Abstract
Background:
Previous studies have attempted to determine if certain risk factors can predict the occurrence of a lateral ankle sprain (LAS) in female soccer players. Unfortunately, there is limited evidence with regard to risk factors associated with an LAS in female soccer players.
Purpose:
To identify intrinsic risk factors for an LAS among young female soccer players.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Participants were 161 young female soccer players in Japan who were evaluated for LAS risk factors during a preseason medical assessment. The assessment included anthropometric, joint laxity, joint range of motion, muscle flexibility, muscle strength, and balance measurements. Each athlete’s history of LASs was also collected. The participants were monitored during a single-yearseason for LASs, as diagnosed by physicians.
Results:
There were 26 instances of an LAS in 25 players (15.5%) during the season. Injured players were significantly more likely to have sustained a previous ankle sprain (P = .045) and demonstrated significantly worse balance than their peers without an LAS during the double- and single-leg balance tests (P = .008 for both). Athletes with lower hamstring-to-quadriceps muscle strength ratios were also significantly more likely to sustain an LAS (P = .02).
Conclusion:
Poor balance, a low hamstring-to-quadriceps ratio, and a history of ankle sprains were associated with an increased risk of LASs in young female soccer players in the current study. These findings may be useful for developing a program to prevent LASs in this population.
Keywords: lateral ankle sprain, risk factor, collegiate soccer player, injury prevention, female athlete
Ankle sprains are common lower extremity musculoskeletal sports injuries. The most typical are inversion or lateral ankle sprains (LASs).10,12,19 LASs are relatively common and have a high recurrence rate of up to 47%. 28 Some athletes with acute ankle sprains develop mechanical and/or functional ankle instability, resulting in residual symptoms commonly referred to as chronic ankle instability. 20
A study of sports in the National Collegiate Athletic Association (NCAA) found that an LAS was more common in basketball, soccer, volleyball, football, and gymnastics. 6 Soccer is among the most popular sports globally, and it is characterized by rapid speed changes, pivoting, jumping, kicking, and cutting movements; therefore, ankle sprains are common among soccer players.4,35 In recent years, there has been growing interest in female soccer, and the number of female soccer players is increasing. A systematic review revealed that ankle sprains are more common in female athletes compared to their male counterparts. 10 Ankle sprains are the most common injury in NCAA female soccer players, with an incidence of 8.6%. 7 Despite their frequent occurrence, few studies have attempted to identify intrinsic risk factors for an LAS, specifically in female soccer players. 25
Because of their prominence in the sports injury landscape and the tendency for ongoing complications after an injury, preventing ankle sprains is important. 17 Previously identified intrinsic risk factors for an ankle sprain include a history of injuries,1,11,23 age, 1 lower limb range of motion (ROM), 14 balance,16,26,37 body mass index (BMI),16,29 and muscular strength.3,21,29 A study by Mason et al 24 found that male and female patients have different risk factors for an LAS. In male athletes, previous ankle sprains, a greater BMI, greater weight, lower isometric hip abduction strength, and lower dynamic balance performance were found to be risk factors, whereas only lower concentric dorsiflexion strength was found to be a risk factor in female athletes. Importantly, the authors noted the relatively scarcity of data on female athletes. 24
The aim of the current study was to identify intrinsic risk factors for an LAS in a relatively large population of young female soccer players.
Methods
In this prospective cohort study, we evaluated female high school and collegiate soccer players during the 2018-2020 season. Risk factor data were collected during a preseason medical assessment. All participants were subsequently monitored for injuries during a single soccer season. This study was a part of the Prospective Study of Predictors of Sports Injuries: UTokyo Sports Science Institute Sports Injury Prevention Project.32,33 Our institution’s ethics committee approved the study protocol, and written consent was obtained from all participants.
