Abstract
Lipoprotein(a) [Lp(a)] is made up of a low-density lipoprotein (LDL) particle and a specific apolipoprotein(a). The blood concentration of Lp(a) is approximately 90% genetically determined, and the main genetic factor determining Lp(a) levels is the size of the apo(a) isoform, which is determined by the number of KIV2 domain repeats. The size of the apo(a) isoform is inversely proportional to the blood concentration of Lp(a). Lp(a) is a strong and independent cardiovascular risk factor. Elevated Lp(a) levels ≥ 50 mg/dl (≥ 125 nmol/l) are estimated to occur in more than 1.5 billion people worldwide. However, determination of Lp(a) levels is performed far too rarely, including Poland, where, in fact, it is only since the 2021 guidelines of the Polish Lipid Association (PoLA) and five other scientific societies that Lp(a) measurements have begun to be performed. Determination of Lp(a) concentrations is not easy due to, among other things, the different sizes of the apo(a) isoforms; however, the currently available certified tests make it possible to distinguish between people with low and high cardiovascular risk with a high degree of precision. In 2022, the first guidelines for the management of patients with elevated lipoprotein(a) levels were published by the European Atherosclerosis Society (EAS) and the American Heart Association (AHA). The first Polish guidelines are the result of the work of experts from the two scientific societies and their aim is to provide clear, practical recommendations for the determination and management of elevated Lp(a) levels.
Keywords: cardiovascular disease, lipoprotein(a), management, recommendations, cardiovascular risk
Introduction
Lipoprotein(a) [Lp(a)] was discovered in 1963 by Norwegian scientist Kåre Berg [1]. Over the following 60 years, knowledge about lipids and cardiovascular diseases (CVD) progressed significantly. Over the past decade, it has become increasingly clear that Lp(a) is a key component of residual cardiovascular disease risk [2]. Lp(a) has been shown to be strongly and independently associated with atherosclerotic cardiovascular disease (ASCVD) and the occurrence of aortic valve stenosis (AVS). Lp(a) is also associated with peripheral artery disease (PAD) and, to a lesser extent, with ischaemic stroke (IS) and heart failure (HF) [3]. Recent studies also suggest that higher levels of Lp(a) may be associated with an increased risk of atrial fibrillation (AF), but this requires further confirmation in studies [4–6]. In contrast, the association between Lp(a) and the risk of venous thromboembolism is not supported by most recent studies [7, 8].
Elevated Lp(a) levels ≥ 50 mg/dl (≥ 125 nmol/l) are estimated to occur in more than 1.5 billion people worldwide [9]. However, tests on this parameter are performed far too rarely [10–12], most often due to insufficient knowledge. There are currently no dedicated medicines that target the reduction of Lp(a) concentrations and available lipid-lowering treatment can only modify the concentration of this parameter to a certain extent (20–30%). The aim of this Expert Opinion prepared by the two most important scientific societies in Poland in the relevant area is to provide clinical recommendations for the determination and treatment of elevated Lp(a) levels.
Lipoprotein(a) molecular structure
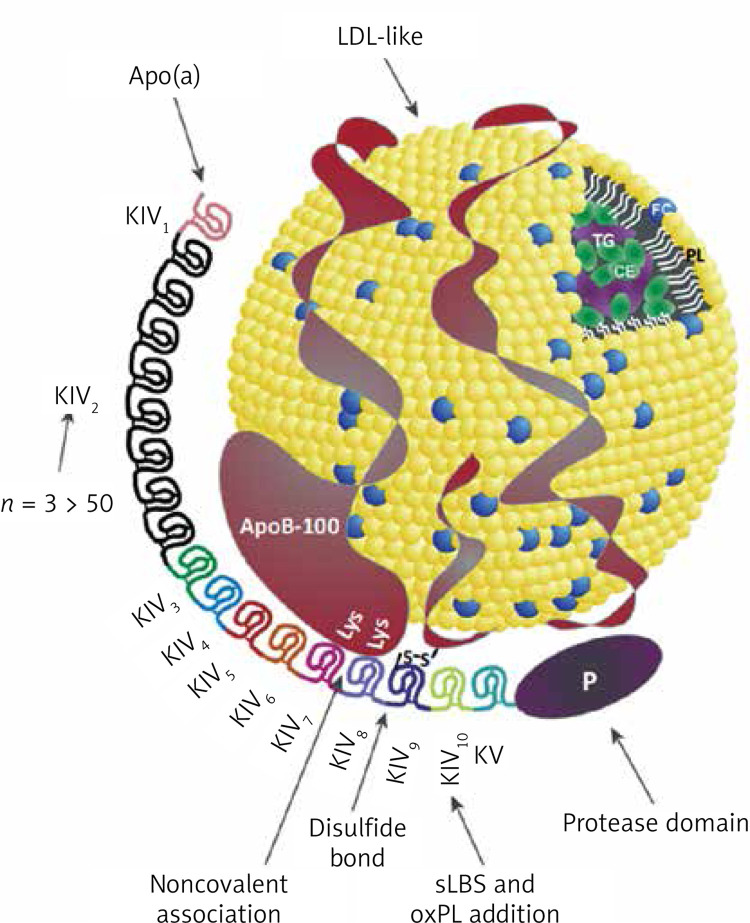
Lp(a) is a lipoprotein composed of a low-density lipoprotein (LDL)-like particle and a specific apolipoprotein(a) [apo(a)] [13] (Figure 1). Apo(a) is synthesised in hepatocytes, a characteristic feature of apo(a) is the presence of protein triple-loop (kringle) structures. Apo(a) is composed of a single kringle V (KV) domain, a non-reactive serine protease-like domain, and 10 KIV subtypes (KIV1-KIV10), among them the KIV2 subtype, which occurs in < 3 to > 50 copies [14, 15] (Figure 1). The number of KIV2 repeats is determined by the LPA gene [16]. Apo(a) is covalently linked to apoB100 via a single disulphide bond involving a unique unpaired cysteine residue (Cys4057) in the KIV9 domain [17], and via non-covalent interactions involving the KIV7 and KIV8 domains [18]. The KIV10 domain contains a strong lysine binding site (sLBS) that mediates interactions between apo(a) and biological ligands such as fibrin [19]. Importantly, KIV10 also contains a site to which oxidised phospholipids (OxPL) are covalently attached [20] (Figure 1). Most individuals (~80%) have two apo(a) alleles of different magnitudes, each inherited from one parent [21]. Thus, a person may have two types of molecules: two large, two small or different sized apo(a) molecules [22].
Figure 1.
Structure of the lipoprotein(a) molecule, reprinted and modified from [22] with permission (Licence number: 5705320305220)
P – protease-like domain, PL – phospholipids, FC – free cholesterol, CE – cholesterol esters, TG – triglycerides.
Lp(a) is rich in cholesterol esters and phospholipids and contains lower amounts of free cholesterol and triglycerides [23]. Lp(a) particles are the main carrier of OxPL among apolipoprotein B (apoB)-containing lipoproteins [24]. Lp(a) is predominantly removed and catabolised by the liver (and to a lesser extent by the kidney) via a number of putative pathways mediated by LDL receptors (LDLR), class B1 scavenger receptors (SRB1) and the plasminogen receptors PLGR and PLGRKT [25, 26].
The physiological function of Lp(a) is still not known [16]. The mechanism of pathophysiological action of Lp(a) associated with CVD risk involves multiple pathways, most notably an apoB-mediated proatherogenic effect [27, 28] and a pro-inflammatory effect through its oxidised phospholipid content [29–31]. The chemoattractant for type 1 monocytes (MCP-1) present on the Lp(a) molecule increases the migration of monocytes across the endothelial cell barrier into the vessel wall. At the same time, Lp(a) stimulates monocytes to increase production and release of pro-inflammatory cytokines (including interleukin (IL)-1β, IL-6, IL-8, tumour necrosis factor-α [TNF-α]) [30]. Lp(a) is also associated with AVS/CVD risk through the proinflammatory and procalcifying effects of OxPL, which are thought to be able to enter the aortic valve through binding by apo(a). Lipoprotein-associated phospholipase A2 (Lp-PLA2) and autotaxin, enzymes present on Lp(a), are also likely to be involved in the pathogenesis of AVS/CVD [32]. It is worth noting here that the Lp(a) molecule has a high homology (75–99%) with plasminogen, but lacks protease activity, and was therefore assumed to inhibit fibrinolysis and show prothrombotic potential [33], but this has not been confirmed by recent studies on the effect of lowering Lp(a) on fibrinolytic activity or by studies on the effect of elevated Lp(a) levels on venous thrombosis [7, 8].
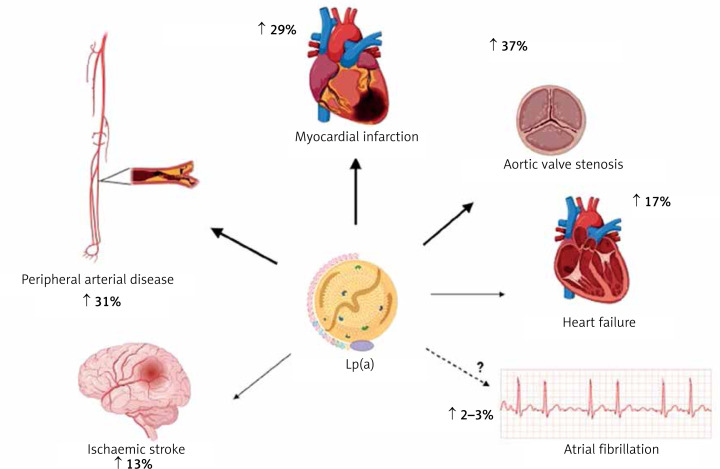
Lipoprotein(a) and cardiovascular disease
Results from a number of prospective, epidemiological, genetic, and randomised Mendelian randomization (MR) studies have shown that elevated Lp(a) levels are independently and causally associated with ASCVD and aortic valve stenosis (AVS) [34–42]. Results from recent studies show that exposure to higher concentrations of Lp(a) has the greatest effect on the risk of myocardial infarction (MI) and AVS, while the effect on the risk of ischaemic stroke, PAD, HF, CVD mortality and overall mortality is significant but somewhat weaker (Figure 2) [3, 43, 44].
Figure 2.
Association between high plasma lipoprotein(a) levels and CVD (risk increase based on analysis of genetically determined increase in Lp(a) risk by one standard deviation according to: [63])
An analysis of UK Biobank data covering 460,000 people showed that the risk of ASCVD was 11% higher for each Lp(a) increment of 50 nmol/l (−20 mg/dl; risk ratio 1.11 per 50 nmol/l [95% CI: 1.10–1.12]) [45]. In individuals with very high Lp(a) levels (e.g. > 180 mg/dl [(450 nmol/l)]), the risk of ASCVD may be comparable to those with a family history of premature CVD or those with heterozygous familial hypercholesterolaemia (heFH) [46]. In a study on a large population of ~50,000 people, high Lp(a) levels significantly correlated with an increased incidence of ischaemic stroke [47]. A study in a Danish population of 69,764 participants showed that Lp(a) levels > 69 mg/dl (−172 nmol/l) were associated with a higher risk of death from CVD causes, and Lp(a) levels > 93 mg/dl (−232 nmol/l) resulted in a higher risk of death from any cause [47]. The association of Lp(a) with the risk of overall and CVD-related mortality has also been confirmed by other studies [48]. A recent study showed that each 50 mg/dl increase in Lp(a) concentration (−125 nmol/l) was associated with a 31% increase in the risk of death from any cause and from ASCVD in the general population and 15% in patients with ASCVD [49].
Lp(a) is recognised as a strong risk factor for the development of AVS, promotes aortic valve calcification (CAVS) and is associated with the progression of CAVS as confirmed in several studies [47, 50–52]. Available research indicates that Lp(a) influences the risk of developing AVS, even in patients with Lp(a) levels between 20 and 64 mg/dl (−50–160 nmol/l) (RR = 1.6, 95% CI: 1.1–2.4), while those with levels > 90 mg/dl (> 225 nmol/l) show an almost threefold increase in risk [37]. A meta-analysis involving 8 studies and 52,931 participants found that plasma Lp(a) levels ≥ 50 mg/dl (≥ 125 nmol/l) were associated with a 1.76-fold increased risk of CAVS (RR = 1.76; 95% CI: 1.47–2.11) [53]. An analysis of two prospective cohorts including a total of 145 patients with CAVS, showed that those with Lp(a) levels > 35 mg/dl (> 87.5 nmol/l) had faster disease progression, as well as a higher risk of the composite endpoint of aortic valve replacement and death [52].
