Abstract
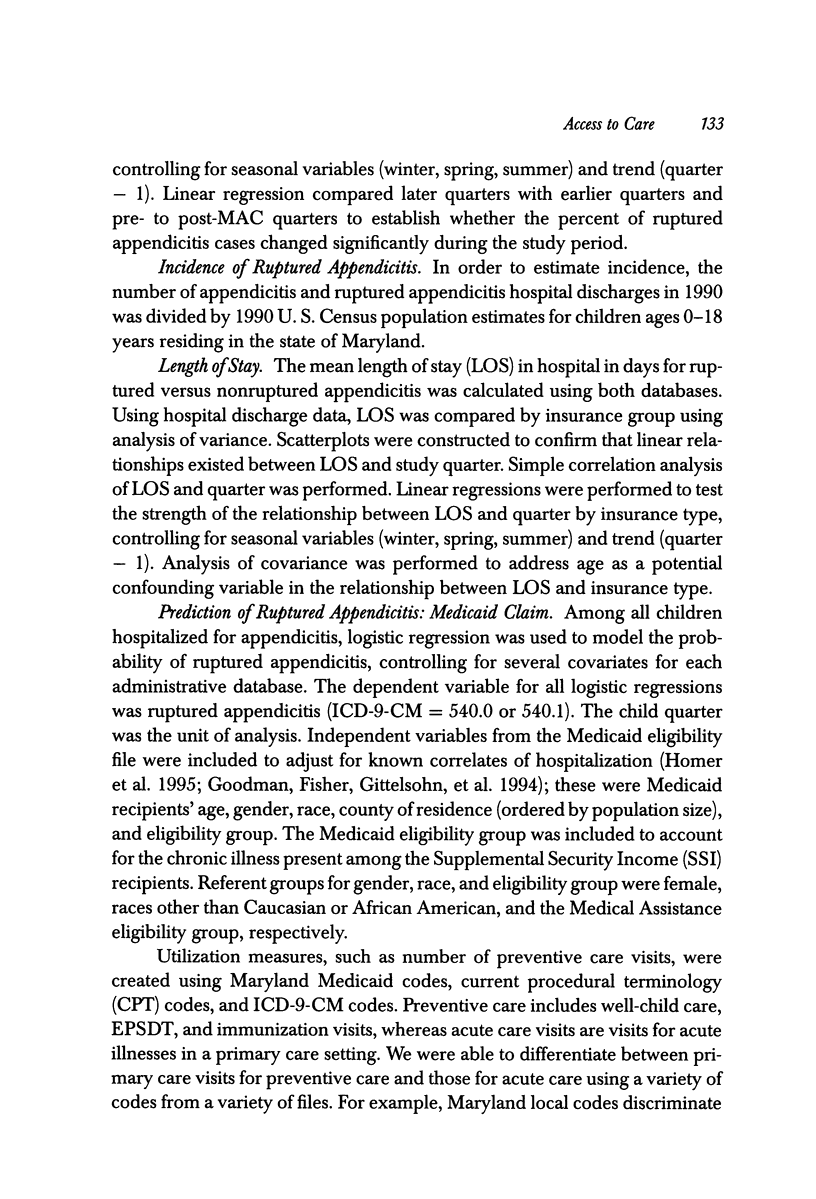
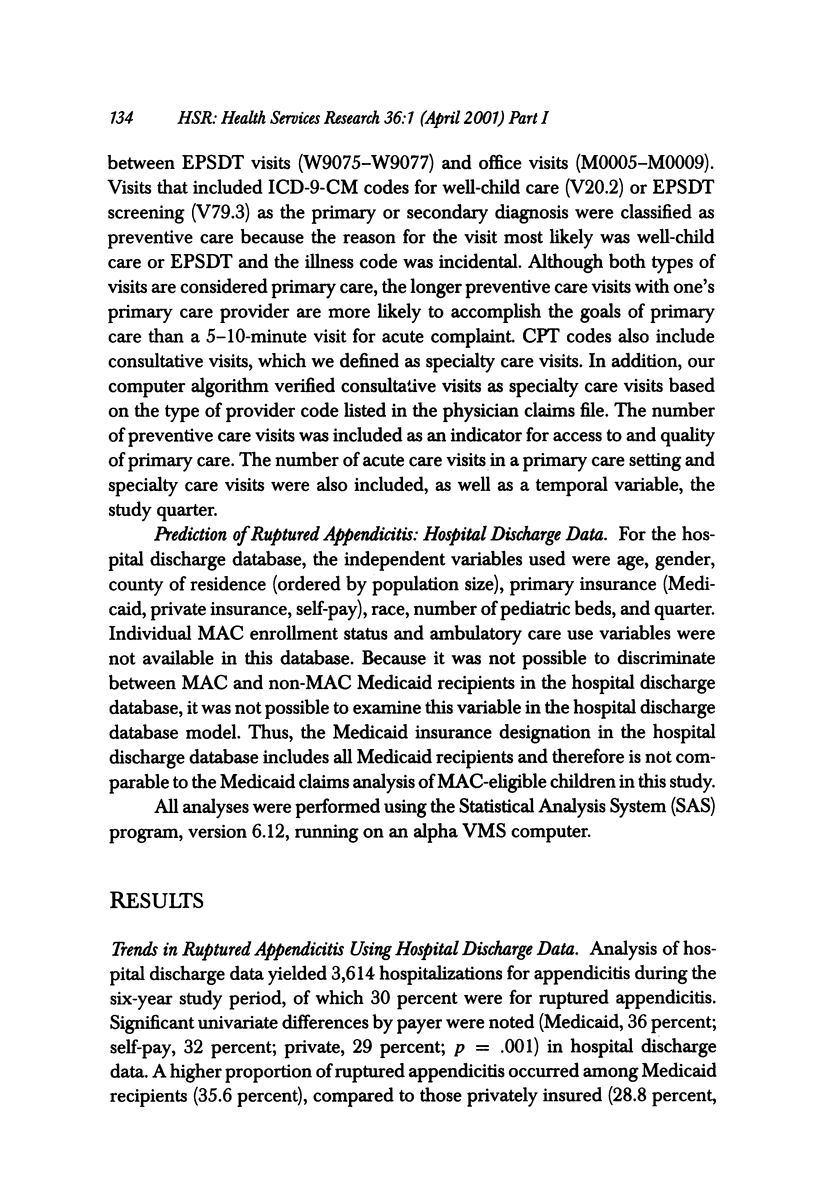
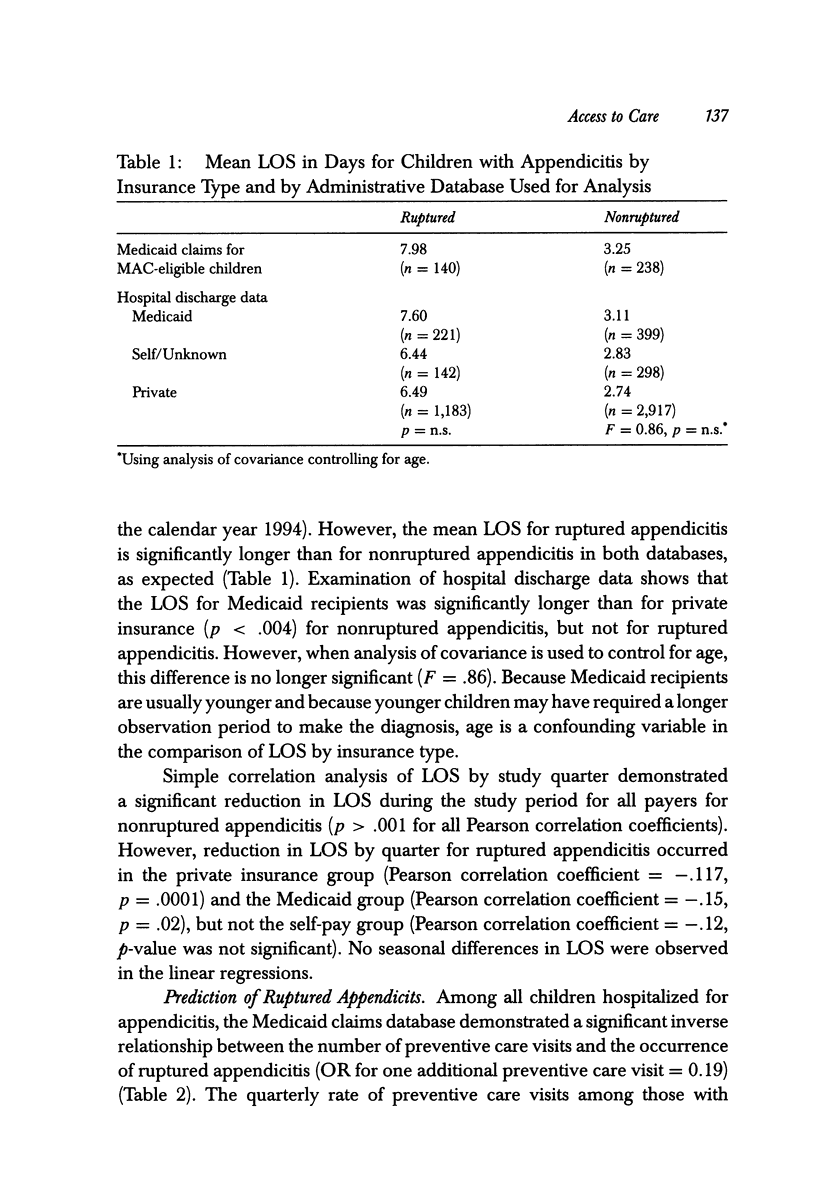
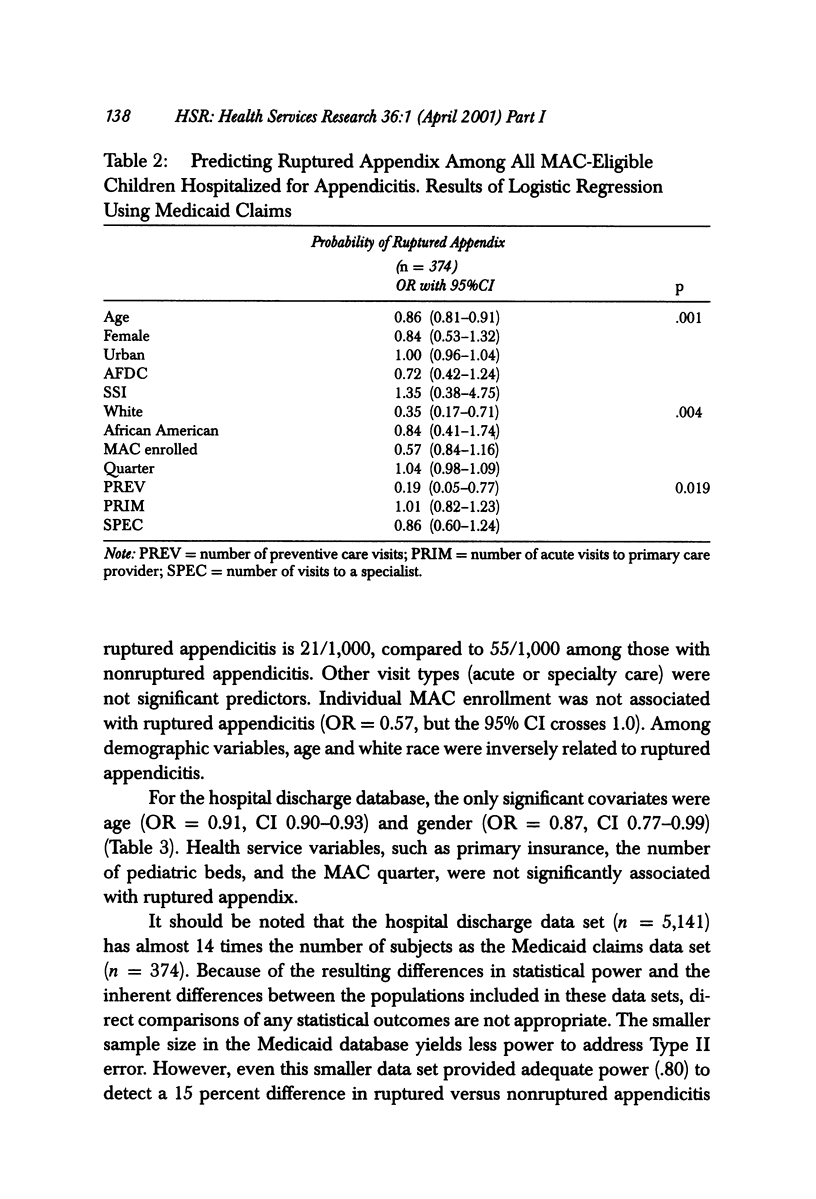
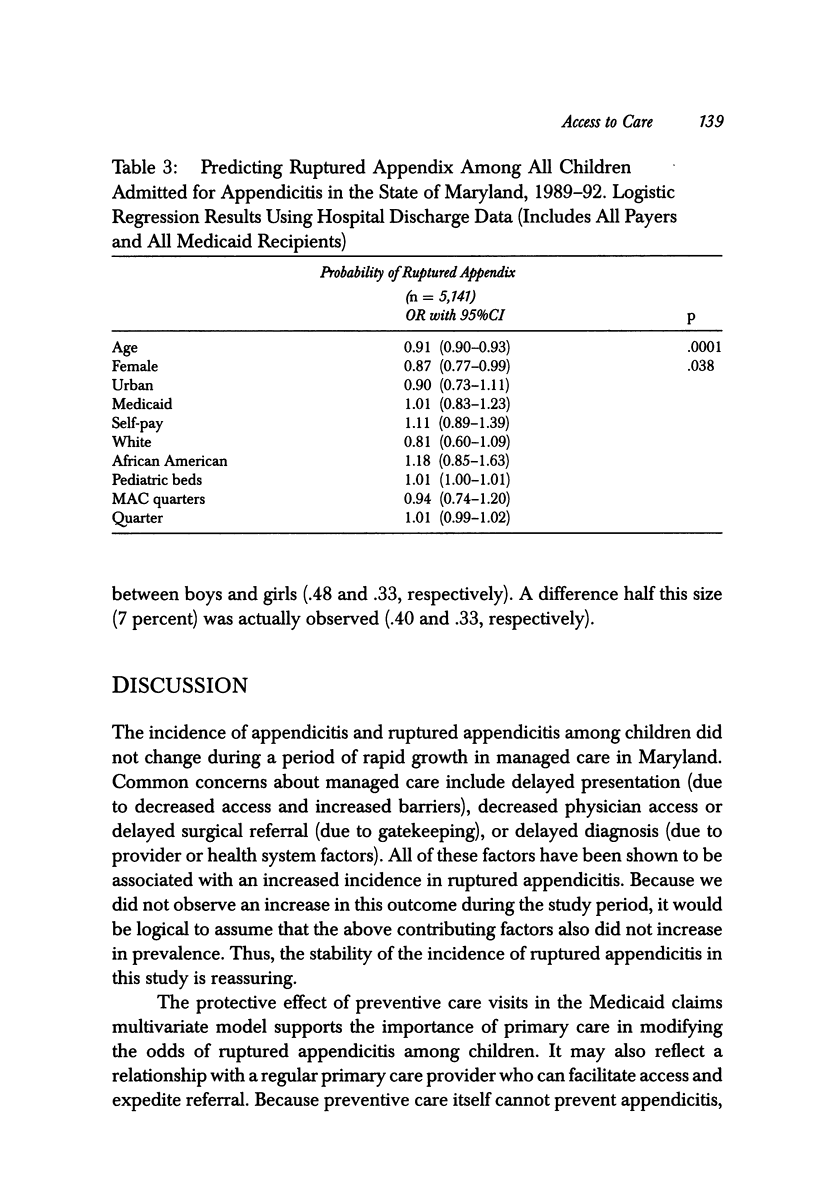
OBJECTIVE: To determine factors associated with ruptured appendicitis among children, using administrative databases. Insurance-related differences in the risk of ruptured appendix among adults in California have previously been described (Braveman, Schaaf, Egerter, et al. 1994). DATA SOURCES/STUDY SETTING: State of Maryland Medicaid claims data for children < or = 18 years of age from 1989 to 1993 and hospital discharge data for children < or = 19 years of age from 1989 to 1994 were analyzed. STUDY DESIGN: Administrative data analysis pre- and post-implementation of a Medicaid managed care program called Maryland Access to Care. DATA COLLECTION/EXTRACTION METHODS: Medicaid claims and hospital discharge ICD-9-CM codes were used to define hospitalization for ruptured and nonruptured appendicitis. Linear regression was used to model trends. Logistic regression was used to model the probability of ruptured appendicitis. PRINCIPAL FINDINGS: Among the 374 Medicaid