Abstract
Some of the vernacular or scientific names are related to possible medicinal and/or toxic properties that can reveal the presence of potential bioactive agents, contributing to the discovery of new drugs and/or knowledge of the risks associated with their use. This study sought to list the scientific and vernacular names of plants whose lexicons are related to those possible properties of plants and to compare them with the “ethno” (ethnobotanical and ethnopharmacological) and pharmacological data available in the scientific literature. A floating reading of the two classical and reference works on Brazilian medicinal plants was performed, and plants with vernacular and/or scientific names related to the possible medicinal and/or toxic properties were listed. Correlations between the meanings of the species' names (lexicon) and their possible biological properties were made from their translation from Latin by consulting dictionaries. A bibliographic survey was conducted on the “ethno” and pharmacological data for each species. Finally, data from these three dimensions (lexicon, “ethno,” and pharmacology) were classified and compared using a bioprospection classification. It resulted in a list of 90 plant species belonging to 47 families. 66 of the 90 species presented “ethno” data from the scientific literature, while 46 species presented pharmacological data. Of these, 46 (69.7%) and 27 (58.7%), respectively, showed equivalence with the possible medicinal and/or toxic properties of plants according to their lexicons. According to this study, half of the plants investigated demonstrate equivalence in the three dimensions analyzed (lexicons, “ethno,” and pharmacological data from the scientific literature). Gastrointestinal and nervous system categories are among the most common in all three dimensions. Plant lexicons may be closely linked to the possible medicinal and/or toxic properties and the study of plant lexicons may represent one more approach for the search for new drugs, mainly considering the gastrointestinal, nervous, and parasites categories.
1. Introduction
Taxonomy, which is based on identification, description, nomenclature, and classification, is an extremely important area and one of the oldest disciplines in biology [1, 2]. A taxon, a grouping of defined organisms in which living beings are classified hierarchically [3], follows a classification code consolidated by Carolus Linnaeus in the 18th century. This classification is based on a binomial system to define the genus and species of each living organism. Currently, the botanical nomenclature for algae, fungi, and plants is regulated by the International Nomenclature Code (CIN), but it still follows the binomial standard proposed by Linnaeus. The binomial is composed of the genus, specific epithet, and followed by the name(s) of the author(s). Both generic names and epithets are always latinized and follow the international code. It is important to note that although each taxonomic group has only one valid name, a group can present several synonyms according to its classification over time [4]. In addition, consensus among taxonomists about a valid name is not always reached on the accuracy of the plant nomenclature. Thus, there are ongoing debates on the validity of a given botanical name.
In general, the generic epithet provides information on the taxon to which the organism belongs, and the specific epithet can refer to the morphological, environmental, or toponymic characteristics of the plant, to popular knowledge of the plant, and to its organoleptic properties, biological activities, medicinal/toxic applications, or the honour of people and others [5, 6]. In this sense, an interesting example is Papaver somniferum, whose generic epithet refers to the family to which it belongs “Papaveraceae,” and the specific epithet “somniferum” is associated with sleep, which in turn is correlated with the pharmacological activity of opium and morphine, which are substances extracted from this plant species.
Some taxonomists were inspired by this traditional knowledge to name scientific species. A concrete example is the species whose specific epithet is “officinalis, -e,” since this Latin term is translated as an “official product, which comes from the pharmacy,” referring to medicines sold in pharmacies in the past. Therefore, Salvia officinalis L., Melissa officinalis L., and Calendula officinalis L., among many others, are European medicinal species and have been known as such since the 18th century since they were described by Linneaus, who lived in Europe in that century. Another example from Brazil is the Pantanal Matogrossense plant Heteropterys aphrodisiaca O. Mach. (popularly known as dog knot), indicated as an aphrodisiac by African descendants [7]. Both the scientific and the vernacular names of this plant refer to this biological activity. Thus, the specific epithet “aphrodisiaca” is translated as “aphrodisiac,” yet the vernacular name of the species “dog knot” alludes to the canine penis after intercourse since the roots of this plant resemble the shape of a penis under such condition.
Despite this standardization of academic science, human populations tend to classify the world according to their own languages and cultures [8]. According to Rodrigues and Barnes [9, 10], among the Krahô people, there are plants called caprãnkohiréhô; caprãn means “turtle,” kohiré “vertebra,” and hô “leaf/plant.” The pharmacological effect of these plants refers to the “slowness of a turtle.” In fact, these plants are used in the form of cigarettes by these indigenous people in search of anxiolytic effects. The most interesting thing about these plants is the way indigenous people acquire knowledge of their effects. They observed that deer, one of the fastest animals in the Cerrado biome, after consuming this plant exhibits altered behaviour, becoming “slower” than usual. In this sense and because they made this observation, they began to apply this plant in different ways until they reached the cigarette, which has a relaxing and anxiolytic effect.
Furthermore, the plant Dysphania ambrosioides (L.) Mosyakin & Clemants (Amaranthaceae) is an example of how the colonization process changed vernacular plant names in Brazil. In Ilhabela, a city on the coast of the state of São Paulo, this plant is known as caanema by fishermen communities, which in the Tupi language, “caa” means leaves and “nema” fetid. This name is an inheritance of the Tupinambá population, which occupied the Brazilian coast in the past. Today, this plant species has other names throughout Brazilian territory; erva-de-Santa-Maria (southeast of the country), mastruz (north), and mastruço (several locations). From this example, it is possible to notice that several plants named in native languages changed with the arrival of Europeans, and many of the names paid homage to saints such as Santa Maria.
New bioactive compounds were searched using approaches such as (i) random collections; (ii) chemotaxonomy; (iii) chemical ecology; (iv) zoopharmacognosy, and last, (v) ethnopharmacology/ethnobotany [11–13]. In addition to these methodologies, we suggest a new approach based on the search for clues and indications about plant uses and properties in vernacular and scientific names. This approach alone and/or combined with the others mentioned above could increase our chances of achieving success in the search for new bioactive molecules. Would this not be a universe of possibilities little explored in addressing traditional and vernacular knowledge? It is important to recall that this knowledge was used to “baptize” many genera and epithets, which, in fact, can give us important pharmacological clues of a given specimen, which up until now may have been poorly explored. In addition, although they are often included in the composition of scientific names, are lexicons not overlooked, and thus poorly understood?
In this way, both the scientific (genus name and the specific adjective/epiphyte) and vernacular names of species can be rich sources of data on their possible biological properties/toxicity, guiding chemical and pharmacological research aimed at the development of new drugs. Based on the reading of the two classical and reference works on Brazilian medicinal plants, this study sought to list the scientific and vernacular names of plants whose lexicons are related to the possible medicinal and/or toxic properties of plants and to compare them with the “ethno” (ethnobotanical and ethnopharmacological) and pharmacological data available in the scientific literature.
2. Materials and Methods
2.1. Books Consulted and Selection of Species
To carry out this study, two classic and reference works on Brazilian medicinal plants were selected, namely, “Dicionário das plantas úteis do Brasil e das exóticas cultivadas” (Dictionary of Useful Native Plants and Cultivated Exotic Plants in Brazil) by Pio Correa [14] and “Plantas medicinais no Brasil. Nativas e exóticas” (Medicinal Plants in Brazil. Native and Exotic) by Lorenzi and Matos [15] (Figure 1). The former consists of six volumes, describes approximately 10,000 plant species, and is considered one of the most important and comprehensive publications on the subject in Brazil; the latter, although more modest in relation to the number of species, identifying approximately 2,800 vernacular names, was included in this study due to its recognized importance [16].
Figure 1.
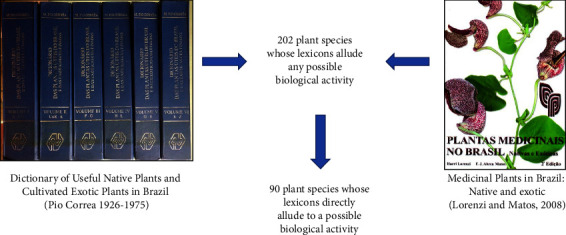
The two literary works from which the 202 plant species were extracted. The 90 plant species whose lexicons directly allude to a possible biological activity are analyzed in the present study.
When consulting these books, based on fluctuating reading, that is, based on generic capture of information [17], we searched for native and exotic plants whose scientific and/or vernacular names refer to any biological activity (medicinal and/or toxic). After selecting plant species, new bibliographic surveys were conducted on a scientific basis, and the following data are organized in Table 1: taxonomic family; currently accepted scientific name; scientific name as found in the literature; vernacular name if found (original in Portuguese and translated into English); possible biological properties according to the meaning of the epithets and/or vernacular names of the plant; literature related to ethnobotany/ethnopharmacology (here called “ethno”); and pharmacology. Table 1 presents the data for each plant species that refers to the following three dimensions: possible medicinal and/or toxic properties according to their lexicons, “ethno,” and pharmacological data from the scientific literature.
Table 1.
Ninety species grouped by family, currently accepted name, name found in the literature, vernacular name, possible medicinal and/or toxic properties, ethnobotanical/ethnopharmacological data (“ethno”), and pharmacological data (both obtained from the scientific literature).
| Family | Currently accepted name | Species found in the literature | Vernacular name | Possible medicinal and/or toxic properties | “ETHNO” data (ethnobotany/ethnopharmacology) | Pharmacological data |
|---|---|---|---|---|---|---|
| Achariaceae (2 species) | Asclepias campestris Vell. | Asclepias curassavica L. | Cega-olhos | POI (cega-olhos = blind eyes)∗ | May cause corneal edema∗, used for fever, bleeding control, and as a purgative [18–23] | Anti-inflammatory, analgesic, antipyretic, antimicrobial, cytotoxic, and cardiovascular properties [24] |
| Carpotroche brasiliensis (Raddi) A Gray♦ | Carpotroche brasiliensis (Raddi) A. Gray | Fructa-de-arara-de-lepra | INF (lepra = Hansen's disease)∗ | Antileprosy∗ [25] | Anti-inflammatory and antinociceptive properties [26] | |
| Herva-de-piolho | DER (herva-de-piolho = herb of lice)∗ | Treatment of skin conditions∗ [27] | ||||
|
| ||||||
| Amaranthaceae (3 species) | Blutaparon vermiculare (L.) Mears♦ | Gomphrena vermicularis L. | PAR (vermicularis = worm-like)∗ | Dysentery∗, diarrhoea∗, stomach and kidney problems [28] | ND | |
| Dysphania ambrosioides (L.) Mosyakin & Clemants | Chenopodium anthelminticum L. | PAR (anthelminticum = vermifuge, worm expelling)∗ | Antiparasitic ∗, analgesic, antiasthmatic, digestive, and antihemorrhoidal activities [29–32] | Antiparasitic, trypanocidal, and antileishmanial activities∗ [33] | ||
| Gomphrena antilethargica Silveira | Gomphrena antilethargica Silveira | NER (anti-lethargica = antilethargic) | ND | ND | ||
|
| ||||||
| Amaryllidaceae (3 species) | Boophone disticha (L.f.) Herb. | Brunsvigia toxicaria (L.f. ex Aiton) Ker Gawl. | POI (toxicaria = toxic, containing a poisonous substance)∗ | hallucinations∗, stupor and coma∗, hysteria, headaches, used for boils, burns and abdominal pain [34–37] | Depressive effects on the central nervous system∗, can cause seizures and difficulty breathing∗ [38] | |
| Crinum asiaticum L. | Crinum toxicarium Roxb. | POI (toxicarium = toxic, containing a poisonous molecule) | Edema, fever, bruises, fractures, rheumatism, earache, mumps, tonsillitis, gastrointestinal complaints, hernia, to treat vomiting and urinary difficulties [39–41] | Antioxidant, anti-inflammatory, analgesic, cytotoxic, and antimicrobial activities in wound healing [42] | ||
