Abstract
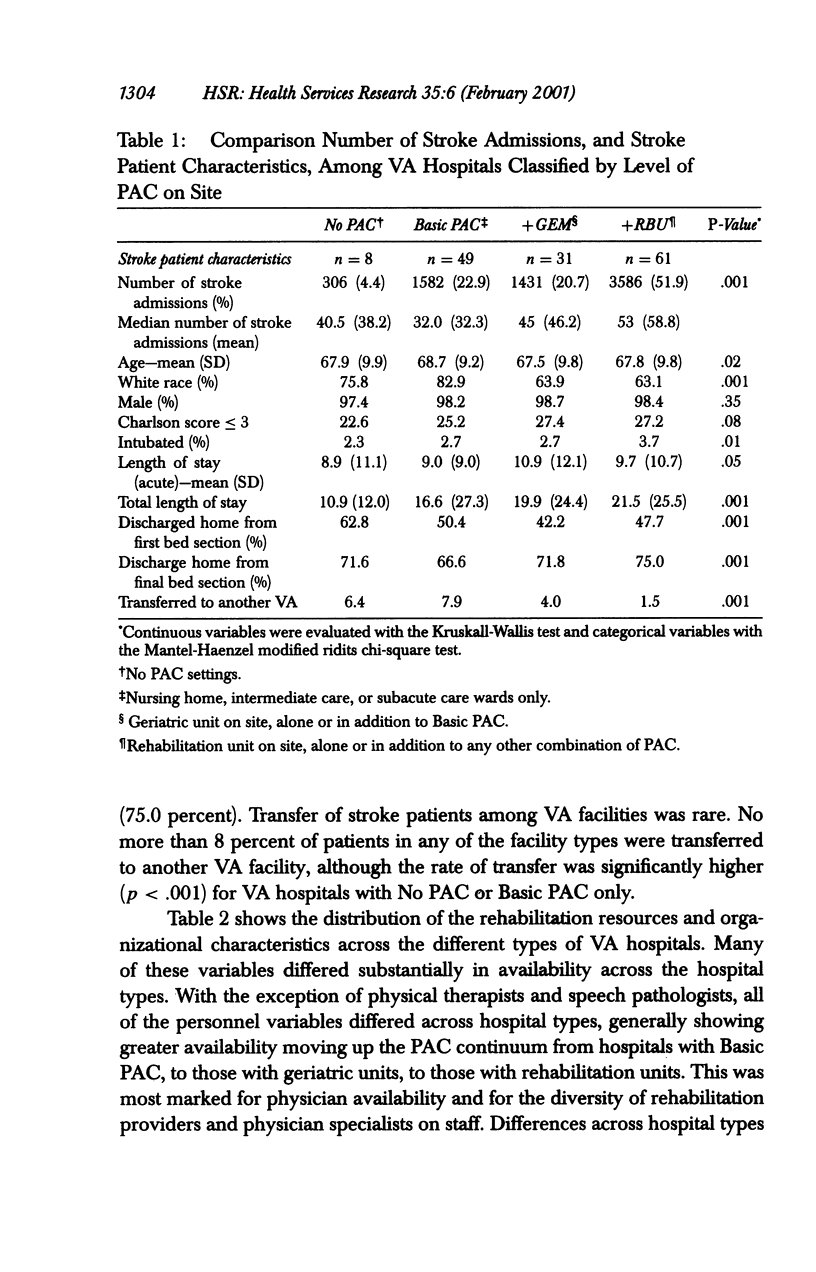
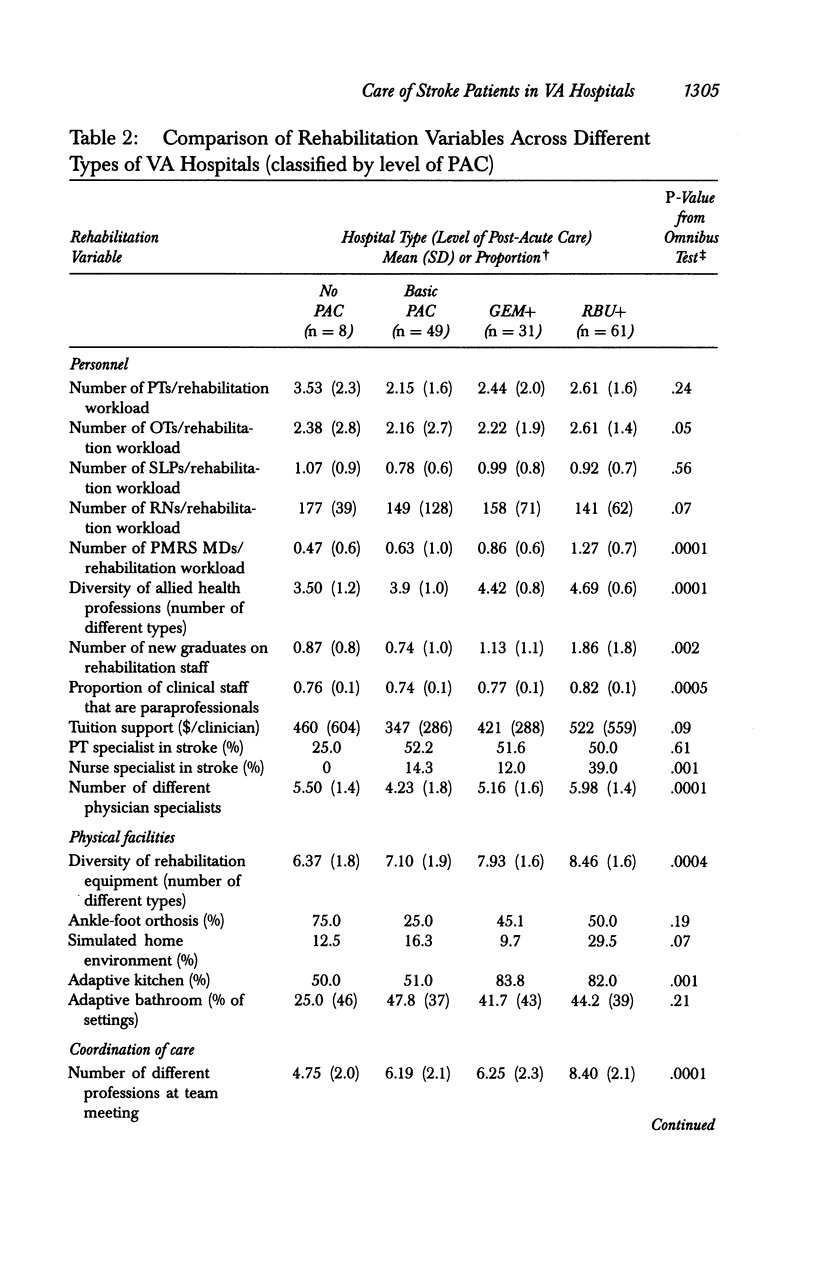
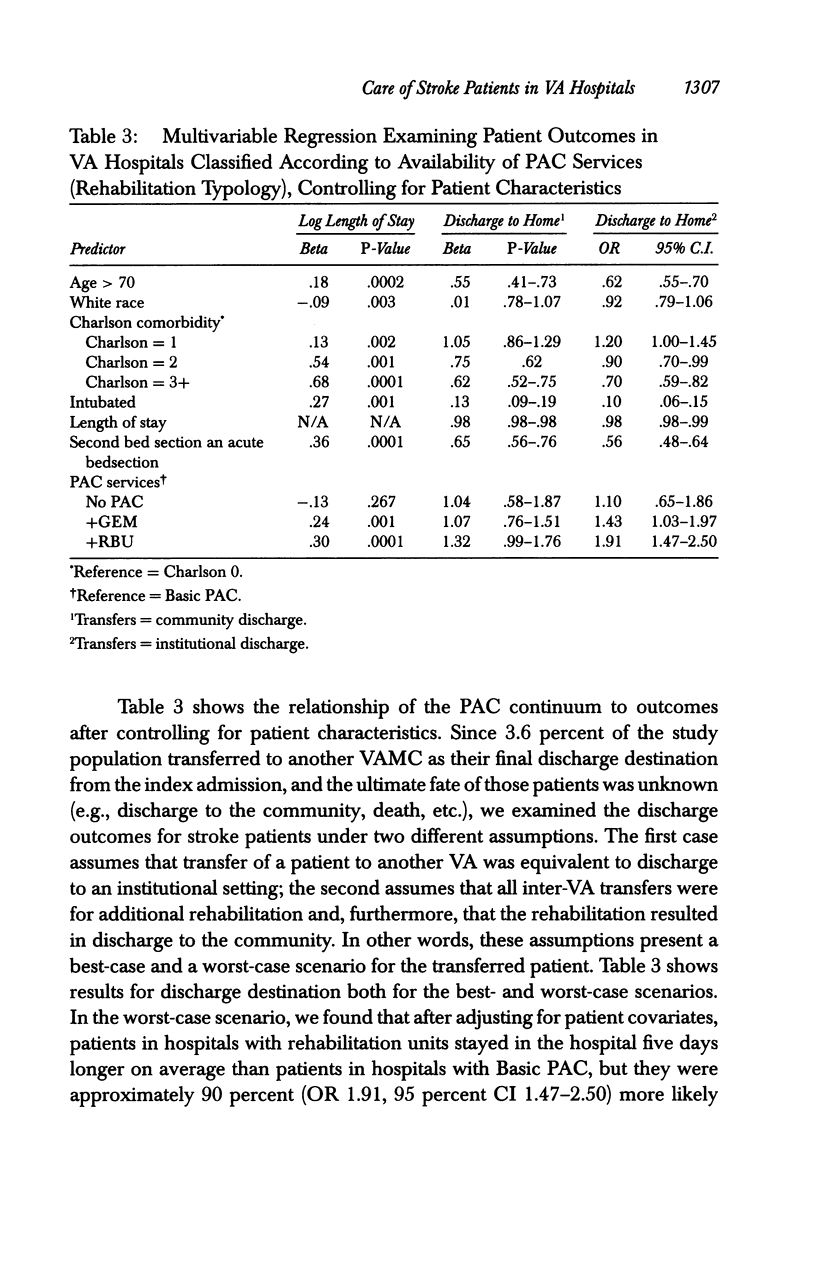
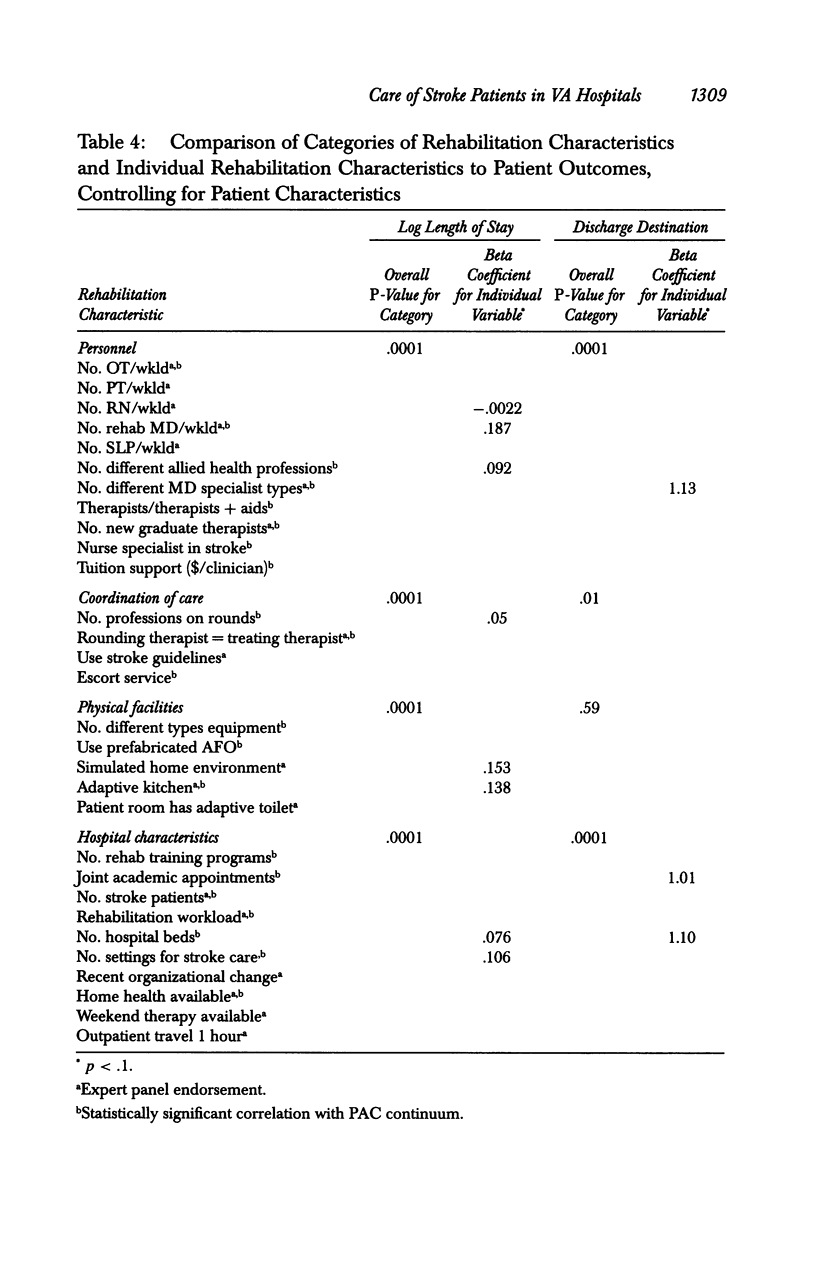
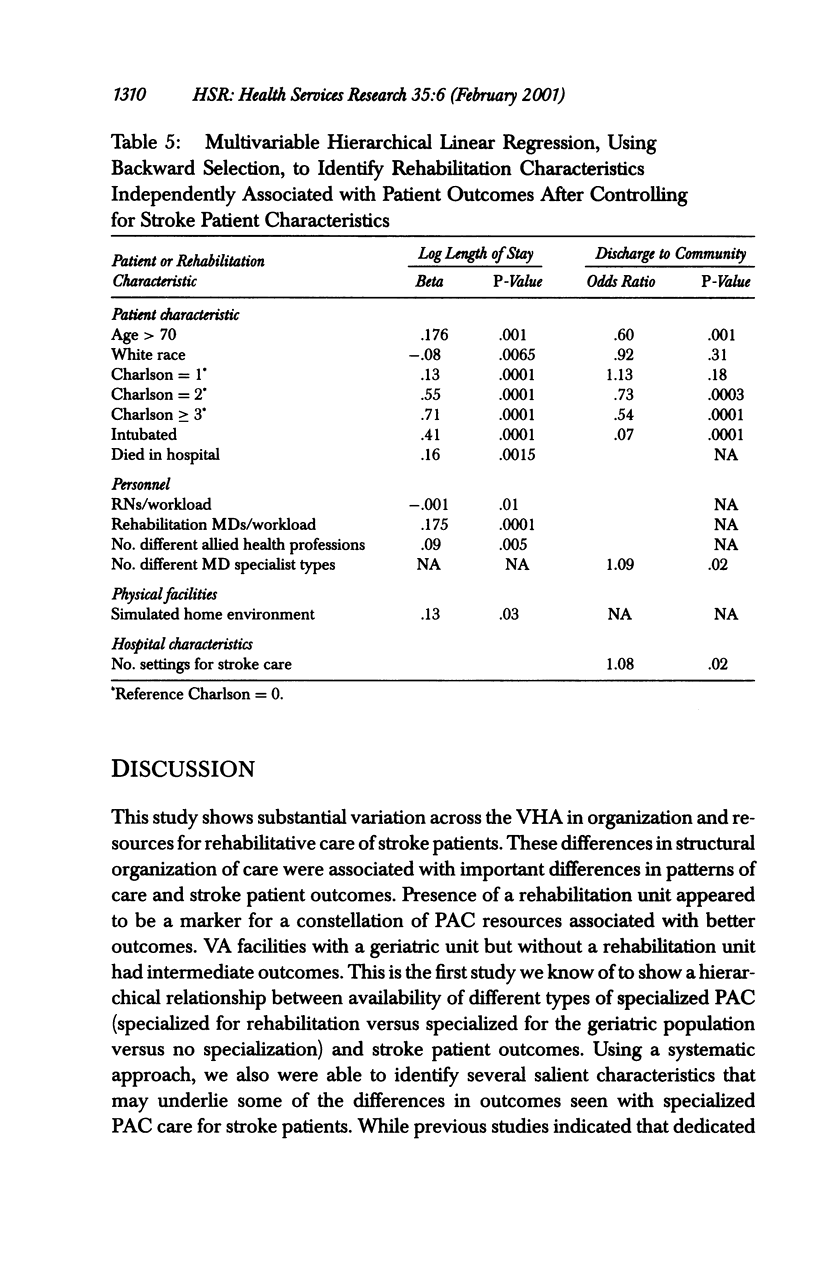
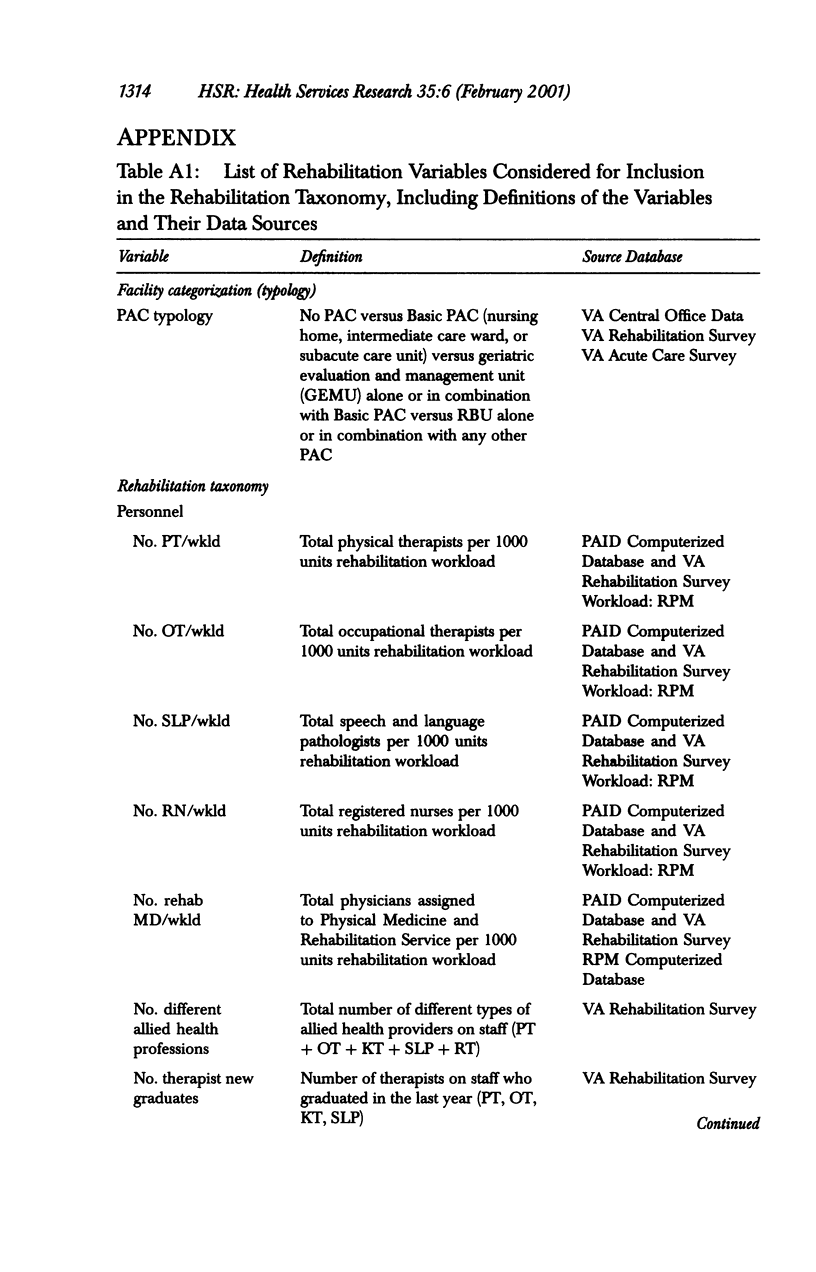
OBJECTIVE: To examine the relationship of services for post-acute care (PAC) to stroke patient outcomes. DATA SOURCES/STUDY SETTING: Veterans Health Administration (VHA) hospitals from two facility-level surveys and extant data files. STUDY DESIGN: Cross-sectional study of veterans hospitalized with acute stroke during the period June 1995 through May 1996 in one of 182 geographically distinct locations within the