Abstract
Increased awareness of the conditions associated with prenatal substance exposure may enhance care delivery among professionals working in child welfare. The ways in which prenatal substance exposure intersects with child welfare are critically important, yet prenatal substance exposure knowledge is uneven among these professionals. Also, caregivers may lack information that prepares them to care for children with prenatal substance exposure, particularly children with prenatal alcohol exposure. This study explores what professionals working in child welfare and caregivers know about prenatal substance exposure and prenatal alcohol exposure and their training and support needs.
Prenatal exposures to alcohol and other drugs, including prescription drugs, can result in long-term neurocognitive, developmental, and behavioral effects (Mattson et al., 2019; Guille & Aujla, 2019). Although some prenatal substance exposures1 may be identified at birth, other exposures—particularly alcohol—may not be identified until later in development (Wozniak et al., 2019; Coles, 2011). Yet identifying children who are substance-exposed, particularly alcohol-exposed, is important so that they can receive needed treatment and support to avoid negative long-term outcomes such as mental and physical health challenges, negative life outcomes (e.g., poor educational performance, homelessness, encounters with law enforcement, etc.) and child welfare (Bakhireva et al., 2018; Popova et al., 2020). Note that a 2014 article that reviewed 128 articles comparing the effects of a wide variety of drugs, including cocaine, marijuana, opioids, amphetamines, alcohol, and tobacco, concluded that “Alcohol was the most common substance associated with fetal anomalies,” including “alterations in the central nervous system development” (Viteri et al., 2015, p.405). As far back as 1996, the medical field has known that “Of all the substances of abuse (including cocaine, heroin, and marijuana), alcohol produces by far the most serious neurobehavioral effects in the fetus.” (Stratton et al., 1996). Yet the child welfare field and others have been slow to absorb this information, as indicated by the results described in this paper. Professionals who work with children may benefit from greater awareness of the signs, symptoms, associated conditions, and the short- and long-term effects of prenatal substance exposure, as well as strategies/services to mitigate effects and optimize outcomes.
For service providers (e.g., doctors, nurses, counselors) and professionals who work in child welfare2, the ways in which prenatal substance exposure intersects with child welfare involvement and outcomes are critically important (Burns et al., 2020; Petrenko et al., 2019) as awareness of a child’s prenatal exposure informs case workers’ assessments of the child’s needs and patterns of interactions in the family. For example, children with prenatal alcohol exposure can have difficulty paying attention, controlling their impulses, and regulating their behavior; they can easily forget previously learned material and lag behind their peers in being able to understand cause-and-effect relationships and learn from their own experiences (Wozniak et al., 2019; Novick Brown & Greenspan, 2022). Because these children often score in typical ranges of intelligence on standardized tests, these behaviors can be misinterpreted as defiance or purposeful misbehavior and can lead to extreme frustration on the part of the caregiver (Joseph et al., 2022; Kautz et al., 2020; Petrenko et al., 2016). Because of the parenting challenges associated with prenatal alcohol exposure, children with unrecognized prenatal exposure to alcohol may be at higher risk for preventable removal from the home by professionals working in child welfare (Joseph et al., 2022; Petrenko et al., 2016). For example, if professionals who work in child welfare do not know that children exposed to alcohol may have neurocognitive deficits that can lead to difficult behaviors, they may perceive parent frustration and parent-child conflict as evidence of poor parenting skills (Petrenko et al., 2016). Difficult behaviors are especially true for children who meet the criteria for a diagnosis falling under the umbrella of fetal alcohol spectrum disorders [FASDs] (Joseph et al., 2022). Once the underlying reason for difficult behaviors and other long-term effects of prenatal alcohol exposure is known, this may help professionals who work in child welfare to work with parents to reframe the frustration that they may experience as a logical response to challenging behaviors (Joseph et al., 2022). These professionals can then support parents in addressing this frustration through parenting strategies that have been shown to be effective in caring for children with an FASD (Marcellus & Badry, 2021; Pei et al., 2023).
Despite the benefits of having professionals who work in child welfare who are knowledgeable in prenatal substance exposure, research to date suggests that prenatal substance exposure knowledge is uneven among professionals who work in child welfare (Lloyd et al., 2018; McCormack et al., 2022). For example, in interviews with professionals working in a single urban public child welfare agency, most reported no training or formal classes related to prenatal substance exposure, and some provided incorrect information or held inaccurate assumptions about the effects of prenatal substance exposure (Usher et al., 2022). In studies outside of the U.S., researchers also found that professionals who work in child welfare had limited training and knowledge related to FASDs and that those who were knowledgeable had acquired this knowledge on their own (Curran & Danbrook, 2023; Gilbert et al., 2021).
Similarly, families (foster, kinship, and adoptive, hereafter referred to as “caregivers”) may lack information that prepares them to care for children with prenatal substance exposure, particularly children with prenatal alcohol exposure (Lee et al., 2018). Caregivers who do not understand that negative child behaviors are a result of an alcohol-based brain impairment may grow frustrated and angry (Joseph et al., 2022). Thus, children prenatally exposed to substances who are placed in temporary care may be at a higher risk of placement moves (Flannigan et al., 2021; Leathers et al., 2019). Since the effects of prenatal alcohol exposure are permanent and lifelong, caregivers may benefit from education to increase their knowledge of prenatal alcohol exposure and develop skills to better parent and access services for their children (Chasnoff et al., 2015; Marcellus & Badry, 2021). Currently, little is known about how caregivers are supported within child welfare contexts.
Information is lacking regarding how professionals working in child welfare obtain information regarding prenatal alcohol and other substance exposures and their impacts, how they use this information in case planning, and how they apply it to support caregivers (Richards et al., 2020). This study addresses this gap by exploring what professionals who work in child welfare and caregivers know about prenatal substance exposure and their perceived training needs.
