Abstract
Objective: Borderline personality disorder (BPD) is a serious public health problem. Dialectical Behavior Therapy (DBT) is a program that has provided encouraging results for its treatment. However, scientific evidence about its efficacy is scarce. Therefore, we aimed to describe the scientific production on the components of the DBT program and its therapeutic efficacy in the treatment of people with BPD.
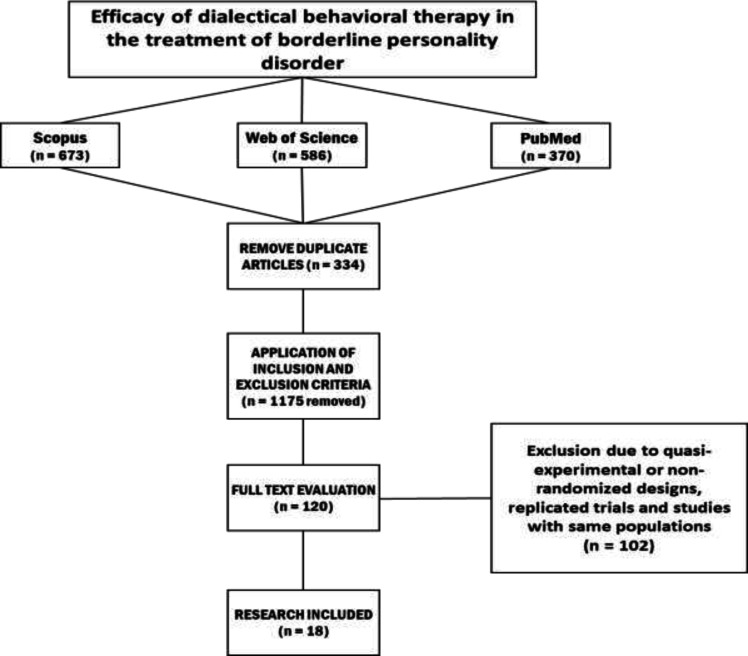
Method : A systematic review with relevant keywords was conducted based on studies available in Scopus, Web of Science, and PubMed until June 2023, including studies in English, research on therapeutic intervention, studies with a randomized controlled trial (RCT) design that included people with the diagnosis of BPD.
Results: We found 18 RCTs, most of which supported the effectiveness of DBT for BPD. There were a total of 1,755 participants in these studies, most of whom were women. These studies looked for treating self-injurious behaviors, suicidal thoughts or ideations, number of visits to emergency services, and frequency of hospital admissions. Most studies revealed that both short-term DBT and standard DBT improved suicidality in BPD patients with small or moderate effect sizes, lasting up to 24 months after the treatment period. Furthermore, these studies showed that DBT can significantly improve general psychopathology and depressive symptoms in patients with BPD. Improvement of compliance, impulsivity, mood instability, as well as reduction in hospitalization rate are other findings observed in the trials following DBT.
Conclusion: Although DBT shows efficacy in the treatment of BPD, heterogeneity in the methodologies employed is highlighted. Therefore, it is necessary to design studies from a homogeneous theoretical and methodological framework.
Key Words: Borderline Personality Disorder, Dialectical Behavior Therapy, Randomized Controlled Trial, Suicidal Ideation, Systematic Review
Borderline personality disorder (BPD) constitutes a serious health problem due to the severity of symptoms, the presence of comorbidities, and the recurrence of treatment dropouts, which have a significant impact on the overall functioning of the person, complicating the work of multidisciplinary teams and the management of health services (1, 2). Statistical indicators confirm the severity of this health problem, with the global prevalence estimated at 2% in the general population, 3% in adolescents, and 1.5% in adults (3, 4). The range of prevalence is also established at 15% to 28% among hospitalized patients and users of outpatient psychiatric care (5). BPD exhibits a variety of symptoms, including emotional instability, altered self-image, feelings of worthlessness, impulsivity, micropsychotic episodes, fear of abandonment, self-injurious behaviors, and attempts to diminish the self (6, 7). Previous neuroimaging studies have suggested that dysfunction in the prefrontal cortex may contribute to impulsivity and unstable emotional symptoms in patients with BPD (8, 9). The literature shows that about 70% of individuals diagnosed with BPD engage in self-harming behaviors, and the suicide rate in these patients is about 50 times higher than in the general population (3, 10). Therefore, this disorder is associated with a high disease burden for the individual, family and society, which doubles the need for effective treatment (11). In this regard, the role of psychotherapy as a fundamental tool for the treatment of BPD is valued (12). While the paradigms of classical and operant conditioning in the 1950s and cognitive-behavioral therapy in the 1970s were established as the first and second generation therapies, respectively, Dialectical Behavior Therapy (DBT) belongs to the third-generation therapies; this third generation also includes acceptance and commitment models, behavioral activation, and mindfulness-based stress reduction (13).
