Abstract
Introduction:
Initiation of breastfeeding has been associated with reduced post-perinatal infant mortality. Although most states have initiatives to protect, promote, and support breastfeeding, no analysis of the association between breastfeeding and infant mortality has been conducted at the state and regional levels. To understand the associations between breastfeeding and post-perinatal infant mortality, the initiation of breastfeeding with post-perinatal infant mortality was analyzed by geographic region and individual states within each region.
Methods:
This study was a prospective cohort analysis linking U.S. national birth and post-perinatal infant death data for nearly 10 million infants born in 2016–2018, who were then followed for 1 year after birth and analyzed in 2021–2022.
Results:
A total of 9,711,567 live births and 20,632 post-perinatal infant deaths from 48 states and the District of Columbia were included in the analysis. The overall AOR and 95% CIs for breastfeeding initiation with post-perinatal infant mortality was 0.67 (0.65, 0.69, p<0.0001) for days 7–364. All 7 U.S. geographic regions had significant reductions in post-perinatal infant deaths associated with breastfeeding initiation; Mid-Atlantic and Northeast regions had the largest reductions with AOR of 0.56 (95% CI=0.51, 0.61, p<0.001 and 0.50, 0.63, p<0.001, respectively), whereas the Southeast had the smallest reduction with AOR of 0.79 (95% CI=0.75, 0.84, p<0.001). Statistically significant results were noted for 35 individual states for reduction in total post-perinatal infant deaths.
Conclusions:
Although regional and state variation in the magnitude of the association between breastfeeding and infant mortality exists, the consistency of reduced risk, together with existing literature, suggests that breastfeeding promotion and support may be a strategy to reduce infant mortality in the U.S.
INTRODUCTION
The health and well-being of a nation are reflected in its infant mortality rate (IMR), defined as death before the first birthday per 1,000 live births.1 The U.S. continues to have higher infant mortality than other high-income countries around the world.2,3 The 5 leading causes of infant death in the U.S. are congenital anomalies, preterm birth, sudden infant death syndrome, injuries, and maternal complications of pregnancy.4 Within the U.S. population, there are pronounced racial, ethnic, and geographic disparities in infant mortality, with the highest rates among American Indian/Alaska Native (AI/AN) populations.4 In 2020, there were 5.4 infant deaths per 1,000 live births in the U.S. overall, but with a diverging rate of 10.6 per 1,000 for non-Hispanic Black infants compared with 4.5 per 1,000 in non-Hispanic White infants. Geographically, the highest IMRs were found in Southern states.4 Similarly, racial and ethnic disparities were found in breastfeeding rates in the U.S., with 85.3% breastfeeding initiation among non-Hispanic White infants, compared with 74.1% among non-Hispanic Black infants, on the basis of the 2019 birth cohort.5 Geographic disparities also persist, with the lowest breastfeeding initiation rates in much of the Southeastern region, compared with the highest initiation rates in the Northwestern states.5 Disparities by race occur for many outcomes, including both infant mortality and breastfeeding,6 because of a multitude of factors, including social determinants of health.7 It is well accepted that breastfeeding is associated with reduced infant mortality in low- and middle-income countries,8 and several recent U.S. studies have also documented an association of decreased infant mortality with the initiation of breastfeeding.9–11 Accordingly, the inclusion of breastfeeding support as an infant mortality reduction strategy is emerging as an important priority in the U.S.
Breastfeeding is recognized as normative nutrition for infants and is considered a public health imperative with many short- and long-term improved health outcomes for both mother and child, including significant reductions in all-cause infant mortality12–15 and specific protection against sudden infant death syndrome13 and necrotizing enterocolitis in preterm infants.14 The updated American Academy of Pediatrics policy statement on “Breastfeeding and the Use of Human Milk” continues to recommend exclusive breastfeeding for about 6 months, with a continuation of breastfeeding, along with complementary foods, for up to 2 years and beyond,12 in alignment with WHO recommendations.15 The updated American Academy of Pediatrics policy statement on reducing the risk of sleep-related deaths also recommends breastfeeding for at least 1 year and as long thereafter as mutually desirable.16 Despite these recommendations, the rates for both exclusivity and duration of breastfeeding in the U.S. remain low, with only 24.9% of women exclusively breastfeeding at 6 months and only 35.9% continuing with any breastfeeding through 1 year.5 Similar racial, ethnic, and geographic disparities exist in breastfeeding exclusivity and duration.5
Previous U.S. studies examined infant mortality with initiation of breastfeeding, documenting a statistically significant 21% reduced risk for post-neonatal infant death (28–364 days) in a representative 1988 sample,9 a 19% reduced risk in post-perinatal infant death (7–364 days) in a single county cohort of 149,679 live births and 598 deaths from 2004 to 2014,10 and a 26% reduced risk of post-perinatal infant death for almost 3 million infants in the U.S. 2017 birth cohort.11
Although most states advocate breastfeeding promotion, protection, and support activities,17 analysis of the association between breastfeeding and infant mortality has not been conducted at the state and regional levels. To provide data that could support state breastfeeding efforts, the association of breastfeeding with post-perinatal infant mortality by region and state was analyzed for almost 10 million infants born in the U.S. from 2016 to 2018.
METHODS
Study Sample
The National Vital Statistics System, led by the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS), is a census of all live births and deaths in the U.S., derived from the Standard Certificates for Live Birth and Death.18,19 Starting in 2016, all 50 states and the District of Columbia (DC) adopted a 2003 revision of the birth certificate that records breastfeeding initiation, allowing analysis of U.S. national data to examine the impact of breastfeeding on post-perinatal infant death, linking birth and infant death files. National Vital Statistics System birth/death linked data were used to create the cohort of this study that includes infants born in 2016, 2017, or 2018 and post-perinatal infant death data occurring in the same birth year or the following year (up to 1 calendar year after birth).20 Births in California and Michigan were excluded; California did not report breastfeeding data to NCHS, and Michigan collected breastfeeding data inconsistently. Data on births and post-perinatal infant deaths occurring in the other 48 states and DC were used for this analysis.
Measures
Two outcome variables were used for infant deaths: total post-perinatal infant deaths, defined as deaths from 7 to 364 days and early post-perinatal infant deaths, defined as deaths from 7 to 182 days. The main exposure variable, breastfeeding initiation, was collected with the question, Is the infant being breastfed at discharge? and a Yes or No response. NCHS provided detailed guidance to assist in the completion of the facility worksheet for the birth certificate, including instructions that breastfeeding should be determined from medical records on the basis of receipt of any breast milk or colostrum at any time during the period between delivery and hospital discharge.21 Home births and births occurring in free-standing birth centers were included. No data were available regarding the duration or exclusivity of breastfeeding or formula supplementation.