Methods
The current study was part of a descriptive mixed methods study conducted in 22 local or regional public child welfare agencies across five geographically diverse states. States were purposively sampled to reflect contextual characteristics associated with child welfare practice (e.g., state vs. county administration) and geographic substance use patterns (e.g., indicators of opioid use). The study was funded by the Administration for Children and Families, Children’s Bureau with additional support through an interagency agreement with the Centers for Disease Control and Prevention, and aimed to explore prenatal substance exposure and prenatal alcohol exposure policies and practices as well as any gaps in knowledge and practice policies. To examine the extent of prenatal substance exposure and exposure-related knowledge and training among professionals who work in child welfare, and among caregivers of children with prenatal substance exposure in the child welfare system, interviews and surveys were conducted with professionals working in child welfare. In two of the five states, focus groups and interviews were conducted with caregivers of children with prenatal substance exposure. One objective of exploring the prenatal substance exposure knowledge of professionals who work in child welfare was to illuminate how to enhance training and provide tools and resources to better recognize and care for children with prenatal substance exposure and their families.
Data are drawn from three methods; surveys, interviews, and focus groups (see Table 1 for sample details by method). Findings from, and instruments utilized in a similar exploratory study (Usher et al., 2022) were reviewed, adapted, and expanded when developing the design and methods of the current study. Instruments were pilot tested to ensure clarity and alignment to the objectives of this study. Individual semi-structured interviews were conducted with 171 professionals working in child welfare. Six to nine interviews were conducted at each of the 22 sites. Each interview was approximately 45 minutes and included questions about training, sources of knowledge about prenatal substance exposure in general as well as prenatal alcohol exposure specifically, training needs, and questions about child welfare agency policies and practices to identify and care for children with prenatal substance exposure and support caregivers. Online surveys exploring similar topics were administered to 271 additional professionals in child welfare (see footnote 2). Interviews took up to 60 minutes to complete and surveys took up to 30 minutes to complete. In two of the five states, focus groups and interviews with caregivers were conducted that explored caregiver training experiences and knowledge of prenatal substance exposure, interactions with professionals working in child welfare regarding prenatal substance exposure, and recommendations for additional supports. Almost all caregivers (n = 44, 89%) reported caring for at least one child with known or suspected prenatal substance exposure (a desired selection criteria), including children with prenatal alcohol exposure.3 At each site, an agency liaison assisted the study team in identifying and recruiting the participants. Data collection occurred from fall 2018 through summer 2020. Due to travel and safety concerns during the COVID-19 pandemic, data collection in the fifth state was conducted virtually using slightly modified instruments.
Table 1.
Study Sample: Number of Participants by Method and Role
| Data collection method | Total in-person | Total virtual/phone | Total |
|---|---|---|---|
| State child welfare director interview | 2 | 3 | 5 |
| Local area child welfare director interview | 21 | 5 | 26 |
| Professionals in child welfare interview | 107 | 33 | 140 |
| Professionals in child welfare online survey | n/a | n/a | 271 |
| Caregiver focus group/interviewa | 23 | 21 | 44 |
In one state, virtual interviews were conducted with individual caregivers in lieu of in-person focus groups because of the COVID-19 pandemic. Twenty-three caregivers participated in four focus groups in one state and 21 caregivers participated in individual interviews in the other state.
Data Analysis
The study team conducted descriptive analyses within method (i.e., survey, interview, and focus group). Qualitative data were analyzed applying content analysis and theme identification (Williams & Moser, 2019; Vaismoradi et al., 2016), and were examined for frequency of code applications, code presence, and code co-occurrence to identify saliency and relative strength of themes. An iterative-inductive process helped establish inter-coder consensus and reliability (Cascio et al., 2019). Paired coding was conducted with 25% of transcripts, then coders discussed and resolved any paired coding discrepancies throughout the analysis.
The team examined quantitative data (survey and close-ended interview items) with descriptive statistics including frequencies, averages, percentages, and measures of variation. Descriptive data were produced by subgroups to explore data by type of informant (e.g., role), data source, or contextual factor (e.g., state- vs. county-administered child welfare systems) as relevant. The team employed crosstabs to explore relationships among constructs. Little variation was observed across sites or states which informed the decision to present the following results in aggregate.
Results
Study results address three primary questions: (1) What do professionals working in child welfare know about prenatal substance exposure and how do they obtain this knowledge and training? (2) How do caregivers obtain knowledge about prenatal substance exposure and how prepared are they to care for children with prenatal substance exposure and prenatal alcohol exposure? And (3) what do professionals working in child welfare and caregivers perceive as needs or gaps in training, knowledge, and supportive care? Quantitative and qualitative results are presented, along with illustrative quotes to provide additional context.
What do Professionals Working in Child Welfare Know about Prenatal Substance Exposure and how do they Obtain this Knowledge and Training?
Perceived Knowledge of Prenatal Substance Exposure
Professional interviewees and survey respondents were asked to rate their awareness of the effects of prenatal substance exposure. Most professionals who work in child welfare (71%) self-reported at least an intermediate level of general knowledge about the effects of prenatal substance exposure (see Figure 1). When professionals rated their knowledge of prenatal alcohol exposure, slightly fewer (68%) rated their knowledge as at least intermediate. Patterns were similar when examined by state and across different roles (not presented).
Figure 1.