inpatient claims for appendicitis, 37 percent were for ruptured appendicitis. Among the 5,141 hospital discharges for appendicitis, 30 percent were for ruptured appendicitis. Using Medicaid claims data, the probability of ruptured appendicitis was inversely related to age (OR = 0.86, 95% CI 0.81-0.91), white race (OR = 0.35, 95% CI 0.17-0.71) and preventive care visits (OR = 0.19, 95% CI 0.05-0.77). Using hospital discharge data, age (OR = 0.91, 95% CI 0.90-0.93) and female gender (OR = 0.87, 95% CI 0.77-0.99) were significant covariates. Insurance-related covariates were not significant in multivariate models addressing the probability of ruptured appendicitis. CONCLUSIONS: During a period of rapid managed care growth, insurance type was not associated with an increased risk of ruptured appendicitis among children in this geographic area. Age, female gender, and the number of preventive care visits are inversely related to the risk of ruptured appendix among children. The protective effect of preventive care visits suggests that a primary care relationship facilitates access to care, thus reducing delay in the management of appendicitis.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Addiss D. G., Shaffer N., Fowler B. S., Tauxe R. V. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990 Nov;132(5):910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- Balthazar E. J., Rofsky N. M., Zucker R. Appendicitis: the impact of computed tomography imaging on negative appendectomy and perforation rates. Am J Gastroenterol. 1998 May;93(5):768–771. doi: 10.1111/j.1572-0241.1998.222_a.x. [DOI] [PubMed] [Google Scholar]
- Braveman P., Schaaf V. M., Egerter S., Bennett T., Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994 Aug 18;331(7):444–449. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- Brender J. D., Marcuse E. K., Koepsell T. D., Hatch E. I. Childhood appendicitis: factors associated with perforation. Pediatrics. 1985 Aug;76(2):301–306. [PubMed] [Google Scholar]
- Chande V. T., Kinnane J. M. Role of the primary care provider in expediting care of children with acute appendicitis. Arch Pediatr Adolesc Med. 1996 Jul;150(7):703–706. doi: 10.1001/archpedi.1996.02170320049008. [DOI] [PubMed] [Google Scholar]
- Eldar S., Nash E., Sabo E., Matter I., Kunin J., Mogilner J. G., Abrahamson J. Delay of surgery in acute appendicitis. Am J Surg. 1997 Mar;173(3):194–198. doi: 10.1016/s0002-9610(96)00011-6. [DOI] [PubMed] [Google Scholar]
