Abstract
Background
Parental psychosocial health can have a significant effect on the parent‐child relationship, with consequences for the later psychological health of the child. Parenting programmes have been shown to have an impact on the emotional and behavioural adjustment of children, but there have been no reviews to date of their impact on parental psychosocial wellbeing.
Objectives
To address whether group‐based parenting programmes are effective in improving parental psychosocial wellbeing (for example, anxiety, depression, guilt, confidence).
Search methods
We searched the following databases on 5 December 2011: CENTRAL (2011, Issue 4), MEDLINE (1950 to November 2011), EMBASE (1980 to week 48, 2011), BIOSIS (1970 to 2 December 2011), CINAHL (1982 to November 2011), PsycINFO (1970 to November week 5, 2011), ERIC (1966 to November 2011), Sociological Abstracts (1952 to November 2011), Social Science Citation Index (1970 to 2 December 2011), metaRegister of Controlled Trials (5 December 2011), NSPCC Library (5 December 2011). We searched ASSIA (1980 to current) on 10 November 2012 and the National Research Register was last searched in 2005.
Selection criteria
We included randomised controlled trials that compared a group‐based parenting programme with a control condition and used at least one standardised measure of parental psychosocial health. Control conditions could be waiting‐list, no treatment, treatment as usual or a placebo.
Data collection and analysis
At least two review authors extracted data independently and assessed the risk of bias in each study. We examined the studies for any information on adverse effects. We contacted authors where information was missing from trial reports. We standardised the treatment effect for each outcome in each study by dividing the mean difference in post‐intervention scores between the intervention and control groups by the pooled standard deviation.
Main results
We included 48 studies that involved 4937 participants and covered three types of programme: behavioural, cognitive‐behavioural and multimodal. Overall, we found that group‐based parenting programmes led to statistically significant short‐term improvements in depression (standardised mean difference (SMD) ‐0.17, 95% confidence interval (CI) ‐0.28 to ‐0.07), anxiety (SMD ‐0.22, 95% CI ‐0.43 to ‐0.01), stress (SMD ‐0.29, 95% CI ‐0.42 to ‐0.15), anger (SMD ‐0.60, 95% CI ‐1.00 to ‐0.20), guilt (SMD ‐0.79, 95% CI ‐1.18 to ‐0.41), confidence (SMD ‐0.34, 95% CI ‐0.51 to ‐0.17) and satisfaction with the partner relationship (SMD ‐0.28, 95% CI ‐0.47 to ‐0.09). However, only stress and confidence continued to be statistically significant at six month follow‐up, and none were significant at one year. There was no evidence of any effect on self‐esteem (SMD ‐0.01, 95% CI ‐0.45 to 0.42). None of the trials reported on aggression or adverse effects.
The limited data that explicitly focused on outcomes for fathers showed a statistically significant short‐term improvement in paternal stress (SMD ‐0.43, 95% CI ‐0.79 to ‐0.06). We were unable to combine data for other outcomes and individual study results were inconclusive in terms of any effect on depressive symptoms, confidence or partner satisfaction.
Authors' conclusions
The findings of this review support the use of parenting programmes to improve the short‐term psychosocial wellbeing of parents. Further input may be required to ensure that these results are maintained. More research is needed that explicitly addresses the benefits for fathers, and that examines the comparative effectiveness of different types of programme along with the mechanisms by which such programmes bring about improvements in parental psychosocial functioning.
Keywords: Female, Humans, Anxiety, Anxiety/therapy, Depression, Depression/therapy, Maternal Behavior, Maternal Behavior/psychology, Maternal Welfare, Mother‐Child Relations, Parenting, Parenting/psychology, Parents, Parents/education, Parents/psychology, Paternal Behavior, Paternal Behavior/psychology, Program Evaluation, Randomized Controlled Trials as Topic, Self Concept
Plain language summary
Parent training for improving parental psychosocial health
Parental psychosocial health can have a significant effect on the parent‐child relationship, with consequences for the later psychological health of the child. Some parenting programmes aim to improve aspects of parental wellbeing and this review specifically looked at whether group‐based parenting programmes are effective in improving any aspects of parental psychosocial health (for example, anxiety, depression, guilt, confidence).
We searched electronic databases for randomised controlled trials in which participants had been allocated to an experimental or a control group, and which reported results from at least one scientifically standardised measure of parental psychosocial health.
We included a total of 48 studies that involved 4937 participants and covered three types of programme: behavioural, cognitive‐behavioural and multimodal. Overall, the results suggested statistically significant improvements in the short‐term for parental depression, anxiety, stress, anger, guilt, confidence and satisfaction with the partner relationship. However, only stress and confidence continued to be statistically significant at six month follow‐up, and none were significant at one year. There was no evidence of effectiveness for self‐esteem at any time point. None of the studies reported aggression or adverse outcomes.
Only four studies reported the outcomes for fathers separately. These limited data showed a statistically significant short‐term improvement in paternal stress but did not show whether the parenting programmes were helpful in terms of improving depressive symptoms, confidence or partner satisfaction.
This review shows evidence of the short‐term benefits of parenting programmes on depression, anxiety, stress, anger, guilt, confidence and satisfaction with the partner relationship. The findings suggest that further input may be needed to support parents to maintain these benefits. However, more research is needed that explicitly addresses the benefits for fathers, and that provides evidence of the comparative effectiveness of different types of programme and identifies the mechanisms involved in bringing about change.
Background
Description of the condition
Parental psychosocial functioning is a significant factor influencing a range of aspects of children's development and wellbeing (see below). It consists of a wide range of components but those most frequently researched in terms of their impact on the wellbeing of children include parental mental health (that is depression and anxiety, parental confidence and parental conflict). The available evidence relates to infancy and toddlerhood, and to mid‐childhood and adolescence.
1. Infant and toddlerhood
The postnatal period has been identified as being of particular importance in terms of the infant's need for affectively attuned parenting (Jaffe 2001) and for parental reflective functioning (Fonagy 1997), both of which are now thought to be central to the infant's capacity to develop a secure attachment to the primary caregiver (Van IJzendoorn 1995; Grienenberger 2005). Parental psychosocial functioning can impact on the parent's capacity to provide this type of parenting. For example, one study found that depressed mothers were less sensitively attuned to their infants, less affirming and more negating of infant experience compared with parents not experiencing postnatal depression (Murray 1992); and that these infants had poorer cognitive outcomes at 18 months (Murray 1996), performed less well on object concept tasks, were more insecurely attached to their mothers and showed more behavioural difficulties (Murray 1996). Boys of postnatally depressed mothers may also score lower on standardised tests of intellectual attainment (Sharp 1995). A clinical diagnosis of postnatal depression is associated with a fourfold increase in risk of psychiatric diagnosis at age 11 years (Pawlby 2008). Recent research has also identified that the impact of postnatal depression on insecure child attachment may be moderated by maternal attachment state of mind (McMahon 2006). The chronicity of the depression appears to be a significant predictor, with depression lasting throughout the first 12 months being associated with poorer cognitive and psychomotor development for both boys and girls compared with no evidence of impact for brief periods of depression (Cornish 2008).
Recent research shows that paternal postnatal depression can have an effect that is similar in magnitude to that of maternal depression. Ramchandani 2008 showed that boys of fathers who were depressed during the postnatal period had an increased risk of conduct problems at age 3.5 years, and that boys of fathers who were depressed during both the prenatal and postnatal periods had the highest risks of subsequent psychopathology at 3.5 years and psychiatric diagnosis at seven years of age (Ramchandani 2008).
Neurodevelopmental research suggests that postnatal depression impacts the child's developing neurological system (Schore 2005). For example, one study found that infants of depressed mothers exhibited reduced left frontal electroencephalogram (EEG) activity (Dawson 1997). Parent‐infant interaction can also impact on the infant's stress regulatory system, one study showing that exposure to stress during the early postnatal period that was not mediated by sensitive parental caregiving had an impact on the infant's hypothalamic‐pituitary‐adrenocorticol (HPA) system (Gunnar 1994), which plays a major role in both the production and regulation of glucocorticoid cortisol in response to such stress.
Maternal anxiety during the postnatal period is also associated with poorer outcomes. For example, Beebe 2011 found that maternal anxiety biased the interaction toward interactive contingencies that were both heightened (vigilant) in some modalities and lowered (withdrawn) in others, as opposed to being in the 'mid‐range', which has been identified as optimal for later development, including secure attachment (Beebe 2011).
2. Mid‐childhood and adolescence
There is also evidence to show a significant impact of parental psychosocial functioning on older children. A review of longitudinal studies found that by the age of 20 years, children of affectively ill parents have a 40% chance of experiencing an episode of major depression and are more likely to exhibit general difficulties in functioning, including increased guilt and interpersonal difficulties such as problems with attachment (Beardslee 1998). More recently, maternal psychological distress has been identified as being a risk factor for conduct and emotional problems. Parry‐Langdon 2008 found that higher scores on the General Health Questionnaire (GHQ‐12) were an independent risk factor for conduct disorder (odds ratio (OR) 2.2) and for child emotional problems (OR 2.2). This OR increased to 3.5 for both emotional and behavioural problems where maternal scores on the GHQ‐12 were initially low and then subsequently increased.
One longitudinal study that focused on parental conflict found that adolescents' perceptions of typical interparental conflict directly predicted increases in depressive symptoms (particularly for girls) and aggressive behaviours (particularly for boys) over a period of a year, and that this was not mediated by parental style or quality (McGuinn 2004). This study found a significant impact on the wellbeing of adolescents who witnessed even 'normative' marital discord. Another aspect of parental psychosocial functioning is parental confidence, which has been shown to be strongly associated with parent‐child interactions that are characterised by inconsistency, guilt, detachment and anxiety (Martin 2000). One meta‐analysis also found that paternal depression was significantly related to internalising and externalising psychopathology in children, and to father‐child conflict (Kane 2004).
It is suggested that the mechanism linking parental psychosocial functioning and child outcomes is the impact of such functioning on parenting behaviours, and Waylen 2010 found that worsening parental mental health was associated with reduced parenting capacity. Similarly, Wilson 2010 found a significant deleterious impact of paternal depression on both positive and negative parenting behaviours. One longitudinal study also suggested a more complex pathway in which parental depressive symptoms were associated 12 months later with increased insecurity in adult close relationships and interparental conflict (Shelton 2008). This study showed that such conflict had a negative impact on children's appraisals of parents, which was in turn was associated with children's internalising and externalising problems (Shelton 2008).
Overall, this evidence suggests that parental psychosocial functioning can impact on the parents' capacity to provide affectively attuned interaction during infancy and toddlerhood, and an impact on older children as a result of the consequences of compromised parental psychosocial functioning for parenting behaviours and marital adjustment.There is, therefore, considerable potential for interventions aimed at promoting the psychosocial wellbeing of parents to reduce the disruption to the child's emotional, educational and social adjustment, and thereby to promote the mental health of future generations.
Description of the intervention
Parenting programmes are underpinned by a range of theoretical approaches (including behavioural, cognitive‐behavioural, family systems, Adlerian) and can involve the use of a range of techniques in their delivery including discussion, role play, watching video vignettes and homework. Behavioural parenting programmes are based on social learning principles and teach parents how to use a range of basic behavioural strategies for managing children’s behaviour, and some of these programmes involve the use of videotape modelling. Cognitive parenting programmes are aimed at helping parents to identify and change distorted patterns of belief or thought that may be influencing their behaviour, and cognitive‐behavioural programmes combine elements of both types of strategy. Other types of programme often combine some of these strategies. For example, Adlerian programmes focus on the use of 'natural and logical consequences' and 'reflective listening' strategies.
Parenting programmes are typically offered to parents over the course of eight to 12 weeks, for about one to two hours each week. They can be delivered on a one‐to‐one basis or to groups of parents and are provided in a number of settings, ranging from hospital or social work clinics to community‐based settings such as general practitioner (GP) surgeries, schools and churches. They typically involve the use of a manualised and standardised programme or curriculum, and are aimed at increasing the knowledge, skills and understanding of parents.
Recent evidence shows that parenting programmes can improve the emotional and behavioural adjustment of children under three years (Barlow 2010) and of children aged three to 10 years with conduct and behaviour problems (Dretze 2005). A review of studies focused on teenage parents found that parenting programmes improved parental responsiveness to the child and parent‐child interaction (Barlow 2011). Reviews of qualitative evidence point to a range of benefits of taking part in a group with other parents (Kane 2003).
How the intervention might work
The mechanism by which parenting programmes may impact on parental psychosocial wellbeing is thought to be twofold. Firstly, parenting programmes are, on the whole, strengths‐based, and are aimed at enhancing parental capacity and changing parenting attitudes and practices in a non‐judgemental and supportive manner, with the overall aim of improving child emotional and behavioural adjustment. For example, Patterson’s coercion theory (Patterson 1992) demonstrates the way in which parents are increasingly disempowered as a result of a process of escalation in which parents who 'give in' to child demands are increasingly likely to need more coercive strategies on the next occasion. The process in which problems escalate and parents feel increasingly disempowered may explain in part why parents experience stress and depression directly related to the parenting role.The potential impact of parenting programmes on parental psychosocial functioning may be due to the way in which such programmes help parents to address significant issues in terms of their child's wellbeing, and increase their skills and capacity to support their child's physical and emotional development (for example, Dretze 2005; Barlow 2011).
Secondly, many parenting programmes, particularly those that are underpinned by a cognitive or cognitive‐behavioural approach, may also provide parents with strategies that are directly aimed at improving parental psychological functioning. Any improvements that occur may be a result of the parents' application of such strategies to themselves instead of, or in addition to, the use of strategies focused on improving child behaviour.
Research also suggests that parenting programmes can improve other aspects of parental psychosocial functioning such as marital relations and parenting stress (Todres 1993). Factors such as marital conflict and parental stress can have a direct impact on children, in addition to being mediators of other parental problems (for example, poor mental health). Improvements in marital conflict and parental stress will, as such, have beneficial consequences in terms of children's later development.
Thus, although a number of studies have shown that parenting programmes can have an impact on aspects of maternal mental health and wellbeing, including reducing anxiety (Morawska 2009) and depression (Pisterman 1992a), it is not currently clear whether such improvements reflect the impact of strategies directly targeting parental mental health or whether they occur as an indirect result of the parent's improved ability to manage their children's behaviour and of improvements in family functioning more generally.
Therefore, although the causal mechanism is not entirely clear, parenting programmes appear to have considerable potential to impact one or more aspects of parental psychosocial functioning. It should be noted, however, that although parents who are experiencing anxiety and depression unrelated to the parenting role may also have a compromised ability to function as a parent, with consequences in terms of their children's wellbeing. The needs of such parents are not addressed by the current review, which does not include programmes provided to parents with clinical mental health or psychiatric problems.
Why it is important to do this review
The aim of this review is to evaluate the effectiveness of group‐based parenting programmes in improving the psychosocial health of parents, by appraising and collating evidence from existing studies that have used rigorous methodological designs and a range of standardised outcome instruments. The results will inform the broader debate concerning the role and effectiveness of parenting programmes.
Objectives
To update an existing review examining the effectiveness of group‐based parenting programmes in improving parental psychosocial health (for example, anxiety, depressive symptoms, self‐esteem).
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐randomised controlled trials in which participants had been randomly allocated to an experimental or a control group, the latter being a waiting‐list, no treatment, treatment as usual (normal service provision) or a placebo control group.
Quasi‐randomised controlled trials are defined as trials where allocation was done on the basis of a pseudo‐random sequence, for example, odd or even hospital number, date of birth or alternation (Higgins 2008).
We did not include studies comparing two different therapeutic modalities (that is, without a control group).