The study participants were 161 female soccer players from 3 soccer teams (1 high school and 2 collegiate teams) in Japan. None of the players were injured at the start of the study, and none reported a history of lower limb musculoskeletal injuries over the preceding 3 months. All participants received preseason medical checkups and completed a questionnaire that collected data on age, years of soccer experience, injury history, and medication use. In addition to anthropometric measurements, preseason data from 5 physical screening tests were used: joint laxity, joint ROM, muscle flexibility, muscle strength, and balance. Each participant’s LAS history was recorded, beginning immediately after informed consent was provided and continuing until the season’s completion. Consequently, each player only generated one set of measurement data. The latest data were used for players who underwent the medical assessment more than once.
Anthropometric Measurements
Body weight and height were measured for each player at the preseason medical checkup, and BMI was calculated from these variables. Each body composition parameter was measured using InBody 270 (InBody), a multifrequency impedance analyzer that can record each player’s lean soft tissue mass (skeletal muscle mass), body fat mass, and percentage of body fat. 27 Additionally, the height of each player’s navicular tubercle was measured as a flat-foot index. In the standing position, the navicular tuberosity was palpated, and the height of the navicular tuberosity was measured from the ground. 5
Joint Laxity and ROM Testing
Joint Laxity
Each player underwent general joint laxity testing using methods as described by Watanabe et al 34 and Fujitaka et al. 13 Testing consisted of 7 conditions: thumb-to-forearm position, elbow hyperextension ≥15°, shoulder hyperrotation, hip hyper–external rotation ≥90° while standing, knee hyperextension ≥10°, ankle hyperdorsiflexion at ≥45° of knee flexion, and trunk flexion with both palms touching the floor and knees fully extended. Shoulder hyperrotation was considered positive when participants could clasp their hands from both the cranial and caudal sections of their back. Hip hyper–external rotation was considered positive when participants could maintain their hips at 90° of external rotation with both legs in a neutral position. All tests, except for trunk flexion and hip hyper–external rotation, were performed bilaterally. A point value of 0.5 was given each time a player surpassed the designated laxity measurement on both the right and left sides of the tested joints (wrists, elbows, shoulders, knees, and ankles), and 1 point each was given for the trunk and hip, for a maximum possible score of 7 points.
Joint ROM
Joint ROM was measured for hip internal rotation, ankle dorsiflexion, and knee extension based on previous studies.2,3 The passive hip internal rotation angle in the prone position served as the measure of hip internal rotation. The weightbearing ankle dorsiflexion angle with knee flexion served as the measure of ankle dorsiflexion. For knee extension, the knee hyperextension angle was measured in a standing position with the quadriceps engaged.
Muscle Flexibility and Strength Testing
Muscle Flexibility
Muscle flexibility testing was performed on the iliopsoas, quadriceps femoris, hamstring, gastrocnemius, and soleus muscles bilaterally using methods described previously.21,32,33 These methods are known to be highly reliable. 34
Iliopsoas: The iliopsoas was measured by determining the angle of the hip joint when the participants passively bent their opposite hip joint to the maximum, holding the knee with their hands in a supine position.
Quadriceps: The participants grasped their lower leg proximal to the ankle and pulled it toward the buttocks to measure quadriceps flexibility. The quadriceps muscle measurement was performed by bending the knee joint while in a prone position. The examiner (S.Takei) verbally reminded the participants not to engage their buttocks during the measurement.
Hamstring: Hamstring muscle flexibility was measured with the hip at 90° of flexion in a supine position. While holding the participant’s heel, a researcher (S.Takei) measured the angle between the vertical line to the floor and the long axis of the tibia after the knee joint was maximally extended.
Gastrocnemius: We measured the ankle joint’s active dorsiflexion angle during maximum dorsiflexion in the supine position, with the knee extended and maintained in a neutral position relative to the varus-valgus angle of the ankle.
Soleus: The ankle joint’s active dorsiflexion angle was measured when maximally dorsiflexed in the prone position with the knee at 90° of flexion.