Polish and international data indicate that the ASCVD population, which is least effectively treated and monitored for lipid disorders are patients with peripheral artery disease. Unfortunately, elevated Lp(a) levels also further increase this risk of PAD and its complications. In a study involving 1,472 patients with PAD, participants with Lp(a) levels > 30 mg/dl (> 75 nmol/l) had a higher risk of PAD-related surgery (HR = 1.20, 95% CI: 1.02–1.41) and lower limb peripheral revascularisation (HR = 1.33, 95% CI: 1.06–1.66]) [54]. In a systematic review including 15 studies and 493,650 patients, most studies confirmed a significant association between high Lp(a) levels and the risk of PAD. High Lp(a) levels have also been found to be associated with increased PAD progression, risk of intermittent claudication, recurrence of significant stenosis and risk of hospitalisation and death [55]. Higher levels of Lp(a) have been shown to be independently associated with an increased risk of major adverse limb events (MALE) [56]. A recently published analysis of pooled data from two randomised clinical trials TRA2P-TIMI 50 and FOURIER involving patients with stable atherosclerotic vascular disease confirms a significant association of Lp(a) with progression of lower extremity arteriosclerosis (PAD) [57].
The association between Lp(a) and HF is highly dependent on the effect of Lp(a) on coronary artery disease (CAD) and CAVS. Results from a large case-control study involving 143,087 participants confirmed the association of LPA genetic variants with HF risk; each 50 nmol/l (~20 mg/dl) increase in concentration was associated with a 5% increase in the risk of developing HF [58].
The role of Lp(a) in the development of atrial fibrillation (AF) is also not fully established. An analysis of UK biobank data involving 435,579 participants showed that each increase in Lp(a) of 50 nmol/l (−20 mg/dl) was associated with a 3% increase in the risk of AF [59]. Although coronary artery disease (CAD) itself is a risk factor for the occurrence of AF, according to some authors, Lp(a) may influence the development of AF independently of ASCVD [60, 61]. A meta-analysis including 275,647 AF cases and 2.1 million patients with Lp(a) showed that increased Lp(a) was associated with a very small increased risk of AF in studies based on Mendelian randomisation (OR = 1.024, 95% CI: 1.007–1.042, p < 0.001). The authors found a higher risk of AF in the European cohort (OR = 1.023, 95% CI: 1.007–1.040, p < 0.001) and a low risk (OR = 0.940, 95% CI: 0.893–0.990) in the Chinese population [4]. On the other hand, Garg et al. noted an inverse relationship between Lp(a) concentration and AF incidence after a follow-up period of almost 13 years [62]. A recent systematic review covering 11 observational studies and almost 1.25 million patients did not conclusively confirm the usefulness of Lp(a) assessment as a marker of AF risk in clinical practice and highlighted the need for further studies in this area [63].
Expert opinion: Elevated lipoprotein(a) concentrations are an independent (residual) risk factor for cardiovascular disease and Lp(a) should be determined at least once in every person’s lifetime (IA). Available data indicate a strong causal relationship between elevated Lp(a) concentrations and an increased risk of cardiovascular disease and its complications, peripheral artery disease, ischaemic stroke (by up to 30% for each increase in concentration of 20–50 mg/dl [50–125 nmol/l]), as well as a very high risk of developing aortic valve stenosis (up to three times higher for high Lp(a) concentrations).
Lp(a) concentration, genetic factors
Blood Lp(a) levels range from < 0.1 mg/dl to > 300 mg/dl (< 0.2 – > 750 nmol/l) and are approximately 90% genetically determined [64]. The main genetic factor determining blood Lp(a) levels is (apo(a) isoform size-dependent) the differential number of copies associated with the number of coding kringle-IV (K-IV) repeats in the LPA gene. The number of K-IV type 2 domain repeats determines the size of the apo(a) isoforms and is inversely proportional to Lp(a) concentration [65]. A low number of K-IV type 2 domain repeats (≤ 22) characterises small apo(a) isoforms and is associated with higher Lp(a) concentrations compared to large apo(a) isoforms [16]. However, the exact relationship between apo(a) isoform and Lp(a) concentrations is complex rather than linear and is also modified by functional single nucleotide polymorphisms (SNPs) [66]. Two well-known SNPs affecting Lp(a) concentrations are rs10455872 and rs3798220 usually observed for small apo(a) isoforms and indicative of high Lp(a) concentrations [39].
At birth, Lp(a) concentration is low and increases with age until about 5 years of age, when it usually reaches the value that is determined in adulthood [67]; however, it has been shown that it can continue to rise until adulthood [68, 69]. Lp(a) concentrations are influenced by race and gender. Lower Lp(a) concentrations are found in Chinese (mean 16 nmol/l [−6.4 mg/dl]), Caucasians (19 nmol/l [−7.6 mg/dl]) and South Asians (31 nmol/l [−12.4 mg/dl]), and highest in Black people (75 nmol/l [−50 mg/dl]) [45]. Women of both Caucasian and Black race are observed to have higher Lp(a) levels by approximately 5–10% compared to men [70–72]. Additionally, in women, Lp(a) levels are more variable and usually increase during menopause [73]. A recent study showed a 27% increase in Lp(a) levels in postmenopausal women [71].
Other factors influencing Lp(a) concentrations
Genetic factors have a strong influence on Lp(a) concentrations; however, some non-genetic factors can also modify them. Lifestyle changes have a minimal effect on Lp(a) levels [74]. Results from a recent dietary study show that a low-carbohydrate diet (LCD) rich in saturated fat reduced Lp(a) concentrations by 15%, and decreased insulin and triglyceride levels (after 20 weeks compared with a high-carbohydrate diet) [75]. In another study, the use of a ketogenic diet resulted in a 26% reduction in Lp(a) (after 3 weeks) [76]. However, on the other hand, it has been shown that a ketogenic diet can lead to increased total cholesterol, LDL-C and apoB [77], higher risk of type 2 diabetes [78] and, consequently, higher cardiovascular and all-cause mortality [79]. Hence, studies to date are not sufficient to consider a low-carbohydrate or ketogenic diet in people with elevated Lp(a) [80].
Reducing saturated fatty acids (SFA) intake, which is associated with lower LDL-C and reduced CVD risk, resulted in an increase in Lp(a) [81]. The inverse effect of dietary SFA reduction on LDL-C and Lp(a) [82], despite the lack of data on the clinical significance of this discrepancy, raises some questions regarding dietary recommendations [83]. It seems likely that the increase in Lp(a) concentrations as a result of SFA reduction may play an underestimated role as a determinant of CVD risk in individuals with very high Lp(a) concentrations and elevated LDL-C concentrations [83]. Therefore, the approach to dietary recommendations should be personalised [84].
Physical activity, increasing physical exertion, such as intensive strength training, or increasing cardiorespiratory fitness, has very little or no effect on Lp(a) concentrations, whereas it significantly affects the concentrations of other lipids and lipoproteins, especially triglycerides and HDL-C, and only has an impact on LDL-C when accompanied with weight loss [85]. A minimal modulating effect of exercise on Lp(a) levels has been reported in children and adults under 35 years of age and in diabetic patients, but this needs to be confirmed in further studies [74].
Endogenous sex hormones have little or no effect on Lp(a) levels [73] although recent data indicate an increase in Lp(a) concentrations in menopausal women. Post-menopausal hormone replacement therapy, on the other hand, reduces Lp(a) concentrations by 20-25% [86]. During pregnancy, Lp(a) values increase ~2-fold and return to baseline levels after delivery [87], hence some available studies have indicated an increased risk of pregnancy complications, including preeclampsia, low birth weight or preterm delivery, and some guidelines recommend monitoring Lp(a) levels during pregnancy [88]. However, the data are inconclusive, and a recent Mendelian Randomisation study does not appear to support a causal relationship between Lp(a) levels and the risk of preeclampsia [89].
Growth hormone treatment in adults with growth hormone deficiency results in a 2-fold increase in Lp(a) concentration [90, 91]. Lp(a) levels are decreased in hyperthyroidism and increased in hypothyroidism [92]. Treatment of overt hyperthyroidism with thyroxine or radioactive iodine therapy increased Lp(a) concentrations by 20–25% [92]. Levothyroxine in overt and subclinical hypothyroidism slightly reduces Lp(a) levels [93].
Kidney diseases increase Lp(a) levels, which start to rise even in the early stages of kidney damage [94]. Nephrotic syndrome causes a 3–5-fold increase [95] (compared to controls), and a 2-fold increase in Lp(a) levels has been observed in peritoneal dialysis patients (compared to controls) [96]. Kidney transplantation normalises Lp(a) levels to baseline values [97].
The concentration of Lp(a) depends on the synthesis of apo(a), which takes place in liver cells, hence Lp(a) concentrations decrease with the progression of liver damage [98, 99] (Table I [100–104]).
Table I.
Non-genetic factors and their influence on Lp(a) concentrations. Modified based on [100] completed with the information from: 1[101]; 2[102]; 3[103]; 4[104]
| Risk factor/disease/intervention | Impact on Lp(a) | Comments/recommendations |
|---|---|---|
| Related to lifestyle changes | ||
| Reducing the concentration of saturated fatty acids (SFA) | ↑ Up to 15% | No change in dietary recommendations to reduce SFA is recommended (III B). |
| Low carbohydrate/ketogenic diet | ↓ 15–25% | A ketogenic diet is not recommended for the reduction of Lp(a) (III B). |
| Natural products1 (nutraceuticals, dietary supplements), including L-carnitine (1–4 g/day), CoQ10 (120–300 mg/day), fibre (15 g/day) and Ginkgo biloba (240 mg/day) | ↓ 30% | Depending on baseline Lp(a) concentration. Limited data, needs confirmation in further studies (IIb B). |
| Endocrine disruption | ||
| Hyperthyroidism | ↓ Up to 25% during thyrostatic treatment or with radioactive iodine | No modification of therapy is recommended. |
| Hypothyroidism | ↑; ↓ Up to 20% for replacement therapy | No modification of therapy is recommended. |
| Growth hormone | ↑ 2× during treatment | No modification of therapy is recommended. |
| Pregnancy | ↑ 2× | Determination and monitoring of the maternal condition is recommended due to the increased risk of miscarriage, recurrent pregnancy loss and/or intrauterine growth restriction. Appears to have no causal relationship with preeclampsia. |
| Menopause | ↑ Up to 30% | |
| Postmenopausal hormone replacement therapy (e.g. with tibolone or raloxifene)2,3 | ↓ Up to 30% | No modification of therapy is recommended. |
| Chronic comorbidities | ||
| Chronic kidney disease | ↑ < 2× | Optimisation of treatment is recommended. |
| Nephrotic syndrome | ↑ 3–5× | Optimisation of treatment is recommended. |
| Dialysis therapy | ↑ 2× | Optimisation of treatment is recommended. |
| Chronic liver disease | ↓ | Optimisation of treatment is recommended. |
| Pharmacological interventions | ||
| Tocilizumab | ↓ Up to 40% | No modification of therapy is recommended. |
| Tamoxifen4 | ↓ | No modification of therapy is recommended. |
| Protease inhibitors and/or antiretroviral therapy | ↑ | No modification of therapy is recommended. |
| Statins | ↑ 6–7% | Not clinically relevant. No modification of therapy is recommended. |
Expert opinion: Genetic factors are responsible for approximately 90% of Lp(a) concentrations. The remaining approx. 10 % can be influenced mainly by diet, hormonal disorders or kidney and/or liver disease. There are differences in Lp(a) concentrations between men and women (Lp(a) values are on average up to 10% higher in women, with an additional increase after menopause of up to 30%), depending on race, and to a lesser extent on age. Apart from general prevention principles aimed at changing lifestyle and optimising treatment of comorbidities, there are no additional management recommendations in the context of nongenetic factors for Lp(a).
Who should be tested for Lp(a) and when
The most recent guidelines from the European Atherosclerosis Society (EAS) and the American Heart Association (AHA) recommend that every adult should have their Lp(a) levels determined at least once in their lifetime to identify individuals with very high congenital Lp(a) levels, which significantly increase cardiovascular risk [100, 105] (Table II). It seems that, similarly to the determination of a complete lipid profile in a 6-year-old’s health check-up, which is likely to become possible in Poland in the near future to allow early diagnosis of familial hypercholesterolaemia (FH), Lp(a) testing in childhood also seems reasonable, even though we still essentially lack effective management (beyond monitoring) to successfully lower Lp(a) as early as possible (and studies showing significant benefits of such an intervention).
Table II.
Recommendations for lipoprotein(a) testing
| Recommendations | Class | Level |
|---|---|---|
| Lp(a) concentration is recommended to be determined at least once in the lifetime of every adult. | I | C |
| Lp(a) determination should be considered as early as possible, even in people under 18 years of age, for risk assessment, cascade screening, monitoring and lifestyle modification. | IIa | C |
| Measurement of Lp(a) should be considered in all patients with premature cardiovascular disease, lack of expected effect of statin treatment, and those with a borderline risk between moderate and high, for better risk stratification. | IIa | B |
| Measurement of Lp(a) can be considered in very high-risk patients with atherosclerotic cardiovascular disease, in patients with familial hypercholesterolaemia, and in pregnant women as an assessment of miscarriage risk, in the case of recurrent pregnancy loss and intrauterine growth restriction. | IIb | B |
| More than one Lp(a) measurement may be considered in people with Lp(a) concentrations in the grey zone –- 30–50 mg/dl (75–125 nmol/l), with cut-off values for risk groups (Table III) and/or with risk factors/diseases that may significantly affect Lp(a) concentrations (Table I). | IIb | C |
| It is recommended that re-measurement be performed using a test whose result is expressed in nmol/l (determining the number of Lp(a) molecules) in order to better stratify the risk. | I | C |
| Screening of relatives of individuals with high Lp(a) levels should be considered. | IIa | C |
| If available, apo(a) isoform size and genetic testing may be considered to optimize the risk estimation and response to treatment. | IIb | C |
Hence, for the time being, it is particularly important to determine the level of this lipoprotein in patients with premature cardiovascular disease, in the absence of the intended effect of statin treatment (data indicate that elevated Lp(a) levels can be expected in patients with little or no response to statin treatment [106]), and in those with a borderline risk between moderate and high, for better risk stratification. Measurement of Lp(a) should also be considered in very high cardiovascular risk patients with ASCVD, in patients with FH, and in pregnant women with recurrent pregnancy loss and intrauterine growth restriction as prevention of miscarriage [88].