Types of participants
We included studies that targeted adult (rather than teenage) parents (including mothers, fathers, grandparents, foster parents, adoptive parents or guardians) from either population or clinical samples (that is, with or without child behavioural problems) with parental responsibility for the day‐to‐day care of children, and who were eligible to take part in a parent training programme aimed at helping them to address some aspect of parental functioning (for example, attitudes and behaviour).
We included studies of parenting programmes delivered to all parents, not just those at risk of poor psychosocial health and child behavioural problems. Although we are addressing the impact of parenting programmes on aspects of parental psychosocial functioning such as anxiety and depression, we excluded studies that explicitly targeted and thereby focused solely on parents with a diagnosed psychiatric disorder, for example, clinical depression. This reflects the fact that parenting programmes are primarily provided to address children's social, emotional and behavioural functioning, and although parents with clinical psychiatric conditions may benefit from a parenting programme, these would not typically be provided as the primary source of treatment. Parents with clinical psychiatric conditions should be the focus of a separate review.
We included studies of parents who had children with a disability if the intervention was aimed at supporting or changing parenting and the study also measured parental psychosocial health.
We excluded studies that focused solely on child outcomes, preparation of parents for parenthood or that were directed at pregnant or parenting teenagers (below the age of 20 years).
Types of interventions
We included parenting programmes meeting the following criteria:
group‐based format;
standardised or manualised programme;
any theoretical framework including behavioural, cognitive and cognitive‐behavioural (please see Description of the intervention);
developed largely with the intention of helping parents to manage children's behaviour and improve family functioning and relationships.
We excluded programmes:
provided to parents on an individual or self‐administered basis;
that involved direct work with children;
that involved other types of service provision, such as home visits;
in studies that included only measures of parental attitudes (for example, Parental Attitude Test) or of family functioning (for example, McMaster Family Assessment Device) because, although these may reflect the family's functioning as a group, they are not direct measures of parental psychosocial health.
Types of outcome measures
Primary outcomes
Outcomes measured using standardised instruments including the measures detailed below.
Depressive symptoms
Parental depressive symptoms measured, for example, through improvement in scores on the Beck Depression Inventory (BDI) (Beck 1961) or similar standardised instrument.
Anxiety symptoms
Parental anxiety measured, for example, through improvement in scores on the Beck Anxiety Inventory (BAI) (Beck 1988) or similar standardised instrument.
Stress
Parental stress measured, for example, through improvement in scores on the Parenting Stress Index (PSI) (Abidin 1983) or similar standardised instrument.
Self‐esteem
Parental self‐esteem measured, for example, through improvement in scores on the Rosenberg Self‐Esteem scale (RSE) (Rosenberg 1965) or similar standardised instrument.
Anger
Parental anger measured, for example, through improvement in scores on the Brief Anger‐Aggression Questionnaire (BAAQ) (Maiuro 1987) or similar standardised instrument.
Aggression
Parental aggression measured, for example, through improvement in scores on the Brief Anger‐Aggression Questionnaire (BAAQ) (Maiuro 1987) or similar standardised instrument.
Guilt
Parental guilt measured, for example, through improvement in scores on the Situation of Guilt Scale or similar (SGS) (Klass 1987) or similar standardised instrument.
Secondary outcomes
Confidence
Parental confidence measured through improvement in scores on the Parent Sense of Competence Scale (PSC) (Johnston 1989) or similar standardised instrument.
Partner satisfaction
Marital or partner satisfaction measured through improvement in scores on the Dyadic Adjustment Scale (DAS) (Spanier 1976) or similar standardised instrument.
Adverse effects
Any adverse effects relating to parental psychosocial health including, for example, increase in tension between parents.
Search methods for identification of studies
Electronic searches
The previous version of this review was based on searches run in 2002. This update is based on searches run in 2008, 2010 and 2011. We added the metaRegister of Controlled Trials to search for completed and ongoing trials. We could not update the searches in SPECTR or the National Research Register because they had ceased to exist by 2008. Since the previous version of the review, Sociological Abstracts replaced Sociofile and PsycINFO replaced PsycLIT. During the update, ERIC and Sociological Abstracts moved to new search platforms and the original search strategies were adapted accordingly. All search strategies used for this update are reported in Appendix 1.
We searched the following electronic databases.
Cochrane Central Register of Controled Trials (CENTRAL), part of the Cochrane Library (2011, Issue 4), last searched 5 December 2011.
MEDLINE (Ovid) 1950 to November 2011, last searched 5 December 2011.
EMBASE (Ovid) 1980 to 2011 Week 48, last searched 5 December 2011.
CINAHL (EBSCO) 1982 to current, last searched 5 December 2011.
BIOSIS 1970 to 2 December 2011, last searched 5 December 2011.
PsycINFO 1970 to week 5 November 2011, last searched 5 December 2011.
Sociological Abstracts (Proquest), 1952 to current, last searched 5 December 2011.
Sociological Abstracts (CSA), 1963 to current, last searched March 2010.
Social Science Citation Index, 1956 to 2 December 2011, last searched 5 December 2011.
ASSIA 1980 to current, last searched 10 November 2011.
ERIC (via www.eric.ed.gov), 1966 to current, last searched 7 December 2011.
ERIC (via OVID), 1966 to current, last searched March 2010.
Searching other resources
NSPCC library database (last searched 5 December 2011).
metaRegister of Controlled Trials (last searched 5 December 2011).
Reference lists of articles identified through database searches were examined for further relevant studies. We also examined bibliographies of systematic and non‐systematic review articles to identify relevant studies.
Data collection and analysis
Selection of studies
For the first published versions of this review (Barlow 2001; Barlow 2003), we identified titles and abstracts of studies through searches of electronic databases and reviewed the results to determine whether the studies that appeared relevant met the inclusion criteria. For the original review Esther Coren (EC) identified titles and abstracts and these were screened by EC and JB. Two review authors (EC and JB) independently assessed full copies of papers that appeared to meet the inclusion criteria. We resolved uncertainties concerning the appropriateness of studies for inclusion in the review through consultation with a third review author, Sarah Stewart‐Brown (SS‐B). For the update of the review, Nadja Smailagic (NS) and Nick Huband (NH) carried out the eligibility assessments in consultation with JB and Cathy Bennett (CB). JB had overall responsibility for the inclusion or exclusion of studies in this review.
Data extraction and management
Two review authors extracted data independently (JB and EC or SS‐B; later NS and NH) using a data extraction form and entered the data into Review Manager 5 (RevMan) (RevMan 2011). Where data were not available in the published trial reports, we contacted trial investigators to supply missing information.
Some of the standardised measures used in the studies included in this review are reversed, such that a high score is considered to represent an improvement in outcome. We investigated whether the study investigators had used any methods to correct for this, for example, by reversing the direction of the scale by multiplying the mean values by ‐1 or by subtracting the mean from the maximum possible for the scale, to ensure that all the scales pointed in the same direction. For data entry into RevMan, we consistently multiplied the mean values by ‐1 for those scales where a higher score implies lower disease severity, unless this correction had already been made in the published report. Where there was ambiguity about the method of correction, we contacted the study investigators for further information.
Timing of outcome assessment
We extracted data for the following time points:
post‐intervention assessment, immediately post‐intervention (up to one month following the delivery of the intervention);
short‐term follow‐up assessment, two to six months post‐intervention;
long‐term follow‐up assessment, more than six months post‐intervention.
Assessment of risk of bias in included studies
For each included study, three review authors (NH, NS and HJ) independently completed the Cochrane Collaboration’s tool for assessing risk of bias (Higgins 2008, Section 8.5.1). Any disagreement was resolved in consultation with a third review author (CB). We assessed the degree to which:
the allocation sequence was adequately generated (‘sequence generation’);
the allocation was adequately concealed (‘allocation concealment’);
knowledge of the allocated interventions was adequately prevented during the study (‘blinding’);
incomplete outcome data were adequately addressed;
reports of the study were free of suggestion of selective outcome reporting;
the study was apparently free of other problems that could put it at high risk of bias.
Each domain was allocated one of three possible categories for each of the included studies: low risk of bias, high risk of bias, or 'unclear risk' where the risk of bias was uncertain or unknown.
The first published version of this review used a quality assessment method that we elected not to use in this updated review, instead following guidance from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) concerning the assessment of risk of bias.
Measures of treatment effect
For continuous data that were reported using standardised scales, we calculated a standardised mean difference (effect size) by subtracting the mean post‐intervention scores for the intervention and control groups and dividing by the pooled standard deviation.
Unit of analysis issues
Cluster‐randomised trials
The randomisation of clusters can result in an overestimate of the precision of the results (with a higher risk of a Type I error) where their use has not been compensated for in the analysis. Some meta‐analyses involved combining data from cluster‐randomised trials with data from individually‐randomised trials. Five of the included studies were cluster‐randomised (Wolfson 1992; Gross 2003; Hiscock 2008; Gross 2009; Hanisch 2010). The impact of the cluster RCTs was explored using a sensitivity analysis (see Sensitivity analysis, below) and we made no adjustments to the data.
Cross‐over trials
None of the included studies involved cross‐over randomisation.
Multi‐arm trials
Eleven studies utilised more than one intervention group (Sirbu 1978; Webster Stratton 1988; Spaccerelli 1992; Blakemore 1993; Cunningham 1995; Greaves 1997; Taylor 1998; Gross 2003; Gallart 2005; Gutierrez 2007; Larsson 2009). None of the interventions in these studies were sufficiently similar to be combined to create a single pair‐wise comparison, therefore for studies where there was more than one active intervention and only one control group, we selected the intervention that most closely matched our inclusion criteria and excluded the others. In only one study (Gutierrez 2007) was it possible to include both intervention arms in the study without double counting, as a result of the use of a second control group. Gutierrez 2007 compared two parenting programmes: the 1‐2‐3 Magic Program (classified as behavioural parenting program in our review) and the STEP program (Adlerian, assigned to 'other' types of parenting in our review) against attention placebo (where parents received lectures on topics of interest unrelated to parenting) or a wait‐list control condition. In our analyses we compared the behavioural parenting program with the wait‐list control group and the STEP program with the attention placebo group.
Dealing with missing data
We assessed missing data and dropouts for each included study and we report the number of participants who were included in the final analysis as a proportion of all participants in each study. We provide reasons for missing data in the 'Risk of bias' tables of the 'Characteristics of included studies' section.
We attempted to contact the trial investigators to request missing data and information.
Assessment of heterogeneity
We assessed the extent of between‐trial differences and the consistency of results of meta‐analyses in three ways. We assessed the extent to which there were between‐study differences, including the extent to which there were variations in the population group or clinical intervention, or both. We combined studies only if the between‐study differences were minor.
We assessed heterogeneity using the I2 statistic. The importance of the observed value of I2 is dependent on the magnitude and direction of effects and strength of evidence for heterogeneity (for example, P value from the Chi2 test, or a confidence interval for I2) (Higgins 2008), and we interpreted I2 > 50% as evidence of substantial heterogeneity. We also performed the Chi2 test of heterogeneity (where a significance level less than 0.10 was interpreted as evidence of heterogeneity). We used a random‐effects model as the standard approach and identified significant heterogeneity using subgroup analyses.
Data synthesis
The included studies used a range of standardised instruments to measure similar outcomes. For example, depression was measured using the Beck Depression Inventory, the Irritability, Depression and Anxiety Scale and the Centre for Epidemiological Studies Depression Scale. We standardised the results from these different measures by calculating the treatment effect for each outcome in each study and dividing the mean difference in post‐intervention scores for the intervention and treatment groups by the pooled standard deviation to produce an effect size. Where appropriate, we then combined the results in a meta‐analysis. The decision about whether to combine data in this way was determined by the levels of clinical and statistical heterogeneity present in the population, intervention and outcomes used in the primary studies.
We have presented the effect sizes and 95% confidence intervals for individual outcomes in individual studies using figures only and have not provided a narrative presentation of individual study results.
Subgroup analysis and investigation of heterogeneity
No subgroup analysis was undertaken because there was insufficient evidence of heterogeneity.
Sensitivity analysis
At the time of the first update of this review (2003), sensitivity analyses were conducted to assess the impact on the results of the two studies classified as quasi‐randomised. This was not repeated for the current update since both studies were reclassified as excluded. We conducted a sensitivity analysis to investigate the potential impact of cluster‐randomisation methods in five studies. We had planned an a priori sensitivity analyses for studies focusing on children with disabilities, but none of the included studies involved parents of disabled children.
Results
Description of studies
Results of the search
The updated electronic searches in January 2008, March 2010 and December 2011 produced 16,609 records. The obvious duplicates were removed by one review author (NS), who inspected the abstracts and discarded 16,477 irrelevant records. Most of articles reviewed were written in English. All studies in languages other than English had abstracts in English and we excluded all these studies on the basis of the information contained in the abstracts, apart from three German studies (Heinrichs 2006; Franz 2007; Naumann 2007), which are awaiting assessment as they need to be translated. We obtained a full text copy of 132 potential included studies and two review authors independently examined each study (NS and NH). JB and CB provided advice on any studies about which there was uncertainty.
Included studies
This updated review includes 48 studies, 28 of which were published since the previous review (Barlow 2003) that were identified using full text screening against inclusion criteria (Bradley 2003; Gross 2003; Martin 2003; Wolfe 2003; DeGarmo 2004; Farrar 2005; Feliciana 2005; Gallart 2005; Lipman 2005; Treacy 2005; Wang 2005; Chronis 2006; Gardner 2006; Fanning 2007; Fantuzzo 2007; Gutierrez 2007; Hutchings 2007; Matsumoto 2007; Turner 2007; van den Hoofdakker 2007; Hiscock 2008; Gross 2009; Larsson 2009; Morawska 2009; Niccols 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010). Two review authors (NS and NH) independently re‐examined the 26 studies included in the previous version of the review against the inclusion criteria and retained 20 of them in this review. Six previously included studies (Van Wyk 1983; Scott 1987; Anastopoulos 1993; Mullin 1994; Sheeber 1994; Zimmerman 1996) were excluded in this update because they did not meet the more rigorous inclusion criteria being applied (see Excluded studies for further details).
We have provided further details about the included studies in the Characteristics of included studies table.
Design
All 48 included studies were randomised controlled trials.
Most studies were two‐condition comparisons of group‐based parenting programmes against a control group (n = 37). Eleven studies utilised more than one intervention group (Sirbu 1978; Webster Stratton 1988; Spaccerelli 1992; Blakemore 1993; Cunningham 1995; Greaves 1997; Taylor 1998; Gross 2003; Gallart 2005; Gutierrez 2007; Larsson 2009). Gutierrez 2007 compared two parent education programmes (behavioural‐based and Adlerian) against two control groups, 'attention placebo' or a wait‐list control condition. In our analyses of data from this trial, we compared the behavioural parenting programme with the wait‐list control group and the Adlerian programme with the attention placebo group.
Seven studies used a no‐treatment control group (Gammon 1991; Schultz 1993; Gross 1995; Greaves 1997; Patterson 2002; DeGarmo 2004; Hanisch 2010); three studies used a treatment‐as‐usual control group (Fantuzzo 2007; van den Hoofdakker 2007; Hiscock 2008), and three studies used an attention placebo control group (Sirbu 1978; Farrar 2005; Gutierrez 2007). In Farrar 2005 the attention placebo group received information about choosing developmentally appropriate books for their pre‐school children; in Gutierrez 2007, which had two control conditions, participants in the 'attention placebo' group were either presented lectures on topics of interest to them, but unrelated to parenting, or assigned to a wait‐list control group. In Sirbu 1978, the attention placebo group did not utilise any materials or have a professional leader, and the sessions were unstructured. The remaining 35 studies used only a wait‐list control group.