- Gadomski A., Jenkins P., Nichols M. Impact of a Medicaid primary care provider and preventive care on pediatric hospitalization. Pediatrics. 1998 Mar;101(3):E1–E1. doi: 10.1542/peds.101.3.e1. [DOI] [PubMed] [Google Scholar]
- Golladay E. S., Sarrett J. R. Delayed diagnosis in pediatric appendicitis. South Med J. 1988 Jan;81(1):38–42. doi: 10.1097/00007611-198801000-00008. [DOI] [PubMed] [Google Scholar]
- Goodman D. C., Fisher E. S., Gittelsohn A., Chang C. H., Fleming C. Why are children hospitalized? The role of non-clinical factors in pediatric hospitalizations. Pediatrics. 1994 Jun;93(6 Pt 1):896–902. [PubMed] [Google Scholar]
- Harrison M. W., Lindner D. J., Campbell J. R., Campbell T. J. Acute appendicitis in children: factors affecting morbidity. Am J Surg. 1984 May;147(5):605–610. doi: 10.1016/0002-9610(84)90123-5. [DOI] [PubMed] [Google Scholar]
- Horwitz J. R., Gursoy M., Jaksic T., Lally K. P. Importance of diarrhea as a presenting symptom of appendicitis in very young children. Am J Surg. 1997 Feb;173(2):80–82. doi: 10.1016/S0002-9610(96)00417-5. [DOI] [PubMed] [Google Scholar]