According to available data, a single accurate measurement of molar Lp(a) concentration appears to be sufficient to estimate cardiovascular risk [107]. However, repeated measurements of the Lp(a) level are recommended in patients whose Lp(a) concentration in the first measurement was 30–50 mg/dl (75–125 nmol/l), i.e. a value in the so-called grey zone or close to the cut-off points for the risk groups (Table III; possibly resulting in a change in the cardiovascular risk of the given patient); ideally, the repeated measurement should be performed using a test whose result is expressed in nmol/l (defining the number of Lp(a) molecules) for better risk stratification [108]. Repeat measurements of Lp(a) may also be considered in patients who have developed chronic kidney disease, particularly nephrotic syndrome, as such conditions can cause a significant increase in Lp(a) [95]. In addition, in women, it is recommended that Lp(a) be re-measured after the age of 50 [73] (Tables I and II).
Table III.
Intervention strategies as a function of total cardiovascular risk and untreated Lp(a) concentration. This table is for reference purposes only, showing that at high Lp(a) values, the risk of a cardiovascular event is significantly underestimated. It also shows that modification of risk factors, such as elevated LDL-C and/or blood pressure, can reduce a person’s overall risk, even if the risk attributable to Lp(a) remains unchanged. To assess the risk associated with elevated Lp(a) and the effects of interventions that reduce Lp(a) and other risk factors, use the calculator available at: http://www.lpaclinicalguidance.com
| Total CV risk excluding Lp(a) (Pol-SCORE) %. | Lp(a) concentration | ||||||
|---|---|---|---|---|---|---|---|
| < 10 mg/dl (< 25 nmol/l) |
10–30 mg/dl (25–75 nmol/l) |
20–50 mg/dl (75–125 nmol/l) |
50–75 mg/dl (125–188 nmol/l) |
75–100 mg/dl (188-250 nmol/l) |
≥ 100 mg/dl (≥ 250 nmol/l) |
||
| Primary prevention | < 1, low risk | Lifestyle changes | Lifestyle changes | Lifestyle changes | Lifestyle changes | Lifestyle changes, pharmacological treatment should be considered* | Lifestyle changes along with concurrent pharmacotherapy |
| ≥ 1 to < 5 or risk moderate | Lifestyle changes | Lifestyle changes | Lifestyle changes | Lifestyle changes, pharmacological treatment should be considered | Lifestyle changes, pharmacological treatment should be considered | Lifestyle changes along with concurrent pharmacotherapy | |
| ≥ 5 to < 10 or risk large | Lifestyle changes | Lifestyle changes | Lifestyle changes, pharmacological treatment should be considered | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | |
| ≥ 10 or risk very large | Lifestyle changes | Lifestyle changes, pharmacological treatment should be considered | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | |
| Secondary prevention | Very high risk | Lifestyle changes, pharmacological treatment should be considered | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy | Lifestyle changes along with concurrent pharmacotherapy |
Pharmacotherapy refers to the optimal treatment of risk factors, related to LDL cholesterol levels, blood pressure, glucose levels. Prepared on the basis of [100].
These recommendations are particularly important because recent results from the OCEAN (a)-Dose study indicate significant long-term individual variability in Lp(a) levels in patients with ASCVD and elevated baseline Lp(a) concentrations, suggesting that it may be necessary to measure this parameter more than once in a lifetime [109]. The study authors observed as much as 10% (SD 3.9%) mean variation in Lp(a) concentration. The absolute differences observed over time in the placebo group at all visits averaged 22 ±21 nmol/l (9 ±8.5 mg/dl), with a maximum absolute difference of up to 135 nmol/l (54 mg/dl).
According to the European Atherosclerosis Society (EAS) consensus published in 2022 and the American Heart Association (AHA) guidelines, screening of relatives of people with high Lp(a) levels is recommended [100, 105]. A recently published UK Biobank cross-sectional study confirmed that the effectiveness of cascade screening of first-degree relatives of people with high Lp(a) levels, is over 40% [110]. Screening is also recommended in young people with a history of ischaemic stroke or a family history of early ASCVD or high Lp(a), without other identifiable risk factors. Cascade testing for high Lp(a) is recommended in cases of familial hypercholesterolaemia, a family history of high Lp(a) and personal or family history of ASCVD [100].
How often is the Lp(a) concentration tested?
Elevated Lp(a) levels > 50 mg/dl (> 125 nmol/l) are estimated to occur in more than 1.4 billion people worldwide [9]. In Europe, approximately 20% of women and 20% of men have Lp(a) levels > 50 mg/dl (> 125 nmol/l) [88,100], and up to >30% of patients with ASCVD and/or FH may have elevated Lp(a), however, Lp(a) levels are still unfortunately not commonly determined [111]. The EAS, as part of the Lipid Clinic Network (LCN) project, conducted a survey to find out how widespread routine testing of Lp(a) levels is. The survey was completed by 151 clinicians and 75.5% of the respondents declared that they routinely measure Lp(a) in clinical practice. However, across all the European centres surveyed, the results varied widely; in Western European countries, ~90% of clinicians reported that they routinely order Lp(a) measurements, while in Central and Eastern European countries, the figure was ~49% [10]. It is also worth noting that these data are definitely overestimated, as they were conducted among physicians working in specialised lipidology centres.
A study of more than 5 million adults at six academic medical centres affiliated with the University of California in the United States found that the frequency of Lp(a) determination remains very low at 0.3%, with a 4% prevalence among patients with cardiovascular diseases [11]. A study including all adults (4.6 million) registered with the largest health organisation in Israel showed that only 0.1% had their Lp(a) levels tested between 2015 and 2021 [12].
Difficulties in determining Lp(a) concentration
Determination of Lp(a) concentration is not easy, as different results can be obtained depending on the assay chosen, which is partly dependent on the size of the apo(a) isoform [100, 112, 113]. Commercially available tests for the determination of Lp(a) concentrations are immunoenzymatic assays using polyclonal antibodies against apo(a). These assays are more or less sensitive to apo(a) isoforms and therefore the determined Lp(a) concentration can potentially be underestimated for small isoforms or overestimated when large isoforms are present. For accurate determination of Lp(a) concentration, assays based on antibodies directed against the unique apo(a) kringle V domain should be used, which would allow each Lp(a) molecule to be recognised only once [100, 114].
Isoform-sensitive tests report the mass of Lp(a) particles (mg/dl), while isoform-insensitive tests report the molar concentration (nmol/l) of the number of apo(a) particles. The use of a standard factor to convert units from mg/dl to nmol/l is inaccurate and therefore not recommended for use by clinicians [115], although, due to existing differences in the tests used, it is still widely practised (the most common conversion factor is: nmol/l = 0.4 × mg/dl and mg/dl = 2.5 × nmol/l). Recent results from a sub-analysis of the ODYSSEY Outcomes study with alirocumab, in which Lp(a) was measured with three different assays (using immunoenzymatic mass assays, molar assays and molar mass spectrometry-based assays), showed a similar risk reduction regardless of the Lp(a) concentration measurement used [116].
Recently, a mass spectrometric method has been developed and validated for the standardisation of Lp(a) measurements, which addresses the problem of size polymorphisms by selecting specific peptides for quantification that are not present in the KIV2 region [117]. Research is also currently underway on the global standardisation of Lp concentration measurements, which will improve diagnostic interpretation and clinical decision-making regarding Lp(a)-dependent CVD risk [117, 118].
Which concentrations indicate increased cardiovascular risk?
The relationship between Lp(a) concentration and cardiovascular risk is linear, meaning that the risk is higher with increasing Lp(a) concentration [45]. There is a need on the part of clinicians to define a threshold Lp(a) concentration at which cardiovascular risk increases. The Lp(a) level that requires appropriate clinical intervention is ≥ 30 mg/dl (≥ 75 nmol/l) (Table IV) [100]. Individuals whose Lp(a) level is between 30 and 50 mg/dl (75–125 nmol/l) belong to the so-called grey zone, which depends both on the accuracy of the test used to assess Lp(a) levels, but also on all risk factors of the individual patient [100]. However, these individuals already have an increased risk of adverse effects and should be classified as being at moderate risk. High risk is predicted for all patients with Lp(a) concentrations > 50 mg/dl (> 125 nmol/l) and actually for the concentration range 50–180 mg/dl (125–450 nmol/l), while very high risk for values > 180 mg/dl (450 nmol/l).
Table IV.
Classification of Lp(a) concentrations according to cardiovascular risk category. Modified from [88]
| Target value | Elevated values | |
|---|---|---|
| Lipoprotein(a) | < 30 mg/dl (75 nmol/l) | 30–50 mg/dl (75–125 nmol/l) moderate risk |
| > 50 mg/dl – 180 mg/dl (>125 nmol/l – 450 nmol/l) high risk | ||
| > 180 mg/dl (> 450 nmol/l) very high cardiovascular risk |
How to stratify risk
Widely used cardiovascular risk assessment tools for primary prevention do not take Lp(a) levels into account. In 2021, the Polish guidelines of six scientific societies for the management of lipid disorders for the first time used an elevated Lp(a) concentration > 50 mg/dl (125 nmol/l) as an additional parameter defining extremely high cardiovascular risk in a patient after an acute coronary syndrome (ACS) with diabetes [88]. If the Lp(a) concentration is high but not included in the risk calculation, then the calculated risk of CVD events is significantly underestimated [43]. Based on an analysis of UK biobank data, the EAS consensus showed that people with Lp(a) levels of 30 (75 nmol/l), 50 (125 nmol/l), 75 (187.5 nmol/l), 100 (250 nmol/l) and 150 mg/dl (375 nmol/l) compared to those with an average Lp(a) concentration of 7 mg/dl (17.5 nmol/l) have an increased cardiovascular risk of 1.22; 1.40; 1.65, 1.95 and 2.72, respectively. Thus, if the baseline risk is 25% and in addition there is a high Lp(a) level of e.g. 150 mg/dl (375 nmol/l) then the risk increases from 25% to 68% [43, 100].
The EAS, in its 2022 recommendations, switched to a new and extremely useful risk assessment calculator that takes into account Lp(a) levels in combination with traditional cardiovascular risk factors (Table III) (http://www.lpaclinicalguidance.com/) [43, 100]. This calculator estimates the risk of myocardial infarction or stroke up to the age of 80 years, with or without consideration of Lp(a) levels.
Currently available therapies affecting Lp(a) levels
Currently available lipid-lowering medicines have an effect on Lp(a) concentrations, but their efficacy in this respect varies and is mostly insufficient (Table V).
Table V.
Effect of currently available hypolipemic therapies on Lp(a) levels
| Intervention | Effect on Lp(a) levels |
|---|---|
| Statins | Possible ↑ by 6–10% |
| Ezetimibe | ↓ Up to 7% |
| Bempedoic acid | No effect |
| Alirocumab | ↓ 25–35% |
| Evolocumab | ↓ 25–35% |
| Inclisiran | ↓ 20–25% |
| Niacin | ↓ 30–40% |
| Lp(a) apheresis | ↓ 25–40% |
In the case of statins, there are conflicting findings regarding their effect on Lp(a) levels. Some studies have shown that statins are effective in lowering Lp(a) levels [119, 120], while others have indicated an increase in Lp(a) of 10–20% [121, 122]. There are also studies showing no effect of statins on Lp(a) levels [123]. Besides, the effect on Lp(a) may vary depending on the type of statins [124]. The discrepancy in study results may be explained by the fact that statins affect Lp(a) levels differently in dyslipidaemic patients, depending on the apo(a) phenotype. Statins only increase Lp(a) levels in patients with a low molecular weight (LMW) apo(a) phenotype (≤ 22 KIV), and in these individuals a mean absolute increase of up to > 30 mg/dl (> 40%) can be observed [125].
Statin-induced increases in Lp(a) levels are not clinically relevant and there are no recommendations to discontinue statin treatment in patients with high Lp(a) levels [43, 88, 100, 125]. A meta-analysis of 20 randomised clinical trials involving 23,605 participants showed that atorvastatin showed a slightly worse effect on Lp(a) levels compared to other statins, whereas pitavastatin could potentially reduce Lp(a) levels [126]. This was also confirmed by the results of the VISION study, indicating no effect of pitavastatin on Lp(a) and even a numerical reduction in Lp(a) levels [127]. A possible change from statin to pitavastatin in patients with elevated Lp(a) needs to be confirmed in further studies. In the just-published recommendations of Polish experts, they indicate the possibility of considering pitavastatin in patients with elevated Lp(a) (IIb) concentrations, while emphasising the need for further studies confirming this relationship, as well as assessing the effect of pitavastatin on the size of apolipoprotein(a) isoforms [128].