| Haemanthus toxicarius L.f. ex Aiton | Haemanthus toxicarius L.f. ex Aiton | POI (toxicarius = toxic, containing a poisonous molecule)∗ | Urinary diseases, skin diseases, swelling, hematoma, respiratory problems, gastrointestinal problems, used as a dart poison∗ [43, 44] | Antimicrobial, anti-inflammatory, causes hallucinations∗, treatment for anxiety, stress, and Alzheimer's disease [45] | ||
|
| ||||||
| Anacardiaceae (2 species) | Persea caustica Spreng. | Persia caustica = Persea caustica Spreng. | POI (caustica = with caustic taste, mouthburn) | ND | ND | |
| Toxicodendron pubescens Mill. | Rhus toxicarium Salisb. | POI (toxicarium = toxic, containing a poisonous molecule)∗ | Causes skin irritation∗, used for swelling, antiseptic activity, used as poison∗ [46] | Protection against inflammatory lesions, hematologic alterations, and arthritis pain [47] | ||
| Rhus toxicodendron L. | POI (toxicodendron = poison tree)∗ | |||||
|
| ||||||
| Annonaceae (1 species) | Xylopia aromatica (Lam.) Mart. ♦ | Uvaria febrifuga Humb. & Bonpl. ex DC. | MET (febrifuga = fever-dispelling)∗ | malaria∗ and fever∗ [48]. | in vitro activity against Plasmodium falciparum∗ [49] | |
|
| ||||||
| Apocynaceae (3 species) | Allamanda schottii Pohl ♦ | Allamanda cathartica Schrad. | GAS (cathartica = purgative, purging, cathartic)∗ | Cathartic∗, emetic, colic ∗, antifungal and antiviral activities, used to treat fever, diabetes, reduces inflammation, diuretic, and increases blood flow [50–55] | Compounds with analgesic, anti-inflammatory, and antidiabetic activities, cause infertility, purgative∗ and wound healing [56] | |
| Aspidosperma illustre (Vell.) Kuhlm. & Pirajá♦ | Aspidosperma illustre (Vell.) Kuhlm. & Pirajá | Erva-venenosa | POI (erva-venenosa = poison weed) | ND | ND | |
| Schubertia multiflora Mart. | Schubertia multiflora Mart. | Maria-da-costa- peidorreira | GAS (peidorreira = farting) | Abortive and emmenagogue [57] | ND | |
|
| ||||||
| Aquifoliaceae (1 species) | Ilex diuretica Mart. ex Reissek♦ | Ilex diuretica Mart. ex Reissek | URO (diuretica = diuretic)∗ | diuretic∗ and used for urinary infections, used for high blood pressure and wound healing [58] | ND | |
|
| ||||||
| Araceae (1 species) | Anthurium parasiticum (Vell.) Stellfeld ♦ | Pothos parasiticus Vell. | PAR (parasiticus = living at the expense of another, parasitic) | ND | ND | |
|
| ||||||
| Aristolochiaceae (2 species) | Aristolochia theriaca Mart. ex Duch. ♦ | Aristolochia theriaca Mart. ex Duch. | GYN (Aristolochia = best-childbirth, abortifacient property)/ANT (theriaca = antidote, theriacs are antidotes to poisons and bites of wild beasts)∗ | Antiophidic action∗ [59] | ND | |
| Aristolochia triangularis Cham. ♦ | Aristolochia antihysterica Mart. ex Duch. | GYN (Aristolochia = abortive)/NER (antihysterica = antihysteria)∗ | Hysteria attacks∗, soothing nerves ∗, antiseptic use, infections, skin diseases, ulcers, diuretic, edema, malaria, parasites, hypertension, dysentery, diarrhoea, abortive∗ and antirheumatic [27, 60, 61] | Anti-inflammatory activity [61] | ||
|
| ||||||
| Bignoniaceae (4 species) | Cybistax antisyphilitica (Mart.) Mart. ♦ | Bignonia antisyphilitica Mart. | INF (syphilitica = to treat syphilis)∗ | Antisyphilitic activity, lotions against syphilitic ulcers∗, decoction and infusion to treat dysuria, swelling, and water retention [62] | Larvicidal activity against Aedes aegypti [63] | |
| Cybistax antisyphilitica (Mart.) Mart. | ||||||
| Phryganocydia antisyphilitica Mart. ex DC. | ||||||
| Handroanthus barbatus (E.Mey.) Mattos ♦ | Couralia toxophora (Mart.) Benth. & Hook.f. ex K.Schum. | POI (toxophora = toxic, containing a poisonous substance) | Antimalarial activity [64] | ND | ||
| Handroanthus impetiginosus (Mart. ex DC.) Mattos ♦ | Tecoma impetiginosa Mart. | ipê-contra-sarna | DER (sarna = scabies)∗ | Fever reducer, venereal and rheumatic disorders, for skin disorders (eczema, herpes, and mange) and ulcers∗ [64] | Anti-inflammatory, antiautoimmune activities ∗, and anticancer [60, 65, 66] | |
| Kordelestris syphilitica Arruda | Kordelestris syphilitica Arruda | INF (antisyphilitica = anti- syphilis) | Treatment of skin diseases (scarring) ∗, respiratory and digestive disorders [67] | ND | ||
|
| ||||||
| Cactaceae (2 species) | Rhipsalis baccifera (J.S.Muell.) Stearn ♦ | Rhipsalis parasitica (Lam.) Haw. | PAR (parasitica = living at the expense of another, parasitic) | ND | ND | |
| Rhipsalis undulata Pfeiff. | Cactus parasiticus L. | PAR (parasiticus = living at the expense of another, parasitic) | ND | ND | ||
|
| ||||||
| Caryocaraceae (1 species) | Caryocar glabrum (Aubl.) Pers. | Caryocar toxiferum Barb.Rodr. | POI (toxiferum = toxic, containing a poisonous substance) | ND | ND | |
|
| ||||||
| Celastraceae (1 species) | Monteverdia truncata (Nees) Biral | Monteverdia truncata (Nees) Biral | Erva-botão-cancerosa/erva-botão-cancrosa | CAN (cancerosa/cancrosa = cancerous) | Stomach problems [68] | ND |
|
| ||||||
| Commelinaceae (1 species) | Tripogandra diuretica (Mart.) Handlos ♦ | Tradescantia diuretica Mart. | URO (diuretica = diuretic)∗ | Diuretic, urinary∗, liver, disorders [69]. | ND | |
|
| ||||||
| Compositae (5 species) | Achillea ptarmica L. | Achillea ptarmica L. | DER (Achillea = used by Achilles to staunch wounds)/RES (ptarmica = causing sneezes) | ND | ND | |
| Mikania cynanchifolia Hook. & Arn. ex B.L.Rob. ♦ | Mikania cynanchifolia Hook. & Arn. ex Baker | POI (cynanchifolia- cynanchicus = of quinsy, literally dog throttling, from its former medicinal use) | ND | ND | ||
| Solidago chilensis Meyen♦ | Solidago vulneraria Mart. ex Baker | DER (vulneraria = wounds, healing wounds)∗ | Anti-inflammatory∗, diuretic, and gastrointestinal disorders [70] | Decreased gastric lesions∗ [71] | ||
| Tanacetum parthenium (L.) Sch.Bip. | Parthenium matricaria Gueldenst. | GYN (matricaria = maternal care, former medicinal use in treatment of uterine infections; parthenium = for labor)∗ | Fevers, rheumatoid arthritis, migraines, toothache, stomach pain, insect bites, infertility, and problems with menstruation or during childbirth∗ [72–77] | Treatment for smooth muscle spasms, prophylactic treatment for migraine, inhibition of histamine release (inflammatory processes)∗, uterine-stimulant activities∗ [78, 79] | ||
| Xanthium catharticum Kunth | Xanthium catharticum Kunth | GAS (catharticum = purgative, purging, cathartic) | ND | ND | ||
|
| ||||||
| Convolvulaceae (2 species) | Ipomoea dumosa (Benth.) L.O. Williams ♦ | Exogonium purga (Wender.) Benth. | GAS (purga = purgative)∗ | purgative∗ [80] | ND | |
| Operculina macrocarpa (L.) Urb.♦ | Ipomoea operculata Mart. & Spix | Batata-aipo-de-purga | GAS (purga = purgative)∗ | Purgative∗, anthelmintic, blood purifier and treatment for uterine infection [81] | It has resin glycosides known as purgative ingredients∗ [82]. | |
|
| ||||||
| Cucurbitaceae (3 species) | Ecballium elaterium (L.) A.Rich. | Ecballium purgans Schrad. | GAS (purga = purgative) | ND | ND | |
| Luffa sepium (G.Mey.) C.Jeffrey | Luffa purgans (Mart.) Mart. | GAS (purga = purgative)∗ | Swelling, chronic ophthalmia (eye diseases), and emetic properties [62] | ND | ||
| Momordica anthelmintica Schumach. & Thonn. | Momordica anthelmintica Schumach. & Thonn. | PAR (anthelmintica = vermifuge, worm expelling) | ND | ND | ||
|
| ||||||
| Erythroxylaceae (1 species) | Erythroxylum cataractarum Spruce ex Peyr.♦ | Erythroxylum cataractarum Spruce ex Peyr. | EYE (cataractarum = cataract) | The snuff protects people from bad weather, such as cold and rain, and from long, sleep-disturbing activities [83–85] | ND | |
|
| ||||||
| Euphorbiaceae (4 species) | Cnidoscolus urens (L.) Arthur♦ | Cnidoscolus urens (L.) Arthur | Queimadeira | POI (urens = queimadeira = acrid, stinging, burning, to burn)∗ | Antiparasitic, to treat boils and “ringworm” (superficial skin mycoses), itching, injuries, skin infections, skin wounds, stomach pain, uterine infections, and blood purification [86] | Contains several toxins, such as curcin (toxalbumin phytotoxin), hydrocyanic acid, atropine, tetramethylpyrazine, glycoside, and curcanoleic acid∗ [87, 88] |
| Jatropha urens L. | ||||||
| Croton antisyphiliticus Mart. ♦ | Croton antysiphiliticus Mart. | INF (antisyphilitica = anti-syphilis)∗ | Syphilis∗, rheumatisms, ulcerative lesions, inflammatory diseases, genital infections, and venereal cancers∗ and to treat infections of the urogenital tract [89–91] | Nematocidal activity in vitro∗ [92] | ||
| Euphorbia ophthalmica Pers. ♦ | Euphorbia ophthalmica Pers. | EYE (ophthalmica = ophtalmic) | ND | ND | ||
| Jatropha podagrica Hook. | Jatropha podagrica Hook. | MET (podagrica = snare, of gout, used to treat gout)∗ | Antipyretic, diuretic, choleretic and purgative, to cure oral candidiasis in infants, to treat worms, skin diseases, and as a wound dressing [93, 94] | Antitumor, antimicrobial, molluscicidal, and insecticidal activities [95] | ||
|
| ||||||
| Fabaceae (5 species) | Andira fraxinifolia Benth. ♦ | Andira fraxinifolia Benth. | Mata-baratas | POI (mata-baratas = insecticide)∗ | Antihelminthic activity ∗ (the genus Andira is still used despite its toxic effects)∗ [96] | ND |
| Andira anthelmintica Benth. | PAR (anthelmintica = vermifuge, worm expelling)∗ | |||||
| Andira vermifuga Benth. ♦ | Geoffroea vermifuga Mart. | PAR (vermifuga = vermifuge, worm expelling)∗ | Andira species are commonly used for their antihelminthic properties∗ [97] | ND | ||
| Andira vermifuga Benth. | ||||||
| Chamaecrista cathartica (Mart.) H.S.Irwin & Barneby ♦ | Cassia cathartica Mart. | GAS (cathartica = purgative, purging, cathartic)∗ | ND | Purgative properties∗ [98] | ||
| Chamaecrista nictitans var. jaliscensis (Greenm.) H.S. Irwin & Barneby ♦ | Cassia hypnotica Vell. | NER (hypnotica = hypnotic) | ND | ND | ||
| Vouacapoua vermifuga (Mart. ex Benth.) Kuntze | Vouacapoua vermifuga (Mart. ex Benth.) Kuntze | PAR (vermifuga = vermifuge, worm expelling) | ND | ND | ||
|
| ||||||
| Hypericaceae (1 species) | Vismia latifolia (Aubl.) Choisy ♦ | Vismia latifolia (Aubl.) Choisy | Pau-alazão-de-febre | MET (febre = antipyretic)∗ | Tonic and febrifugal agent∗ [99] | Vasodilator effect [100] |
|
| ||||||
| Iridaceae (2 species) | Trimezia cathartica (Klatt) Niederl. | Cypella cathartica (Klatt) Mart. ex Klatt | GAS (cathartica = purgative, purging, cathartic) | ND | ND | |
| Lansbergia catartica Klatt | ||||||
| Trimezia juncifolia (Klatt) Benth. & Hook.f. ♦ | Cypella purgans Mart. ex Klatt | GAS (purga = purgative) | For blood clearance, for intermittent wounds and as an anti-inflammatory [101] | ND | ||
| Ferraria purgans Mart. | ||||||
| Lansbergia purgans Klatt | ||||||
|
| ||||||
| Lamiaceae (1 species) | Leonurus cardiaca L. | Leonorus cardiaca L. | CAR (cardiaca = heart conditions)∗ | Cardiac∗, nervous system problems, digestive disorders, bronchial asthma, climacteric symptoms, amenorrhoea, skin wounds, and inflammation [102] | Antibacterial, antioxidant, anti-inflammatory, as well as effects on the heart and circulatory system∗, hypotensive effect∗, sedative and analgesic activities [103] | |
|
| ||||||
| Lobariaceae (1 species) | Lobaria pulmonaria (L.) Hoffm. | Sticta pulmonaria (L.) Biroli | RES (pulmonaria = lungwort, the signature of the spotted leaves as indicative of efficacy in the treatment of respiratory disorders)∗ | Used in pulmonary disorders∗ [104] | ND | |
|
| ||||||
| Loganiaceae (3 species) | Spigelia anthelmia L. ♦ | Spigelia anthelmia L. | Lombrigueira/erva-das-lombrigas | PAR (lombrigueira; erva- das-lombrigas = roundword weed)∗ | Anthelmintic∗ and fish poison [105, 106] | Neuralgic and heart diseases [107] |
| Strychnos nux-vomica L. | Strychnos nux-vomica L. | POI (Strychnos = poisonous, solanaceous plants)∗/GAS (nux-vomica = emetic nut) | Eye infection, emetic∗ and snake bites [108] | Nervous system stimulant, analgesic action, aid in alcohol dependence, anti-inflammatory action, affects the immune system, antitumor activity, snake antivenom, effects on pathogenic microorganisms, toxic∗ [47, 131] | ||
| Strychnos pseudoquina A. St.-Hil. ♦ | Geniostoma febrifugum Spreng. | MET (febrifugum = antipyretic)∗ | Abortive [9] | Mutagenic activity (leaves), antimalarial∗ [9, 111] | ||
|
| ||||||
| Lythraceae (2 species) | Heimia salicifolia (Kunth) Link ♦ | Ginoria syphilitica Moc. & Sessé ex DC. | INF (syphilitica = to treat syphilis)∗ | Antimicrobial activity [112] | Antihypertensive, vasorelaxant effect [113] | |
| Nesaea syphilitica (DC.) Steu | Heimia syphilitica DC. | INF (syphilitica = to treat syphilis) | ND | ND | ||
| Nesaea syphilitica (DC.) Steud. | ||||||
|
| ||||||
| Malvaceae (1 species) | Pavonia sidifolia Kunth ♦ | Pavonia diuretica A.St.-Hil. | URO (diuretica = diuretic)∗ | Emollient, diuretic, and dysuria∗ [114] | ND | |
|
| ||||||
| Melastomataceae (1 species) | Miconia tomentosa (Rich.) D. Don ex DC. ♦ | Micania tomentosa (Benth.) Fritsch | Oiti-cagão | GAS (cagão = laxative) | Genital steam baths [115] | ND |
|
| ||||||
| Meliaceae (1 species) | Guarea guidonia (L.) Sleumer ♦ | Guarea purgans A.Juss. | GAS (purga = purgative) | Malaria, flu and fever [116] | Wound-healing properties [117] | |
|
| ||||||