DBT is one of the programs that provides promising results in the treatment of BPD because it integrates the tools of individual format, development of interpersonal skills, telephone calls in crisis and periodic monitoring sessions; in addition, DBT incorporates elements from cognitive and behavioral approaches, while also employing dialectical philosophical approaches for the acceptance of suffering (14). DBT follows a biosocial model that conceives BPD as a disorder of the emotion regulation system that activates a behavioral pattern of instability as a coping mechanism and proposes four guiding skills as its fundamental learning goal: awareness, interpersonal effectiveness, emotion regulation, and discomfort tolerance (15). The therapeutic benefits of DBT are supported by empirical evidence and research which support its effectiveness in reducing self-injurious behaviors, self-harm attempts, suicidal thoughts, as well as behaviors associated with depression or bulimia nervosa (16, 17). However, the broad clinical spectrum and the variables involved in the treatment process for BPD (e.g., the quality of the therapeutic relationship, pharmacological adherence, comorbidities, dropout or dropout rates, among others), necessitate a thorough analysis of the DBT program to identify the value of its components and its therapeutic contribution in the recovery of people who present such diagnosis. Previously, some systematic reviews and meta-analyses have been published on this topic, two of which date back to 2010 and 2014 (18, 19). Considering the publication of several original articles after 2014, it seems necessary to review the latest scientific evidence to investigate the effects of DBT on BPD. Oud et al. systematically reviewed all psychotherapies for adults with BPD, and the lack of focus on DBT made this study a non-exhaustive review of the effects of various aspects of DBT on BPD (20). On the other hand, another meta-analysis study evaluated only some limited outcomes of this type of treatment on BPD (21). Therefore, at present, scientific production on the subject is both scarce and dispersed; thus, in the current context of momentum, as well as the development of new therapeutic approaches, it is important to systematize the clinical evidence of DBT for its potential contribution in the clinical improvement of people with BPD.
Materials and Methods
This is a systematic review based on PRISMA guideline that compiles the scientific evidence on the efficacy of DBT in people with BPD. In order to meet the objective, a search of the existing literature was carried out in the main databases including Scopus, Web of Science, and PubMed. English descriptors were used for borderline personality disorder (BPD), dialectical behavior therapy (DBT), and experimental design (RCT), with adjustments made for searching in the title, abstract and keywords for Scopus and Web of Science. For PubMed, the search included the title, abstract and mesh words. The search strategies were endorsed by a specialized consultant. The inclusion criteria were articles published between January 2000 and June 2023 in English that applied an experimental design with a control group and a random assignment. In addition, the original articles had to include people with the diagnosis of BPD, aged 18 years or older.
Of the articles found after applying the exclusion and inclusion criteria and after eliminating duplicate articles, quasi-experimental, non-randomized, empirical studies and those that were outside the time range, the final sample consisted of 18 papers for analysis. This process was done by screening the title and abstract of the citations and evaluating the full text independently by two experts. To help limit bias in this review and in the interpretation of findings, two experts evaluated the quality of eligible studies through Consolidated Standards of Reporting Trials (CONSORT) checklist (22). This checklist has 25 items related to methodology, findings, and discussion (23-25). Each item in CONSORT has 1 score, and therefore, each study received a total quality score based on this checklist, and any original study whose quality score was less than 12 was excluded from our study. Data extraction from eligible studies was then performed by creating a data sheet in Excel containing columns for authors, publication date, country, number of participants, mean age, sex, DBT protocol, outcome measures, assessment times, and main findings.
Results
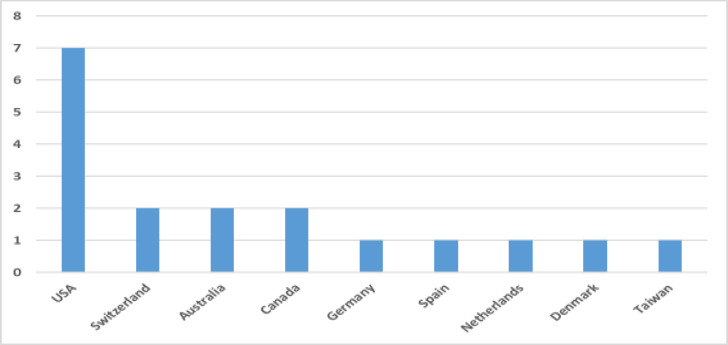
The process of searching online scientific databases made it possible to find 673 articles in Scopus, 586 in Web of Science, and 370 in PubMed (N = 1629 in total). From these articles, pseudo-experimental, non-randomized, experimental and those conducted outside the search period (N = 1611) were excluded, leaving the sample comprising several RCTs (n = 18) (26-43) that met the criteria set forth in the present research (Figure 1). Some studies contained repeated trials with the same study population and were therefore excluded from the current study. Since all studies received a minimum score of 12 in the quality assessment, all 18 studies were included in our review. Most studies described the reasons for dropout and conducted intentional analysis, leading to appropriate data integrity. As shown in Figure 2, most of the eligible studies (7/18) were conducted in the United States. A total of 1,755 individuals participated in these studies, most of whom were women. Table 1 summarizes the details of the selected research on the efficacy of DBT in people with BPD. In all the studies, the participants had a diagnosis of BPD, except for one study in which the participants were BPD patients with post-traumatic stress disorder (36). Only in the study (26), the participants included BPD inpatients, while other studies treated BPD outpatients. The activities have been mainly developed in clinical or healthcare contexts, with the exception of the few studies conducted with students on campus. In the intervention groups, eight studies utilized a short-term DBT protocol (28, 33, 34, 39-43) and the rest utilized standard DBT. In the control groups, six studies utilized usual care (28, 31, 33, 37, 40, 43), and 10 studies utilized non-DBT, such as cognitive processing therapy or community treatment. Linehan et al. compared a standard DBT group with DBT skills training and DBT individual therapy groups (32), and MaMain et al. compared a standard DBT group with a short-term DBT group (34). Regarding the outcome measures, the units of analysis mainly focused on self-injurious behaviors, suicidal thoughts or ideations, the number of visits to emergency services, as well as the frequency of hospitalizations. However, a variety of questionnaires and scales were used to assess the effects of various aspects of DBT on BPD.
