Abstract
Objective
The objective of this systematic review is to assess the effectiveness of digital orthodontics in utilizing implants for maxillary protraction as a treatment for skeletal class III malocclusion in children.
Materials and Methods
The study was registered with PROSPERO with the number CRD42023407406 on 23/03/2023. We conducted an extensive comprehensive literature search in nine electronic databases, including PubMed, PubMed Central, Scopus, Cochrane databases, Google Scholar, MEDLINE, EMBASE, LILACS, and the Web of Sciences databases. The studies were evaluated for their methodology, the intervention technology used, the outcomes, and their quality. Publication bias assessment was conducted using the Jadad scale and the ROBINS-I assessment tool.
Results
We included a total of 17 studies that comprised a total of 376 patients in this analysis. The number of patients and participants fluctuated between 1 and 71, with > 60 % being female. The patients were aged between 1.1 and 19.2 years. We included only nine studies in the meta-analysis, in which we observed a success rate between 71.4 % and 100 % with a 95 % CI of 17.4 ± 2.988 (±17.2 %) [14.412–20.388]. The failure rates, although minimal, ranged from 5.9 % to 28.6 %, with a 95 % CI of 2.3 ± 1.480 (±64.3 %) [0.820–3.780].
Conclusion
The evidence suggests that digital orthodontics is a promising approach for treating children with skeletal class III malocclusion using implants for maxillary protraction. However, further high-quality studies are required for validating our current observations and regulating the stability of treatment outcomes on a long-term basis.
Keywords: Orthodontics, Tomography, Digital, Maxillary protraction, Malocclusion
1. Introduction
Orthodontics is still struggling to adequately treat skeletal class III malocclusion, which continues to be among the most difficult issues. This particular type of malocclusion can arise from a maxilla that is retrognathic, a mandible that is prognathic, or a combination of the two (Nienkemper et al., 2013). Individuals with Class III malocclusion may exhibit various characteristics, including a deficiency in maxillary size, a posterior position of the maxilla, an excess in mandibular size, an anterior position of the mandible, or a combination of these factors. Previous research on the worldwide incidence of Class III malocclusions has demonstrated significant variability in its prevalence across and within various racial and ethnic groups, as well as the geographic locations studied (Zere et al., 2018). Previous studies have reported that protraction treatment impacts the circummaxillary and deeper maxillary sutures. Additionally, computer models have been utilized to simulate the effects of protraction in three dimensions.
For two-dimensional (2D) imaging, cephalometric and panoramic radiography, photos, and plaster representations have historically been employed. These 2D imaging systems, however, have several limitations, including significant projection errors in radiography, enlargement, distortion, and radiation exposure; identification of poor landmarks; erroneous measurement replication; significant differences in positioning the reference points; and a limited ability to evaluate soft tissue balance. Additionally, when doctors attempt to visualize three-dimensional (3D) craniofacial features using 2D imaging, some cephalometric structures and landmarks that are not present in the patient, such as the mandibular symphysis, articulare, pterygoid fossa, and “key ridges,” may emerge. Averaging bilateral components (e.g., the right and left inferior margins of the jaw) to create a uniform anatomic outline, such as the mandibular plane, results in the loss of parasagittal information and probable asymmetry in the patient. In essence, 2D imaging technologies are unable to address the inherent data loss that occurs when a 3D object is reduced to a 2D image.
Cone-beam computed tomography (CBCT) technology enables 2D image alignment in multiple planes, including coronal, sagittal, and oblique inclinations. Unlike traditional imaging systems, CBCT devices acquire all necessary data in a single rotation, thereby minimizing the patient's hospital stay and enhancing their satisfaction with the process (Erten and Yılmaz, 2018). Research has demonstrated that CBCT imaging offers more precise anatomic visualization compared to 2D radiographs and is superior to CT and MRI in identifying osseous alterations (İlgüy et al., 2014). The objective of this study is to evaluate the role of three-dimensional (3D) computerized models in the context of maxillary protraction for malocclusion. This includes analyzing studies that assess the effects of maxillary protraction with implants using 3D imaging, as well as examining the use of 3D-printed protraction appliances and implants.
2. Materials and methods
2.1. Study design
The study was registered with PROSPERO with the number CRD42023407406 on 23/03/2023. We conducted the current systematic review and meta-analysis, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The population (P), intervention (I), comparator (C), and outcome (O) (PICO) statement for this study is as follows: In children with skeletal class III malocclusion, the study aims to investigate the utility of digital orthodontics in maxillary protraction with implants and analyze their outcomes as compared to those of children with skeletal class III malocclusion who did not undergo maxillary protraction with implants or were treated without digital orthodontics. The intervention involved using 3D imaging for evaluating the effects of maxillary protraction with implants, as well as 3D-printed protraction appliances and implants. The outcomes included the efficacy of the digital orthodontic interventions, the ease of the procedures, the ease of surgical procedures, the time required for treatment, and any other effects. The study explored the potential benefits of digital orthodontics in improving the outcomes of maxillary protraction with implants in children with skeletal class III malocclusion. We conducted this study with the purpose of analyzing all published articles in the field of digital orthodontics in maxillary protraction and summing up their success and failure rates, outcomes, complications, and limitations.
