Abstract
Endometriosis is linked to increased infertility and pregnancy complications due to defective endometrial decidualization. We hypothesized that identification of altered signaling pathways during decidualization could identify the underlying cause of infertility and pregnancy complications. Our study reveals that transforming growth factor β (TGFβ) pathways are impaired in the endometrium of individuals with endometriosis, leading to defective decidualization. Through detailed transcriptomic analyses, we discovered abnormalities in TGFβ signaling pathways and key regulators, such as SMAD4, in the endometrium of affected individuals. We also observed compromised activity of bone morphogenetic proteins (BMP), a subset of the TGFβ family, that control endometrial receptivity. Using 3-dimensional models of endometrial stromal and epithelial assembloids, we showed that exogenous BMP2 improved decidual marker expression in individuals with endometriosis. Our findings reveal dysfunction of BMP/SMAD signaling in the endometrium of individuals with endometriosis, explaining decidualization defects and subsequent pregnancy complications in these individuals.
Subject terms: Transcriptomics, Mechanisms of disease
Transcriptomic and genomic studies indicate that disrupted bone morphogenetic protein pathways may be a root cause of flawed endometrial decidualization in individuals with endometriosis. Enhancing these pathways with BMP2 supplementation shows promise in mitigating these defects.
Introduction
Endometriosis is a debilitating disease affecting 190 million women of reproductive age globally1. Defined as the occurrence of endometrial glands and stromal compartments outside of the uterine cavity, endometriosis leads to an inflammatory state, not only locally within the lesion sites and pelvic cavity, but systemically as well2,3. Lesions are typically located within the pelvic areas but can also involve distant sites4. Patients with endometriosis often suffer from chronic pelvic pain, severe dysmenorrhea, or infertility, which significantly decrease the quality of life of the affected patients. Currently, there is no definite explanation for the pathogenesis of endometriosis; however, several theories have been proposed to explain the disease, including retrograde menstruation5, recruitment and transformation of mesenchymal and hematopoietic stem cells6, müllerian duct remnants7, and the coelomic metaplasia theories8. Regardless of their initial pathogenesis, the main symptomatic process involves increased production of inflammatory cytokines and pain mediators, as well as dysfunction of sympathetic nerve fibers9–11. Treatment options for endometriosis are limited to empirical nonsteroidal anti-inflammatory drugs, hormonal therapies, or surgery12.
In addition to causing pain and inflammation, endometriosis often leads to infertility13–15. Around 40 percent of women with endometriosis are estimated to have infertility16,17, and of women with infertility, 25 to 50 percent are estimated to also suffer from endometriosis18,19. Endometriosis affects fecundity by impairing ovarian function, inducing chronic intraperitoneal inflammation and through a state of progesterone resistance14,20. Patients with endometriosis present with an abnormally prolonged follicular phase21, which further leads to dysfunctional folliculogenesis and granulosa cell cycle kinetics22,23. As a key feature of endometriosis, chronic intraperitoneal inflammation stems from increased levels of inflammatory cytokines, chemokines as well as prostaglandins. Such inflammatory processes can lead to infertility by decreasing intrafollicular estrogen level24, oocyte quality25 and sperm motility25.
The normal function of the eutopic endometrium is also compromised in patients with endometriosis, as demonstrated by progesterone resistance that is characterized by declined expression of progesterone receptor (PR) and coactivators26,27. Deficient progesterone signaling pathways likely lead to impaired decidualization, defective embryo implantation and increased infertility rates in patients with endometriosis28. During pregnancy, individuals with endometriosis also experience higher rates of gestational complications, including preterm birth and antepartum hemorrhage29,30. These defects which arise during later pregnancy, are likely fueled by defects during early pregnancy and decidualization, which negatively affect immune cell infiltration and the degree of spiral artery remodeling30. Additional signaling defects have been identified in the endometrium of women with endometriosis, including defective mesenchymal stem cell differentiation31,32, increased decidual senescence and elevated pro-inflammatory stress33. Despite this progress, actionable therapeutic targets to improve the fertility outcomes in individuals with endometriosis are lacking. Uncovering the mechanisms and pathways involved that negatively impact the eutopic endometrium in patients with endometriosis is critical to help optimize chances for successful pregnancy.
Our studies aim to uncover the molecular underpinning of infertility associated with endometriosis by focusing on transcriptomic signatures of the eutopic endometrium from individuals with endometriosis. Here, we use patient-derived stromal cells and state-of-the-art endometrial stromal and epithelial assembloids to define key signaling alterations during decidualization in patients with endometriosis.
Results
Transcriptomic profiling in endometrial stromal cells from individuals with and without endometriosis reveals activation of key pathways during early and late in vitro decidualization
The human endometrium undergoes spontaneous decidualization in response to the rising levels of progesterone34–36. The concerted action of estrogen and progesterone transforms the endometrium from a non-receptive state into a receptive state, subsequently allowing embryo implantation and development to occur. Because patients with endometriosis can have decreased fecundity due in part, to defective endometrial function30, we aimed to systematically determine the transcriptomic differences between the two groups during in vitro stromal cell decidualization. Previous analyses were performed to determine the decidualization potential of endometrial stromal cells from normal patients during the early and late decidualization phases37,38. These studies found unique transcriptional signatures that were activated at each phase, indicating that the process of decidualization is a transcriptionally active process that requires long-term remodeling of chromatin and subsequent changes in gene expression37,38. Other studies compared the decidualization potential of endometrial stromal cells obtained from individuals with and without endometriosis, however these studies focused only on the late phases of decidualization39. To identify markers and pathways that are differentially controlled in the eutopic endometrium of individuals without endometriosis, we performed transcriptomic analyses of stromal cells from individuals with and without endometriosis that were induced to decidualize in vitro during early and late phases.
We used a well-characterized method36,40–42 to induce endometrial stromal cell decidualization and to compare differentially expressed genes between normal and endometriosis samples from the early (2 days) to late (8 days) stages of decidualization. Patient-derived endometrial stromal cells from patients with and without endometriosis were cultured in vitro and treated with estrogen (E2), medroxyprogesterone acetate (MPA) and 8-bromo cyclic adenosine monophosphate (cAMP) (EPC) to induce decidualization in vitro, and then collected at 2, 4, 6, 8 days after EPC cocktail treatment to profile transcriptomic changes using RNA sequencing (Fig. 1A). We performed a time course comparison between the differentially expressed genes at each timepoint respectively. In total, 334 transcripts changed significantly during the EPC treatment in the cells derived from individuals without endometriosis (n = 3, normal), with 152 transcripts showing an increase and 182 showing a decrease by day 8 of EPC treatment (Supplementary Data File 1, > 1.4, < 0.4-fold change, FDR < 0.05). In stromal cells from individuals with endometriosis (n = 4), 878 transcripts showed a significant change after EPC treatment, with 464 being increased and 414 decreased by Day 8 of EPC treatment (Supplementary Data File 1, > 1.4, < 0.4-fold change, FDR < 0.05). Among these, only 122 transcripts (12.4%) were shared between normal and endometriosis upregulated genes, and 105 (10.7%) shared genes were conserved in the downregulated genes between the two groups (Supplementary Fig. 1A). These results indicate that endometrial stromal cells arising from individuals with endometriosis display a unique transcriptomic response to decidualization treatment in vitro that is different to stromal cells derived from individuals without endometriosis.
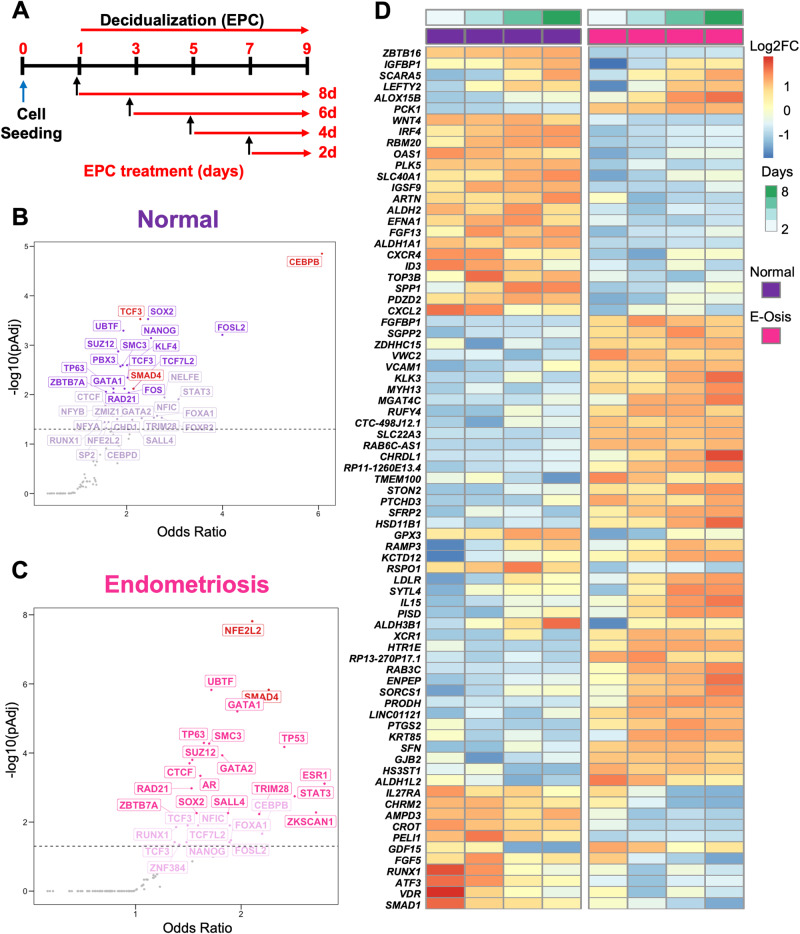
Fig. 1. Transcriptomic profiling of endometrial stromal cells from individuals with or without endometriosis reveals key differences during in vitro decidualization.
A Primary endometrial stromal cell cultures from individuals without (n = 3, “normal”) or with endometriosis (n = 4) were subjected to a time-course decidualization treatment. After plating, cells were treated with vehicle or with the decidualization cocktail (35 nM estradiol, 1 µM medroxyprogesterone acetate, 50 µM cAMP, “EPC”) for 2, 4, 6, or 8 days. RNA sequencing was performed and the decidualization response within normal and endometriosis stromal cells was determined by normalizing differentially expressed genes relative to the Day 0 (vehicle)-treated cells. B, C Upstream transcriptional regulators were identified by searching for conserved ENCODE and ChEA consensus gene targets among the differentially expressed genes in the normal (B) and endometriosis (C) groups. CEBP/β and TCF3 emerged as top transcription regulators for normal decidualizing cells (B), while NFE2L2 and SMAD4 were determined to be major upstream regulators for endometriosis. D Heatmap displays gene expression over time within the normal and endometriosis (“E-Osis”) groups treated with EPC using normalized z-scores. Color represents log2 fold-change relative to baseline (day 0).
Gene ontology classification and upstream factor analyses reveal enrichment of TGFβ signaling and oxidative stress response in endometriosis
To understand the pathways that were overrepresented among the differentially expressed genes, we performed a gene ontology analysis of all the differentially regulated genes (> 1.4, < 0.4-fold change, FDR < 0.05) in the normal or endometriosis datasets (Supplementary Data File 2). Among the top categories in the normal donors, we found that “VEGFA/VEGFR2 signaling” (Day 8) (Supplementary Fig. 1B) corresponded to increased levels of SH2D2A, encoding an adaptor protein that binds to VEGFR and amplifies its signal43. Other enriched categories were “mRNA Protein and Metabolite Inducation Pathway By Cyclosporine A” and “Amino Acid Metabolism in Triple Negative Cancer”, which represented genes such as SLC1A5 and SLC7A5, whose gene expression decreased during decidualization (Supplementary Fig. 1B and Supplementary Data File 2). These transporters have been previously shown to be dynamically controlled in the endometrium during the peri-implantation period of pregnancy in other animal species44,45. Enriched pathways in the endometriosis dataset included “Neuroinflammation and Glutamatergic Signaling”, with genes such as TNFRSF1B showing increased expression during decidualization. TNFRSF1B encodes the TNFα receptor, TNFR2; both TNFR1 and TNFR2 have been investigated as potential biomarkers for endometriosis, given the pro-inflammatory roles of TNFα signaling46,47. The “Nuclear Receptors Meta Pathway,” listed that vitamin D receptor, VDR, as being represented in our dataset of decidualized cells from donors with endometriosis. Our time course decidualization results (Supplementary Data File 1) showed that VDR was consistently decreased during decidualization (EPC Day 8, −2.00 Log FC, FDR = 0.0004). VDR signaling is crucial for stromal cell decidualization and early pregnancy progression, suggesting that defects in this pathway may contribute to fertility defects in women with endometriosis48. Another overrepresented pathway in our analysis included the “BMP2 WNT4 FOXO1 Pathway In Primary Endometrial Stromal Cell Differentiation,” where we observed that the gene encoding the canonical transcription factor for BMP signaling, SMAD1, was decreased during decidualization. We conclude that this time course decidualization profiling identified several gene categories and signaling pathways that are differentially regulated in decidualizing stromal cells from donors with and without endometriosis.
We performed an upstream transcription factor analysis of the differentially regulated genes in the endometriosis or normal stromal cells to identify master regulatory networks driving the differential transcriptional response (Supplementary Data File 3). By mining the consensus gene targets in the ENCODE and ChEA Transcription Factor Targets dataset49,50, we identified that genes regulated by the CCAAT Enhancer Binding Protein Beta (CEBP/β) and Transcription Factor 3 (TCF3) were enriched in the normal stromal cells (Fig. 1B). CEBP/β has been shown to be a key factor in endometrial stromal cell decidualization that controls the transcription of the PR51,52 TCF3 is also shown to control endometrial stromal cell proliferation and decidualization53.
On the other hand, regulation of genes by the NFE2 Like BZIP Transcription Factor 2 (NFE2L2) and SMAD4 transcription factors was highly enriched in the endometriosis dataset (Fig. 1C). NFE2L2, encodes NRF2, and is an important regulator of oxidative stress response that controls the expression of genes that contribute to ferroptosis resistance54–56. SMAD4 is the downstream activated transcription factor controlling expression of genes downstream of bone morphogenetic proteins (BMPs, through SMAD1 and SMAD5) or TGFβ/activin ligands (through SMAD2 and SMAD3)57. Some of these differential responses could also be observed at the gene level (Fig. 1D), as indicated by the expression of IGFBP158, ZBTB1659 (decidualization markers), SLC40A1, GPX3, PTGS260,61 (markers of oxidative stress and ferroptosis), or LEFTY2, SMAD162 (BMP/SMAD-signaling pathways). To further expand on the expression patterns of the TGFβ signaling family, we visualized the time-dependent expression patterns of all members of this family (Supplementary Fig. 1E).
