Abstract
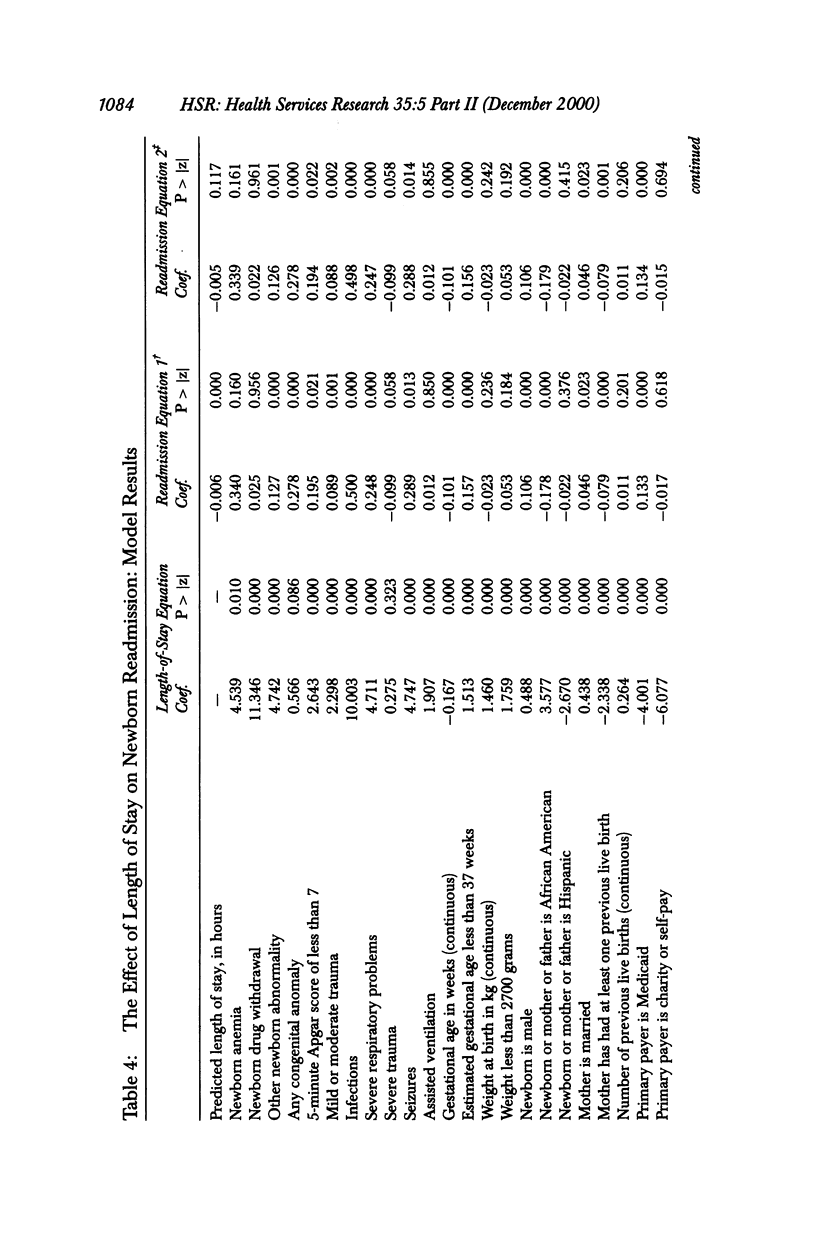
OBJECTIVE: To determine the effect of postpartum length of stay on newborn readmission. DATA SOURCES: Secondary data set consisting of newborns born in Washington state in 1989 and 1990. The data set contains information about the characteristics of the newborn and its parents, physician, hospital, and insurance status. STUDY DESIGN: Analysis of the effect of length of stay on the probability of newborn readmission using hour of birth and method of delivery as instrumental variables (IVs) to account for unobserved heterogeneity. Of approximately 150,000 newborns born in Washington in 1989 and 1990, 108,551 (72 percent) were included in our analysis. PRINCIPAL FINDINGS: Newborns with different lengths of stay differ in unmeasured characteristics, biasing estimates based on standard statistical methods. The results of our analyses show that a 12-hour increase in length of stay is associated with a reduction in the newborn readmission rate of 0.6 percentage points. This is twice as large as the estimate obtained using standard statistical (non-IV) methods. CONCLUSION: An increase in the length of postpartum hospital stays may result in a decline in newborn readmissions. The magnitude of this decline in readmissions may be larger than previously thought.