Cluster‐randomised studies
Five studies were cluster‐randomised trials (Wolfson 1992; Gross 2003; Hiscock 2008; Gross 2009; Hanisch 2010). Gross 2003 used day centres as the unit of allocation; in total seven day centres were randomly assigned to one of the three conditions: ‘parent training plus teacher condition’ (n = 4); ‘teacher training condition’ (n = 4), and ‘control condition’ (n = 3). The control centres received no intervention for at least one year, after which new parents were recruited and the centres were transferred to the ‘parent training condition’ (n = 3). Hanisch 2010 used kindergartens as the unit of allocation: 58 kindergartens were randomised to the intervention group (n = 32) or to the control group (n = 26). Hiscock 2008 used primary‐care nursing centres as the unit of allocation: 40 centres were randomly assigned to the intervention group (n = 18) or to the control group (n = 22). Wolfson 1992 employed randomisation by childbirth class: 25 childbirth classes were randomised but no further details were given.
Sensitivity analysis
The randomisation of clusters can result in an overestimate of the precision of the results (with a higher risk of a Type I error) where their use has not been compensated for in the analysis. We therefore conducted a sensitivity analysis to investigate cluster effects. For this, we assumed the intracluster correlation to be 0.2, which is much bigger than normally expected. For two of the five cluster‐RCTs (Wolfson 1992; Hiscock 2008), we only had information about the number of clusters at randomisation and we therefore assumed a worst case scenario using the maximal possible cluster size, taking into account the dropouts during the study. Based on these assumptions, we assessed that the results of the meta‐analyses were robust to any clustering effects for most outcomes.
In the worst case scenario there is potential for the confidence interval to widen, depending on the weight of the clustered studies in the meta‐analysis. In cases where the effect size is borderline non‐significant (for example, analysis 1.1.2), there is potential for the meta‐analysis to become borderline significant after the adjustment. Conversely, there is potential for previous significance to be overcome following the adjustment.
In all analyses involving cluster‐corrected standard errors, the adjusted effect sizes were equivalent to the unadjusted effect sizes. In addition, in all cases the statistical conclusions were unchanged from the uncorrected to the corrected analyses.
Sample sizes
There was considerable variation in sample size between studies. Altogether the 49 included studies initially randomised 4937 participants, with sample sizes ranging from 22 to 733 (mean 102.9; median 60). Five large trials (Irvine 1999; Gross 2003; DeGarmo 2004; Hiscock 2008; Gross 2009) randomised a total of 1830 participants, with sample sizes ranging from 238 to 733 (mean 366; median 292). A further 11 studies (Webster Stratton 1988; Spaccerelli 1992; Cunningham 1995; Taylor 1998; Patterson 2002; Bradley 2003; Lipman 2005; Fantuzzo 2007; Hutchings 2007; Larsson 2009; Hanisch 2010) randomised 1481 participants, with sample sizes ranging from 110 to 198 (mean 134.6; median 126). The remaining 32 studies involved 1626 participants, with sample sizes ranging from 22 to 96 (mean 50.8; median 51).
Seven studies (Sirbu 1978; Gammon 1991; Spaccerelli 1992; Pisterman 1992b; Blakemore 1993; Schultz 1993; Bradley 2003) did not provide sufficient data to calculate effect sizes. The remaining 41 studies included in total 3416 participants with sample sizes ranging from 16 to 671 (mean 83.3; median 82).
Setting
Twenty‐two studies were conducted in the USA, 10 in Australia, seven in Canada and three in the UK. The remaining studies were conducted in China, Germany, Japan, the Netherlands and New Zealand. Most studies (n = 32) were single‐centre trials.
In 41 studies, participants were recruited from community settings by a variety of methods including flyers, emails and advertisements directed at parents of young children, or self‐referral (Sirbu 1978; Gammon 1991; Spaccerelli 1992; Wolfson 1992; Blakemore 1993; Nixon 1993; Schultz 1993; Gross 1995; Joyce 1995; Odom 1996; Greaves 1997; Taylor 1998; Webster Stratton 1988; Irvine 1999; McGillicuddy 2001; Nicholson 2002; Bradley 2003; Gross 2003; Martin 2003; Wolfe 2003; DeGarmo 2004; Farrar 2005; Feliciana 2005; Gallart 2005; Lipman 2005; Wang 2005; Chronis 2006; Gardner 2006; Fanning 2007; Fantuzzo 2007; Gutierrez 2007; Hutchings 2007; Matsumoto 2007; Turner 2007; Hiscock 2008; Gross 2009; Morawska 2009; Niccols 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); in one study from a primary care setting (Patterson 2002); in three studies from outpatient settings including an outpatient mental health clinic (van den Hoofdakker 2007), child psychiatric outpatients departments (Larsson 2009) and from a university‐based research clinic (Treacy 2005); in three studies parents were recruited from both community and outpatient settings (Pisterman 1992a; Pisterman 1992b; Cunningham 1995).
The intervention was delivered in outpatient clinics (including research clinics and paediatric outpatient departments) in seven studies (Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Taylor 1998; Treacy 2005; van den Hoofdakker 2007; Larsson 2009); in primary care in one study (Patterson 2002); and in the community in the remaining studies.
Participants
An inclusion criterion for this updated review was that participants were parents with responsibility for the day‐to‐day care of children. In 19 studies, both mothers and fathers were recruited (Webster Stratton 1988; Wolfson 1992; Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Nixon 1993; Schultz 1993; Gross 1995; Taylor 1998; Irvine 1999; McGillicuddy 2001; Wang 2005; Fanning 2007; Hutchings 2007; Matsumoto 2007; van den Hoofdakker 2007; Larsson 2009; Hanisch 2010; Matsumoto 2010). Thirteen studies recruited mothers only (Sirbu 1978; Gammon 1991; Odom 1996; Greaves 1997; Wolfe 2003; DeGarmo 2004; Farrar 2005; Feliciana 2005; Lipman 2005; Chronis 2006; Gutierrez 2007; Hiscock 2008; Niccols 2009). Either the mother or the father was recruited in 12 studies (Spaccerelli 1992; Cunningham 1995; Joyce 1995; Patterson 2002; Bradley 2003; Martin 2003; Gallart 2005; Gardner 2006; Fantuzzo 2007; Turner 2007; Morawska 2009; Joachim 2010). Four studies recruited not only biological parents but also grandparents, foster parents, step parents and relatives (Nicholson 2002; Gross 2003; Treacy 2005; Gross 2009). The studies included in this review were largely directed at mothers, and the trial investigators reported results that were mainly derived from the mothers.
Interventions
We provide a description by category of the structure and content of the parenting programmes that were evaluated in the included studies in 'Additional Table 1'. We have grouped the interventions into five categories according to the basic theoretical premise underpinning the programme (for example, behavioural and cognitive‐behavioural programmes) or, where there was a sufficient number of studies, according to the brand of the programme (Incredible Years and Triple‐P parenting programmes). A small group of programmes were unclassifiable (other and non‐branded multimodal programmes). For the purpose of analysis we categorised the studies as below.
1. Description of the parenting programmes.
| Study ID | Aim | Content/delivery |
| Behavioural only | ||
| Bradley 2003 | To evaluate the effects of a brief parenting programme on positive and negative parenting behaviours. | Brief behavioural parenting program consisted of three weekly 2‐hour group meetings with booster session 4 weeks after the third session. The intervention included video material (1‐2‐3 Magic) on managing difficult child behaviours, handouts and mutual support/problem solving work. |
| Cunningham 1995 | To examine the efficacy of a large group‐based parenting programme as a means of increasing the accessibility of such programmes to parents of children with disruptive behaviour; to determine whether parenting programme improve parental sense of competence and decrease depressive symptoms. | Coping modelling problem‐solving parenting programme comprised 11‐12 weekly sessions, involving the formulation of solutions through the observation of videotapes, discussion, modelling and role play. Homework reviewed each week. |
| DeGarmo 2004 | To evaluate changes in parent management and subsequently changes in child behaviour and maternal affects over time. | Parent Management Training (PMT) was a series of parent group meetings and discussion (14 weekly sessions). Interventionists made midweek telephone calls to encourage the participation. The program included a 30‐minute video, and covered 5 theoretically based effective parenting practices (appropriate discipline, skill encouragement, monitoring, problem solving, and positive reinforcement). Individual catch‐up sessions offered to replace missed sessions; 10% participants had at least one individual session. |
|
Gallart 2005 |
To evaluate the effectiveness of a parenting programme and assess the impact of telephone contact sessions in developing positive relationships, in encouraging desirable behaviour, in teaching new skills and behaviours, and in managing misbehaviour. | The full Group Triple‐P program comprised four weekly 2‐hour group sessions and four weekly follow‐up telephone calls. The programmes standard Facilitators Kit (leaders manual, AV materials, participants workbook) was used, plus a video (Every Parents Survival Guide). The modified Group Triple‐P program is the standard programme delivered as four weekly 2‐hour group sessions but without the four follow‐up telephone contacts. |
| Gutierrez 2007 (behavioural) | To evaluate the efficacy of two parenting programmes in reducing perceived parental stress | Behaviourally‐based parenting programme (BPP)1‐2‐3 Magic Parenting Program included components on parents reactions to their child's misbehaviour, using time‐out, dealing with testing and manipulation, positive reinforcement, and preventing relapses. see below for description of Adlerian parenting program. Compared two active parenting interventions with an attention placebo program and a wait‐list control group. Each programme consists of eight 2‐hours‐weekly sessions, delivered in Spanish. |
| Hanisch 2010 | To evaluate the effects of a parenting programme on child behaviour, parenting practices, parent‐child interaction, and parent quality of life | Prevention Programme for Externalising Problem behaviour (PEP) consisted of ten weekly sessions (80‐120 minutes each). The first three sessions focused on defining individual problem situations, introducing unspecific basic strategies. The next three sessions thought participants the classical key strategies of behaviour modification. Sessions 7 to 10 consolidated these strategies by working on common difficult parenting situations. Individual homework assessments and telephone supervision were provided. |
| Hiscock 2008 | To assess the effectiveness of a parenting programme in preventing early childhood behavioural problems |
The Universal parenting programme comprised of three structured sessions, covering normal development and behaviour, strategies to increase desired behaviour, and strategies to reduce unwanted behaviour. First session (child at 8 months) consisted of handouts; second and third sessions (child at 12 and 15 months) were 2‐hour group sessions. Training incorporated didactic teaching, written information, role play and video vignettes of appropriate parenting responses to childhood behaviours. |
| Joachim 2010 | To assess the effectiveness of a brief parent training in preventing behaviour problems on shopping trips. |
Brief, two‐hour, topic‐specific parent discussion group based on the Triple P‐Positive Parenting Program. Intervention entitled Hassle‐free Shopping was for parents looking for specific advice on how to manage their child's behaviour in the supermarket and how to prevent behaviour problems on shopping trips. |
| Irvine 1999 | To evaluate the effectiveness of a parenting programme provided by non‐mental health providers who are more likely to be available in small communities. |
Adolescent Transition Program was a stepwise, skill‐based curriculum designed to teach parenting skills. Content included: positive reinforcement, parental monitoring, limit‐setting, parent‐child communication, and problem solving. 12 weekly sessions (90 minutes‐2 hours each). Skills discussed in group then practiced at home with group feedback the following week. |
| Martin 2003 | To evaluate the effects of a parent training in managing parents successfully functioning at work, at home, and in their parenting role. |
Work Place Triple‐P program (WPTP) consisted of four sessions (2 hours each), and four additional individual telephone consultations (15 to 30 minutes each). It was designed specifically for delivering in the workplace and involved i) teaching parents 17 core positive parenting and child management strategy; ii) planning activities routine for times such as getting ready for work and arrival home from work; iii) active training methods such as video modelling, rehearsal, practice, feedback and goal setting Parents received copy of a workbook that included exercises for completion both in‐session and between sessions. |
| Matsumoto 2007 | To evaluate the efficacy and acceptability of a parenting programme with Japanese parents in learning and practicing positive parenting skills |
Triple P‐Positive Parenting Program comprised of five sessions (2‐hours each), and three telephone consultation sessions (20‐30 minutes each). Active skills training methods were used to facilitate the development of a self‐regulatory framework for parents, involving modelling, role‐plays, feedback and the use of specific homework. All sessions conducted in Japanese by a Japanese accredited Triple P trainer. |
| Matsumoto 2010 | To evaluate the efficacy and acceptability of a parenting programme with Japanese parents in Japanese society in learning and practicing positive parenting skills |
Triple P‐Positive Parenting Program comprised of five sessions (2‐hours each), and three telephone consultation sessions (20‐30 minutes each). Active skills training methods were used to facilitate the development of a self‐regulatory framework for parents, involving modelling, role‐plays, feedback and the use of specific homework. All sessions conducted in Japanese by a Japanese accredited Triple P trainer. |
| Morawska 2009 | To assess the efficacy of a parenting program in enhancing parenting skills, and subsequently in improving the behavioural and emotional adjustment of their gifted child. |
Gifted and Talented Group Triple P programme (based on the Group Triple P intervention) consisted of five weekly sessions (2 hours each), followed by three weekly telephone consultations (15‐minutes each), and a final 2 hours group session. The program involved teaching parents core child management skills: i) promoting children's development, ii) managing misbehaviour, and iii) planned activities and routines |
| Niccols 2009 | To evaluate the effectiveness of a parenting programme in preventing challenging behaviour of their child. | COPEing with toddler behaviour comprised eight weekly group sessions (2 hours each) and focused on parenting styles and strategies in preventing challenging behaviour for children in late infancy/toddlerhood. |
| Odom 1996 | To determine whether parent training would improve a mother's knowledge about ADHD and her feelings of competence and self‐esteem in using problem‐solving strategies. | Educational programme comprised five weekly sessions (60‐90 minutes each), including information on the pathology of ADHD, its impact on family, the effects of stimulant medication, the meaning and development of a child's behaviour, enhancing positive mother‐child attention, time‐out, positive reinforcement, and the use of problem‐solving strategies. Weekly written handouts compiled in a booklet. |
| Pisterman 1992a | To assess the effects of a parenting programme on parenting stress and sense of competence in parents of children with ADHD. |
Parent training programme comprised twelve weekly sessions, including information on ADHD and instruction involving role‐play, modelling and homework assignments. Compliance training component differed slightly for Study 1 and Study 2. Reading material and manuals provided for participants. |
|
Pisterman 1992b |
To evaluate whether a parent mediated behaviour intervention could ameliorate ADHD related deficits and behavioural problems. |
Attention‐training treatment programme comprised twelve weekly sessions, including educational material and information about ADHD, compliance training (behaviour management) and attention training. Teaching methods includes modelling, role‐play, and individual feedback to videotaped interactions. |
| Sirbu 1978 | To investigate the effectiveness of a behavioural parenting programme. To examine whether lecture/written materials/combination were differentially effective in teaching behavioural principles. | Behavioural parenting programme comprised five weekly sessions (2 hours each) and a This intervention was used in Group 1. Group 2 received the same programme but without the text. Group 3 received the text only plus the exercises. Group 4 were a non‐intervention control group. |
| Turner 2007 | To assess the impact of a culturally sensitive adaptation of parenting programme on parental skills, parental stress, anxiety and depression. | Triple‐P Positive Parenting Program, culturally adapted, comprised eight sessions: i) one group introduction session, giving an overview of the program and establishing rapport within the groups (1.5‐2 hours); ii) four group sessions (2‐2.5 hours each); iii) two home‐based consultations (30‐40 minutes each); and iv) one final group session (1.5‐2 hours). The intervention covers modelling, rehearsal, practice, feedback and goal setting, considering needs of Australian Indigenous families. |
| van den Hoofdakker 2007 | To investigate the effectiveness of parenting training as adjunct to routine clinical care in enhancing parenting skills. | Behavioural Parenting Training (BPT) comprised twelve sessions (2 hours each). The program covers the following parenting skills: i) structuring the environment, ii) setting rules, iii) giving instructions, iv) anticipating misbehaviours, v) communicating, vi) reinforcing positive behaviour, vii) ignoring, viii) employing punishment, and ix) implementing token system. As a part of homework assignment, for each session parents read a chapter of a book written for this program (van der Veen‐Mulders et al, 2001); they also practice parental skills during each session, and wrote the reports. |