In summary, we observed that conventional transcriptional programs driving decidualization were found to be overrepresented in the endometrial stromal cells from individuals without endometriosis, indicating a normal decidualization response. However, endometrial stromal cells from individuals with endometriosis displayed an impaired response to oxidative stress and defective BMP/TGFβ signaling pathways.
Identification of perturbed BMP/TGFβ signaling pathways in the decidualizing stromal cells from individuals with endometriosis
We examined the dynamic profiles in the early and late decidual cell transcriptomes and visualized the differentially expressed genes between individuals with and without endometriosis in volcano plots using a >2 or < ½ fold-change and FDR < 0.05 (Fig. 2A–D). At baseline, we observed that 612 transcripts were differentially expressed between the normal and endometriosis groups, with 261 being upregulated and 351 downregulated in the endometriosis group compared to the normal group (Supplementary Data File 4). Two days after EPC administration, 425 genes were downregulated in the endometriosis samples compared to the normal counterparts. We then observed 364, 207, and 179 genes to be downregulated on Day 4, Day 6, and Day 8, in endometriosis samples compared to the normal samples, respectively. Meanwhile, 335, 263, 147 and 97 genes were upregulated in endometriosis compared to normal at Day 2, Day 4, Day 6, and Day 8, respectively (Supplementary Data File 4).
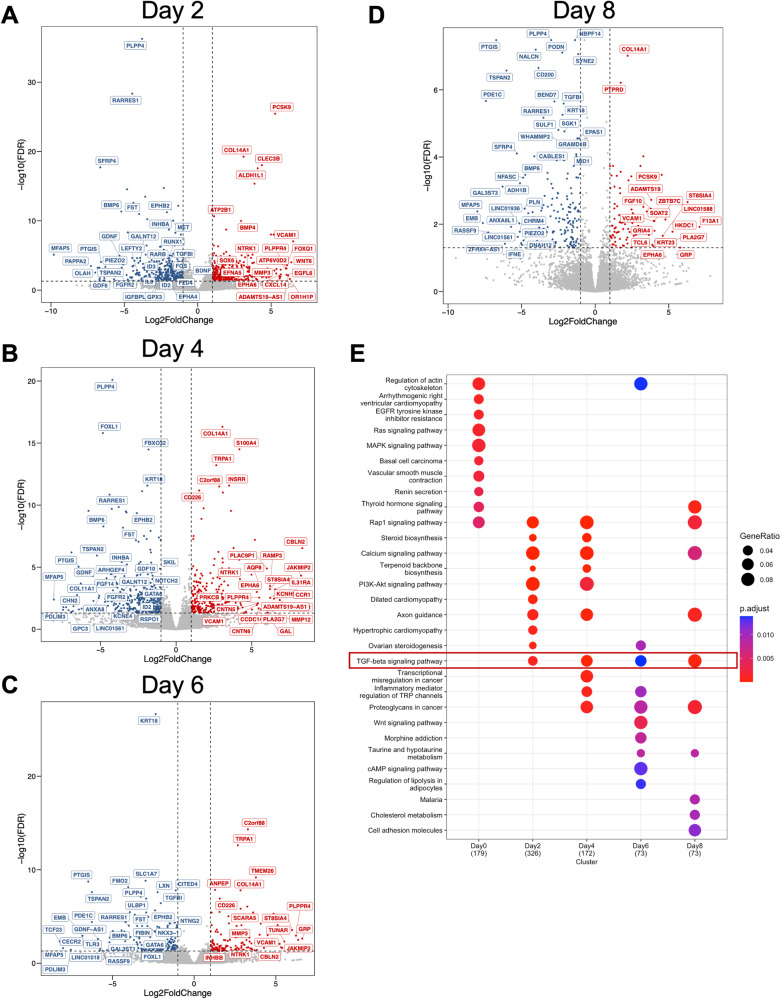
Fig. 2. BMP/TGFβ signaling pathways are defective in the decidualizing stromal cells from individuals with endometriosis.
Differentially expressed genes between the endometrial stromal cells of individuals without (n = 4) or with endometriosis (n = 3) at each time point during the decidualization treatment were identified and visualized as volcano plots. Differentially expressed genes were determined using a cut off ( | log2 fold-change | >1 and FDR < 0.05, red denotes increased genes, blue denotes decreased genes, gray indicates no significant change) and displayed following Day 2 (A), Day 4 (B), Day 6 (C), or Day 8 (D) of treatment with the EPC decidualization cocktail (35 nM estradiol, 1 µM medroxyprogesterone acetate, 50 µM cAMP). E Gene ontology analysis of the differentially expressed genes was performed at each time point and visualized as a dot plot. Genes in the TGFβ signaling pathway were identified to be enriched at each of the time points after EPC treatment.
To understand the pathway dependent differences in the endometriosis groups, we implemented Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis in the differentially expressed genes spanning from Day 0 to Day 8 timepoints between normal and endometriosis donors (Fig. 2E, and Supplementary Data File 4). Our enrichment analysis showed distinct enrichment patterns at each of the different time points we assessed. Of notice, the TGFβ signaling pathway was the only category shared in the timepoints during decidualization. Alterations in this category included mostly the ligands of the TGFβ family, such as BMP4, BMP2, LEFTY2, GDF6, INHBA, and LTBP1, in which BMPs typically signal through the SMAD1/5/4 transcription factors while TGFβ and activins signal through the SMAD2/3/4 transcription factors62. We also observed persistent downregulation of the classical BMP/SMAD1/5/4 target genes, ID2 and ID3, suggesting that impaired BMP signaling was resulting in decreased transcriptional activation by SMAD1/5/4 in stromal cells derived from individuals with endometriosis.
Interestingly, we observed that while the TGFβ signaling pathway was persistently overrepresented during the time course analysis, the difference was less pronounced at day 6 (Fig. 2E). We observed that fewer genes categorized as members of the TGFβ signaling pathway were present at this timepoint (4 genes at day 6, versus 12 genes at day 2, 9 genes at day 4, and 6 genes at day 8) (Supplementary Data File 4). Three of the genes differentially regulated at day 6 were conserved during all the other timepoints, LRRC32 (0.142-fold, FDR < 0.0001), FST (0.109-fold change, FDR < 0.001), and BMP6 (0.027-fold change, FDR < 0.01). Notably, fibrillin (FBN1), was the only gene to show differential expression between the normal and endometriosis groups at day 6 of decidualization. Compared to decidualized cells from normal donors, FBN1 expression was elevated (2.09-fold, FDR < 0.0001) in the decidualized cells of donors with endometriosis (Supplementary Data File 4). Fibrillin is an extracellular glycoprotein that associates with elastic fibers of the extracellular matrix and controls the bioavailability of TGFβ, leading to increased signaling and excessive extracellular matrix deposition63. Fibrillin autoantibodies are commonly found in patients with autoimmune conditions characterized by excessive extracellular matrix deposition, such as systemic sclerosis, connective tissue disease and scleroderma64–66. Increased anti-fibrillin antibodies have also been found in women with recurrent pregnancy loss67, suggesting elevated fibrillin has a pathogenic role in pregnancy progression.
After overlapping the differentially expressed genes from different time points, we identified that 48 genes were consistently down-regulated and that 20 genes were consistently up-regulated regardless of the EPC treatment length (Supplementary Fig. 2A, B). Further enrichment for genes associated with human diseases by DisGeNET68 revealed that the 48 consistently down-regulated genes in the individuals with endometriosis were significantly associated with fertility complications such as early pregnancy loss, miscarriage, and spontaneous abortion (Supplementary Fig. 2C, Supplementary Data File 4).
We also observed that genes related to retinoic acid synthesis and metabolism were persistently decreased in the endometriosis group compared to the normal group during decidualization (Supplementary Data File 4). For example, the retinoic acid receptor responder 1 (RARRES1) was significantly decreased in endometriosis across all the time points. Aldehyde dehydrogenase 1 family member B1 (ALDH1B1) was also significantly decreased in endometriosis relative to normal decreased across all time points. Retinoic acid receptor beta (RARB) was decreased on days 2 and 4 of EPC treatment in endometriosis relative to normal. Reprogramming of the endometrium by retinoic acid signaling is critical for endometrial decidualization and early pregnancy69,70. Furthermore, altered retinoic acid metabolism also affects endometriotic stromal cell decidualization71. Therefore, our results are in line with previous observations, and support the hypothesis that alterations in retinoic acid metabolism drive fertility defects in individuals with endometriosis.
We also observed that the GATA protein binding 6 (GATA6) was significantly decreased in the endometriosis group relative to normal cells on days 0, 2, 4, 6, and 8 of EPC treatment. GATA6 is a PR direct target gene72 and is upregulated in ectopic endometriotic stromal cells from lesions due to methylation defects73,74. Overall, the time course decidualization analysis between normal and endometriosis donors highlighted various pathways that are differentially expressed between the two groups, providing additional therapeutic or diagnostic opportunities for endometriosis-associated infertility. Furthermore, results from our transcriptomic profiling emphasized the critical roles of the BMP signaling pathways in driving the decidualization processes of the normal endometrium.
Time course analysis identifies expression of key branching points during decidualization
Using time course analysis of decidualization at the single cell level, previous studies identified the trajectory of decidualizing cells over time and showed the presence of branching points, with cells diverging into decidual or senescent decidual cells75. In their study, it was shown that non-senescent decidual cells clustered into groups expressing FTL (ferritin light chain) and SCARA5 (scavenger receptor class A member 5), while senescent decidual cells expressed markers of extracellular matrix (ECM) remodeling factors CLU (clusterin), ADAMTS5 (ADAM metallopeptidase with thrombospondin type 1 motif 5), CEMIP (cell migration inducing hyaluronidase 1, also known as KIAA1199), and ABI3BP (ABI family member 3 binding protein). To determine how our time course analysis of decidualization aligned with their results, we correlated the top 50 genes corresponding to the decidual/senescence branchpoint with our set of DEGs from the time course analysis at EPC Day 8 (from Supplementary Data File 1). We identified that genes involved in immune surveillance, such as TIMP3 and CXCL14 were increased in the decidualizing stromal cells from donors with endometriosis relative to cells from normal donors (Supplementary Fig. 1D). These genes are implicated in immune recognition of stressed or senescent cells, suggesting that the expression of these genes rises in decidualizing cells of endometriosis possibly due to decidual senescence. Indicative of a higher state of cellular stress, we also found that the decidualizing cells of donors with endometriosis displayed higher expression of stress response genes, such as CRYAB, HSD11B1 and GLRX (Supplementary Fig. 1D). In the study by Lucas ES et al.76, high expression of DIO2 was identified as a key marker in the divergence into decidual cells along with a cluster of cells expressing high CLU, ALDH1A1, ADAMTS5, ABI3BP, and CEMPI. Our analysis showed that the decidualizing cells from patients with endometriosis displayed decreasing expression of DIO2, CLU and ALDH1A1, but elevated expression of ADAMTS5, ABI3BP, CEMPI and COL14A1 (Supplementary Fig. 1D). Thus, our results suggest that decidualizing cells from patients with endometriosis display expression of genes associated with elevated immune surveillance, stress response, and that their transcriptomic signature partially correlates with the signature of decidual senescence. The discordance in some of the markers of senescence could be attributed to the fact our analysis is based on the results of bulk sequencing versus the more sensitive single cell analysis performed by Lucas ES et al.76.
Altered BMP signaling impairs decidualization in the endometrium of individuals with endometriosis
Our time course transcriptomic analyses revealed that BMP ligands and SMAD1/5/4 transcriptional targets, ID2 and ID3, were consistently downregulated in stromal cells from individuals with endometriosis during in vitro decidualization (Fig. 2). Previous studies in mouse models indicate that BMP signaling via the SMAD1/5 transcription factors is essential for endometrial receptivity, embryo implantation and decidualization77–80. To explore the specific roles of BMP signaling pathways in the decidualization defects observed in individuals with endometriosis, we first assessed the activation of BMP signaling pathways at different time points during time course decidualization. As shown in Fig. 3A, in the samples from individuals without endometriosis (n = 5), SMAD1/5, the signal transducers of the BMPs, were activated in a time-dependent manner. Upon EPC stimulation, phosphorylated SMAD1/5 (pSMAD1/5) gradually increased along with the EPC treatment length. However, in the samples derived from individuals with endometriosis (n = 4), activation of the BMP signaling pathway was impaired, as manifested by the decreased levels of pSMAD1/5 during the time course EPC stimulation (Fig. 3B, C). Gene expression analysis using RT-qPCR demonstrated decidual markers such as BMP2 and IGFBP1 showed increasing levels throughout Day 2 to Day 8 EPC treatment in the stromal cells with blunted induction in the endometriosis cells (Fig. 3D, E). These results indicate that while normal decidualizing stromal cells successfully engage BMP/SMAD1/5 signaling, stromal cells from endometriosis did not induce BMP/SMAD1/5 signaling and failed to decidualize.
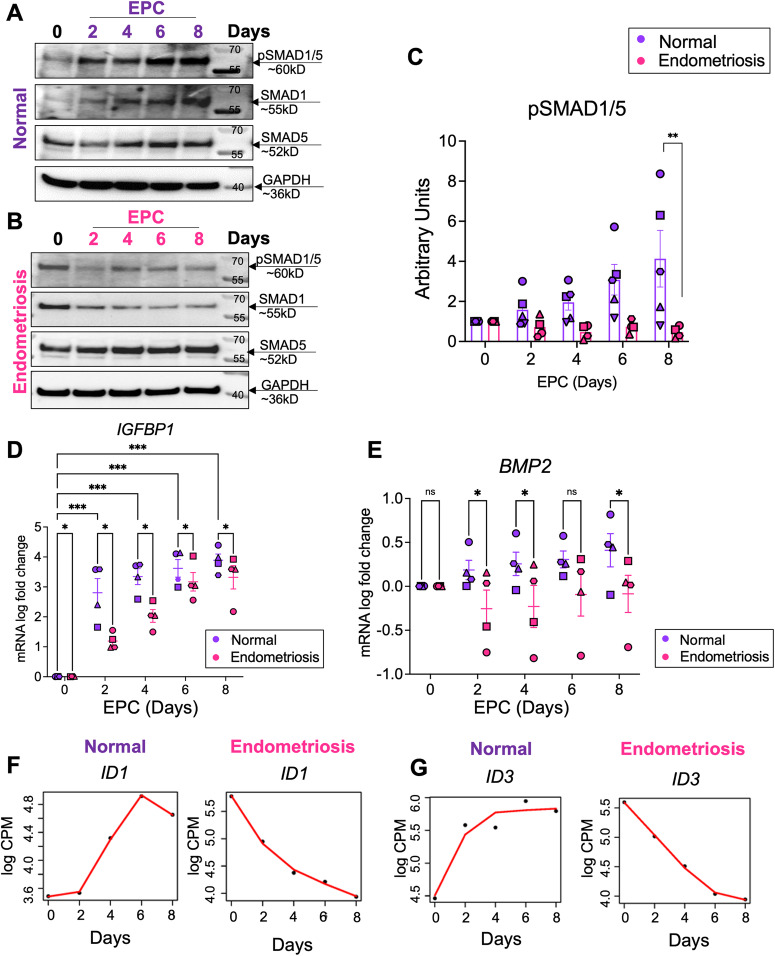
Fig. 3. Impaired BMP signaling perturbs decidualization in the endometrium of individuals with endometriosis.