Ezetimibe has a neutral effect or may cause a slight reduction in Lp(a) although probably not clinically relevant [129]. Similarly, bempedoic acid has been shown to have no clinically significant effect on Lp(a) concentrations [130]. This does, however, imply, in the case of statin-induced increases in Lp(a) concentrations, that combination therapy with a lower dose of statins may be optimal in this group of individuals, although further studies are needed to corroborate the effect of such treatment on Lp(a) concentrations and risk reduction.
The FOURIER and ODYSSEY OUTCOMES studies showed that PCSK9 inhibitors reduced Lp(a) levels: evolocumab by a mean of 29.5% [131, 132] and alirocumab by a mean of 23.5% [133]. Based on sub-analyses of the FOURIER and ODYSSEY OUTCOMES clinical trials, absolute CVD risk reductions from 2.4% to 3.7% (ARR 1.3%, number needed to treat [NNT] = 77) were demonstrated (as an effect of the reduction of Lp(a) concentration) [134]. Another analysis of the same study suggests that the reduction in Lp(a) resulting from the use of alirocumab may also significantly reduce the risk of PAD [135]. A study that assessed the effect of early initiation of evolocumab therapy on Lp(a) levels after primary percutaneous coronary intervention (PCI) in patients with myocardial infarction showed that early initiation of evolocumab in combination with pitavastatin rapidly inhibited the increase in Lp(a) levels compared with pitavastatin alone. Evolocumab (PCSK9 inhibitors) may partially attenuate statin-induced increases in Lp(a) levels, suggesting its benefit in managing residual risk in patients with elevated Lp(a) levels after myocardial infarction [136]. The reduction in Lp(a) as a result of PCSK9i administration is achieved through a dual mechanism involving both increased catabolism and reduced Lp(a) production [137]. In comparison, available data on therapy based on an RNA interference mechanism, based on the results of the ORION 10 and ORION 11 studies, showed a reduction in Lp(a) by ~20% following the administration of inclisiran [138, 139].
It is noteworthy that apo(a) size is an independent determinant of the response to PCSK9i in terms of Lp(a) reduction. The presence of each additional kringle domain is associated with an increased Lp(a) reduction of 3%; in other words, the larger the size of the dominant apo(a) isoform, the greater the relative Lp(a) reduction. This partly explains the variable efficacy of PCSK9i and allows individualisation of therapy by identifying those patients who will benefit most from Lp(a) reduction [140].
It is worth noting that in the B101 drug programme in Poland there is no indication for the use of PCSK9 protein modulators to reduce Lp(a) levels, just like in most European countries [88, 100]. It is possible to use PCSK9 protein modulators to reduce elevated Lp(a) concentrations if the patient simultaneously meets other applicable programme criteria, or as part of the rescue access to drug technology (RDTL) procedure, which is certainly used definitely too rarely in Poland.
Current data suggest that niacin, which is a medicine unfortunately not available in Poland or Europe, may have a beneficial effect on Lp(a) levels [108]. Niacin can reduce Lp(a) in a dose-dependent manner by an average of 30–40% and by about 20% in those with the highest Lp(a) levels [88, 141]. Niacin can be used in combination with statin therapy. It was shown that in individuals with Lp(a) levels above 300 nmol/l (120 mg/dl), the reduction in Lp(a) during niacin treatment was 63% compared to a 3.9% reduction with statin therapy. Genetic studies revealed a specific variant of the LPA promoter gene that appeared to increase the efficacy of niacin treatment [142]. The effect of niacin on Lp(a), similarly to other lipid-lowering drugs, was also shown to be dependent on the size of the apo(a) isoform [143]. The use of niacin reduced Lp(a) levels by 28% and lipoprotein-associated phospholipase A2 (Lp-PLA2) levels by 22% in the low molecular weight (LMW) apo(a) group, while no significant changes in Lp(a) levels were observed in the high molecular weight (HMW) apo(a) isoform group [144]. Another study that analysed the effect of niacin on Lp(a) found that the largest apo(a) isoform sizes (corresponding to lower Lp(a) levels) resulted in a 50% and 4 nmol/l reduction in Lp(a) in absolute terms, while the smallest apo(a) isoform sizes (corresponding to higher Lp(a) levels) showed a reduction in Lp(a) of 16% and 30 nmol/l in absolute terms [141] – a similar effect is observed for PCSK9 inhibitors. Due to the emergence of studies demonstrating a lack of clinical benefit from the use of niacin and the risk of adverse effects [145–147], current EAS and Polish guidelines do not recommend its use [88, 100].
The results of the above studies suggest that genetic testing and phenotyping should be ordered in patients with elevated Lp(a) levels, which could serve as an additional tool to assess CVD risk, to personalise and select the best available therapy (statins, niacin, PCSK9 inhibitors) [142, 143]. However, currently available techniques for the determination of apo(a) isoforms are complex, expensive and their availability is still very limited [148].
Lipoprotein apheresis is an efficient and effective therapeutic option for lowering Lp(a) levels [149, 150]. A single apheresis treatment reduces Lp(a) by approximately 60–75%, and regular treatments every 1–2 weeks reduce Lp(a) by approximately 25–40% compared to baseline values [151–153]. Studies have shown that the use of lipoprotein apheresis in patients with ASCVD and elevated Lp(a) levels results in a significant reduction in CVD events. A prospective multicentre study of 170 patients with ASCVD and Lp(a) > 60 mg/dl (> 150 nmol/l) showed a significant reduction in the annual rate of MACE after implementation of apheresis therapy [154]. Data from the German Lipoprotein Apheresis Registry (GLAR) in ASCVD patients with elevated Lp(a) levels showed a 72.4% reduction in Lp(a) and a significant reduction in the incidence of ASCVD events (> 80%) over 7 years, regardless of baseline LDL-C levels [155]. A US study observed a 63% reduction in Lp(a) and a 94% reduction in major adverse cardiovascular events (MACE) over a mean lipoprotein apheresis treatment period of 48 months [156]. A study in Polish patients showed a 73% reduction in Lp(a) levels and a significant reduction in CV incidents [157]. In addition, an additional effect of changes in the fatty acid profile was observed [158]. In a randomised trial in patients with refractory angina and Lp(a) > 50 mg/dl (> 125 nmol/l), lipoprotein apheresis improved myocardial perfusion on MRI, physical performance in the 6-minute walk test and quality of life [159]. However, there has not yet been a randomised trial evaluating the use of lipoprotein apheresis in patients with high Lp(a) levels, targeting cardiovascular incident analysis [160].
Lipoprotein apheresis is the first treatment for elevated Lp(a) to receive initial Food and Drug Administration (FDA) approval for use in patients with Lp(a) > 60 mg/dl (> 150 nmol/l) regardless of baseline LDL-C levels [160]. Lipoprotein apheresis may be considered in patients with very high Lp(a) levels and progressive ASCVD despite optimal treatment of other risk factors [100]. Apheresis is a safe, effective method; however, it is invasive, costly and of limited availability. The most common (relatively rare – 3–6% and mostly mild to moderate) side effects include puncture site lesions (mainly peripheral veins), transient hypotonia and hypocalcaemia [161].
Mipomersen (antisense oligonucleotide [ASO] – targeting apo(B) mRNA) is able to lower Lp(a) in the range of 21–27% [162–164], but its safety profile limits its use to people with homozygous FH and it is not suitable for routine administration to lower Lp(a) levels [165]. This medicine is not available in Poland.
Current therapies used to lower LDL-C have a moderate effect on Lp(a). Reducing the risk of major adverse cardiovascular events may require greater reductions in Lp(a) with more potent and targeted therapies which are still undergoing clinical trials (Tables VI–VIII).
Table VI.
Recommendations for the management of elevated Lp(a) concentrations
| Recommendations | Class | Level |
|---|---|---|
| It is recommended to test the Lp(a) concentration using a method that assesses the number of Lp(a) molecules (in nmol/l) and is insensitive to the number of kringle IV-2 repeats (KIV-2). | I | C |
| If an elevated Lp(a) level is found, it is recommended that each patient be reassessed for cardiovascular risk using the algorithm proposed in Table III recommended risk calculator, followed by an appropriate modification of treatment. | I | C |
| If an elevated Lp(a) level is found in a patient for primary prevention, a CT scan of the coronary arteries with assessment of the coronary artery calcification (CAC) score should be considered for more appropriate risk stratification. | IIa | B |
| If elevated Lp(a) levels are found in high- and very high-risk patients, a switch from statin monotherapy to a combination treatment of lower-dose statins and ezetimibe or triple therapy with PCSK9 protein modulators (depending on cardiovascular risk and therapeutic goal) may be considered. | IIb | C |
| Lipoprotein apheresis should be considered in patients with clinically or imaging-confirmed progressive cardiovascular disease despite optimal control of all other risk factors and Lp(a) levels ≥ 60 mg/dl (≥ 150 nmol/l) (irrespective of LDL-C levels). | IIa | B |
Table VIII.
New Lp(a)-lowering medicines under clinical development
| Name of medicine | Class | Reduction of Lp(a) | Clinical trial phase | Manufacturer |
|---|---|---|---|---|
|
Pelacarsen (TQJ230; IONIS-APO(a)-LRX, AKCEA-APO(a)-LRX, ISIS 681257) |
ASO | > 70% | III | Novartis Pharmaceuticals |
|
Olpasiran (AMG-890, ARO-LPA) |
siRNA | 71–97% | III | Amgen, Arrowhead Pharmaceuticals |
| Zerlasiran (SLN360) | siRNA | 96–98% | II | Silence Therapeutics plc |
| Lepodisiran (LY3819469) | siRNA | 96–97% | II | Eli Lilly and Company |
| Muvalaplin (LY3473329) | Lp(a) inhibitor | 63–65% | II | Eli Lilly and Company |
| Obicetrapib (TA-8995) | CETP inhibitor | ~50% | III | NewAmsterdam Pharma |
ASO – antisense oligonucleotides, siRNA – small interfering RNAs, CETP – cholesterol ester transport proteins.
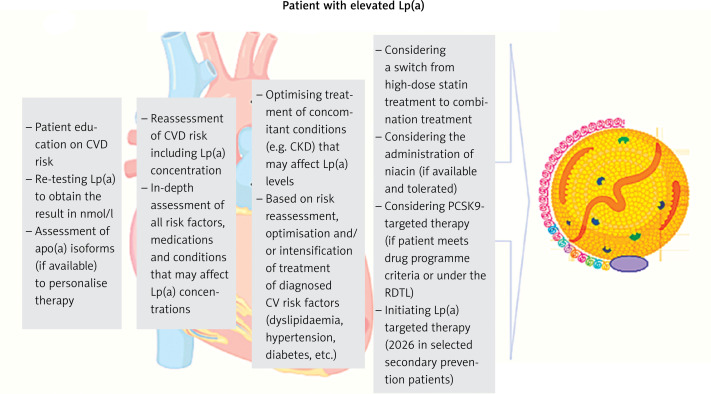
Management of elevated Lp(a) concentrations
Currently, there are no approved medicines targeting the lowering of Lp(a) concentrations, and therefore, with elevated Lp(a) values, the recommended management is aimed at lowering overall risk through lifestyle changes, and intensive treatment or optimisation of treatment of other risk factors that can be effectively treated according to current recommendations (Figure 3 and Table V) [88, 100]).
Figure 3.
Recommended management pathway for patients with elevated Lp(a) levels. Modified from [108]
CVD – cardiovascular, Lp(a) – lipoprotein(a), RDTL – rescue access to drug technology.
Lifestyle changes have a minimal effect on Lp(a), but significantly affect overall cardiovascular risk, optimising blood pressure and concentrations of lipids and glucose, significantly reducing long-term ASCVD risk [88, 166].
A small increase in Lp(a) after treatment with statins does not seem to be clinically relevant. According to recent recommendations by Polish experts, a change from statin to pitavastatin can be considered in patients with elevated Lp(a), but further studies are still needed to confirm this effect, especially in terms of the impact on cardiovascular risk reduction. In the case of elevated Lp(a) values, a change from statin treatment to a combination treatment of statins with available medicines – ezetimibe or a combination of ezetimibe and bempedoic acid (to be available from 2024 in Poland) and a combination treatment based on inhibition of the PCSK9 protein should be considered (Tables VI and VII) [167]. Lipoprotein apheresis may be considered in patients with very high Lp(a) levels (≥ 60 mg/dl [≥ 150 nmol/l]) and progressive ASCVD, despite optimal treatment of other cardiovascular risk factors [100] (Tables VI, VII).
Table VII.