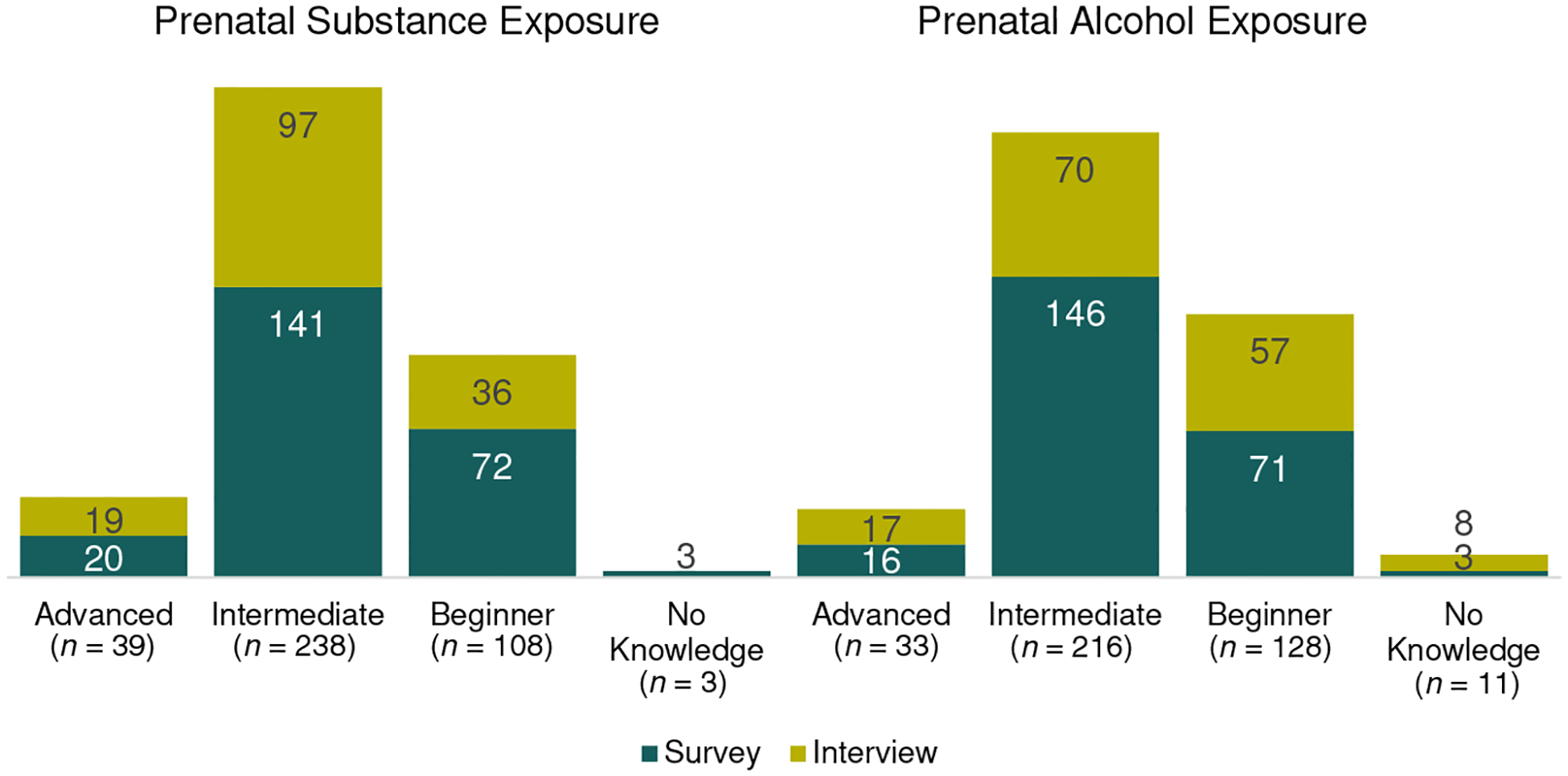
Self-reported Knowledge Level of Prenatal Substance Exposure and Prenatal Alcohol Exposure
Note: Number of professionals working in child welfare reporting advanced, intermediate, or beginner knowledge levels or no knowledge of prenatal substance exposure and prenatal alcohol exposure, respectively. Source: Closed-ended questions from professionals’ interviews and surveys in all five states; N = 152 interviews and 271 surveys (13% of survey responses [n = 35] were missing).
Specific Knowledge about Prenatal Alcohol Exposure
Survey respondents were asked to complete a “true/false” nine-item quiz on prenatal alcohol exposure and child development (see Table 2). Almost two thirds (64%) incorrectly responded that most children with an FASD have unusual facial features. Yet research indicates that 40% of children diagnosed with an FASD do not have facial features that may be associated with prenatal alcohol exposure (May et al., 2018). In subgroup analysis, those with the least experience in child welfare (0–5 years) had the lowest mean number of correct answers, and those with the most child welfare experience (> 20 years) had the highest mean number of correct answers (not presented).
Table 2.
Percentage of Correct Answers on Professionals’ Survey Prenatal Alcohol Exposure Knowledge Quiz
| Survey item | Number (Percentage) of Correct Responses |
|---|---|
| Women only need to avoid hard liquor during pregnancy; beer and wine are okay. (False) | 234 (99%) |
| Alcohol can harm an embryo or fetus at any time during pregnancy. (True) | 231 (97%) |
| There is no cure for fetal alcohol spectrum disorder, although treatment can mitigate some effects. (True) | 227 (96%) |
| A woman can have one or two drinks a day without causing harm to her baby since she isn’t binging. (False) | 223 (94%) |
| Women who drink early in pregnancy but stop drinking are not at risk for having a child with a fetal alcohol spectrum disorder. (False) | 214 (90%) |
| Alcohol use during pregnancy is the leading known cause of developmental disability and birth defects in the United States. (True) | 208 (88%) |
| Fetal alcohol spectrum disorders occur only if the mother is an alcoholic during pregnancy. (False) | 203 (86%) |
| Of all substances of abuse, alcohol produces the most serious neurobehavioral effects in the fetus. (True) | 176 (74%) |
| Most children with a fetal alcohol spectrum disorder have unusual facial features. (False) | 85 (36%) |
Note. Number and percentage of survey respondents who responded correctly to true/false survey items in prenatal alcohol exposure knowledge quiz.
Later in the survey, respondents were asked to identify the effects of prenatal alcohol exposure on a child, and similar to responses on the true/false quiz, a high proportion of respondents cited abnormal facial features (85%). Surveyed professionals were also asked an open-ended question: “What type of prenatal substance exposure is most harmful?” Research has shown that alcohol is the most harmful substance to the developing fetus and that these infants have significant long-term neurodevelopmental effects (Wozniak et al., 2019). Only one quarter of professionals (24%) correctly answered “alcohol.” The largest proportion (39%) of professionals identified multiple or all substances, followed by opioids (7%) and methamphetamine (4%) as being most harmful.