Isometric Knee Extension and Flexion
HUMAC NORM (CSMi) was used to measure isometric muscle strength during knee flexion and extension. Before the measurement, the player warmed up on a stationary exercise bicycle for 5 minutes. The left-right measurement order was randomized. Only a single measurement was taken on each side. Testing comprised isometric contraction with knee flexion and extension at 70°. The highest peak torque value was recorded. Strength measurements were normalized to body weight. The hamstring-to-quadriceps (H/Q) muscle strength ratio was also calculated (Figure 1).
Figure 1.
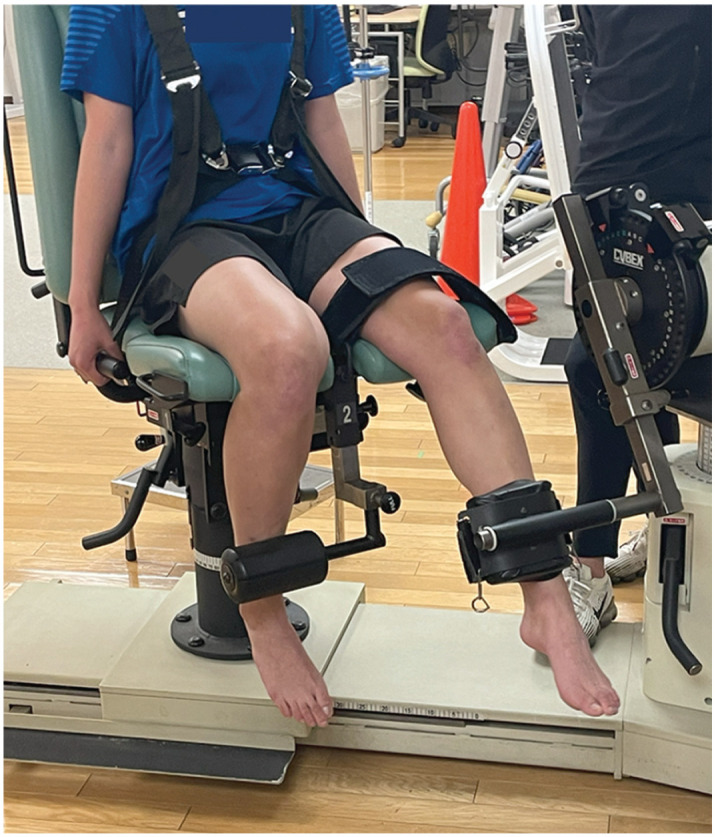
Knee extension and flexion strength testing.
Isometric Hip Abduction
Hip abductor strength was measured isometrically using a handheld dynamometer (μTas F-1; Anima). Each participant was instructed to lie in a supine position with neutral hips next to a wall, with both knees extended and arms crossed over the chest. Only a single measurement was taken on each side. We recorded the peak force generated as the participants abducted their legs maximally over 5 seconds, with 1 minute of rest between contractions. The dynamometer was placed on the lateral epicondyle of the femur, and the distance between the lateral epicondyle and the hip center was measured. Isometric assessments of hip abductor strength using a handheld dynamometer have excellent intratester and intertester reliability. 30 The highest peak torque value was recorded. Strength measurements were normalized to body weight.
Balance Testing
Double- and single-leg standing balance using a 1-m Footscan pressure plate (RSscan International) with 8192 resistive sensors and a pixel resolution of 5.08 × 7.62 mm were measured, with a sampling frequency of 250 Hz, as per previously described methods.8,9 First, the participant performed a 30-second trial of double-leg standing balance barefooted with the arms crossed over the chest and the eyes open. After a 30-second rest, the participant performed a 30-second trial of single-leg standing balance, similar to the double-leg standing balance test but alternating left and right legs. The total distance of the center of pressure during the 30 seconds on both tests was considered the balance parameter (Figure 2).
Figure 2.

Balance testing using a pressure plate.
LAS Diagnosis
An LAS was diagnosed and monitored by the teams’ medical staff under the supervision of an orthopaedic team physician or directly by the team physician. The diagnosis (eg, LAS), date of injury, and site (eg, left ankle) were documented for every injury. An injury was defined as a physical complaint requiring physical activity restrictions for at least 1 day. Injuries were only considered during a soccer practice or game. 29 Injury data were collected every 2 months from the teams’ medical staff.