All covariates for factors commonly associated with both breastfeeding and infant mortality were obtained from birth certificates. Maternal characteristics included age; education; race and ethnicity; participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) during pregnancy; smoking during pregnancy; delivery method; and birth plurality. Infant characteristics included gestational age and infant sex. Because of the small amount of missing data on the delivery method (n=3,663) and gestational age (n=4,436), participants missing these 2 covariates were removed from the models to avoid convergence problems. No data were imputed; a separate unknown category was created for missing covariate data.
Statistical Analysis
Cochran–Mantel–Haenszel tests examined the associations between each maternal and infant characteristic and the binary outcomes of breastfeeding initiation (yes/no) and death (yes/no). Multiple logistic regression was used to model both total post-perinatal infant deaths (7–364 days) and early post-perinatal infant deaths (7–182 days) for each region and state. Using regions defined by the U.S. Department of Agriculture’s Food and Nutrition Service, data were categorized into 7 geographic regions (Mid-Atlantic, Midwest, Mountain Plains, Northeast, Southeast, Southwest, Western) and for each state within the region, in alphabetical order.22 SAS, Version 9.4 (Cary, NC), was used for all data analyses in 2021–2022, and results were considered statistically significant at p<0.05. CDC determined that this study was not subject to IRB review because only deidentified secondary data were analyzed.
RESULTS
Among 11,622,400 births from 2016 to 2018, a total of 66,503 infants died before 365 days of life, yielding an IMR of 5.72 per 1,000 live births in the combined cohort (Figure 1). Subsequent exclusion criteria included infants born to mothers who were foreign residents (n=29,313), birth weight <500 grams (n=18,614), death <7 days of life (n=20,770), and death due to malignant neoplasms (n=162) or congenital anomalies (n=5,667), which focused the study on the U.S. birth population and reduced the possibility of reverse causality. After excluding California (1,410,993), Michigan (330,303), and infants with missing breastfeeding data from other states (95,011), the final analytical population included 9,711,567 births from 2016 to 2018, of which 20,632 infants died between 7 and 364 days (Figure 1). Among these post-perinatal infant deaths (7–364 days), 17,240 were in early infancy (7–182 days), and 3,392 were in late infancy (183–364 days).
Figure 1.
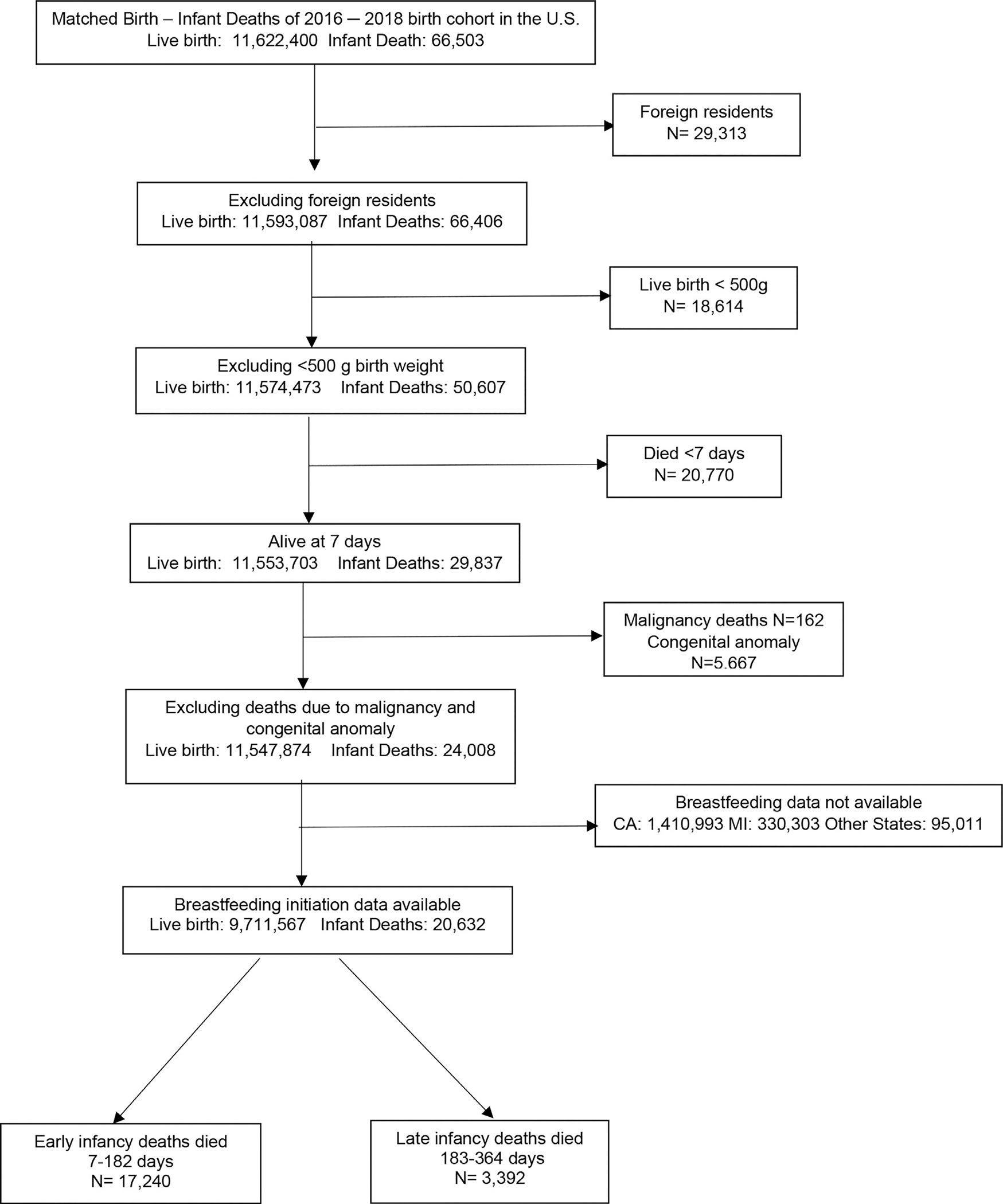
Flow chart of sample size selection for the data analysis.
Table 1 lists the maternal and infant characteristics included in this analysis. Among all live births, 20.6% were born to mothers who were Hispanic, 54.9% were born to mothers who were non-Hispanic White, 15.5% were born to mothers who were non-Hispanic Black, 5.3% were born to mothers who were non-Hispanic Asian, 0.2% were born to mothers who were non-Hispanic Hawaiian/Pacific Islander, and 0.9% were born to mothers who were non-Hispanic AI/AN. Most mothers did not smoke during pregnancy (92.2%), approximately one third had Cesarean delivery (31.9%), and 11.6% were preterm (<37 weeks). Excluded deaths were more likely among infants born to mothers aged >35 years (13% vs 20%), mothers with a college education (14% vs 22%), and mothers of Hispanic origin (15% vs 24%) than included deaths (data not shown).