2.2. Inclusion and exclusion criteria
The inclusion and exclusion criteria for this study have been framed to ensure that relevant and high-quality articles are included in the analysis while excluding articles that do not meet the necessary criteria. The study included descriptive, observational, cohort, cross-sectional, case-control, and randomized or non-randomized trials. Only original research articles with full text in English that focus on patients with children with skeletal class III malocclusion caused by maxillary retrognathism and have full-text in English were included. Conversely, case reports, case series, letters to the editor, and comprehensive and systematic reviews were excluded. Studies published in non-English languages, studies without comparison groups, studies with inadequate information regarding the methods and outcomes used for development and validation, and studies with an inadequate sampling strategy were also excluded. Additionally, studies that only used traditional methods to treat and analyze children with skeletal class III caused by maxillary retrognathism without using digital orthodontics were excluded. No restrictions were placed on the publication year. These inclusion and exclusion criteria helped ensure that the analysis focused on studies that are relevant to the research question and have sufficient methodological rigor to support their findings.
2.3. Literature search strategy
The current study on “Utility of Digital Orthodontics in Maxillary Protraction with Implants in Children with Skeletal Class III—A Systematic Review and Meta-Analysis” involved the analysis of the articles published from databases like PubMed, PubMed Central, Scopus, Google Scholar, Cochrane databases, MEDLINE, EMBASE, LILACS, and Web of Sciences databases from inception until April 31, 2023, without any restriction on the year of publication. The search strings used in the current study are as follows: ([”skeletal class III“ OR ”deficient maxilla“ OR ”retrognathic maxilla“] AND ”maxillary protraction with implants“ OR ”early orthodontics“ AND ”three-dimensional imaging“ OR ”3D imaging“ OR ”3D printing“ OR ”cone-beam computed tomography“ OR ”CBCT“ OR ”scanning“ OR ”intra-oral scanning“ OR ”digital orthodontics“) (Rasteau et al., 2020).
2.4. Study selection and data extraction
Following the first screening, two researchers independently reviewed the whole text and screened the publications that fulfilled the inclusion criteria. If there were any conflicts, another researcher was chosen to assess the work. In this study, all articles were screened to identify relevant data for analysis. The following information were recorded for each article: article type, authors, publication year, number of patients, number of implants, gender and age distribution of the patients, treatment procedures, primary outcomes, secondary outcomes, associated complications, and limitations of the study. These data points allowed for a comprehensive analysis of the studies, including the patient population, treatment methods, outcomes, and any limitations or complications associated with the interventions. By collecting and analyzing this data, the study aims to provide insights into the utility of digital orthodontic interventions for maxillary protraction with implants in children with skeletal class III malocclusion and to identify potential areas for future research in this field.
2.5. Literature quality evaluation
To ensure the accuracy and reliability of the analysis, the included studies were subjected to quality analysis with two assessment tools: the Jadad scale and the ROBINS-I assessment tool for risk of bias. Two researchers independently assessed the quality of each article based on the Jadad scale, which assigns scores of 0 to 2 for low quality, 3 for moderate quality, and 4 to 5 for high quality. Any disagreement was resolved by a third researcher. In addition, the risk of bias in each study was assessed by ROBINS-I assessment tool. The two researchers evaluated the literature independently and discussed any discrepancies to ensure the accuracy of the analysis. By using these two assessment tools, we aimed to provide a thorough and reliable evaluation of the quality of the included articles.
2.6. Statistical analysis
We used IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA) to perform the statistical analysis. Dichotomous variables were analyzed to calculate the incidence rate (odds ratio, OR), and a 95 % confidence interval (CI) was used to express interval estimation. The size of the effect was determined by calculating the standardized mean deviation. To calculate the odds ratio for success rates, a forest plot was generated using Microsoft Excel to represent the overall success rates associated with the use of digital orthodontics in maxillary protraction. These statistical analyses provide a comprehensive evaluation of the outcomes of the studies included in this analysis.
3. Results
3.1. Literature selection
On initial screening, a total of 257 articles were retrieved from nine databases (PubMed, PubMed Central, Scopus, Cochrane databases, Google Scholar, MEDLINE, EMBASE, LILACS, and Web of Science databases). After screening for duplications, non-English articles, and articles without full text, a total of 163 articles were screened for their eligibility. After excluding 56 articles as they did not fall under our scope, i.e., no digital orthodontics was performed or studied (n = 41), and without complete data (n = 15), we included a total of 17 studies in this study. The year of publication was 2009–2022. The PRISMA chart of the study, which provides detailed data on literature collection and screening, is shown in Fig. 1. Among these studies, clinical trials were the most common study type, with seven studies falling into this category. Prospective clinical studies were the second most common, with five studies included in the analysis, two were randomized controlled trials (RCTs), and the remaining two were pilot studies.