Statistical Analysis
All statistical analyses were performed using BellCurve for Excel (SSRI). Parameters, except for lower limb parameters, were compared between injured and uninjured players. In addition, lower limb parameters were compared between the injured limb of the injured players and the average of the left and right limbs of the uninjured players. The unpaired 2-tailed Student t test, Mann-Whitney U test, and Fisher exact test were used to assess continuous, nonparametric, and ordered variables, respectively. P values <.05 were considered statistically significant. The Cohen d effect size was also calculated.
Results
An LAS occurred in 26 ankles of 25 players (15.5%). No participants were lost to follow-up during the injury registration period. Table 1 shows the comparison of player characteristics, anthropometric measurements, joint laxity test findings, and double-leg standing balance test results between the injured and uninjured groups. A previous ankle injury was associated with the risk of an LAS (P = .045), and poorer balance during the double-leg balance task was associated with an increased risk of an LAS (P = .008). Table 2 compares lower limb parameters between the injured and uninjured players. A lower H/Q ratio (P = .02) and poorer single-leg balance (P = .008) were also associated with an increased risk of an LAS. There were no statistically significant between-group differences for any other variables.
Table 1.
Demographic Characteristics and Anthropometric, Joint Laxity, and Double-Leg Balance Measurements a
| Injured Players (n = 25) | Uninjured Players (n = 136) | P | Cohen d | |
|---|---|---|---|---|
| Age, y | 17.5 ± 1.9 | 17.6 ± 1.9 | .72 | 0.08 |
| Playing experience, y | 8.0 ± 4.6 | 8.5 ± 4.1 | .57 | 0.12 |
| History of LAS, n (%) | 10 (40.0) | 29 (21.3) | .045 | NA |
| Weight, kg | 54.8 ± 5.2 | 55.0 ± 6.4 | .84 | 0.04 |
| Height, cm | 159.5 ± 0.1 | 159.8 ± 5.5 | .77 | 0.06 |
| Body mass index, kg/m2 | 22.5 ± 1.5 | 22.5 ± 1.6 | .96 | 0.01 |
| Skeletal muscle mass (lean soft tissue mass), kg | 40.2 ± 3.6 | 39.4 ± 4.0 | .39 | 0.19 |
| Body fat mass, kg | 11.8 ± 2.9 | 13.0 ± 3.1 | .09 | 0.37 |
| Body fat, % | 21.6 ± 4.2 | 23.3 ± 4.4 | .07 | 0.40 |
| General joint laxity test score (of 7) | 3.5 (0.0-5.0) | 2.5 (0.0-7.0) | .48 | 0.01 |
| Center of pressure on double-leg balance test, mm | 49.8 ± 25.6 | 37.9 ± 19.3 | .008 | 0.55 |
Data are reported as mean ± SD or median (range) unless otherwise indicated. Boldface P values indicate a statistically significant difference between the groups (P < .05). LAS, lateral ankle sprain; NA, not applicable.
Table 2.