Table 1.
National Prevalence of Breastfeeding Initiation and Infant Death Among Live Births in 2016–2018, U.S.
| Characteristics | Total live births n (%) | Total postperinatal infant death (7–364 days) n (%) | Breastfeeding initiation rate % | Total postperinatal death rate per 1,000 birth (7–364 days) | Early infancy death rate per 1,000 birth (7–182 days) |
|---|---|---|---|---|---|
|
| |||||
| Overall | 9,711,567 (100) | 20,632 (100) | 83.6 | 2.12 | 1.78 |
| Maternal characteristics | |||||
| Age | |||||
| <20 years | 507,437 (5.2) | 1,966 (9.5) | 72.7 | 3.87 | 3.21 |
| 20–24 years | 1,965,749 (20.2) | 5,995 (29.1) | 78.2 | 3.05 | 2.51 |
| 25–29 years | 2,853,821(29.4) | 5,902 (28.6) | 83.5 | 2.07 | 1.73 |
| 30–34 years | 2,737,146 (28.2) | 4,196 (20.3) | 87.4 | 1.53 | 1.31 |
| ≥35 years | 1,647,414 (17.0) | 2,573 (12.5) | 87.1 | 1.56 | 1.32 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Education | |||||
| Lower than high school | 1,277,447 (13.2) | 4,388 (21.3) | 72.5 | 3.43 | 2.84 |
| High school | 2,459,089 (25.3) | 7,305 (35.4) | 75.4 | 2.97 | 2.46 |
| Some college | 2,776,543 (28.6) | 5,854 (28.4) | 84.7 | 2.11 | 1.79 |
| College graduates | 3,131,297 (32.2) | 2,863 (13.9) | 93.6 | 0.91 | 0.77 |
| Missing | 67,191 (0.7) | 222 (1.1) | 76.7 | 3.30 | 2.78 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Race/ethnicity | |||||
| Hispanic | 1,997,844 (20.6) | 3,153 (15.3) | 87.5 | 1.58 | 1.31 |
| Non-Hispanic White | 5,329,100 (54.9) | 9,529 (46.2) | 84.8 | 1.79 | 1.51 |
| Non-Hispanic Black | 1,509,627 (15.5) | 6,145 (29.8) | 72.0 | 4.07 | 3.39 |
| Non-Hispanic Asian | 511,460 (5.3) | 569 (2.8) | 91.1 | 1.11 | 0.90 |
| Non-Hispanic Hawaiian/Pacific Islander | 22,200 (0.2) | 94 (0.5) | 81.5 | 4.23 | 3.42 |
| Non-Hispanic American Indian/Alaska Native | 83,861 (0.9) | 365 (1.8) | 75.3 | 4.35 | 3.40 |
| 2 or more races | 201,922 (2.1) | 645 (3.1) | 82.8 | 3.19 | 2.64 |
| Missing | 55,553 (0.6) | 132 (0.6) | 82.6 | 2.38 | 2.03 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| WIC during pregnancy | |||||
| Yes | 3,554,083 (36.6) | 10,180 (49.3) | 76.1 | 2.86 | 2.39 |
| No | 6,042,521 (62.2) | 10,163 (49.3) | 88.0 | 1.68 | 1.41 |
| Missing | 114,963 (1.2) | 289 (1.4) | 79.7 | 2.51 | 2.10 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Smoking during pregnancy | |||||
| Yes | 722,061 (7.4) | 4,102 (19.9) | 60.2 | 5.68 | 4.83 |
| No | 8,949,652 (92.2) | 16,344 (79.2) | 85.5 | 1.83 | 1.52 |
| Missing | 39,854 (0.4) | 186 (0.9) | 70.5 | 4.67 | 3.96 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Delivery | |||||
| C-section | 3,099,224 (31.9) | 9,294 (45.0) | 81.7 | 3.00 | 2.55 |
| Vaginal | 6,608,680 (68.0) | 11,319 (54.9) | 84.4 | 1.71 | 1.41 |
| Missing | 3,663 (0) | 19 (0.1) | 82.1 | 5.19 | 4.37 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Plurality | |||||
| Singleton | 9,385,869 (96.6) | 18,647 (90.4) | 83.7 | 1.99 | 1.65 |
| Multiple | 325,698 (3.4) | 1,985 (9.6) | 78.7 | 6.09 | 5.41 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Infant characteristics | |||||
| Gestational age (weeks) | |||||
| <37 | 1,124,261 (11.6) | 8,964 (43.5) | 75.7 | 7.97 | 7.02 |
| ≥37 | 8,582,870 (88.4) | 11,638 (56.4) | 84.6 | 1.36 | 1.09 |
| Missing | 4,436 (0) | 30 (0.1) | 49.8 | 6.80 | 5.86 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
| Sex | |||||
| Male | 4,964,209 (51.1) | 11,780 (57.1) | 83.5 | 2.37 | 1.98 |
| Female | 4,747,358 (48.9) | 8,852 (42.9) | 83.6 | 1.86 | 1.56 |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
Note: Boldface indicates statistical significance (p<0.001).
C-section, cesarian section; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
The overall post-perinatal IMR among non-Hispanic Black mothers was more than twice that among non-Hispanic White mothers (4.07 vs 1.79 per 1,000 births). Preterm infants also had a much higher post-perinatal IMR than term babies (7.97 vs 1.36 per 1,000 births) (Table 1). The breastfeeding initiation rate among all births was 83.6% and was significantly associated with each maternal and infant factor. Factors associated with higher breastfeeding initiation included older age, college education, non-Hispanic Asian race, non-WIC participants, nonsmoking during pregnancy, vaginal delivery, and singleton pregnancies. All of these subpopulations also had the lowest post-perinatal infant mortality. Live births, post-perinatal infant deaths, and breastfeeding initiation rates by region and state are shown in Table 2. This table shows large geographic variations of both breastfeeding initiation rates and IMRs across the U.S. IMRs are generally higher in the states that had lower breastfeeding rates. Results from multiple logistic regression analysis by region and by state, with adjustment for maternal age, education, race/ethnicity, WIC participation, smoking during pregnancy, delivery method, plurality, gestational age, and infant sex, are shown in Appendix Table 1 (available online).
Table 2.