Fig. 1.
PRISMA chart showing detailed data on literature collection and screening.
3.2. Characteristics of the literature
3.2.1. Patient characteristics
In total, 376 patients were included in the analysis from 17 studies, and the number of patients ranged from 1 to 71, with 128 males and 200 females. However, gender was not disclosed in three studies accounting for 50 participants. The ages of the patients ranged between 1.1 and 19.2 years. Table 1 shows the demographic and general characteristics of the patients presented in the included studies of this analysis.
Table 1.
Demographic and general characteristics of the patients.
| S. No | Study details | Sample size | Mean age | Gender distribution (M:F) | Clinical manifestations |
|---|---|---|---|---|---|
| Heymann et al. (2010) | 6 | 11.8 years | 3:3 | Skeletal class III malocclusion | |
| Cevidanes et al. (2009) | 3 | 11.4 years | NR | Skeletal class III malocclusion | |
| De Clerck et al. (2010) | 21 | 11.10 ± 1.8 years | ND | Class III malocclusion | |
| Nguyen et al. (2011) | 25 | 1.10 ± 1.1 years | 12:13 | Dentoskeletal class III malocclusion | |
| Choi et al. (2012) | 30 | 9.6 years | 12:18 | Maxillary malocclusion | |
| Hino et al. (2013) | 46 | 10.15 years | 17:29 | Class III malocclusion | |
| Liu et al. (2015) | 24 | ND | ND | Maxillary retrusion | |
| Lee et al. (2016) | 71 | 19.2 years | 18:53 | Malocclusion | |
| Almuzian et al. (2019) | 14 | 12.05 ± 1.09 years | 7:7 | Class III malocclusions with retrognathic maxillae | |
| Ren et al. (2019) | 18 | 11 years | 12:6 | Skeletal class III malocclusion | |
| de Souza et al. (2019) | 24 | 10 years | 11:13 | Angle class III malocclusion because of the middle third of the face deficiency | |
| Cantarella et al. (2020) | 1 | 12.9 years | 0:1 | Class III malocclusion with the deficiency of the transverse and sagittal maxilla | |
| Buyukcavus et al. (2020) | 55 | 11.4 ± 1.06 years | 26:29 | Class III malocclusion - maxillary retrognathia | |
| Liang et al. (2020) | 1 | 12.5 years | 0:1 | Anterior crossbite and poor facial esthetics | |
| Kim et al. (2021) | 2 | 9.5 years | 2:0 | Skeletal class III malocclusion - maxillary retrognathism, mandible prognathism, and dentofacial deformity | |
| Franchi et al. (2022) | 1 | 8 years | 0:1 | Skeletal class III malocclusion | |
| Kapetanović et al. (2022) | 34 | 27.0 ± 9.4 years | 8:26 | Transverse maxillary deficiency |
ND, not disclosed.
3.2.2. Intervention technology
Six types of intervention technologies were used in the 17 included studies, with CBCT being the most commonly used one. The distribution of intervention technologies was as follows: CBCT (n = 11); CBCT and intraoral scanning (n = 2); non-contrast three-dimensional optical scanner (n = 1); cephalometric analysis (n = 1); Dolphin Imaging computerized cephalometric analysis (n = 1); and Bellus3D DentalPro (n = 1). Cephalometric analysis reported a lower success rate than other techniques.
3.2.3. Outcomes of the study
The duration of treatment in the studies ranged between 31 days and 48 months. Twelve months was the most commonly reported treatment duration in six of the 17 included studies. The minimum success rate was 71.4 %, but most studies reported a 100 % success rate with minimal or no complications. Fifty percent of the included studies did not report success rates for the treatment.
3.2.4. Primary and secondary outcomes
The primary outcomes of the included studies indicate that digital orthodontics, in combination with various techniques and interventions, offers reliable and repeatable methods for assessing growing patients in three dimensions. The use of cone-beam computed tomography provides enhanced visualization and description of treatment changes compared to two-dimensional imaging alone. Positive improvements are observed in intermaxillary skeletal variables, maxillo-mandibular relationships, and dental movements. The findings support the effectiveness of bone-anchored maxillary protraction, mini-implants, and customized devices in correcting class III malocclusion. Digital planning contributes to successful maxillary expansion and protraction while maintaining stable occlusal relationships and satisfactory facial profiles. The study highlights the potential of digital orthodontics to achieve desired treatment outcomes with minimal side effects. The major secondary outcomes observed included facial convexity, soft tissue changes, and lip projection. The detailed primary and secondary outcomes of each study are presented in Table 2 which also shows the included studies and the data extraction for the current analysis.
