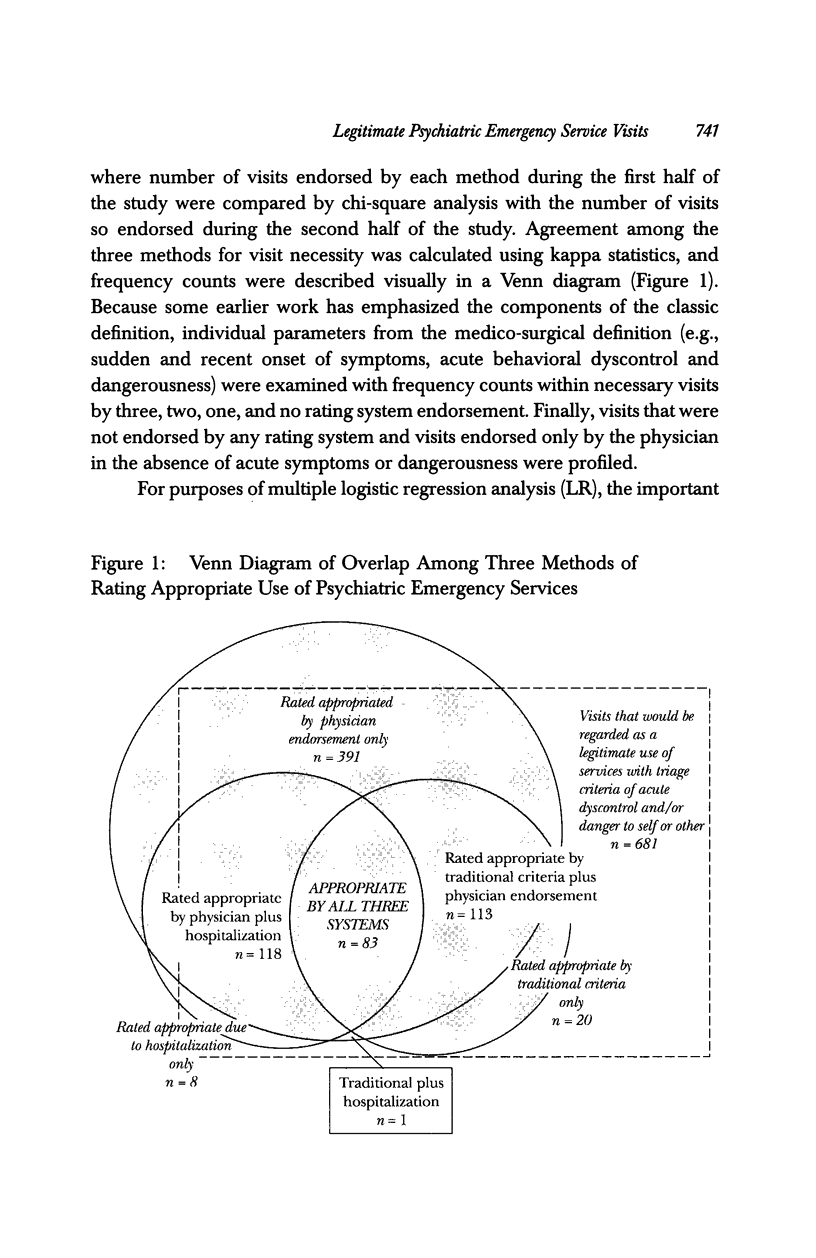
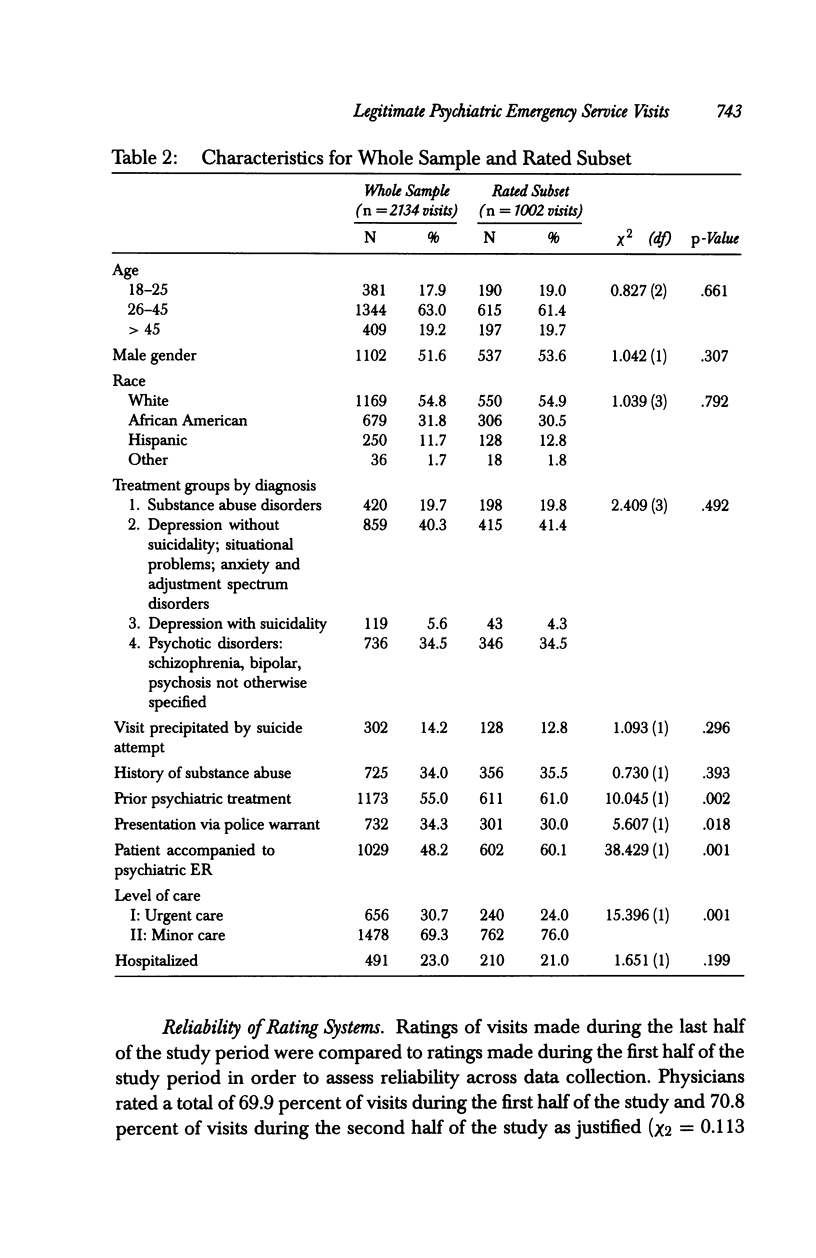
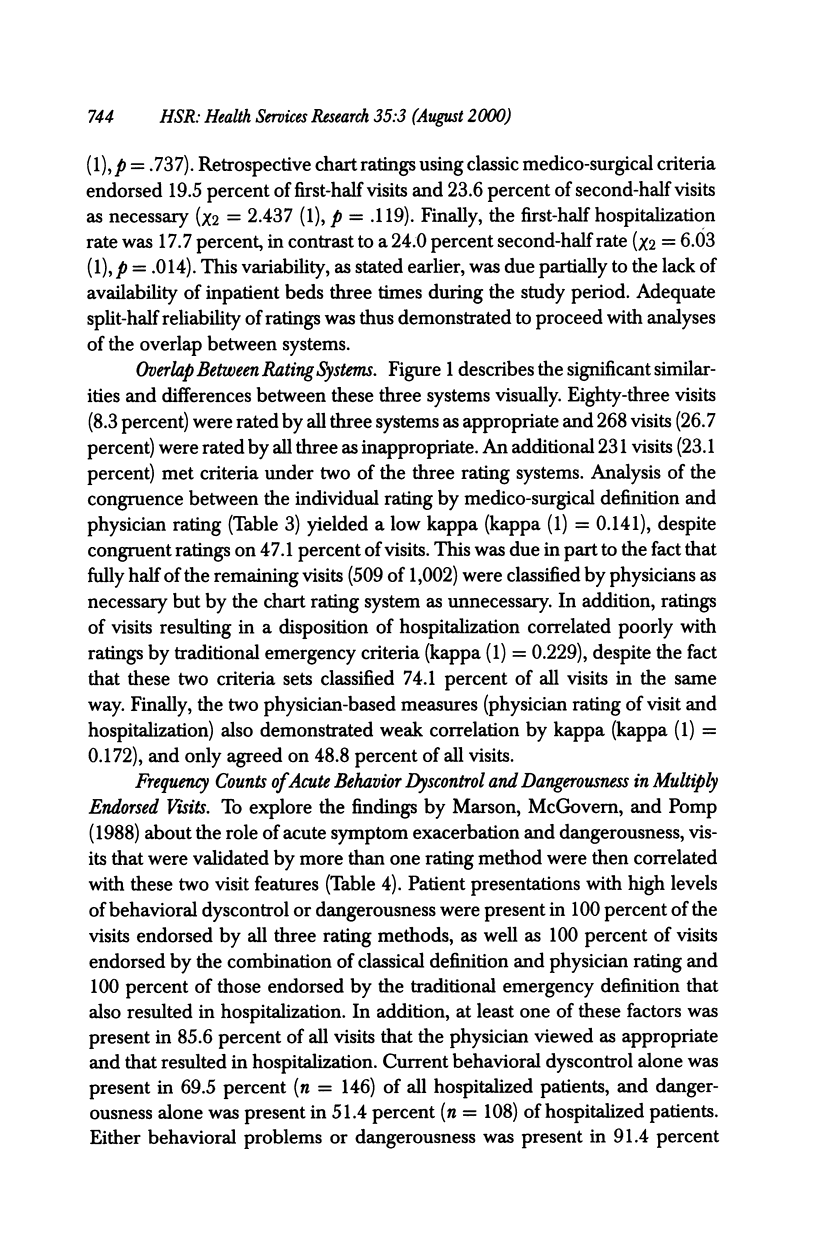
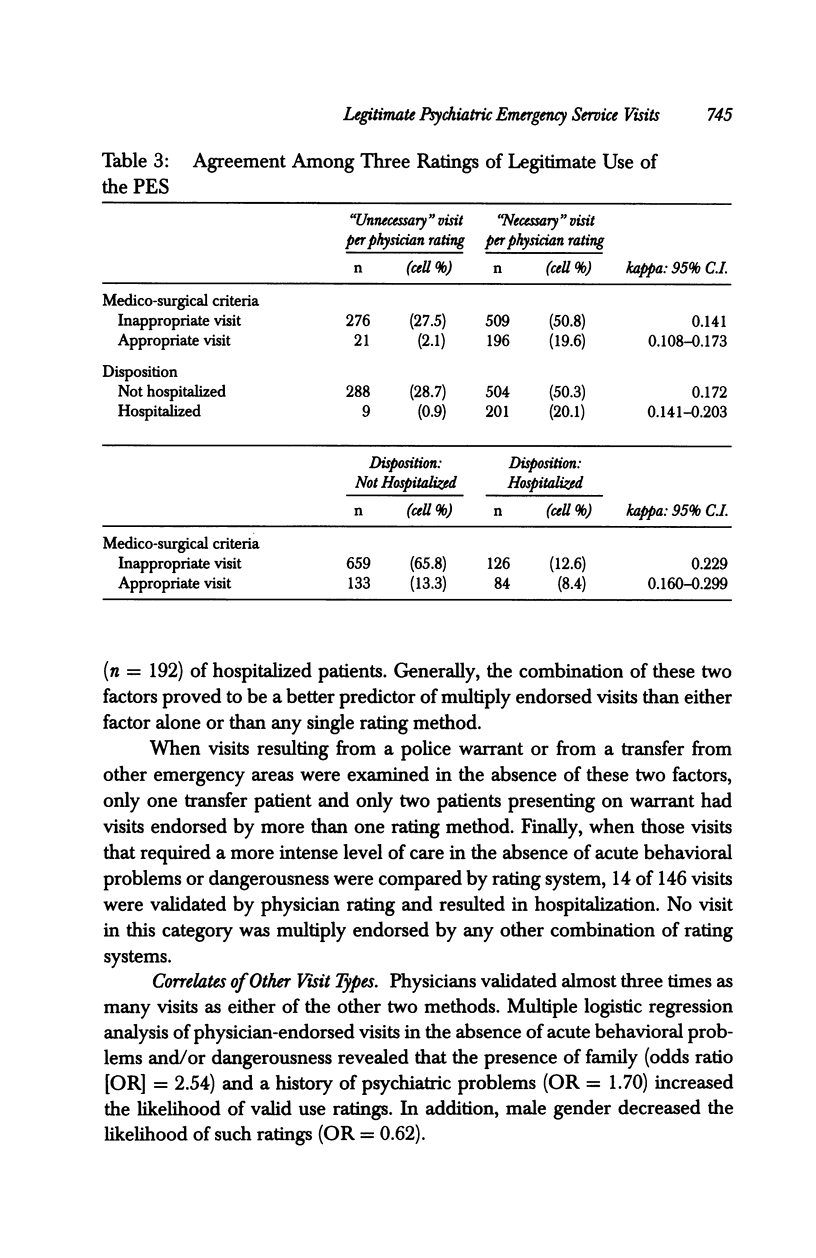
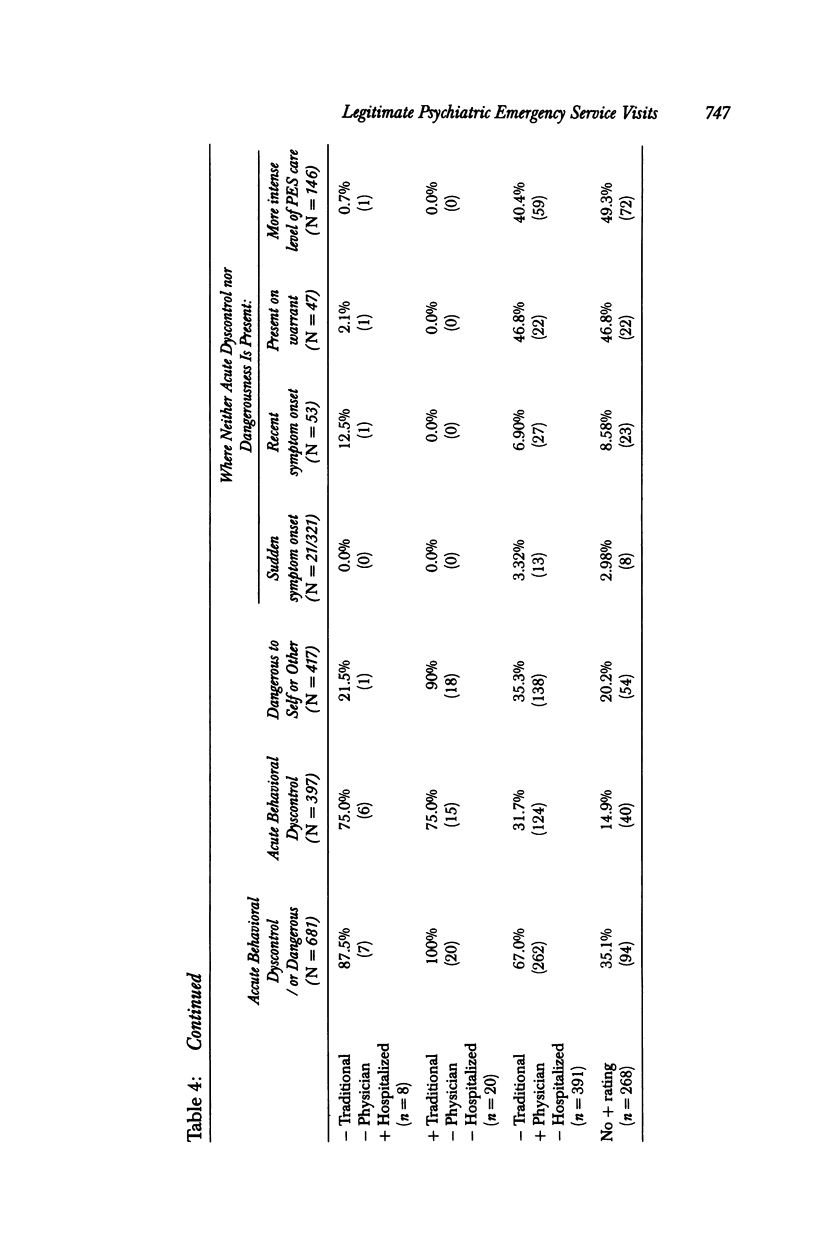
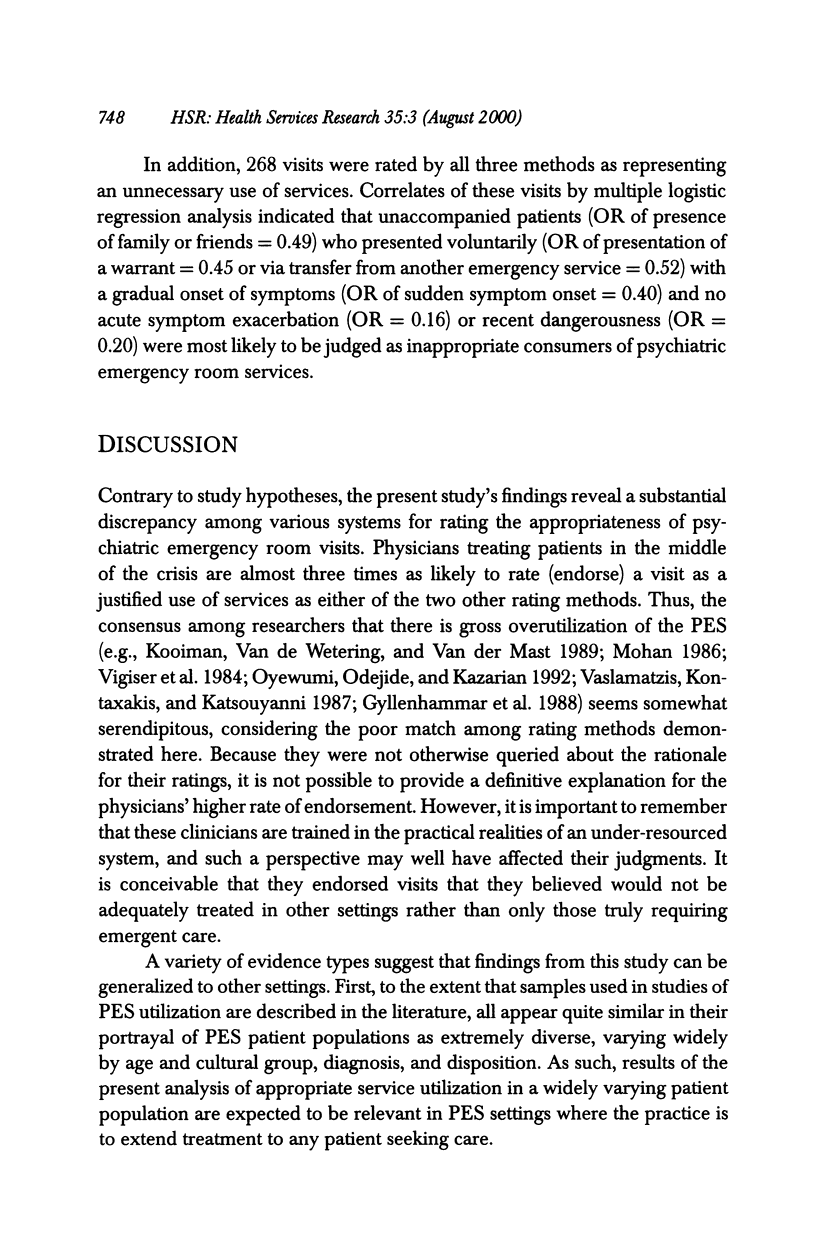
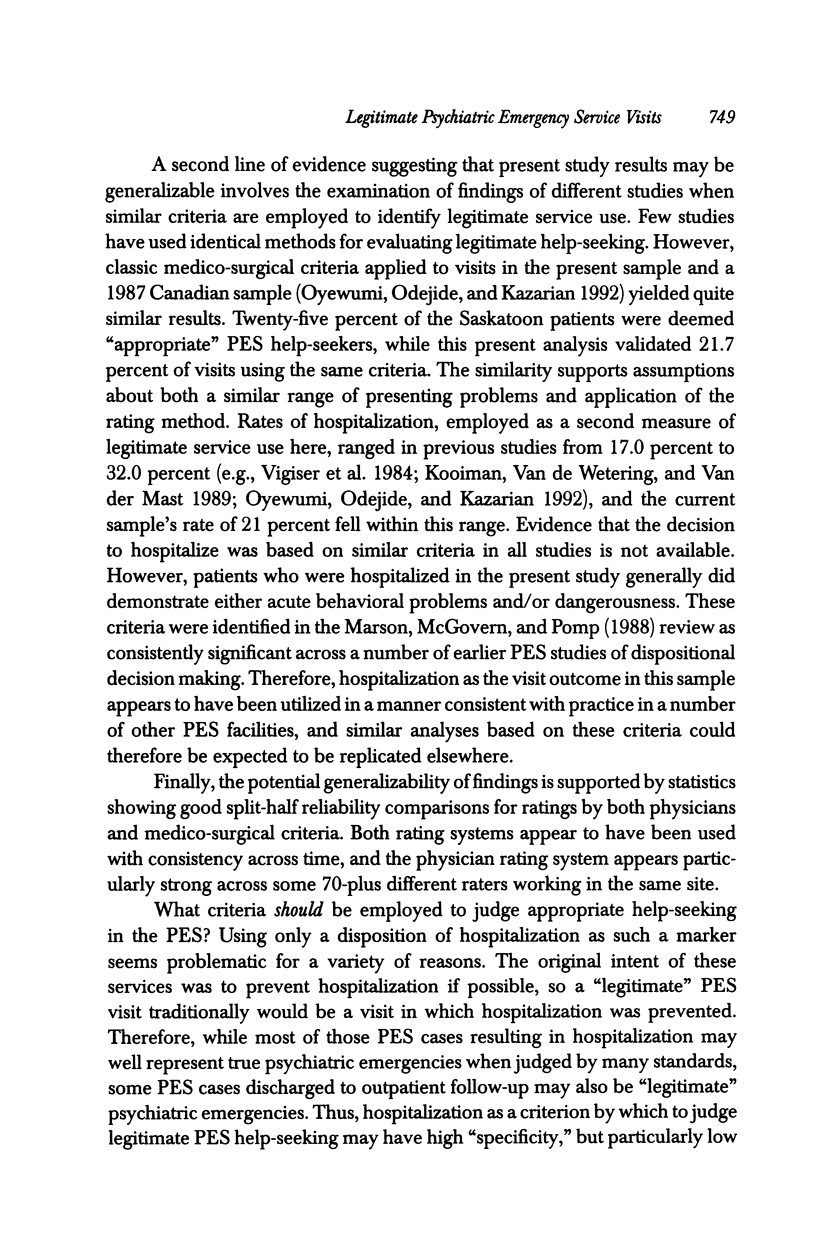
OBJECTIVE: To compare three methods for rating legitimate use of psychiatric emergency services (PES) in order to develop criteria that can differentiate appropriate from inappropriate PES service requests. METHOD: Ratings of PES visits by treating physicians and ratings of the same visits made during review of medical records. STUDY DESIGN: Two previously used methods of identifying justified PES service use were compared with the treating physician's rating of the same: (1) hospitalization as visit outcome and (2) retrospective chart ratings of visit characteristics using traditional medico-surgical criteria for "emergent" illness episodes. DATA