A, B Lysates from endometrial stromal cells of individuals without (A, “normal”) with endometriosis (B) after 2, 4, 6, or 8 days of EPC treatment were probed with antibodies to detect phosphorylated SMAD1/5 (pSMAD1/5), total SMAD1, total SMAD5, or GAPDH expression. C Densitometric analysis of pSMAD1/5 in the EPC-treated stromal cells from individuals without (n = 5) or with endometriosis (n = 4). The different symbols represent individual patient trajectories per sample. One way ANOVA with a Tukey’s posttest. D, E Quantitative reverse transcriptase PCR (qRT-PCR) was used to determine the expression of BMP2 and IGFBP1 in the endometrial stromal cells from individuals without (C, n = 4) or with endometriosis (D, n = 4). The different symbols represent individual patient trajectories per sample. Data in (D, E) were log transformed and analyzed using a 2-Way ANOVA with a Tukey’s multiple comparison posttest. F, G Time course analysis from the RNAseq analysis comparing the increasing gene expression patterns of ID1 and ID3 in normal and decreasing gene expression pattern in endometriosis stromal cells. EPC, 35 nM estradiol, 1 µM medroxyprogesterone acetate, 50 µM cAMP.
The discrepancy in response to the EPC treatment observed between individuals with and without endometriosis was also identified from the RNA-seq data. Figure 3F, G shows exemplary genes that present contrasting trends during our time course decidualization analysis. Similar to BMP2, the ID1 and ID3 genes were progressively increased over the time course treatment in the samples derived from donors without endometriosis while they were conversely downregulated in the endometriosis cohort. Inhibitor of DNA-binding (ID) genes are not only known downstream BMP responsive genes81,82 but also are important for endometrial remodeling and decidua formation83–85. Such inverted trends substantiated the dysfunctional BMP signaling pathways in the endometriosis groups. Our data indicated that in individuals with endometriosis, an impaired BMP signaling pathway is accompanied by dysfunctional endometrial decidualization.
Genome-wide binding of SMAD4 reveals differential binding patterns in the endometrium of individuals with and without endometriosis
Upon ligand binding, canonical BMP signaling pathways use SMAD1/5/4 proteins to initiate transcriptional regulation. SMAD1/5 forms heterodimers and translocate into the nucleus together with common SMAD462. Given that BMP/SMAD1/5/4 signaling is essential for implantation and decidualization77–80,85,86, our goal was to investigate the mechanisms that underpin defective BMP signaling in individuals with endometriosis during decidualization at the transcriptional level. To do so, we utilized the Cleavage Under Targets & Release Using Nuclease (CUT&RUN) method to profile the genome-wide SMAD4 binding sites in the EPC-treated (4 days) endometrial stromal cells derived from both individuals with and without endometriosis. We observed a distinct pattern of SMAD4 binding activities between the two groups (Supplementary Fig. 3A, B). We exemplified the binding activities by showing the Integrative Genomics Viewer (IGV) track view of the ID1 and ID3 loci. We observed that SMAD4 binding was diminished in the endometriosis groups at the ID1 and ID3 loci (Fig. 4A). In total, we identified 2060 peaks showing differences in signal intensity between normal and endometriosis groups (Supplementary Data File 5). Among these, 1190 peaks showed decreased enrichment in the endometriosis group, while 870 peaks had increased enrichment in the endometriosis group.
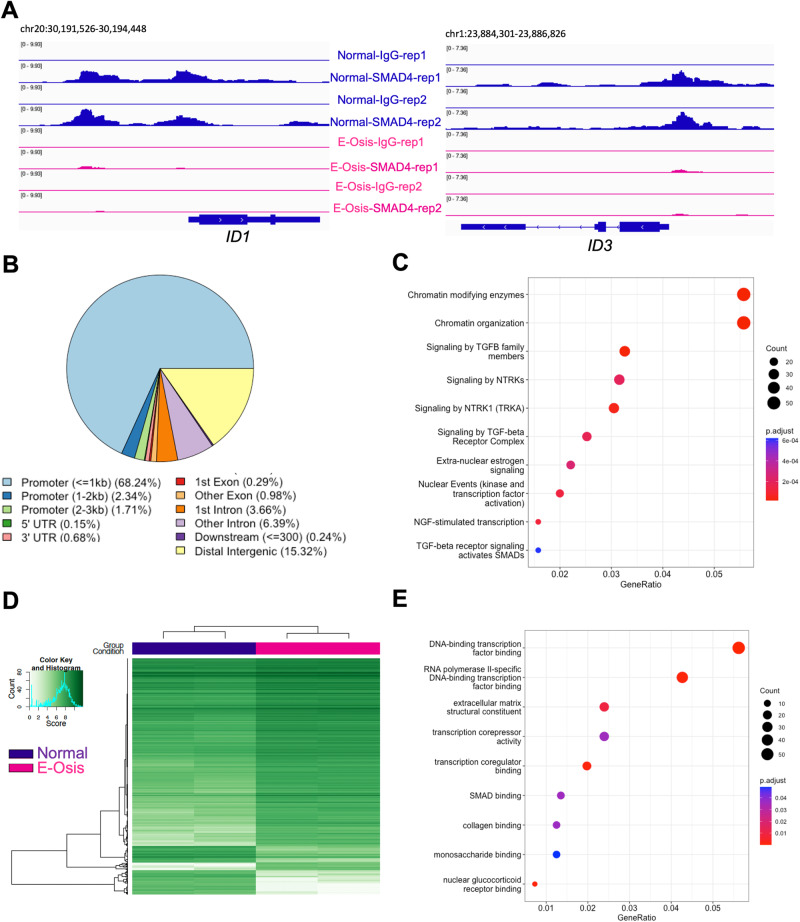
Fig. 4. SMAD4 and H3K27ac CUT&RUN reveals differential binding events in the endometrial stromal cells of individuals with endometriosis.
CUT&RUN was performed for SMAD4 and H3K27ac in endometrial stromal cells from individuals with or without endometriosis induced to decidualize for 4 days to identify differences or similarities in their genome-wide distribution. A Genome track views for the ID1 and ID3 genes displaying the enriched SMAD4 peaks obtained from the normal cells (blue) that are decreased in the endometriosis cells (pink). B Peak annotation of the SMAD4 peaks in 2060 peaks showing differences in signal intensity between normal and endometriosis samples, showing many of the differential peaks (72.29%) were located proximal to the promoter region (within ± 3 kb promoter region). C Reactome analysis showing classification of genes that were differentially bound by SMAD4 in the endometriosis samples. Chromatin modifications and signaling by TGFβ family members were in the top three categories. D H3K27ac CUT&RUN was performed in endometrial stromal cells from individuals without endometriosis (“Normal”) or with endometriosis (“E-Osis”) after 4 days of EPC treatment. The heatmap shows the peak signal obtained for H3K27Ac in normal versus endometriosis stromal cells. E Gene ontology classification of the 1122 peaks that were more enriched in the endometriosis samples.
Peak annotation revealed that the majority of these peaks were located within the ± 3 kb promoter region (72.29%) (Fig. 4B, Supplementary Data File 5). Additionally, we performed the Reactome pathway enrichment87 for the genes that were differentially bound by SMAD4 in the endometriosis group (Fig. 4C, Supplementary Data File 5). We found that categories related to ‘signaling by TGFβ family members’, ‘signaling by TGFβ receptor complexes’, and ‘TGFβ activated SMADs’ were enriched. These findings agreed with our transcriptomic results and indicated that a defective TGFβ/SMAD4 signaling program is abnormal in the endometrium of individuals with endometriosis. Because SMAD4 is the “common” SMAD that forms a complex with both BMP-SMAD1/5 and TGFβ/activin-SMAD2/3, our CUT&RUN experiments cannot specifically differentiate between the two pathways or differentiate between SMAD1/5 and SMAD2/3-mediated signaling. However, given that SMAD4 enrichment was decreased at the ID1 and ID3 promoter regions, and this corresponds with decreased ID gene expression, it was likely that BMP signaling pathways also impair SMAD1/5/4 binding activities in the stromal cells from individuals with endometriosis. To identify the potential for a direct transcriptional regulation of SMAD4 on canonical decidualization genes (IGFBP1, PRL, SPP1, FOXO1), we searched for SMAD4 peaks mapping to these genes. While no significant peaks were identified for IGFBP1, PRL or SPP1, we did observe SMAD4 enrichment mapping to the FOXO1 TSS and gene body (Supplementary Fig. 3C). The data suggest that BMP2/SMAD4 signaling directly control the transcriptional activation of FOXO1 during decidualization, but not of other decidual markers. However, this does not rule out that the expression of key decidual markers was affected by a secondary cascade.
Interestingly, apart from TGFβ related categories, pathways involved in ‘chromatin modifying enzymes’, ‘signaling by NTRKs,’ and ‘NGF-stimulated transcription,’ were also among the top enriched categories (Fig. 4C). Neurotrophic tyrosine receptor kinases (NTRKs) are well-documented for their roles in pain and inflammation in endometriosis and are elevated in the endometriotic lesions of affected patients88–90. Nerve growth factors91 signal through the NTRKs and were recently shown to be associated with endometriosis through genome-wide association studies92. Hence, our studies suggest that abnormal NTRK signaling may also impact the eutopic endometrium and affect receptivity in patients with endometriosis.
To further delineate the chromatin level differences between the normal and endometriosis groups, we profiled the depositions of histone mark H3K27 acetylation (H3K27ac) in the EPC-treated stromal cells (Supplementary Data File 6). H3K27ac modification on the chromatin has been well-defined in the enhancer and promoter regions and is usually accompanied by active transcription activities93–95. Similar to SMAD4 binding patterns, H3K27ac marks also showed distinct patterns between the normal and endometriosis groups following a 4-day EPC treatment (Fig. 4D, Supplementary Fig. 4A). We identified 1439 peaks that had increased enrichment in the normal group and 1122 peaks that had more enrichment in the endometriosis group (Supplementary Data File 6).
For the genes that preferentially have more H3K27ac peaks in the endometriosis group, Gene Ontology (GO) enrichment analysis indicated positive regulation of cell adhesion being the most enriched category (Supplementary Fig. 4B, Supplementary Data File 6). This includes genes such as vascular cell adhesion molecule 1 (VCAM1), CD44 molecule (CD44), and Wnt family member 5A (WNT5A) (Supplementary Data File 6). Higher levels of VCAM1 are found in ectopic endometriotic lesions and in the eutopic endometrium of individuals with endometriosis and may contribute to disease establishment and progression96. CD44 was previously shown to be elevated in the eutopic endometrium of patients with endometriosis and is involved in the attachment and invasion of endometrial cells into the peritoneum97,98. WNT5A controls endometrial mesenchymal stem cell renewal by activating WNT/β-catenin signaling99. Overall, these results corroborate previous studies indicating that the increased cell adhesion abilities in the eutopic endometrium of those with endometriosis facilitate lesion establishment at ectopic sites100 (Supplementary Fig. 4B, and Supplementary Data File 6).
GO enrichment on the genes that have less H3K27ac peaks in the endometriosis group indicated that categories involving transcription factor binding, extracellular matrix structural constituent and transcription corepressor activity were deficient during decidualization in the endometrium of individuals with endometriosis (Fig. 4E, Supplementary Data File 6). Additionally, genes in the SMAD binding category, such as SMAD3, SMAD6, the SMAD specific E3 ubiquitin protein ligase 2 (SMURF2), and the transforming growth factor beta receptor 1 (TGFBR1/ALK5), had fewer H3K27ac peaks in the endometrial stromal cells from individuals with endometriosis, corroborating our previous transcriptomic results in which a dysfunctional TGFβ/BMP signaling pathway was identified in the decidualizing stromal cells from individuals with endometriosis (Fig. 4E, Supplementary Data File 6). Additional defects in H3K27ac deposition in individuals with endometriosis were observed in the well-known progesterone-responsive genes RARB and CEBPA loci101,102 (Supplementary Fig. 4C). These results show that defective endometrial transcriptional responses driven by TGFβ and BMP signaling in individuals with endometriosis are detected at the chromatin level, as evidenced by different genome wide SMAD4 and H3K27ac binding patterns in normal versus endometriosis groups.
We also calculated the overlapping numbers of endometriosis-associated DEGs (determined from Day 4 EPC, FC > 1.4, < 0.4, FDR < 0.05), SMAD4, and H3K27Ac bound genes (Supplementary Fig. 4D, E). The genes are visualized as Venn diagrams and grouped by Up- and Down-regulated (Supplementary Fig. 4D) or as a Venn diagram without distinguishing between Up or Down-regulated genes (Supplementary Fig. 4E). Overall, we found that out of the 512 DEGs in the endometriosis dataset at Day 4 EPC, 90 (17.5%) also shared both a SMAD4 and H3K27Ac peak, while 15 (2.9%) shared only a SMAD4 peak, and 282 (55%) shared only an H3K27Ac peak (Supplementary Data File 6).