- Körner H., Söndenaa K., Söreide J. A., Andersen E., Nysted A., Lende T. H., Kjellevold K. H. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg. 1997 Mar-Apr;21(3):313–317. doi: 10.1007/s002689900235. [DOI] [PubMed] [Google Scholar]
- Linz D. N., Hrabovsky E. E., Franceschi D., Gauderer M. W. Does the current health care environment contribute to increased morbidity and mortality of acute appendicitis in children? J Pediatr Surg. 1993 Mar;28(3):321–328. doi: 10.1016/0022-3468(93)90225-a. [DOI] [PubMed] [Google Scholar]
- O'Toole S. J., Karamanoukian H. L., Allen J. E., Caty M. G., O'Toole D., Azizkhan R. G., Glick P. L. Insurance-related differences in the presentation of pediatric appendicitis. J Pediatr Surg. 1996 Aug;31(8):1032–1034. doi: 10.1016/s0022-3468(96)90079-2. [DOI] [PubMed] [Google Scholar]
- Pappas G., Hadden W. C., Kozak L. J., Fisher G. F. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997 May;87(5):811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin J. M., Homer C. J., Berwick D. M., Woolf A. D., Freeman J. L., Wennberg J. E. Variations in rates of hospitalization of children in three urban communities. N Engl J Med. 1989 May 4;320(18):1183–1187. doi: 10.1056/NEJM198905043201805. [DOI] [PubMed] [Google Scholar]
- Perrin J. M. Variations in pediatric hospitalization rates: why do they occur? Pediatr Ann. 1994 Dec;23(12):676-7, 681-3. doi: 10.3928/0090-4481-19941201-08. [DOI] [PubMed] [Google Scholar]
- Rao P. M., Rhea J. T., Novelline R. A., Mostafavi A. A., McCabe C. J. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998 Jan 15;338(3):141–146. doi: 10.1056/NEJM199801153380301. [DOI] [PubMed] [Google Scholar]
- Rappaport W. D., Peterson M., Stanton C. Factors responsible for the high perforation rate seen in early childhood appendicitis. Am Surg. 1989 Oct;55(10):602–605. [PubMed] [Google Scholar]
- Weissman J. S., Gatsonis C., Epstein A. M. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992 Nov 4;268(17):2388–2394. [PubMed] [Google Scholar]
- Williams N., Bello M. Perforation rate relates to delayed presentation in childhood acute appendicitis. J R Coll Surg Edinb. 1998 Apr;43(2):101–102. [PubMed] [Google Scholar]
- Young I., Moss K. W. Acute appendicitis in children in a community hospital: a five year review. Alaska Med. 1997 Apr-Jun;39(2):34–42. [PubMed] [Google Scholar]