Figure 1.
Flow Chart in the Research Selection Process to Review the Effects of Dialectical Behavior Therapy on Borderline Personality Disorder
Figure 2.
Number of Randomized Controlled Trial Studies Assessing the Effects of Dialectical Behavior Therapy on Borderline Personality Disorder
Table 1.
Characteristics of Selected Research on the Efficacy of Dialectical Behavior Therapy (DBT) in Persons with Borderline Personality Disorder (BPD)
| Study (Year; Country) | Participants | Intervention | Outcome Measures | Assessment Times | Main Results |
|---|---|---|---|---|---|
| Clarkin et al. (2007; USA) (26) | 90 inpatients with BPD in three DBT (n = 30), ST (n = 30) and TFP (n = 30) groups; 30.9 ± 7.85 years old; 92.2% female | A weekly individual and group session and available telephone consultation for DBT group for one year | MOAS, AIAQ, BIS-II, BSI, BDI, GAF, SAS | 0, 4, 8, and 12 months with no follow up | Improvement in suicidality. Generally, DBT had no effect or small effect sizes on outcome measures |
| Linehan et al. (2006; USA) (27) | 101 outpatients with BPD in two DBT (n = 52) and CTBE (n = 49) groups; 29.3 ± 7.5 years old; 100% female | A weekly individual and group session and available telephone consultation as well as weekly therapist consultation team meeting for DBT group for one year | SASII, SBQ, RFL, THI, HDRS | 0 and 12 months with one year follow up | Improvements in suicidality, hospitalization, compliance and medical risks with small effect sizes |
| Koons et al. (2001; USA) (28) | 28 outpatients with BPD in two DBT (n = 14) and TAU (n = 14) groups; 34.5 ± 7.5 years old; 100% female | Weekly individual therapy, group session and therapists’ consultation meeting for six months | PSI, SSI, BHS, BDI, HDRS, HARS, DES, THI | 0, 3 and 6 months with no follow up | Improvement in suicidality, hopelessness, depression, dissociation and anger with large effect sizes. Improvement in BPD main symptoms with a moderate effect size |
| Linehan et al. (2002; USA) (29) | 23 outpatients with BPD and opiate dependence in two DBT (n = 11) and CVT (n = 12) groups; 36.1 ± 7.3 years old; 100% female | A weekly individual and group session and available telephone consultation as well as weekly therapist consultation team meeting for DBT group for one year | Urinalysis, TLFB, PHI, SAS, GAS, GAF, BSI | 0, 4, 8 and 12 months with four months follow up | Improvement in all measures with small effect sizes |
| McMain et al. (2009; Canada) (30) | 180 outpatients with BPD in two DBT (n = 90) and GPM (n = 90) groups; 29.4 ± 9.1 years old; 90% female | Individual sessions (1 hour weekly); skills group (2 hours weekly); phone coaching (2 hours weekly); Consultation team for therapists mandated (2 hours weekly) for one year | SASII, ZAN-BPD, SCL-90-R, STAXI, BDI, IIP-64, THI, EQ-5D | 0, 4, 8 and 12 months with no follow up | Most outcome measures showed statistically significant improvement, with effect sizes ranging from moderate to large. No significant differences across any outcomes were found between groups. |
| van den Bosch et al. (2005; Netherlands) (31) | 58 outpatients with BPD in two DBT (n = 27) and TAU (n = 31) groups; 34.9 ± 7.7 years old; 100% female | Weekly individual and skills training groups as well as weekly supervision and consultation meetings for the therapists for one year | BPDSI, LPC | 0 and 12 months with six months follow up | Improvement in suicidality and impulsive behaviors post-intervention and at follow up |
| Linehan et al. (2015; USA) (32) | 99 patients with BPD in three standard DBT (n = 33), DBT skills training (n = 33) and DBT individual therapy (n = 33) groups; 30.3 ± 8.9 years old; 100% female | A weekly individual therapy, group skills training, therapist consultation team, and as-needed between-session telephone coaching for one year | SASII, SBQ, RFL, THI, HDRS, HARS | 0 and 12 months with one year follow up | All treatment conditions resulted in similar improvements in the frequency and severity of suicide attempts, suicide ideation, use of crisis services due to suicidality, and reasons for living |
| Pistorello et al. (2012; USA) (33) | 63 outpatients with BPD in two DBT (n = 31) and TAU (n = 32) groups; 20.86 ± 1.92 years old; 81% female | A weekly individual therapy, group skills training, therapist consultation team, and as-needed between-session telephone coaching for 7-12 months | SCID-II, SASII, BDI-II, SBQ, SAS-SR, GAF | 0, 3, 6, 9, and 12 months with six months follow up | Significant improvements in depression, suicidality, BPD criteria, number of NSSI events and social adjustment post-treatment and at follow up |
| McMain et al. (2022; Canada) (34) | 240 outpatients with BPD in two groups for receiving 6 (n = 120) or 12 (n = 120) months of DBT; 28.27 ± 8.62 years old; 79% female | Weekly individual therapy sessions, weekly DBT skills training group sessions, telephone consultation as needed, and weekly therapist consultation team meetings for 6 or 12 months | SASII, BDI-II, IIP-64, STAXI, SCL-90-R | 0, 3, 6, 9, 12 months with one year follow up | Six months treatment led to significant improvements in suicidality, general psychopathology and BPD symptoms |
| Keefe et al. (2021; USA) (35) | 156 patients with BPD in two DBT (n = 78) and GPM (n = 78) groups; 18-60 years old; 86.1% female | Weekly group and individual sessions for a combined total of 3-h plus 1-h of optional phone coaching for one year | GSI, ZAN-BPD, SCL-90-R, BDI-II, STAXI, IIP-64, CTQ | 0 and 12 months with 6-month, 12-month, 18-month and 24-month follow up | Significant improvements in suicidality and BPD symptoms after DBT treatment and at follow ups |