| Moraceae (3 species) | Antiaris toxicaria Lesch. | Antiaris toxicaria Lesch. | POI (Antiaris = against association). The Javan upas tree, Antiaris toxicaria, reputedly causes the death of anyone who sleeps under it∗ | Antioxidant, anti-inflammatory, febrifuge, antifungal, antibacterial, and for the treatment of dysentery [118] | Anticonvulsant activity, toxic∗ [119] | |
| Ficus adhatodifolia Schott ♦ | Ficus anthelminthica Mart. | PAR (anthelmintica = vermifuge, worm expelling)∗ | Vermifuge∗ [120, 121] | Antioxidant and mutagenic activity [122] | ||
| Ficus vermifuga (Miq.) Miq. | ||||||
| Pharmacosycea anthelmintica (rich. ex DC.) Miq. | ||||||
| Pharmacosycea vermifuga Miq. | ||||||
| Ficus gomelleira Kunth & C.D. Bouché ♦ | Ficus gomelleira Kunth & C.D. Bouché | Gameleira-de-purga | GAS (purga = purgative)∗ | vermifuge and purgative∗ [114] | Modulator of bacterial activity [123] | |
|
| ||||||
| Myrtaceae (3 species) | Eugenia dysenterica DC. ♦ | Eugenia dysenterica DC. | GAS (dysenterica = disinteric)∗ | Hookworm (anemia), high blood pressure, inflammation, vaginal discharge, diarrhoea∗, depurative, diabetes, malaria, and hepatic disease [86] | Antifungal activity, molluscicidal activity, therapeutic benefits in recovery from chronic constipation and irritable bowel syndrome ∗, anticancer effects; hepatoprotection; antidiabetes; antimicrobials; and cardioprotective [124, 125] | |
| Stenocalyx dysentericus (DC.) O.Berg | ||||||
| Eugenia myrcianthes Nied. ♦ | Campomanesia cagaiteira Kiaersk. | GAS (cagaiteira = cathartic) | ND | ND | ||
| Myrtus dysenterica Mart. ♦ | Myrtus dysenterica Mart. | GAS (dysenterica = disinteric)∗ | Diabetes, malaria, jaundice, and hepatic disease [124] | Anticancer effects, hepatoprotection, antidiabetes, antimicrobials, and cardioprotective [124] | ||
|
| ||||||
| Passifloraceae (2 species) | Passiflora coccinea Aubl. ♦ | Passiflora toxicaria Barb. Rodr. | POI (toxicaria = toxic, containing a poisonous substance) | Psychoactive, hallucinogenic, stimulating, anxiolytic, dysmenorrhea of the genitourinary system, kidney stones, kidney disorders, and fever [126] | ND | |
| Turnera diffusa Willd. ex Schult. ♦ | Turnera aphrodisiaca Ward | NER (afrodisíaca = aphrodisiac)∗ | Aphrodisiac, stimulant, nervous tonic∗, laxative, also acts in kidney, menstrual, and pregnancy disorders [127, 128] | Hypoglycemic activity, aphrodisiac activity∗ [129] | ||
|
| ||||||
| Phyllanthaceae (1 species) | Phyllanthus urinaria L. ♦ | Phyllanthus urinaria L. | URO (urinaria = diuretic)∗ | Diabetes∗, malaria, jaundice, and liver disease [130–132] | Anticancer, hepatoprotective, antidiabetic ∗, antimicrobial, and cardioprotective effects [133] | |
|
| ||||||
| Phytolaccaceae (1 species) | Microtea debilis Sw. ♦ | Microtea debilis Swartz | Herva-mijona | URO (mijona = diuretic)∗ | proteinuria∗ [134] | proteinuria∗ [135] |
|
| ||||||
| Poaceae (1 species) | Digitaria setigera Roth | Panicum pruriens Trin. | POI (pruriens = irritant, stinging, itch-causing) | ND | ND | |
|
| ||||||
| Polygonaceae (1 species) | Polygonum antihaemorrhoidale Mart. | Polygonum antihaemorrhoidale Mart. | GAS (antihemorrhoidale = antihemorrhoidal)∗ | Depurative, hemorrhoids, and diarrhoea∗ [86] | Hemorrhoids∗ and vermicide [136] | |
|
| ||||||
| Ranunculaceae (2 species) | Handroanthus barbatus (E.Mey.) Mattos | Tecoma toxophora Mart. | POI (toxophora = toxic, containing a poisonous substance). | Antimalarial [137] | Cytotoxic activity [138] | |
| Helleborus foetidus L. | Helleborus foetidus L. | POI (Helleborus = poison-food) | ND | ND | ||
|
| ||||||
| Resedaceae (1 species) | Reseda odorata L. | Reseda odorata L. | DER (Reseda = the name, resedo, in Pliny refers to its use in treating bruises)∗ | Stomach cramps [139] | anti-inflammatory∗ and diuretic activities [140, 141] | |
|
| ||||||
| Rhamnaceae (1 species) | Discaria americana Gillies & Hook. ♦ | Discaria febrifuga Mart. | MET (febrifuga = antipyretic)∗ | Tonic and febrifuge∗ [142] | Antimicrobial activity [143] | |
|
| ||||||
| Rubiaceae (3 species) | Palicourea rigida Kunth ♦ | Palicourea diuretica Mart. | URO (diuretica = diuretic)∗ | Kidney disease, inflammation, and urinary tract infections ∗ and female genital tract, hepatitis, and malaria [144–146] | Anti-inflammatory, antioxidant, antibacterial, and antifungal activities∗ [147] | |
| Richardia brasiliensis Gomes ♦ | Richardsonia emetica Mart. | GAS (emetica = emetic)∗ | Expectorant, diaphoretic, vermifuge, emetic∗, and to treat hemorrhoids [148]. | Emetic∗, treat hemorrhoids, antidiabetic, vermifuge, eczema treatment, burns, bronchitis, flu, and avian malaria [149, 150]. | ||
| Ronabea emetica (L.f.) A.Rich. ♦ | Cephaelis emetica (L.f.) Pers. | GAS (emetica = emetic)∗ | emetic∗, anti-inflammatory, antineoplastic ∗, expectorant, to treat hemorrhoids ∗, diaphoretic, and vermifuge [151, 152] | Antimicrobial, antitumor, and antiproliferative activities [153] | ||
| Psychotria emetica L.f. | ||||||
|
| ||||||
| Rutaceae (4 species) | Angostura trifoliata (Willd.) T.S.Elias | Cusparia febrifuga Humb. ex DC. | MET (febrifuga = antipyretic)∗ | Tonic, antidiarrhoeal, diaphoretic, sweating∗, and bronchitis [154] | ND | |
| Conchocarpus toxicarius (Spruce ex Engl.) Kallunki & Pirani ♦ | Cusparia toxicaria Engl. | POI (toxicaria = toxic, containing a poisonous substance) | ND | ND | ||
| Galipea toxicaria Spruce ex Engl. | ||||||
| Esenbeckia febrifuga (A.St.-Hil.) A.Juss. ex Mart. ♦ | Evodia febrifuga A.St.-Hil. | MET (febrifuga = antipyretic)∗ | Fevers∗, adenitis, dyspepsia, malaria∗, and constipation [155] | Antimalarial ∗ [156, 157] | ||
| Esenbeckia febrifuga (A.St.-Hil.) A.Juss. ex Mart. | ||||||
| Galipea jasminiflora (A.St.-Hil.) Engl.♦ | Galipea febrifuga (A.St.-Hil.) Baill. | MET (febrifuga = antipyretic)∗ | Against venereal warts, astringent, intermittent fevers∗, dyspepsia, antidiarrhoeal, infections, malaria, and venereal warts [158, 159] | Treatment for intermittent fever∗ [86] | ||
| Ticorea febrifuga A.St.-Hil. | ||||||
|
| ||||||
| Salicaceae (1 species) | Xylosma salzmannii (Clos) Eichler ♦ | Xylosma salzmanni Eichl. | Quarenta- feridass/sessenta- feridas | INF (feridas = wounds)∗ | Astringent and dye [160] | ND |
|
| ||||||
| Sapindaceae (1 species) | Matayba purgans (Poepp.) Radlk. ♦ | Matayba purgans (Poepp.) Radlk. | GAS (purga = purgative) | ND | ND | |
|
| ||||||
| Scrophulariaceae (1 species) | Capraria biflora L.♦ | Capraria biflora L. | chá-bravo | POI (chá-bravo = wild tea) | For kidneys, stomach pains, ulcers, hemorrhoids, diarrhoea, vomiting, pain, flu, fever, rheumatism [161, 162] | Antibacterial, antitumor, analgesic, and anti-inflammatory activity [163] |
|
| ||||||
| Solanaceae (1 species) | Solanum stagnale Moric. ♦ | Solanum stagnale Moric. | não-me-toque | POI (não-me-toque = do not touch me) | ND | ND |
|
| ||||||
| Tropaeolaceae (1 species) | Tropaeolum pentaphyllum Lam. ♦ | Tropaeolum pentaphyllum Lam. | Chagas/chagueira | INF (chagas/chagueira = Chagas disease) | Cold and diabetes [164] | Anticoagulant [165] |
|
| ||||||
| Urticaceae (2 species) | Urera caracasana (Jacq.) Gaudich. ex Griseb. ♦ | Urera caracasana (Jacq.) Griseb. | Urtiga-brava-de-fogo | POI (urtiga = Nettle) | Relief from inflammation, diabetes, blood purification [166–168] | ND |
| Urtica urens L. | Urtica urens L. | POI (Urtica = sting; urens = acrid, stinging, burning, to burn)∗ | Allergy and atopic dermatitis∗ antidiabetic, diuretic, depurative, and antirheumatic [169] | Tonic, sedative, analgesic, chemoprotective and anti-inflammatory activity, phytodermatoses∗ [169, 170] | ||
∗ The 22 species whose “ethno” and pharmacological data are equivalent to plant lexicons. ♦ The 56 species native to Brazil. Bioprospecting categories: antidote (ANT), cancer (CAN), cardiovascular diseases (CAR), dermatologic disorders (DER), ophthalmic problems (EYE), gastrointestinal problems (GAS), gynecology (GYN), infections (INF), metabolic syndromes (MET), nervous system (NER), parasites (PAR), poisons (POI), respiratory complaints (RES), and urology (URO). ND: no data found. The possible medicinal and/or toxic property column follows the bioprospecting classification.
The scientific names of the species and their families were confirmed using the World Flora Online database (https://www.worldfloraonline.org/). Both the scientific name found in the literature and the currently accepted scientific name according to this database were included. Subsequently, the geographical origin was verified through Flora do Brasil 2020 (https://floradobrasil.jbrj.gov.br/reflora/listaBrasil/PrincipalUC/PrincipalUC.do#CondicaoTaxonCP); native species are marked with the notation (♦) in Table 1.
2.2. Bibliographic Survey and Correlations
Correlations between the meanings of the species' epithets and their possible biological properties were made from their translation from Latin by consulting online Latin dictionaries (https://www.dicio.com.br/vermiculares/, https://www.infopedia.pt/dicionarios/termos-medicos/CASTRENS), Vocabulário Latim-Português-Lingua Latina [171], and other bibliographies such as Brown [172], Gledhill [6], and Stearn [173]. Therefore, for example, in the case of Allamanda cathartica L., the specific epithet cathartica was used as a reference for the correlation mentioned, as its Latin translation is “cathartic,” that is, laxative activity. The correlation of vernacular names with possible biological activities was determined by the actual meaning of the word in Portuguese. Therefore, for example, the poisonous herb plant already contains the term “poisonous.” In Table 1, the terms (specific epithet and vernacular name) that were used in this translation are presented in bold text to facilitate visualization.
To compare the aforementioned correlations with the “ethno” and pharmacological data present in the scientific literature, bibliographic surveys of various databases (Scopus, PubMed, Scielo, Google Scholar, Science Direct, and others) were conducted in December 2022. In the pharmacological survey, searches involving the scientific names of the plants and terms such as “medicinal,” “toxic,” “toxicity,” and “treatment” were used. The terms “ethnobotany,” “ethnopharmacology,” “traditional knowledge,” and “vernacular name” were used in the ethnobotanical/ethnopharmacological survey, and the search results were limited to English, Spanish, and Portuguese. The “ethno” and/or pharmacological data that coincide with the possible biological properties, lexicon of the plants, are highlighted with asterisks (∗) in Table 1. Figure 2 shows these data schematically.
Figure 2.

Number and percentage of species that had equivalence in the three dimensions analyzed (lexicon, “ethno,” and pharmacology).
2.3. Categorization and Comparison of the Data
The categorization of the data on the possible biological properties, according to the scientific/vernacular names of plants (lexicons), the “ethno” data, and the pharmacological data on large therapeutic groups in biomedicine was based on the categorization called bioprospection that was proposed by Staub et al. [174]. Accepted by the World Health Organization, this classification proposes 17 broad categories of appropriate use for the discovery of new drugs: antidote (ANT), andrology (AND), cancer (CAN), cardiovascular diseases (CAR), dermatologic disorders (DER), ophthalmic problems (EYE), food (FOO), gastrointestinal problems (GAS), gynecology (GYN), infections (INF), metabolic syndromes (MET), nervous system (NER), parasites (PAR), poisons (POI), respiratory complaints (RES), skeletomuscular system (SKE), and urology (URO). Finally, the categories identified for these three dimensions (lexicons, “ethno,” and pharmacological data) are compared in Figure 3.
Figure 3.

The 17 categories of bioprospecting classification∗ considering each species in their three dimensions: possible biological property (according to the lexicon of the plant), ethnobotanical/ethnopharmacological, and pharmacological data. ∗Bioprospecting classification: andrology (AND), antidote (ANT), cancer (CAN), cardiovascular diseases (CAR), dermatologic disorders (DER), ophthalmic problems (EYE), food (FOO), gastrointestinal problems (GAS), gynecology (GYN), infections (INF), metabolic syndromes (MET), nervous system (NER), parasites (PAR), poisons (POI), respiratory complaints (RES), skeletomuscular system (SKE), and urology (URO).
3. Results and Discussion
Based on the bibliographic survey conducted herein, 202 plant species were found to exhibit some pharmacological properties considering the inherent characteristics of their binomial identification (Figure 1). One hundred and twelve (112) of them, although denoted some medicinal use, was not explicit on which category of bioprospection they could be related. Therefore, for example, Melissa officinalis L., whose specific epithet “officinalis” means “medicinal,” could not be categorized in any of the bioprospection classifications. For this reason, these species are not presented in Table 1 but will be addressed later in this article.
On the other hand, the other 90 species had scientific/vernacular names (lexicons) highly related to direct biological or pharmacological activity. They are presented in Table 1 and belong to 47 families; Compositae and Fabaceae (5 species each) being the predominant families, followed by Bignoniaceae, Euphorbiaceae, and Rutaceae (4 species each).