Table 2.
Data extraction from the included studies.
| S. No | Author name and Year of Publication | Type of study | Objective of the study | Interventions | Digital analysis used | Treatment / follow-up period | Primary outcomes | Secondary outcomes | Success rate | Limitations / disadvantages / complications |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Heymann et al. (2010) | Controlled clinical trials | The skeletal and dental changes in 3D resulting from the use of temporary anchorage devices and intermaxillary elastics were being described. | Intermaxillary elastics from temporary anchorage devices | CBCT | 9 to 12 months | The use of cone-beam computed tomography allowed for more detailed visualization and description of treatment changes compared to 2D imaging alone. | The use of intermaxillary elastics from temporary anchorage devices improves skeletal relationships in maxillary-deficient Class III patients with minimal compensatory dental changes. | NR | Small sample size. |
| 2. | Cevidanes et al. (2009) | Controlled clinical trials | A new technique for superimposing 3D models of growing subjects was being evaluated. | Orthopedic treatment with miniplates | CBCT | 12 months | This study's technique is a reliable and repeatable method for assessing growing patients in 3D. | The use of 3D modeling provides a more detailed description of treatment outcomes and different remodeling patterns. | NR | None declared. |
| 3. | De Clerck et al. (2010) | Controlled clinical trials | The effectiveness of a treatment protocol for Class III malocclusion that involved surgically placing mini-plates in the maxilla and mandible, connected by Class III elastics, was being assessed. | Surgical mini-plate placement | CBCT | 12 months | Intermaxillary skeletal variables showed significant improvements. | The treatment protocol prevented the lingual tipping of mandibular incisors often seen in untreated Class III subjects. | NR | None reported. |
| 4. | Nguyen et al. (2011) | Controlled clinical trials | The 3D changes in the maxilla, surrounding hard and soft tissues, and circummaxillary sutures resulting from bone-anchored maxillary protraction treatment were being evaluated. | Class III intermaxillary elastics and bilateral miniplates | CBCT | 2 to 3 months | This treatment approach resulted in significant orthopedic changes in the maxilla and zygoma of growing Class III patients. | Significant and comparable soft-tissue changes were observed. | NR | None reported |
| 5. | Choi et al. (2012) | Controlled clinical trials | The accuracy of a 3D superimposition method for digital models in rapid maxillary expansion and maxillary protraction headgear treatments was being evaluated. | Rapid maxillary expansion and maxillary protraction headgear treatment | Non-contact 3D optical scanner | 8.4 ± 2.5 months | Antero-posterior incisor and molar movements measured with 3D superimposed models showed a strong correlation with cephalometric radiographs. | The 3D maxillary superimposition method is a clinically reliable tool for assessing antero-posterior tooth movement in RME protraction headgear cases. | 100 % | Only moderate agreement has been reported. |
| 6. | Hino et al. (2013) | Controlled clinical trials | The growth and treatment effects on the midface and maxillary dentition were being evaluated in 3D. | Rapid maxillary expansion compared with bone-anchored maxillary protraction | CBCT | 10 to 12 months | The treatment produced greater dental than skeletal changes and a primarily vertical maxillary displacement. | 3D measurements are a reliable means of assessment. | NR | None reported |
| 7. | Liu et al. (2015) | RCT | The effects of maxillary protraction combined with repetitive rapid palatal expansions and constrictions versus rapid palatal expansion alone were being investigated using CBCT. | Maxillary protraction and repetitive rapid palatal expansions and constrictions vs. rapid palatal expansion | CBCT | NR | Significantly greater maxillary protraction was observed when combined with repetitive, rapid palatal expansions. | Maxillary protraction with RPE/C may be more effective at moving the maxilla forward than the RPE alone protocol in the early treatment of maxillary retrusion patients. | NR | None reported. |
| 8. | Lee et al. (2016) | Controlled clinical trials | The success rate of orthodontic microimplants was being evaluated using CBCT images and their relationship with bone densities. | Orthodontic microimplants implanted into the maxillary buccal alveolar bone | CBCT | NR | Higher cancellous and total bone densities resulted in a greater success rate for orthodontic microimplants. | Cortical bone density does not significantly affect treatment outcomes. | 85.0 % | Follow-up period not reported. |