State Prevalence of Breastfeeding Initiation and Infant Death Among Live Births in 2016–2018, U.S.
| Regions and states | Total live births n (%) | Total postperinatal infant death (7–364 days) n (%) | Breastfeeding initiation rate % | Total postperinatal death rate per 1,000 birth (7–364 days) | Early infancy death rate per 1,000 birth (7–182 days) |
|---|---|---|---|---|---|
|
| |||||
| Mid-Atlantic | 1,323,100 (13.62) | 2,546 (12.34) | 82.3 | 1.92 | 1.63 |
| Delaware | 33,307 (0.34) | 77 (0.37) | 79.5 | 2.31 | 1.92 |
| District of Columbia | 42,515 (0.44) | 112 (0.54) | 86.8 | 2.63 | 2.23 |
| Maryland | 204,564 (2.11) | 412 (2.00) | 84.6 | 2.01 | 1.71 |
| New Jersey | 296,785 (3.06) | 444 (2.15) | 81.0 | 1.50 | 1.29 |
| Pennsylvania | 396,171 (4.08) | 723 (3.50) | 81.6 | 1.82 | 1.54 |
| Virginia | 294,220 (3.03) | 612 (2.97) | 86.3 | 2.08 | 1.74 |
| West Virginia | 55,538 (0.57) | 166 (0.80) | 63.4 | 2.99 | 2.65 |
| Midwest | 1,588,961 (16.36) | 3,416 (16.56) | 80.8 | 2.15 | 1.79 |
| Illinois | 433,635 (4.47) | 860 (4.17) | 81.9 | 1.98 | 1.64 |
| Indiana | 248,012 (2.55) | 617 (2.99) | 82.1 | 2.49 | 2.12 |
| Iowa | 114,478 (1.18) | 211 (1.02) | 82.1 | 1.84 | 1.43 |
| Minnesota | 200,949 (2.07) | 341 (1.65) | 89.1 | 1.70 | 1.44 |
| Ohio | 407,362 (4.19) | 1,004 (4.87) | 74.2 | 2.46 | 2.05 |
| Wisconsin | 184,525 (1.90) | 383 (1.86) | 81.2 | 2.08 | 1.77 |
| Mountain plains | 734,237 (7.56) | 1,516 (7.35) | 85.9 | 2.06 | 1.71 |
| Colorado | 194,799 (2.01) | 296 (1.43) | 91.7 | 1.52 | 1.24 |
| Kansas | 114,546 (1.18) | 217 (1.05) | 89.0 | 1.89 | 1.55 |
| Missouri | 217,254 (2.24) | 522 (2.53) | 79.1 | 2.40 | 2.04 |
| Montana | 35,365 (0.36) | 95 (0.46) | 89.6 | 2.69 | 2.01 |
| North Dakota | 36,861 (0.38) | 63 (0.31) | 82.6 | 1.71 | 1.44 |
| Nebraska | 78,585 (0.81) | 186 (0.90) | 89.2 | 2.37 | 2.02 |
| South Dakota | 37,959 (0.39) | 101 (0.49) | 80.3 | 2.66 | 2.21 |
| Wyoming | 18,868 (0.19) | 36 (0.17) | 83.1 | 1.91 | 1.43 |
| Northeast | 1,123,823 (11.57) | 1,608 (7.79) | 87.2 | 1.43 | 1.19 |
| Connecticut | 104,579 (1.08) | 128 (0.62) | 88.2 | 1.22 | 1.04 |
| Maine | 35,367 (0.36) | 61 (0.30) | 87.5 | 1.72 | 1.58 |
| Massachusetts | 211,931 (2.18) | 226 (1.10) | 87.3 | 1.07 | 0.90 |
| New Hampshire | 36,035 (0.37) | 46 (0.22) | 90.4 | 1.28 | 1.19 |
| New York | 686,702 (7.07) | 1,063 (5.15) | 87.4 | 1.55 | 1.26 |
| Rhode Island | 32,936 (0.34) | 47 (0.23) | 73.0 | 1.43 | 1.12 |
| Vermont | 16,273 (0.17) | 37 (0.18) | 89.5 | 2.27 | 1.90 |
| Southeast | 2,251,231 (23.18) | 5,814 (28.18) | 79.9 | 2.58 | 2.18 |
| Alabama | 170,335 (1.75) | 573 (2.78) | 68.1 | 3.36 | 2.79 |
| Florida | 663,389 (6.83) | 1,450 (7.03) | 86.9 | 2.19 | 1.83 |
| Georgia | 383,014 (3.94) | 1,011 (4.90) | 82.6 | 2.64 | 2.24 |
| Kentucky | 155,637 (1.60) | 357 (1.73) | 70.9 | 2.29 | 1.91 |
| Mississippi | 109,146 (1.12) | 349 (1.69) | 56.1 | 3.20 | 2.74 |
| North Carolina | 363,700 (3.75) | 907 (4.40) | 81.6 | 2.49 | 2.11 |
| South Carolina | 159,428 (1.64) | 401 (1.94) | 77.4 | 2.52 | 2.11 |
| Tennessee | 246,582 (2.54) | 766 (3.71) | 80.5 | 3.11 | 2.66 |
| Southwest | 2,049,463 (21.10) | 4,562 (22.11) | 85.0 | 2.23 | 1.84 |
| Arizona | 243,107 (2.50) | 460 (2.23) | 89.8 | 1.89 | 1.49 |
| Arkansas | 105,843 (1.09) | 348 (1.69) | 71.9 | 3.29 | 2.83 |
| Louisiana | 179,200 (1.85) | 611 (2.96) | 69.6 | 3.41 | 2.80 |
| New Mexico | 66,237 (0.68) | 129 (0.63) | 85.6 | 1.95 | 1.69 |
| Oklahoma | 146,566 (1.51) | 422 (2.05) | 81.7 | 2.88 | 2.33 |
| Texas | 1,159,887 (11.94) | 2,363 (11.45) | 88.0 | 2.04 | 1.70 |
| Utah | 148,623 (1.53) | 229 (1.11) | 84.3 | 1.54 | 1.26 |
| Western | 640,752 (6.60) | 1,170 (5.67) | 92.1 | 1.83 | 1.49 |
| Alaska | 31,132 (0.32) | 77 (0.37) | 92.4 | 2.47 | 1.99 |
| Hawaii | 51,335 (0.53) | 111 (0.54) | 92.7 | 2.16 | 1.89 |
| Idaho | 64,745 (0.67) | 98 (0.47) | 92.6 | 1.51 | 1.22 |
| Nevada | 103,127 (1.06) | 255 (1.24) | 81.7 | 2.47 | 2.06 |
| Oregon | 130,916 (1.35) | 227 (1.10) | 94.7 | 1.73 | 1.41 |
| Washington | 259,497 (2.67) | 402 (1.95) | 94.7 | 1.55 | 1.23 |
The AOR and its 95% CI for the associations between breastfeeding and infant mortality are illustrated in Figure 2A (total post-perinatal death) and 2B (early post-perinatal infant death). For the entire U.S. cohort, breastfeeding initiation and post-perinatal infant mortality had an overall AOR of 0.67 (95% CI=0.65, 0.69, p<0.0001) for days 7–364. All 7 geographic regions showed significant reductions; the Mid-Atlantic and Northeast had the largest reductions with AOR of 0.56 (95% CI=0.51, 0.61 and 95% CI=0.50, 0.63, respectively; p<0.001) for total post-perinatal infant deaths, and the Southeast had the smallest but still significant reduction with AOR of 0.79 (95% CI=0.75, 0.84, p<0.001) for total post-perinatal infant deaths. Similar to regional estimates, the adjusted analysis for each state showed a smaller effect size of breastfeeding after controlling for maternal and infant characteristics. Across the 48 states plus DC, statistically significant results were noted in 35 states for total post-perinatal infant deaths and in 32 states for post-perinatal early infant deaths (p<0.05).