Extent and Sources of Training on Prenatal Alcohol and other Substance Exposures
The majority of professionals working in child welfare (82% of survey respondents and 79% of interviewees) reported receiving training in prenatal substance exposure and prenatal alcohol exposure, yet there were gaps in training experiences. Sixty percent of survey respondents reported participating in training on indicators and effects of prenatal substance exposure through their state child welfare agency as part of their employment. However, in interviews, less than two-thirds of professionals who work in child welfare indicated that agency trainings included information specifically on prenatal alcohol exposure. These professionals often mentioned state and agency training and professional development opportunities that specifically focused on current parental substance use and identification of newborns who are substance-exposed (e.g., indicators, effects, and care needs of infants with neonatal abstinence syndrome who have been exposed to drugs, most often opioids). The lack of attention on alcohol-related impacts, and corresponding faulty assumptions resulting from that gap emerged strongly in interviews. One professional who works with families at the front end of a case only (frontline) noted “I would like to learn more about alcohol especially … Because of the opioid epidemic that we’re in, it’s like alcohol kind of gets pushed back.” A professional with investigation and needs assessment responsibilities stated “I would have to say drugs are more harmful because they have the worst effect on a child. I am not sure what effects alcohol has to a child because I do not have any training or understanding on its effects.” One fifth (21%) of interviewees reported no or minimal training in either prenatal substance exposure or prenatal alcohol exposure.
How do Caregivers Obtain Knowledge about Prenatal Substance Exposure and how Prepared are they to Care for Children with Prenatal Substance Exposure and Prenatal Alcohol Exposure?
Extent and Sources of Training for Caregivers
In the two states with data from caregivers, almost half of caregivers (43%) reported receiving formal training on prenatal substance exposure as part of their initial orientation from child welfare agencies. However, 14% of caregivers reported never receiving information or training related to prenatal substance exposure from the child welfare agency. Across the five states included in this study, only one third (34%) of professionals reported that they were aware of whether caregiver trainings addressed prenatal substance exposure.
One third (33%) of caregivers who stated they had cared for a child with prenatal substance exposure reported they were not at all prepared to care for the child. As one caregiver explained, “No, I did not feel prepared. I feel like they were like, ‘Here’s your kid, we will be back in a month and check on them and make sure you take them to the doctor.’”
What do Professionals who Work in Child Welfare and Caregivers Perceive as Needs or Gaps in Training, Knowledge, and Supportive Care?
Needs Perceived by Professionals
The most common knowledge gaps or areas for training mentioned by professionals reflected the need to understand the indicators and pathways of prenatal substance exposure and prenatal alcohol exposure, long-term effects, and how to identify prenatal substance exposure and prenatal alcohol exposure among families involved with child welfare (see Table 3). As one frontline professional shared, “Our agency needs more training in those topics that can tell us about how to look for [prenatal substance exposure] in different developmental stages and different ages of children.” Professionals described methods to enhance training in these areas, noting the importance of ongoing training, as one professional working with families on a longer-term basis (e.g., ongoing case management) described, “I really think to learn it, ongoing training is what’s important…reviewing information at different points instead of having a training…and then [again] five years down the road.” Professionals also noted the need to receive high-quality instruction and guidance as noted by a local area director: “I think if we had an expert come in to talk about prenatal substance exposure, what it looks like, what are the symptoms, what would be a good line of questioning or observation depending on the age of the child. Those are tools that case managers and supervisors can latch onto immediately.” About one quarter of professionals who work in child welfare interviewed also wanted resources, tools, and interventions to expand their professional capacity to support families, and 13% identified a specific need for agencies to have readily available educational materials to provide to caregivers. Some comments reflecting these themes:
Table 3.
Perceived Training Needs and Requests of Child Welfare Professionals (n = 171)
| Training need | n (percentage) |
|---|---|
| Indicators of prenatal substance exposure and prenatal alcohol exposure | 83 (48%) |
| Long-term effects of prenatal substance exposure and prenatal alcohol exposure | 57 (33%) |
| Identification processes | 39 (23%) |
| Resources, tools, and services | 40 (23%) |
| Educate and support caregivers | 22 (13%) |
| Enhanced methods of training, including ongoing training and training conducted by experts | 46 (27%) |
Note. Response categories are not exclusive, and each respondent could have contributed to multiple categories. Source: Interviews with all professionals who work in child welfare across the five states.
“It would be great if hospitals would share the information that they give parents, to teach us about what to look out for.”
—Frontline professional
“I’d like to learn a lot more to be able to educate parents on the dangers of all this, and I can’t share this information if I’m not taught this information.”
—Ongoing case management professional
“[We need information that addresses] what…the caretakers need to do to help this child when they get home.”
—Frontline professional
Needs Perceived by Caregivers
Similar needs were expressed by caregivers, the majority of whom (84%) wanted additional training. When interviewed about knowledge gaps or areas for training regarding prenatal substance exposure, the most common information needs focused on how to identify prenatal substance exposure, the impact of prenatal substance exposure, and available interventions for the children in their care who may have been prenatally exposed (see Table 4).
Table 4.
Perceived Training Needs and Requests of Caregivers Raised in Focus Groups and Interviews
| Training need |
|---|
How to identify prenatal substance exposure, including:
|
| Knowing what to expect when parenting children with prenatal substance exposure across development |
| Available interventions, services, or resources for these children or caregivers |
| Training provided to professionals to enhance their ability to support caregivers related to the topics noted in rows above |
Note. Not all caregivers provided a suggestion on training needs (25 of 45 total participants raised needs).
Some comments reflecting these themes:
“I think identification is the most important, knowing what to look for because there are physiological signs that we can teach people that would get people or kids into support earlier and faster.”
—Caregiver
“I would like to know more about the overall impact on their psychological and physical development, specifically with alcohol, marijuana, illicit drugs, and tobacco.”
—Caregiver
“I now have a baby who was drug exposed to multiple different drugs and I don’t know how those all play together. I have no idea. I don’t know what to look for. I don’t know as they grow older if there’s something that could be pinpointed toward drug exposure or if that’s just a normal, typical toddler behavior…I’ve never had any kind of training on that and that would be super useful.”
—Caregiver
“Knowing what to expect and then that treatment options can actually save on some foster failures or moving a child from home to home to home because that doesn’t fix the problem.”