| 9. | Almuzian et al. (2019) | Pilot study | The 3D treatment changes resulting from intra-oral protraction combined with an alternate rapid maxillary expansion and constriction protocol in treating Class III patients were described. | Intra-oral protraction and alternate rapid maxillary expansion and constriction | CBCT | 9 weeks | The use of bone-anchored class III protraction, along with a MARME appliance and an Alt-RAMEC protocol, improved the maxillo-mandibular relationship in class III malocclusion. | Short-term treatment effects include both skeletal and soft tissue changes. | 71.4 % | Small sample size and lack of control group |
| 10. | Ren et al. (2019) | Controlled clinical trials | The effect of bone-anchored maxillary protraction therapy in cleft children with Class III malocclusion was being evaluated using cone-beam computed tomography-derived 3D surface models. | Bone-anchored maxillary protraction therapy | CBCT | 18 months | Bone-anchored maxillary protraction therapy was effective in correcting Class III malocclusion in cleft children. | Improvement was observed in lip projection and facial convexity in two-thirds of the subjects. | NR | None reported. |
| 11. | de Souza et al. (2019) | Controlled clinical trials | The treatment of Class III patients with maxillary retrusion using orthodontic mini-implants associated with intermaxillary elastics was being compared with the rapid maxillary expansion and facemask protocol. | Rapid maxillary expansion (with addition of 0.9 mm orthodontic wire on the vestibular and palatine surfaces) vs. conventional orthodontic mini-implants | Cephalometric analysis | 12.5 to 16.0 months | Mini-implants may be a viable option for correcting Class III malocclusion caused by maxillary deficiency. | The maxilla was more protracted than the mandible, resulting in increased facial convexity. | 83.3 % | 16.7 % implants failed. |
| 12. | Cantarella et al. (2020) | Controlled clinical trials | A novel methodology had been developed to plan the position of a maxillary skeletal expander using digital models of dental arches and CBCT. | The digital model of dental arches and CBCT was used to create virtual model of Maxillary Skeletal Expander | CBCT | 7 months | Digital planning was associated with a positive outcome for maxillary expansion and protraction with minimal safety concerns. | Treatment successfully resolved lateral cross-bite and over-corrected the OVJ from 1.5 mm to 3.9 mm. | 100 % | None reported. CBCT may expose children to additional radiations. |
| 13. | Buyukcavus et al. (2020) | RCT | The efficacy of different maxillary protraction methods in patients with skeletal Class III malocclusion resulting from maxillary retrognathia was being compared. | Alternate rapid maxillary expansion and constriction | The Dolphin Imaging computerized cephalometric analysis | 6 to 11 months | The modified Alternate Rapid Maxillary Expansion and Constriction group had a higher rate of protraction. | A greater skeletal effect was found in the skeletal anchorage group. | NR | CBCT was not used. |
| 14. | Liang et al. (2020) | Controlled clinical trials | The influence of 3D digital technology in offering individualized treatment was being evaluated. | Rapid maxillary expansion and protraction performed using three-dimensional-printed mini-plates for anchorage | CBCT | 48 months | The occlusal relationship, overbite, and overjet remained stable, and the facial profile was satisfactory. | Customized mini-plates offer a clinical application with a small incision, individualized insertion points, an easy surgical procedure, and a short surgical duration. | 100 % | None reported |
| 15. | Kim et al. (2021) | Pilot Controlled clinical trials | The feasibility of individualized bone-anchored maxillary protraction using preoperative simulation and 3D titanium printing was being analyzed. | Bone-anchored maxillary protraction | CBCT and intraoral scanning | 24 months | Preoperative simulation and 3D titanium printing allowed for the precise fabrication and placement of customized BAMP devices. | Clinical results demonstrate the stability and effectiveness of this modality for treating skeletal Class III malocclusion. | 100 % | Mild infection in right mandible. |
| 16. | Franchi et al. (2022) | Controlled clinical trials | A customized maxillary protraction facemask, produced by 3D face scanning, digital design, and additive manufacturing, was being evaluated for its effectiveness. | Hyrax-type rapid palatal expander | Bellus3D DentalPro | 10 to 12 months | The patient responded well to the customized facemask, and it produced the intended treatment results. | NR | 100 % | Small sample size |
| 17. | Kapetanović et al. (2022) | Controlled clinical trials | A higher level of evidence on the efficacy of miniscrew-assisted rapid palatal expansion was being provided. | Dutch Maxillary Expansion Device (a 3D device) | CBCT and intraoral scanning | 31.7 ± 8.0 days | A significant amount of skeletal expansion was observed with minimal side effects. | High-quality evidence supports miniscrew-assisted rapid palatal expansion as a safe and successful non-surgical treatment option for transverse maxillary deficiency. | 94.1 % | Shorter observation period. |
CBCT, cone-beam computed tomography; RCT, randomized controlled trials.