| Bohus et al. (2020; Germany) (36) | 193 outpatients with BPD + PTSD in two DBT (n = 98) and CPT groups (n = 95); 36.3 ± 11.1 years old; 100% female | One-on-one outpatient treatment with a maximum of 45 sessions of 50 minutes each for one year | CAPS-5, GAF, BSL-23, BDI-II, DTS, SCL-90-R | 0, 3, 6, 9 and 12 months with three months follow up | Significant improvements in BPD symptoms |
| Euler et al. (2019; Switzerland) (37) | 31 outpatients with BPD in two DBT (n = 16) and TAU (n = 15) groups; 34.5 ± 9.6 years old; 87% female | 20 weekly 90-min group sessions | DMRS, OQ-45.2, BSL-23 | Before and after treatment | Significant improvement in overall defense function |
| Walton et al. (2020; Australia) (38) | 162 outpatients with BPD in two DBT (n = 81) and CM (n = 81) groups; 18-65 years old; 77% female | Weekly individual therapy, weekly group skills training and having access to after-hours phone coaching for 14 months | SASII, BDI-II, BPDSI, IIP-64, DES, SSI, KIMS, DERS | 0, 7 and 14 months with no follow up | Significant improvements in suicidality and depressive symptoms |
| Lin et al. (2019; Taiwan) (39) | 82 outpatients with BPD in two DBT (n = 42) and CPT (n = 40) groups; 20.4 ± 0.76 years old; 38% female | A weekly training group for 120 min each time for eight weeks | CMSADS-L, BPDFS, KDI, ASIQ-S, CEQ-S, ERS | 0, 4 and 8 weeks with six months follow up | Significant improvements in suicidality, depression and suppression symptoms |
| Carter et al. (2010; Australia) (40) | 70 outpatients with BPD in two DBT (n = 37) and TAU (n = 33) groups; 24.5 ± 6.1 years old; 100% female | A weekly individual therapy, group skills training, therapist consultation team, and as-needed between-session telephone coaching for six months | IPDEQ, BDQ, PHI-2, WHOQOL-BREF | 0 and 6 months with six months follow up | Non-significant improvements in some BPD symptoms |
| Andreasson et al. (2016; Denmark) (41) | 108 outpatients in two DBT (n = 57) and CAMS (n = 51) groups; 31.69 ± 12.7 years old; 74.1% female | Weekly individual therapy, skills training in groups, access to telephone coaching with therapists, and supervision and consultations for the team of therapists for 16 weeks | ZAN-BPD, HDRS, BDI-II, BHS, RSE | 0 and 17 weeks with nine months follow up | No significant improvement in suicidality and BPD symptoms |
| Soler et al. (2009; Spain) (42) | 30 outpatients in two DBT (n = 19) and SGT (n = 11) groups; 29.1 ± 6.1 years old; 54% female | A weekly individual therapy, group skills training, therapist consultation team, and as-needed between-session telephone coaching for 13 weeks | CGI-BPD, HDRS, HARS, BPRS, SCL-90-R, BDI, BIS | 0, 2, 4, 6, 8, 10 and 13 weeks without follow up | Significant improvements in depression, irritability, anger, anxiety, mood instability and general psychiatric symptoms |
| Kramer et al. (2016; Switzerland) (43) | 41 outpatients in two DBT (n = 21) and TAU (n = 20) groups; 34.4 ± 9.1 years old; 88% female | 20 weekly DBT skills group training sessions | OQ-45.2 | Before and after treatment | Significant improvement in BPD symptoms |
BPD = borderline personality disorder; DBT = dialectical behavior therapy; ST = supportive treatment; TFP = transference-focused psychotherapy; MOAS = modified overt aggression scale; AIAQ = anger, irritability, and assault questionnaire; BIS-II = Barratt impulsive scale-II; BSI = brief symptom inventory; BDI = Beck depression inventory; GAF = global assessment of functioning scale; SAS = social adjustment scale; CTBE = community treatment by experts; SASII = suicide attempt self-injury interview; SBQ = suicidal behaviors questionnaire; RFL = reasons for living inventory; THI = treatment history interview; HDRS = Hamilton depression rating scale; TAU = treatment as usual; PHI = parasuicide history interview; SSI = Beck scale for suicide ideation; BHS = Beck hopelessness scale; CVT = comprehensive validation therapy; CM = conversational model; HARS = Hamilton anxiety rating scale; DES = dissociative experiences scale; TLFB = timeline follow-back; GAS = global adjustment scale; GPM = general psychiatric management; ZAN-BPD = Zanarini rating scale for BPD; SCL-90-R = symptom checklist–90–revised; STAXI = state-trait anger expression inventory; IIP-64 = inventory of interpersonal problems, 64-item version; EQ-5D = EuroQol 5 Dimension; BPDSI = BPD severity index; LPC = lifetime parasuicide count; CTQ = childhood trauma questionnaire; PTSD = posttraumatic stress disorder; CPT = cognitive processing therapy; CAPS-5 = clinician-administered PTSD scale; BSL-23 = borderline symptom list (short version); DTS = dissociation tension scale; DMRS = defense mechanism rating scale; OQ-45.2 = outcome questionnaire; KIMS = Kentucky inventory of mindfulness skills; DERS = difficulties in emotion regulation scale; CMSADS-L = Chinese version of the modified schedule of affective disorders and schizophrenia-lifetime; BPDFS = BPD features scale; KDI = Ko’s depression inventory; CAMS = collaborative assessment and management of suicidality treatment; ASIQ-S = adult suicidal ideation questionnaire-shortened version; CEQ-S: cognitive error questionnaire-shortened version; ERS = emotion regulation scale; IPDEQ = international personality disorder examination questionnaire; BDQ = brief disability questionnaire; WHOQOL-BREF = world health organization quality of life-BREF version; RSE = Rosenberg self-esteem scale; SGT = standard group therapy; CGI-BPD = clinical global impression-BPD; BPRS = brief psychiatric rating scale.