Lower Limb Parameters for Injured Limb of Injured Players Versus Uninjured Limbs of Uninjured Players a
| Injured Limb of Injured Players (n = 26) | Uninjured Limbs of Uninjured Players b (n = 136) | P | Cohen d | |
|---|---|---|---|---|
| Height of navicular tubercle, cm | 4.4 ± 0.4 | 4.4 ± 0.5 | .99 | 0.003 |
| Joint ROM, deg | ||||
| Knee extension angle | 6.9 ± 4.2 | 6.5 ± 4.3 | .64 | 0.10 |
| Ankle dorsiflexion angle | 42.0 ± 7.8 | 42.8 ± 5.5 | .60 | 0.28 |
| Hip internal rotation angle | 52.9 ± 9.9 | 50.5 ± 9.7 | .27 | 0.25 |
| Muscle flexibility, deg | ||||
| Iliopsoas | 7.4 ± 3.7 | 6.0 ± 3.2 | .05 | 0.42 |
| Quadriceps | 30.2 ± 4.3 | 30.4 ± 4.8 | .82 | 0.05 |
| Hamstring | 13.8 ± 7.5 | 12.1 ± 6.3 | .24 | 0.25 |
| Gastrocnemius | 11.9 ± 4.9 | 12.5 ± 4.4 | .54 | 0.13 |
| Soleus | 20.2 ± 6.7 | 21.4 ± 5.3 | .32 | 0.21 |
| Muscle strength, N·m/kg | ||||
| Normalized isometric knee extension | 3.0 ± 0.4 | 2.7 ± 0.5 | .07 | 0.32 |
| Normalized isometric knee flexion | 1.3 ± 0.3 | 1.3 ± 0.2 | .95 | 0.02 |
| Normalized isometric hip abduction | 2.0 ± 0.4 | 1.9 ± 0.4 | .55 | 0.08 |
| H/Q ratio | 0.45 ± 0.09 | 0.50 ± 0.10 | .02 | 0.50 |
| Center of pressure on single-leg balance test, mm | 417.1 ± 123.2 | 359.7 ± 4.2 | .008 | 0.58 |
Data are reported as mean ± SD. Boldface P values indicate a statistically significant difference between the groups (P < .05). deg, degree; H/Q, hamstring to quadriceps; ROM, range of motion.
Calculated as the average of the left and right limbs of the uninjured players.
Discussion
The most important finding in this study was that poorer single- and double-leg balance, a lower H/Q ratio, and a history of LASs were associated with an increased risk of new-onset LASs in young female soccer players. None of the other variables that we studied were associated with the incidence of LASs.
Poorer leg balance reflects poor postural control 18 and is a frequent cause of LASs. A previous study identifying intrinsic LAS risk factors in 94 female netball players reported that poor balance as assessed by the Star Excursion Balance Test was the only significant predictor of ankle sprains. 2 Another study of 159 female physical education students found diminished postural control to be a risk factor for inversion ankle sprains. 37 Although methods for assessing balance differ, the results of both prior studies were consistent with our findings: poor balance increased the risk during both single- and double-leg tests. Thus, poor balance appears to be a risk factor for LASs in female athletes. Another study found sex differences related to the LAS risk. 24 Specifically, lower dynamic balance performance was a risk factor in male but not female athletes. However, that review noted the scarcity of data on female athletes. The relationship between LASs and balance in female athletes may become clearer as more studies are published.
We found a lower H/Q ratio to be a factor associated with LASs. Few studies have reported that the H/Q ratio is a risk for LASs in female athletes. A prospective investigation of female soccer players reported that a lower H/Q ratio increased the risk of traumatic leg injuries. 31 Knapik et al 22 studied female collegiate athletes and found that those with lower H/Q ratios experienced more lower extremity injuries. However, these studies did not focus on LASs but rather on lower extremity injuries, including ankle sprains. Hadzic et al 15 found that a lower H/Q concentric strength ratio significantly predicted ankle sprains in male national league volleyball players. According to that study, compared to uninjured athletes, injured athletes had greater concentric quadriceps strength on the uninjured side. Injured players’ H/Q ratios on the injured sides were low because of quadriceps muscle strength asymmetry. Our results revealed that a lower H/Q ratio was a risk factor for injuries, although we focused solely on LASs in female soccer players. They showed that there was no difference in knee flexor strength, and knee extensor strength tended to be stronger in the injured limb, although there was no significant difference. In light of this, we considered that the cause of the smaller H/Q ratio associated with an increased risk of new-onset LASs was muscle imbalance in which the hamstring muscles are not strong enough to match the overdeveloped quadriceps muscles.