Practical recommendations for the management of patients from different risk groups with elevated Lp(a) levels > 50 mg/dl (> 125 nmol/l).1 Treatment based on a fixed-dose combination tablet (FDC) is preferred2 for both primary and secondary prevention3 under the B101 drug programme or the rescue access to drug technology (RDTL) procedure
| Patient groups | Suggested procedure |
|---|---|
| Patient aged > 40 years with low or moderate cardiovascular risk not previously treated. | Lifestyle changes, optimisation of management of other cardiovascular risk factors, consideration of low-dose statin administration. |
| High-risk patient treated with a statin. | Lifestyle changes, optimisation of the management of other cardiovascular risk factors, intensification of statin treatment; addition of ezetimibe1 may be considered. |
| Patient at very high cardiovascular risk2 treated with maximum statin dose. | Lifestyle changes, optimisation of management of other cardiovascular risk factors, immediate maximum-dose statin combination therapy with ezetimibe, consideration of PCSK9 protein modulators addition3. |
| Patient with progressive cardiovascular disease confirmed clinically or by imaging, despite optimal control of all other risk factors and persistent Lp(a) ≥ 60 mg/dl (≥ 150 nmol/l) (irrespective of LDL-C level). | Lifestyle changes, optimisation of management of other cardiovascular risk factors, immediate maximum-dose statin combination therapy with ezetimibe, consideration of PCSK9 protein modulators3 addition, consideration of Lp(a) apheresis. |
Management of asymptomatic patients with high Lp(a) levels involves a recommendation of changes in modifiable risk factors through lifestyle changes and treatment according to guidelines. Assessment of the coronary artery calcification (CAC) score can be considered as early as in patients at 45–50 years of age, a low score, or zero, helps to reduce patient concerns about elevated Lp(a) levels. A family history of (premature) ASCVD should be checked, and family screening for high Lp(a) should be suggested. For some patients, referral to a lipid clinic or outpatient specialist care (AOS) should be considered [88, 100].
Future targeted Lp(a) lowering therapies
The strong association between Lp(a) and cardiovascular risk has contributed to the development of new medicines aimed at reducing Lp(a) levels (Table VIII) [168]. Medicines targeting Lp(a) reduction are mainly RNA-based therapies, including antisense oligonucleotides (ASOs) and small interfering RNAs (siRNAs), which allow selective silencing of the LPA gene. The mechanism of action of ASOs and siRNAs is to reduce Lp(a) levels by inhibiting apo(a) protein synthesis.
Pelacarsen, a second-generation antisense oligonucleotide, is covalently bound to N-acetylgalactosamine (GalNAc), which provides uptake via asialoglycoprotein receptors located on hepatocytes, thus improving the potency and safety of the medicine. Previous studies have shown that the medicine was well tolerated and resulted in a 72% and 80% reduction in Lp(a) levels, depending on the dose of 60 mg every 4 weeks and 20 mg every week, respectively [169]. The reduction in Lp(a) was independent of LPA genetic variants and isoform size [170]. Currently, pelacarsen, administered at a dose of 80 mg administered subcutaneously once a month, is in a phase 3 clinical trial determining the effect of the medicine on reducing the risk of cardiovascular events (Lp(a)HORIZON trial, NCT04023552). Anticipated study completion date is May 2025 [168].
Olpasiran (AMG-890), Zerlasiran (SLN360) and Lepodisiran (LY3819469) are GalNAc-conjugated siRNAs administered subcutaneously. Olpasiran resulted in a dose-dependent reduction in Lp(a) ranging from 71% to 97% [171]. It is currently in a phase 3 clinical trial (Ocean(a) study, NCT05581303) with an expected study completion date of December 2026. The results, which can be expected in 2027, will provide new information on the pharmacokinetic and pharmacodynamic properties of olpasiran, the best dosing and its effect on cardiovascular events.
Zerlasiran at the two highest single doses of 300 mg and 600 mg reduced Lp(a) levels by 96% and 98%, respectively, and plasma Lp(a) levels were still significantly reduced (by 70% and 81%, respectively) 150 days after administration [172]. A randomised, placebo-controlled phase II study (NCT05537571) has recently commenced, enrolling 160 high-risk ASCVD participants with Lp(a) levels above 125 nmol/l (50 mg/dl). The aim of this study is to investigate the safety, efficacy, and tolerability profile of zerlasiran, with an estimated completion date of June 2024 [173].
Lepodisiran is in early-stage trials. Phase I clinical trial (NCT04914546) is now completed, which involved 48 adults without CVD and with Lp(a) levels ≥ 75 nmol/l (or ≥ 30 mg/dl) [174]. After 168 days, the greatest reductions in Lp(a) concentrations were achieved for the subcutaneously administered single dose of 304 mg –96% and 608 mg – 97%. At day 337, the median change in Lp(a) concentration was –94% in the group receiving 608 mg lepodisiran. A phase 2, placebo-controlled study (NCT05565742) is currently underway that will evaluate the efficacy and safety of lepodisiran in 254 participants with Lp(a) levels above 175 nmol/l (70 mg/dl) over 20 months. The study is expected to end in October 2024 [175].
Muvalaplin (LY3473329) is a selective small-molecule inhibitor of Lp(a) synthesis taken orally that inhibits Lp(a) formation by blocking the apo(a)-apo B100 interaction, while avoiding interaction with the homologous protein plasminogen. Results from a phase I study (NCT04472676) showed that it was well tolerated and produced a maximum reduction in Lp(a) of 63% to 65% [176]. A phase II study (KRAKEN trial, NCT05563246) is currently underway to evaluate the efficacy and safety of muvalaplin in adult participants with elevated Lp(a) levels (≥ 175 nmol/l; 70 mg/dl) at high risk of cardiovascular events. The study is scheduled for completion in January 2024 [177].
Obicetrapib is a next-generation selective cholesteryl ester transporter protein (CETP) inhibitor, currently in clinical trials for reducing both LDL-C levels and the incidence of major adverse cardiovascular events. A randomised, double-blind, placebo-controlled trial in dyslipidaemic patients (the ROSE trial, NCT04753606) showed that obicetrapib at oral doses of 5 mg and 10 mg, compared with placebo, as an adjunct to intensive statin therapy (40 mg or 80 mg of atorvastatin or 20 mg or 40 mg of rosuvastatin) resulted in reductions in Lp(a) of 33.8% and 56.5%, respectively [178] (Table VIII).
Acknowledgments
This expert document was written on the initiative of the experts of two scientific societies, the Polish Cardiac Society (PTK) and the Polish Lipid Society (PTL), without any additional funding. No additional person outside the group of invited experts (medical writers) participated in the writing of this document.
After final approval of the content, the recommendations will be simultaneously published in the Archives of Medical Science (indicated by PoLA), and Zeszyty Edukacyjne of the Polish Heart Journal (indicated by PCS) to reach as many interested parties as possible.
Conflict of interest
Przemysław Mitkowski – remuneration for lectures/advisory panels from Novartis, Sanofi, Amgen; Agata Bielecka-Dąbrowa – remuneration for lectures from Novartis; Beata Bobrowska – collaborated as consultant and received remuneration for lectures from Amgen, Exceed Orphan, Novartis, Polpharma, Sanofi; Pawel Burchardt – remuneration for lectures from Amgen, Novartis, Sanofi, Sandoz, Teva; Piotr Dobrowolski – remuneration for lectures/advisory panels from: Amgen, Sanofi, Novartis; Piotr Jankowski – remuneration for lectures from: Amgen, Novartis, Sanofi; Jacek Kubica – remuneration for lectures from: Amgen, Novartis, Sanofi; Agnieszka Mickiewicz – remuneration for lectures from Novartis, Amgen, Sanofi, Fresenius Medical Care; Aleksander Prejbisz – participation in a clinical trial funded by Amgen; Renata Rajtar-Salwa – consultant/remuneration for lectures from Amgen, Sanofi, Novartis, Exceed Orphan, Polfarma; Adam Witkowski – advisory panels and remuneration for lectures form Novartis and Sanofi; Robert Gil – remuneration from lectures from Novartis, Amgen, Sanofi; Maciej Banach – remuneration for lectures from Adamed, Amgen, Daiichi Sankyo, Exceed Orphan, KRKA, Polpharma, Mylan/Viatris, Novartis, Novo-Nordisk, Pfizer, Sanofi, Teva, Zentiva; participation in advisory panels for Adamed, Amgen, Daiichi Sankyo, Esperion, NewAmsterdam, Novartis, Novo-Nordisk, Sanofi; grants from: Amgen, Daiichi Sankyo, Mylan/Viatris, Sanofi; other authors reported no conflict of interest.
References
- 1.Berg K. A New serum type system IN MAN--THE LP system. Acta Pathol Microbiol Scand 1963; 59: 369–382. [DOI] [PubMed] [Google Scholar]
- 2.Cybulska B, Kłosiewicz-Latoszek L, Penson PE, Banach M. What do we know about the role of lipoprotein(a) in atherogenesis 57 years after its discovery? Prog Cardiovasc Dis 2020; 63: 219–27. [DOI] [PubMed] [Google Scholar]
- 3.Arsenault BJ, Kamstrup PR. Lipoprotein(a) and cardiovascular and valvular diseases: a genetic epidemiological perspective. Atherosclerosis 2022; 349: 7–16. [DOI] [PubMed] [Google Scholar]
- 4.Singh S, Baars DP, Desai R, Singh D, Pinto-Sietsma SJ. Association between lipoprotein (a) and risk of atrial fibrillation: a systematic review and meta-analysis of mendelian randomization studies. Curr Probl Cardiol 2023; 49: 102024. [DOI] [PubMed] [Google Scholar]
- 5.Yang M, Nasr B, Liu J, Du Y, Yang J. The association between lipoprotein(a) and atrial fibrillation: a systemic review and meta-analysis. Clin Cardiol 2023; 46: 899–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masson W, Barbagelata L, Nogueira JP, Corral P, Lavalle-Cobo A, Romeo FJ. Elevated lipoprotein(a) levels and atrial fibrillation: a systematic review. J Lipid Atheroscler 2023; 12: 267–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boffa MB, Marar TT, Yeang C, et al. Potent reduction of plasma lipoprotein (a) with an antisense oligonucleotide in human subjects does not affect ex vivo fibrinolysis. J Lipid Res 2019; 60: 2082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Maio S, Lamina C, Coassin S, et al. Lipoprotein(a) and SARS-CoV-2 infections: susceptibility to infections, ischemic heart disease and thromboembolic events. J Intern Med 2022; 291: 101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsimikas S, Marcovina SM. Ancestry, lipoprotein(a), and cardiovascular risk thresholds: the JACC review topic of the week. J Am Coll Cardiol 2022; 80: 934–46. [DOI] [PubMed] [Google Scholar]
- 10.Catapano AL, Tokgözoğlu L, Banach M, et al. ; Lipid Clinics Network Group . Evaluation of lipoprotein(a) in the prevention and management of atherosclerotic cardiovascular disease: a survey among the Lipid Clinics Network. Atherosclerosis 2023; 370: 5–11. [DOI] [PubMed] [Google Scholar]
- 11.Bhatia HS, Hurst S, Desai P, Zhu W, Yeang C. Lipoprotein(a) testing trends in a large academic health system in the United States. J Am Heart Assoc 2023; 12: e031255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zafrir B, Aker A, Saliba W. Lipoprotein(a) testing in clinical practice: real-life data from a large healthcare provider. Eur J Prev Cardiol 2022; 29: e331–3. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt K, Noureen A, Kronenberg F, Utermann G. Structure, function, and genetics of lipoprotein (a). J Lipid Res 2016; 57: 1339–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koschinsky ML, Beisiegel U, Henne-Bruns D, Eaton DL, Lawn RM. Apolipoprotein(a) size heterogeneity is related to variable number of repeat sequences in its mRNA. Biochemistry 1990; 29: 640–4. [DOI] [PubMed] [Google Scholar]
- 15.Kostner KM, März W, Kostner GM. When should we measure lipoprotein (a)? Eur Heart J 2013; 34: 3268–76. [DOI] [PubMed] [Google Scholar]
- 16.Kronenberg F, Utermann G. Lipoprotein(a): resurrected by genetics. J Intern Med 2013; 273: 6–30. [DOI] [PubMed] [Google Scholar]
- 17.Koschinsky ML, Côté GP, Gabel B, van der Hoek YY. Identification of the cysteine residue in apolipoprotein(a) that mediates extracellular coupling with apolipoprotein B-100. J Biol Chem 1993; 268: 19819–25. [PubMed] [Google Scholar]