Among the RCTs reviewed, six studies (26, 28, 30, 37, 38, 43) had no follow-up to assess post-DBT effects on patients, and the remaining 12 studies had a follow-up of 3 to 24 months. Most trials reported small to moderate effect sizes of DBT on BPD. McMinn et al. reported moderate to large effect sizes for DBT on BPD symptoms (30). However, two studies failed to observe a significant improvement in BPD symptoms after DBT treatment (40, 41). The most effective area of DBT was on self-harm and suicidal behavior of BPD patients. Indeed, most studies found that both short-term DBT and standard DBT improved suicidality in BPD patients with small or moderate effect sizes, lasting up to 24 months after the treatment period. Linehan et al. even demonstrated that DBT individual therapy can significantly improve suicidal behaviors in these patients (32). Furthermore, these studies indicated that DBT can significantly improve general psychopathology and depressive symptoms in patients with BPD. However, some studies reported that DBT was not superior to other active psychological interventions such as general psychiatric management (30). Improvement of compliance, impulsivity, and mood instability, as well as reduction of hospitalization rate are other findings observed in the trials applying DBT.
Discussion
In this review, we systematically searched for evidence on the efficacy of DBT for BPD. A total of 18 RCTs were reviewed in this study. In general, the findings of these studies support the effectiveness of DBT for patients with BPD. Our systematic review found that DBT alleviates suicidality and self-injurious behaviors in BPD patients, which is consistent with previous reviews (18-21). Self-injurious behaviors in BPD constitute an important concern. Different mechanisms of change have been mentioned by these studies to elucidate the DBT effects on BPD symptoms. Some studies have suggested that improvements in behavioral control and emotion regulation are associated with better outcomes in patients with BPD (34, 43). BPD may be considered an emotion regulation disorder, and these RCTs studying it, either indirectly or in combination with other factors, are a good indication that improvements in emotion regulation are part of the answer to how DBT reduces BPD symptoms. However, it should be noted that improvement in emotion regulation is more of an outcome rather than a therapeutic approach or tool. In addition, the use of therapeutic modality skills and skills training may play an essential role in the BPD treatment outcomes through DBT. Linehan et al. showed that DBT skills training was more effective in improving self-injurious behaviors compared to DBT individual therapy without skills training (32). Latest evidence has supported the mediating role of DBT skills training in the relationship between baseline level of predictors such as emotion regulation difficulties and outcomes such as self-harm and BPD symptoms (44, 45). Overall, improvements in mindfulness skills, particularly nonjudgmental acceptance, appear to have a substantial effect on various treatment outcomes in BPD patients receiving DBT. This effect may result from the fact that nonjudgmental acceptance helps people cope with feelings of shame and diminishes the inclination to judge and then act to avoid symptomatic manifestations such as self-harm (46).
On the other hand, mindfulness skills, as one of the main four skills training modalities in DBT, help people develop positive physical and emotional responses to stressful situations that improve their depressed mood (47). This is consistent with our findings that DBT can improve depressive symptoms in patients with BPD. In addition, the therapeutic alliance as an interpersonal factor may be another mechanism of change in BPD symptoms in patients receiving DBT. Linehan et al. indicated that treatment approaches that foster a more favorable therapeutic relationship are associated with better suicidality outcomes (29). However, some studies do not agree that the therapeutic alliance is a mechanism of change in DBT (44). From a public health perspective, DBT helps improve the person’s quality of life with BPD and strengthens the management of mental health professional teams. Two forms of DBT (i.e., individual and group therapy) promote the development of psychosocial and motivational skills that help promote adaptive and functional behaviors (32). Meanwhile, the neural correlates of BPD and its changes during the course of DBT cannot be ignored. Indeed, it is reasonable to expect that changes in the neural networks of the brain involved in emotion regulation will finally be necessary for treatment change in DBT. In this regard, several studies have reported neurophysiological changes such as reduced activity of the amygdala and other brain areas involved in emotion regulation in BPD patients after DBT treatment (48, 49). However, these studies provide preliminary evidence that needs to be replicated and confirmed in future studies.
A point to be noted here is the existence of heterogeneity between the reviewed studies. In relation to the selection of the sample, the sociodemographic and clinical characteristics of the participants were heterogeneous among the studies. Although the activities were mainly developed in clinical or healthcare contexts, some trials were conducted on students in university campuses. One study recruited participants from inpatients, while the other studies recruited participants from outpatients. Furthermore, the gender composition varied widely among studies, from trials with only female patients to trials with 38% female participants. The selection of the sample size, the characteristics of the interventions applied to the control group, the difficulty in establishing equivalent comparison criteria between the different subcomponents of the therapeutic programs are also questionable.