Full text
PDF













Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bollen K. A., Guilkey D. K., Mroz T. A. Binary outcomes and endogenous explanatory variables: tests and solutions with an application to the demand for contraceptive use in Tunisia. Demography. 1995 Feb;32(1):111–131. [PubMed] [Google Scholar]
- Braveman P., Egerter S., Pearl M., Marchi K., Miller C. Problems associated with early discharge of newborn infants. Early discharge of newborns and mothers: a critical review of the literature. Pediatrics. 1995 Oct;96(4 Pt 1):716–726. [PubMed] [Google Scholar]
- Catz C., Hanson J. W., Simpson L., Yaffe S. J. Summary of workshop: early discharge and neonatal hyperbilirubinemia. Pediatrics. 1995 Oct;96(4 Pt 1):743–745. [PubMed] [Google Scholar]
- Edmonson M. B., Stoddard J. J., Owens L. M. Hospital readmission with feeding-related problems after early postpartum discharge of normal newborns. JAMA. 1997 Jul 23;278(4):299–303. [PubMed] [Google Scholar]
- Fox M. H., Kanarek N. The effects of newborn early discharge on hospital readmissions. Am J Med Qual. 1995 Winter;10(4):206–212. doi: 10.1177/0885713X9501000407. [DOI] [PubMed] [Google Scholar]
- Gazmararian J. A., Koplan J. P., Cogswell M. E., Bailey C. M., Davis N. A., Cutler C. M. Maternity experiences in a managed care organization. Health Aff (Millwood) 1997 May-Jun;16(3):198–208. doi: 10.1377/hlthaff.16.3.198. [DOI] [PubMed] [Google Scholar]
- Gazmararian J. A., Koplan J. P. Length-of-stay after delivery: managed care versus fee-for-service. Health Aff (Millwood) 1996 Winter;15(4):74–80. doi: 10.1377/hlthaff.15.4.74. [DOI] [PubMed] [Google Scholar]
- Gifford D. S., Morton S. C., Fiske M., Keesey J., Keeler E., Kahn K. L. Lack of progress in labor as a reason for cesarean. Obstet Gynecol. 2000 Apr;95(4):589–595. doi: 10.1016/s0029-7844(99)00575-x. [DOI] [PubMed] [Google Scholar]
- Grullon K. E., Grimes D. A. The safety of early postpartum discharge: a review and critique. Obstet Gynecol. 1997 Nov;90(5):860–865. doi: 10.1016/S0029-7844(97)00405-5. [DOI] [PubMed] [Google Scholar]
- Hillman A. L., Pauly M. V., Kerstein J. J. How do financial incentives affect physicians' clinical decisions and the financial performance of health maintenance organizations? N Engl J Med. 1989 Jul 13;321(2):86–92. doi: 10.1056/NEJM198907133210205. [DOI] [PubMed] [Google Scholar]
- James M. L., Hudson C. N., Gebski V. J., Browne L. H., Andrews G. R., Crisp S. E., Palmer D., Beresford J. L. An evaluation of planned early postnatal transfer home with nursing support. Med J Aust. 1987 Nov 2;147(9):434-5, 437-8. [PubMed] [Google Scholar]
- Kanaaneh H. The relationship of bottle feeding to malnutrition and gastroenteritis in a pre-industrial setting. J Trop Pediatr Environ Child Health. 1972 Dec;18(4):302–306. doi: 10.1093/tropej/18.4.302. [DOI] [PubMed] [Google Scholar]
- Keeler E. B., Park R. E., Bell R. M., Gifford D. S., Keesey J. Adjusting cesarean delivery rates for case mix. Health Serv Res. 1997 Oct;32(4):511–528. [PMC free article] [PubMed] [Google Scholar]
- Lemmer C. M. Early discharge: outcomes of primiparas and their infants. J Obstet Gynecol Neonatal Nurs. 1987 Jul-Aug;16(4):230–236. doi: 10.1111/j.1552-6909.1987.tb01578.x. [DOI] [PubMed] [Google Scholar]
- Liu L. L., Clemens C. J., Shay D. K., Davis R. L., Novack A. H. The safety of newborn early discharge. The Washington State experience. JAMA. 1997 Jul 23;278(4):293–298. [PubMed] [Google Scholar]
- Margolis L. H., Kotelchuck M., Chang H. Y. Factors associated with early maternal postpartum discharge from the hospital. Arch Pediatr Adolesc Med. 1997 May;151(5):466–472. doi: 10.1001/archpedi.1997.02170420036006. [DOI] [PubMed] [Google Scholar]
- McClellan M., McNeil B. J., Newhouse J. P. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994 Sep 21;272(11):859–866. [PubMed] [Google Scholar]
- Schneider A. P., 2nd Breast milk jaundice in the newborn. A real entity. JAMA. 1986 Jun 20;255(23):3270–3274. [PubMed] [Google Scholar]