Furthermore, it was observed that of 90 species, 56 (62.2%) are native to Brazilian territory and are identified by the sign “♦” in Table 1. Of the 90 species, 73 lexicons indicate some type of medicinal/toxic property according to their genus/epithet, while 19 lexicons make this allusion according to their vernacular names. These names are shown in bold in Table 1. The epithets vermicularis, anthelminticum, antilethargica, toxicaria, febrifuga, cathartica, diuretica, parasiticus, antihysterica, and antisyphilitica, among others were found in the current study (Table 1). In a study conducted by Hecklau et al. [5], the authors observed that most of the specific epithets used in the names of angiosperms in central French Guiana resemble some biological activity; they are officinalis, ophthalmia, pectoralis, and toxifera, among others.
Table 1 shows that 66 of the 90 species (73.3%) presented “ethno” data from the scientific literature, while 46 species, or 51.1%, presented pharmacological data. Of the 66 species with “ethno” data, 46 species (69.7%) showed equivalence with the possible medicinal and/or toxic properties of plants according to the plant lexicons (Figure 2), furthermore, of the 46 selected only 27 species (58.7%) exhibited the equivalence between pharmacological data with their lexicons. However, of the 90 species, only 45 had scientific studies in both the “ethno” and pharmacological dimensions, and 22 of them (48.9%), almost half, had equivalence in the three dimensions (lexicon, “ethno,” and pharmacology) (Figure 2). Species with such equivalences are highlighted with asterisks (∗) in Table 1. Thus, for example, Eugenia dysenterica DC. (Myrtaceae) was classified as having possible gastrointestinal biological properties. Data from the “ethno” literature indicate diarrhoea and for pharmacology, therapeutic benefits in recovery from chronic constipation, and irritable bowel syndrome [125, 175]; because all these sources refer to the category of gastrointestinal problems category (GAS) and/or have similarities in the symptoms and disease, these three dimensions are highlighted with asterisks in Table 1.
Table 1 shows and Figure 3 compares the distribution of the 17 categories, bioprospecting classification [174], considering each species in their three dimensions, i.e., lexicons, “ethno,” and pharmacological data; in some cases, the same species was classified in more than one category. For possible biological properties, according to the lexicons of plants, 11 categories were observed; the most frequent being poisonous (20 species), gastrointestinal problems (13), and nervous system (11). The “ethno” data were organized into 14 categories, the most prevalent being gastrointestinal problems (21), nervous system (17), metabolic syndromes (17), and dermatological problems (10). Similarly, pharmacological data were distributed into 15 categories: nervous system (17), gastrointestinal problems (17 species), and dermatologic and poisonous problems (9 species each).
By comparing the three dimensions of the data (Figure 3), the lexicon differs from the “ethno” and pharmacological data, while the last two show greater similarity considering the number of categories and species per category of bioprospecting. This may be related to the fact that many “ethno” and pharmacological studies have been conducted with these species, providing more scientific data compared to the lexicon, which generally has only one possible data. Furthermore, the gastrointestinal and nervous system categories are among the most recurrent in the 3 dimensions. The parasites category was consistent across the 3 dimensions. The category of poisons was the most frequent in the lexical dimension, but these species presented other data from “ethno” and pharmacology and, therefore, in these last two dimensions, this category was diluted among others.
The Compositae family includes plants of different sizes and cosmopolitan distribution and is also one of the largest families of angiosperms, with approximately 1600 genera [124]. Many species have been commercialized for medicinal, ornamental. and culinary purposes, in addition to species known to be invasive in our country [176]. In Table 1, although Achillea ptarmica L. has no “ethno” and/or pharmacological studies in the scientific literature, its genus Achillea refers to its use by Achilles “to staunch wounds,” and for this reason, it has been categorized as possibly having properties to treat dermatologic disorders (DER). Furthermore, its epithet ptarmica, which can be translated as “causing sneezes,” was classified as a plant with biological properties related to respiratory complaints. Other species belonging to the Achillea genus, but not surveyed in the present study, such as A. millefolium L., show agreement between the three dimensions analyzed here. Therefore, Achillea millefolium L., popularly known as atroveran and novalgine, has “ethno” records on its use in wounds, as an antipyretic and analgesic [177, 178], while its pharmacological activity includes anti-inflammatory, antipyretic, and analgesic effects [179]. In addition, these vernacular names are the same as two synthetic drugs, Novalgine® (antipyretic and analgesic) and Atroveran® (antispasmodic, used for cramps and pain during menstruation), since according to traditional knowledge, the effect of this species resembles them. As can be seen in Table 1, Tanacetum parthenium (L.) Sch. Bip. (Compositae), previously named Parthenium matricaria Gueldenst., was classified as gynecology (GYN) since its epithet matricaria means “Mothercare” (former medicinal use in the treatment of uterine infections) and parthenium mentions labor. According to Pareek et al. [180], it has been used by traditional communities in the treatment of infertility and problems with menstruation or during childbirth, while pharmacological investigations showed its effects in the treatment of smooth muscle spasms and as a uterine stimulant. Thus, this species shows an agreement between the three dimensions analyzed here. Solidago chilensis Meyen, previously named Solidago vulneraria Mart. ex Baker (Compositae), has the ephitet vulneraria meaning wound healing property. “Ethno” studies recorded its anti-inflammatory property [78], while pharmacological studies describe its use as an antiulcerogenic [70]. Finally, Table 1 shows that the species Xanthium catharticum Kunth (Compositae) alludes to cathartic activity; however, no studies were found in the “ethno” and pharmacological literature to investigate this possible use. However, the species Allamanda cathartica Schrad. (Apocynaceae), whose possible property is cathartic according to the lexicon, may be purgative, according to pharmacological studies [71], and has been recorded as a cathartic plant during an ethnobotanical survey [56].
As one of the largest families of angiosperms, Euphorbiaceae currently includes approximately 8,000 species distributed in 317 genera. Found all over the world, these species stand out economically in food and medicine, according to popular knowledge [50]. In Table 1 the species Cnidoscolus urens (L.) was categorized as poisons (POI) since both its epithet urens and its vernacular name queimadeira, resembles the effects “acrid, stinging, burning, to burn.” García et al. [181] confirmed the poisonous activity from a pharmacological study. Table 1 also shows species belonging to the genera Euphorbia and Jatropha, which have many other examples from the literature, such as Euphorbia tirucalli L., also known as Devil's Finger, which produces a toxic and caustic latex that can cause allergic reactions [87] and Jatropha curcas L. which has seeds rich in toxic oil [182]. Jatropha cathartica Terán & Berland. is another example; its seeds can also cause nausea, vomiting, diarrhoea, and suppression of intestinal functioning, and a single seed can cause severe poisoning [183]. In Table 1, the species Croton antisyphiliticus Mart. has been categorized as infections (INF) since its epithet resembles the antisyphilitic activity. In fact, ethnobotanical studies show similar data, such as syphilis, to treat genital infections and venereal cancers [89, 90, 184].
The species Leonurus cardiaca L. (Lamiaceae) shows the relationship between the three dimensions analyzed here. Its epithet cardiaca brings the idea of “heart conditions.” In fact, ethnobotanical and pharmacological studies showed symptoms and effects correlated with the heart [91, 103]; in this sense, the species has been categorized as cardiovascular diseases (CAR). The vernacular name batata-aipo-de-purga (Operculina macrocarpa (L.) Urb.-Convolvulaceae), where purga brings the idea of purgative, has been studied by ethnobotanical and pharmacological fields and both confirm its purgative activity [82, 102], and the species has been classified as for gastrointestinal problems (GAS). As can be seen in Table 1, the species Strychnos nux-vomica L. (Loganiaceae) has both medicinal and toxic possibilities since Strychnos means poisonous from solanaceous plants; while nux-vomica means an emetic nut. We know that the difference between medicine and poison is subtle and that many properties that are apparently harmful can be used therapeutically, as indicated, for example, by the epithets nux vomica, whose emetic property has been recorded in ethnobotanical studies [81], and the toxic property in pharmacological surveys [108]. In the literature, a clear example of this is Physostigma venenosum Balf., which, although it has the specific epithet venenosum, has already been used as a medicine (physostigmine) in the treatment of Alzheimer's disease [109].
In Table 1, we can observe other plants that have “ethno” studies equivalent to their lexicons and could be studied pharmacologically as follows: Uvaria febrifuga Humb. & Bonpl. ex DC. (Annonaceae) as febrifuge; Urtica urens L. (Urticaceae), which causes phytodermatoses; Richardsonia emetica Mart. (Rubiaceae) as emetic; Polygonum antihaemorrhoidale Mart. (Polygonaceae) as an antihemorrhoid; and Turnera aphrodisiaca Ward (Passifloraceae) as an aphrodisiac, among others. Other plants have “ethno” studies equivalent to their lexicons but do not have pharmacological data; Ilex diuretica Mart. ex Reissek (Aquifoliaceae) as a diuretic; Luffa purgans (Mart.) Mart. (Cucurbitaceae) as a purgative; Aristolochia theriaca Mart. ex Duch (Aristolochiaceae), with antiophidic action; Andira vermifuga Benth. (Fabaceae) as a vermifuge; and Lobaria pulmonaria (L.) Hoffm. (Lobariaceae) for pulmonary disorders, among others. In the same table, we observe some other species that have no studies in the scientific literature (“ethno”/pharmacology), only the lexical indication, and therefore, they and their respective potentialities should be the target of future studies as follows: Pothos parasiticus Vell. (Araceae), Rhipsalis parasitica (Lam.) Haw. (Cactaceae), Anthurium parasiticum (Vell.) Stellfeld (Araceae), Cactus parasiticus L. (Cactaceae), and Momordica anthelmintica Schumach. & Thonn. (Cucurbitaceae) as possible antiparasitics; Xanthium catharticum Kunth (Compositae) and Trimezia cathartica (Klatt) Niederl. (Iridaceae) as cathartics; Ecballium purgans Schrad. (Cucurbitaceae) as purgative; and Nesaea syphilitica (DC.) Steud (Lythraceae) as an anti-infectious agent, among others.
In addition to the 90 species listed in Table 1, another 112 were found in the works analyzed here. Although they do not show a direct correlation between their names (genus, epithet, and vernacular name) and a possible biological activity, they present exciting names from the medicinal and/or toxic point of view. In this sense, these 112 species will be presented and discussed in the following.
3.1. Correlation of Vernacular Names and Biological Properties
In the present work, nine vernacular names that indirectly refer to a possible biological activity were found in this search. Plants whose vernacular names in Portuguese include the word “diabo” (devil), such as jarro-do-diabo (devil's pitcher), whose scientific name is Aristolochia cymbifera Mart. & Zucc. (Aristolochiaceae), indicating a negative property. This vernacular name suggests “a pitcher belonging to the devil,” most likely due to its toxicity. This plant, in particular, is known for its carcinogenic and nephrotoxic properties as a member of the Aristolochiaceae family [185]. Other species in this category include herva-do-diabo (devil's herb), Elephantopus mollis Kunth. (Compositae), and café-do-diabo (devil's coffee), Casearia guianensis (Aubl.) Johnson (Salicaceae).
Other vernacular names stand out, such as sanguinaria (sanguinary), Persicaria acuminata (Kunth) M. Gómez (Polygonaceae), which may refer to an antihaemorrhagic or, conversely, haemorrhagic action. Finally, herva-almiscar-dos-feridos (musk herb of the wounded), Canna glauca L. (Cannaceae), refers to positive benefits for injured people, without further details.
All of the abovementioned names are vague, precluding a correlation between them and possible biological activity despite providing some type of information on medicinal properties and/or toxicity.
3.2. Correlation of Genera and Biological Properties
In this work, 51 species whose genera refer to medicinal uses and/or toxicity were recorded. Translations of these terms for possible medicinal and/or toxic potentials were based on readings of Latin dictionaries, as described in the Methods section. Many of them refer to historical facts in medicine, including the genus Herniaria of H. paico Molina (Amaranthaceae), which means “hernia rupture,” a term previously used in medicine, as well as Angelica archangelica L. (Apiaceae). In fact, a review shows us dozens of biological activities attributed to this plant from contemporary studies [186], whose genus means “healing power.” Consolida major Garsault (Boraginaceae) is an old Latin name used for “curative drugs.” Matricaria proealta (Matricaria praealta Poir.) (Compositae) refers to “maternal care” (previously used in medicine to treat uterine infections). Furthermore, various genera refer to toxic properties, such as Cerbera triphylla Rudge (Apocynaceae), a genus referring to the term Cerberus, which means poisonous, and Toxicodendron divaricatum Greene, where Toxicodendron means poisonous tree. The term Aethusa of the species A. cynapium L. means “burning, due to its pungency.”
3.3. Correlation of Epithets and Biological Properties
In total, 52 species were found in this search, with the following epithets: officinalis, officinale, officinarum, medica, medicinalis, salutaris, or ipecacuanha. All of these terms refer to some medicinal activity, albeit without a specific reference.
The terms officinale and officinarum can be translated as synonyms of officinalis and have the same meaning. Most, or more specifically, 90% of these 52 species have one of these three epithets. In fact, some of these species have already been widely studied and their medicinal activities have been established, for example, Melissa officinalis L., which reduces depression, anxiety, and stress and acts on sleep disorders [187]; Mikania officinalis Mart. as an anti-inflammatory, analgesic, and antibacterial [188]; and Calendula officinalis Hohen. as anti-inflammatory [189].
Three other species have the epithets medica or medicinalis, namely, Ilex medica Reissek (Aquifoliaceae), Psychotria medica Müll. Arg. (Rubiaceae), and Simarouba medicinalis Endl. (Simaroubaceae), which refers to medicinal use, although without specifying the possible effect. The epithet salutaris of the species Vitis salutaris (Kunth) Baker (Vitaceae) also refers to its beneficial use. Finally, the ipecacuanha epithet of the Evea ipecacuanha (Brot.) species W. Wight (Rubiaceae) means “drug producer” and may be related to some medicinal activity.