Figure 2.
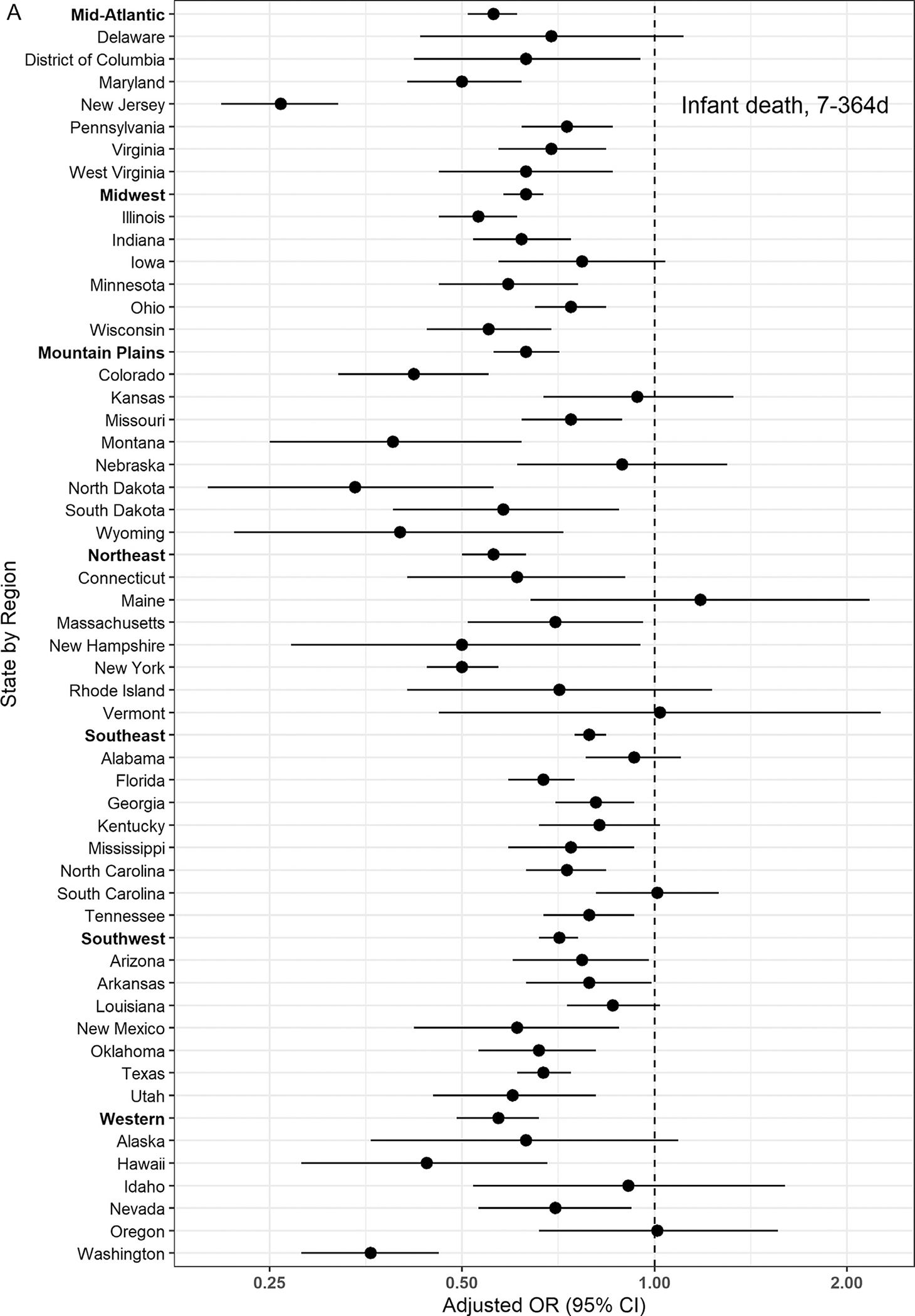
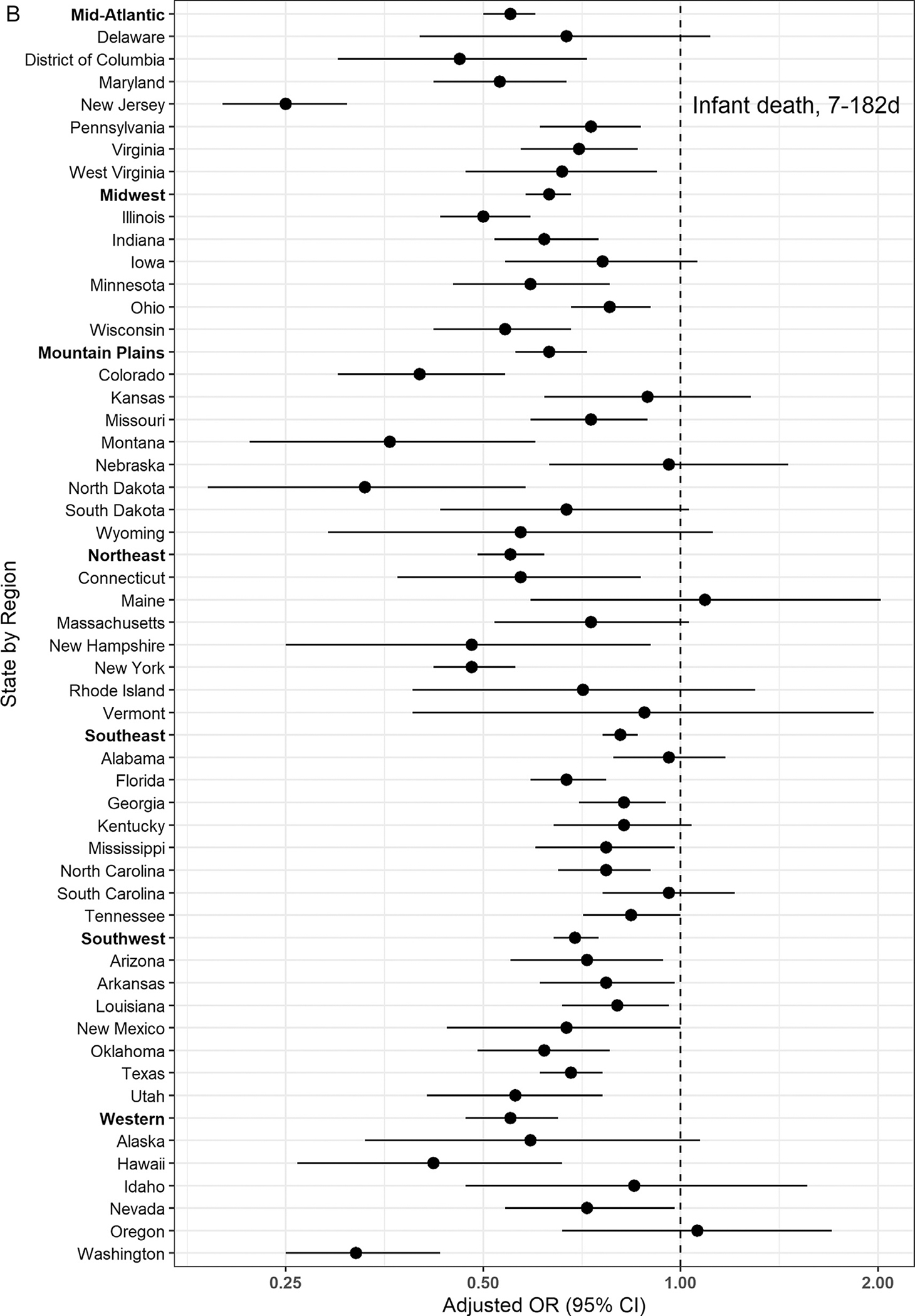
AORs and 95% CIs of breastfeeding initiation and post-perinatal death by region and state in the U.S. (A) Total post-perinatal infant death: infant death from 7 to 364 days. (B) Early post-perinatal infant death: infant death from 7 to 182 days. Adjusted covariates are maternal age, education, race/ethnicity, WIC participation, smoking during pregnancy, delivery method, plurality, gestational age, and infant sex.
WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
DISCUSSION
This study of nearly 10 million U.S. infants reaffirms previous studies documenting the strong association between breastfeeding initiation and reduced post-perinatal infant mortality.9–11 A significant association (AOR=0.67) between breastfeeding and post-perinatal infant mortality for deaths was identified in the first year of life (7–364 days) and early post-perinatal infant deaths (7–182 days) (AOR=0.67). Significant associations were also noted for all 7 U.S. geographic regions, with the largest effect size in the Northeast and Mid-Atlantic (AOR=0.56) and the smallest effect size in the Southeast (AOR=0.79) for post-perinatal infant death. Large geographic variation in the association between breastfeeding initiation and post-perinatal infant death was also found across most of the 48 states and DC, with significant protective associations noted in most states. However, it is important to recognize that this observational study cannot show causation.
This study excluded infants who died at <7 days, to reduce the possibility of reverse causality because these infants may have been too ill to breastfeed and/or receive mother’s milk. This approach is supported by recent research suggesting that specifically for sudden unexpected infant death in the first 7 days of life, there are different risk factors such that the first 7 days should be considered separately in epidemiologic studies.23 Early neonatal death (deaths between 0 and 7 days) continues to be a challenge worldwide, with prematurity and congenital anomalies as the leading causes in high-income countries.24
State IMRs vary widely, and disparities between non-Hispanic Black and non-Hispanic White infants are significant.4 There are also disparities in infant mortality between non-Hispanic White infants and non-Hispanic Native Hawaiian or Pacific Islander and for non-Hispanic AI/AN infants.4 Variations in the non-Hispanic Black–White infant mortality ratio are evident, yet improvements in this gap were reported using 1999–2013 birth–death linked data.25 In addition, there are marked disparities in breastfeeding rates between non-Hispanic Black and non-Hispanic White infants.5
In 2013, former Secretary of Health and Human Services, Kathleen Sebelius, called for the first national strategy to address infant mortality, with 33 mentions of the importance of breastfeeding.26 The committee identified 5 areas of evidenced-based strategies for reducing infant mortality through primary prevention, including breastfeeding. Some states highlight the importance of breastfeeding support in their infant mortality reduction efforts.27–33 The lowest breastfeeding initiation rates (Table 2) were seen in Mississippi, Loss Angeles, West Virginia, Arkansas, Alabama, and Kentucky, overlapping with some of the highest IMRs.4 These observations also align with local data in the recent CDC county breastfeeding initiation map, which identifies low breastfeeding initiation in counties within the Delta and Appalachian regions,34 consistent with published IMR county data.35 These correlations suggest opportunities for breastfeeding promotion, protection, and support to be included as one component in comprehensive infant mortality reduction initiatives across the U.S.