Silencing of SMAD1 and SMAD5 perturbs endometrial stromal cell decidualization
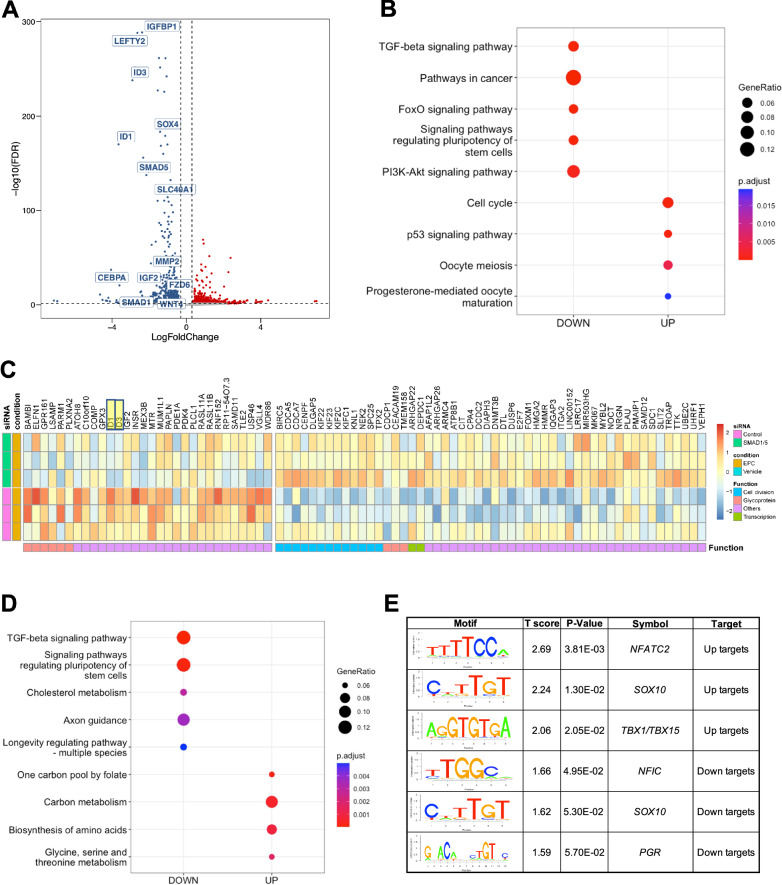
Previously published studies in mouse models indicate that the BMP/SMAD1/5 signaling pathways are critical for decidualization and endometrial receptivity77–80,85,86. In our present study, we found that the decreased decidualization potential of stromal cells from individuals with endometriosis correlated with defective BMP/SMAD1/5 activation. To functionally examine the role of BMP signaling pathway in mediating decidualization, we perturbed the SMAD1/5 complex using small interfering RNA (siRNA) in endometrial stromal cells from individuals without endometriosis and treated them with EPC to induce in vitro decidualization (Supplementary Fig. 5A). The knockdown effect was validated at the transcript and protein level (Fig. 5A, Supplementary Fig. 5B, Supplementary Data File 7). Upon the knockdown of SMAD1/5, we observed that canonical decidualization markers such as IGFBP1 and WNT4 were significantly downregulated (Fig. 5A). KEGG pathway enrichment on the differentially expressed genes revealed that the TGFβ and FOXO signaling pathways were also enriched within the downregulated group of genes (Fig. 5B). FOXO family plays a critical role in regulating progesterone-dependent differentiation and decidualization103 and is indispensable for implantation and decidua formation104. We highlighted several key genes changes in the heatmap format to visualize the effect of SMAD1/5 knockdown (Fig. 5C).
Fig. 5. Knockdown of SMAD1 and SMAD5 perturbs decidualization in endometrial stromal cells.
A Volcano plot showing the expression of differentially expressed genes in siCTL + EPC vs. siSMAD1/5 + EPC treated endometrial stromal cells (using a cutoff of Log 2 FC > 0.30, < −0.30, FDR < 0.05). Blue indicates genes that are down-regulated in siSMAD1/5 + EPC vs. siCTL + EPC, red indicates genes that are increased. (n = 1 individual without endometriosis). B Dot plot showing the enrichment of genes in key signaling pathways after SMAD1/5 knockdown. C Heatmap showing the expression and functional classification of key genes following SMAD1/5 knockdown + EPC versus siCTL + EPC treatment (n = 3 individuals without endometriosis). D The Binding and expression target analysis program was used to integrate SMAD4 binding peaks with the transcriptional changes after SMAD1/5 knockdown in EPC-treated endometrial stromal cells. Dotplot displays the gene ontology classification of genes that were activated by SMAD1/5 (i.e., were downregulated by SMAD1/5 and have a SMAD4 binding site). E Motif analysis was performed on the group genes identified to be SMAD1/5/4 direct targets and displayed as “uptargets” (genes that were increased after SMAD1/5 knockdown and had a SMAD4 peak) or as “downtargets” (genes that were downregulated after SMAD1/5 knockdown and had a SMAD4 peak).
To further map the direct target genes and potential co-factors of SMAD1/5 during decidualization, we used the Binding and expression target analysis program105 to consolidate our genomic profiling of SMAD4 and the transcriptomic profiling of SMAD1/5 perturbation. Among the direct targets that were activated by SMAD1/5 (which were down regulated upon SMAD1/5 perturbation and were bound by SMAD4, labeled as Down-targets), were the TGFβ signaling pathway and pathways regulating the pluripotency of stem cells (Fig. 5D). We also performed motif analysis on the direct target genes to provide mechanistic insight to the SMAD1/5 mediated gene expression during decidualization. We uncovered potential SMAD1/5 co-repressors such as NFATC2 and T-box family (TBX1/TBX15). NFATC2 is involved in cGMP-PKG signaling pathways and has a role in regulating immune, inflammatory responses106, it is also reported to be elevated in the thin-endometrium patients who usually have deficient implantation and lower pregnancy rate107. Acting mainly as repressors, TBX family genes are crucial for embryonic development and tissue differentiation and formation108. A recent study has shown that TBX15 was elevated in patients with adenomyosis109. As for transcriptional co-activators, apart from the canonical pan-tissue co-activator NFIC110, the PR motif was enriched in the SMAD1/5 direct target genes, confirming our previous finding that SMAD1/5 may regulate progesterone-responsive genes at the transcriptional level (Fig. 5E).
We also identified two genes, MALAT1 and HDAC4, that contained a SMAD4 binding site and were decreased by SMAD1/5 siRNA knockdown in EPC-treated stromal cells, suggesting that they are direct target genes that are activated by BMP/SMAD1/5/4. The direct SMAD4 binding activities in MALAT1 and HDAC4 loci were visualized as genome track views in Supplementary Fig. 5C, D. MALAT1 and HDAC4 are both involved in facilitating decidualization and in the pathogenesis of endometriosis111–116. In summary, our studies combine datasets from SMAD1/5 siRNA-mediated knockdowns with SMAD4 binding studies in endometrial stromal cells during decidualization. The results from these not only validated the indispensable roles of SMAD1/5 during human decidualization, but also provided additional layers of regulation in the downstream networks of SMAD1/5 mediated BMP signaling pathways.
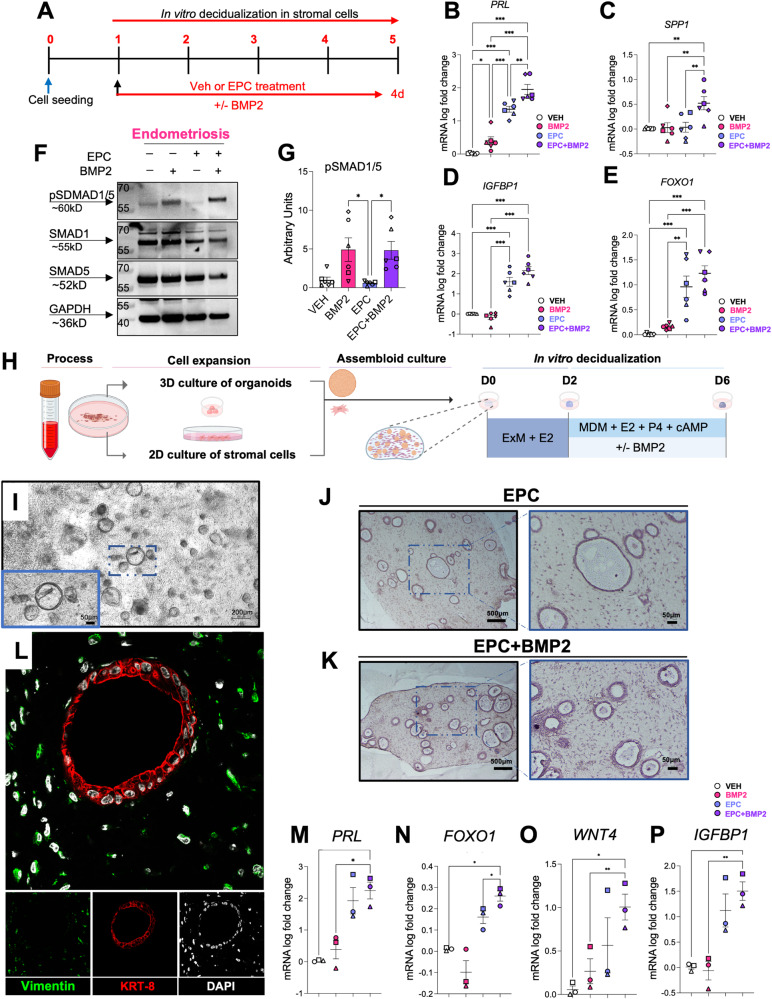
BMP2 supplementation enhances the decidualization potential in stromal cells and endometrial assembloids of individuals with endometriosis
We consistently observed alterations in the BMP/SMAD1/5/4 signaling pathway in the decidualizing stromal cells from individuals with endometriosis, suggesting that inherent defects in the activation of this pathway were present in the affected individuals. We also identified that BMP/SMAD1/5/4 signaling networks are essential for decidualization in the normal eutopic endometrium. To test whether the addition of recombinant BMP2 supplementation could restore the decidual response in the endometrium from individuals with endometriosis, we added BMP2 to endometrial stromal cell cultures and to 3-dimensional endometrial stromal/epithelial co-cultures, or “assembloids” (Fig. 6). For the stromal cell experiments, cells derived from the eutopic endometrium of patients with endometriosis were treated as shown in Fig. 6A with the EPC cocktail or EPC + BMP2 for a total of 4 days. The extent of decidualization was examined using RT-qPCR analysis of the decidual markers, PRL, SPP1, IGFBP1, and FOXO1 (Fig. 6B–E). IGFBP1 and FOXO1 showed an increased trend in expression following EPC + BMP2 treatment versus EPC treatment alone. However, only the expression of PRL and SPP1 changed significantly after BMP2 supplementation (Fig. 6B–E). Correspondingly, we observed that the combined addition of EPC + BMP2 synergized the expression of pSMAD1/5 relative to EPC treatment alone (Fig. 6F, G).
Fig. 6. BMP2 supplementation improves the decidualization potential of 2D and 3D endometriosis patient-derived endometrial cultures.
A Experimental outline showing the treatment groups used to test how the addition of recombinant BMP2 affects decidualization in EPC-treated stromal cells from individuals with endometriosis. B–E qRT-PCR quantification of decidualization markers PRL (B), SPP1 (C), IGFBP1 (D), and FOXO1 (E) following Vehicle, BMP2, EPC, or EPC + BMP2 treatment in stromal cells from individuals with endometriosis (n = 6). The different symbols represent individual patient trajectories per sample, plotted as mean +/− standard error of the mean. One-way ANOVA with a Tukey’s postdoc test. F, G Western blot analysis (F) and quantification (G) of endometrial stromal cells from individuals with endometriosis following 4 days of treatment with Vehicle, BMP2, EPC, or EPC + BMP2. H Diagram showing the experimental procedure for establishing endometrial epithelial and stromal co-cultures or “assembloids” from endometrial tissues of individuals with endometriosis. After the assembloids were established, they were pre-treated with 10 nM estradiol (E2) followed by decidualization with the EPC decidualization cocktail (1 µM MPA, 0.5 mM cAMP and 1 µM E2) +/− 25 ng/ml BMP2 for an additional 4 days. Image was created using BioRender. I Phase contrast micrograph of the endometrial epithelial and stromal assembloids showing the endometrial epithelial organoids and the distribution of stromal cells in the collagen matrix. J–L Histological analysis of cross sections obtained from the endometrial assembloids stained with hematoxylin and eosin (J, K) or using immunofluorescence using vimentin (green), cytokeratin 8 (KRT-8, red) or DAPI (white) (L). M–P qRT-PCR analysis of decidualization markers, PRL (M), FOXO1 (N), WNT4 (O), or IGFBP1 (P) in the endometrial assembloids treated with Vehicle, BMP2, EPC, or EPC + BMP2. Plotted values represent mean +/− standard error of the mean, with the different symbols corresponding to each patient’s trajectory. Data were analyzed using a one-way ANOVA with a Tukey’s posthoc test.
To test the impact of BMP2 supplementation on the decidualization potential of endometrial stromal and epithelial assembloids we generated co-cultures as previously described using the strategy outlined in Figure 6H117. Individual cultures of endometrial stromal cells and epithelial organoids were established. Four days after initial establishment, the co-cultures were created by encapsulating stromal cells and epithelial organoids in the collagen matrix cultured in expansion medium supplement with E2 for 2 days. The culturing medium was then switched to a minimal decidualization media containing the decidualization cocktail (EPC) +/− BMP2 for an additional 4 days. Live assembloid cultures were visualized using phase microscopy (Fig. 6I) and using histology or fluorescence microscopy after fixation and staining (Fig. 6J–L). RT-qPCR analysis of the treated assembloids showed that the BMP2 + EPC supplementation significantly increased FOXO1 expression and caused an increased trend in the expression of decidual markers PRL, WNT4, IGFBP1, PAEP and SPP1 relative to EPC treatment alone (Fig. 6M–P and Supplementary Fig. 6B, C). We also observed fewer FOXJ1-positive ciliated cells in the endometrial assembloids following EPC + BMP2 treatment, compared with EPC treatment alone (Supplementary Fig. 6A). These results confirm that BMP2 supplementation increases decidual gene expression in endometrial stromal or in 3D assembloid cultures from individuals with endometriosis.
Discussion
Our study, which performs a time course analysis of decidualization in stromal cells from individuals with and without endometriosis, reveals that dysregulated TGFβ and BMP signaling is prevalent in the endometrium of individuals with endometriosis and may underlie the fertility defects experienced by this group. As such, our results present transcriptomic evidence supporting the hypothesis that patients with endometriosis display abnormal decidualization programs that can partially explain the elevated infertility rates within that population. Previous studies analyzed the time-course gene expression profiles of in vitro decidualized normal endometrial stromal cells37,38, while others have analyzed the expression differences between normal and endometriosis stromal cells in the late decidualization phase39. Our data, on the other hand, present a comprehensive transcriptomic analysis of the decidualization profiles of stromal cells derived from individuals without and with endometriosis during early and late phases. We first performed a time-course transcriptomic analysis of the datasets to identify the genes that are expressed within each group as they undergo in vitro decidualization and identified that stromal cells from patients with endometriosis displayed gene expression signatures that were controlled by NFE2L2, a marker of oxidative stress, and SMAD4, the effector of TGFβ and BMP signaling. In the second analysis of the datasets, we directly compared the transcriptomes of stromal cells from individuals without endometriosis to those from individuals with endometriosis as they underwent in vitro decidualization. From these studies, we found that TGFβ/BMP signaling pathways emerged once again as a consistently enriched pathway during each decidualization time point. Hence, while we highlight several signaling pathways that are differentially expressed between the two groups during decidualization, we focused on characterizing the TGFβ/BMP signaling differences in the endometrium of individuals with and without endometriosis.