We found a history of ankle sprains to be a significant factor associated with LASs in young female soccer players. The previous ankle injuries may be responsible for the poor balance, and therefore, it is possible that the 2 risk factors are related to each other and are not independent risk factors. Although multivariate analysis is necessary to know whether such confounding exists in this study, at the present time, we do not have sufficient statistical power to conduct multivariate analysis. An LAS history is broadly considered a risk factor for repeat LASs in male athletes.1,11,23 In contrast, no consensus exists for female athletes. A systematic review affirmed the association between a history of LASs and the risk of new-onset LASs in male athletes but not in female athletes. 36 Another meta-analysis concluded that a previous ankle sprain was a prognostic risk factor only in male athletes. 24 Despite this, several articles, although few in number, have suggested that an LAS was also a risk factor for a new-onset LAS in female athletes. McCann et al 25 found that players with a history of LASs were predisposed to LASs in a prospective cohort study of female collegiate soccer players. Once again, systematic reviews found a lack of data for female athletes.24,36 Given our exclusive focus on female soccer players, our results add considerable evidence supporting the risk for LASs in female athletes with prior LASs.
Poor performance on balance testing and muscle strength imbalance are intrinsic, but modifiable, risk factors. Therefore, the results of the present study may help inform LAS prevention strategies focused on improving balance and correcting thigh muscle imbalance with hamstring strengthening. Thus, our results have considerable clinical relevance. On the other hand, an LAS history is not modifiable. However, a history of LASs is important information for the prevention of LASs, as female soccer players with a history of LASs may require more interventions.
Limitations
This study has several limitations. First, multivariate analysis was not performed in this study. Multivariate analysis should be performed, because associated factors in univariate analysis may be confounded by each other. There were 4 risk factors identified from univariate analysis in this study. To perform multivariate analysis on these 4 factors, more than 40 incidents of an LAS would be needed. At present, we do not have sufficient statistical power to conduct this analysis, as we have not recorded data on this many LAS incidents. Second, although dynamic balance is needed for complex maneuvers in soccer, we evaluated only isometric muscle strength and static balance. Therefore, dynamic muscle strength and balance measures should be included in future studies. We did not evaluate functional and mechanical ankle instability, nor did we distinguish between contact and noncontact injuries; both factors should be addressed in future studies. Third, extrinsic factors such as surface of the pitch, field conditions, training intensity, footwear, and playing style, among others, which may have influenced the occurrence of LASs and data on the grade of injury, were not evaluated. Fourth, the history of LASs was self-reported, and muscle flexibility, joint laxity, and joint ROM were measured manually. Self-reporting is prone to recall bias, and errors in manual testing may affect the accuracy and reliability of the data. However, the examiners in this study were trained and remained the same throughout testing.
As an additional limitation, we only monitored participants over a single-year soccer season, which may not have captured the long-term development and changes in risk factors for an LAS. Longer follow-up periods would provide a more comprehensive understanding of the relationship between the identified risk factors and injury occurrence. On the other hand, there may be a problem that physical characteristics, which are intrinsic risk factors, may have changed from baseline in long-term monitoring. Sixth, we may not have measured all possible intrinsic factors. Lastly, given that our study cohort comprised a convenience sample of 3 young female teams, we cannot be sure that our results are generalizable to other soccer teams. Furthermore, because the data are from Japanese soccer players only, the results of this study may not be applicable to other sports or populations, as cultural and contextual factors can influence the injury risk.
Conclusion
Poor single- and double-leg balance, a lower H/Q ratio, and a history of ankle sprains were associated with an increased risk of new-onset LASs in female high school and collegiate soccer players. These findings will be useful when developing strategies to prevent LASs in young female soccer players.
Acknowledgments
The authors thank all the doctors, physical therapists, athletic trainers, and students who participated in the University of Tokyo Sports Science Initiative project as volunteer examiners.