Compared with those of other high-income countries, the U.S. has a relatively high IMR. IMRs in the U.S. are inversely associated with disadvantaged SES, income inequality, and race.36 Race is a social construct, but the systemic or structural disadvantages associated with race contribute to health disparities,37 including IMR and differences in breastfeeding practices.38 Therefore, the impact of race is important to consider. A Black infant is 2.4 times more likely to die before his or her first birthday in the U.S. than a White infant,4 and in certain local regions, such as Shelby County Tennessee, this disparity is even greater.10 Suboptimal breastfeeding is associated with higher infant mortality and may play a role in the 2.2 times number of excess child deaths (95% CI=1.6, 2.8) in the non-Hispanic Black population compared with that in the non-Hispanic White population.6 However, several studies have reported that non-Hispanic Black infants have weaker protective associations between breastfeeding initiation and infant mortality than those of other races as documented in a recent mediation analysis,39 suggesting that competing risks correlated with structural and social disadvantages may somewhat dilute the protective association of breastfeeding in non-Hispanic Black infants.10,11,40 Nevertheless, breastfeeding is associated with a strongly protective effect against infant mortality in all populations. Chiang and colleagues have noted that states with the largest racial/ethnic disparities in breastfeeding initiation generally have lower overall breastfeeding initiation.41 Working to improve breastfeeding in population subgroups with low breastfeeding rates, along with addressing other health inequities with a focus on improved social determinants of health, may save lives in the populations most impacted by high infant mortality.
A notable aspect of this study was the additional analysis of early post-perinatal infant deaths from 7 to 182 days of life, with an AOR (0.67, 33% reduction) in the adjusted analysis identical to the AOR for total post-perinatal infant death (7–364 day) period. Most post-perinatal infant deaths, including sudden unexpected infant deaths, occurred in the first 6 months, which is relevant because only 55.8% of U.S. women are breastfeeding or providing any breastmilk at 6 months, and only 24.9% are exclusively breastfeeding as recommended through 6 months.5 For the 5 states with the highest infant mortality,4 all had <50% provision of any breastmilk at 6 months,5 suggesting that some of the variability in associations between breastfeeding initiation and mortality may be a result of not accounting for breastfeeding duration as well as a number of other factors. Because breastfeeding duration for ≥3 months has been associated with decreased infant mortality,9 the current analysis using only breastfeeding initiation may underrepresent the actual association of breastfeeding on infant mortality.