- 18.Becker L, Cook PM, Wright TG, Koschinsky ML. Quantitative evaluation of the contribution of weak lysine-binding sites present within apolipoprotein(a) kringle IV types 6-8 to lipoprotein(a) assembly. J Biol Chem 2004; 279: 2679–88. [DOI] [PubMed] [Google Scholar]
- 19.Harpel PC, Gordon BR, Parker TS. Plasmin catalyzes binding of lipoprotein (a) to immobilized fibrinogen and fibrin. Proc Natl Acad Sci USA 1989; 86: 3847–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leibundgut G, Scipione C, Yin H, et al. Determinants of binding of oxidized phospholipids on apolipoprotein(a) and lipoprotein (a). J Lipid Res 2013; 54: 2815–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Enkhmaa B, Anuurad E, Berglund L. Lipoprotein (a): impact by ethnicity and environmental and medical conditions. J Lipid Res 2016; 57: 1111–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borrelli MJ, Youssef A, Boffa MB, Koschinsky ML. New frontiers in Lp(a)-targeted therapies. Trends Pharmacol Sci 2019; 40: 212–25. [DOI] [PubMed] [Google Scholar]
- 23.Jawi MM, Frohlich J, Chan SY. Lipoprotein(a) the insurgent: a new insight into the structure, function, metabolism, pathogenicity, and medications affecting lipoprotein(a) molecule. J Lipids 2020; 2020: 3491764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koschinsky ML, Kronenberg F. The long journey of lipoprotein(a) from cardiovascular curiosity to therapeutic target. Atherosclerosis 2022; 349: 1–6. [DOI] [PubMed] [Google Scholar]
- 25.Siekmeier R, Scharnagl H, Kostner GM, Grammer T, Stojakovic T, März W. Lipoprotein (a) – structure, epidemiology, function and diagnostics of a cardiovascular risk marker. Open Clin Chem J 2008; 1: 79–91. [Google Scholar]
- 26.Sharma M, Redpath GM, Williams MJ, McCormick SP. Recycling of apolipoprotein(a) after PlgRKT-mediated endocytosis of lipoprotein(a) Circ Res 2017; 120: 1091–102. [DOI] [PubMed] [Google Scholar]
- 27.Tsimikas S. A test in context: lipoprotein(a): diagnosis, prognosis, controversies, and emerging therapies. J Am Coll Cardiol 2017; 69: 692–711. [DOI] [PubMed] [Google Scholar]
- 28.Tsimikas S, Fazio S, Ferdinand KC, et al. NHLBI Working Group recommendations to reduce lipoprotein(a)-mediated risk of cardiovascular disease and aortic stenosis. J Am Coll Cardiol 2018; 71: 177–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taleb A, Witztum JL, Tsimikas S. Oxidized phospholipids on apoB-100-containing lipoproteins: a biomarker predicting cardiovascular disease and cardiovascular events. Biomarkers Med 2011; 5: 673–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Der Valk FM, Bekkering S, Kroon J, et al. Oxidized phospholipids on lipoprotein(a) elicit arterial wall inflammation and an inflammatory monocyte response in humans. Circulation 2016; 134: 611–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsimikas S, Witztum JL. Oxidized phospholipids in cardiovascular disease. Nat Rev Cardiol 2023. Oct 17. doi: 10.1038/s41569-023-00937-4. [DOI] [PubMed] [Google Scholar]
- 32.Yeang C, Wilkinson MJ, Tsimikas S. Lipoprotein(a) and oxidized phospholipids in calcific aortic valve stenosis. Curr Opin Cardiol 2016; 31: 440–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boffa MB, Koschinsky ML. Lipoprotein(a): truly a direct prothrombotic factor in cardiovascular disease? J Lipid Res 2016; 57: 745–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee SR, Prasad A, Choi YS, et al. LPA gene, ethnicity, and cardiovascular events. Circulation 2017; 135: 251–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Donoghue ML, Morrow DA, Tsimikas S, et al. Lipoprotein(a) for risk assessment in patients with established coronary artery disease. J Am Coll Cardiol 2014; 63: 520–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paré G, Çaku A, McQueen M, et al. Lipoprotein(a) levels and the risk of myocardial infarction among 7 ethnic groups. Circulation 2019; 139: 1472–82. [DOI] [PubMed] [Google Scholar]
- 37.Kamstrup PR, Tybjærg-Hansen A, Nordestgaard BG. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J Am Coll Cardiol 2014; 63: 470–7. [DOI] [PubMed] [Google Scholar]
- 38.Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA 2009; 301: 2331–9. [DOI] [PubMed] [Google Scholar]
- 39.Clarke R, Peden JF, Hopewell JC, et al. ; PROCARDIS Consortium . Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med 2009; 361: 2518–28. [DOI] [PubMed] [Google Scholar]
- 40.Dubé JB, Boffa MB, Hegele RA, Koschinsky ML. Lipoprotein(a): more interesting than ever after 50 years. Curr Opin Lipidol 2012; 23: 133–40. [DOI] [PubMed] [Google Scholar]
- 41.Emdin CA, Khera AV, Natarajan P, et al. ; CHARGE-Heart Failure Consortium; CARDIoGRAM Exome Consortium . Phenotypic characterization of genetically lowered human lipoprotein(a) levels. J Am Coll Cardiol 2016; 68: 2761–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arsenault BJ, Boekholdt M, Dubé MP, et al. Lipoprotein(a) levels, genotype, and incident aortic valve stenosis. Circ Cardiovasc Genet 2014; 7: 304–10. [DOI] [PubMed] [Google Scholar]
- 43.Kronenberg F, Mora S, Stroes ESG, et al. Frequent questions and responses on the 2022 lipoprotein(a) consensus statement of the European Atherosclerosis Society. Atherosclerosis 2023; 374: 107–20. [DOI] [PubMed] [Google Scholar]
- 44.Welsh P, Welsh C, Celis-Morales CA, et al. Lipoprotein(a) and cardiovascular disease: prediction, attributable risk fraction, and estimating benefits from novel interventions. Eur J Prev Cardiol 2022; 28: 1991–2000. [DOI] [PubMed] [Google Scholar]
- 45.Patel AP, Wang M, Pirruccello JP, et al. Lp(a) (Lipoprotein[a]) concentrations and incident atherosclerotic cardiovascular disease: new insights from a Large National Biobank. Arterioscler Thromb Vasc Biol 2021; 41: 465–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020; 41: 111–88. [DOI] [PubMed] [Google Scholar]
- 47.Langsted A, Kamstrup PR, Nordestgaard BG. High lipoprotein(a) and high risk of mortality. Eur Heart J 2019; 40: 2760–70. [DOI] [PubMed] [Google Scholar]
- 48.Wang ZW, Li M, Li JJ, Liu NF. Association of lipoprotein(a) with all-cause and cause-specific mortality: a prospective cohort study. Eur J Intern Med 2022; 106: 63–70. [DOI] [PubMed] [Google Scholar]
- 49.Amiri M, Raeisi-Dehkordi H, Verkaar AJCF, et al. Circulating lipoprotein (a) and all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis. Eur J Epidemiol 2023; 38: 485–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stewart B, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. J Am Coll Cardiol 1997; 29: 630–4. [DOI] [PubMed] [Google Scholar]
- 51.Després AA, Perrot N, Poulin A, et al. Lipoprotein(a), oxidized phospholipids, and aortic valve microcalcification assessed by 18F-sodium fluoride positron emission tomography and computed tomography. CJC Open 2019; 1: 131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zheng KH, Tsimikas S, Pawade T, et al. Lipoprotein(a) and oxidized phospholipids promote valve calcification in patients with aortic stenosis. J Am Coll Cardiol 2019; 73: 2150–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu Q, Yu Y, Xi R, et al. Association between lipoprotein(a) and calcific aortic valve disease: a systematic review and meta-analysis. Front Cardiovasc Med 2022; 9: 877140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Golledge J, Rowbotham S, Velu R, et al. Association of serum lipoprotein(a) with the requirement for a peripheral artery operation and the incidence of major adverse cardiovascular events in people with peripheral artery disease. J Am Heart Assoc 2020; 9: e015355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Masson W, Lobo M, Barbagelata L, Molinero G, Bluro I, Nogueira JP. Elevated lipoprotein (a) levels and risk of peripheral artery disease outcomes: a systematic review. Vasc Med 2022; 27: 385–91. [DOI] [PubMed] [Google Scholar]
- 56.Guédon AF, De Freminville JB, Mirault T, et al. Association of lipoprotein(a) levels with incidence of major adverse limb events. JAMA Netw Open 2022; 5: e2245720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bonaca M, Morrow DA, Giugliano RP, et al. Lipoprotein(a) and the risk of major adverse limb events in patients with stable atherosclerotic vascular disease. European Heart J 2023; 44 Suppl 2: ehad655.2022. [Google Scholar]
- 58.Gudbjartsson DF, Thorgeirsson G, Sulem P, et al. Lipoprotein(a) concentration and risks of cardiovascular disease and diabetes. J Am Coll Cardiol 2019; 74: 2982–94. [DOI] [PubMed] [Google Scholar]
- 59.Mohammadi-Shemirani P, Chong M, Narula S, et al. Elevated lipoprotein(a) and risk of atrial fibrillation: an observational and mendelian randomization study. J Am Coll Cardiol 2022; 79: 1579–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Benjamin EJ, Levy D, Vaziri SM, D’Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994; 271: 840–4. [PubMed] [Google Scholar]
- 61.Greve AM, Gerdts E, Boman K, et al. Prognostic importance of atrial fibrillation in asymptomatic aortic stenosis: the Simvastatin and Ezetimibe in Aortic Stenosis study. Int J Cardiol 2013; 166: 72–6. [DOI] [PubMed] [Google Scholar]
- 62.Garg PK, Guan W, Karger AB, et al. Lp(a) (lipoprotein [a]) and risk for incident atrial fibrillation: a multi-ethnic study of atherosclerosis. Circ Arrhythm Electrophysiol 2020; 13: e008401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Emdin CA, Khera AV, Natarajan P, et al. ; CHARGE-Heart Failure Consortium; CARDIoGRAM Exome Consortium . Phenotypic characterization of genetically lowered human lipoprotein(a) levels. J Am Coll Cardiol 2016; 68: 2761–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Boerwinkle E, Leffert CC, Lin J, et al. Apolipoprotein(a) gene accounts for greater than 90% of the variation in plasma lipoprotein(a) concentrations. J Clin Invest 1992; 90: 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Iannuzzo G, Tripaldella M, Mallardo V, et al. Lipoprotein(a) where do we stand? From the physiopathology to innovative therapy. Biomedicines 2021; 9: 838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Coassin S, Kronenberg F. Lipoprotein(a) beyond the kringle IV repeat polymorphism: the complexity of genetic variation in the LPA gene. Atherosclerosis 2022; 349: 17–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kenet G, Lütkhoff LK, Albisetti M, et al. Impact of thrombophilia on risk of arterial ischemic stroke or cerebral sinovenous thrombosis in neonates and children: a systematic review and meta-analysis of observational studies. Circulation 2010; 121: 1838–47. [DOI] [PubMed] [Google Scholar]
- 68.de Boer LM, Hof MH, Wiegman A, Stroobants AK, Kastelein JJP, Hutten BA. Lipoprotein(a) levels from childhood to adulthood: data in nearly 3,000 children who visited a pediatric lipid clinic. Atherosclerosis 2022; 349: 227–32. [DOI] [PubMed] [Google Scholar]
- 69.Strandkjær N, Hansen MK, Nielsen ST, et al. Lipoprotein(a) levels at birth and in early childhood: the COMPARE study. J Clin Endocrinol Metab 2022; 107: 324–35. [DOI] [PubMed] [Google Scholar]
- 70.Virani SS, Brautbar A, Davis BC, et al. Associations between lipoprotein(a) levels and cardiovascular outcomes in black and white subjects: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2012; 125: 241–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Simony SB, Mortensen MB, Langsted A, Afzal S, Kamstrup PR, Nordestgaard BG. Sex differences of lipoprotein(a) levels and associated risk of morbidity and mortality by age: The Copenhagen General Population Study. Atherosclerosis 2022; 355: 76–82. [DOI] [PubMed] [Google Scholar]
- 72.Varvel S, McConnell JP, Tsimikas S. Prevalence of elevated Lp(a) mass levels and patient thresholds in 532,359 patients in the United States. Arterioscler Thromb Vasc Biol 2016; 36: 2239–45. [DOI] [PubMed] [Google Scholar]