| Wang 2005 | To evaluate the effects of a parenting program on the interactive skills of parents of children with autism. | Educational parenting program comprised four weekly sessions (4 hours each), supported by home visits (4 hours in total). Training program included lectures, handouts, live modelling and group discussion, which was supported by individual home visits. The purpose of the individual home visits was to observe the parent/child interaction in the natural environment and assist parents in applying the intervention strategies thought during group training. |
| Wolfson 1992 | To evaluate the effectiveness of a parenting programme in promoting healthy, self‐sufficient sleep in infants; to test the hypothesis that parent training would reduce both stress and response to child wakefulness. | Behavioural parenting training comprised two prenatal sessions and two post‐natal sessions (1‐1/2 hours each). Content included information on infant sleep and methods to assist in establishing early good sleep habits. Handouts, questions and answers, group discussion and problem‐solving strategy used. Diaries and daily practice records completed and discussed. |
| Cognitive‐Behavioural Parenting Programme | ||
|
Blakemore 1993 |
To evaluate the effectiveness of a parenting programme in enhancing the self‐directedness of children with ADHD and responsibility for their own behaviour. |
Behaviour management parenting programme consisted of 12 weekly 2‐hour sessions delivered using a lecture format. Follow‐up (maintenance) sessions at 3‐ and 6‐months. Optional school consultation time offered. Topics included the re‐framing of ADHD, behaviour management based on the use of various techniques, the grief cycle, communication skills, listening, acknowledging feelings, self‐esteem, and anger‐management. |
| Chronis 2006 | To examine whether a parenting programme improve maternal functioning in terms of depressive symptoms, anxiety, self‐esteem, perceived stress and cognitions about child behaviour. | Maternal Stress and Coping Group Program was a modified version of the Coping With Depression Course Program (CWDCP), which increases its relevance for mothers of children with ADHD. It comprised twelve weekly sessions, including four treatment models: i) relaxing training, ii) increasing pleasurable activities, iii) cognitive restructuring, and iv) increasing social skills/assertiveness training. Homework exercises that involved practising behavioural skills were completed. |
| Gammon 1991 | To examine the effectiveness of a parenting programme in promoting coping skills in parents of children with developmental disabilities. | Coping Skills Training Programme consisted of ten 2‐hour weekly sessions, involving cognitive restructuring, interpersonal skills training, problem solving and individual goal attainment. |
| Gardner 2006 | To examine the effectiveness of a parenting programme in reducing child conduct problem, in enhancing positive parenting skills and confidence, and in decreasing parental depression |
Webster‐Stratton Incredible Years intervention comprised a video‐based 14‐week group programme which teaches behavioural principles for managing behaviours using a collaborative, practical problem‐solving approach. Topics included parent‐child play praise, incentives, limit‐setting, problem‐solving and discipline. Each week parents practice tasks at home. Telephone calls made to encourage progress. |
| Gross 1995 | To evaluate the effectiveness of a parenting programme in promoting positive parent‐child relationships; to promote parental self‐efficacy. | Parent and Children Series (PACS) training programme for promoting positive parent‐child relationship consisted of 10‐weekly sessions, using manual, written materials and videos. Topics included: how to play with a child, use of praise, limit setting, use of time‐out. Video‐tape vignettes used to model skills and stimulate discussion. Weekly homework assignments used. |
| Gross 2003 | To evaluate the relative effectiveness of a parenting programme on parenting competence (higher parenting self‐efficacy, less reliance on coercive discipline strategies, and more positive parent behaviour) | Webster‐Stratton Incredible Years BASIC Programme comprised 12 weekly sessions (2 hours each). Topics covered included child‐directed play, helping young children to learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. Home work assignments were also used. The course was taught using video vignettes which were appropriate for toddlers. |
| Gross 2009 | To evaluate the effectiveness of a parenting programme in improving parenting competence and child behaviour. | Chicago Parent Programme (CPP) comprised 12 weekly sessions, employing videotaped vignettes and group discussion. The topics covered the concept of child‐centred time, helping young children to learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. |
| Greaves 1997 | To assess the effectiveness of a parenting programme in reducing parental stress in parents of children with disabilities. | Rational‐Emotive Parent Education programme comprised eight weekly sessions. Content focused on core irrational beliefs and links with stress response. Programme thought the disputation of these beliefs and their replacement with rational beliefs. Teaching based on a didactic approach and included homework, completion of worksheets, and the distribution of a prepared summary sheet. |
| Hutchings 2007 | To evaluate the effectiveness of a parenting programme as a preventative intervention for parents with children considered to be at risk of developing conduct disorder | Webster‐Stratton Incredible Years Basic parenting programme comprised twelve weekly sessions (2 to 2.5 hours each) and promoted positive parenting, using a collaborative approach (for example: role play, modelling, discussion, etc). |
| Joyce 1995 | To evaluate the effectiveness of a parenting programme in reducing levels of parent irrationality, negative emotions, and to assess whether the change in irrationality is correlated with changes in emotionality. | Rational‐Emotive based Parent Education programme comprised nine weekly sessions Content focused on identifying and disputing parental irrational beliefs that lead to emotional stress; the reinforcement of rational beliefs; rational problem‐solving; teaching children rational personality traits. |
| Larsson 2009 | To examine the efficacy of a parenting programme in reducing child conducts problems. |
Webster‐Stratton Incredible Years Basic parenting programme consisted of twelve to fourteen weekly sessions (2 hours each), focusing on positive disciplinary strategies, effective parenting skills, strategies coping with stress, and ways to strengthen children's social skills. Video vignettes for discussion, role play, rehearsals and home work assessments used. |
| Lipman 2005 | To evaluate the effects of a community group‐based parenting programme on vulnerable single mothers in improving maternal wellbeing (mood, self‐esteem and social support) and parenting. | Social support and education parenting programme consisted of 10 weekly group sessions (1.5 hours each). The program covered two thematic areas: i) child related area (for example: child development and behaviour, behaviour management, school involvement, child welfare agencies), and maternal area (for example: social isolation, stress and coping, personal care and development, relationships, grief). Cognitive behavioural techniques and structured counselling were provided. |
| McGillicuddy 2001 | To examine the effectiveness of a coping skill training programme for parents of substance‐abusing adolescents |
Behavioural‐analytic parenting programme comprised eight weekly sessions (2 hours each). Aims were to teach participants more effective skills for coping with problems resulting from their adolescent's substance abuse. |
| Nicholson 2002 | To examine the effectiveness of a parenting programme with at‐risk parents of young children. | Psycho‐educational programme STAR (Stop Think Ask Respond) comprised 10 weekly sessions (1.5 hours each), employing 'segments' in which parents learned thoughtful ways to respond to children, how to have realistic expectations of children, and how to implement positive parenting and discipline strategies. |
| Nixon 1993 | To examine the effect of a short‐term intervention to reduce self‐blame and guilt in parents of children with severe disabilities. |
Cognitive‐behavioural parenting programme comprised five weekly sessions (2 hours each). Content delivered using a lecture format. Homework assigned each week consisted of monitoring automatic thoughts, cognitive distortions, negative feelings, and attempts at cognitive restructuring. Sessions focused on the cognitive distortions that contribute to self‐blame and guilt in families of children with disabilities, and techniques to deal with such distortions. |
|
Patterson 2002 |
To assess effects of a parenting programme delivered by health visitors in primary care in improving mental health of children and parents | Webster Stratton parenting programme comprised 10 weekly sessions (2 hours each). The sessions included video vignettes of parent‐child interactions, group discussion, role play, rehearsal of parenting techniques, and home practice. |
| Spaccerelli 1992 | To evaluate the additional benefit of providing a problem‐solving parenting intervention in improving parental and child behaviour. | Problem‐solving skills parenting training comprised 6 units (1 hour each), focusing on aspects of problem‐solving including: problem definition, goal setting, alternative solutions, and decision‐making. This training was used as a supplement to a 10‐hour Parent and Children Series (PACS) programme based on the work of Webster‐Stratton. Topics included how to play with a child, use of praise, limit setting, use of time‐out. Video‐tape vignettes used to model skills and stimulate discussion. Written materials and homework assignments used. |
| Taylor 1998 | To evaluate the effectiveness of parent training in reducing parental psychosocial difficulties and conduct problems in children. | Parent and Children Series (PACS) treatment intervention consisted of 11‐14 weekly sessions (2 ¼ each), using manual, written materials and videos. |
| Webster Stratton 1988 | To compare different treatment modes in reducing parental stress and improving child behaviour. |
GDVM: Group‐based video‐tape modelling parenting skills followed by discussion. IVM: Weekly in‐clinic sessions for approximately 1‐hour viewing of self‐administered videotape without therapist or discussion. GD: Weekly therapist‐led discussion sessions covering same topics as other groups. All modes of delivery comprised 10‐12 weekly sessions (2 hours each). Content, sequencing and number of sessions constant between groups. Topics covered play skills, praises, rewards, discipline and problem‐solving approaches |
| Other or multimodal | ||
| Fanning 2007 | To investigate the feasibility, implementation, and potential effects of a parenting programme on positive changes in parenting stress and child behaviour. | Success in Parenting Preschoolers (SIP) programme consisted of 8 weekly group sessions, each lasted 2 hours. The programme included both language facilitation techniques and behaviour management strategies. The parents viewed 100 instructional pages, watched four video vignettes, and received weekly session outlines, handouts, and home reminder magnets highlighting specific parenting skills presented during that weekly session. Additional weekly phone sessions were provided. All group sessions were videotaped. |
| Fantuzzo 2007 | To evaluate the effectiveness of a community‐based intervention on enhancing pro‐social interaction and psychological wellbeing of urban, Head Start parents. |
The COPE (Community Outreach through Parent Empowerment) intervention has two components: (a) informal support groups, and (b) implementation of the Parent as Change Agent for Self module. Involved 10 group‐training sessions (each ˜3 hrs) focusing on the relationship between stress and social support. The 10 sessions had two main purposes: to identify major categories of stressful events for urban, African‐American Head Start parents, and to consider and discuss the ways in which friendships and various connections within the community can mitigate these stressors. |
| Farrar 2005 | To examine the effect of a parenting intervention on parental stress scores. | A brief cognitively‐based group parenting training is a 30‐minute single‐session, which targeted mothers perception of a preschool‐age child. The session focused on shifting parent perception of the child. Parents learned about the connection between thoughts, feelings and behaviours. Duration of the training was in total 1.5 hours with questionnaire completion. Sessions were audio‐taped. Attention‐placebo control group received information regarding [use of] developmentally appropriate books for preschool age children during 30 minutes. The session (1.5 hours) involved questionnaire completion. |
| Feliciana 2005 | To examine the effects of a parenting programme on maternal sense of competency and stress | Active Parenting Programme was an educational programme and consisted of sessions (11/2 hours each). Content focused on understanding children's behaviour and misbehaviour, responsible parenting, effective communication and discipline, and developing responsibility in children. The training format used a variety of teaching techniques including lecture, videos, group discussion, and role‐play. |
| Gutierrez 2007 (Adlerian) | To evaluate the efficacy of two parenting programmes in reducing perceived parental stress | Adlerian‐based parenting programme (APP) is the Systematic Training for Effective Parenting (STEP) program which included components on understanding yourself and your child, beliefs and feelings, encouraging your child and yourself, listening and talking to your child and problem solving. Each programme consists of eight 2 hour weekly sessions, delivered in Spanish. |
| Schultz 1993 | To evaluate the effectiveness of a parenting programme in empowering parents to strengthen family resources. | Model based on a three‐tiered approach to developing personal coping and social support. Designed to strengthen interpersonal, intrapersonal and social resources by means of group work, discussion and didactic input. Topics included: family dynamics, loss and grief, communication and conflict resolution, networking and resource utilisation, stress management and relaxation skills. 12 2‐hourly sessions over 6 weeks. |
| Treacy 2005 | To assess the effectiveness of a parenting programme in reducing parenting stress, and in improving parental mood, family functioning, parenting style, locus of control, and perceived social support of children with ADHD. | Parent Stress Management (PSM) training program comprised nine weekly sessions (2 hour each). The program covered: Session 1: Orientation to the program and understanding stress; Session 2: Education about ADHD; Session 3: Rights and reasons; Session 4: Problem‐solving skills; Session 5: Cognitive restructuring; Session 6: Communication skills; Session 7: Self‐care skills; Session 8: Parenting skills; Session 9: Wrap‐up session. |
| Wolfe 2003 | To evaluate the effects of a parenting programme in enhancing parent adaptive behaviour through emphasis on parental self‐reflection, social support and the emotional roots of children's misbehaviour and parenting stress. | Study 1 ‐ Counselling and social support parent programme. Listening to Children (LTC) parent training comprised eight weekly sessions (2.5 hours each) and was based on re‐evaluation counselling. It focused on the three core themes: recognising the effects of parents own childhood experience, spending special time with children, and understanding and handling children's emotions and upsets. Each session involved in‐class activities, reading assignments, and homework projects built around those themes. |
i) Behavioural parenting programmes
Twenty‐two studies evaluated the effectiveness of a behavioural parenting programme (Sirbu 1978; Wolfson 1992; Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Cunningham 1995; Odom 1996; Irvine 1999; DeGarmo 2004; Wang 2005; Gutierrez 2007; van den Hoofdakker 2007; Hiscock 2008; Niccols 2009; Hanisch 2010; Martin 2003; Gallart 2005; Matsumoto 2007; Turner 2007; Morawska 2009; Joachim 2010; Matsumoto 2010). This category included programmes which are primarily behavioural in orientation and that are based on social learning principles. These programmes teach parents how to use a range of basic behavioural strategies for managing children’s behaviour. Triple‐P programmes are included in this category.
ii) Cognitive‐behavioural parenting programmes
Nineteen studies evaluated the effectiveness of a cognitive‐behavioural parenting programme (Webster Stratton 1988; Gammon 1991; Spaccerelli 1992; Blakemore 1993; Nixon 1993; Gross 1995; Joyce 1995; Greaves 1997; Taylor 1998; McGillicuddy 2001; Nicholson 2002; Patterson 2002; Gross 2003; Lipman 2005; Chronis 2006; Gardner 2006; Hutchings 2007; Gross 2009; Larsson 2009). These programmes combined the basic behavioural type strategies with cognitive strategies aimed at helping parents to identify and change distorted patterns of belief or thought that may be influencing their behaviour. Webster‐Stratton Incredible Years programmes were included in this category.
iii) Other and multimodal
It was not possible to classify the interventions from eight studies (Schultz 1993; Wolfe 2003; Farrar 2005; Feliciana 2005; Treacy 2005; Fanning 2007; Fantuzzo 2007; Gutierrez 2007) based on the information provided. See Table 1 for further information about these programmes.
Duration of the intervention
We have described the duration of the intervention as 'standard' in 36 studies (8 to 14 sessions), 'brief' in 10 studies (1 to 6 sessions) and 'long' in two studies (16 weeks or more).
Outcomes
All outcomes were parent‐report and involved the use of a variety of standardised instruments. We assessed outcomes at three time points: immediately post‐intervention (up to one month following the delivery of the intervention), short‐term follow‐up (two to six months post‐intervention) and long‐term follow‐up (more than six months post‐intervention).