We correlated the expression of DEGs from our time course analysis of decidualization with the top 50 genes indicating the key branching points between a decidual and non-decidual cells from the study by Lucas ES et al.76 With this correlation we found that cells from endometriosis donors displayed higher expression signatures associated with immune surveillance (TIMP3, CXCL14), cellular stress (CRYAB, GLRX, HSD11B1), increased iron storage (FTL, SCARA5), and partial alignment with genes characteristic of decidual senescence (ADAMTS5, ABI3BP, CEMPI and COL14A1). One limitation is that our analysis represents bulk RNAseq of stromal cells, while the study by Lucas ES et al., represents sensitive single cell RNAseq analyses. Hence, future analysis of decidualization between normal and endometriosis stromal cells could focus on using more sensitive sequencing platforms to obtain relevant information.
To identify the regulatory factors that could be driving the different transcriptional responses between the endometrial stromal cells from individuals with or without endometriosis, we explored consensus gene targets in the ENCODE and ChEA Transcription Factor Targets datasets49,50. This analysis indicated that CEBP/β is a major transcription factor controlling the transcriptional response to decidualization in the normal endometrium, controlling genes such as FBXO32, YARS, and MMP19. CEBP/β has also been shown to be a master regulator of human endometrial cell decidualization, which controls the expression of PGR by directly binding to its promoter51,52. Analysis of endometrial stromal cells from individuals with endometriosis identified NFE2L2 and SMAD4 as the top two transcription factors controlling gene expression during decidualization. NFE2L2 is a central factor controlling the intracellular response to stress and was previously shown to be activated in the endometrial epithelial cells of cows exposed to heat stress118. NFE2L2 (also known as NRF2) controls the expression of antioxidant genes in the cell by binding to DNA antioxidant response elements (or “AREs”)119. One class of genes controlled by NFE2L2 are the glutathione peroxidase genes (i.e., GPX3 and GPX4), which play key roles in the control of cellular oxidative stress damage60. Hence, our data supports theories regarding the altered response to oxidative stress in the endometrium of individuals with endometriosis as a possible leading cause for impaired decidualization120. Others have also suggested that impaired response to oxidative stress through defective iron metabolism is an underlying factor in women with recurrent pregnancy loss121.
The ENCODE and ChEA Transcription Factor gene target analysis also identified SMAD4 as a major regulatory factor controlling transcription in endometriosis. The TGFβ signaling pathway was also notably altered in the endometrium of individuals with endometriosis when we directly compared the genes that were differentially regulated between normal and endometriosis groups at each time point during decidualization (Fig. 2E). SMAD4 is the common SMAD that can transmit BMP signaling (via SMAD1/5) or activin/TGFβ signaling62. Our previous studies, which show that BMP/SMAD1/5 signaling and TGFβ/SMAD2/3 signaling are critical for decidualization and fertility, are in line with these results78–80,122–124. We focused on the roles of BMP/SMAD1/5 signaling given that we observed altered expression of BMP ligands (BMP4, BMP6) as well as decreased expression of canonical SMAD1/SMAD5 targets in the decidualizing stromal cells from individuals with endometriosis. The canonical SMAD1/5 target genes, ID2 and ID3, were significantly decreased during days 4 and 6 of EPC treatment in the endometrial stromal cells derived from individuals with endometriosis relative to those without. GREMLIN2, which is a secreted antagonist of the BMPs was increased in the endometrial stromal cells from individuals with endometriosis on Day 0. The expression of FST was decreased in the endometriosis group after 2, 4, 6, and 8 days of EPC treatment. Thus, using gene ontology analysis and upstream regulatory factor analyses, we concluded that the transcriptional control by BMP/SMAD signaling was a key pathway controlling decidualization the endometrium of individuals without endometriosis that was perturbed in individuals with endometriosis. However, this does not exclude potential defects in the activin/TGFβ/SMAD2/3 signaling axis in these patients.
To further characterize the genome-wide distribution of the downstream effectors of the BMPs, we used CUT&RUN to detect SMAD4 binding events in stromal cells from individuals with and without endometriosis after EPC treatment. To detect the chromatin-level changes between the two cohorts, we also mapped H3K27ac marks in the endometrial stromal cells from the normal and endometriosis groups. The binding studies showed that there were notable changes in the distribution of both SMAD4 and H3K27ac between the endometrial stromal cells of individuals with and without endometriosis, suggesting that the gene expression changes were a result of altered transcription factor binding events. This was further confirmed by intersecting the SMAD4 binding events with differentially expressed genes following SMAD1/SMAD5 siRNA-mediated knockdown in endometrial stromal cells treated with EPC to induce in vitro decidualization. We first identified that the double knockdown of SMAD1 and SMAD5 blunted the decidualization capacity of endometrial stromal cells, as evidenced by the decrease of the canonical decidualization markers, IGFBP1 and WNT4. Merging of the SMAD4 binding peaks and downregulated genes after SMAD1/5 knockdown showed enrichment of genes with consensus sequences related to transcription by NFIX, SOX10, and PR. Progesterone receptor is the master regulator of decidualization125,126, suggesting that impaired BMP/SMAD1/5 signaling perturbs transcriptional activation of PR, blunting endometrial cell reprogramming. Furthermore, we identified direct SMAD4 binding sites on the genes of the MALAT1 and HDAC4 genes, which are critical for endometrial stromal cell decidualization111–116. Our results show molecular evidence that impaired BMP/SMAD signaling underlies the decidualization defects in the endometrium of individuals with endometriosis.
To verify the findings that an impaired BMP/SMAD1/5 signaling pathway was driving decidualization defects in endometriosis, we tested whether the addition of recombinant human BMP2 to decidualizing cultures of endometrium could increase endometrial decidualization markers in individuals with endometriosis. Previous studies have shown that ectopic expression of BMP2 in endometrial stromal cells could potentiate decidualization in the normal endometrium86. We used both 2D endometrial stromal cells as well as 3D epithelial/stromal cocultures or “assembloids” to recapitulate paracrine signaling events between the two cell types. We found that relative to EPC treatment alone, the addition of BMP2 + EPC increased the expression of canonical decidual genes in both the stromal cell and assembloid cultures of endometrium from individuals with endometriosis. Our findings indicate that BMP2 and the downstream activated signaling pathways are defective in the endometrium of patients with endometriosis and that BMP2 supplementation may correct the defect. Several compounds have been developed to modulate BMP signaling pathway; for example, the chemical inhibitor LDN-193189 inhibits BMP signaling by blocking the ALK1/ALK2/ALK3/ALK6 BMP type 1 receptors127. Chemical activators of the BMP signaling have been identified using high throughput assay screens in reporter cell lines, however their specificity for BMP receptor activation remains to be determined128. Another emerging platform for activation of the BMP signaling pathway includes the use of small BMP peptide mimetics, which can potently and specifically promote BMP signaling cascades129. Hence, activation of BMP signaling with pharmacological approaches could be a feasible therapeutic option.
BMPs are subgroups of the TGFβ ligand family and BMP signaling pathways are indispensable in the female reproductive tract, especially during early pregnancy establishment62,124. Upon binding of BMP ligands, the serine-threonine kinase receptors (ALK1/ALK2/ALK3/ALK6 and BMPR2/ACVR2A/ACVR2B) will subsequently phosphorylate the signal transducers, SMAD1 and SMAD5 and phosphorylated SMAD1/5 will then form homodimers and translocate into the nucleus together with a common SMAD4 protein to initiate transcriptional programming62. BMP signaling pathways are key in transforming the maternal endometrium into a receptive environment for further support embryo implantation. From the uterine-specific knockout mouse models, BMP ligands77,79, kinase receptors, and SMAD signal transducers51,78,80,130,131 are essential in decidualization and implantation, which are prerequisites for the establishment of a healthy pregnancy. Apart from regulating the decidualization and implantation process, BMP signaling pathways are also involved in immunomodulation in the endometrium. Conditional deletion of Bmpr2 in the mouse uterus diminishes the uterine natural killer cell populations, which regulate the immune response in the endometrium, preventing the rejection of the embryo as a foreign entity. Such an immune-privileged microenvironment is crucial in the early stages of pregnancy131.
Indeed, the essential roles that BMP signaling pathways play in cell differentiation, proliferation, and anti-inflammation potentiates its significance in the context of endometriosis. Interestingly, BMP2 levels were decreased in the peritoneal fluid of women with endometriosis132. Recent large-scale genome-wide association studies (GWAS) also identified BMPR2 as one of the endometriosis risk loci92. In women with recurrent implantation loss, BMP7 was identified to harbor a deleterious mutation that was predicted to be disease-causing133. Our studies highlight that the BMP signaling pathway is abnormal in the endometrium of individuals with endometriosis and may underlie the fertility defects in that population of patients.
Using transcriptomic and genome-wide binding analyses in patient-derived 2D and 3D-endometrial cultures, we show that abnormal BMP signaling pathways affect fertility in individuals with endometriosis by directly affecting the decidualization process of the endometrium. Because our samples represent primary patient-derived material, some of our analyses showed a wide range in their response to the decidualization treatment. These differences could be attributed to inherent patient-to-patient variability as well as to the clinical history of the patient. Despite this variability across patients, our findings presented here corroborate previous studies that noted the abnormal endometrial response to hormones in individuals with endometriosis31–33. However, they also reveal alterations in additional pathways, such as the BMP/SMAD signaling pathways, oxidative stress responses, and retinoic acid signaling pathways, opening potential avenues for the development of biomarkers or therapeutics for endometriosis-associated infertility.
Methods
Ethics statement and endometrial sample collection
All patient specimens were collected following informed patient consent approved under protocol H-21138 and through the Human Tissue and Pathology Core at Baylor College of Medicine, following guidelines approved by the Institutional Review Board at Baylor College of Medicine. All ethical regulations relevant to human research participants were followed. Samples are maintained using de-identified codes to preserve confidentiality. Endometrial samples were obtained from women with confirmed endometriosis (n = 7, mean age, 36.7 + /− 6.9) or from women without endometriosis (n = 7, mean age, 38.4 + /− 5.3) undergoing endometrial biopsies or hysterectomies. Samples categorized in the normal group were free of endometriosis, according to pathology examination reports.
Establishment and decidualization of primary endometrial stromal cells
Primary endometrial stromal cells were isolated from surgically resected endometrial biopsies, which were immediately placed in stromal culturing media, DMEM/F12 (Gibco #11330032) supplemented with 10% FBS, 1% Antibiotic-Antimycotic (Gibco #15240062), and 100 µg/mL of Primocin (InvivoGen, Cat # MSPP-ANTPM2). Endometrial biopsies were cut into small pieces, digested in Hanks’ Balanced Salt Solution (HBSS) containing 5 mg/mL of collagenase (Sigma, #C0130-1G) and 0.2 mg/mL of DNase I (Sigma, Cat #DN25-100MG), and then incubated at 37 °C for 20 min on an orbital shaker at 120 rpm. After incubation, the digested tissues were spun down, and the pellets were resuspended in stromal culturing media. The cell suspension was passed through 100 µm cell strainers and then 20 µm cell strainers. The cell fraction from the flowthrough after the 20 µm cell strainers contains the stromal cells and was cultured in stromal culturing media. Stromal cells were passaged once they reached 90% confluency. For decidualization, stromal cells were seeded on 12-well plates at 2 × 105 cells/well and 10 cm dishes at 1 × 106 cells/dish and treated with phenol red-free DMEM/F12 (Gibco #11039021) supplemented with 2% charcoal-stripped FBS and EPC cocktail (1 µM MPA, Sigma Cat#1378001-200MG, 0.05 mM cAMP, Axxora Cat #JBS-NU-1502-50, and 35 nM E2, Sigma Cat #E1024-1G).
Establishment and decidualization of endometrial assembloids
Establishment of endometrial assembloids was performed according to a published protocol117,134 with minor modifications. In brief, primary endometrial stromal cells and glandular epithelial organoids were established from human endometrial samples. After culturing epithelial organoids and stromal cells separately for two passages, the two were mixed gently at a ratio of 1:2 (v/v) and resuspended in 20 times ice-cold Collagen (Sigma, Cat # C0130-1G). Cells were then aliquoted in 20 µl volumes into a 48-well plate and allowed to polymerize at 37 °C for 45 min, after which the collagen assembloid droplets were overlayed with 500 µl of Expansion Medium and maintained in a 37 °C cell culture incubator. The collagen droplets were maintained under constant shaking at 90 rpm for 48 h. (Expansion Medium consists of: Advanced DMEM/F12 (Invitrogen, Cat #12634010), supplemented with 1X N2 supplement (Invitrogen, Cat # 17502048), 1X B27 supplement (Invitrogen, Cat # 12587010), 100 μg/ml Primocin (Invivogen, Cat # MSPP-ANTPM2), 2 mM L-glutamine (Invitrogen, Cat # 25030-024), 500 nM A83-01 (Sigma, Cat #2939), 10% WNT3a, 10% R-Spondin conditioned media, 10 mM Nicotinamide (Sigma, Cat # N0636-100G), 1.25 mM N-acetyl-L-cysteine (Sigma, Cat # A9165-5G), 10% Noggin conditioned media, 100 ng/ml FGF10 (Peprotech, Cat # 100-26), 50 ng/ml HGF (Peprotech, Cat #100-39), 50 ng/ml EGF (Peprotech, Cat # AF-100-15) and 10 nM E2 (Sigma, Cat. #E1024-1G). Conditioned media was produced in HEK293 cells and obtained from the Center for Digestive Diseases and Organoid Core Facility at Baylor College of Medicine. To induce decidualization of the assembloids, the culturing media was changed to decidualization media in minimal differentiation media (MDM) (Advanced DMEM/F12 supplemented with 1X N2 supplement, 1X B27 supplement, 100 μg/ml Primocin, 2 mM L-glutamine, 1.25 mM N-acetyl-L-cysteine, 1 µM MPA, 0.5 mM cAMP, and 1 µM E2) supplemented with or without rhBMP2 (R&D, Cat #355-BM-010/CF) at 25 ng/ml. Media was refreshed every 48 h.