Future Directions
Generally, the methodological quality of the eligible RCTs was moderate. Therefore, high-quality RCTs are required on this topic for future research. All trials so far have been conducted on adult patients, and the vast majority of subjects are women. Therefore, further studies are needed to elucidate the effects of age and gender variables on the mechanisms of DBT change. In addition to designing protocols to compare the therapeutic efficacy of DBT on the basis of a homogeneous methodological framework that evaluates the contribution of each subprogram in the clinical improvement of BPD, the major challenge for further research will be the possibility of efficiently implementing this therapeutic approach to local care contexts.
Limitation
Lack of access to other scientific databases (such as PsycInfo and ProQuest) limited our search to retrieve all related articles. In addition, the heterogeneity of scales and instruments measuring outcomes in original studies made the meta-analysis very difficult. Therefore, the lack of meta-analysis is one of the important limitations of this study. On the other hand, the strength of our study is to include only experimental studies with an RCT design, which contributes to the scientific quality of the present research.
Conclusion
DBT promotes the formation of psychosocial and motivational skills. It employs evaluation protocols, individual and group therapy, telephone contact, and follow-up, with strategies based on a proposal for change within the context of the dialectical acceptance of reality. DBT provides an optimal therapeutic response in the reduction of self-injurious behaviors, suicidal thoughts and attempts, the frequency of emergency care and hospitalizations in BPD, which constitutes a valuable contribution from a public health perspective. The challenge for further research will be to design protocols that compare the efficacy of DBT on the basis of a homogeneous methodological framework that evaluates the contribution of each subprogram in the clinical improvement of BPD and to efficiently implement its application to local care contexts.
Acknowledgment
The authors thank the institutions where they work for encouraging the development of research.
Conflict of Interest
None.
References
- 1.Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Primers. 2018;4:18029. doi: 10.1038/nrdp.2018.29. [DOI] [PubMed] [Google Scholar]
- 2.Akbari V, Rahmatinejad P, Mohammadi SD. Comparing Neurocognitive Profile of Patients with Borderline Personality and Bipolar-II Disorders. Iran J Psychiatry. 2019;14(2):113–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Reichl C, Kaess M. Self-harm in the context of borderline personality disorder. Curr Opin Psychol. 2021;37:139–44. doi: 10.1016/j.copsyc.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Mohammadi MR, Shamohammadi M, Salmanian M. The prevalence of borderline personality symptoms in adolescents. Iran J Psychiatry. 2014;9(3):147–51. [PMC free article] [PubMed] [Google Scholar]
- 5.Ellison WD, Rosenstein LK, Morgan TA, Zimmerman M. Community and Clinical Epidemiology of Borderline Personality Disorder. Psychiatr Clin North Am. 2018;41(4):561–73. doi: 10.1016/j.psc.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Gratz KL, Kiel EJ, Mann AJD, Tull MT. The prospective relation between borderline personality disorder symptoms and suicide risk: The mediating roles of emotion regulation difficulties and perceived burdensomeness. J Affect Disord. 2022;313:186–95. doi: 10.1016/j.jad.2022.06.066. [DOI] [PubMed] [Google Scholar]
- 7.Zashchirinskaia O, Isagulova E. Childhood Trauma as a Risk Factor for High Risk Behaviors in Adolescents with Borderline Personality Disorder. Iran J Psychiatry. 2023;18(1):65–71. doi: 10.18502/ijps.v18i1.11414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Husain SF, Tang TB, Tam WW, Tran BX, Ho CS, Ho RC. Cortical haemodynamic response during the verbal fluency task in patients with bipolar disorder and borderline personality disorder: a preliminary functional near-infrared spectroscopy study. BMC Psychiatry. 2021;21(1):201. doi: 10.1186/s12888-021-03195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruocco AC, Rodrigo AH, McMain SF, Page-Gould E, Ayaz H, Links PS. Predicting Treatment Outcomes from Prefrontal Cortex Activation for Self-Harming Patients with Borderline Personality Disorder: A Preliminary Study. Front Hum Neurosci. 2016;10:220. doi: 10.3389/fnhum.2016.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lieslehto J, Tiihonen J, Lähteenvuo M, Mittendorfer-Rutz E, Tanskanen A, Taipale H. Comparative Effectiveness of Pharmacotherapies for the Risk of Attempted or Completed Suicide Among Persons With Borderline Personality Disorder. JAMA Netw Open. 2023;6(6):e2317130. doi: 10.1001/jamanetworkopen.2023.17130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bailey RC, Grenyer BF. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–58. doi: 10.1097/HRP.0b013e3182a75c2c. [DOI] [PubMed] [Google Scholar]