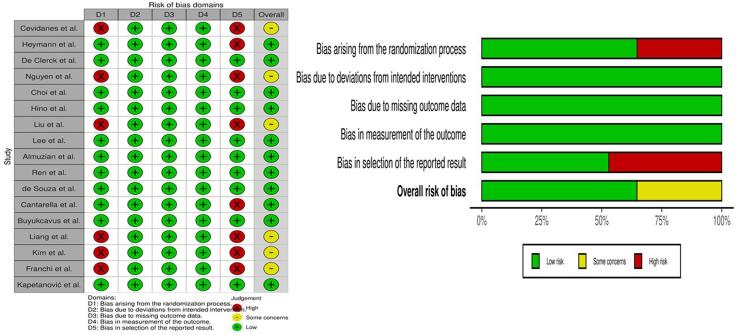
3.2.5. Literature quality and risk of bias assessment
Table 3 shows the quality of the included studies based on the Jadad scale scores. Eleven out of 17 studies were of high quality, whereas the remaining six showed moderate quality. Fig. 2 shows the variables included in the risk of bias assessment plot and summary, respectively.
Table 3.
Quality of the literature based on to the Jadad scale scores.
| Name of the Study | Selection bias | Performance bias | Reporting bias | Attribution bias | Other bias | Results | Quality of the study |
|---|---|---|---|---|---|---|---|
| Heymann et al. (2010) | 1 | 1 | 1 | 1 | 0 | 4 | High |
| Cevidanes et al. (2009) | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| De Clerck et al. (2010) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Nguyen et al. (2011) | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| Choi et al. (2012) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Hino et al. (2013) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Liu et al. (2015) | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| Lee et al. (2016) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Almuzian et al. (2019) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Ren et al. (2019) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| de Souza et al. (2019) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Cantarella et al. (2020) | 1 | 1 | 1 | 1 | 0 | 4 | High |
| Buyukcavus et al. (2020) | 1 | 1 | 1 | 1 | 1 | 5 | High |
| Liang et al. (2020) | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| Kim et al. (2021) | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| Franchi et al. (2022) | 0 | 1 | 1 | 1 | 0 | 3 | Moderate |
| Kapetanović et al. (2022) | 1 | 1 | 1 | 1 | 1 | 5 | High |
Selection bias: Has the study included comparison between groups or existing data?
Performance bias: Has the study reported the estimated effects clearly?
Reporting bias: Was the study free from problems with measurements or classification of outcomes?
Attribution bias: Has the study reported complete outcome data?
Other Bias: Was the study free from limitations?
Fig. 2.
Risk of bias assessment plot.
3.2.6. Meta-analysis results
Only nine studies were subjected to meta-analysis, which included an analysis of the success rates of treatments using digital technologies. Eight studies were excluded as there were no details reported on success or complication rates. The studies that reported success and failure rates constituted a total of 178 patients (95 % confidence intervals (CI), 19.7 ± 3.217 (±16.3 %) [16.483–22.917]); success rates ranged from 71.4 % to 100 %, with a 95 % CI of 17.4 ± 2.988 (±17.2 %) [14.412–20.388]. The failure rates, although minimal, ranged from 5.9 % to 28.6 %, with a 95 % CI of 2.3 ± 1.480 (±64.3 %) [0.820–3.780]. Fig. 3 shows the forest plot constructed to represent the success rates of digital orthodontics in maxillary protraction in skeletal class III malocclusion.
Fig. 3.
Forest plot showing the success rates of digital orthodontics among the studies.
4. Discussion
The current study analyzed the use of digital technology in children with skeletal class III malocclusion for maxillary protraction. To plan for orthognathic surgery, the key elements include the facial soft tissues, facial skeleton, and dentition. However, to capture these important tissue groups, it is necessary to use a technique called “image fusion,” which involves combining 3D facial image capture with CBCT images (Rasteau et al., 2020) This results in a virtual 3D patient that orthodontists and surgeons may use to analyze the patient's craniofacial skeleton and soft tissue. The dynamic 3D models may be seen from any angle, allowing for full diagnosis and treatment planning (Erten and Yılmaz, 2018).
We reviewed 17 articles retrieved from nine databases that investigated digital orthodontics, which included 376 patients with ages ranging from 1.1 to 19.2 years and 128 males and 200 females, with three studies not disclosing gender information. The main findings of this study are that the success rates of using digital technologies like CBCT have been higher than those of conventional methods. Of the 17 included studies, eleven had a low risk of publication bias, whereas the other six had some concerns with the randomization process and reporting their outcomes.
A comprehensive evaluation of three randomized controlled trials found that, while not clinically significant, using a facemask attached to the patient's skeleton resulted in a higher rise in the SNA angle at the conclusion of therapy. On the other hand, using a facemask anchored to the patient's teeth resulted in a greater inclination of the maxillary incisors and an increased risk of complications compared to the skeletal anchorage method (Rutili et al., 2023). In our analysis, the most common clinical manifestation was malocclusion, with class III and retrognathic maxillae being the most reported. According to a recent study, CBCT can be used to generate lateral cephalograms, which can provide some useful comparisons with 2D images. However, there are concerns regarding the practicality and suitability of 3D imaging for all patients. This is because 3D imaging involves a greater exposure to ionizing radiation, and it takes a significant amount of time to prepare each patient's DICOM files through processes such as segmentation, registration, and visualization. In fact, the study found that it took an average of 25 to 40 h to complete these tasks for each patient, which highlights the potential challenges associated with implementing 3D imaging techniques in routine clinical practice (Heymann et al., 2010). The majority of the included studies used CBCT as their intervention technology. The study outcomes showed a success rate ranging between 45 % and 100 % and duration of treatment ranging between 31 days and 48 months.