Histological assessment of endometrial assembloids
Assembloids were fixed in 4% PFA at room temperature for 15 min and then immobilized in the Histogel (Thermo Fisher, Cat #22-110-678). After processing the assembloids in Histogel, assembloid blocks were dehydrated through a series of ethanol washes and processed for paraffin embedding at the Human Tissue Acquisition and Pathology Core at Baylor College of Medicine. Paraffin blocks were sectioned using 5 µm thick sections. Assembloid sections were deparaffinized in Histoclear and rehydrated in a series of 100%, 95%, 80%, and 70% ethanol washes, followed by washing in dH2O. For identifying the morphological structures, assembloid sections were sectioned and stained with hematoxylin and eosin. For immunofluorescence staining, assembloid sections were heated in boiling 10 mM sodium citrate, pH 6.0 for 20 min for antigen retrieval and quenched in 3% hydrogen peroxide for 10 min. After blocking with 3% BSA for 1 h, assembloid sections were incubated with primary and fluorescent secondary antibodies according to the manufacturer’s instructions and nuclei were stained with 1 mg/ml DAPI (1:100- dilution, ThermoFisher, Cat # D1306). The stained slides were mounted in VECTASHIELD antifade mounting medium (Vector Laboratories #H-1000-10). Fluorescence images were taken on a Zeiss LSM780 confocal microscope at the Optical and Vital Microscopy Core at Baylor College of Medicine.
RNA extraction and quantitative PCR from endometrial stromal cells and endometrial assembloids
The RNAs of endometrial stromal cells were extracted by using QIAGEN RNeasy micro kit (QIAGEN, Cat #74004) according to the manufacturer’s instruction. The assembloids were lysed in Trizol reagent (Life Tech, Cat #10296010) and the RNAs were extracted by using Direct-zol RNA microprep kit (Zymo Research, Cat #R2062). A total of 50–200 ng of RNA from each sample was transcribed into cDNA by using qScript cDNA supermix (Quantabio, Cat #95048-100). Real time quantitative PCR was performed on Bio-Rad CFX384 Touch Real-Time PCR Detection System. Fold changes of target genes were calculated using delta Ct method and normalized GAPDH135. Primer sequences are listed in Supplementary Table 1.
Protein extraction and western blotting
Cells were washed with ice-cold 1×DPBS and lysed in M-PER mammalian protein extraction reagent (ThermoFisher, Prod#78505) supplement with protease inhibitor cocktail (ThermoFisher, Cat #78437) and phosphatase inhibitor cocktail (ThermoFisher, Cat #78426). Protein concentrations were quantified by using Pierce BCA protein assay kit (ThermoFisher, Cat #23225). A total of 20 µg of protein lysate was loaded onto 4–12% Bis-Tris Plus Mini protein gels (ThermoFisher, Cat # NW04122BOX) and transferred onto nitrocellulose membranes (Bio-Rad, Cat #1704270). The membranes were blocked with 5% non-fat milk in TBST buffer for an hour at room temperature and then incubated with primary antibodies at 4 °C overnight. Antibody information is listed in Supplementary Table 2. The next day, the membranes were probed with HRP-conjugated secondary antibodies (Jackson ImmunoResearch) for two hours at room temperature and protein bands were visualized by using SuperSignal West chemiluminescent substrate (Pierce) on Bio-Rad Chemidoc Touch Imaging system. Protein bands were quantified by using Image Lab software (Bio-Rad). All the uncropped blots are included in Supplementary Figs. 7–9.
Statistics and reproducibility
All experiments were performed using > 3 biological replicates using technical triplicates in each experiment. Data in graphs are presented as mean +/− standard error of the mean, or as described in each of the figure legends. Statistical tests were performed using t-tests or one-way ANOVA tests with multiple comparison post-tests, as indicated in the figure legend for each experiment. Multiple testing for the large datasets was performed using cut-offs and FDR < 0.05. GraphPad Prism was used for statistical analyses, *, 0.033; **, 0.002; ***, <0.001
Gene expression profiling using RNA sequencing
All sequencing data are available in the NCBI Gene Expression Ominibus under SuperSeries GSE243158.
Time course EPC studies
Endometrial stromal cells from 4 normal and 4 endometriosis samples were treated with 35 nM estradiol, 1 µM medroxyprogesterone acetate and 50 µM 8-Br-cyclic AMP for 0, 2, 4, 6, or 8 days. RNA expression profiles were obtained at each timepoint using RNA sequencing analyses (20–30 million paired-end reads using NovaSeq System from Novogene Corporation Inc. Reads were trimmed with fastp v0.23.2 and aligned using STAR 2.7.10a to human genome assembly GRCh38.p13. Differentially expressed genes between normal patients and endometriosis EPC-treated cells were obtained by comparing to the baseline samples (Day 0). Significantly changed genes during the time course treatment were obtained using an ANOVA F-test using an FDR < 0.05 from patients without (n = 3) and with endometriosis (n = 4). All DEGs are presented in Supplementary Data File 1. EnrichR136–138 was used to identify the gene ontology classifications (Supplementary Data File 2), as well as ENCODE and ChEA consensus transcription factors known to regulate differentially expressed genes in the normal and endometriosis EPC-treated stromal cells (Supplementary Data File 3). Differentially expressed genes between normal and endometriosis stromal cells were obtained by comparing transcripts at each time point of treatment. Differentially expressed genes between normal (n = 4) and endometriosis (n = 3) were identified using a Wald test with cutoff values of fold-change > 2 or < 1/2 and FDR < 0.05 (Supplementary Data File 4). Gene and pathway enrichment analysis was conducted using R package Cluster Profiler139.
SMAD1/5 siRNA studies
Endometrial stromal cells from 3 individuals without endometriosis were treated with either 80 nM negative control (siCTL, Horizon Cat #D-001810-10-20) or 40 nM of SMAD1 plus 40 nM of SMAD5 (siSMAD1/5, Horizon Cat # L-012723-00-0005 & L-015791-00-0005) siRNA followed by 4 days’ EPC treatment. Cells were transfected using Lipofectamine RNAiMAX (LifeTechnologies, Cat #13778500). RNAs were isolated by using QIAGEN RNeasy micro kit and subjected to RNA sequencing analysis to identify differentially regulated transcripts. Samples were normalized through effective library sizes and DESeq2 was used identify differentially expressed genes between the siCTL and siSMAD1/5 EPC-treated cells using an FDR < 0.05 (Supplementary Data File 7). Gene and pathway enrichment analysis was conducted using R package Cluster Profiler139.
SMAD4 and H3K27 genome-wide binding studies using CUT & RUN
CUT&RUN experiments were performed according to a protocol by Skene and Henikoff140. After endometrial stromal cells were treated with EPC for 4 days, they were collected by digesting with 0.25% Trypsin (ThermoFisher, Cat #25200056) for 3 min. After the digestion, cells were pelleted down at 300 × g for 3 min and viably frozen down in the freezing medium (90% FBS with 10% DMSO) until experiment day. On the day of the experiment, cell vials were quickly thawed and washed 3 times with washing buffer (20 mM HEPES pH 7.5, 150 mM NaCl, 0.5 mM Spermidine, 1 X Protease Inhibitor). For each reaction, 1.3 × 106 cells were used for the subsequent Concanavalin A bead binding step. After 10 min incubation with Concanavalin A beads, bead-cell complexes were resuspended in 100 μl antibody buffer (washing buffer supplemented with 0.01% digitonin, and 2 mM EDTA) per reaction. 1 μl of IgG antibody (Sigma, Cat #I5006), H3K27ac (Cell Signaling, Cat #8173) and SMAD4 antibody (Abcam, Cat #ab40759) were added to each reaction respectively. After overnight incubation at 4 °C, bead-cell complexes were washed twice with 200 μl cold dig-washing buffer (washing buffer supplemented with 0.01% digitonin) and resuspended in 50 μl cold dig-washing buffer with 1 μl pAG-MNase (EpiCypher, Cat #15-1016). After incubation at room temperature for 10 min, bead-cell complexes were washed twice with 200 μl cold dig-washing buffer and resuspended in 50 μl cold dig-washing buffer, then 1 μl 100 mM CaCl2 was added to each reaction. The mixture was incubated at 4 °C for 2 h and the reaction was stopped by adding 50 μl stop buffer (340 mM NaCl, 20 mM EDTA, 4 mM EGTA, 0.05% Digitonin, 100 ug/mL RNase A, 50 mg/mL glycogen, 0.5 ng E. coli DNA Spike-in (EpiCypher, Cat #18–1401) and incubated at 37 °C for 10 min. The supernatant was collected and subjected to DNA purification with phenol-chloroform and ethanol precipitation. Sequencing libraries were prepared using NEBNext Ultra II DNA Library Prep Kit (New England BioLabs, Cat #E7645) following manufacture’s protocol. Paired-end 150 bp sequencing was performed on a NEXTSeq550 (Illumina) platform and each sample was targeted for 10 million reads.
Sequencing raw data were de-multiplexed by bcl2fastq v2.20 with fastqc for quality control and then mapped to reference genome hg19 by Bowtie2, with parameters of -end-to-end -very-sensitive -no-mixed -no-discordant -phred33 -I 10 -X 700. For Spike-in mapping, reads were mapped to E. coli genome U00096.3. Spike-in normalization was achieved through multiply primary genome coverage by scale factor (100000 / fragments mapped to E. coli genome). CUT&RUN peaks were called by Model-based Analysis of ChIP-Seq (MACS/2.0.10)141 with the parameters of -f BAMPE -g 1.87e9 -q 0.05 (H3K27ac) or -q 0.1 (SMAD4). Track visualization was done by bedGraphToBigWig, bigwig files were imported to Integrative Genomics Viewer for visualization. For peak annotation, genomic coordinates were annotated by ChIPseeker142. Differential binding analysis and clustering were conducted using DiffBind143. Direct targets motif analysis was conducted through Binding and Expression Target Analysis (BETA)105 with parameter BETA plus –p –e –k LIM –g hg19 -gs hg19.fa -bl. Gene and pathway enrichment analysis was conducted using R package Cluster Profiler139. Annotated peak files were included in Supplementary Data File 5 (SMAD4) and Supplementary Data File 6 (H3K27ac).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
We are grateful to Dr. Martin M. Matzuk (M.M.M) for support and guidance on this project. Studies were supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development grants R00-HD096057 (D.M.), R01-HD105800 (D.M.), R01-HD032067 (M.M.M.) and R01-HD110038 (M.M.M). Diana Monsivais, Ph.D. holds a Next Gen Pregnancy Award (NGP10125) from the Burroughs Wellcome Fund.
Author contributions
Study conception and design: Z.L., S.T., P.J., T.G., D.M. Performed experiment or data collection: Z.L., S.T., P.J., T.G., T.N.D, J.G., D.I.C., L.A.R., X.G., D.M. Computation and statistical analysis: Z.L., S.T., P.J., T.G., D.I.C., D.M. Data interpretation and analysis: Z.L., S.T., P.J., T.G., D.I.C., D.M. Writing, reviewing, and editing: All. Supervision: D.M.
Peer review
Peer review information
Communications Biology thanks Rong Li and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Frank Avila and Manuel Breuer.
Data availability
Sequencing data are available in the NCBI Gene Expression Ominibus under SuperSeries GSE243158. All source data for figures in this study are provided in the supplementary data files. All source data for figures in this study are provided in Supplementary Data file 8. Uncropped blots are included in Supplementary Figs. 7–9.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Zian Liao, Suni Tang.
Supplementary information
The online version contains supplementary material available at 10.1038/s42003-024-05898-z.