- 12.McLenan J, Lazzari C, McMillan G, Mackie R. Psychopathology of the General Population Referred by Primary Care Physicians for Urgent Assessment in Psychiatric Hospitals. Iran J Psychiatry. 2016;11(4):201–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Rabiee N, Nazari AM, Keramat A, Khosravi A, Bolbol-Haghighi N. The Effectiveness of Dialectical Behavioral Therapy on the Success of Breast Feeding in Traumatic Childbirth: A Randomized Controlled Trial. Iran J Psychiatry. 2022;17(2):118–26. doi: 10.18502/ijps.v17i2.8901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linehan MM, Wilks CR. The Course and Evolution of Dialectical Behavior Therapy. Am J Psychother. 2015;69(2):97–110. doi: 10.1176/appi.psychotherapy.2015.69.2.97. [DOI] [PubMed] [Google Scholar]
- 15.Gillespie C, Murphy M, Joyce M. Dialectical Behavior Therapy for Individuals With Borderline Personality Disorder: A Systematic Review of Outcomes After One Year of Follow-Up. J Pers Disord. 2022;36(4):431–54. doi: 10.1521/pedi.2022.36.4.431. [DOI] [PubMed] [Google Scholar]
- 16.Barnicot K, Redknap C, Coath F, Hommel J, Couldrey L, Crawford M. Patient experiences of therapy for borderline personality disorder: Commonalities and differences between dialectical behaviour therapy and mentalization-based therapy and relation to outcomes. Psychol Psychother. 2022;95(1):212–33. doi: 10.1111/papt.12362. [DOI] [PubMed] [Google Scholar]
- 17.Lakeman R, Crighton J. The Impact of Social Distancing on People with Borderline Personality Disorder: The Views of Dialectical Behavioural Therapists. Issues Ment Health Nurs. 2021;42(5):410–6. doi: 10.1080/01612840.2020.1817208. [DOI] [PubMed] [Google Scholar]
- 18.Kliem S, Kröger C, Kosfelder J. Dialectical behavior therapy for borderline personality disorder: a meta-analysis using mixed-effects modeling. J Consult Clin Psychol. 2010;78(6):936–51. doi: 10.1037/a0021015. [DOI] [PubMed] [Google Scholar]
- 19.Panos PT, Jackson JW, Hasan O, Panos A. Meta-Analysis and Systematic Review Assessing the Efficacy of Dialectical Behavior Therapy (DBT) Res Soc Work Pract. 2014;24(2):213–23. doi: 10.1177/1049731513503047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oud M, Arntz A, Hermens ML, Verhoef R, Kendall T. Specialized psychotherapies for adults with borderline personality disorder: A systematic review and meta-analysis. Aust N Z J Psychiatry. 2018;52(10):949–61. doi: 10.1177/0004867418791257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen SY, Cheng Y, Zhao WW, Zhang YH. Effects of dialectical behaviour therapy on reducing self-harming behaviours and negative emotions in patients with borderline personality disorder: A meta-analysis. J Psychiatr Ment Health Nurs. 2021;28(6):1128–39. doi: 10.1111/jpm.12797. [DOI] [PubMed] [Google Scholar]
- 22.Khaleghi A, Zarafshan H, Vand SR, Mohammadi MR. Effects of Non-invasive Neurostimulation on Autism Spectrum Disorder: A Systematic Review. Clin Psychopharmacol Neurosci. 2020;18(4):527–52. doi: 10.9758/cpn.2020.18.4.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mostafavi SA, Khaleghi A, Mohammadi MR, Akhondzadeh S. Is transcranial direct current stimulation an effective modality in reducing food craving? A systematic review and meta-analysis. Nutr Neurosci. 2020;23(1):55–67. doi: 10.1080/1028415X.2018.1470371. [DOI] [PubMed] [Google Scholar]
- 24.Mostafavi SA, Khaleghi A, Mohammadi MR. Noninvasive brain stimulation in alcohol craving: A systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2020;101:109938. doi: 10.1016/j.pnpbp.2020.109938. [DOI] [PubMed] [Google Scholar]
- 25.Khaleghi A, Pirzad Jahromi G, Zarafshan H, Mostafavi SA, Mohammadi MR. Effects of transcranial direct current stimulation of prefrontal cortex on risk-taking behavior. Psychiatry Clin Neurosci. 2020;74(9):455–65. doi: 10.1111/pcn.13025. [DOI] [PubMed] [Google Scholar]
- 26.Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry. 2007;164(6):922–8. doi: 10.1176/ajp.2007.164.6.922. [DOI] [PubMed] [Google Scholar]
- 27.Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–66. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- 28.Koons CR, Robins CJ, Tweed JL, Lynch TR, Gonzalez AM, Morse JQ, et al. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behav Ther. 2001;32(2):371–90. [Google Scholar]
- 29.Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, Kivlahan DR. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67(1):13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- 30.McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, Streiner DL. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am J Psychiatry. 2009;166(12):1365–74. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- 31.van den Bosch LM, Koeter MW, Stijnen T, Verheul R, van den Brink W. Sustained efficacy of dialectical behaviour therapy for borderline personality disorder. Behav Res Ther. 2005;43(9):1231–41. doi: 10.1016/j.brat.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 32.Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA Psychiatry. 2015;72(5):475–82. doi: 10.1001/jamapsychiatry.2014.3039. [DOI] [PubMed] [Google Scholar]