- 73.Derby CA, Crawford SL, Pasternak RC, Sowers M, Sternfeld B, Matthews KA. Lipid changes during the menopause transition in relation to age and weight: the Study of Women’s Health Across the Nation. Am J Epidemiol 2009; 169: 1352–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Enkhmaa B, Berglund L. Non-genetic influences on lipoprotein(a) concentrations. Atherosclerosis 2022; 349: 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ebbeling CB, Knapp A, Johnson A, et al. Effects of a low-carbohydrate diet on insulin-resistant dyslipoproteinemia-a randomized controlled feeding trial. Am J Clin Nutr 2022; 115: 154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Scholl JG. Does a ketogenic diet lower a very high Lp(a)? A striking experiment in a male physician. BMJ Nutr Prev Health 2020; 3: 413–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Joo M, Moon S, Lee YS, Kim MG. Effects of very low-carbohydrate ketogenic diets on lipid profiles in normal-weight (body mass index < 25 kg/m2) adults: a meta-analysis. Nutr Rev 2023; 81: 1393–401. [DOI] [PubMed] [Google Scholar]
- 78.Wang Y, Hu Y, Wan Y, Rimm EB, Hu FB, Sun Q. Low-carbohydrate diets and risk of type 2 diabetes in U.S. men and women. Circulation 2022; 146: A13226. [Google Scholar]
- 79.Mazidi M, Katsiki N, Mikhailidis DP, Sattar N, Banach M. Lower carbohydrate diets and all-cause and cause-specific mortality: a population-based cohort study and pooling of prospective studies. Eur Heart J 2019; 40: 2870–9. [DOI] [PubMed] [Google Scholar]
- 80.Surma S, Sahebkar A, Banach M; endorsed by the International Lipid Expert Panel (ILEP) . Low carbohydrate/ketogenic diet in the optimization of lipoprotein(a) levels: do we have sufficient evidence for any recommendation? Eur Heart J 2023; 44: 4904–6. [DOI] [PubMed] [Google Scholar]
- 81.Enkhmaa B, Petersen KS, Kris-Etherton PM, Berglund L. Diet and Lp(a): does dietary change modify residual cardiovascular risk conferred by Lp(a)? Nutrients 2020; 12: 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fitó M, Estruch R, Salas-Salvadó J, et al. ; PREDIMED Study Investigators . Effect of the Mediterranean diet on heart failure biomarkers: a randomized sample from the PREDIMED trial. Eur J Heart Fail 2014; 16: 543–50. [DOI] [PubMed] [Google Scholar]
- 83.Law HG, Meyers FJ, Berglund L, Enkhmaa B. Lipoprotein(a) and diet-a challenge for a role of saturated fat in cardiovascular disease risk reduction? Am J Clin Nutr 2023; 118: 23–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rodgers GP, Collins FS. Precision nutrition-the answer to “What to Eat to Stay Healthy”. JAMA 2020; 324: 735–6. [DOI] [PubMed] [Google Scholar]
- 85.Banach M, Lewek J, Surma S, et al. The association between daily step count and all-cause and cardiovascular mortality: a meta-analysis. Eur J Prev Cardiol 2023; 30: 1975–85. [DOI] [PubMed] [Google Scholar]
- 86.Salpeter SR, Walsh JM, Ormiston TM, Greyber E, Buckley NS, Salpeter EE. Meta-analysis: effect of hormone-replacement therapy on components of the metabolic syndrome in postmenopausal women. Diabetes Obes Metab 2006; 8: 538–54. [DOI] [PubMed] [Google Scholar]
- 87.Sattar N, Clark P, Greer IA, Shepherd J, Packard CJ. Lipoprotein (a) levels in normal pregnancy and in pregnancy complicated with pre-eclampsia. Atherosclerosis 2000; 148: 407–11. [DOI] [PubMed] [Google Scholar]
- 88.Banach, M, Burchardt, P, Chlebus, K, et al. PoLA/CFPiP/PCS/PSLD/PSD/PSH guidelines on diagnosis and therapy of lipid disorders in Poland 2021. Arch Med Sci 2021; 17: 1447–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Golawski M, Lejawa M, Osadnik T, et al. Genetically determined lipoprotein(a) levels do not cause an increased risk of preeclampsia –- a two-sample Mendelian randomization study. Eur Heart J 2023; 44 (Suppl. 2): ehad655.2728. [Google Scholar]
- 90.Edén S, Wiklund O, Oscarsson J, Rosén T, Bengtsson BA. Growth hormone treatment of growth hormone-deficient adults results in a marked increase in Lp(a) and HDL cholesterol concentrations. Arterioscler Thromb 1993; 13: 296–301. [DOI] [PubMed] [Google Scholar]
- 91.Glynn N, Halsall DJ, Boran G, et al. Growth hormone replacement may influence the biological action of thyroid hormone on liver and bone tissue. Growth Horm IGF Res 2021; 57–58: 101393. [DOI] [PubMed] [Google Scholar]
- 92.Kotwal A, Cortes T, Genere N, et al. Treatment of thyroid dysfunction and serum lipids: a systematic review and meta-analysis. J Clin Endocrinol Metab 2020; 105: dgaa672. [DOI] [PubMed] [Google Scholar]
- 93.Kaftan AN, Naser FH, Enaya MA. Changes of certain metabolic and cardiovascular markers fructosamine, H-FABP and lipoprotein(a) in patients with hypothyroidism. Med Arch 2021; 75: 11–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kronenberg F, Kuen E, Ritz E, et al. Lipoprotein(a) serum concentrations and apolipoprotein(a) phenotypes in mild and moderate renal failure. J Am Soc Nephrol 2000; 11: 105–15. [DOI] [PubMed] [Google Scholar]
- 95.Kronenberg F, Lingenhel A, Lhotta K, et al. The apolipoprotein(a) size polymorphism is associated with nephrotic syndrome. Kidney Int 2004; 65: 606–12. [DOI] [PubMed] [Google Scholar]
- 96.Kronenberg F, König P, Neyer U, et al. Multicenter study of lipoprotein(a) and apolipoprotein(a) phenotypes in patients with end-stage renal disease treated by hemodialysis or continuous ambulatory peritoneal dialysis. J Am Soc Nephrol 1995; 6: 110–20. [DOI] [PubMed] [Google Scholar]
- 97.Kronenberg F, Köni P, Lhotta K, et al. Apolipoprotein(a) phenotype-associated decrease in lipoprotein(a) plasma concentrations after renal transplantation. Arterioscler Thromb 1994; 14: 1399–404. [DOI] [PubMed] [Google Scholar]
- 98.Malaguarnera M, Giugno I, Trovato BA, Panebianco MP, Siciliano R, Ruello P. Lipoprotein(a) concentration in patients with chronic active hepatitis C before and after interferon treatment. Clin Ther 1995; 17: 721–8. [DOI] [PubMed] [Google Scholar]
- 99.Jung I, Kwon H, Park SE, et al. Serum lipoprotein(a) levels and insulin resistance have opposite effects on fatty liver disease. Atherosclerosis 2020; 308: 1–5. [DOI] [PubMed] [Google Scholar]
- 100.Kronenberg F, Mora S, Stroes ESG, et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur Heart J 2022; 43: 3925–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Momtazi-Borojeni AA, Katsiki N, Pirro M, Banach M, Rasadi KA, Sahebkar A. Dietary natural products as emerging lipoprotein(a)-lowering agents. J Cell Physiol 2019; 234: 12581–94. [DOI] [PubMed] [Google Scholar]
- 102.Kotani K, Sahebkar A, Serban C, et al. ; Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group . Tibolone decreases lipoprotein(a) levels in postmenopausal women: a systematic review and meta-analysis of 12 studies with 1009 patients. Atherosclerosis 2015; 242: 87–96. [DOI] [PubMed] [Google Scholar]
- 103.Ferretti G, Bacchetti T, Simental-Mendía LE, Reiner Ž, Banach M, Sahebkar A. Raloxifene lowers plasma lipoprotein(a) concentrations: a systematic review and meta-analysis of randomized placebo-controlled trials. Cardiovasc Drugs Ther 2017; 31: 197–208. [DOI] [PubMed] [Google Scholar]
- 104.Sahebkar A, Serban MC, Penson P, et al. ; Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group . The effects of tamoxifen on plasma lipoprotein(a) concentrations: systematic review and meta-analysis. Drugs 2017; 77: 1187–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Reyes-Soffer G, Ginsberg HN, Berglund L, et al. ; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; and Council on Peripheral Vascular Disease . Lipoprotein(a): a genetically determined, causal, and prevalent risk factor for atherosclerotic cardiovascular disease: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol 2022; 42: e48–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ma GS, Schwartz GG, Olsson AG, Willeit P, Tsimikas S, Yeang C. Elevated lipoprotein(a) is associated with statin resistance. Circulation 2021; 144: A11456. [Google Scholar]
- 107.Trinder M, Paruchuri K, Haidermota S, et al. Repeat measures of lipoprotein(a) molar concentration and cardiovascular risk. J Am Coll Cardiol 2022; 79: 617–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Banach M. Lipoprotein(a): the enemy that we still don’t know how to defeat. Eur Heart J Open 2023; 3: oead080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gaba P, O’Donoghue M, Lopez JA, et al. Abstract 12103: intraindividual variability in serial lipoprotein(a) concentration among placebo-treated patients in the OCEAN(a)-DOSE Trial. Circulation 2023; 148: A12103. [Google Scholar]
- 110.Reeskamp LF, Tromp TR, Patel AP, et al. Concordance of a high lipoprotein(a) concentration among relatives. JAMA Cardiol 2023; 8: 1111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Catapano AL, Daccord M, Damato E, et al. How should public health recommendations address Lp(a) measurement, a causal risk factor for cardiovascular disease (CVD)? Atherosclerosis 2022; 349: 136–43. [DOI] [PubMed] [Google Scholar]
- 112.Scharnagl H, Stojakovic T, Dieplinger B, et al. Comparison of lipoprotein(a) serum concentrations measured by six commercially available immunoassays. Atherosclerosis 2019; 289: 206–13. [DOI] [PubMed] [Google Scholar]
- 113.Wyness SP, Genzen JR. Performance evaluation of five lipoprotein(a) immunoassays on the Roche cobas c501 chemistry analyser. Pract Lab Med 2021; 25: e00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ruhaak LR, Cobbaert CM. Quantifying apolipoprotein(a) in the era of proteoforms and precision medicine. Clin Chim Acta 2020; 511: 260–8. [DOI] [PubMed] [Google Scholar]
- 115.Tsimikas S, Fazio S, Viney NJ, Xia S, Witztum JL, Marcovina SM. Relationship of lipoprotein(a) molar concentrations and mass according to lipoprotein(a) thresholds and apolipoprotein(a) isoform size. J Clin Lipidol 2018; 12: 1313–23. [DOI] [PubMed] [Google Scholar]
- 116.Szarek M, Reijnders E, Steg PG, et al. ; ODYSSEY OUTCOMES Investigators . Comparison of change in lipoprotein(a) mass and molar concentrations by alirocumab and risk of subsequent cardiovascular events in ODYSSEY OUTCOMES. Circulation 2023; 148: A13567. [DOI] [PubMed] [Google Scholar]
- 117.Marcovina SM, Clouet-Foraison N, Koschinsky ML, et al. Development of an LC-MS/MS proposed candidate reference method for the standardization of analytical methods to measure lipoprotein(a). Clin Chem 2021; 67: 490–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ruhaak LR, Romijn FPHTM, Begcevic Brkovic I, et al. Development of an LC-MRM-MS-based candidate reference measurement procedure for standardization of serum apolipoprotein(a) tests. Clin Chem 2023; 69: 251–61. [DOI] [PubMed] [Google Scholar]
- 119.Xu MX, Liu C, He YM, Yang XJ, Zhao X. Long-term statin therapy could be efficacious in reducing the lipoprotein(a) levels in patients with coronary artery disease modified by some traditional risk factors. J Thorac Dis 2017; 9: 1322–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gonbert S, Malinsky S, Sposito AC, et al. Atorvastatin lowers lipoprotein(a) but not apolipoprotein(a) fragment levels in hypercholesterolemic subjects at high cardiovascular risk. Atherosclerosis 2002; 164: 305–11. [DOI] [PubMed] [Google Scholar]
- 121.Kosmas CE, Sourlas A, Mallarkey G, et al. Therapeutic management of hyperlipoproteinemia(a). Drugs Context 2019; 8: 212609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tsimikas S, Gordts PLSM, Nora C, Yeang C, Witztum JL. Statin therapy increases lipoprotein(a) levels. Eur Heart J 2020; 41: 2275–84. [DOI] [PubMed] [Google Scholar]
- 123.Bos S, Yayha R, van Lennep JE. Latest developments in the treatment of lipoprotein(a). Curr Opin Lipidol 2014; 25: 452–60. [DOI] [PubMed] [Google Scholar]
- 124.Vavlukis M, Mladenovska K, Daka A, et al. Effects of rosuvastatin versus atorvastatin, alone or in combination, on lipoprotein(a). Ann Pharmacother 2016; 50: 609–15. [DOI] [PubMed] [Google Scholar]
- 125.Yahya R, Berk K, Verhoeven A, et al. Statin treatment increases lipoprotein(a) levels in subjects with low molecular weight apolipoprotein(a) phenotype. Atherosclerosis 2019; 289: 201–5. [DOI] [PubMed] [Google Scholar]
- 126.Wang X, Li J, Ju J, Fan Y, Xu H. Effect of different types and dosages of statins on plasma lipoprotein(a) levels: a network meta-analysis. Pharmacol Res 2021; 163: 105275. [DOI] [PubMed] [Google Scholar]
- 127.Yoshida H, Shoda T, Yanai H, et al. Effects of pitavastatin and atorvastatin on lipoprotein oxidation biomarkers in patients with dyslipidemia. Atherosclerosis 2013; 226: 161–4. [DOI] [PubMed] [Google Scholar]