Primary outcome measures
Depressive symptoms
Twenty‐nine studies assessed the impact of a parent training programme on parental depressive symptoms. Nine studies used the Beck Depression Inventory (Nixon 1993; Cunningham 1995; Taylor 1998; Irvine 1999; McGillicuddy 2001; Treacy 2005; Chronis 2006; Gardner 2006; Hutchings 2007); nine studies used the Depression Anxiety Stress Scale (Martin 2003; Gallart 2005; Matsumoto 2007; Turner 2007; Hiscock 2008; Morawska 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); six studies used the Center for Epidemiological Studies Depression scale (Gross 1995; Gross 2003; DeGarmo 2004; Lipman 2005; Gross 2009; Niccols 2009); three studies used the Parent Stress Index (Pisterman 1992a; Greaves 1997; Feliciana 2005); Patterson 2002 used the General Health Questionnaire; and Bradley 2003 used the Irritability Depression Anxiety Scale.
Anxiety symptoms
Thirteen studies measured parental anxiety. Most studies (n = 8) used the Depression Anxiety Stress Scale (Martin 2003; Gallart 2005; Matsumoto 2007; Hiscock 2008; Morawska 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); one study used the State‐Trait Anxiety Inventory (Joyce 1995); one study (McGillicuddy 2001) used the Brief Symptom Inventory; one (Patterson 2002) used the General Health Questionnaire; and one (Chronis 2006) used the Beck Anxiety Inventory.
Stress
Almost three‐quarters (n = 36) of included studies assessed parental stress using nine scales. Seventeen studies used the Parenting Stress Index (Webster Stratton 1988; Spaccerelli 1992; Pisterman 1992a; Pisterman 1992b; Blakemore 1993; Gross 1995; Greaves 1997; Nicholson 2002; Patterson 2002; Wolfe 2003; Feliciana 2005; Treacy 2005; Wang 2005; Gutierrez 2007; Hutchings 2007; van den Hoofdakker 2007; Larsson 2009); nine studies used the Depression Anxiety Stress Scale (Martin 2003; Gallart 2005; Matsumoto 2007; Turner 2007; Hiscock 2008; Morawska 2009; Hanisch 2010; Joachim 2010; Matsumoto 2010); two studies used the Every Day Stress Index (Gross 2003; Gross 2009); two studies used the modified Uplifts and Hassles Scale (Wolfson 1992; Fantuzzo 2007); and six studies (Sirbu 1978; Gammon 1991; Bradley 2003; Farrar 2005; Chronis 2006; Fanning 2007) used the Brief Symptom Inventory, Perceived Stress Scale, Parental Stress Scale, Confidence Rating Questionnaire, Profile of Mood State and Stress Satisfaction Questionnaire, respectively.
Self‐esteem
Three studies (Patterson 2002; Lipman 2005; Chronis 2006) assessed parental self‐esteem using the Rosenberg Self‐Esteem Scale (Rosenberg 1965).
Anger
Three studies assessed parental anger using the Berger Feeling Scale (Joyce 1995; Greaves 1997) and the State‐Trait Anger Inventory (McGillicuddy 2001).
Aggression
None of the included studies assessed aggression.
Guilt
Three studies measured guilt using the Berger Feeling Scale (Joyce 1995; Greaves 1997) and Situational Guilt Scale (Nixon 1993).
Secondary outcome measures
Confidence
One‐third (n = 16) of included studies assessed parental confidence and used seven scales or subscales to measure this outcome. Four studies used the Parenting Sense of Competence Scale (Cunningham 1995; Odom 1996; Feliciana 2005; Gardner 2006); four studies used the Problem Setting and Behaviour Checklist (Martin 2003; Matsumoto 2007; Morawska 2009; Matsumoto 2010); three studies used the Toddler Care Questionnaire (Gross 1995; Gross 2003; Gross 2009); two studies used the Parent Stress Index (Pisterman 1992a; Pisterman 1992b); and three studies (Wolfson 1992; Farrar 2005; Joachim 2010) used the Kansas Parent satisfaction Scale, Parenting Task Checklist and Parental Efficacy measures, respectively.
Partner satisfaction
Eight included studies reported partner satisfaction and used five scales to measure this. Three studies (Matsumoto 2007; Morawska 2009; Matsumoto 2010) used the Relationship Quality Index; two studies (Taylor 1998; Chronis 2006) used the Dyadic Adjustment Scale; one study (Pisterman 1992a) used the Parenting Stress Index; one study (Schultz 1993) used the Marital Adjustment Inventory; and one study used the Locke‐Wallace Marital Adjustment Scale (Treacy 2005).
Adverse effects
None of the included studies set out to report any adverse effects and none reported any adverse effects.
Excluded studies
In this updated review, 121 studies (85 new and 36 from the earlier review) did not meet all the inclusion criteria. We excluded studies from the review if random allocation was not used (n = 14), if participants or the control group did not meet the inclusion criteria (n = 28), if the intervention was not group‐based (n = 34), if the study did not focus on parental psychosocial health (n = 54), if the study involved direct work with children (n = 9) or was a summary of another study (n = 5), and if standardised outcome measures were not used (3). We excluded 23 studies because of more than one reason mentioned above. Six excluded studies were listed as included studies in a previous version of the review but are now excluded (Van Wyk 1983; Scott 1987; Anastopoulos 1993; Mullin 1994; Sheeber 1994; Zimmerman 1996). We excluded Anastopoulos 1993, Scott 1987, Sheeber 1994 and Mullin 1994 on the basis that they did not meet the definition of a randomised or quasi‐randomised trial (Higgins 2008). Anastopoulos 1993 and Mullin 1994 were described as 'quasi‐experimental', but on inspection they were pre and post‐test studies and no attempt was made to randomly assign the participants to groups. Scott 1987 allocated by group alternation. Sheeber 1994 was a partially randomised trial. We excluded Van Wyk 1983, which reported changes in personality outcomes only, because it did not focus on parental mental health or parenting. Zimmerman 1996 did not focus on parental psychosocial health; the study investigated the influence of parenting skills strategies on family functioning. We have given the reasons for the exclusion of the 121 excluded studies in the Characteristics of excluded studies table.
Risk of bias in included studies
The 'Risk of bias' table provides a summary of our assessment of the risk of bias for the 48 included studies (see Characteristics of included studies and Figure 1). Each risk of bias table provides a decision about the adequacy of the study in relation to the criterion, summarised as 'low risk of bias'; 'high risk of bias' and 'unclear risk of bias’ (Higgins 2008). We attempted to contact the investigators where insufficient information was provided and we succeeded in obtaining further information for 22 studies.
1.
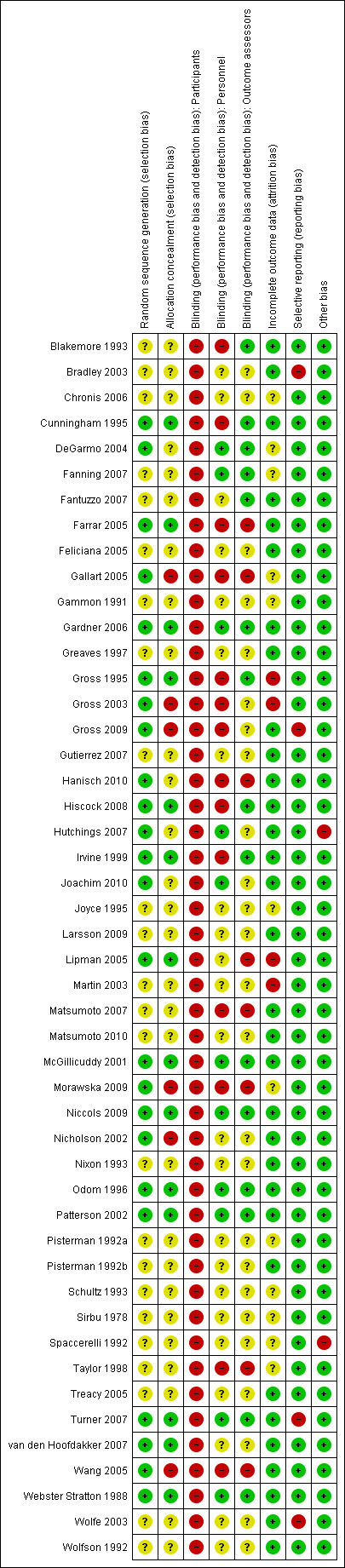
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
The method of sequence generation was adequate in 24 studies: 18 studies used allocation based on random numbers that were computer‐generated or derived from a table (Cunningham 1995; Gross 1995; Irvine 1999; McGillicuddy 2001; Nicholson 2002; Gross 2003; DeGarmo 2004; Farrar 2005; Lipman 2005; Gardner 2006; Hutchings 2007; Turner 2007; van den Hoofdakker 2007; Hiscock 2008; Gross 2009; Morawska 2009; Niccols 2009; Joachim 2010); four studies used allocation by drawing lots from a hat (Webster Stratton 1988; Odom 1996; Gallart 2005; Hanisch 2010); two studies allocated participants by throwing a dice or coin flipping (Patterson 2002; Wang 2005). We classified adequacy of sequence generation as ‘unclear’ in the 24 remaining studies.
We assessed that allocation was adequately concealed in 14 studies (Webster Stratton 1988; Cunningham 1995; Gross 1995; Odom 1996; Irvine 1999; McGillicuddy 2001; Patterson 2002; Farrar 2005; Lipman 2005; Gardner 2006; Turner 2007; van den Hoofdakker 2007; Hiscock 2008; Niccols 2009). Six studies (Nicholson 2002; Gross 2003; Gallart 2005; Wang 2005; Gross 2009; Morawska 2009) reported that allocation was not adequately concealed. We classified adequacy of allocation sequence as ‘unclear’ in the 28 remaining studies.
Blinding
We judged that it would not be possible to fully blind participants in studies of the type included in this review. We found no indication of any specific additional measures taken to reduce the risk of bias in the majority of included studies (n = 45). Farrar 2005 reported that one assessor was assigned to each group in order to ensure that participants did not have contact with members of the other group. Gallart 2005 reported that participants were kept blind to the fact that there were two different formats of the programme. Sirbu 1978 attempted to ensure that participants were unaware of the type of intervention they were receiving. However, review authors judged that those specific measures were not sufficient to reduce the risk of bias.
Trial investigators reported that outcome assessors were blind to the allocation status of participants in 15 studies (Blakemore 1993; Cunningham 1995; Gross 1995; Odom 1996; Webster Stratton 1988; Irvine 1999; McGillicuddy 2001; Patterson 2002; DeGarmo 2004; Gardner 2006; Fanning 2007; Fantuzzo 2007; Turner 2007; Hiscock 2008; Niccols 2009). In eight studies, outcome assessors were either not blinded or blinding was compromised during the trial (Taylor 1998; Farrar 2005; Gallart 2005; Lipman 2005; Wang 2005; Matsumoto 2007; Morawska 2009; Hanisch 2010). We classified the blinding of outcome assessors as ‘unclear’ in the remaining 25 studies.
Incomplete outcome data
We judged that most of the studies (n = 32) adequately addressed incomplete outcome data; eight of those studies (Blakemore 1993; Greaves 1997; McGillicuddy 2001; Nicholson 2002; Wolfe 2003; Feliciana 2005; Fantuzzo 2007; Matsumoto 2007) reported that none of the participants dropped out and the study data were collected on all participants at each data collection point; four studies (Gross 1995; Gross 2003; Martin 2003; Larsson 2009) did not adequately address incomplete outcome data; the remaining 12 studies were classified as ‘unclear’.
Selective reporting
Most studies (n = 44) appeared to have included all expected outcomes and were free of selective reporting. Four studies were not free of selective reporting: Bradley 2003 did not report endpoint and follow‐up data for depressive symptoms from the BSI subscale; Gross 2009 stated that three outcomes (depressive symptoms, stress and confidence) were not included in the paper because of length and their lack of association with the outcome variables; Turner 2007 did not report scores for the anxiety scale of the DASS; Wolfe 2003 did not report endpoint and follow‐up data for the parent‐child dysfunctional interaction subscale of the PSI.
Other potential sources of bias
While the use of randomisation should in theory ensure that any possible confounders are equally distributed between the arms of the trial, the randomisation of small numbers of respondents may result in an unequal distribution of confounding factors. It is therefore important that the distribution of known potential confounders is: (i) compared between the different study groups at the outset, or (ii) adjusted for at the analysis stage.
Spaccerelli 1992 used two newly developed measures, which also raised the possibility of bias. Hutchings 2007 reported a competing interest as both author and provider of occasional parent training courses. The remaining 46 studies appeared to be free of other bias.
Effects of interventions
In the text below, an I2 value for heterogeneity was only reported if it exceeded 50% or if the P value from the Chi2 test was < 0.05. Numbers given are the total number of participants randomised. Where it has been possible to calculate an effect size, we have reported these with 95% confidence intervals (CI). Where we calculated and reported effect sizes, a minus sign indicates that the results favour the intervention group. Where the calculated effect size is statistically significant (P < 0.05), we state whether the result favours the intervention or control condition.
In terms of effect sizes, values > 0.70 have been treated as large; those between 0.40 and 0.70 as moderate; values < 0.40 and > 0.10 have been treated as small; and values < 0.10 have been treated as no evidence of effectiveness (Higgins 2008, Section 12.6.2).
We have summarised the results below under headings corresponding to the seven primary and the three secondary outcomes outlined in the section entitled Types of outcome measures. For each outcome, we have presented the results according to the timing of the outcome assessment. Three categories of outcome assessment were used: post‐intervention (up to four weeks after the end of the intervention), short‐term follow‐up (two to six months post‐intervention), and long‐term follow‐up (more than six months post‐intervention). Under each heading, results of subgroup analyses (to compare types of intervention) are included where these were conducted. For clarity, results of two further subgroup analyses (impact of paternal‐only outcomes; impact of duration of intervention) are summarised in a separate section.
Primary outcomes
Depressive symptoms
Post‐intervention
Meta‐analysis of data from 22 studies revealed a statistically significant difference between intervention and control conditions, favouring the intervention (SMD ‐0.17, CI ‐0.28 to ‐0.07, P = 0.001, n = 1591, I2 = 7%, Analysis 1.1.1). This result was broadly consistent with the meta‐analysis of 11 studies reported in the previous version of this review (SMD ‐0.26) (Barlow 2003).
1.1. Analysis.
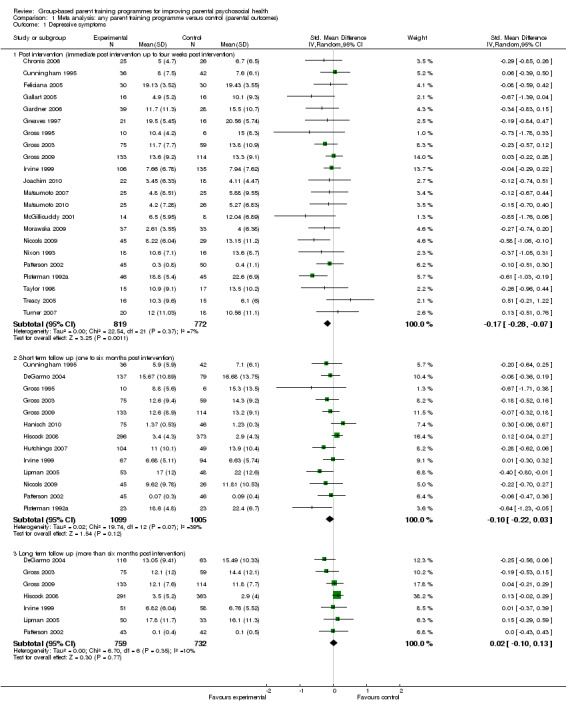
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 1 Depressive symptoms.
Short‐term follow‐up
Meta‐analysis of data from 13 studies indicated no statistically significant difference between intervention and control conditions at short‐term follow‐up (Analysis 1.1.2). In the previous version of this review, meta‐analysis of six studies similarly failed to achieve statistical significance (95% CI ‐0.40 to 0.002) (Barlow 2003).