EXTRACTION METHODS: Data were extracted through use of a physician questionnaire, and medical and administrative record review. PRINCIPAL FINDINGS: Agreement between the methods ranged from 47.1 percent to 74.1 percent. A total of 21.7 percent of visits were rated as true health "emergencies" by the traditional definition, while 70.4 percent of visits were rated as "necessary" by treating physicians, and 21.0 percent resulted in hospitalization. Acuteness of behavioral dyscontrol and imminent dangerousness at the time of the visit were common characteristics of appropriate use by most combinations of the three methods of rating visits. CONCLUSIONS: The rating systems employed in similar recent studies produce widely varying percentages of visits so classified. However, it does appear likely that a minimum of 25-30 percent of visits are nonemergent and could be triaged to other, less costly treatment providers. Proposed criteria by which to identify "legitimate" psychiatric emergency room treatment requests includes only patient presentations with (a) acute behavioral dyscontrol or (b) imminent dangerousness to self or others.
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adityanjee, Mohan D., Wig N. N. Determinants of emergency room visits for psychological problems in a general hospital. Int J Soc Psychiatry. 1988 Spring;34(1):25–30. doi: 10.1177/002076408803400104. [DOI] [PubMed] [Google Scholar]
- Bachrach L. L. The effects of deinstitutionalization on general hospital psychiatry. Hosp Community Psychiatry. 1981 Nov;32(11):786–790. doi: 10.1176/ps.32.11.786. [DOI] [PubMed] [Google Scholar]
- Bartolucci G., Drayer C. S. An overview of crisis intervention in the emergency rooms of general hospitals. Am J Psychiatry. 1973 Sep;130(9):953–960. doi: 10.1176/ajp.130.9.953. [DOI] [PubMed] [Google Scholar]