Footnotes
Final revision submitted July 27, 2023; accepted August 10, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: Scholarship donations were received from East Japan Railway Company and Shimamura-Syoukai. Grants were received from the Nakatomi Foundation, Japan Sports Medicine Foundation, Japan Sport Council, Japanese Orthopaedic Society for Sports Medicine, Watanabe Memorial Foundation for the Advancement of New Technology, Japan Keirin Autorace Foundation, Japan Society for the Promotion of Science (KAKENHI 20K11358), Japan Orthopaedics Traumatology Foundation, and Japanese Orthopaedic Society of Knee, Arthroscopy and Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Tokyo (No. 11907-(2)).
References
- 1. Arnason A, Sigurdsson SB, Gudmundsson A, et al. Risk factors for injuries in football. Am J Sports Med. 2004;32(1)(suppl):5S-16S. [DOI] [PubMed] [Google Scholar]
- 2. Attenborough AS, Sinclair PJ, Sharp T, et al. The identification of risk factors for ankle sprains sustained during netball participation. Phys Ther Sport. 2017;23:31-36. [DOI] [PubMed] [Google Scholar]
- 3. Baumhauer JF, Alosa DM, Renström AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564-570. [DOI] [PubMed] [Google Scholar]
- 4. Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376-380. [PMC free article] [PubMed] [Google Scholar]
- 5. Carrasco AC, Silva MF, Guenka LC, et al. Non-radiographic validity and reliability measures for assessing foot types: a systematic review. Foot Ankle Surg. 2021;27(8):839-850. [DOI] [PubMed] [Google Scholar]
- 6. Chandran A, Moffit RE, DeJong Lempke AF, et al. Epidemiology of lateral ligament complex tears of the ankle in National Collegiate Athletic Association (NCAA) sports: 2014-15 through 2018-19. Am J Sports Med. 2023;51(1):169-178. [DOI] [PubMed] [Google Scholar]
- 7. Chandran A, Morris SN, Boltz AJ, Robison HJ, Collins CL. Epidemiology of injuries in National Collegiate Athletic Association women’s soccer: 2014-2015 through 2018-2019. J Athl Train. 2021;56(7):651-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clark T, Redding E. The relationship between postural stability and dancer’s past and future lower-limb injuries. Med Probl Perform Art. 2012;27(4):197-204. [PubMed] [Google Scholar]
- 9. De Cock A, Vanrenterghem J, Willems T, Witvrouw E, De Clercq D. The trajectory of the centre of pressure during barefoot running as a potential measure for foot function. Gait Posture. 2008;27(4):669-675. [DOI] [PubMed] [Google Scholar]
- 10. Doherty C, Delahunt E, Caulfield B, et al. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123-140. [DOI] [PubMed] [Google Scholar]
- 11. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for acute ankle injuries among male soccer players: a prospective cohort study. Scand J Med Sci Sports. 2010;20(3):403-410. [DOI] [PubMed] [Google Scholar]
- 12. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73-94. [DOI] [PubMed] [Google Scholar]
- 13. Fujitaka K, Taniguchi A, Isomoto S, et al. Pathogenesis of fifth metatarsal fractures in college soccer players. Orthop J Sports Med. 2015;3(9):2325967115603654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gabbe BJ, Finch CF, Wajswelner H, Bennell KL. Predictors of lower extremity injuries at the community level of Australian football. Clin J Sport Med. 2004;14(2):56-63. [DOI] [PubMed] [Google Scholar]
- 15. Hadzic V, Sattler T, Pori P, et al. Quadriceps strength asymmetry as predictor of ankle sprain in male volleyball players. J Sports Med Phys Fitness. 2022;62(6):822-829. [DOI] [PubMed] [Google Scholar]
- 16. Hartley EM, Hoch MC, Boling MC. Y-Balance Test performance and BMI are associated with ankle sprain injury in collegiate male athletes. J Sci Med Sport. 2018;21(7):676-680. [DOI] [PubMed] [Google Scholar]
- 17. Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54(6):572-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Howells BE, Ardern CL, Webster KE. Is postural control restored following anterior cruciate ligament reconstruction? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1168-1177. [DOI] [PubMed] [Google Scholar]