3.4. More than One Term Indicating Some Biological Activity
Some names are related to biological activity in more than one term (genus/epithet/vernacular name). Therefore, in the case of the species Avicennia officinalis L., both terms contain this information and Avicennia refers to Avicena (980–1037), an Arabic philosopher and physician, while its epithet officinalis has already been discussed in the previous section. Valeriana officinalis L., whose genus means “health (valere),” was named in medieval times for its medicinal use. Artemisia absinthium L., whose genus means “female pains,” refers to the Goddess Artemisia and its epithet absinthium is a Greek term that refers to the aromatic herb used in medicine. Althaea officinalis L., whose genus mentions “healer,” was named by Theophrastus.
3.5. Limitations of the Present Study
One of the limitations of the present study is the translation of the Latin term “gender” and/or “specific epithet” into a possible biological property. For example, the epithet lumbricoides may be associated with the worm format (roundworm) but also with some biological activity related to this worm, such as being worm-like. The same is true for Ilex fertilis Reissek and Avena sterilis L., epithets related to plant fertility and sterility, respectively. However, these characteristics could be as closely related to the characteristics of the plant as to its use. Thus, “ethno” and pharmacological studies can help clarify the possible properties of plant lexicons.
However, the intended analysis, comparing the possible biological property of the plant from its lexicon with ethno and pharmacological studies, was hampered since few “ethno” and pharmacological studies were located in the scientific literature, 66 and 46 in 90 plants, respectively. The pharmacological studies found in the scientific literature were not based on the possible biological activities investigated here, that is, the fact that the species Blutaparon vermiculare (L.) Mears has not been investigated for possible worming activity does not mean that it does not have this activity. Finally, most of the time, the lexicon refers only to a possible biological activity, while many uses can be attributed to the same species, both from an “ethno” and a pharmacological point of view. All these factors limited the analysis of this study, but despite them, a high percentage of coincidence was observed considering the three dimensions for 48.9% of the investigated plants.
3.6. Future Perspectives
The data collected in the present study favor new bioprospecting investigations that consider, in addition to the approaches already used (at random; collecting orientated by chemotaxonomy; biorational collecting, guided by chemical ecology; and collecting based on traditional knowledge, known as ethnopharmacology), another approach that basically considers plant lexicons. The sum of these approaches when choosing a future plant species to be tested by pharmacology and phytochemistry can and should increase the chances of achieving success in the search for new bioactive potentials.
4. Conclusions
In the present review, two classical Brazilian books on native and exotic plants were consulted and based on both, 10,394 plant species were collected and analyzed by fluctuating reading, allowing to associate scientific and vernacular names with biological activity. Furthermore, it was observed that according to the classic literature of medicinal plants, a high rate of concordance between scientific names and biological activity was observed, which was further validated by elegant ethnopharmacological and pharmacological studies. According to this study, 22 (48.9%) of the 45 plants surveyed showed equivalence in the three dimensions (lexicon, “ethno,” and pharmacology). We, therefore, conclude that plant lexicons may be closely linked to the possible medicinal and/or toxic properties of plants, and thus it is conceivable that plant lexicons may represent one additional approach for the characterization of new drugs. Therefore, in addition to data extracted from ethnopharmacology, random, or chemotaxonomy, lexicons may represent an interesting method to guide medicinal plant research. Therefore, based on a robust number of analyzed species, it was possible to conclude that plant lexicons were correlated with scientific names and, more importantly, with medicinal, pharmacological, or toxic properties. Finally, lexicons may represent an important approach for the search of new drugs, mainly directed to gastrointestinal, nervous, and parasites diseases.
Acknowledgments
The authors would like to thank the Federal University of São Paulo, FAPESP-BIOTA PROGRAM (process number 2019/19313-5), FAPESP (2018/24077-6), and CNPq (process number 400802/2016-3), which has supported several researchers at the Center for Ethnobotanical and Ethnopharmacological Studies. The authors also thank CNPq for the grant award to LFDP.
Contributor Information
Luiz Felipe Domingues Passero, Email: felipepassero@yahoo.com.br.
Eliana Rodrigues, Email: 68.eliana@gmail.com.
Data Availability
The data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Ullah F., Gao Y., Sari I., Jiao R.-F., Saqib S., Gao X.-F. Macro-morphological and ecological variation in Rosa sericea complex. Agronomy . 2022;12(5):p. 1078. doi: 10.3390/agronomy12051078. [DOI] [Google Scholar]
- 2.Usma A., Ahmad M., Zafar M., et al. Palynological study of weed flora from potohar plateau. Agronomy . 2022;12(10):p. 2500. doi: 10.3390/agronomy12102500. [DOI] [Google Scholar]
- 3.Francisco J. N. C., Sauthier L., Giaretta A., Della A. P. VIII Botânica No Inverno . Fortaleza: Federal University of Ceara; 2018. Fundamentos de Taxonomia vegetal; pp. 125–144. [Google Scholar]
- 4.Lírio E. J., Sarnaglia Júnior V. B. E se as plantas não tivessem nome? A importância do Código de Nomenclatura Botânica. Proceedings of the III Simpósio sobre a biodiversidade da Mata Atlântica; March 2014; Mata Atlântica. [Google Scholar]
- 5.Hecklau E. F., Mori S. A., Brown J. L. Specific epithets of the flowering plants of Central French Guiana. Brittonia . 2005;57(1):68–87. doi: 10.1663/0007-196x(2005)057[0068:seotfp]2.0.co;2. [DOI] [Google Scholar]
- 6.Gledhill D. The Names of Plants . New York, NY, USA: Cambridge University Press; 2008. [Google Scholar]
- 7.Rodrigues E., Carlini E. A. Plants used by a Quilombola group in Brazil with potential central nervous system effects. Phytotherapy Research . 2004;18(9):748–753. doi: 10.1002/ptr.1535. [DOI] [PubMed] [Google Scholar]
- 8.Zaman W., Ahmad M., Zafar M., et al. Diversity of medicinal plants used as male contraceptives: an initiative towards herbal contraceptives. Indian Journal of Traditional Knowledge . 2022;21(3):616–624. [Google Scholar]
- 9.Rodrigues E., Barnes J. Pharmacovigilance of herbal medicines: the potential contributions of ethnobotanical and ethnopharmacological studies. Drug Safety . 2013;36(1):1–12. doi: 10.1007/s40264-012-0005-7. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues E., Carlini E. A. Ritual use of plants with possible action on the central nervous system by the Krahô Indians, Brazil. Phytotherapy Research . 2005;19(2):129–135. doi: 10.1002/ptr.1636. [DOI] [PubMed] [Google Scholar]
- 11.Cox P. A., Balick M. J. The ethnobotanical approach to drug discovery. Scientific American . 1994;270(6):82–87. doi: 10.1038/scientificamerican0694-82. [DOI] [PubMed] [Google Scholar]
- 12.Verpoorte R. Antimicrobial activity of alkaloids. In: Roberts M. F., Wink M., editors. Alkaloids: Biochemistry, Ecology and Medicinal Applications . New York, NY, USA: Plenum Publishing Corporation; 1998. pp. 397–433. [Google Scholar]
- 13.Khafagi I., Dewedar A. The efficiency of random versus ethno-directed research in the evaluation of Sinai medicinal plants for bioactive compounds. Journal of Ethnopharmacology . 2000;71(3):365–376. doi: 10.1016/S0378-8741(00)00164-1. [DOI] [PubMed] [Google Scholar]
- 14.Correa M. P. Dicionário das plantas úteis do Brasil e das exóticas cultivadas, Ministério da Agricultura . Rio de Janeiro, Brazil: Instituto Brasileiro de Desenvolvimento Florestal; 1984. [Google Scholar]
- 15.Lorenzi H., Matos A. F. J. Plantas Medicinais no Brasil: nativas e exóticas. Editora Plantarum . Nova Odessa, SP: 2008. [Google Scholar]
- 16.Martins D. T., Rodrigues E., Casu L., Benítez G., Leonti M. The historical development of pharmacopeias and the inclusion of exotic herbal drugs with a focus on Europe and Brazil. Journal of Ethnopharmacology . 2019;240 doi: 10.1016/j.jep.2019.111891. [DOI] [PubMed] [Google Scholar]
- 17.Minayo M. C. S. O Desafio Do Conhecimento: Pesquisa Qualitativa Em Saúde . São Paulo, Brazil: Hucitec-Abrasco; 1998. [Google Scholar]
- 18.Chakraborty S., Siegenthaler J., Büchi E. R. Corneal edema due to Asclepias curassavica. Archives of Ophthalmology . 1995;113:p. 8. doi: 10.1001/archopht.1995.01100080024013. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton W. On the properties of the Asclepias curassavica, or bastard ipecacuanha. In: Daydon J. B., editor. Vegetable Technology . London, UK: Forgotten Books; 2013. pp. 78–79. [Google Scholar]
- 20.Wijayakusuma H. M. H. Ensiklopedia Milenium: Tumbuhan Berkhasiat Obat Indonesia . Jakarta, Indonesia: Prestasi Insan Indonesia; 2000. [Google Scholar]
- 21.Nadkarni K. M., Nadkarni A. K. DR. K.M. Nadkarni’s Indian Materia Medica: With Ayurvedic, Unani-Tibbi, Sidda, Allopathic, Homeopathic, Naturopathic & home Remedies, Appendices & Indexes . Bombay, India: Popular Prakashan Private Ltd; 1976. [Google Scholar]
- 22.Oliver B. B. Medicinal Plants in Tropical West Africa . Cambridge, London, UK: Cambridge University Press; 1986. [Google Scholar]
- 23.Timothy J. CRC Ethnobotany Desk Reference . Boca Raton, FL, USA: CRC Press LLC; 1998. [Google Scholar]
- 24.Al-Snafi A. E. Chemical constituents and pharmacological effects of Asclepias curassavica – a review. Asian Journal of Pharmaceutical Research . 2015;5(2):83–87. [Google Scholar]
- 25.Sahoo M. R., Dhanabalb S. P., Jadhav A. N., et al. Hydnocarpus: an ethnopharmacological, phytochemical and pharmacological review. Journal of Ethnopharmacology . 2014;154(1):17–25. doi: 10.1016/j.jep.2014.03.029. [DOI] [PubMed] [Google Scholar]
- 26.Lima J. A., Oliveira A. S., Miranda A. L. P., Pinto A. C. Anti-inflammatory and antinociceptive activities of an acid fraction of the seeds of Carpotroche brasiliensis (Raddi) (Flacourtiaceae) Brazilian Journal of Medical and Biological Research . 2005;38(7):1095–1103. doi: 10.1590/S0100-879X2005000700013. [DOI] [PubMed] [Google Scholar]
- 27.Fenner R., Betti A. H., Mentz L. A., Rates S. M. K. Plantas utilizadas na medicina popular brasileira com potential atividade antifúngica. Brazilian Journal of Pharmaceutical Sciences . 2006;42(3):369–394. [Google Scholar]
- 28.Khan S., Jan G., Bibi H., Murad W., Ullah K., Ihsanulla An ethnomedicinal survey of plants used in traditional medicine in arid and semi-arid zone of Bahadur Khel, district Karak, Khyber Pakhtunkhwa, Pakistan. Journal of Pharmacognosy and Phytochemistry . 2018;7(3):337–349. [Google Scholar]
- 29.Franca F., Lago E. L., Marsden P. D. Plant used in the treatment of leishmanial ulcers due to Leishmania (Vianna) braziliensis in an endemic area of Bahia, Brazil. Revista da Sociedade Brasileira de Medicina Tropical . 1996;29:229–232. doi: 10.1590/s0037-86821996000300002. [DOI] [PubMed] [Google Scholar]
- 30.Giove N. R. A. Traditional medicine in the treatment of enteroparasitosis. Revista de Gastroenterología del Perú . 1996;16(3):197–202. [PubMed] [Google Scholar]
- 31.Kiuchi F., Itano Y., Uchiyama N., et al. Monoterpene hydroperoxides with trypanocidal activity from Chenopodium ambrosioides. Journal of Natural Products . 2002;65(4):509–512. doi: 10.1021/np010445g. [DOI] [PubMed] [Google Scholar]
- 32.Monzote L., Sariego I., Montalvo A. M., Garrido N., Scull R., Abreu J. Propiedades antiprotozoarias de aceites esenciales extraidos de plantas cubanas. Revista Cubana de Medicina Tropical . 2004;56:230–233. [Google Scholar]
- 33.Kokanova-Nedialkova Z., Nedialkov P. T., Nikolov S. D. The genus Chenopodium: phytochemistry, ethnopharmacology and pharmacology. Pharmacognosy Reviews . 2009;3(6):280–309. [Google Scholar]