- Bassuk E. L., Gerson S. Into the breach: emergency psychiatry in the general hospital. Gen Hosp Psychiatry. 1979 Apr;1(1):31–45. doi: 10.1016/0163-8343(79)90076-8. [DOI] [PubMed] [Google Scholar]
- Gerson S., Bassuk E. Psychiatric emergencies: an overview. Am J Psychiatry. 1980 Jan;137(1):1–11. doi: 10.1176/ajp.137.1.1. [DOI] [PubMed] [Google Scholar]
- Gyllenhammar C., Lundin T., Otto U., Wistedt B. The panorama of psychiatric emergencies in three different parts of Sweden. Eur Arch Psychiatry Neurol Sci. 1988;237(2):61–64. doi: 10.1007/BF00382368. [DOI] [PubMed] [Google Scholar]
- Hughes D. H. Trends and treatment models in emergency psychiatry. Hosp Community Psychiatry. 1993 Oct;44(10):927–928. doi: 10.1176/ps.44.10.927. [DOI] [PubMed] [Google Scholar]
- Kooiman C. G., Van de Wetering B. J., Van der Mast R. C. Clinical and demographic characteristics of emergency department patients in The Netherlands: a review of the literature and a preliminary study. Am J Emerg Med. 1989 Nov;7(6):632–638. doi: 10.1016/0735-6757(89)90288-x. [DOI] [PubMed] [Google Scholar]