—Caregiver
As an extension of wanting to know how to identify prenatal substance exposure, caregivers wanted to learn how to distinguish between prenatal substance exposure-related cognitive and developmental delays, and those caused by other conditions. As one caregiver described, “Like how to identify the difference, or some of the signs or symptoms as it relates to being exposed to drugs or is it just from not having a caregiver with the child that [has been] educated in parenting [children who have been impacted].” In addition, caregivers expressed the need for prenatal substance exposure information specific to the individual children for whom they are caring, including the substance(s) a child was exposed to and the amount and duration of exposure, if known.
Across both groups of participants (professionals and caregivers) there also was a lack of awareness about available services for children prenatally exposed to substances. As one case management professional noted, “To be honest with you, I will have to rely on the doctor’s office because I personally know of no other services [for children with prenatal substance exposure] that are for children over three.”
Discussion
This multisite mixed-methods descriptive study examined gaps in training and knowledge in child welfare related to prenatal substance exposure, with special emphasis on prenatal alcohol exposure. While professionals reported high levels of perceived awareness and knowledge of prenatal alcohol and other drug exposures, they also discussed the need to better understand differential indicators of specific substances/polysubstance use and their developmental pathways, as well as interventions to integrate into service plans and to support caregivers. The findings illustrate the need for increased, or updated, training and resources for professionals working in child welfare and caregivers so that they can better serve and care for children with prenatal substance exposure. The following discussion draws links between identified gaps and opportunities to develop resources to address gaps.
Despite widespread awareness of prenatal substance exposure, professionals have key misperceptions about prenatal substance exposure effects that likely affect practice and offer important targets for improvements. Most respondents rated their prenatal substance exposure and prenatal alcohol exposure knowledge as intermediate, and most responded correctly to seven of the nine true/false items in prenatal alcohol exposure knowledge quiz. Yet most professionals who work in child welfare falsely believed that all, or almost all, children with FASDs have distinct facial features. This is not present in children with alcohol-related neurodevelopmental disorder (ARND), which may occur in 40% of children diagnosed with an FASD (May et al., 2018). This reliance on facial characteristics may result in underestimation of FASDs. Some of these professionals tended to incorrectly perceive that the substances that result in worse long-lasting effects were those substances they see most often among newborns and infants referred to child welfare—opioids, methamphetamines, cocaine, etc.—rather than those substances known to cause lifelong, significant neurodevelopmental effects, such as alcohol. Research suggests that polysubstance use is frequent, even among women who are pregnant (England et al., 2020). Without professional awareness to consider alcohol exposure as potentially part of prenatal substance exposure relevant to the child welfare case, the opportunity to obtain important information needed for differential diagnosis across development may be overlooked or lost. As noted in Wang and colleagues (2023), professionals in child welfare rely primarily on hospital and medical tests to identify prenatal substance exposure at birth, but this focus on children who are younger can lead to under-identification of prenatal alcohol exposures and subsequent gaps in services particularly for children that are an older age. The results from this study suggest that more in-depth and ongoing training on prenatal substance exposure and prenatal alcohol exposure may enhance care provided by professionals working in child welfare and caregivers, or if trainings are already in place, auditing them so that the most accurate and current information is presented. Consideration of prenatal alcohol exposure and resulting conditions (FASDs) may be needed given their lifelong effects as well as the frequency of alcohol use with other drugs (i.e., polysubstance use). It is well established that child welfare agencies have high rates of turnover (Willis et al., 2016) and in this study, professionals who had fewer years of experience self-perceived lower levels of knowledge, which emphasizes the importance of ongoing training on prenatal substance exposure vs. one-time instruction. Professionals who work in child welfare spoke about the challenges of infrequent trainings on prenatal substance exposure. Self-guided trainings, such as prerecorded webinars or interactive learning sessions, may help address this issue given time constraint for overburdened child welfare professionals. Even with some knowledge, professionals may find it difficult to apply prenatal substance exposure information to their work. Professionals benefit from in-depth resources and training—that include practice and coaching—to obtain a prenatal substance exposure history, identify children affected by prenatal substance exposure, understand effects on development and parenting implications, and effectively refer caregivers to appropriate and available interventions (Chasnoff et al., 2015; McCormack et al., 2022).
Professionals working in child welfare raised a need for accurate training information from experts, given the evolving knowledge base related to prenatal substance exposure. A recent exploration of professionals’ perceptions of successful training experiences (Radey & Stanley, 2019) emphasized five attributes: structured, non-redundant content relevant to their positions; interactive content delivery; practice with job responsibilities; practice with system protocols; and recognition of the ongoing and constant learning process. The researchers suggested that trainings that consider workers’ knowledge level and position; offer step-by-step procedural manuals and checklists; and establish agency policies that foster mentorship and support will likely engender the most successful transfer of knowledge, skills, and competencies. Other research has emphasized the importance of simulation (use of case scenarios, practice, coaching) and reflective supervision (Julien-Chinn & Lietz, 2019; Kourgiantakis et al., 2020), and providing training to all professionals who work in child welfare (beyond frontline, including agency leadership), not simply those who elect to participate voluntarily (Kuhn et al., 2019). These principles could be applied to develop new training on prenatal substance exposure or to modify existing agency training.