Long‐term follow‐up
Meta‐analysis of data from seven studies revealed no statistically significant difference between intervention and control conditions at long‐term follow‐up (Analysis 1.1.3).
Anxiety symptoms
Post‐intervention
Meta‐analysis of data from nine studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.22, CI ‐0.43 to ‐0.01, P = 0.04, n = 464, I2 = 22%, Analysis 1.2.1). The previous version of this review did not report an analysis for anxiety symptoms alone, although a statistically significant effect favouring the intervention was identified for the combined outcome of anxiety and stress (SMD ‐0.4, 95% CI ‐0.6 to ‐0.2) (Barlow 2003).
1.2. Analysis.
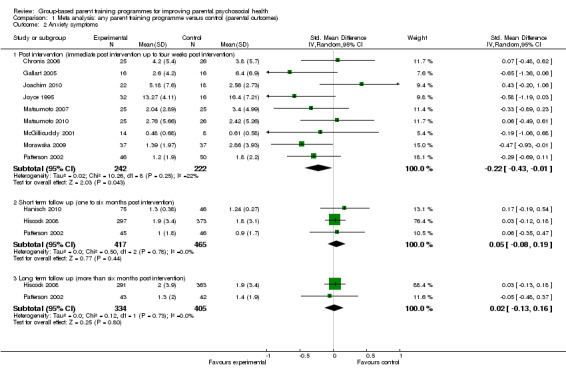
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 2 Anxiety symptoms.
Short‐term follow‐up
Meta‐analysis of data from three studies indicated no statistically significant difference between intervention and control conditions at short‐term follow‐up (Analysis 1.2.2).
Long‐term follow‐up
Meta‐analysis of data from two studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.2.3).
Stress
Post‐intervention
Meta‐analysis of data from 25 studies, which included data from both arms (behavioural versus wait‐list control, Adlerian parent training versus attention placebo control) and both control conditions for Gutierrez 2007, revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.29, 95% CI ‐0.42 to ‐0.15, P < 0.0001, n = 1567, Analysis 1.3.1) but with evidence of significant heterogeneity (I2 = 35%; P = 0.04). The previous version of this review did not report an analysis for stress symptoms alone, although a statistically significant effect was found for the combined outcome of anxiety and stress, again favouring the intervention (SMD ‐0.4, 95% CI ‐0.6 to ‐0.2, 10 studies).
1.3. Analysis.
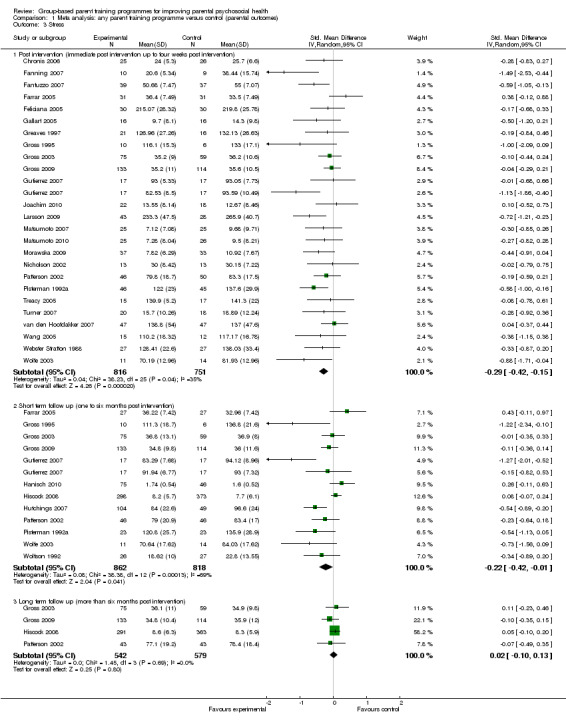
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 3 Stress.
Short‐term follow‐up
Meta‐analysis of data from 12 studies again indicated a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.22, 95% CI ‐0.42 to ‐0.01, P = 0.04, n = 1680, Analysis 1.3.2) but with evidence of statistically significant heterogeneity (I2 = 69%; P < 0.0001). One possible reason for the large I2 value is that the impact of parent training on stress scores varied with the modality of the intervention (see below).
Long‐term follow‐up
Meta‐analysis of data from four studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.3.3).
Self‐esteem
Post‐intervention
Meta‐analysis of data from two studies at post‐intervention indicated no statistically significant difference between intervention and control conditions (Analysis 1.4.1).
1.4. Analysis.
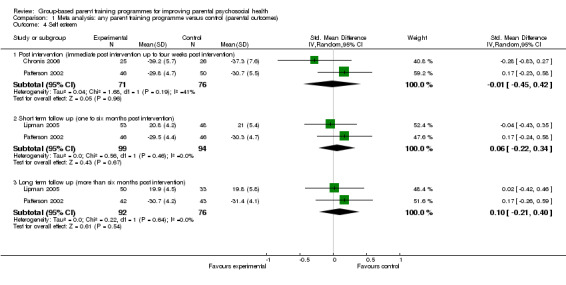
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 4 Self esteem.
Short‐term follow‐up
Meta‐analysis of data from two studies at short‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.4.2).
Long‐term follow‐up
Meta‐analysis of data from two studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.4.3).
Anger
Post‐intervention
Meta‐analysis of data from three studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.60, 95% CI ‐1.00 to ‐0.20, P = 0.004, n = 107, I2 = 0%, Analysis 1.5.1).
1.5. Analysis.
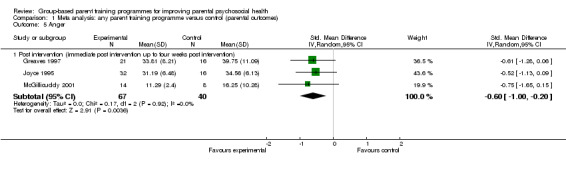
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 5 Anger.
Short‐ and long‐term follow‐up
Anger was not reported in any study at short‐ or long‐term follow‐up.
Aggression
No study reported aggression.
Guilt
Post‐intervention
Meta‐analysis of data from three studies showed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.79, 95% CI ‐1.18 to ‐0.41, P < 0.0001, n = 119, I2 = 0%, Analysis 1.6.1).
1.6. Analysis.
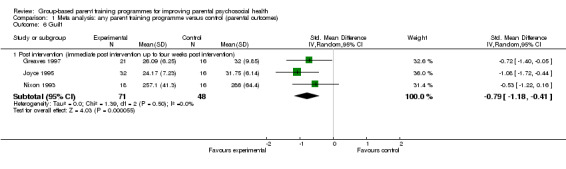
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 6 Guilt.
Short‐ and long‐term follow‐up
No study reported guilt at short‐ or long‐term follow‐up.
Secondary outcomes
Confidence
Post‐intervention
Meta‐analysis of data from 14 studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.34, 95% CI ‐0.51 to ‐0.17, P < 0.0001, n = 1001, I2 = 36%, Analysis 1.7.1).
1.7. Analysis.
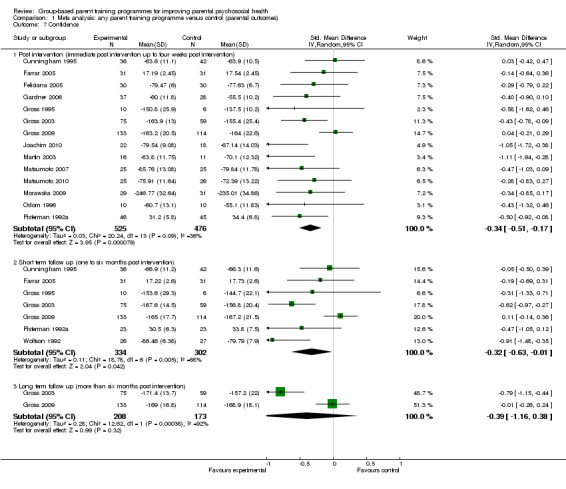
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 7 Confidence.
Short‐term follow‐up
Meta‐analysis of data from seven studies revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.32, 95% CI ‐0.63 to ‐0.01, P = 0.04, n = 636, Analysis 1.7.2) but with evidence of significant heterogeneity (I2 = 68%; P = 0.005).
Long‐term follow‐up
Meta‐analysis of data from two studies at long‐term follow‐up indicated no statistically significant difference between intervention and control conditions (Analysis 1.7.3).
Partner satisfaction
Post‐intervention
Meta‐analysis of data from nine studies revealed a moderate, statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.28, 95% CI ‐0.47 to ‐0.09, P = 0.005, n = 432, I2 = 0%, Analysis 1.8.1). This was consistent with the meta‐analysis of four studies reported in the previous version of this review (Barlow 2003), which produced an SMD of ‐0.4.
1.8. Analysis.
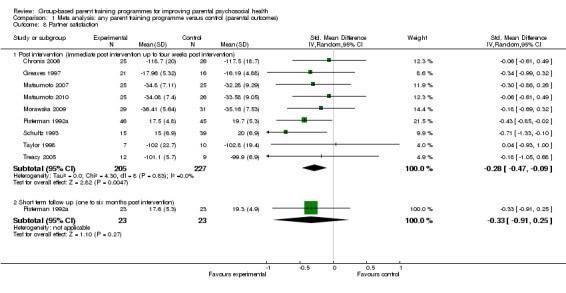
Comparison 1 Meta analysis: any parent training programme versus control (parental outcomes), Outcome 8 Partner satisfaction.
Short‐term follow‐up
At short‐term follow up, results of analysis of data from a single study indicated no statistically significant difference between intervention and control conditions (Analysis 1.8.2).
Long‐term follow‐up
No study reported partner satisfaction at short‐ or long‐term follow‐up.
Adverse effects
No study reported adverse effects.
Paternal outcome measures
Only four studies reported outcome data from fathers separately. These data were available for four outcomes (depressive symptoms, stress, confidence, and partner satisfaction) but with meta‐analysis possible for the outcome of stress only. Meta‐analysis of data from four studies for paternal stress at post‐intervention revealed a statistically significant difference between intervention and control conditions favouring the intervention (SMD ‐0.43, 95% CI ‐0.79 to ‐0.06, P = 0.02, n = 123, I2 = 0%, Analysis 2.42.1). This effect size is larger than the overall figure (for mothers and for both parental figures) obtained in Analysis 1.3.1 (SMD ‐0.29). Examining data from individual studies revealed no statistically significant effect from paternal‐only data for depressive symptoms, confidence or partner satisfaction (Analysis 2.40.1; Analysis 2.41.1; Analysis 2.43.1; Analysis 2.44.1).
2.42. Analysis.
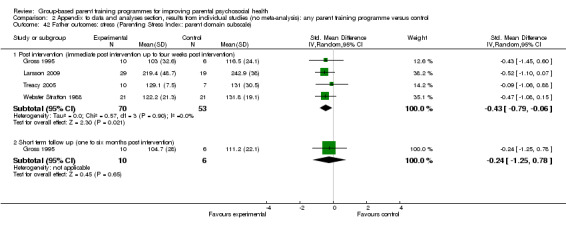
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 42 Father outcomes: stress (Parenting Stress Index: parent domain subscale).
2.40. Analysis.
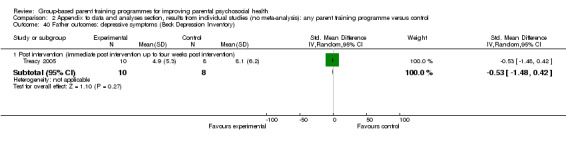
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 40 Father outcomes: depressive symptoms (Beck Depression Inventory).
2.41. Analysis.
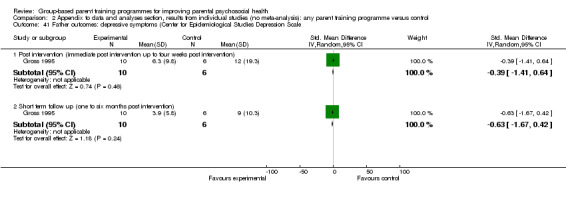
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 41 Father outcomes: depressive symptoms (Center for Epidemiological Studies Depression Scale.
2.43. Analysis.
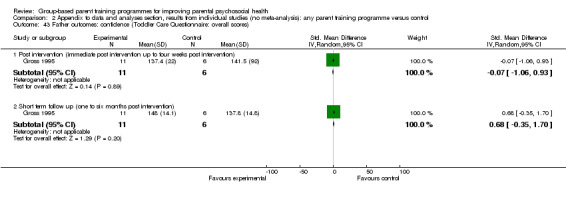
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 43 Father outcomes: confidence (Toddler Care Questionnaire: overall scores).
2.44. Analysis.
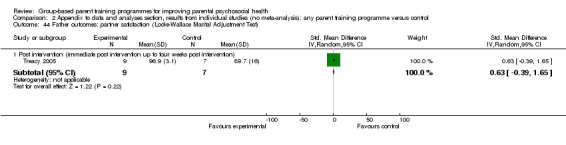
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 44 Father outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test).
Discussion
Summary of main results
This updated review includes a total of 48 studies. Eight meta‐analyses were conducted evaluating the immediate post‐intervention impact and four evaluating the short‐term (six months) and long‐term (one year or more) impact of behavioural (n = 22), cognitive‐behavioural (n = 19) and non‐classifiable or multimodal (n = 8) parenting programmes on a range of aspects of parental psychosocial wellbeing. The results indicate that parenting programmes were effective immediately post‐intervention in producing statistically significant improvements in a number of aspects of parental psychosocial functioning including depression (SMD ‐0.17, 95% CI ‐0.28 to ‐0.07); anxiety (SMD ‐0.22, 95% CI ‐0.43 to ‐0.01); stress (SMD ‐0.29, 95% CI ‐0.42 to ‐0.15); anger (SMD ‐0.60, 95% CI ‐1.00 to ‐0.20); guilt (SMD ‐0.79, 95% CI ‐1.18 to ‐0.41); confidence (SMD ‐0.34, 95% CI ‐0.51 to ‐0.17), and satisfaction with the partner relationship (SMD ‐0.28, 95% CI ‐0.47 to ‐0.09). There was, however, evidence of significant statistical heterogeneity for the meta‐analyses of stress outcomes post‐intervention and for parental confidence at short‐term follow‐up.
Although the results suggest that stress (SMD ‐0.22, 95% CI ‐0.42 to ‐0.01) and confidence (SMD ‐0.32, 95% CI ‐0.63 to ‐0.01) continued to be statistically significant at six month follow‐up, none of the outcomes measured remained statistically significant at one year. This finding strongly points to the need for parents to receive 'top ups' or post‐intervention support to help them to maintain the short‐term benefits.
There were only sufficient data from fathers to conduct one meta‐analysis. This showed a statistically significant short‐term improvement in paternal stress (SMD ‐0.43, 95% CI ‐0.79 to ‐0.06). The deleterious consequences of compromised paternal psychosocial functioning has now been clearly recognised (for example, Kane 2004; Ramchandani 2008), and the need to support fathers has been highlighted at policy level (Department of Health 2009). This finding points to the need for further research focusing explicitly on the impact of such programmes on the psychosocial functioning of fathers.
Overall completeness and applicability of evidence
These data provide a comprehensive picture about the impact of the key types of parenting programme (for example, behavioural and cognitive‐behavioural) on parental psychosocial functioning.
The studies were conducted in a wide range of settings and countries including the USA, Australia, Canada, UK, China, Germany, Japan, the Netherlands and New Zealand.
Only a small number of studies examined the effectiveness of parenting programmes in terms of the psychosocial functioning of fathers, and this is a serious omission given that fathers now play a significant role in childcare, and research suggests that their psychosocial functioning is key to the wellbeing of children (see Background).