VHA. Study variables included (1) a typological classification of hospitals according to the level of PAC; (2) a taxonomy of rehabilitation characteristics, including personnel, physical facilities, coordination of care, and hospital characteristics; and (3) patient outcomes (discharge destination, length of stay). DATA COLLECTION/EXTRACTION METHODS: Data were collected from two mailed surveys and extant data files. Rehabilitation variables were identified for the study in conjunction with a panel of expert rehabilitation researchers and clinicians, using an a priori model for measuring rehabilitation characteristics. Two sets of variables were derived to categorize these rehabilitation characteristics: (1) a rehabilitation typology, classifying the VA hospitals according to the continuum of PAC settings in the facility, and (2) a rehabilitation taxonomy that used an empirical approach to derive a list of key rehabilitation characteristics. PRINCIPAL FINDINGS: Twenty-seven percent of veterans with acute stroke were cared for in VA hospitals with neither a geriatric nor a rehabilitation unit, and 50 percent were cared for in hospitals without a rehabilitation unit. Hospitals with rehabilitation units had the greatest sophistication, and those with geriatric units had intermediate sophistication in rehabilitation organization and resources. Statistically significant differences were found in outcomes for stroke patients cared for in hospitals classified according to the continuum of post-acute care on site. Exploratory multivariable analyses revealed independent associations between stroke patient outcomes and (1) staffing ratios for nurses and physicians, (2) the diversity of physician and rehabilitation staff, (3) presence of a simulated home environment, and (4) the total number of care settings on site. CONCLUSIONS: The PAC continuum defines an important hierarchy of stroke rehabilitation services.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
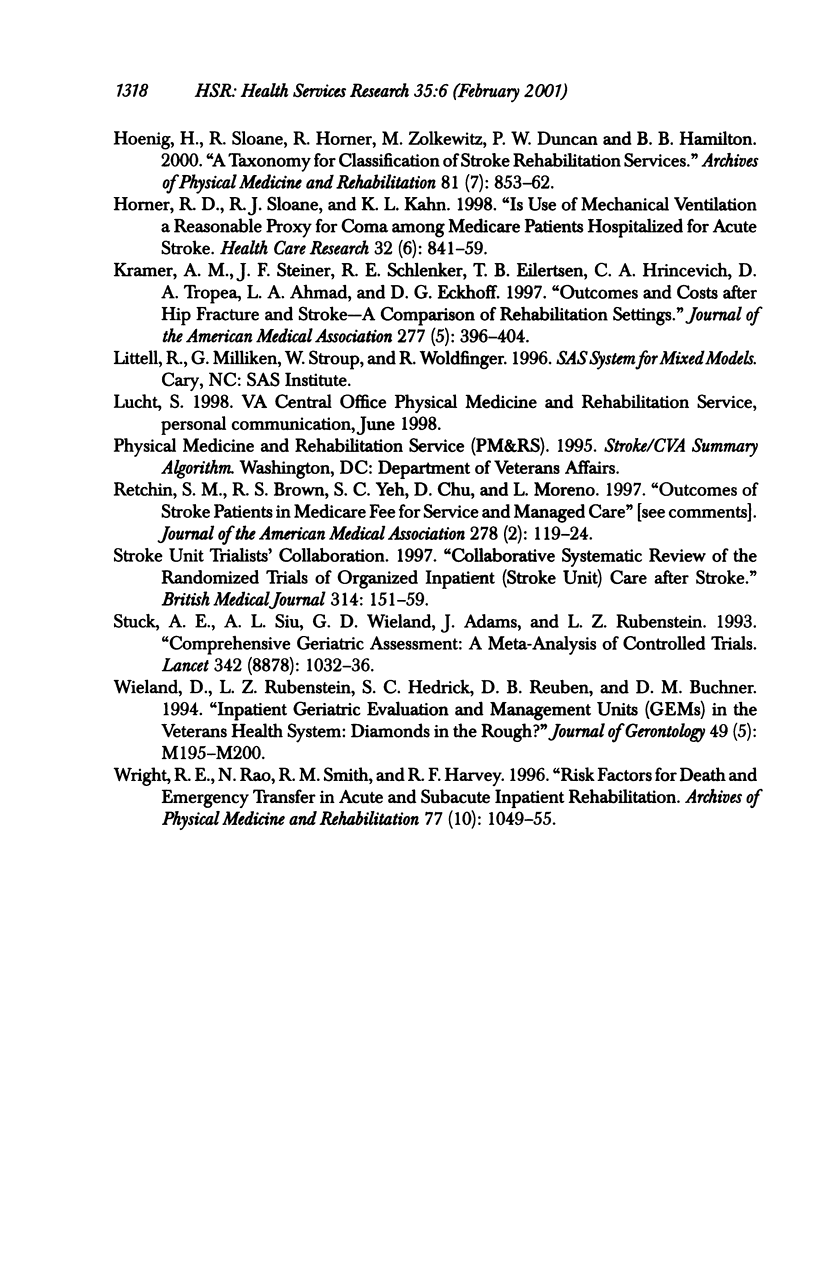