In this analysis, almost all states have AOR <1.00, and most are statistically significant, as illustrated in Figure 2. For those that are not, the CI is generally very wide, influenced in large measure by the relatively small number of infant deaths in those states. Regional estimates are also more reliable with smaller CIs and can be used for reference. The higher AOR in the Southeastern region, including states where CI crosses 1.00, may be explained by competing risk factors for infant mortality and breastfeeding, including social determinants of health not captured in this analysis such as stress, poverty, structural health inequality, and racism, which have been documented in previous studies.10,39
Strengths of this study include (1) the inclusion of nearly 10 million infants born in the U.S. from 2016 to 2018, (2) a prospective study design with infants followed for an entire year to ascertain a possible outcome of death, and (3) the first study examining regional and state variations on the associations of ever breastfeeding with post-perinatal infant mortality across the U.S.
Limitations
Limitations of this study include the finite number of available characteristics recorded on the birth certificate and the fact that only receipt of any breastmilk before hospital discharge was captured, so the associations of breastfeeding duration or exclusivity could not be examined. In addition, only about 57% of the eligible population participated in WIC,42 which was used as a proxy for poverty. Finally, the lack of information regarding social determinants of health on the birth certificate at the individual level, including economic stability, the neighborhood and built environment, social and community support, access to quality health care, lack of paid maternity leave, and racism, all represents limitations.
CONCLUSIONS
This study of a large cohort of approximately 10 million U.S. infants born during 2016–2018 found a strong association between breastfeeding initiation and reduced post-perinatal infant mortality across all 7 geographic regions and for most individual states. There were geographic variations in these associations ranging from a 44% reduction in odds for overall post-perinatal deaths in the mid-Atlantic and Northeast regions to 21% in the Southeast region. Addressing breastfeeding disparities may improve the health of mothers and their babies and help to reduce adverse outcomes. The consistency of the association between breastfeeding and lower infant mortality supports the inclusion of the promotion, protection, and support of breastfeeding as a strategy for all states and regions in their infant mortality reduction initiatives.
Supplementary Material
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
No funding was secured for this study.
ALM has a research grant from Friesland Campina, a formula ingredients company, and has a minor stake in Glycosyn, LLC & Company, which produces technology for manufacturing oligosaccharides bioidentical to those in human milk. No other financial disclosures were reported.
Footnotes
CREDIT AUTHOR STATEMENT
Julie L. Ware: Conceptualization, Visualization, Methodology, Writing – original draft, Writing – review & editing. Ruowei Li: Conceptualization, Methodology, Data curation, Software, Validation, Formal analysis, Writing – original draft, Writing – review & editing. Aimin Chen: Conceptualization, Methodology, Software, Validation, Formal analysis, Writing – review & editing. Jennifer M. Nelson: Data curation, Writing – review & editing. Jennifer M. Kmet: Methodology, Software, Writing – review & editing. Sharyn E. Parks: Writing – review & editing. Ardythe L. Morrow: Conceptualization, Methodology, Writing – review & editing. Jian Chen: Methodology, Data curation, Software, Validation, Formal analysis, Writing – review & editing. Cria G. Perrine: Conceptualization, Visualization, Data curation, Writing – review & editing.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2023.05.015.
REFERENCES
- 1.Reidpath DD, Allotey P. Infant mortality rate as an indicator of population health. J Epidemiol Community Health. 2003;57(5):344–346. 10.1136/jech.57.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen A, Oster E, Williams H. Why is infant mortality higher in the United States than in Europe? Am Econ J Econ Policy. 2016;8(2):89–124. 10.1257/pol.20140224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Central Intelligence Agency. The world fact book: country comparisons – infant mortality rate. https://www.cia.gov/the-world-factbook/field/infant-mortality-rate. Accessed May 15, 2023.
- 4.Centers for Disease Control and Prevention, Division of Reproductive Health, National Center for Chronic Disease, Health Promotion. Infant mortality. https://www.cdc.gov/reproductivehealth/maternalin-fanthealth. Accessed May 15, 2023.
- 5.Centers for Diseases Control and Prevention. National immunization survey: breastfeeding rates. Atlanta, GA. https://www.cdc.gov/breastfeeding/data/nis_data/data-files/2019/rates-any-exclusive-bf-socio-dem-2019.html. Accessed May 15, 2023. [Google Scholar]
- 6.Bartick MC, Jegier BJ, Green BD, Schwarz EB, Reinhold AG, Stuebe AM. Disparities in breastfeeding: impact on maternal and child health outcomes and costs. J Pediatr. 2017;181:49–55.e6. 10.1016/j.jpeds.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Singh GK, Daus GP, Allender M, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935–2016. Int J MCH AIDS. 2017;6(2):139–164. 10.21106/ijma.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Victora CG, Bahl R, Barros AJ, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387 (10017):475–490. 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 9.Chen A, Rogan WJ. Breastfeeding and the risk of postneonatal death in the United States. Pediatrics. 2004;113(5):e435–e439. 10.1542/peds.113.5.e435. [DOI] [PubMed] [Google Scholar]
- 10.Ware JL, Chen A, Morrow AL, Kmet J. Associations between breast-feeding initiation and infant mortality in an urban population. Breastfeed Med. 2019;14(7):465–474. 10.1089/bfm.2019.0067. [DOI] [PubMed] [Google Scholar]
- 11.Li R, Ware J, Chen A, et al. Breastfeeding and post-perinatal infant deaths in the United States, a national prospective cohort analysis. Lancet Reg Health Am. 2022;5. 10.1016/j.lana.2021.100094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meek JY, Noble L. Section on Breastfeeding [Policy statement]. Policy Statement: Breastfeeding and the Use of Human Milk. Pediatrics. 2022;150(1):e2022057988. 10.1542/peds.2022-057988. [DOI] [PubMed] [Google Scholar]
- 13.Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128(1):103–110. 10.1542/peds.2010-3000. [DOI] [PubMed] [Google Scholar]
- 14.Cacho NT, Parker LA, Neu J. Necrotizing enterocolitis and human milk feeding: A systematic review. Clin Perinatol. 2017;44(1):49–67. 10.1016/j.clp.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Breastfeeding recommendations. https://www.who.int/health-topics/breastfeeding#tab=tab_2. Accessed May 15, 2023.