Quality of the evidence
The overall quality of the included studies is summarised in Figure 1. Many studies were unclear about important quality criteria, including allocation concealment, sequence generation and blinding. We examined the included studies for evidence of other potential biases, including that of conflict of interest, which was implicated in one study only (Hutchings 2007) where the study author also delivered the intervention. A number of the included studies (in particular the Webster‐Stratton and Triple‐P programmes) involved the programme developer in the evaluation.
Potential biases in the review process
In the original review we estimated the standardised mean difference by calculating the treatment effect for each outcome in each study by dividing the mean difference in post‐intervention scores for the intervention and treatment groups by the pooled standard deviation. To promote consistency we have continued with this method. It should be noted, however, that random allocation does not guarantee equality of means between groups at pre‐test, and also that post‐test standard deviation (SD) may be inflated by a differential response to intervention, and may underestimate the effect size attributable to the intervention.
Agreements and disagreements with other studies or reviews
These findings are consistent with the earlier review (Barlow 2003) of the effectiveness of parent training programmes in improving the psychosocial wellbeing of parents. However, the significant addition of new studies has enabled us to reach a number of new conclusions in terms of the evidence about effectiveness being limited to standard (10 to 12 week) parent training programmes and in the short term only. This is largely consistent with the findings of reviews that examine the impact of parenting programmes on children's behaviour, which is again mostly limited to evidence of short‐term benefits (Dretze 2005; Barlow 2011).
Authors' conclusions
Implications for practice.
This review provides sufficient evidence to support the use of parenting programmes to improve parental psychosocial functioning. However, the findings also suggest that the benefits are short‐term and that parents may need additional support if the improvements are to be maintained over time. Although there is insufficient evidence to clearly demonstrate an impact on paternal psychosocial functioning, the limited evidence available suggests that parenting programmes have potential to improve the psychosocial functioning of fathers as well as mothers. Evidence about the importance of paternal psychosocial functioning on the wellbeing of children, alongside numerous policy directives pointing to the need to provide better support for fathers, suggest that parenting programmes should also be offered to fathers.
Implications for research.
Only a small number of studies examined the effectiveness of parenting programmes in terms of the psychosocial functioning of fathers, and this is a serious omission given that fathers now play a significant role in childcare and research suggests that their psychosocial functioning is key to the wellbeing of children (see Background). The findings also suggest that effectiveness is limited to the short term only and future research should as such address the reasons for this, including the need for longer or more intensive programmes or for post‐intervention support. Further research is also needed to identify whether brief programmes can impact on parental wellbeing.
These results do not enable us to address whether parenting programmes bring about improvements in some aspects of parental psychosocial functioning as a consequence of improvements in children's behaviour and family functioning more generally, or as a result of strategies within the programmes explicitly targeting parental psychosocial functioning. This finding warrants explicit examination as part of future research on parenting programmes.
What's new
| Date | Event | Description |
|---|---|---|
| 21 April 2011 | New citation required and conclusions have changed | New search. New authors. |
| 21 April 2011 | New search has been performed | Updated with new included studies. |
History
Protocol first published: Issue 2, 2000 Review first published: Issue 4, 2000
| Date | Event | Description |
|---|---|---|
| 10 June 2008 | Amended | Converted to new review format. |
| 26 July 2003 | New citation required and conclusions have changed | This review was updated with the addition of 3 new included studies. |
Acknowledgements
We thank Esther Coren for her work as author of the previously published versions of the review and for her advice on this update. We also thank Sarah Stewart‐Brown for her work as an author on the original review.
We thank the editorial team of the Cochrane DPLP Group (Jane Dennis, Chris Champion, Laura MacDonald, Jo Abbott and Margaret Anderson) for their support and advice.
We thank Julian Higgins (MRC Biostatistics Unit, Cambridge) who gave advice about the analysis plan.
CB thanks the University of Bristol and Queen’s University Belfast for awarding visiting fellowships to support her in the academic activities of writing this review between 2008 and 2012.
Appendices
Appendix 1. Search strategies
MEDLINE
1 (parent$‐program$ or parent$‐training or parent$‐education or parent$‐promotion).tw.
2 (parent$ program$ or parent$ training or parent$ education or parent$ promotion).tw.
3 1 or 2
ASSIA (Applied Social Sciences Index and Abstracts database)
(((parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion)) or ((parent* program* or parent* training or parent* education or parent* promotion)))
BIOSIS
(ts= (parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion)) or( ts=(parent* program* or parent* training or parent* education or parent* promotion))
CENTRAL
#1 parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion
#2 parent next program* or parent* next training or parent* next education or parent* next promotion
#3 (#1 OR #2)
CINAHL
( parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion ) or ( parent* program* or parent* training or parent* education or parent* promotion )
EMBASE
1 (parent$‐program$ or parent$‐training or parent$‐education or parent$‐promotion).tw.
2 (parent$ program$ or parent$ training or parent$ education or parent$ promotion).tw.
3 1 or 2
PsycINFO
(parent* promotion OR parent* training OR parent* education OR parent* program* OR parent*‐promotion OR parent*‐training OR parent*‐education OR parent*‐program*)
Sociological Abstracts via CSA (March 2010 and February 2008)
(TI=((parent* program*) or (parent*training) or (parent* education) or (parent* promotion)) or AB=((parent* program*) or (parent* training) or (parent* education) or (parent* promotion)) or DE=((parent* program*) or (parent*training) or (parent*education) or (parent*promotion))) or (TI=(parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion) or AB=(parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion) or DE=(parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion))
Sociological Abstracts via Proquest ( December 2011)
all(parent*‐program* OR parent*‐training OR parent*‐education OR parent*‐promotion) Limits applied Databases:Sociological Abstracts Limited by: Date: After 2010 Document type:Journal Article
Social Science Citation Index
Social Science Citation Index searched using ISI Web of Knowledge.
(ts= (parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion)) or( ts=(parent* program* or parent* training or parent* education or parent* promotion))
ERIC via Ovid (March 2010 and February 2008)
1 randomi?ed.tw. 2 ((singl$ or doubl$ or treb$ or tripl$) adj3 (blind$ or mask$)).tw. 3 placebo.tw. 4 (clin$ adj3 trial$).tw. 5 exp methods research/ 6 (random$ adj5 (allocat$ or assign$ or select$)).tw. 7 ((control$ or prospectiv$) adj5 (trial$ or study or studies)).tw. 8 1 or 2 or 3 or 4 or 5 or 6 or 7 9 (parent$ adj3 (program$ or educat$ or train$ promot$)).tw. 10 "parent‐program$".tw. 11 "parent‐train$".tw 12 "parent‐educat$".tw. 13 "parent‐promot$".tw. 14 9 or 10 or 11 or 12 or 13 15 8 and 14
ERIC via www.eric.ed.gov (December 2011)
((Keywords:"parent train*" or Keywords:"parent promot*" or Keywords:"parent educat*" or Keywords:"parent program*") or (Keywords:"parent‐program*" or Keywords:"parent‐train*" or Keywords:"parent‐educat*" or Keywords:"parent‐promot*")
National Research Register
#1(parent*‐program* or parent*‐training or parent*‐education or parent*‐promotion) in ti, ab, de
#2(parent* program* or parent* training or parent* education or parent* promotion) in ti, ab, de
#3 #1 or #2
NSPCC Library Catalogue
parent program OR parent training OR parent education OR parent promotion (Title or Subject Term. Truncation box ticked)
mRCT
Searched using the following key words:
parent program
parent programme
parent training
parent education
parent promotion
Data and analyses
Comparison 1. Meta analysis: any parent training programme versus control (parental outcomes).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depressive symptoms | 27 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Post intervention (immediate post intervention up to four weeks post intervention) | 22 | 1591 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.28, ‐0.07] |
| 1.2 Short term follow up (one to six months post intervention) | 13 | 2104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.22, 0.03] |
| 1.3 Long term follow up (more than six months post intervention) | 7 | 1491 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.10, 0.13] |
| 2 Anxiety symptoms | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Post intervention (immediate post intervention up to four weeks post intervention) | 9 | 464 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.43, ‐0.01] |
| 2.2 Short term follow up (one to six months post intervention) | 3 | 882 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.08, 0.19] |
| 2.3 Long term follow up (more than six months post intervention) | 2 | 739 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.13, 0.16] |
| 3 Stress | 29 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Post intervention (immediate post intervention up to four weeks post intervention) | 25 | 1567 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.42, ‐0.15] |
| 3.2 Short term follow up (one to six months post intervention) | 12 | 1680 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.42, ‐0.01] |
| 3.3 Long term follow up (more than six months post intervention) | 4 | 1121 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.10, 0.13] |
| 4 Self esteem | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | 147 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.45, 0.42] |
| 4.2 Short term follow up (one to six months post intervention) | 2 | 193 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.22, 0.34] |
| 4.3 Long term follow up (more than six months post intervention) | 2 | 168 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.21, 0.40] |
| 5 Anger | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.00, ‐0.20] |
| 6 Guilt | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | 119 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.18, ‐0.41] |
| 7 Confidence | 15 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Post intervention (immediate post intervention up to four weeks post intervention) | 14 | 1001 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.51, ‐0.17] |
| 7.2 Short term follow up (one to six months post intervention) | 7 | 636 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.63, ‐0.01] |
| 7.3 Long term follow up (more than six months post intervention) | 2 | 381 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.16, 0.38] |
| 8 Partner satisfaction | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Post intervention (immediate post intervention up to four weeks post intervention) | 9 | 432 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.47, ‐0.09] |
| 8.2 Short term follow up (one to six months post intervention) | 1 | 46 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.91, 0.25] |
Comparison 2. Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parental outcomes: depressive symptoms (Beck Depression Inventory) | 9 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Post intervention (immediate post intervention up to four weeks post intervention) | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short term follow up (one to six months post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Parental outcomes: depressive symptoms (subscale of Irritability Depression & Anxiety Scale) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Post intervention (immediate post intervention up to four weeks post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Parental outcomes: depressive symptoms (subscale of Depression Anxiety Stress Scale) | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Post intervention (immediate post intervention up to four weeks post intervention) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Parental outcomes: depressive symptoms (Centre for Epidem. Studies Depression Scale) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Post intervention (immediate post intervention up to four weeks post intervention) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Short term follow up (one to six months post intervention) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Long term follow up (more than six months post intervention) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Parental outcomes: depressive symptoms (subscale of Parenting Stress Index) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Parental outcomes: depressive symptoms (subscale of General Health Questionnaire) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Parental outcomes: anxiety symptoms (subscale of Depression Anxiety Stress Scale) | 7 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Post intervention (immediate post intervention up to four weeks post intervention) | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Parental outcomes: anxiety symptoms (subscale of Irritability, Depression and Anxiety Scale) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Post intervention (immediate post intervention up to four weeks post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Parental outcomes: anxiety symptoms (subscale of General Health Questionnaire) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Parental outcomes: anxiety symptoms (STAI State scale) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Parental outcomes: anxiety symptoms (STAI Trait scale) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Post intervention (immediate post intervention up to four weeks post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Short term follow up (one to six months post intervention) | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Parental outcomes: anxiety symptoms (Beck Anxiety Inventory) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Parental outcomes: anxiety symptoms (Brief Symptom Inventory) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Parental outcomes: stress (Perceived Stress Scale) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Parental outcomes: stress (Parenting Stress Index: overall score) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Parental outcomes: stress (Parenting Stress Index: parent domain score) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 Post intervention (immediate post intervention up to four weeks post interven | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Parental outcomes: stress (Parenting Stress Index ‐ short form: overall score) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 17.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Short term follow up (one to six months post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Parental outcomes: stress (Parenting Stress Index ‐ short form: distress subscale) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Parental outcomes: stress (Everyday Stress Index) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 19.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 Long term follow up (more than six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Parental outcomes: stress (Ability & Confidence Rating Questionnaire) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 20.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Parental outcomes: stress (Parental Stress Scale) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 21.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 21.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Parental outcomes: stress (modified Uplifts & Hassles Scale: hassles scale) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 22.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Parental outcomes: stress (subscale of Depression Anxiety Stress Sscale) | 8 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 23.1 Post intervention (immediate post intervention up to four weeks post intervention) | 6 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 Long term follow up (more than six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Parental outcomes: self‐esteem (Rosenberg Self‐Esteem scale) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 24.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Short term follow up (one to six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.3 Long term follow up (more than six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Parental outcomes: anger (subscale of Berger's Feeling Scale) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 25.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Parental outcomes: anger (State‐Trait Anger Expression Inventory scale) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 26.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 Parental outcomes: guilt (subscale of Berger's Feeling Scale) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 27.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 28 Parental outcomes: guilt (Situation Guilt Scale) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 28.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Parental outcomes: confidence (Parenting Task Checklist) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 29.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Parental outcomes: confidence (Parental Efficacy measure) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 30.1 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31 Parental outcomes: confidence (Parenting Stress Index) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 31.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 Parental outcomes: confidence (Toddler Care Questionnaire) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 32.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.2 Short term follow up (one to six months post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.3 Long term follow up (more than six months post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 33 Parental outcomes: confidence (Parenting Sense of Competence Scale: total score) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 33.1 Post intervention (immediate post intervention up to four weeks post intervention) | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 33.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 34 Parental outcomes: confidence (Problem Setting & Behaviour Checklist) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 34.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35 Parental outcomes: confidence (Kansas Parental Satisfaction Scale: satisfaction in parental role) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 35.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 36 Parental outcomes: partner satisfaction (Dyadic Adjustment Scale) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 36.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 37 Parental outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 37.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 38 Parental outcomes: partner satisfaction (Parenting Stress Index) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 38.1 Post intervention (immediate post intervention up to four weeks post intervention) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 38.2 Short term follow up (one to six months post intervention) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 39 Parental outcomes: partner satisfaction (Relation Quality Index) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 39.1 Post intervention (immediate post intervention up to four weeks post intervention) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 40 Father outcomes: depressive symptoms (Beck Depression Inventory) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 40.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 18 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.48, 0.42] |
| 41 Father outcomes: depressive symptoms (Center for Epidemiological Studies Depression Scale | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 41.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.41, 0.64] |
| 41.2 Short term follow up (one to six months post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.67, 0.42] |
| 42 Father outcomes: stress (Parenting Stress Index: parent domain subscale) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 42.1 Post intervention (immediate post intervention up to four weeks post intervention) | 4 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.79, ‐0.06] |
| 42.2 Short term follow up (one to six months post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.25, 0.78] |
| 43 Father outcomes: confidence (Toddler Care Questionnaire: overall scores) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 43.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 17 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐1.06, 0.93] |
| 43.2 Short term follow up (one to six months post intervention) | 1 | 17 | Std. Mean Difference (IV, Random, 95% CI) | 0.68 [‐0.35, 1.70] |
| 44 Father outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 44.1 Post intervention (immediate post intervention up to four weeks post intervention) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | 0.63 [‐0.39, 1.65] |
2.1. Analysis.
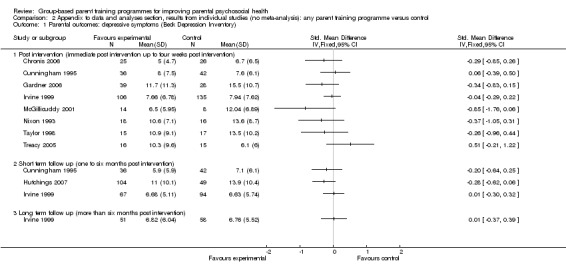
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 1 Parental outcomes: depressive symptoms (Beck Depression Inventory).