Targeted resources for professionals and supervisors working in child welfare may support both their own knowledge and their practice with families. These professionals would benefit from access to informational materials to which they can refer at any point in a case. In this study, they indicated wanting information and tangible resources on indicators of prenatal substance exposure and the effects of prenatal substance exposure through a child’s life, for quick reference in their ongoing work and to share with caregivers. Professionals working in child welfare rely on general developmental or medical assessments to identify children with prenatal substance exposure; however, these services do not include focused attention to gathering information about prenatal exposure history (Wang et al., 2023) and more targeted resources could help ensure children are being connected to more targeted and specialized care. Both professionals and caregivers noted resources could outline the types of services that are appropriately matched and available to children affected by prenatal alcohol and/or other substances and their families, including child-focused interventions (e.g., social-emotional-behavioral interventions) and parenting and family-based interventions (Pei et al., 2023). These materials would not only assist the professionals to solidify their own knowledge and awareness but also build competency to recognize presenting behaviors and needs of children who are or may be affected by prenatal substance exposure, and to discuss the presence of prenatal substance exposure as well as possible available services with caregivers. Caregivers also noted the need for and requested more in-depth specialized training and learning opportunities. The majority of caregivers participated in trainings that included material related to prenatal substance exposure, most often as a brief component in state agency-provided orientations to becoming a foster parent. Yet even among this sample of caregivers who had experience caring for children with suspected or known prenatal exposures, some for children with diagnosed conditions such as an FASD, only 18% of caregivers reported that they were “fully prepared” in advance to care for these children. “On-the-job” learning and individual internet searches were deemed insufficient by caregivers. Improved caregiver education related to prenatal substance exposure, and FASDs in particular, regarding effects on child development/developmental pathways, implications for caregiving/parenting, and appropriate as well as available interventions for affected children may reduce caregiver stress and improve caregiver-child interactions (Cleversey et al., 2017; Petrenko et al., 2016). Caregivers from the two states perceived professionals as also needing training in these areas to better partner with and support caregivers on behalf of children with prenatal substance exposure.
The training and resources suggested by professionals and caregivers in the study also could be applied to support biological parents and mitigate further involvement in child welfare. If prenatal substance exposure—especially prenatal alcohol exposure—is not understood, parents may misinterpret challenging behaviors as disobedience rather than brain-based impairments (Joseph et al., 2022; Petrenko et al., 2016). This may, in turn, contribute to frustration, parent-child conflict, and parental stress leading to an increased risk of child maltreatment and repeated cycles of abuse and/or neglect. Identification of prenatal substance exposure and prenatal alcohol exposure, combined with relevant training and education about exposure effects and parenting strategies, can alter the parent-child dynamic through improved understanding of the cause of child behaviors. This improved parental understanding has the potential to reduce future harm and prevent unnecessary entry or reentry into foster care (Flannigan et al., 2021; Joseph et al., 2022). Child welfare agencies could consider providing biological parents with access to training developed for caregivers related to prenatal substance exposure and FASDs and their effects on child development and parenting.
Study Limitations
This study has some limitations. First, this study is exploratory and descriptive, and although agencies were selected to represent diverse child welfare practice and geography, results are not generalizable to other state and local agencies. Some relevant data were limited (e.g., data collection with caregivers only occurred in two states) or not collected in the study (e.g., training materials from state agencies other than those publicly available). Data collection did not include exploration of the preferred instructional modalities (e.g., online vs. in-person training; individually focused vs. supervisory team-focused training, etc.).
Although a diverse group of caregivers (foster, kinship, and adoptive) provided important viewpoints, the study lacks parent of origin perspectives. Future work that includes parents of origin would be helpful. Finally, although not sufficiently assessed as a focal point, this research acknowledges the effects of racial and socioeconomic disparities that exist within the child welfare system (Harp & Bunting, 2020) since this study also encountered an understanding of the disproportionate number of women who were Black and low-income that may be reported to child welfare because of substance use during pregnancy (Chasnoff et al., 2018; Rebbe et al., 2019; Weber et al., 2021). It likewise acknowledges that those children exposed to substances that may be more commonly used among minority communities—but that are not more harmful to the child (e.g., cocaine, amphetamines)—may have higher rates of removal than those children exposed to substances more prevalent in White communities (e.g., alcohol, opioids; Rebbe et al., 2019; Prindle et al., 2018). These factors merit consideration in future steps to train professionals to effectively and equitably address prenatal substance exposure within the child welfare field to avoid oversurveillance, disproportionate involvement, and disparate outcomes for children and families of color. Such efforts could add significantly to the field by including that aspect of the population that comes into contact with the child welfare system. This important subject is addressed in greater detail in a separate article by Richards and colleagues (2023).
Summary
This study was conducted to explore what professionals working in child welfare and caregivers know about prenatal substance exposure, emphasizing prenatal alcohol exposure, and their perceived training needs. This was part of a descriptive mixed methods study conducted in 22 local child welfare agencies across five states. Findings showed that despite widespread awareness of prenatal substance exposure, professionals have misperceptions about prenatal substance exposure effects that likely affect practice and offer important targets for improvements. Professionals and caregivers also raised targeted needs and requests for more training in many areas. Findings from this study provide initial insights into the knowledge, policies, practice, and educational needs of child welfare agencies, professionals who work in child welfare, and caregivers. Professionals and agencies can use these findings to inform approaches, practices and trainings which may help improve developmental outcomes for children and improve family functioning, thereby reducing the risk of child maltreatment and foster care placements. This study adds to the limited research published on professional’s knowledge of prenatal substance exposure and to practical child welfare training applications.
Footnotes
Note: The findings and conclusions in this report are those of the authors and do not necessarily represent the offi cial position of the Centers for Disease Control and Prevention, the Children’s Bureau of the Administration for Children and Families, or the Department of Health and Human Services.
Throughout this article, references to “prenatal substance exposure” include both alcohol and other types of legal and illegal substances (e.g., opioids, cocaine, nicotine, etc.). In some instances, the article will explore findings that are unique to prenatal alcohol exposure vs. other types of substances.
Th roughout this article, references made to “professionals in child welfare” could include the following types of child welfare roles/positions: hotline/intake; investigative; frontline; family needs assessors; ongoing case management; supervisors; local and state child welfare directors; data administrators; and child welfare specialists such as prevention, permanency, and developmental assessors.
Note that caregivers who had experience with children who have prenatal substance exposure and/or prenatal alcohol exposure were prioritized to participate which most likely impacted results.
Contributor Information
Erin Morehouse, James Bell Associates.
Erin Ingoldsby, James Bell Associates.
Sharon Newburg-Rinn, Children’s Bureau, Administration for Children and Families U.S. Department of Health and Human Services.
Jacquelyn Bertrand, National Center on Birth Defects and Developmental Disabilities Centers for Disease Control and Prevention.
Kristen Usher, ICF.