- 34.Botha E. W., Kahler C. P., du Plooy W. J., du Plooy S. H., Mathibe L. Effect of Boophone disticha on human neutrophils. Journal of Ethnopharmacology . 2005;96:385–388. doi: 10.1016/j.jep.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 35.Gelfand M., Mavi S., Drummond R. B., Ndemera B. The Traditional Medical Practitioner in Zimbabwe . Gweru, Zimbabwe: Mambo Press; 1985. [Google Scholar]
- 36.Van Wyk B. E., van Heerden F. R., van Oudtshoorn B. Poisonous Plants of South Africa . Pretoria, South Africa: Briza Publications; 2002. [Google Scholar]
- 37.Watt J. M., Breyer-Brandwijk M. G. The Medicinal and Poisonous Plants of Southern Africa . Edinburgh and London, UK: E & S Livingstone Publishers; 1962. [Google Scholar]
- 38.Gadaga L. L., Tagwireyi D., Dzangare J., Nhachi C. F. B. Acute oral toxicity and neurobehavioural toxicological effects of hydroethanolic extract of Boophone disticha in rats. Human & Experimental Toxicology . 2011;30(8):972–980. doi: 10.1177/0960327110384524. [DOI] [PubMed] [Google Scholar]
- 39.Asmawi M., Arafat O., Amirin S., Eldeen I. In vivo antinociceptive activity of leaf extract of Crinum asiaticum and phytochemical analysis of the bioactive fractions. International Journal of Pharmacology . 2011;7(1):125–129. doi: 10.3923/ijp.2011.125.129. [DOI] [Google Scholar]
- 40.Haque M., Jahan S., Rahmatullah M. Ethnomedicinal uses of Crinum asiaticum: a review. World Journal of Pharmacy and Pharmaceutical Sciences . 2014;3(9):119–128. [Google Scholar]
- 41.Samud A. M., Asmawi M. Z., Sharma J. N., Yusof A. P. Anti-inflammatory activity of Crinum asiaticum plant and its effect on bradykinin-induced contractions on isolated uterus. Immunopharmacology . 1999;43(2-3):311–316. doi: 10.1016/s0162-3109(99)00132-0. [DOI] [PubMed] [Google Scholar]
- 42.Mahomoodally M. F., Sadeer N. B., Suroowan S., Jugreet S., Lobine D., Rengasamy K. R. R. Ethnomedicinal, phytochemistry, toxicity and pharmacological benefits of poison bulb–Crinum asiaticum L. South African Journal of Botany . 2021;136:16–29. doi: 10.1016/j.sajb.2020.06.004. [DOI] [Google Scholar]
- 43.Nair J. J., Staden J. V. Traditional usage, phytochemistry and pharmacology of the South African medicinal plant Boophone disticha (L.f.) Herb. (Amaryllidaceae) Journal of Ethnopharmacology . 2014;151(1):12–26. doi: 10.1016/j.jep.2013.10.053. [DOI] [PubMed] [Google Scholar]
- 44.Schapera I. The Bantu Speaking Tribes of South Africa: An Ethnographical Survey . London, UK: G Routledge & Sons Ltd; 1937. Magic and medicine; pp. 221–245. [Google Scholar]
- 45.Barnett S. R. T. TX, USA: Texas State University. Master of Arts with a Major in Anthropology; 2013. Ancestral Pharmacopoeias: A Paleoethnobotanical Assessment of Plant Use in the Western Free State, South Africa. Thesis (Master) [Google Scholar]
- 46.Senchina D. S. Ethnobotany of poison ivy, poison oak, and relatives (Toxicodendron spp., Anacardiaceae) in America: veracity of historical accounts. Rhodora . 2006;108(935):203–227. [Google Scholar]
- 47.Patil C. R., Rambhade A. D., Jadhav R. B., et al. Modulation of arthritis in rats by Toxicodendron pubescens and its homeopathic dilutions. Homeopathy . 2011;100(3):131–137. doi: 10.1016/j.homp.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 48.García-Barriga H. Flora Medicinal Colombiana . Bogota, Colombia: Tercer Mundo Editores; 1992. [Google Scholar]
- 49.Garavito G., Rincón J., Arteaga L., et al. Antimalarial activity of some Colombian medicinal plants. Journal of Ethnopharmacology . 2006;107(3):460–462. doi: 10.1016/j.jep.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 50.Araújo Júnior G. N., Souza M. S., Simões V. J. L. P., et al. Espécies da família Euphorbiaceae na alimentação animal. PUBVET . 2018;12(8):1–8. doi: 10.31533/pubvet.v12n8a147.1-8. [DOI] [Google Scholar]
- 51.Dutta M. L. Plants used as ethnomedicine by the thengal kacharies of Assam, India. Asian Journal of Plant Science & Research . 2017;7(1):7–8. [Google Scholar]
- 52.David W. N. Poisonous Plants and Animals of Florida and the Caribbean . Hong Kong, China: Sing Cheong Print Co Ltd; 2012. [Google Scholar]
- 53.Fasola T. R., Iyamah P. C. The use of ethnobotanicals in the management of inflammation in Nigeria: a review. International Journal of Environment . 2015;4(2):1–18. doi: 10.3126/ije.v4i2.12620. [DOI] [Google Scholar]
- 54.Mahbubur Rahman A. H. M., Akter M. Taxonomy and traditional medicinal uses of apocynaceae (Dogbane) family of Rajshahi district, Bangladesh. International Journal of Botany Studies . 2016;1:5–13. [Google Scholar]
- 55.Suprapta D. N., Khalimi K. Anti-fungal activities of selected tropical plants from Bali Island. Phytopharmacology . 2012;2:265–270. [Google Scholar]
- 56.Bharath Kumar R., Asha S., Babu B. S. A note on phytodiversity and phytochemistry of important plant species of Vignan University Campus, Vadlamudi, Andhra Pradesh. International Journal of Pharma and Bio Sciences . 2014;5(1):373–386. [Google Scholar]
- 57.Agra M. F., Silva K. N., Basílio I. J. L. D., Freitas P. F., Barbosa-Filho J. M. Survey of medicinal plants used in the region Northeast of Brazil. Brazilian Journal of Pharmacognosy . 2008;18(3):472–508. [Google Scholar]
- 58.GrandiI T. S. M., TrindadeII J. A., PintoII M. J. F., Ferreira L. L., Catella A. C. Plantas medicinais de Minas gerais, Brasil. Acta Botanica Brasilica . 1989;3(2):p. 1. doi: 10.1590/S0102-33061989000300018. [DOI] [Google Scholar]
- 59.Indriunas A., Aoyama E. M. Systema materiae medicae vegetabilis brasiliensis de Martius: plantas empregadas para acidentes ofídicos. Ethnoscientia . 2018;3:1–7. doi: 10.22276/ethnoscientia.v3i0.97. [DOI] [Google Scholar]
- 60.Heinrich M., Chan J., Wanke S., Neinhuis C., Simmonds M. S. J. Local uses of Aristolochia species and content of nephrotoxic aristolochic acid 1 and 2—a global assessment based on bibliographic sources. Journal of Ethnopharmacology . 2009;125(1):108–144. doi: 10.1016/j.jep.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 61.Oliveira S., Kratz J. M., Chaves V. C., et al. Chemical Constituents and Pharmacology properties of Aristolochia triangularis: a south brazilian highly-consumed botanical with multiple bioactivities. Anais da Academia Brasileira de Ciências . 2019;91:p. 3. doi: 10.1590/0001-3765201920180621. [DOI] [PubMed] [Google Scholar]
- 62.Breitbach U. B., Niehues M., Lopes N. P., Faria J. E. Q., Brandão M. G. L. Amazonian Brazilian medicinal plants described by C.F.P. von Martius in the 19th century. Journal of Ethnopharmacology . 2013;147(1):180–189. doi: 10.1016/j.jep.2013.02.030. [DOI] [PubMed] [Google Scholar]
- 63.Rahmatullah M., Samarrai W., Jahan R., et al. An ethnomedicinal, pharmacological and phytochemical review of some Bignoniaceae family plants and a description of Bignoniaceae plants in folk medicinal uses in Bangladesh. Advances in Natural and Applied Sciences . 2010;4(3):236–253. [Google Scholar]
- 64.Mowrey D. B. Ancient Herb, Modern Medicine . Salt Lake City, Utah: Mountainwest Institute of Herbal Sciences; 2001. [Google Scholar]
- 65.Castellanos J. R., Prieto J. M., Heinrich M. Red Lapacho (Tabebuia impetiginosa)—a global ethnopharmacological commodity? Journal of Ethnopharmacology . 2009;121(1):1–13. doi: 10.1016/j.jep.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 66.Zhang J., Hunto S. T., Yang Y., Lee J., Cho J. Y. Tabebuia impetiginosa: a comprehensive review on traditional uses, phytochemistry, and immunopharmacological properties. Molecules . 2020;25(18):p. 4294. doi: 10.3390/molecules25184294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rai M., Bhattarai S., Feitosa C. M. Wild Plants: The Treasure of Natural Healers . New York, NY, USA: CRC Press; 2020. [Google Scholar]
- 68.Vieira B. B. Monografia (Bacharelado Em Gestão Ambiental) Rio de Janeiro, Brazil: Instituto Três Rios, Universidade Federal Rural do Rio de Janeiro; 2019. Averiguação do conhecimento botânico tradicional na comunidade rural do Brejal, distrito de Posse, Petrópolis, Rio de Janeiro. [Google Scholar]
- 69.Brandão M. G. L., Cosenza G. P., Grael C. F. F., onte-Mór R. L. M. Traditional uses of American plant species from the 1st edition of Brazilian Official Pharmacopoeia. Revista Brasileira de Farmacognosy . 2009;19 doi: 10.1590/S0102-695X2009000300023. [DOI] [Google Scholar]
- 70.Bucciarelli A., Minetti A., Milczakowskyg C., Skliar M. Evaluation of gastroprotective activity and acute toxicity of Solidago chilensis Meyen (Asteraceae) Pharmaceutical Biology . 2010;48(9):1025–1030. doi: 10.3109/13880200903453131. [DOI] [PubMed] [Google Scholar]
- 71.Petricevich V. L., Abarca-Vargas R. Allamanda cathartica: a review of the phytochemistry, pharmacology, toxicology, and biotechnology. Molecules . 2019;24(7):1238–1260. doi: 10.3390/molecules24071238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chavez M. L., Chavez P. I. Feverfew. Hospital Pharmacy . 1999;34:436–461. doi: 10.1177/001857879903400408. [DOI] [Google Scholar]
- 73.Jain N. K., Kulkarni S. K. Antinociceptive and anti-inflammatory effects of Tanacetum parthenium L. extract in mice and rats. Journal of Ethnopharmacology . 1999;68(1-3):251–259. doi: 10.1016/s0378-8741(99)00115-4. [DOI] [PubMed] [Google Scholar]
- 74.Heptinstall S., Awang D. W., Dawson B. A., Kindack D., Knight D. W. Parthenolide content and bioactivity of feverfew (Tanacetum parthenium (L.) schultz-bip.). Estimation of commercial and authenticated feverfew products. Journal of Pharmacy and Pharmacology . 1992;44(5):391–395. doi: 10.1111/j.2042-7158.1992.tb03631.x. [DOI] [PubMed] [Google Scholar]
- 75.Pittler M. H., Ernst E. Feverfew for preventing migraine. Cochrane Database of Systematic Reviews . 2004;1:p. 2286. doi: 10.1002/14651858.CD002286.pub2. [DOI] [PubMed] [Google Scholar]
- 76.Setty A. R., Sigal L. H. Herbal medications commonly used in the practice of rheumatology: mechanisms of action, efficacy, and side effects. Seminars in Arthritis and Rheumatism . 2005;34(6):773–784. doi: 10.1016/j.semarthrit.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 77.Sumner H., Salan U., Knight D. W., Hoult J. R. Inhibition of 5-lipoxygenase and cyclo-oxygenase in leukocytes by feverfew. Involvement of sesquiterpene lactones and other components. Biochemical Pharmacology . 1992;43(11):2313–2320. doi: 10.1016/0006-2952(92)90308-6. [DOI] [PubMed] [Google Scholar]
- 78.Goleniowski M. E., Bongiovanni G. A., Palacio L., Nuñez C. O., Cantero J. J. Medicinal plants from the sierra de Comechingones. Argentina Journal of Ethnopharmacology . 2006;107(3):324–341. doi: 10.1016/j.jep.2006.07.026. [DOI] [PubMed] [Google Scholar]
- 79.Rateb M. E. M., ElGendy A. N. A. M., ElHawary S. S., ElShamy A. M. Phytochemical and biological investigation of Tanacetum parthenium (L.) cultivated in Egypt. Journal of Medicinal Plants Research . 2007;1(1):18–26. [Google Scholar]
- 80.Linajes A., Rico-Gray V., Carrión G. Traditional production system of the root of jalapa, Ipomoea purga (convolvulaceae), in Central Veracruz, Mexico. Economic Botany . 1994;48:84–89. [Google Scholar]
- 81.Xavier T. F., Kanna M., Lija L., et al. Ethnobotanical study of kani tribes in thoduhills of Kerala, south India. Journal of Ethnopharmacology . 2014;152(1):78–90. doi: 10.1016/j.jep.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 82.Lira-Ricárdez J., Pereda-Miranda R., Castañeda-Gómez J., Fragoso-Serrano M., Simas R. C., Leitão S. G. Resin glycosides from the roots of Operculina macrocarpa (Brazilian jalap) with purgative activity. Journal of Natural Products . 2019;82(6):1664–1677. doi: 10.1021/acs.jnatprod.9b00222. [DOI] [PubMed] [Google Scholar]
- 83.França R. C. M., da Silva T. R., Santos E. E. S., Severo D. O., Daniel V. P., Hoefel M. G. L. Rapé como prática cultural integrativa e terapêutica dos povos indígenas: um estudo de caso a partir do olhar indígena. Antropología Andina . 2015;2(2):87–104. [Google Scholar]
- 84.White D. M., Islam M. B., Mason-Gamer R. J. Phylogenetic inference in section Archerythroxylum informs taxonomy, biogeography, and the domestication of coca (Erythroxylum species) American Journal of Botany . 2019;106(1):154–165. doi: 10.1002/ajb2.1224. [DOI] [PubMed] [Google Scholar]
- 85.Castro V. P. A virada ontológica da antropologia e o futuro da literatura comparada. Remate de Males . 2020;40:p. 1. doi: 10.20396/remate.v40i1.8656229. [DOI] [Google Scholar]
- 86.Ribeiro R. V., Bieski I. G. C., Balogun S. O., Martins D. T. O. Ethnobotanical study of medicinal plants used by ribeirinhos in the north araguaia microregion, mato grosso, Brazil. Journal of Ethnopharmacology . 2017;205(9):69–102. doi: 10.1016/j.jep.2017.04.023. [DOI] [PubMed] [Google Scholar]