The study's findings are important because they provide an overview of the current research on digital orthodontics, which is a rapidly growing field. The use of digital technology in orthodontics has revolutionized the field, allowing for more precise and accurate diagnosis, treatment planning, and monitoring. The inclusion of a variety of patient ages and clinical manifestations in the selected studies provides a more comprehensive picture of the potential applications of digital orthodontics. Additionally, using CBCT as the most common intervention technology highlights the importance of this tool in the diagnosis and planning of treatments in orthodontic cases. However, the lower success rate reported for cephalometric analysis highlights the limitations of traditional methods. The study's scope is limited by the small number of studies that were included in the analysis. Furthermore, we have included only the articles published in English, which may have induced selection and publication bias. Additionally, the heterogeneity of the included studies regarding patient characteristics and treatment protocols makes it difficult to draw definitive conclusions about the effectiveness of digital orthodontics. We cannot rule out the possibility of publication bias, as our studies ranged from moderate to high quality.
5. Conclusion
In conclusion, the available literature suggests that digital orthodontics is capable of improving diagnosis, treatment plans, and monitoring of orthodontic cases. However, more studies are necessary to establish the efficacy and long-term outcomes of digital orthodontics in comparison to traditional methods.
6. Authors' contributions
1. Collection of data and bibliography.
2. Idea and concept and manuscript preparation.
3. Review of Literature.
4 Discussion.
5. Registration of review in Prospero and follow up.
6. Statistical Analyses.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Kindly mention manuscriptedit for the editing services.
Footnotes
Peer review under responsibility of King Saud University. Production and hosting by Elsevier.
Contributor Information
Fawaz Hassan Alzahrani, Email: fawaz199919@gmail.com.
Raghu Devanna, Email: r.devanna@tu.edu.sa.
Yousef Althomali, Email: yalthomali@tu.edu.sa.
Nayef Hassan Felemban, Email: nfelemban@tu.edu.sa.
Prashant Manjunath Battepati, Email: drprashant@tudent.org.
Amith V. Holenarasipur, Email: amith.taif@tudent.org.
References
- Almuzian M., Almukhtar A., Ulhaq A., Alharbi F., Darendeliler M.A. 3D effects of a bone-anchored intra-oral protraction in treating class III growing patient: a pilot study. Prog. Orthod. 2019;20:37. doi: 10.1186/s40510-019-0290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buyukcavus M.H., Kale B., Aydemir B. Comparison of treatment effects of different maxillary protraction methods in skeletal class III patients. Orthodont. Craniofac. Res. 2020;23:445–454. doi: 10.1111/ocr.12389. [DOI] [PubMed] [Google Scholar]
- Cantarella D., Savio G., Grigolato L., Zanata P., Berveglieri C., Lo Giudice A., Isola G., Del Fabbro M., Moon W. A new methodology for the digital planning of micro-implant-supported maxillary skeletal expansion. Med. Devices (Auckl) 2020;13:93–106. doi: 10.2147/MDER.S247751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cevidanes L.H., Heymann G., Cornelis M.A., DeClerck H.J., Tulloch J.F. Superimposition of 3-dimensional CBCT models of growing patients. Am. J. Orthodont. Dentofac. Orthoped. 2009;136:94–99. doi: 10.1016/j.ajodo.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.I., Cha B.K., Jost-Brinkmann P.G., Choi D.S., Jang I.S. Validity of palatal superimposition of 3-dimensional digital models in cases treated with rapid maxillary expansion and maxillary protraction headgear. Korean J. Orthod. 2012;42:235–241. doi: 10.4041/kjod.2012.42.5.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clerck H., Cevidanes L., Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am. J. Orthodont. Dentofac. Orthoped. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Souza R.A., Rino Neto J., de Paiva J.B. Maxillary protraction with rapid maxillary expansion and facemask versus skeletal anchorage with mini-implants in class III patients: a non-randomized clinical trial. Prog. Orthod. 2019;20:35. doi: 10.1186/s40510-019-0288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erten O., Yılmaz B.N. Three-dimensional imaging in orthodontics. Turk. J. Orthod. 