- 128.Banach M, Surma S, Kapłon-Cieślicka A, et al. Position Paper of the Polish Expert Group on the use of pitavastatin in the treatment of lipid disorders in Poland endorsed by the Polish Lipid Association. Arch Med Sci 2024; 20: 28–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Awad K, Mikhailidis DP, Katsiki N, Muntner P, Banach M. Lipid and Blood Pressure Meta-Analysis Collaboration (LBPMC) Group effect of ezetimibe monotherapy on plasma lipoprotein(a) concentrations in patients with primary hypercholesterolemia: a systematic review and meta-analysis of randomized controlled trials. Drugs 2018; 78: 453–62. [DOI] [PubMed] [Google Scholar]
- 130.Ridker PM, Lei L, Ray KK, Ballantyne CM, Bradwin G, Rifai N. Effects of bempedoic acid on CRP, IL-6, fibrinogen and lipoprotein(a) in patients with residual inflammatory risk: a secondary analysis of the CLEAR harmony trial. J Clin Lipidol 2023; 17: 297–302. [DOI] [PubMed] [Google Scholar]
- 131.Maloberti A, Fabbri S, Colombo V, et al. Lipoprotein(a): cardiovascular disease, aortic stenosis and new therapeutic option. Int J Mol Sci 2022; 24: 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.O’Donoghue ML, Fazio S, Giugliano RP, et al. Lipoprotein(a), PCSK9 inhibition, and cardiovascular risk. Circulation 2019; 139: 1483–92. [DOI] [PubMed] [Google Scholar]
- 133.Stone NJ, Smith SC Jr, Orringer CE, et al. Managing atherosclerotic cardiovascular risk in young adults: a JACC state-of-the-art review. J Am Coll Cardiol 2022; 79: 819–36. [DOI] [PubMed] [Google Scholar]
- 134.Katsiki N, Vrablik M, Banach M, Gouni-Berthold I. Inclisiran, low-density lipoprotein cholesterol and lipoprotein (a). Pharmaceuticals (Basel) 2023; 16: 577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Schwartz GG, Steg PG, Szarek M, et al. ; ODYSSEY OUTCOMES Committees and Investigators* . Peripheral artery disease and venous thromboembolic events after acute coronary syndrome: role of lipoprotein(a) and modification by alirocumab: prespecified analysis of the ODYSSEY OUTCOMES randomized clinical trial. Circulation 2020; 141: 1608–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Okada T, Miyoshi T, Doi M, et al. Effect of early initiation of evolocumab on lipoprotein(a) in patients with acute myocardial infarction: sub-analysis of a randomized controlled trial. J Cardiovasc Dev Dis 2022; 9: 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Croyal M, Tran TT, Blanchard RH, et al. PCSK9 inhibition with alirocumab reduces lipoprotein(a) levels in nonhuman primates by lowering apolipoprotein(a) production rate. Clin Sci (London) 2018; 132: 1075–83. [DOI] [PubMed] [Google Scholar]
- 138.Raal FJ, Kallend D, Ray KK, et al. ; ORION-9 Investigators . Inclisiran for the treatment of heterozygous familial hypercholesterolemia. N Engl J Med 2020; 382: 1520–30. [DOI] [PubMed] [Google Scholar]
- 139.Ray KK, Wright RS, Kallend D, et al. ; ORION-10 and ORION-11 Investigators . Two phase 3 trials of inclisiran in patients with elevated LDL cholesterol. N Engl J Med 2020; 382: 1507–19. [DOI] [PubMed] [Google Scholar]
- 140.Blanchard V, Chemello K, Hollstein T, et al. The size of apolipoprotein(a) is an independent determinant of the reduction in lipoprotein (a) induced by PCSK9 inhibitors. Cardiovasc Res 2022; 118: 2103–11. [DOI] [PubMed] [Google Scholar]
- 141.Parish S, Hopewell JC, Hill MR, et al. Impact of apolipoprotein(a) isoform size on lipoprotein(a) lowering in the HPS2-THRIVE study. Circ Genom Precis Med 2018; 11: e001696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Echeverry T, Anthony JA, Fishberg RD. Niacin treatment effective for reducing lp(a) levels. J Am Coll Cardiol 2023; 81: 3313. [Google Scholar]
- 143.Boffa MB, Koschinsky ML. Therapeutic lowering of lipoprotein(a): a role for pharmacogenetics? Circ Genom Precis Med 2018; 11: e002052. [DOI] [PubMed] [Google Scholar]
- 144.Artemeva NV, Safarova MS, Ezhov MV, Afanasieva OI, Dmitrieva OA, Pokrovsky SN. Lowering of lipoprotein(a) level under niacin treatment is dependent on apolipoprotein(a) phenotype. Atheroscler Suppl 2015; 18: 53–8. [DOI] [PubMed] [Google Scholar]
- 145.HPS2-THRIVE Collaborative Group HPS2-THRIVE randomised placebo-controlled trial in 25,673 high-risk patients of ER niacin/laropiprant: trial design, pre-specified muscle and liver outcomes, and reasons for stopping study treatment. Eur Heart J 2013; 34: 1279–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.HPS2-THRIVE Collaborative Group. Landray MJ, Haynes R, Hopewell JC, et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med 2014; 371: 203–12. [DOI] [PubMed] [Google Scholar]
- 147.Haynes R, Valdes-Marquez E, Hopewell JC, et al. Serious adverse effects of extended-release niacin/laropiprant: results from the Heart Protection Study 2-Treatment of HDL to Reduce the Incidence of Vascular Events (HPS2-THRIVE) trial. Clin Ther 2019; 41: 1767–77. [DOI] [PubMed] [Google Scholar]
- 148.Fogacci F, Di Micoli V, Avagimyan A, Giovannini M, Imbalzano E, Cicero AFG. Assessment of apolipoprotein(a) isoform size using phenotypic and genotypic methods. Int J Mol Sci 2023; 24: 13886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Connelly-Smith L, Alquist CR, Aqui NA, et al. Guidelines on the use of therapeutic apheresis in clinical practice – evidence-based approach from the Writing Committee of the American Society for Apheresis: the ninth special issue. J Clin Apher 2023; 38: 77–278. [DOI] [PubMed] [Google Scholar]
- 150.Safarova MS, Moriarty PM. Lipoprotein apheresis: current recommendations for treating familial hypercholesterolemia and elevated lipoprotein(a). Curr Atheroscler Rep 2023; 25: 391–404. [DOI] [PubMed] [Google Scholar]
- 151.Waldmann E, Parhofer KG. Lipoprotein apheresis to treat elevated lipoprotein(a). J Lipid Res 2016; 57: 1751–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Arai K, Orsoni A, Mallat Z, et al. Acute impact of apheresis on oxidized phospholipids in patients with familial hypercholesterolemia. J Lipid Res 2012; 53: 1670–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Stefanutti C, Mazza F, Pasqualetti D, et al. Lipoprotein apheresis downregulates IL-1α, IL-6 and TNF-α mRNA expression in severe dyslipidaemia. Atherosclerosis 2017; 30 Suppl: 200–8. [DOI] [PubMed] [Google Scholar]
- 154.Leebmann J, Roeseler E, Julius U, et al. ; Pro(a)LiFe Study Group . Lipoprotein apheresis in patients with maximally tolerated lipid-lowering therapy, lipoprotein(a)-hyperlipoproteinemia, and progressive cardiovascular disease: a prospective observational multicenter study. Circulation 2013; 128: 2567–76. [DOI] [PubMed] [Google Scholar]
- 155.Schettler VJJ, Peter C, Zimmermann T, et al. ; Scientific Board of GLAR for the German Apheresis Working Group . The German Lipoprotein Apheresis Registry-Summary of the ninth annual report. Ther Apher Dial 2022; 26 Suppl 1: 81–8. [DOI] [PubMed] [Google Scholar]
- 156.Moriarty PM, Gray JV, Gorby LK. Lipoprotein apheresis for lipoprotein(a) and cardiovascular disease. J Clin Lipidol 2019; 13: 894–900. [DOI] [PubMed] [Google Scholar]
- 157.Mickiewicz A, Marlega J, Kuchta A, et al. Cardiovascular events in patients with familial hypercholesterolemia and hyperlipoproteinaemia(a): indications for lipoprotein apheresis in Poland. J Clin Apher 2021; 36: 370–8. [DOI] [PubMed] [Google Scholar]
- 158.Mickiewicz A, Marlęga-Linert J, Czapiewska M, et al. Fatty acid analysis in serum of patients with elevated lipoprotein(a) and cardiovascular disease undergoing lipoprotein apheresis. J Clin Lipidol 2023. Nov 28:S1933-2874(23)00343-4. [DOI] [PubMed] [Google Scholar]
- 159.Khan TZ, Gorog DA, Arachchillage DJ, et al. Impact of lipoprotein apheresis on thrombotic parameters in patients with refractory angina and raised lipoprotein(a): findings from a randomized controlled cross-over trial. J Clin Lipidol 2019; 13: 788–96. [DOI] [PubMed] [Google Scholar]
- 160.Nugent AK, Gray JV, Gorby LK, Moriarty PM. Lipoprotein apheresis: first FDA indicated treatment for elevated lipoprotein(a). J Clin Cardiol 2020; 1: 16–21. [Google Scholar]
- 161.Hanssen R, Gouni-Berthold I. Lipoprotein(a) management: pharmacological and apheretic treatment. Curr Med Chem 2017; 24: 957–68. [DOI] [PubMed] [Google Scholar]
- 162.Nandakumar R, Matveyenko A, Thomas T, et al. Effects of mipomersen, an apolipoprotein B100 antisense, on lipoprotein(a) metabolism in healthy subjects. J Lipid Res 2018; 59: 2397–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Fogacci F, Ferri N, Toth PP, Ruscica M, Corsini A, Cicero AFG. Efficacy and safety of mipomersen: a systematic review and meta-analysis of randomized clinical trials. Drugs 2019; 79: 751–66. [DOI] [PubMed] [Google Scholar]
- 164.Reeskamp LF, Kastelein JJ, Moriarty PM, et al. Safety and efficacy of mipomersen in patients with heterozygous familial hypercholesterolemia. Atherosclerosis 2019; 280: 109–17. [DOI] [PubMed] [Google Scholar]
- 165.Thomas GS, Cromwell WC, Ali S, Chin W, Flaim JD, Davidson M. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol 2013; 62: 2178–84. [DOI] [PubMed] [Google Scholar]
- 166.Visseren FLJ, Mach F, Smulders YM, et al. ; ESC National Cardiac Societies; ESC Scientific Document Group . 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021; 42: 3227–337. [DOI] [PubMed] [Google Scholar]
- 167.Banach M, Penson PE. Statins and Lp(a): do not make perfect the enemy of excellent. Eur Heart J 2020; 41: 190–1. [DOI] [PubMed] [Google Scholar]
- 168.Sosnowska B, Surma S, Banach M. Targeted treatment against lipoprotein(a): the coming breakthrough in lipid lowering therapy. Pharmaceuticals 2022; 15: 1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Tsimikas S, Karwatowska-Prokopczuk E, Gouni-Berthold I, et al. ; AKCEA-APO(a)-LRx Study Investigators . Lipoprotein(a) reduction in persons with cardiovascular disease. N Engl J Med 2020; 382: 244–55. [DOI] [PubMed] [Google Scholar]
- 170.Karwatowska-Prokopczuk E, Clouet-Foraison N, Xia S, et al. Prevalence and influence of LPA gene variants and isoform size on the Lp(a)-lowering effect of pelacarsen. Atherosclerosis 2021; 324: 102–8. [DOI] [PubMed] [Google Scholar]
- 171.Koren MJ, Moriarty PM, Baum SJ, et al. Preclinical development and phase 1 trial of a novel siRNA targeting lipoprotein(a). Nat Med 2022; 28: 96–103. [DOI] [PubMed] [Google Scholar]
- 172.Nissen SE, Wolski K, Balog C, et al. Single ascending dose study of a short interfering RNA targeting lipoprotein(a) production in individuals with elevated plasma lipoprotein(a) levels. JAMA 2022; 327: 1679–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.ClinicalTrials.gov Identifier: NCT05537571 A Multi-Centre, Randomised, Double-Blind, Placebo-Controlled, Phase 2 Study to Investigate Efficacy, Safety and Tolerability of SLN360 in Participants with Elevated Lipoprotein(a) at High Risk of Atherosclerotic Cardiovascular Disease Events. [(accessed on 24 October 2023)]; Available online: https://beta.clinicaltrials.gov/study/NCT05537571.
- 174.Nissen SE, Linnebjerg H, Shen X, et al. Lepodisiran, an extended-duration short interfering RNA targeting lipoprotein(a): a randomized dose-ascending clinical trial. JAMA 2023; 330: 2075–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.ClinicalTrials.gov Identifier: NCT05565742 A Phase 2, Randomized, Double-Blind, Placebo-enkControlled Study to Investigate the Efficacy and Safety of LY3819469 in Adults with Elevated Lipoprotein(a) [(accessed on 24 October 2023)]; Available online: https://beta.clinicaltrials.gov/study/NCT05565742.
- 176.Nicholls SJ, Nissen SE, Fleming C, et al. Muvalaplin, an oral small molecule inhibitor of lipoprotein(a) formation: a randomized clinical trial. JAMA 2023; 330: 1042–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.ClinicalTrials.gov Identifier: NCT05563246 Phase 2, Randomised, Double-Blind, Placebo-Controlled Study to Investigate the Efficacy and Safety of Oral Once-Daily LY3473329 in Adults With Elevated Lipoprotein(a) at High Risk for Cardiovascular Events. (accessed on 24 October 2023); Available online: https://clinicaltrials.gov/study/NCT05563246.
- 178.Nicholls SJ, Ditmarsch M, Kastelein JJ, et al. Lipid lowering effects of the CETP inhibitor obicetrapib in combination with high-intensity statins: a randomized phase 2 trial. Nat Med 2022; 28: 1672–8. [DOI] [PubMed] [Google Scholar]