References
- 1.Ellis K, Munro D, Clarke J. Endometriosis Is Undervalued: A Call to Action. Front Glob. Women’s Health. 2022;3:902371. doi: 10.3389/fgwh.2022.902371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bulun SE, et al. Endometriosis. Endocr. Rev. 2019;40:1048–1079. doi: 10.1210/er.2018-00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zondervan KT, Becker CM, Missmer SA. Endometriosis. N. Engl. J. Med. 2020;382:1244–1256. doi: 10.1056/NEJMra1810764. [DOI] [PubMed] [Google Scholar]
- 4.Davis AC, Goldberg JM. Extrapelvic Endometriosis. Semin. Reprod. Med. 2017;35:98–101. doi: 10.1055/s-0036-1597122. [DOI] [PubMed] [Google Scholar]
- 5.Sampson J. Heterotopic or misplaced endometrial tissue. Am. J. Obstet. Gynecol. 1925;10:649–664. doi: 10.1016/S0002-9378(25)90629-1. [DOI] [Google Scholar]
- 6.Sasson IE, Taylor HS. Stem cells and the pathogenesis of endometriosis. Ann. N. Y Acad. Sci. 2008;1127:106–115. doi: 10.1196/annals.1434.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Longo LD. Classic pages in obstetrics and gynecology. Aberrant portions of the mullerian duct found in an ovary: William Wood Russell Johns Hopkins Hospital Bulletin, vol. 10, pp. 8–10, 1899. Am. J. Obstet. Gynecol. 1979;134:225–226. [PubMed] [Google Scholar]
- 8.Gruenwald P. Origin of endometriosis from the mesenchyme of the celomic walls. Am. J. Obstet. Gynecol. 1942;44:470–474. doi: 10.1016/S0002-9378(42)90484-8. [DOI] [Google Scholar]
- 9.Arnold J, et al. Imbalance between sympathetic and sensory innervation in peritoneal endometriosis. Brain Behav. Immun. 2012;26:132–141. doi: 10.1016/j.bbi.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 10.Anaf V, et al. Relationship between endometriotic foci and nerves in rectovaginal endometriotic nodules. Hum. Reprod. 2000;15:1744–1750. doi: 10.1093/humrep/15.8.1744. [DOI] [PubMed] [Google Scholar]
- 11.McKinnon BD, Bertschi D, Bersinger NA, Mueller MD. Inflammation and nerve fiber interaction in endometriotic pain. Trends Endocrinol. Metab. 2015;26:1–10. doi: 10.1016/j.tem.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Vercellini P, Vigano P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat. Rev. Endocrinol. 2014;10:261–275. doi: 10.1038/nrendo.2013.255. [DOI] [PubMed] [Google Scholar]
- 13.Gupta S, et al. Pathogenic mechanisms in endometriosis-associated infertility. Fertil. Steril. 2008;90:247–257. doi: 10.1016/j.fertnstert.2008.02.093. [DOI] [PubMed] [Google Scholar]
- 14.Holoch KJ, Lessey BA. Endometriosis and infertility. Clin. Obstet. Gynecol. 2010;53:429–438. doi: 10.1097/GRF.0b013e3181db7d71. [DOI] [PubMed] [Google Scholar]
- 15.Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364:1789–1799. doi: 10.1016/S0140-6736(04)17403-5. [DOI] [PubMed] [Google Scholar]
- 16.Macer ML, Taylor HS. Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet. Gynecol. Clin. North Am. 2012;39:535–549. doi: 10.1016/j.ogc.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prescott J, et al. A prospective cohort study of endometriosis and subsequent risk of infertility. Hum. Reprod. 2016;31:1475–1482. doi: 10.1093/humrep/dew085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith S, Pfeifer SM, Collins JA. Diagnosis and management of female infertility. JAMA. 2003;290:1767–1770. doi: 10.1001/jama.290.13.1767. [DOI] [PubMed] [Google Scholar]
- 19.Tanahatoe SJ, Hompes PG, Lambalk CB. Investigation of the infertile couple: should diagnostic laparoscopy be performed in the infertility work up programme in patients undergoing intrauterine insemination? Hum. Reprod. 2003;18:8–11. doi: 10.1093/humrep/deg034. [DOI] [PubMed] [Google Scholar]
- 20.MacLean JA, 2nd, Hayashi K. Progesterone Actions and Resistance in Gynecological Disorders. Cells. 2022;11:647. doi: 10.3390/cells11040647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cahill DJ, Hull MG. Pituitary-ovarian dysfunction and endometriosis. Hum. Reprod. Update. 2000;6:56–66. doi: 10.1093/humupd/6.1.56. [DOI] [PubMed] [Google Scholar]
- 22.Garrido N, Navarro J, Remohi J, Simon C, Pellicer A. Follicular hormonal environment and embryo quality in women with endometriosis. Hum. Reprod. Update. 2000;6:67–74. doi: 10.1093/humupd/6.1.67. [DOI] [PubMed] [Google Scholar]
- 23.Cahill DJ, Wardle PG, Maile LA, Harlow CR, Hull MG. Ovarian dysfunction in endometriosis-associated and unexplained infertility. J. Assist Reprod. Genet. 1997;14:554–557. doi: 10.1023/A:1022568331845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pellicer A, et al. The follicular and endocrine environment in women with endometriosis: local and systemic cytokine production. Fertil. Steril. 1998;70:425–431. doi: 10.1016/S0015-0282(98)00204-0. [DOI] [PubMed] [Google Scholar]
- 25.Punnonen J, Teisala K, Ranta H, Bennett B, Punnonen R. Increased levels of interleukin-6 and interleukin-10 in the peritoneal fluid of patients with endometriosis. Am. J. Obstet. Gynecol. 1996;174:1522–1526. doi: 10.1016/S0002-9378(96)70600-2. [DOI] [PubMed] [Google Scholar]
- 26.Lessey BA, et al. Aberrant integrin expression in the endometrium of women with endometriosis. J. Clin. Endocrinol. Metab. 1994;79:643–649. doi: 10.1210/jcem.79.2.7519194. [DOI] [PubMed] [Google Scholar]
- 27.Aghajanova L, Velarde MC, Giudice LC. The progesterone receptor coactivator Hic-5 is involved in the pathophysiology of endometriosis. Endocrinology. 2009;150:3863–3870. doi: 10.1210/en.2009-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marquardt RM, Kim TH, Shin JH, Jeong JW. Progesterone and Estrogen Signaling in the Endometrium: What Goes Wrong in Endometriosis? Int J. Mol. Sci. 2019;20:3822. doi: 10.3390/ijms20153822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vannuccini S, et al. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum. Reprod. Update. 2016;22:104–115. doi: 10.1093/humupd/dmv044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brosens I, et al. Risks of adverse pregnancy outcome in endometriosis. Fertil. Steril. 2012;98:30–35. doi: 10.1016/j.fertnstert.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 31.Barragan F, et al. Human Endometrial Fibroblasts Derived from Mesenchymal Progenitors Inherit Progesterone Resistance and Acquire an Inflammatory Phenotype in the Endometrial Niche in Endometriosis. Biol. Reprod. 2016;94:118. doi: 10.1095/biolreprod.115.136010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nikoo S, et al. Menstrual blood-derived stromal stem cells from women with and without endometriosis reveal different phenotypic and functional characteristics. Mol. Hum. Reprod. 2014;20:905–918. doi: 10.1093/molehr/gau044. [DOI] [PubMed] [Google Scholar]
- 33.Shih AJ, et al. Single-cell analysis of menstrual endometrial tissues defines phenotypes associated with endometriosis. BMC Med. 2022;20:315. doi: 10.1186/s12916-022-02500-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ng SW, et al. Endometrial Decidualization: The Primary Driver of Pregnancy Health. Int J. Mol. Sci. 2020;21:4092. doi: 10.3390/ijms21114092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Critchley HOD, Maybin JA, Armstrong GM, Williams ARW. Physiology of the Endometrium and Regulation of Menstruation. Physiol. Rev. 2020;100:1149–1179. doi: 10.1152/physrev.00031.2019. [DOI] [PubMed] [Google Scholar]
- 36.Gellersen B, Brosens JJ. Cyclic decidualization of the human endometrium in reproductive health and failure. Endocr. Rev. 2014;35:851–905. doi: 10.1210/er.2014-1045. [DOI] [PubMed] [Google Scholar]
- 37.Rytkonen KT, et al. Decidualization of Human Endometrial Stromal Fibroblasts is a Multiphasic Process Involving Distinct Transcriptional Programs. Reprod. Sci. 2019;26:323–336. doi: 10.1177/1933719118802056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tamura I, et al. Genome-wide analysis of histone modifications in human endometrial stromal cells. Mol. Endocrinol. 2014;28:1656–1669. doi: 10.1210/me.2014-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aghajanova L, et al. The protein kinase A pathway-regulated transcriptome of endometrial stromal fibroblasts reveals compromised differentiation and persistent proliferative potential in endometriosis. Endocrinology. 2010;151:1341–1355. doi: 10.1210/en.2009-0923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Michalski SA, Chadchan SB, Jungheim ES, Kommagani R. Isolation of Human Endometrial Stromal Cells for In Vitro Decidualization. J. Vis. Exp. 2018;1:57684. doi: 10.3791/57684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lockwood CJ, et al. Steroid-modulated stromal cell tissue factor expression: a model for the regulation of endometrial hemostasis and menstruation. J. Clin. Endocrinol. Metab. 1993;77:1014–1019. doi: 10.1210/jcem.77.4.8408448. [DOI] [PubMed] [Google Scholar]
- 42.Brosens JJ, Hayashi N, White JO. Progesterone receptor regulates decidual prolactin expression in differentiating human endometrial stromal cells. Endocrinology. 1999;140:4809–4820. doi: 10.1210/endo.140.10.7070. [DOI] [PubMed] [Google Scholar]
- 43.Wu LW, et al. VRAP is an adaptor protein that binds KDR, a receptor for vascular endothelial cell growth factor. J. Biol. Chem. 2000;275:6059–6062. doi: 10.1074/jbc.275.9.6059. [DOI] [PubMed] [Google Scholar]
- 44.Gibson C, de Ruijter-Villani M, Rietveld J, Stout TAE. Amino acid transporter expression in the endometrium and conceptus membranes during early equine pregnancy. Reprod. Fertil. Dev. 2018;30:1675–1688. doi: 10.1071/RD17352. [DOI] [PubMed] [Google Scholar]
- 45.Forde N, et al. Amino acids in the uterine luminal fluid reflects the temporal changes in transporter expression in the endometrium and conceptus during early pregnancy in cattle. PLoS One. 2014;9:e100010. doi: 10.1371/journal.pone.0100010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alam MS, et al. TNF plays a crucial role in inflammation by signaling via T cell TNFR2. Proc. Natl Acad. Sci. USA. 2021;118:e2109972118. doi: 10.1073/pnas.2109972118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steff AM, et al. Serum concentrations of insulin-like growth factor-1, soluble tumor necrosis factor receptor-1 and angiogenin in endometriosis patients. Am. J. Reprod. Immunol. 2004;51:166–173. doi: 10.1046/j.8755-8920.2003.00138.x. [DOI] [PubMed] [Google Scholar]
- 48.Cermisoni GC, et al. Vitamin D and Endometrium: A Systematic Review of a Neglected Area of Research. Int J. Mol. Sci. 2018;19:2320. doi: 10.3390/ijms19082320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lachmann A, et al. ChEA: transcription factor regulation inferred from integrating genome-wide ChIP-X experiments. Bioinformatics. 2010;26:2438–2444. doi: 10.1093/bioinformatics/btq466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Keenan AB, et al. ChEA3: transcription factor enrichment analysis by orthogonal omics integration. Nucleic Acids Res. 2019;47:W212–W224. doi: 10.1093/nar/gkz446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clementi C, et al. Activin-like kinase 2 functions in peri-implantation uterine signaling in mice and humans. PLoS Genet. 2013;9:e1003863. doi: 10.1371/journal.pgen.1003863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tamura I, et al. Novel Function of a Transcription Factor WT1 in Regulating Decidualization in Human Endometrial Stromal Cells and Its Molecular Mechanism. Endocrinology. 2017;158:3696–3707. doi: 10.1210/en.2017-00478. [DOI] [PubMed] [Google Scholar]
- 53.Wei XW, et al. TCF3 regulates human endometrial stromal cell proliferation and migration in RPL. Reproduction. 2022;163:281–291. doi: 10.1530/REP-21-0463. [DOI] [PubMed] [Google Scholar]
- 54.Liu N, Lin X, Huang C. Activation of the reverse transsulfuration pathway through NRF2/CBS confers erastin-induced ferroptosis resistance. Br. J. Cancer. 2020;122:279–292. doi: 10.1038/s41416-019-0660-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Takahashi N, et al. 3D Culture Models with CRISPR Screens Reveal Hyperactive NRF2 as a Prerequisite for Spheroid Formation via Regulation of Proliferation and Ferroptosis. Mol. Cell. 2020;80:828–844.e826. doi: 10.1016/j.molcel.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dodson M, Castro-Portuguez R, Zhang DD. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23:101107. doi: 10.1016/j.redox.2019.101107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Derynck R, Budi EH. Specificity, versatility, and control of TGF-beta family signaling. Sci. Signal. 2019;12:eaav5183. doi: 10.1126/scisignal.aav5183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bell SC, Jackson JA, Ashmore J, Zhu HH, Tseng L. Regulation of insulin-like growth factor-binding protein-1 synthesis and secretion by progestin and relaxin in long term cultures of human endometrial stromal cells. J. Clin. Endocrinol. Metab. 1991;72:1014–1024. doi: 10.1210/jcem-72-5-1014. [DOI] [PubMed] [Google Scholar]
- 59.Szwarc MM, et al. Human endometrial stromal cell decidualization requires transcriptional reprogramming by PLZF. Biol. Reprod. 2018;98:15–27. doi: 10.1093/biolre/iox161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pei J, Pan X, Wei G, Hua Y. Research progress of glutathione peroxidase family (GPX) in redoxidation. Front. Pharm. 2023;14:1147414. doi: 10.3389/fphar.2023.1147414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lei P, Bai T, Sun Y. Mechanisms of Ferroptosis and Relations With Regulated Cell Death: A Review. Front Physiol. 2019;10:139. doi: 10.3389/fphys.2019.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Katagiri T, Watabe T. Bone Morphogenetic Proteins. Cold Spring Harb. Perspect. Biol. 2016;8:a021899. doi: 10.1101/cshperspect.a021899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chaudhry SS, et al. Fibrillin-1 regulates the bioavailability of TGFbeta1. J. Cell Biol. 2007;176:355–367. doi: 10.1083/jcb.200608167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tan FK, et al. Autoantibodies to the extracellular matrix microfibrillar protein, fibrillin-1, in patients with scleroderma and other connective tissue diseases. J. Immunol. 1999;163:1066–1072. doi: 10.4049/jimmunol.163.2.1066. [DOI] [PubMed] [Google Scholar]
- 65.Tan FK, et al. Autoantibodies to fibrillin 1 in systemic sclerosis: ethnic differences in antigen recognition and lack of correlation with specific clinical features or HLA alleles. Arthritis Rheum. 2000;43:2464–2471. doi: 10.1002/1529-0131(200011)43:11<2464::AID-ANR13>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 66.Senecal JL, Hoa S, Yang R, Koenig M. Pathogenic roles of autoantibodies in systemic sclerosis: Current understandings in pathogenesis. J. Scleroderma Relat. Disord. 2020;5:103–129. doi: 10.1177/2397198319870667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Atanasova MA, et al. Anti-fibrillin-1 autoantibodies in normal pregnancy and recurrent pregnancy loss. Autoimmun. Rev. 2011;10:131–136. doi: 10.1016/j.autrev.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 68.Pinero J, Sauch J, Sanz F, Furlong LI. The DisGeNET cytoscape app: Exploring and visualizing disease genomics data. Comput Struct. Biotechnol. J. 2021;19:2960–2967. doi: 10.1016/j.csbj.2021.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ozaki R, et al. Reprogramming of the retinoic acid pathway in decidualizing human endometrial stromal cells. PLoS One. 2017;12:e0173035. doi: 10.1371/journal.pone.0173035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yin Y, Haller ME, Chadchan SB, Kommagani R, Ma L. Signaling through retinoic acid receptors is essential for mammalian uterine receptivity and decidualization. JCI Insight. 2021;6:e150254. doi: 10.1172/jci.insight.150254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pavone ME, Malpani S, Dyson M, Bulun SE. Altered retinoid signaling compromises decidualization in human endometriotic stromal cells. Reproduction. 2017;154:207–216. doi: 10.1530/REP-16-0592. [DOI] [PubMed] [Google Scholar]