- 19. Kaminski TW, Hertel J, Amendola N, et al. National Athletic Trainers’ Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48(4):528-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kawaguchi K, Taketomi S, Mizutani Y, et al. Dynamic postural stability is decreased during the single-leg drop landing task in male collegiate soccer players with chronic ankle instability. Orthop J Sports Med. 2022;10(7):23259671221107343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kawaguchi K, Taketomi S, Mizutani Y, et al. Hip abductor muscle strength deficit as a risk factor for inversion ankle sprain in male college soccer players: a prospective cohort study. Orthop J Sports Med. 2021;9(7):23259671211020287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19(1):76-81. [DOI] [PubMed] [Google Scholar]
- 23. Kofotolis ND, Kellis E, Vlachopoulos SP. Ankle sprain injuries and risk factors in amateur soccer players during a 2-year period. Am J Sports Med. 2007;35(3):458-466. [DOI] [PubMed] [Google Scholar]
- 24. Mason J, Kniewasser C, Hollander K, Zech A. Intrinsic risk factors for ankle sprain differ between male and female athletes: a systematic review and meta-analysis. Sports Med Open. 2022;8(1):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McCann RS, Kosik KB, Terada M, et al. Acute lateral ankle sprain prediction in collegiate woman’s soccer players. Int J Sports Phys Ther. 2018;13(1):12-18. [PMC free article] [PubMed] [Google Scholar]
- 26. McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10(4):239-244. [DOI] [PubMed] [Google Scholar]
- 27. McLester CN, Nickerson BS, Kliszczewicz BM, McLester JR. Reliability and agreement of various InBody body composition analyzers as compared to dual-energy X-ray absorptiometry in healthy men and women. J Clin Densitom. 2020;23(3):443-450. [DOI] [PubMed] [Google Scholar]
- 28. Pasanen K, Ekola T, Vasankari T, et al. High ankle injury rate in adolescent basketball: a 3-year prospective follow-up study. Scand J Med Sci Sports. 2017;27(6):643-649. [DOI] [PubMed] [Google Scholar]
- 29. Powers CM, Ghoddosi N, Straub RK, Khayambashi K. Hip strength as a predictor of ankle sprains in male soccer players: a prospective study. J Athl Train. 2017;52(11):1048-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Scott DA, Bond EQ, Sisto SA, Nadler SF. The intra- and interrater reliability of hip muscle strength assessments using a handheld versus a portable dynamometer anchoring station. Arch Phys Med Rehabil. 2004;85(4):598-603. [DOI] [PubMed] [Google Scholar]
- 31. Söderman K, Alfredson H, Pietilä T, Werner S. Risk factors for leg injuries in female soccer players: a prospective investigation during one out-door season. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):313-321. [DOI] [PubMed] [Google Scholar]
- 32. Taketomi S, Kawaguchi K, Mizutani Y, et al. Anthropometric and musculoskeletal gender differences in young soccer players. J Sports Med Phys Fitness. 2021;61(9):1212-1218. [DOI] [PubMed] [Google Scholar]
- 33. Taketomi S, Kawaguchi K, Mizutani Y, et al. Musculoskeletal asymmetry in young soccer players: differences between the dominant and nondominant leg. Int J Hum Mov Sports Sci. 2022;10(2):294-302. [Google Scholar]
- 34. Watanabe H, Fujii M, Yoshimoto M, et al. Pathogenic factors associated with Osgood-Schlatter disease in adolescent male soccer players: a prospective cohort study. Orthop J Sports Med. 2018;6(8):2325967118792192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279-2284. [DOI] [PubMed] [Google Scholar]
- 36. Wikstrom EA, Cain MS, Chandran A, et al. Lateral ankle sprain and subsequent ankle sprain risk: a systematic review. J Athl Train. 2021;56(6):578-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Willems TM, Witvrouw E, Delbaere K, et al. Intrinsic risk factors for inversion ankle sprains in female subjects: a prospective study. Scand J Med Sci Sports. 2005;15(5):336-345. [DOI] [PubMed] [Google Scholar]