- Lieberman P. B., Baker F. M. The reliability of psychiatric diagnosis in the emergency room. Hosp Community Psychiatry. 1985 Mar;36(3):291–293. doi: 10.1176/ps.36.3.291. [DOI] [PubMed] [Google Scholar]
- MacKenzie D. M., Mackie J. Psychiatric emergency clinic attenders: what can we learn from them? Health Bull (Edinb) 1993 Mar;51(2):67–71. [PubMed] [Google Scholar]
- Marson D. C., McGovern M. P., Pomp H. C. Psychiatric decision making in the emergency room: a research overview. Am J Psychiatry. 1988 Aug;145(8):918–925. doi: 10.1176/ajp.145.8.918. [DOI] [PubMed] [Google Scholar]
- Murdach A. D. Decision making in psychiatric emergencies. Health Soc Work. 1987 Fall;12(4):267–274. doi: 10.1093/hsw/12.4.267. [DOI] [PubMed] [Google Scholar]
- Oyewumi L. K., Odejide O., Kazarian S. S. Psychiatric emergency services in a Canadian city: I. Prevalence and patterns of use. Can J Psychiatry. 1992 Mar;37(2):91–95. doi: 10.1177/070674379203700203. [DOI] [PubMed] [Google Scholar]
- Padgett D. K., Brodsky B. Psychosocial factors influencing non-urgent use of the emergency room: a review of the literature and recommendations for research and improved service delivery. Soc Sci Med. 1992 Nov;35(9):1189–1197. doi: 10.1016/0277-9536(92)90231-e. [DOI] [PubMed] [Google Scholar]
- Ries R. Advantages of separating the triage function from the psychiatric emergency service. Psychiatr Serv. 1997 Jun;48(6):755–756. doi: 10.1176/ps.48.6.755. [DOI] [PubMed] [Google Scholar]
- Rissmiller D. J., Steer R., Ranieri W. F., Rissmiller F., Hogate P. Factors complicating cost containment in the treatment of suicidal patients. Hosp Community Psychiatry. 1994 Aug;45(8):782–788. doi: 10.1176/ps.45.8.782. [DOI] [PubMed] [Google Scholar]