References
- Bakhireva LN, Garrison L, Shrestha S, Sharkis J, Miranda R, & Rogers K (2018). Challenges of diagnosing fetal alcohol spectrum disorders in foster and adopted children. Alcohol, 67, 37–43. 10.1016/j.alcohol.2017.05.004 [DOI] [PubMed] [Google Scholar]
- Burns J, Badry DE, Harding KD, Roberts N, Unsworth K, & Cook JL (2021). Comparing outcomes of children and youth with fetal alcohol spectrum disorder (FASD) in the child welfare system to those in other living situations in Canada: Results from the Canadian National FASD Database. Child: Care, Health and Development, 47(1), 77–84. 10.1111/cch.12817 [DOI] [PubMed] [Google Scholar]
- Cascio MA, Lee E, Vaudrin N, & Freedman DA (2019). A team-based approach to open coding: Considerations for creating intercoder consensus. Field Methods, 31(2), 116–130. 10.1177/1525822X19838237 [DOI] [Google Scholar]
- Chasnoff IJ, Barber G, Brook J, & Akin BA (2018). The Child Abuse Prevention and Treatment Act: Knowledge of health care and legal professionals. Child Welfare, 96(3), 41–58. https://www.jstor.org/stable/48623615 [Google Scholar]
- Chasnoff IJ, Wells AM, & King L (2015). Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics, 15(3), 264–270. 10.1542/peds.2014-2171 [DOI] [PubMed] [Google Scholar]
- Cleversey K, Brown J, & Kapasi A (2017). Educating adolescents with fetal alcohol spectrum disorder: Caregiver support needs. Journal of Child and Family Studies, 26, 2843–2851. 10.1007/s10826-017-0776-7 [DOI] [Google Scholar]
- Coles CD (2011). Discriminating the effects of prenatal alcohol exposure from other behavioral and learning disorders. Alcohol Research & Health, 34(1), 42. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860548/ [PMC free article] [PubMed] [Google Scholar]
- Curran WC, & Danbrook MC (2023). Hearing the voice of child welfare social workers: planning safe care for a child with or suspected of having fetal alcohol spectrum disorders (FASDs). Advances in Dual Diagnosis (online ahead of print). https://www.emerald.com/insight/content/doi/10.1108/ADD-04-2022-0014/full/html [Google Scholar]
- England LJ, Bennett C, Denny CH, Honein MA, Gilboa SM, Kim SY, Guy GP, Tran EL, Rose CE, Bohm MK, & Boyle CA (2020). Alcohol use and co-use of other substances among pregnant females aged 12–44 years – United States, 2015–2018. Morbidity and Mortality Weekly Report, 69(31), 1009–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannigan K, Kapasi A, Pei J, Murdoch I, Andrew G, & Rasmussen C (2021). Characterizing adverse childhood experiences among children and adolescents with prenatal alcohol exposure and Fetal Alcohol Spectrum Disorder. Child Abuse & Neglect, 112(104888). 10.1016/j.chiabu.2020.104888 [DOI] [PubMed] [Google Scholar]
- Gilbert DJ, Mukherjee RA, Kassam N, & Cook PA (2021). Exploring the experiences of social workers in working with children suspected to have fetal alcohol spectrum disorders. Adoption & Fostering, 45(2), 155–172. 10.1177/03085759211011735 [DOI] [Google Scholar]
- Guille C, & Aujla R (2019). Developmental consequences of prenatal substance use in children and adolescents. Journal of Child and Adolescent Psychopharmacology, 29(7), 479–486. 10.1089/cap.2018.0177 [DOI] [PubMed] [Google Scholar]
- Harp KL, & Bunting AM (2020). The racialized nature of child welfare policies and the social control of Black bodies. Social Politics: International Studies in Gender, State & Society, 27(2), 258–281. 10.1093/sp/jxz039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph JJ, Mela M, & Pei J (2022). Aggressive behaviour and violence in children and adolescents with FASD: A synthesizing review. Clinical psychology review, 94, 102155. 10.1016/j.cpr.2022.102155 [DOI] [PubMed] [Google Scholar]
- Julien-Chinn FJ, & Lietz CA (2019). Building learning cultures in the child welfare workforce. Children and Youth Services Review, 99, 360–365. 10.1016/j.childyouth.2019.01.023 [DOI] [Google Scholar]
- Kautz C, Parr J, & Petrenko CL (2020). Self-care in caregivers of children with FASD: How do caregivers care for themselves, and what are the benefits and obstacles for doing so?. Research in developmental disabilities, 99, 103578. 10.1016/j.ridd.2020.103578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kourgiantakis T, Sewell KM, Hu R, Logan J, & Bogo M (2020). Simulation in social work education: A scoping review. Research on Social Work Practice, 30(4), 433–450. 10.1177/1049731519885015 [DOI] [Google Scholar]
- Kuhn T,M, Cyperski MA, Shaffer AM, Gracey KA, Adams MK, Billings GM, & Eber JS (2019). Installing trauma-informed care through the Tennessee Child Protective Services Academy. Psychological Services, 16(1), 143–152. 10.1037/ser0000320 [DOI] [PubMed] [Google Scholar]
- Leathers SJ, Spielfogel JE, Geiger J, Barnett J, & Voort BLV (2019). Placement disruption in foster care: Children’s behavior, foster parent support, and parenting experiences. Child Abuse & Neglect, 91, 147–159. 10.1016/j.chiabu.2019.03.012 [DOI] [PubMed] [Google Scholar]
- Lee BR, Kobulsky JM, Brodzinsky D, & Barth RP (2018). Parent perspectives on adoption preparation: Findings from the Modern Adoptive Families project. Children and Youth Services Review, 85, 63–71. 10.1016/j.childyouth.2017.12.007 [DOI] [Google Scholar]
- Lloyd MH, Akin BA, Brook J, & Chasnoff IJ (2018). The policy to practice gap: Factors associated with practitioner knowledge of CAPTA 2010 mandates for identifying and intervening in cases of prenatal alcohol and drug exposure. Families in Society, 99(3), 232–243. 10.1177/1044389418785326 [DOI] [Google Scholar]