- 33.Pistorello J, Fruzzetti AE, Maclane C, Gallop R, Iverson KM. Dialectical behavior therapy (DBT) applied to college students: a randomized clinical trial. J Consult Clin Psychol. 2012;80(6):982–94. doi: 10.1037/a0029096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McMain SF, Chapman AL, Kuo JR, Dixon-Gordon KL, Guimond TH, Labrish C, et al. The Effectiveness of 6 versus 12 Months of Dialectical Behavior Therapy for Borderline Personality Disorder: A Noninferiority Randomized Clinical Trial. Psychother Psychosom. 2022;91(6):382–97. doi: 10.1159/000525102. [DOI] [PubMed] [Google Scholar]
- 35.Keefe JR, Kim TT, DeRubeis RJ, Streiner DL, Links PS, McMain SF. Treatment selection in borderline personality disorder between dialectical behavior therapy and psychodynamic psychiatric management. Psychol Med. 2021;51(11):1829–37. doi: 10.1017/S0033291720000550. [DOI] [PubMed] [Google Scholar]
- 36.Bohus M, Kleindienst N, Hahn C, Müller-Engelmann M, Ludäscher P, Steil R, et al. Dialectical Behavior Therapy for Posttraumatic Stress Disorder (DBT-PTSD) Compared With Cognitive Processing Therapy (CPT) in Complex Presentations of PTSD in Women Survivors of Childhood Abuse: A Randomized Clinical Trial. JAMA Psychiatry. 2020;77(12):1235–45. doi: 10.1001/jamapsychiatry.2020.2148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Euler S, Stalujanis E, Allenbach G, Kolly S, de Roten Y, Despland JN, Kramer U. Dialectical behavior therapy skills training affects defense mechanisms in borderline personality disorder: An integrative approach of mechanisms in psychotherapy. Psychother Res. 2019;29(8):1074–85. doi: 10.1080/10503307.2018.1497214. [DOI] [PubMed] [Google Scholar]
- 38.Walton CJ, Bendit N, Baker AL, Carter GL, Lewin TJ. A randomised trial of dialectical behaviour therapy and the conversational model for the treatment of borderline personality disorder with recent suicidal and/or non-suicidal self-injury: An effectiveness study in an Australian public mental health service. Aust N Z J Psychiatry. 2020;54(10):1020–34. doi: 10.1177/0004867420931164. [DOI] [PubMed] [Google Scholar]
- 39.Lin TJ, Ko HC, Wu JY, Oei TP, Lane HY, Chen CH. The Effectiveness of Dialectical Behavior Therapy Skills Training Group vs. Cognitive Therapy Group on Reducing Depression and Suicide Attempts for Borderline Personality Disorder in Taiwan. Arch Suicide Res. 2019;23(1):82–99. doi: 10.1080/13811118.2018.1436104. [DOI] [PubMed] [Google Scholar]
- 40.Carter GL, Willcox CH, Lewin TJ, Conrad AM, Bendit N. Hunter DBT project: randomized controlled trial of dialectical behaviour therapy in women with borderline personality disorder. Aust N Z J Psychiatry. 2010;44(2):162–73. doi: 10.3109/00048670903393621. [DOI] [PubMed] [Google Scholar]
- 41.Andreasson K, Krogh J, Wenneberg C, Jessen HK, Krakauer K, Gluud C, et al. EFFECTIVENESS OF DIALECTICAL BEHAVIOR THERAPY VERSUS COLLABORATIVE ASSESSMENT AND MANAGEMENT OF SUICIDALITY TREATMENT FOR REDUCTION OF SELF-HARM IN ADULTS WITH BORDERLINE PERSONALITY TRAITS AND DISORDER-A RANDOMIZED OBSERVER-BLINDED CLINICAL TRIAL. Depress Anxiety. 2016;33(6):520–30. doi: 10.1002/da.22472. [DOI] [PubMed] [Google Scholar]
- 42.Soler J, Pascual JC, Tiana T, Cebrià A, Barrachina J, Campins MJ, et al. Dialectical behaviour therapy skills training compared to standard group therapy in borderline personality disorder: a 3-month randomised controlled clinical trial. Behav Res Ther. 2009;47(5):353–8. doi: 10.1016/j.brat.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 43.Kramer U, Pascual-Leone A, Berthoud L, de Roten Y, Marquet P, Kolly S, et al. Assertive Anger Mediates Effects of Dialectical Behaviour-informed Skills Training for Borderline Personality Disorder: A Randomized Controlled Trial. Clin Psychol Psychother. 2016;23(3):189–202. doi: 10.1002/cpp.1956. [DOI] [PubMed] [Google Scholar]
- 44.Uliaszek AA, Hamdullahpur K, Chugani CD, Tayyab R. Mechanisms of change in group therapy for treatment-seeking university students. Behav Res Ther. 2018;109:10–7. doi: 10.1016/j.brat.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krantz LH, McMain S, Kuo JR. The unique contribution of acceptance without judgment in predicting nonsuicidal self-injury after 20-weeks of dialectical behaviour therapy group skills training. Behav Res Ther. 2018;104:44–50. doi: 10.1016/j.brat.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 46.Mehlum L. Mechanisms of change in dialectical behaviour therapy for people with borderline personality disorder. Curr Opin Psychol. 2021;37:89–93. doi: 10.1016/j.copsyc.2020.08.017. [DOI] [PubMed] [Google Scholar]
- 47.Creswell JD. Mindfulness Interventions. Annu Rev Psychol. 2017;68:491–516. doi: 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- 48.Goodman M, Carpenter D, Tang CY, Goldstein KE, Avedon J, Fernandez N, et al. Dialectical behavior therapy alters emotion regulation and amygdala activity in patients with borderline personality disorder. J Psychiatr Res. 2014;57:108–16. doi: 10.1016/j.jpsychires.2014.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schmitt R, Winter D, Niedtfeld I, Herpertz SC, Schmahl C. Effects of Psychotherapy on Neuronal Correlates of Reappraisal in Female Patients With Borderline Personality Disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2016;1(6):548–57. doi: 10.1016/j.bpsc.2016.07.003. [DOI] [PubMed] [Google Scholar]