- Sales G. N. A comparison of referrals by police and other sources to a psychiatric emergency service. Hosp Community Psychiatry. 1991 Sep;42(9):950–952. doi: 10.1176/ps.42.9.950. [DOI] [PubMed] [Google Scholar]
- Segal S. P., Egley L., Watson M. A., Goldfinger S. M. The quality of psychiatric emergency evaluations and patient outcomes in county hospitals. Am J Public Health. 1995 Oct;85(10):1429–1431. doi: 10.2105/ajph.85.10.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon P., Beck S. Patients' perceived service needs when seen in a psychiatric emergency room. Psychiatr Q. 1989 Fall;60(3):215–226. doi: 10.1007/BF01064797. [DOI] [PubMed] [Google Scholar]
- Solomon P., Gordon B. The psychiatric emergency room and follow-up services in the community. Psychiatr Q. 1986;58(2):119–127. doi: 10.1007/BF01064053. [DOI] [PubMed] [Google Scholar]
- Vaslamatzis G., Kontaxakis V., Markidis M., Katsouyanni K. Social and resource factors related to the utilization of emergency psychiatric services in the Athens area. Acta Psychiatr Scand. 1987 Jan;75(1):95–98. doi: 10.1111/j.1600-0447.1987.tb02758.x. [DOI] [PubMed] [Google Scholar]
- Vigiser D., Apter A., Aviram U., Maoz B. Overutilization of the general hospital emergency room for psychiatric referrals in an Israeli hospital. Am J Public Health. 1984 Jan;74(1):73–75. doi: 10.2105/ajph.74.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Way B. B., Evans M. E., Banks S. M. Factors predicting referral to inpatient or outpatient treatment from psychiatric emergency services. Hosp Community Psychiatry. 1992 Jul;43(7):703–708. doi: 10.1176/ps.43.7.703. [DOI] [PubMed] [Google Scholar]
- White-Means S. I., Thornton M. C. Nonemergency visits to hospital emergency rooms: a comparison of blacks and whites. Milbank Q. 1989;67(1):35–57. [PubMed] [Google Scholar]
- Woogh C. M. A cohort through the revolving door. Can J Psychiatry. 1986 Apr;31(3):214–221. doi: 10.1177/070674378603100306. [DOI] [PubMed] [Google Scholar]