- 87.Lorenzi H., de Souza H. M., Torres M. A. V., Bacher L. B. Árvores Exóticas no Brasil-madeireiras, ornamentais e aromáticas . São Paulo, Brazil: Editora Plantarum; 2003. [Google Scholar]
- 88.Dillon P. M., Lowrie S., McKey D. Disarming the evil woman: petiole constriction by a sphingid larva circumvents mechanical defenses of its host plant, Cnidoscolus urens (Euphorbiaceae) Biotropica . 1983;15(2):112–116. doi: 10.2307/2387953. [DOI] [Google Scholar]
- 89.Dos Reis G. O., Vicente G., Carvalho F. K., et al. Croton antisyphiliticus Mart. attenuates the inflammatory response to carrageenan-induced pleurisy in mice. Inflammopharmacology . 2014;22(2):115–126. doi: 10.1007/s10787-013-0184-6. [DOI] [PubMed] [Google Scholar]
- 90.Oliveira T. G., Pereira A. M. S., Coppede J. S., Franca S. C., Ming L. C., Bertoni B. W. Genetic diversity analysis of Croton antisyphiliticus Mart. using AFLP molecular markers. Genetics and Molecular Research . 2016;15:p. 1. doi: 10.4238/gmr.15017461. [DOI] [PubMed] [Google Scholar]
- 91.Wojtyniak K., Szymański M., Matławska I. Leonurus cardiaca L. (motherwort): a review of its phytochemistry and pharmacology. Phytotherapy Research . 2012;27(8):1115–1120. doi: 10.1002/ptr.4850. [DOI] [PubMed] [Google Scholar]
- 92.Carvalho F. K. Programa de Pós-Graduação em Química . Santa Catarina, Brazil: Universidade Federal de Santa Catarina, Centro de Ciências Físicas e Matemáticas; 2013. Análise fitoquímica e atividade biológica de Croton antisyphiliticus Martius e Croton heterodoxus Baillon. [Google Scholar]
- 93.Aiyelaagbe O. O., Adesogan E. K., Ekundayo O., Adeniyi B. A. The antimicrobial activity of roots of Jatropha podagrica (Hook) Phytoterapy Research . 2000;14(1):60–62. doi: 10.1002/(sici)1099-1573(200002)14:1<60::aid-ptr597>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 94.Irvine F. R. Woody Plants of Ghana . London, UK: Oxford University Press; 1961. [Google Scholar]
- 95.Bhaskarwar B., Itankar P., Fulke A. Evaluation of antimicrobial activity of medicinal plant Jatropha podagrica (Hook) Romanian Biotechnological Letters . 2008;13(5):3873–3877. [Google Scholar]
- 96.Cunha e Silva S. L., Borba H. R., Bonfim T. C. B., Carvalho M. G., Cavalcanti H. L., Barbosa C. G. Ação anti-helmíntica de extratos brutos de Andira anthelmia (Vell.) Macbr. e Andira fraxinifolia Benth, em camundongos naturalmente infectados por Vampirolepis nana e Aspiculuris tetráptera. Parasitología latinoamericana . 2003;58(1-2) doi: 10.4067/S0717-77122003000100004. [DOI] [Google Scholar]
- 97.Garcia C., Urso-Guimarães M. V. Three new species of lopesia rübsaamen (Diptera: cecidomyiidae) from Brazil. Florida Entomologist . 2018;101(2):203–211. doi: 10.1653/024.101.0208. [DOI] [Google Scholar]
- 98.Silberbauer-Gottsberger I. O Cerrado como potencial de plantas medicinais e tóxicas. Oréades . 1982;8(14-15):15–30. [Google Scholar]
- 99.Hussain H., Hussain J., Al-Harrasi A., Saleem M., Green I. R. Chemistry and biology of genus Vismia. Pharmaceutical Biology . 2012;50(11):1448–1462. doi: 10.3109/13880209.2012.680972. [DOI] [PubMed] [Google Scholar]
- 100.Vizcaya M., Morales A., Rojas J., Nuñez R. Revisión bibliográfica sobre la composición química y actividades farmacológicas del género Vismia (Guttiferae) Boletin Latinoamericano y del Caribe de Plantas Medicinales y Aromaticas . 2012;11(1):12–34. [Google Scholar]
- 101.Godinho C. C. Caracterização morfo-anatômica de beressol [Trimezia juncifolia (Klatt.) Benth]. 67f. Dissertação (Bacharelado em Farmácia-Bioquímica), Universidade Estadual Paulista (UNESP) Araraquara, Brazil: Faculdade de Ciências Farmacêuticas; 2012. [Google Scholar]
- 102.Ono M. Resin glycosides from Convolvulaceae plants. Journal of Natural Medicines . 2017;71(4):591–604. doi: 10.1007/s11418-017-1114-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Llorente A. A., Esteve N. M. Therapeutic potential of motherwort (Leonurus cardiaca L) Revista de Fitoterapia . 2015;15(2):101–107. [Google Scholar]
- 104.Brinkman A. H. Notes on some Canadian hepatics, no. 2 (concluded) The Bryologist . 1931;34(3):38–44. doi: 10.2307/3239651. [DOI] [Google Scholar]
- 105.Peckolt G. Anatomical description, alkaloid content and quality control of the bark of Pau-pereira (Geissospermum laeve, Apocynaceae) Revista da Flora Medicinal . 1942;9:p. 333. [Google Scholar]
- 106.Altschul S. Drugs and Foods from Little Known Plants . Cambridge, UK: Harvard University Press; 1973. [Google Scholar]
- 107.Achenbach H., Hübner H., Vierling W., Brandt W., Reiter M. Spiganthine, the cardioactive principle of Spigelia anthelmia. Journal of Natural Products . 1995;58(7):1092–1096. doi: 10.1021/np50121a019. [DOI] [PubMed] [Google Scholar]
- 108.Xu X.-L., Yang L.-J., Jiang J.-G. Renal toxic ingredients and their toxicology from traditional Chinese medicine. Expert Opinion on Drug Metabolism and Toxicology . 2016;12(2):149–159. doi: 10.1517/17425255.2016.1132306. [DOI] [PubMed] [Google Scholar]
- 109.Ayaz M., Ullah F., Sadiq A., Kim M. O., Ali T. Editorial: natural products-based drugs: potential therapeutics against alzheimer’s disease and other neurological disorders. Frontiers in Pharmacology . 2019;10:p. 1417. doi: 10.3389/fphar.2019.01417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Guo R., Wang T., Zhou G., et al. Botany, phytochemistry, pharmacology and toxicity of Strychnos nux-vomica L.: a review. The American Journal of Chinese Medicine . 2018;46(1):1–23. doi: 10.1142/S0192415X18500015. [DOI] [PubMed] [Google Scholar]
- 111.Andrade-Neto V. F., Brandão M. G. L., Stehmann J. R., Oliveira L. A., Krettli A. U. Antimalarial activity of Cinchona-like plants used to treat fever and malaria in Brazil. Journal of Ethnopharmacology . 2003;87(2-3):253–256. doi: 10.1016/s0378-8741(03)00141-7. [DOI] [PubMed] [Google Scholar]
- 112.Anesini C., Perez C. Screening of plants used in Argentine folk medicine for antimicrobial activity. Journal of Ethnopharmacology . 1993;39(2):119–128. doi: 10.1016/0378-8741(93)90027-3. [DOI] [PubMed] [Google Scholar]
- 113.Guzman-Hernandez E. A., Segura-Cobos D., Amato D., Avila-Acevedo J. G., Vazquez-Cruz B. Evaluation of antihypertensive and vasorelaxant effects of Heimia salicifolia (family: lythraceae) African Journal of Pharmacy and Pharmacology . 2018;12(3):41–51. doi: 10.5897/AJPP2017.4860. [DOI] [Google Scholar]
- 114.Ricardo L. M., Paula-Souza J., Andrade A., Brandão N. G. L. Plants from the Brazilian traditional medicine: species from the books of the polish physician piotr czerniewicz (pedro luiz napoleão chernoviz, 1812–1881) Revista Brasileira de Farmacognosia . 2017;27(3):388–400. doi: 10.1016/j.bjp.2017.01.002. [DOI] [Google Scholar]
- 115.Van Andel T., Korte S., Koopmans D., Behari-Ramdas J., Ruysschart S. Dry sex in Suriname. Journal of Ethnopharmacology . 2008;116(1):84–88. doi: 10.1016/j.jep.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 116.Queiroz M. S., Cargnin R. A., Castilho L. O., Vieira M. C., Heredia N. A., Scalon S. P. Q. Ethnobotanic study of medicinal plants in traces of native forest of the Paradouro farm, in Dourados-MS, Brazil. Revista da Associação Brasileira de Horticultura . 2006;29:p. 2. [Google Scholar]
- 117.Gaitén Y. I. G., Yaque J. G. Medicinal plants and natural products. Revista de Ciencias Farmacéuticas y Alimentarias . 2019;5:174–195. [Google Scholar]
- 118.Porchselvi C., Muthulakshmi S. Pharmacognostic and phytochemical evaluation of Antiaris toxicaria (Pers). Lesch. Journal of Medicinal Plants Studies . 2018;6(6):217–221. [Google Scholar]
- 119.Mante P. K., Adongo D. W., Woode E., Kukuia K. K. E., Ameyaw E. O. Anticonvulsant effect of Antiaris toxicaria (pers.) lesch. (Moraceae) aqueous extract in rodents. ISRN Pharmacology . 2013;2013:9. doi: 10.1155/2013/519208.519208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Van den Berg M. E., Silva M. H. L. Contribuição ao conhecimento da flora medicinal de Roraima. Acta Amazoniza . 1988;18:1–2. doi: 10.1590/1809-43921988185035. [DOI] [Google Scholar]
- 121.Pereira L. J. Characterization Anatomical and Phytochemical the Bark the Ficus Adhatodifolia Schott Ex Spreng (Moraceae) Viçosa, Brazil: Universidade Federal de Viçosa; 2014. [Google Scholar]
- 122.Rody H. V. S., Gontijo D., Coelho V. P., et al. Mutagenic activity and chemical composition of phenolic-rich extracts of leaves from two species of Ficus medicinal plants. Journal of Toxicology and Environmental Health . 2018;81(17):861–872. doi: 10.1080/15287394.2018.1498420. [DOI] [PubMed] [Google Scholar]
- 123.Oliveira A. H., Andrade A. O., Silva M. A. P., Coutinho H. D. M. Atividade biológica de Ficus gomelleira KUNTH (Moraceae) Caderno de Cultura e Ciência . 2015;14:p. 1. doi: 10.14295/cad.cult.cienc.v14i1.938. [DOI] [Google Scholar]
- 124.Hattori E. K. O., Nakajima J. N. A família asteraceae na estação de pesquisa e desenvolvimento ambiental Galheiro, Perdizes, Minas Gerais, Brasil. Rodriguesia . 2008;59(4):687–749. [Google Scholar]
- 125.Queiroz J. M. G., Suzuki M. C. M., Motta A. P. R., Nogueira J. M. R., Carvalho E. M. Popular and scientific aspects of Eugenia species use as herbal. Revista Fitos . 2015;9(2):73–159. doi: 10.5935/2446-4775.20150008. [DOI] [Google Scholar]
- 126.Santos J. F. L., Pagani E., Ramos J., Rodrigues E. Observations on the therapeutic practices of riverine communities of the Unini River, AM, Brazil. Journal of Ethnopharmacology . 2012;142(2):503–515. doi: 10.1016/j.jep.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 127.Hocking G. N. A Dictionary of Terms in Pharmacognosy and Other Divisions of Economic Botany . Springfield, IL, USA: Charles C Thomas; 1955. [Google Scholar]
- 128.Parfitt K. Turnera aphrodisiaca (damiana) In: Giron L., Caceres A., editors. Martindale. The Complete Drug Reference . London, UK: Pharmaceutical Press; 1999. [Google Scholar]
- 129.Kumar S., Taneja R., Sharma A. Pharmacognostic standardization of Turnera aphrodisiaca ward. Journal of Medicinal Food . 2006;9:p. 2. doi: 10.1089/jmf.2006.9.254. [DOI] [PubMed] [Google Scholar]
- 130.Chudapongse N., Kamkhunthod M., Poompachee K. Effects of Phyllanthus urinaria extract on HepG2 cell viability and oxidative phosphorylation by isolated rat liver mitochondria. Journal of Ethnopharmacology . 2010;130(2):315–319. doi: 10.1016/j.jep.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 131.Hout S., Chea A., Bun S. S., et al. Screening of selected indigenous plants of Cambodia for antiplasmodial activity. Journal of Ethnopharmacology . 2006;107(1):12–18. doi: 10.1016/j.jep.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 132.Suthienkul O., Miyazaki O., Chulasiri M., Kositanont U., Oishi K. Retroviral reverse transcriptase inhibitory activity in Thai herbs and spices: screening with Moloney murine leukemia viral enzyme. Southeast Asian Journal of Tropical Medicine and Public Health . 1993;24:751–755. [PubMed] [Google Scholar]
- 133.Geethangili M., Ding S. T. A review of the phytochemistry and pharmacology of Phyllanthus urinaria L. Frontiers in Pharmacology . 2018;9:p. 1109. doi: 10.3389/fphar.2018.01109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hasrat J. A., Vlietinck A. J., De Backer J. P., Vauquelin G. Medicinal plants in Surinami: screening of plant extracts for receptor binding activity, part 1. Phytomedicine . 1997a;4:59–65. doi: 10.1016/S0944-7113(97)80029-3. [DOI] [PubMed] [Google Scholar]
- 135.Hasrat J. A., De Bruyne T., Backer J.-P., Vauquelin G., Vlietinck J. Cirsimarin and cirsimaritin, flavonoids of Microtea debilis (phytolaccaceae) with adenosine antagonistic properties in rats: leads for new therapeutics in acute renal failure. Journal of Pharmacy and Pharmacology . 1997b;49(11):1150–1156. doi: 10.1111/j.2042-7158.1997.tb06059.x. [DOI] [PubMed] [Google Scholar]
- 136.Quattrocchi U. CRC World Dictionary of Medicinal and Poisonous Plants: Common Names, Scientific Names, Eponyms, Synonyms, and Etymology . Boca Raton, FL, USA: CRC Press; 2012. [Google Scholar]
- 137.Tomchinsky B., Ming L. C., Kinupp V. F., Hidalgo A. F., Chaves F. C. M. Etnobotânica de plantas antimaláricas no médio Rio Negro, Amazonas, Brasil. Acta Amazonica . 2017;47:p. 3. doi: 10.1590/1809-4392201701191. [DOI] [Google Scholar]
- 138.Silva A. M. P., Paiva S. R., Figueiredo M. R., Kaplan M. A. C. Atividade biológica de Naftoquinonas de Espécies de Bignoniaceae. Revista Fitos . 2012;7(4):207–215. [Google Scholar]