- 16.Moon RY, Carlin RF, Hand I, TASK FORCE ON SUDDEN INFANTDEATH SYNDROME AND THE COMMITTEE ON FETUS AND NEWBORN. Sleep-related infant deaths: updated 2022 recommendations for reducing infant deaths in the sleep environment. Pediatrics. 2022;150(1):e2022057990. 10.1542/peds.2022-057990. [DOI] [PubMed] [Google Scholar]
- 17.US Breastfeeding Committee, USBC. www.usbreastfeeding.org. Accessed May 15, 2023. [Google Scholar]
- 18.Centers for Disease Control and Prevention, National Center for Health Statistics. US Standard certificate of live birth. https://www.cdc.gov/nchs/data/dvs/birth11-03final-ACC.pdf. Accessed April 17, 2023. [Google Scholar]
- 19.Centers for Disease Control and Prevention, National Center for Health Statistics. US Standard certificate of death. https://www.cdc.gov/nchs/data/dvs/DEATH11-03final-acc.pdf. Accessed April 17, 2023. [Google Scholar]
- 20.Centers for Disease Control and Prevention, National Center for Health Statistics. Vital statistics online. Cohort linked birth-infant death. www.cdc.gov/nchs/data_access/Vitalstatsonline.htm. Accessed April 17, 2023. [Google Scholar]
- 21.Centers for Disease Control and Prevention, National Center for Health Statistics. Guide to Completing the Facility Worksheet for the Certificate of Live Birth and Report of Fetal Death. https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. Accessed May 15, 2023. [Google Scholar]
- 22.U.S. Department of Agriculture, Food and Nutrition Service. https://www.fns.usda.gov/fns-regional-offices. Accessed May 15, 2023.
- 23.Lavista Ferres JM, Anderson TM, Johnston R, Ramirez JM, Mitchell EA. Distinct populations of sudden unexpected infant death based on age. Pediatrics. 2020;145(1):e20191637. 10.1542/peds.2019-1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lehtonen L, Gimeno A, Parra-Llorca A, Vento M. Early neonatal death: A challenge worldwide. Semin Fetal Neonatal Med. 2017;22(3):153–160. 10.1016/j.siny.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Brown Speights JS, Goldfarb SS, Wells BA, Beitsch L, Levine RS, RustG. State-level progress in reducing the black–white infant mortality gap, United States, 1999–2013. Am J Public Health. 2017;107(5):775–782. 10.2105/AJPH.2017.303689.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Department of Health and Human Services. Secretary’s advisory committee on infant mortality: recommendations for Department of Health and Human Services (HHS) action and framework for a national strategy. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/infant-mortality/reports/final-recommendations.pdf. Accessed May 15, 2023. [Google Scholar]
- 27.Minnesota Department of Health. Infant mortality reduction plan for Minnesota (Part 1); 2015. https://www.health.state.mn.us/docs/people/womeninfants/infantmort/infantmortalityacc.pdf. Accessed May 15, 2023.
- 28.Alabama public health; 2018. State of Alabama Infant Mortality Reduction Plan. https://www.alabamapublichealth.gov/perinatal/assets/alabama-imreduction-plan.pdf. Accessed May 15, 2023.
- 29.Washington State Department of Health. Infant Mortality Reduction Report. https://doh.wa.gov/sites/default/files/legacy/Documents/Pubs//140-157-InfantMortalityReductionReport.pdf. Accessed May 15, 2023; 2017.
- 30.Tennessee Department of Health. Infant mortality vital signs. https://www.tn.gov/health/health-program-areas/tennessee-vital-signs/redirect-tennessee-vital-signs/vital-signs-actions/infant-mortality.html. Accessed May 15, 2023. [Google Scholar]
- 31.Mississippi State Department of Health; 2019 & 2020 Infant mortality report. https://www.supremecourt.gov/opinions/URLs_Cited/OT2021/19-1392/19-1392-19.pdf Accessed May 15, 2023.
- 32.Adams JM. Breastfeeding and infant mortality in Indiana: changing the culture and saving lives: a model for other states. Breastfeed Med. 2017;12(8):456–458. 10.1089/bfm.2017.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Louisiana Department of Health. Louisiana commission on perinatal care and prevention of infant mortality: a review of priorities and progress: SFY 2019–2020. https://www.partnersforfamilyhealth.org/wp-content/uploads/2022/03/PC-REPORT-FINAL-5-26-20.pdf. Accessed May 15, 2023.
- 34.Center for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Breastfeeding initiation rates and maps by county; 2018–2019. https://www.cdc.gov/breastfeeding/data/county/breastfeeding-initiation-rates.html. Accessed May 15, 2023. [Google Scholar]
- 35.Driscoll AK, Ely DM, Centers for Disease Control and Prevention, National Center for Health Statistics. Declines in infant mortality in Appalachia and the Delta: 1995–1996 through 2017–2018. Natl Vital Stat Rep. 2021;70(6). 10.15620/cdc:104994. [DOI] [PubMed] [Google Scholar]
- 36.Lorenz JM, Ananth CV, Polin RA, D’Alton ME. Infant mortality in the United States. J Perinatol. 2016;36(10):797–801. 10.1038/jp.2016.63. [DOI] [PubMed] [Google Scholar]
- 37.Trent M, Dooley DG, Douge J, SECTION ON ADOLESCENT HEALTH, COUNCIL ON COMMUNITY PEDIATRICS, COMMITTEE ON ADOLESCENCE. The impact of racism on child and adolescent health. Pediatrics. 2019;144(2):e20191765. 10.1542/peds.2019-1765. [DOI] [PubMed] [Google Scholar]
- 38.Morrow AL, McClain J, Conrey SC, et al. Breastfeeding disparities and their mediators in an urban birth cohort of black and white mothers. Breastfeed Med. 2021;16(6):452–462. 10.1089/bfm.2020.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bartick M, Barr AW, Feldman-Winter L, Guxens M, Tiemeier H. The role of breastfeeding in racial and ethnic disparities in sudden unexpected infant death: a population-based study of 13 million infants in the United States. Am J Epidemiol. 2022;191(7):1190–1201. 10.1093/aje/kwac050. [DOI] [PubMed] [Google Scholar]
- 40.Tennessee Department of Health, Office of Policy, Planning, and Assessment, Division of Health Statistics. Death Record Data 2004–2014. [Google Scholar]
- 41.Chiang KV, Li R, Anstey EH, Perrine CG. Racial and ethnic disparities in breastfeeding initiation – United States, 2019. MMWR Morb Mortal Wkly Rep. 2021;70(21):769–774. 10.15585/mmwr.mm7021a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.United States Census Bureau. Women, infants, and children (WIC) program eligibility and participation; 2021. https://www.census.gov/library/visualizations/interactive/wic-eligibility-participation.html. Accessed December 9, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


