Abstract
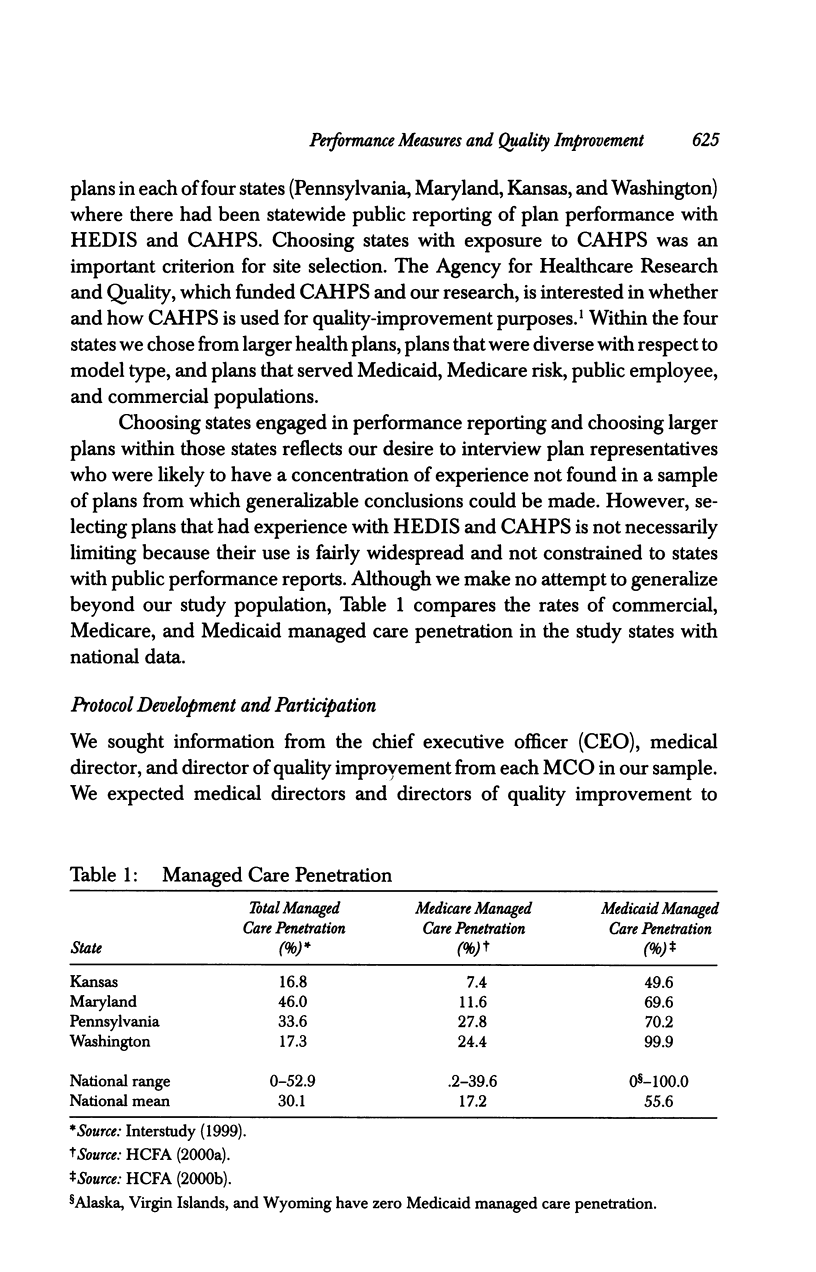
OBJECTIVES: To understand how managed care plans use performance measures for quality improvement and to identify the strengths and weaknesses of currently used standardized performance measures such as the Health Plan Employer Data and Information Set (HEDIS) and the Consumer Assessment of Health Plans (CAHPS) survey. DATA SOURCES/STUDY SETTING: Representatives (chief executive officers, medical directors, and quality-improvement directors) from 24 health plans in four states were surveyed. The overall response rate was 58.3 percent, with a mean of 1.8 respondents per plan. STUDY DESIGN: This exploratory qualitative research used a purposive sample of respondents. Two study authors conducted separate one-hour tape-recorded telephone interviews with multiple respondents from each health plan. PRINCIPAL FINDINGS: All managed care organizations interviewed use performance measures for quality improvement but the degree and sophistication of use varies. Many of our respondent plans use performance measures to target quality-improvement initiatives, evaluate current performance, establish goals for quality improvement, identify the root cause of problems, and monitor performance. CONCLUSION: Performance measures are used for quality improvement in addition to informing external constituents, but additional research is needed to understand how the benefits of measurement can be maximized.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chernew M., Scanlon D. P. Health plan report cards and insurance choice. Inquiry. 1998 Spring;35(1):9–22. [PubMed] [Google Scholar]
- Goverman I. L. Orienting health care information systems toward quality: how Group Health Cooperative of Puget Sound did it. Jt Comm J Qual Improv. 1994 Nov;20(11):595–605. doi: 10.1016/s1070-3241(16)30107-9. [DOI] [PubMed] [Google Scholar]
- Hillman A. L., Goldfarb N. Exemplary quality improvement programs in HMOs. Jt Comm J Qual Improv. 1995 Sep;21(9):457–464. doi: 10.1016/s1070-3241(16)30172-9. [DOI] [PubMed] [Google Scholar]
- Kinney C. F., Gift R. G. Building a framework for multiple improvement initiatives. Jt Comm J Qual Improv. 1997 Aug;23(8):407–423. doi: 10.1016/s1070-3241(16)30328-5. [DOI] [PubMed] [Google Scholar]
- Landon B. E., Epstein A. M. Quality management practices in Medicaid managed care: a national survey of Medicaid and commercial health plans participating in the Medicaid program. JAMA. 1999 Nov 10;282(18):1769–1775. doi: 10.1001/jama.282.18.1769. [DOI] [PubMed] [Google Scholar]
- Landon B. E., Tobias C., Epstein A. M. Quality management by state Medicaid agencies converting to managed care: plans and current practice. JAMA. 1998 Jan 21;279(3):211–216. doi: 10.1001/jama.279.3.211. [DOI] [PubMed] [Google Scholar]
- Peterson M. A. Introduction: politics, misperception, or apropos? J Health Polit Policy Law. 1999 Oct;24(5):873–886. doi: 10.1215/03616878-24-5-873. [DOI] [PubMed] [Google Scholar]
- Scanlon D. P., Chernew M. HEDIS measures and managed care enrollment. Med Care Res Rev. 1999;56 (Suppl 2):60–84. [PubMed] [Google Scholar]
- Scanlon D. P., Hendrix T. J. Health plan accreditation: NCQA, JCAHO, or both? Manag Care Q. 1998 Autumn;6(4):52–61. [PubMed] [Google Scholar]
- Scanlon D. P., Rolph E., Darby C., Doty H. E. Are managed care plans organizing for quality? Med Care Res Rev. 2000;57 (Suppl 2):9–32. doi: 10.1177/1077558700057002S02. [DOI] [PubMed] [Google Scholar]
- Stolar M. W. Clinical management of the NIDDM patient. Impact of the American Diabetes Association practice guidelines, 1985-1993. Endocrine Fellows Foundation Study Group. Diabetes Care. 1995 May;18(5):701–707. doi: 10.2337/diacare.18.5.701. [DOI] [PubMed] [Google Scholar]
- Worrall G., Freake D., Kelland J., Pickle A., Keenan T. Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines. J Fam Pract. 1997 Apr;44(4):374–381. [PubMed] [Google Scholar]