- Marcellus L, & Badry D (2021). Infants, children, and youth in foster care with prenatal substance exposure: a synthesis of two scoping reviews. International Journal of Developmental Disabilities, 1–26. 10.1080/20473869.2021.1945890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson SN, Bernes GA, & Doyle LR (2019). Fetal alcohol spectrum disorders: Neurobehavioral deficits associated with prenatal alcohol exposure. Alcoholism Clinical and Experimental Research, 43(6), 1046–1042. 10.1111/acer.14040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Chambers CD, Kalberg WO, Zellner J, Feldman H, Buckley D, … & Hoyme HE (2018). Prevalence of fetal alcohol spectrum disorders in 4 US communities. JAMA, 319(5), 474–482. doi:10.1001/jama.2017.21896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack JC, Chu JTW, Marsh S, & Bullen C (2022). Knowledge, attitudes, and practices of fetal alcohol spectrum disorder in health, justice, and education professionals: A systematic review. Research in Developmental Disabilities, 131, 104354. 10.1016/j.ridd.2022.104354 [DOI] [PubMed] [Google Scholar]
- Novick Brown N, & Greenspan S (2022). Diminished culpability in fetal alcohol spectrum disorders (FASD). Behavioral Sciences & the Law, 40(1), 1–13. 10.1002/bsl.2535 [DOI] [PubMed] [Google Scholar]
- Pei J, Kapasi A, & Rasmussen C (2023). Fetal Alcohol Spectrum Disorder: Interventions. In Neurodevelopmental Pediatrics: Genetic and Environmental Influences (pp. 457–465). Cham: Springer International Publishing. 10.1007/978-3-031-20792-1_29 [DOI] [Google Scholar]
- Petrenko CL, Alto ME, Hart AR, Freeze SM, & Cole LL (2019). “I’m doing my part, I just need help from the community”: Intervention implications of foster and adoptive parents’ experiences raising children and young adults with FASD. Journal of Family Nursing, 25(2), 314–347. 10.1177/1074840719847185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrenko CL, Pandolfino ME, & Roddenberry R (2016). The association between parental attributions of misbehavior and parenting practices in caregivers raising children with prenatal alcohol exposure: A mixed-methods study. Research in Developmental Disabilities, 59, 255–267. 10.1016/j.ridd.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popova S, Dozet D, & Burd L (2020). Fetal alcohol spectrum disorder: can we change the future?. Alcoholism, clinical and experimental research, 44(4), 815. 10.1111/acer.14317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prindle JJ, Hammond I, & Putnam-Hornstein E (2018). Prenatal substance exposure diagnosed at birth and infant involvement with child protective services. Child Abuse & Neglect, 76, 75–83. 10.1016/j.chiabu.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Radey M, & Stanley L (2019). Beginning the “never-ending” learning process: Training experiences of newly-hired child welfare workers. Children and Youth Services Review, 104 (104378). 10.1016/j.childyouth.2019.06.013 [DOI] [Google Scholar]
- Rebbe R, Mienko JA, Brown E, & Rowhani-Rahbar A (2019a). Hospital variation in child protection reports of substance exposed infants. The Journal of Pediatrics, 208, 141–147. 10.1016/j.jpeds.2018.12.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards T, Bertrand J, Newburg-Rinn S, McCann H, Morehouse E, & Ingoldsby E (2020). Children prenatally exposed to alcohol and other drugs: What the literature tells us about child welfare information sources, policies, and practices to identify and care for children. Journal of Public Child Welfare, 16(1), 71–94. 10.1080/15548732.2020.1814478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards T, Miller N, Eaton E, Newburg-Rinn S, & Bertrand J (2023). Challenges and opportunities to care for children in child welfare with fetal alcohol spectrum disorders while working towards preserving their families. Child Welfare, 101(3), 2092013234. [PMC free article] [PubMed] [Google Scholar]
- Stratton K, Howe C, & Battaglia FC (Eds.). (1996). Fetal alcohol syndrome: Diagnosis, epidemiology, prevention, and treatment. National Academies Press. [Google Scholar]
- Usher K, Brizzo A, Leicht C, Newburg-Rinn S, Reynolds MR, McCann H, & Bertrand J (2022) Child welfare policies and practices regarding children with prenatal exposure to alcohol and other drugs: An exploratory study. Child Welfare, 99(6). https://www.proquest.com/openview/3cc21ae3acb45b8d1cc54417d0ecc644/1 [PMC free article] [PubMed] [Google Scholar]
- Vaismoradi M, Jones J, Turunen H, & Snelgrove S (2016). Theme development in qualitative analysis and thematic analysis. Journal of Nursing Education and Practice, 6(5), 100–110. 10.5430/jnep.v6n5p100 [DOI] [Google Scholar]
- Viteri OA, Soto EE, Bahado-Singh RO, Christensen CW, Chauhan SP, & Sibai BM (2014). Fetal anomalies and long-term effects associated with substance abuse in pregnancy: a literature review. American Journal of Perinatology, 32(5), 405–416. doi:10.1055/s-0034-1393932 [DOI] [PubMed] [Google Scholar]
- Wang K, Richards T, Kopiec K, Newburg-Rinn S, & Bertrand J (2023). Exploring child welfare practices to care for children with prenatal substance exposure. Child Welfare, 101(2), 141–168. [PMC free article] [PubMed] [Google Scholar]
- Weber A, Miskle B, Lynch A, Arndt S, & Acion L (2021). Substance use in pregnancy: identifying stigma and improving care. Substance Abuse and Rehabilitation, 105–121. 10.2147/SAR.S319180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M, & Moser T (2019). The art of coding and thematic exploration in qualitative research. International Management Review, 15(1), 45–55. http://www.imrjournal.org/uploads/1/4/2/8/14286482/imr-v15n1art4.pdf [Google Scholar]
- Willis N, Chavkin N, & Leung P (2016). Finding “health” and “meaning” in Texas-sized turnover: Application of seminal management principles for administration and research in U.S. public child welfare agencies. Advances in Social Work, 17(2), 116–133. 10.18060/20856 [DOI] [Google Scholar]
- Wozniak JR, Riley EP, & Charness ME (2019). Clinical presentation, diagnosis, and management of fetal alcohol spectrum disorder. The Lancet Neurology, 18(8), 760–770. 10.1016/S1474-4422(19)30150-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