- 72.Mazur EC, et al. Progesterone receptor transcriptome and cistrome in decidualized human endometrial stromal cells. Endocrinology. 2015;156:2239–2253. doi: 10.1210/en.2014-1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bernardi LA, et al. The Essential Role of GATA6 in the Activation of Estrogen Synthesis in Endometriosis. Reprod. Sci. 2019;26:60–69. doi: 10.1177/1933719118756751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dyson MT, et al. Genome-wide DNA methylation analysis predicts an epigenetic switch for GATA factor expression in endometriosis. PLoS Genet. 2014;10:e1004158. doi: 10.1371/journal.pgen.1004158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xu J, et al. Inhibitor of the tyrosine phosphatase STEP reverses cognitive deficits in a mouse model of Alzheimer’s disease. PLoS Biol. 2014;12:e1001923. doi: 10.1371/journal.pbio.1001923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lucas ES, et al. Recurrent pregnancy loss is associated with a pro-senescent decidual response during the peri-implantation window. Commun. Biol. 2020;3:37. doi: 10.1038/s42003-020-0763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee KY, et al. Bmp2 is critical for the murine uterine decidual response. Mol. Cell Biol. 2007;27:5468–5478. doi: 10.1128/MCB.00342-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Monsivais D, et al. Endometrial receptivity and implantation require uterine BMP signaling through an ACVR2A-SMAD1/SMAD5 axis. Nat. Commun. 2021;12:3386. doi: 10.1038/s41467-021-23571-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Monsivais D, et al. BMP7 Induces Uterine Receptivity and Blastocyst Attachment. Endocrinology. 2017;158:979–992. doi: 10.1210/en.2016-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tang S, Cope DI, Vasquez YM, Monsivais D. BMP/SMAD1/5 Signaling in the Endometrial Epithelium Is Essential for Receptivity and Early Pregnancy. Endocrinology. 2022;163:bqac043. doi: 10.1210/endocr/bqac043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Peng Y, et al. Inhibitor of DNA binding/differentiation helix-loop-helix proteins mediate bone morphogenetic protein-induced osteoblast differentiation of mesenchymal stem cells. J. Biol. Chem. 2004;279:32941–32949. doi: 10.1074/jbc.M403344200. [DOI] [PubMed] [Google Scholar]
- 82.Yang J, et al. Id proteins are critical downstream effectors of BMP signaling in human pulmonary arterial smooth muscle cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2013;305:L312–L321. doi: 10.1152/ajplung.00054.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luo J, et al. The regulation of IGFBP3 by BMP2 has a role in human endometrial remodeling. FASEB J. 2020;34:15462–15479. doi: 10.1096/fj.202000508R. [DOI] [PubMed] [Google Scholar]
- 84.Deepak V, Ravikumar N, Badell ML, Sidell N, Rajakumar A. Transcription factor ID1 is involved in decidualization of stromal cells: Implications in preeclampsia. Pregnancy Hypertens. 2020;21:7–13. doi: 10.1016/j.preghy.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 85.Luo J, et al. ID3 mediates BMP2-induced downregulation of ICAM1 expression in human endometiral stromal cells and decidual cells. Front Cell Dev. Biol. 2023;11:1090593. doi: 10.3389/fcell.2023.1090593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Li Q, et al. WNT4 acts downstream of BMP2 and functions via beta-catenin signaling pathway to regulate human endometrial stromal cell differentiation. Endocrinology. 2013;154:446–457. doi: 10.1210/en.2012-1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gillespie M, et al. The reactome pathway knowledgebase 2022. Nucleic Acids Res. 2022;50:D687–D692. doi: 10.1093/nar/gkab1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lee HC, Lin SC, Wu MH, Tsai SJ. Inhibiting NTRK2 signaling causes endometriotic lesion regression. Reproduction. 2021;161:11–19. doi: 10.1530/REP-20-0163. [DOI] [PubMed] [Google Scholar]
- 89.Dewanto A, et al. Localization of TrkB and p75 receptors in peritoneal and deep infiltrating endometriosis: an immunohistochemical study. Reprod. Biol. Endocrinol. 2016;14:43. doi: 10.1186/s12958-016-0178-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Greaves E, et al. Estradiol is a critical mediator of macrophage-nerve cross talk in peritoneal endometriosis. Am. J. Pathol. 2015;185:2286–2297. doi: 10.1016/j.ajpath.2015.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hechtman JF. NTRK insights: best practices for pathologists. Mod. Pathol. 2022;35:298–305. doi: 10.1038/s41379-021-00913-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rahmioglu N, et al. The genetic basis of endometriosis and comorbidity with other pain and inflammatory conditions. Nat. Genet. 2023;55:423–436. doi: 10.1038/s41588-023-01323-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Heintzman ND, et al. Distinct and predictive chromatin signatures of transcriptional promoters and enhancers in the human genome. Nat. Genet. 2007;39:311–318. doi: 10.1038/ng1966. [DOI] [PubMed] [Google Scholar]
- 94.Creyghton MP, et al. Histone H3K27ac separates active from poised enhancers and predicts developmental state. Proc. Natl Acad. Sci. USA. 2010;107:21931–21936. doi: 10.1073/pnas.1016071107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sur I, Taipale J. The role of enhancers in cancer. Nat. Rev. Cancer. 2016;16:483–493. doi: 10.1038/nrc.2016.62. [DOI] [PubMed] [Google Scholar]
- 96.Kuessel L, et al. Soluble VCAM-1/soluble ICAM-1 ratio is a promising biomarker for diagnosing endometriosis. Hum. Reprod. 2017;32:770–779. doi: 10.1093/humrep/dex028. [DOI] [PubMed] [Google Scholar]
- 97.Pazhohan A, et al. Expression and shedding of CD44 in the endometrium of women with endometriosis and modulating effects of vitamin D: A randomized exploratory trial. J. Steroid Biochem Mol. Biol. 2018;178:150–158. doi: 10.1016/j.jsbmb.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 98.Knudtson JF, et al. CD44 variant 6 is involved in the attachmental cells to peritoneum. F. S Sci. 2020;1:188–194. doi: 10.1016/j.xfss.2020.08.002. [DOI] [PubMed] [Google Scholar]
- 99.Li T, et al. WNT5A Interacts With FZD5 and LRP5 to Regulate Proliferation and Self-Renewal of Endometrial Mesenchymal Stem-Like Cells. Front Cell Dev. Biol. 2022;10:837827. doi: 10.3389/fcell.2022.837827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Witz CA. Cell adhesion molecules and endometriosis. Semin. Reprod. Med. 2003;21:173–182. doi: 10.1055/s-2003-41324. [DOI] [PubMed] [Google Scholar]
- 101.Chi RA, et al. Human Endometrial Transcriptome and Progesterone Receptor Cistrome Reveal Important Pathways and Epithelial Regulators. J. Clin. Endocrinol. Metab. 2020;105:e1419–e1439. doi: 10.1210/clinem/dgz117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nacht AS, et al. C/EBPalpha mediates the growth inhibitory effect of progestins on breast cancer cells. EMBO J. 2019;38:e101426. doi: 10.15252/embj.2018101426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kajihara T, Brosens JJ, Ishihara O. The role of FOXO1 in the decidual transformation of the endometrium and early pregnancy. Med Mol. Morphol. 2013;46:61–68. doi: 10.1007/s00795-013-0018-z. [DOI] [PubMed] [Google Scholar]
- 104.Vasquez YM, et al. FOXO1 regulates uterine epithelial integrity and progesterone receptor expression critical for embryo implantation. PLoS Genet. 2018;14:e1007787. doi: 10.1371/journal.pgen.1007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wang S, et al. Target analysis by integration of transcriptome and ChIP-seq data with BETA. Nat. Protoc. 2013;8:2502–2515. doi: 10.1038/nprot.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pan MG, Xiong Y, Chen F. NFAT gene family in inflammation and cancer. Curr. Mol. Med. 2013;13:543–554. doi: 10.2174/1566524011313040007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Xu L, Fan Y, Wang J, Shi R. Dysfunctional intercellular communication and metabolic signaling pathways in thin endometrium. Front. Physiol. 2022;13:1050690. doi: 10.3389/fphys.2022.1050690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Papaioannou VE. The T-box gene family: emerging roles in development, stem cells and cancer. Development. 2014;141:3819–3833. doi: 10.1242/dev.104471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Prasnikar E, et al. Determining the Molecular Background of Endometrial Receptivity in Adenomyosis. Biomolecules. 2020;10:1311. doi: 10.3390/biom10091311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ravasi T, et al. An atlas of combinatorial transcriptional regulation in mouse and man. Cell. 2010;140:744–752. doi: 10.1016/j.cell.2010.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gujral P, Mahajan V, Lissaman AC, Ponnampalam AP. Histone acetylation and the role of histone deacetylases in normal cyclic endometrium. Reprod. Biol. Endocrinol. 2020;18:84. doi: 10.1186/s12958-020-00637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Xu Y, et al. A novel mechanism regulating pyroptosis-induced fibrosis in endometriosis via lnc-MALAT1/miR-141-3p/NLRP3 pathwaydagger. Biol. Reprod. 2023;109:156–171. doi: 10.1093/biolre/ioad057. [DOI] [PubMed] [Google Scholar]
- 113.Liang Z, et al. Silencing of lncRNA MALAT1 facilitates erastin-induced ferroptosis in endometriosis through miR-145-5p/MUC1 signaling. Cell Death Discov. 2022;8:190. doi: 10.1038/s41420-022-00975-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Du Y, et al. Estradiol promotes EMT in endometriosis via MALAT1/miR200s sponge function. Reproduction. 2019;157:179–188. doi: 10.1530/REP-18-0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Shi L, et al. LncRNA MALAT1 promotes decidualization of endometrial stromal cells via sponging miR-498-3p and targeting histone deacetylase 4. Cell Biol. Int. 2022;46:1264–1274. doi: 10.1002/cbin.11814. [DOI] [PubMed] [Google Scholar]
- 116.Marquardt RM, Tran DN, Lessey BA, Rahman MS, Jeong JW. Epigenetic Dysregulation in Endometriosis: Implications for Pathophysiology and Therapeutics. Endocr. Rev. 2023;44:1074–1095. doi: 10.1210/endrev/bnad020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rawlings TM, et al. Modelling the impact of decidual senescence on embryo implantation in human endometrial assembloids. Elife. 2021;10:e69603. doi: 10.7554/eLife.69603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Murata H, et al. Heat stress induces oxidative stress and activates the KEAP1-NFE2L2-ARE pathway in bovine endometrial epithelial cellsdagger. Biol. Reprod. 2021;105:1114–1125. doi: 10.1093/biolre/ioab143. [DOI] [PubMed] [Google Scholar]
- 119.Rushmore TH, Morton MR, Pickett CB. The antioxidant responsive element. Activation by oxidative stress and identification of the DNA consensus sequence required for functional activity. J. Biol. Chem. 1991;266:11632–11639. doi: 10.1016/S0021-9258(18)99004-6. [DOI] [PubMed] [Google Scholar]
- 120.Wyatt J, et al. The role of iron in the pathogenesis of endometriosis: a systematic review. Hum. Reprod. Open. 2023;2023:hoad033. doi: 10.1093/hropen/hoad033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sun F, et al. Decidual Stromal Cell Ferroptosis Associated with Abnormal Iron Metabolism Is Implicated in the Pathogenesis of Recurrent Pregnancy Loss. Int J. Mol. Sci. 2023;24:7836. doi: 10.3390/ijms24097836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kriseman ML, et al. SMAD2/3 signaling in the uterine epithelium controls endometrial cell homeostasis and regeneration. Commun. Biol. 2023;6:261. doi: 10.1038/s42003-023-04619-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kriseman M, et al. Uterine double-conditional inactivation of Smad2 and Smad3 in mice causes endometrial dysregulation, infertility, and uterine cancer. Proc. Natl. Acad. Sci. USA. 2019;116:3873–3882. doi: 10.1073/pnas.1806862116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Monsivais D, Matzuk MM, Pangas SA. The TGF-beta Family in the Reproductive Tract. Cold Spring Harb. Perspect. Biol. 2017;9:a022251. doi: 10.1101/cshperspect.a022251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wetendorf M, DeMayo FJ. The progesterone receptor regulates implantation, decidualization, and glandular development via a complex paracrine signaling network. Mol. Cell Endocrinol. 2012;357:108–118. doi: 10.1016/j.mce.2011.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cope DI, Monsivais D. Progesterone Receptor Signaling in the Uterus Is Essential for Pregnancy Success. Cells. 2022;11:1474. doi: 10.3390/cells11091474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yu PB, et al. BMP type I receptor inhibition reduces heterotopic [corrected] ossification. Nat. Med. 2008;14:1363–1369. doi: 10.1038/nm.1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Vrijens K, et al. Identification of small molecule activators of BMP signaling. PLoS One. 2013;8:e59045. doi: 10.1371/journal.pone.0059045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Carlson WD, Keck PC, Bosukonda D, Carlson FR., Jr. A Process for the Design and Development of Novel Bone Morphogenetic Protein-7 (BMP-7) Mimetics With an Example: THR-184. Front Pharm. 2022;13:864509. doi: 10.3389/fphar.2022.864509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Monsivais D, et al. Uterine ALK3 is essential during the window of implantation. Proc. Natl Acad. Sci. USA. 2016;113:E387–E395. doi: 10.1073/pnas.1523758113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nagashima T, et al. BMPR2 is required for postimplantation uterine function and pregnancy maintenance. J. Clin. Invest. 2013;123:2539–2550. doi: 10.1172/JCI65710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Janusz J, et al. Participation of Selected Soluble BMP-2 and BMP-7 Bone Morphogenetic Proteins and Their Soluble Type I ALK-1 and Type II BMPR2 Receptors in Formation and Development of Endometriosis. Biomedicines. 2021;9:1292. doi: 10.3390/biomedicines9101292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Quintero-Ronderos P, et al. Novel genes and mutations in patients affected by recurrent pregnancy loss. PLoS One. 2017;12:e0186149. doi: 10.1371/journal.pone.0186149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hewitt SC, et al. From cup to dish: how to make and use endometrial organoid and stromal cultures derived from menstrual fluid. Front Endocrinol. (Lausanne) 2023;14:1220622. doi: 10.3389/fendo.2023.1220622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008;3:1101–1108. doi: 10.1038/nprot.2008.73. [DOI] [PubMed] [Google Scholar]
- 136.Chen EY, et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinforma. 2013;14:128. doi: 10.1186/1471-2105-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kuleshov MV, et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016;44:W90–W97. doi: 10.1093/nar/gkw377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Xie Z, et al. Gene Set Knowledge Discovery with Enrichr. Curr. Protoc. 2021;1:e90. doi: 10.1002/cpz1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yu G, Wang LG, Han Y, He Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16:284–287. doi: 10.1089/omi.2011.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Skene PJ, Henikoff S. An efficient targeted nuclease strategy for high-resolution mapping of DNA binding sites. Elife. 2017;6:e21856. doi: 10.7554/eLife.21856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhang Y, et al. Model-based analysis of ChIP-Seq (MACS) Genome Biol. 2008;9:R137. doi: 10.1186/gb-2008-9-9-r137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yu G, Wang LG, He QY. ChIPseeker: an R/Bioconductor package for ChIP peak annotation, comparison and visualization. Bioinformatics. 2015;31:2382–2383. doi: 10.1093/bioinformatics/btv145. [DOI] [PubMed] [Google Scholar]
- 143.Ross-Innes CS, et al. Differential oestrogen receptor binding is associated with clinical outcome in breast cancer. Nature. 2012;481:389–393. doi: 10.1038/nature10730. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
Sequencing data are available in the NCBI Gene Expression Ominibus under SuperSeries GSE243158. All source data for figures in this study are provided in the supplementary data files. All source data for figures in this study are provided in Supplementary Data file 8. Uncropped blots are included in Supplementary Figs. 7–9.