- Deyo R. A., Cherkin D. C., Ciol M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Hoenig H., Sloane R., Horner R. D., Zolkewitz M., Duncan P. W., Hamilton B. B. A taxonomy for classification of stroke rehabilitation services. Arch Phys Med Rehabil. 2000 Jul;81(7):853–862. doi: 10.1053/apmr.2000.5569. [DOI] [PubMed] [Google Scholar]
- Horner R. D., Sloane R. J., Kahn K. L. Is use of mechanical ventilation a reasonable proxy indicator for coma among Medicare patients hospitalized for acute stroke? Health Serv Res. 1998 Feb;32(6):841–859. [PMC free article] [PubMed] [Google Scholar]
- Kramer A. M., Steiner J. F., Schlenker R. E., Eilertsen T. B., Hrincevich C. A., Tropea D. A., Ahmad L. A., Eckhoff D. G. Outcomes and costs after hip fracture and stroke. A comparison of rehabilitation settings. JAMA. 1997 Feb 5;277(5):396–404. [PubMed] [Google Scholar]
- Retchin S. M., Brown R. S., Yeh S. C., Chu D., Moreno L. Outcomes of stroke patients in Medicare fee for service and managed care. JAMA. 1997 Jul 9;278(2):119–124. [PubMed] [Google Scholar]
- Stuck A. E., Siu A. L., Wieland G. D., Adams J., Rubenstein L. Z. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993 Oct 23;342(8878):1032–1036. doi: 10.1016/0140-6736(93)92884-v. [DOI] [PubMed] [Google Scholar]
- Vannah W. M., Drvaric D. M., Hastings J. A., Stand J. A., 3rd, Harning D. M. A method of residual limb stiffness distribution measurement. J Rehabil Res Dev. 1999 Jan;36(1):1–7. [PubMed] [Google Scholar]
- Wieland D., Rubenstein L. Z., Hedrick S. C., Reuben D. B., Buchner D. M. Inpatient geriatric evaluation and management units (GEMs) in the veterans health system: diamonds in the rough? J Gerontol. 1994 Sep;49(5):M195–M200. doi: 10.1093/geronj/49.5.m195. [DOI] [PubMed] [Google Scholar]
- Wright R. E., Rao N., Smith R. M., Harvey R. F. Risk factors for death and emergency transfer in acute and subacute inpatient rehabilitation. Arch Phys Med Rehabil. 1996 Oct;77(10):1049–1055. doi: 10.1016/s0003-9993(96)90067-2. [DOI] [PubMed] [Google Scholar]