2018;31:86–94. doi: 10.5152/TurkJOrthod.2018.17041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franchi L., Vichi A., Marti P., Lampus F., Guercio S., Recupero A., Giuntini V., Goracci C. 3D printed customized facemask for maxillary protraction in the early treatment of a class iii malocclusion: proof-of-concept clinical case. Materials (Basel) 2022;15:3747. doi: 10.3390/ma15113747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann G.C., Cevidanes L., Cornelis M., De Clerck H.J., Tulloch J.F. Three-dimensional analysis of maxillary protraction with intermaxillary elastics to miniplates. Am. J. Orthodont. Dentofac. Orthoped. 2010;137:274–284. doi: 10.1016/j.ajodo.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hino C.T., Cevidanes L.H., Nguyen T.T., De Clerck H.J., Franchi L., McNamara J.A., Jr. Three-dimensional analysis of maxillary changes associated with facemask and rapid maxillary expansion compared with bone anchored maxillary protraction. Am. J. Orthodont. Dentofac. Orthoped. 2013;144:705–714. doi: 10.1016/j.ajodo.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- İlgüy D., İlgüy M., Fişekçioğlu E., Dölekoğlu S., Ersan N. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. Sci. World J. 2014;2014 doi: 10.1155/2014/761714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapetanović A., Odrosslij B.M., Baan F., Bergé S.J., Noverraz R.R., Schols J.G., Xi T. Efficacy of Miniscrew-Assisted Rapid Palatal Expansion (MARPE) in late adolescents and adults with the Dutch Maxillary Expansion Device: a prospective clinical cohort study. Clin. Oral Invest. 2022;26:6253–6263. doi: 10.1007/s00784-022-04577-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M., Li J., Kim S., Kim W., Kim S.H., Lee S.M., Park Y.L., Yang S., Kim J.W. Individualized 3d-printed bone-anchored maxillary protraction device for growth modification in skeletal class iii malocclusion. J. Pers. Med. 2021;11:1087. doi: 10.3390/jpm11111087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M.Y., Park J.H., Kim S.C., Kang K.H., Cho J.H., Cho J.W., Chang N.Y., Chae J.M. Bone density effects on the success rate of orthodontic microimplants evaluated with cone-beam computed tomography. Am. J. Orthodont. Dentofac. Orthoped. 2016;149:217–224. doi: 10.1016/j.ajodo.2015.07.037. [DOI] [PubMed] [Google Scholar]
- Liang S., Xie X., Wang F., Chang Q., Wang H., Bai Y. Maxillary protraction using customized mini-plates for anchorage in an adolescent girl with skeletal Class III malocclusion. Korean J. Orthod. 2020;50:346–355. doi: 10.4041/kjod.2020.50.5.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Song Y., Wang X., He D., Zhou Y. A cone-beam computed tomography evaluation of maxillary protraction with repetitive rapid palatal expansions and constrictions. Zhonghua Kou Qiang Yi Xue Za Zhi. 2015;50:78–83. [PubMed] [Google Scholar]
- Nguyen T., Cevidanes L., Cornelis M.A., Heymann G., de Paula L.K., De Clerck H. Three-dimensional assessment of maxillary changes associated with bone anchored maxillary protraction. Am. J. Orthodont. Dentofac. Orthoped. 2011;140:790–798. doi: 10.1016/j.ajodo.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nienkemper M., Wilmes B., Pauls A., Drescher D. Maxillary protraction using a hybrid hyrax-facemask combination. Prog. Orthod. 2013;14:5. doi: 10.1186/2196-1042-14-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasteau S., Sigaux N., Louvrier A., Bouletreau P. Three-dimensional acquisition technologies for facial soft tissues – Applications and prospects in orthognathic surgery. J. Stomatol. Oral Maxillofac. Surg. 2020;121:721–728. doi: 10.1016/j.jormas.2020.05.013. [DOI] [PubMed] [Google Scholar]
- Ren Y., Steegman R., Dieters A., Jansma J., Stamatakis H. Bone-anchored maxillary protraction in patients with unilateral complete cleft lip and palate and Class III malocclusion. Clin. Oral Invest. 2019;23:2429–2441. doi: 10.1007/s00784-018-2627-3. [DOI] [PubMed] [Google Scholar]
- Rutili V., Nieri M., Franceschi D., Pierleoni F., Giuntini V., Franchi L. Effects produced by the facemask with and without skeletal anchorage for the orthopaedic treatment of Class III malocclusion in growing patients: a systematic review and meta-analysis of RCTs. Eur. J. Orthod. 2023;45:157–168. doi: 10.1093/ejo/cjac048. [DOI] [PubMed] [Google Scholar]
- Zere E., Chaudhari P.K., Sharan J., Dhingra K., Tiwari N. Developing Class III malocclusions: challenges and solutions. Clin. Cosmet. Investig. Dent. 2018;10:99–116. doi: 10.2147/CCIDE.S134303. [DOI] [PMC free article] [PubMed] [Google Scholar]