- 139.Vázquez M. A. A., Estrada A. R., Limón S. M., editors. De la lechuguilla a las biopelículas vegetales: las plantas útiles de nuevo león . Mexico: Universidad Autónoma de Nuevo León; 2010. [Google Scholar]
- 140.Cañavate J. L. R. Fitoterapia de la inflamación. Natura Medicatrix: Revista Médica para el Estudio y Difusión de las Medicinas Alternativas . 1995;37:80–85. [Google Scholar]
- 141.Silva F. N. G. M. Plantas indicadas como diuréticas no Brasil desde Martius, 1843. 586p. Dissertação (Mestrado). Programa de Pós-Graduação em Fisiologia . Recife, Brazil: Universidade Federal de Pernambuco; 2003. [Google Scholar]
- 142.Mentz L. A., Lutzemberger L. C., Schenkel E. P. Da flora medicinal do Rio Grande do Sul: notas sobre a obra de D’Ávila (1910) Caderno de Farmácia . 1997;13(1):25–47. [Google Scholar]
- 143.Giacomelli S. R. 333f. Tese (Doutorado em Química), Curso de Pós Graduação em Química . Santa Maria, CA, USA: Universidade Federal de Santa Maria (RS); 2005. Estudo fitoquímico de três espécies pertencentes à família Rhamnaceae: Discaria americana, Colletia paradoxa e Gouania ulmifolia. [Google Scholar]
- 144.Dias S. R. K., Alcantara M. M. A. C., Pessoa D. M. A. Ethnobotanical, phytochemical and pharmacological aspects Rubiaceae species in Brazil. Revista Cubana de Plantas Medicinales . 2013;18(1):140–156. [Google Scholar]
- 145.Moraes M. A. Potencial químico-farmacológico de Palicourea rigida Kunth. 120f. Dissertação (Mestrado) – Programa de Pós-Graduação em Ciências Farmacêuticas . Juiz de Fora, Brazil: Universidade Federal de Juiz de Fora; 2013. Análise da legislação sobre o uso de plantas medicinais no Brasil. [Google Scholar]
- 146.Moraes M. A., Santos B. C. S., Fabri R. L., Scio E. Pharmacological potential of Palicourea rigida kunth: a possible participation of flavonoid. Academics Journals . 2017;11(10):194–206. doi: 10.5897/JMPR2016.6320. [DOI] [Google Scholar]
- 147.Ferreira I. V. Perspectiva de Uso da Palicourea rigida na odontologia. 33f. Monografia (Graduação) Lavras, Brazil: Centro Universitário de Lavras; 2019. [Google Scholar]
- 148.Souza R. K. D., Mendonça A. C. A. M., Silva M. A. P. Aspectos etnobotânicos, fitoquímicos e farmacológicos de espécies de Rubiaceae no Brasil. Revista Cubana de Plantas Medicinales . 2013;18(1):140–156. [Google Scholar]
- 149.Figueiredo A. D. L., Bustamante K. G. L., Soares M. L., et al. Avaliação da atividade antimicrobiana das partes aéreas (folhas e caules) e raízes de Richardia brasiliensis Gomez (Rubiaceae) Revista de Ciências Farmacêutica e Básica Aplicada . 2009;30(2):193–196. [Google Scholar]
- 150.Souza F. H. T. Fitoquímica de Borreria verticillata (L.) G. Mey., Borreria ocymoides (Burm. f.) DC. e Richardia brasiliensis Gomes (Rubiaceae) João Pessoa: Universidade Federal da Paraíba; 2013. [Google Scholar]
- 151.Schinnerl J. Vienna: University of Vienna; 2013. Tropical Chemodiversity in Selected Angiosperm Families. 105f. Dissertation (PhD) [Google Scholar]
- 152.Oliveira T. D. Levantamento etnobotânico de plantas medicinais utilizadas no bairro Saramenha de Cima, Ouro Preto, Minas Gerais . Ouro Preto, Brazil: Universidade Federal de Ouro Preto, Escola de Farmácia; 2017. [Google Scholar]
- 153.Dornelles R. C. Programa de Pós-Graduação em Agrobiologia . Santa Maria: Universidade Federal de Santa Maria; 2015. Potencial antiproliferativo, genotóxico e fitoquímica de Richardia brasiliensis Gomes. [Google Scholar]
- 154.Ricardo L. M. Programa de Pós-Graduação em Medicamentos e Assistência Farmacêutica . Minas Gerais, Brazil: Universidade Federal de Minas Gerais; 2017. Evidência de tradicionalidade de uso de plantas medicinais: proposta de metodologia para o desenvolvimento de fitoterápicos para tratamento de feridas no Brasil. [Google Scholar]
- 155.Botsaris A. S. Plants used traditionally to treat malaria in Brazil: the archives of Flora Medicinal. Journal of Ethnobiology and Ethnomedicine . 2007;3(18):1–8. doi: 10.1186/1746-4269-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Carvalho L. H., Brandao M. G. L., Santos-Filho D., Lopes J. L. C., Krettli A. U. Antimalarial activity of crude extracts from Brazilian plants studied in vivo in Plasmodium berghei infected mice and in vitro against Plasmodium falciparum in culture. Brazilian Journal of Medical and Biological Research . 1991;24(11):1113–1123. [PubMed] [Google Scholar]
- 157.Dolabela M. F., Oliveira S. G., Nascimento J. M., et al. In vitro antiplasmodial activity of extract and constituents from Esenbeckia febrifuga, a plant traditionally used to treat malaria in the Brazilian Amazon. Phytomedicine . 2008;15(5):367–372. doi: 10.1016/j.phymed.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 158.Brandão M. G. L., Pignal M., Romaniuc S., Grael C. F. F., Fagg C. W. Useful Brazilian plants listed in the field books of the French naturalist Auguste de Saint-Hilaire (1779–1853) Journal of Ethnopharmacology . 2012;143(2):488–500. doi: 10.1016/j.jep.2012.06.052. [DOI] [PubMed] [Google Scholar]
- 159.Burger M. C. M. Alcaloides e diidrochalconas de Metrodorea stipularis: química e bioatividade. 145f. Tese (Doutorado) São Carlos, Brazil: Universidade Federal de São Carlos; 2014. [Google Scholar]
- 160.Biavatti M. W., Marensi V., Leite S. N., Reis A. Ethnopharmacognostic survey on botanical compendia for potential cosmeceutic species from Atlantic Forest. Revista Brasileira de Farmacognosia . 2007;17:p. 4. doi: 10.1590/S0102-695X2007000400025. [DOI] [Google Scholar]
- 161.Rodríguez-Echeverry J. J. Uso y manejo tradicional de plantas medicinales y mágicas en el Valle de Sibundoy, Alto Putumayo, y su relación con procesos locales de construcción ambiental. Revista de la Academia Colombiana de Ciencias Exactas Fisicas y Naturales . 2010;34(132):309–326. [Google Scholar]
- 162.Méndez R. M., editor. El Huerto familiar del Sureste de México . Mexico: Secretaria de Recursos Naturales y Protección Ambiental; 2012. [Google Scholar]
- 163.Vasconcellos M. C., Bezerra D. P., Fonseca A. M., et al. Antitumor activity of biflorin, an o-naphthoquinone isolated from Capraria biflora. Biological and Pharmaceutical Bulletin . 2007;30(8):1416–1421. doi: 10.1248/bpb.30.1416. [DOI] [PubMed] [Google Scholar]
- 164.Ritter M. R., Sobierajski G. R., Schenkel E. P., Mentz L. A. Plantas usadas como medicinais no município de Ipê, RS, Brasil. Revista Brasileira de Farmacognosia . 2002;12(2):51–62. [Google Scholar]
- 165.Santo A. P. E. Faculdade de Ciências Farmacêuticas . São Paulo, Brazil: Universidade de São Paulo; 2007. Estudo farmacognóstico comparativo entre duas espécies da família Tropaeolaceae que ocorrem na região sul do Brasil: tropaeolum majus L. e Tropaeolum pentaphyllum Lam-em busca de atividade anti-Leishmania chagasi e anticoagulante sobre plasma humano. Dissertação (Mestrado) [Google Scholar]
- 166.Madriz-Masís J. P. Exploración etnobotánica de la flora silvestre comestible en los bosques húmedos tropicales de la reserva aborigen Tayní, Limón, Costa Rica. Tecnología em Marcha . 1997;13(5):188–192. doi: 10.18845/tm.v13i0.2931. [DOI] [Google Scholar]
- 167.Patzlaff R. G. Estudo etnobotânico de plantas de uso medicinal e místico na comunidade da Capoeira Grande, Pedra de Guaratiba, Rio de Janeiro, RJ, Brasil. 124f. Dissertação (mestrado) Rio de Janeiro, Brazil: Instituto de Pesquisas Jardim Botânico do Rio de Janeiro, Escola Nacional de Botânica Tropical; 2007. [Google Scholar]
- 168.Ayme Y. M. Estudio etnobotánico y etnofarmacológico de plantas medicinales de Tambopata, Madre de Dios, Perú. Ciencia y Desarrollo . 2021;24(1):80–98. [Google Scholar]
- 169.Rueda M. G., Torres M. T. Etnobotanica y usos de las plantas de la comunidad rural de Sogamoso, Boyacá, Colombia. Revista de Investigación Agraria y Ambiental . 2017;8(2):187–206. [Google Scholar]
- 170.Marrassini C., Acevedo C., Miño J., Ferraro G., Gorzalczany S. Evaluation of antinociceptive, antinflammatory activities and phytochemical analysis of aerial parts of Urtica urens L. Phytotherapy Research . 2010;24(12):1807–1812. doi: 10.1002/ptr.3188. [DOI] [PubMed] [Google Scholar]
- 171.Azevedo K. T. C., Quednau L., Costa M. K. Vocabulário Latim-Português Baseado No Livro Lingua Latina Per Se Illustrata – Familia Romana . Porto Alegre, Brazil: Academia; 2016. [Google Scholar]
- 172.Brown R. W. Composition of Scientific Words . Washington, DC, USA: Smithsonian Institution; 1956. [Google Scholar]
- 173.Stearn W. T. Botanical Latin . Portland, OR, USA: Timber Press; 2006. [Google Scholar]
- 174.Staub P. O., Geck M. S., Weckerle C. S., Casu L., Leonti M. Classifying diseases and remedies in ethnomedicine and ethnopharmacology. Journal of Ethnopharmacology . 2015;174:514–519. doi: 10.1016/j.jep.2015.08.051. [DOI] [PubMed] [Google Scholar]
- 175.Silva S. M. M., Silva C. A. G., Fonseca-Bazzo Y. M., Magalhães P. O., Silveira D. Eugenia dysenterica Mart. Ex dc. (cagaita): planta brasileira com potential terapêutico. Ciências Farmacêuticas . 2015;27(1):49–95. doi: 10.14450/2318-9312.v27.e1.a2015.pp49-95. [DOI] [Google Scholar]
- 176.Barbosa B. B., Júnior L. C. Plantas medicinais: camomila. Escola superior de Agricultura luiz de Queiroz. Piracicaba – ESALQ . 2019;67:p. 42. [Google Scholar]
- 177.Chandler R. F., Hooper S. N., Hooper D. L., Jamieson D. W., Flinn C. G. Herbal remedies of the maritime Indian: sterols and triterpenes of Achillea millefolium L (Yarrow) Journal of Pharmaceutical Sciences . 1982;7(1):690–693. doi: 10.1002/jps.2600710621. [DOI] [PubMed] [Google Scholar]
- 178.Begum S., AbdEIslam N. M., Adnan M., Tariq A., Yasmin A., Hameed R. Ethnomedicines of highly utilized plants in the temperate Himalayan region. African Journal of Traditional, Complementary and Alternative Medicines . 2014;11(3):132–142. doi: 10.4314/ajtcam.v11i3.20132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.El-Sadek S. E., El-Gendy A. A. M., Tohamy M. A., Abd El-Aa M. A. Anti-inflammatory, antipyretic and analgesic effect of Achillea millefolium and Salix plants. Journal of Veterinary Medical Research . 2007;17(1):86–92. doi: 10.21608/jvmr.2007.77898. [DOI] [Google Scholar]
- 180.Pareek A., Suthar M., Rathore G. S., Bansal V. Feverfew (Tanacetum parthenium L.): a systematic review. Pharmacognosy Reviews . 2011;5(9):103–110. doi: 10.4103/0973-7847.79105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.García M. S., Martinez M. P., Díaz S., Del V., Sansó R. L., Capote E. M. Intoxicación exógena por Jatropha urens (chaya) Medisan . 2002;6(3):103–106. [Google Scholar]
- 182.Stewart A. N., Morrow-Cribbs B., Rosen J. Wicked Plants: The Weed that Killed Lincoln’s Mother & Other Botanical Atrocities . Chapel Hill, North Carolina: Algonquin Books of Chapel Hill; 2009. [Google Scholar]
- 183.Shih R. D., Nelson L., Balick M. J. Handbook of Poisonous and Injurious Plants . India: Springer; 2007. [Google Scholar]
- 184.Pereira S., Taleb-Contini S., Coppede J., et al. An ent-kaurane-type diterpene in Croton antisyphiliticus Mart. Molecules . 2012;17(8):8851–8858. doi: 10.3390/molecules17088851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Li W., Hu Q., Chan W. Uptake and accumulation of nephrotoxic and carcinogenic aristolochic acids in food crops grown in Aristolochia clematitis-contaminated soil and water. Journal of Agricultural and Food Chemistry . 2016;64(1):107–112. doi: 10.1021/acs.jafc.5b05089. [DOI] [PubMed] [Google Scholar]
- 186.Kaur A., Bhatti R. Understanding the phytochemistry and molecular insights to the pharmacology of Angelica archangelica L. (garden angelica) and its bioactive components. Phytotherapy Research . 2021;35(11):5961–5979. doi: 10.1002/ptr.7206. [DOI] [PubMed] [Google Scholar]
- 187.Haybar H., Javid A. Z., Haghighizadeh M. H., Valizadeh E. The effects of Melissa officinalis supplementation on depression, anxiety, stress, and sleep disorder in patients with chronic stable angina. Clinical Nutrition . 2018;26:47–52. doi: 10.1016/j.clnesp.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 188.Da Silva A. S. B., Owiti A. O., Barbosa W. L. R. Pharmacology of Mikania genus: a systematic review. Pharmacognosy Reviews . 2018;12(24):230–237. doi: 10.4103/phrev.phrev_10_18. [DOI] [Google Scholar]
- 189.Parente L. M. L., Júnior R. S. L., Tresvenzol L. M. F., Vinaud M. C., de Paula J. R., Paulo N. M. Wound healing and anti-inflammatory effect in animal models of Calendula officinalis L. Growing in Brazil. Evidence-based Complementary and Alternative Medicine . 2012;2012:7. doi: 10.1155/2012/375671.375671 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.