2.3. Analysis.
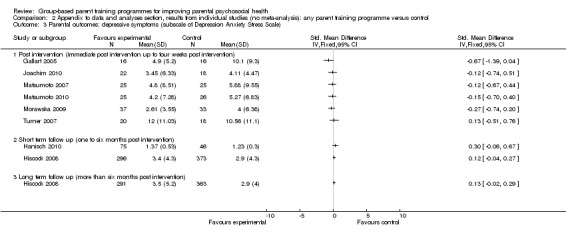
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 3 Parental outcomes: depressive symptoms (subscale of Depression Anxiety Stress Scale).
2.4. Analysis.
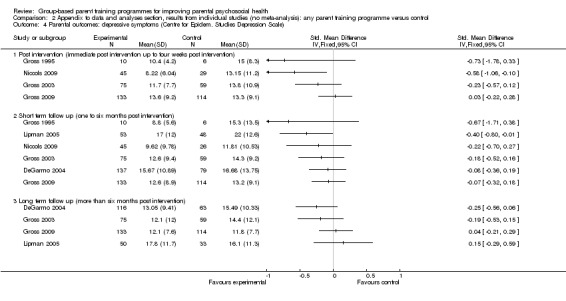
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 4 Parental outcomes: depressive symptoms (Centre for Epidem. Studies Depression Scale).
2.5. Analysis.
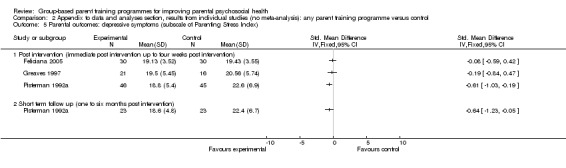
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 5 Parental outcomes: depressive symptoms (subscale of Parenting Stress Index).
2.6. Analysis.
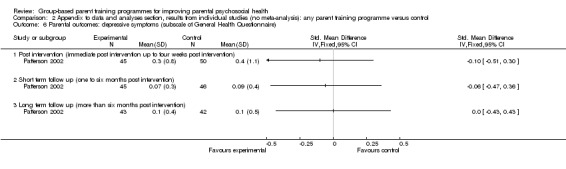
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 6 Parental outcomes: depressive symptoms (subscale of General Health Questionnaire).
2.7. Analysis.
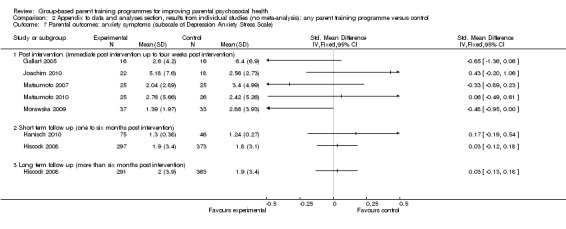
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 7 Parental outcomes: anxiety symptoms (subscale of Depression Anxiety Stress Scale).
2.9. Analysis.
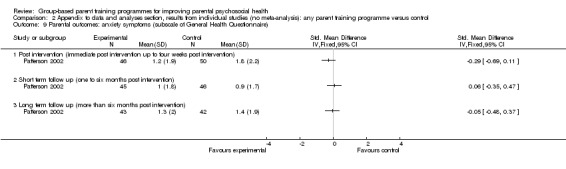
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 9 Parental outcomes: anxiety symptoms (subscale of General Health Questionnaire).
2.10. Analysis.
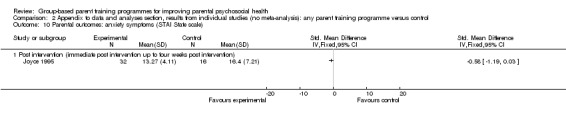
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 10 Parental outcomes: anxiety symptoms (STAI State scale).
2.12. Analysis.
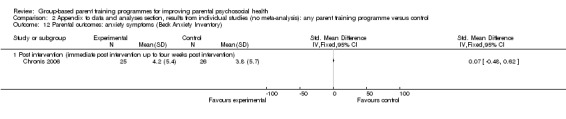
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 12 Parental outcomes: anxiety symptoms (Beck Anxiety Inventory).
2.13. Analysis.
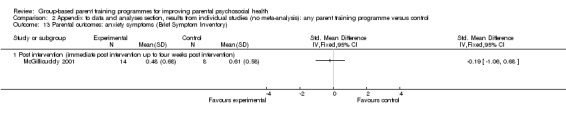
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 13 Parental outcomes: anxiety symptoms (Brief Symptom Inventory).
2.14. Analysis.
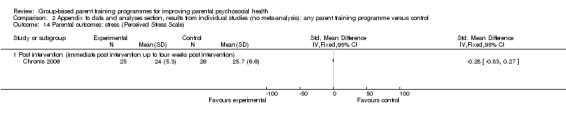
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 14 Parental outcomes: stress (Perceived Stress Scale).
2.15. Analysis.
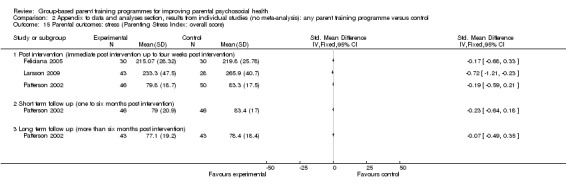
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 15 Parental outcomes: stress (Parenting Stress Index: overall score).
2.16. Analysis.
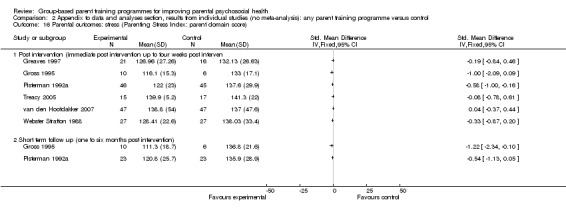
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 16 Parental outcomes: stress (Parenting Stress Index: parent domain score).
2.17. Analysis.
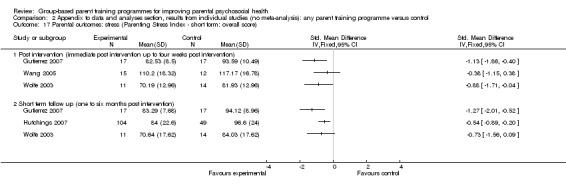
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 17 Parental outcomes: stress (Parenting Stress Index ‐ short form: overall score).
2.18. Analysis.
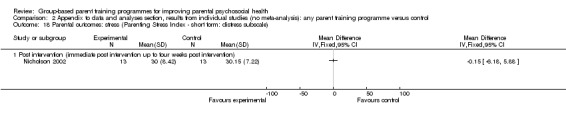
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 18 Parental outcomes: stress (Parenting Stress Index ‐ short form: distress subscale).
2.19. Analysis.
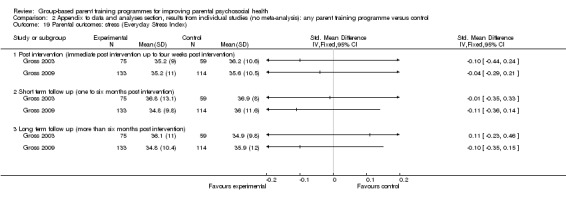
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 19 Parental outcomes: stress (Everyday Stress Index).
2.20. Analysis.
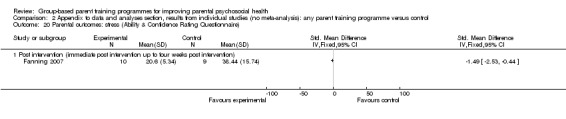
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 20 Parental outcomes: stress (Ability & Confidence Rating Questionnaire).
2.21. Analysis.
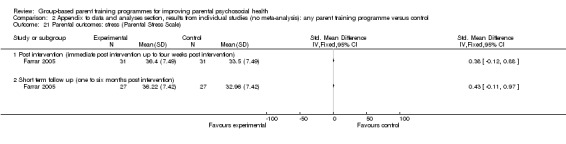
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 21 Parental outcomes: stress (Parental Stress Scale).
2.22. Analysis.
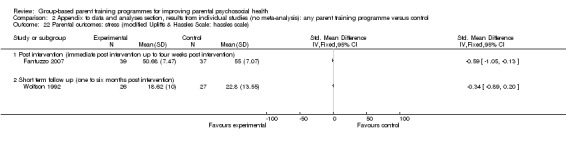
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 22 Parental outcomes: stress (modified Uplifts & Hassles Scale: hassles scale).
2.23. Analysis.
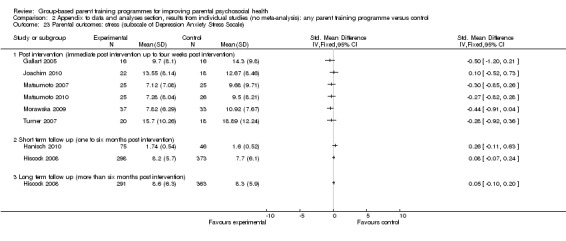
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 23 Parental outcomes: stress (subscale of Depression Anxiety Stress Sscale).
2.24. Analysis.
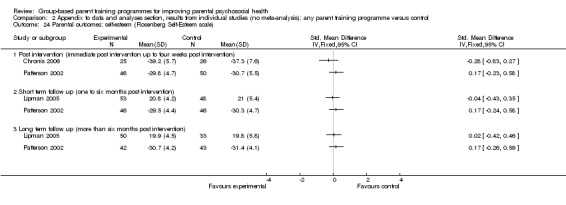
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 24 Parental outcomes: self‐esteem (Rosenberg Self‐Esteem scale).
2.25. Analysis.
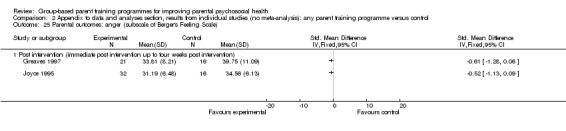
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 25 Parental outcomes: anger (subscale of Berger's Feeling Scale).
2.26. Analysis.
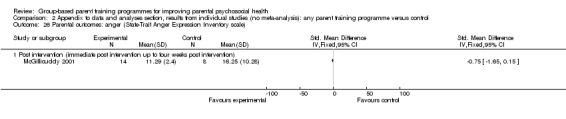
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 26 Parental outcomes: anger (State‐Trait Anger Expression Inventory scale).
2.27. Analysis.
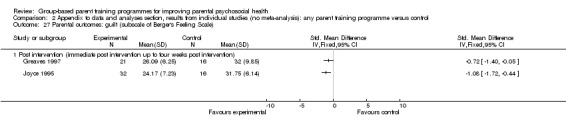
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 27 Parental outcomes: guilt (subscale of Berger's Feeling Scale).
2.28. Analysis.
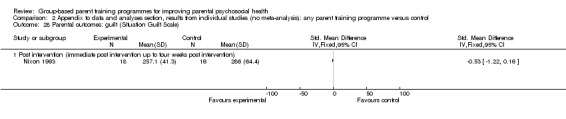
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 28 Parental outcomes: guilt (Situation Guilt Scale).
2.29. Analysis.
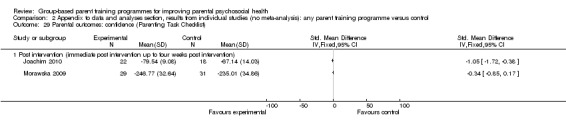
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 29 Parental outcomes: confidence (Parenting Task Checklist).
2.30. Analysis.
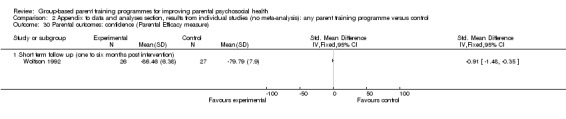
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 30 Parental outcomes: confidence (Parental Efficacy measure).
2.31. Analysis.
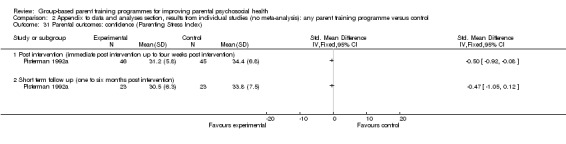
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 31 Parental outcomes: confidence (Parenting Stress Index).
2.32. Analysis.
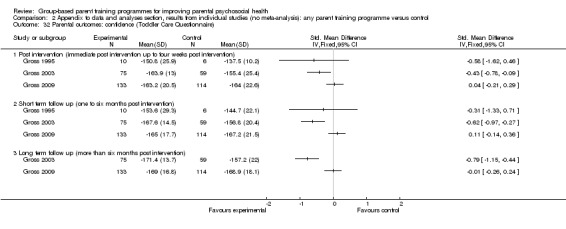
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 32 Parental outcomes: confidence (Toddler Care Questionnaire).
2.33. Analysis.
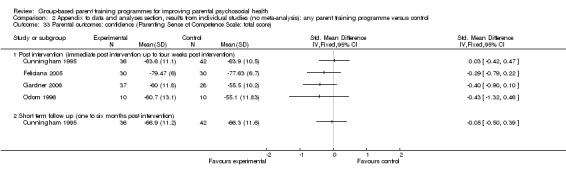
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 33 Parental outcomes: confidence (Parenting Sense of Competence Scale: total score).
2.34. Analysis.
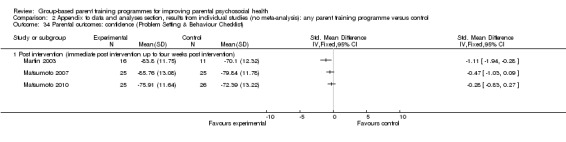
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 34 Parental outcomes: confidence (Problem Setting & Behaviour Checklist).
2.35. Analysis.
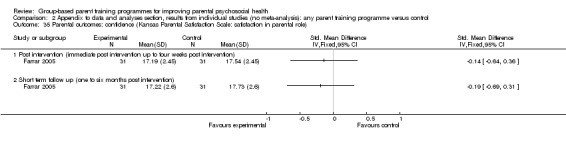
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 35 Parental outcomes: confidence (Kansas Parental Satisfaction Scale: satisfaction in parental role).
2.36. Analysis.
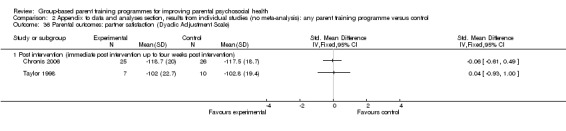
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 36 Parental outcomes: partner satisfaction (Dyadic Adjustment Scale).
2.37. Analysis.
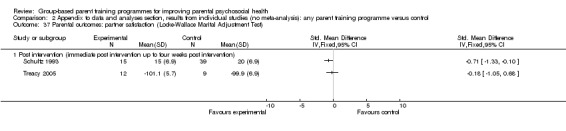
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 37 Parental outcomes: partner satisfaction (Locke‐Wallace Marital Adjustment Test).
2.38. Analysis.
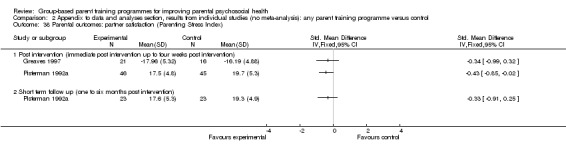
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 38 Parental outcomes: partner satisfaction (Parenting Stress Index).
2.39. Analysis.
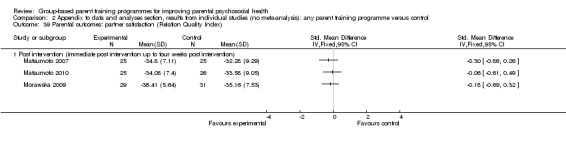
Comparison 2 Appendix to data and analyses section, results from individual studies (no meta‐analysis): any parent training programme versus control, Outcome 39 Parental outcomes: partner satisfaction (Relation Quality Index).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Blakemore 1993.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteers or professionally referred parents of children with ADHD. Sex: 24 mothers; 24 fathers. Age of participants: not stated. Unit of allocation: individual family. Number randomised: 24 families per year (8 group‐based intervention; 8 individual‐based intervention; 8 control). Number used in analysis: number available for analysis n=16 (8 intervention; 8 control)*. Country & setting: Canada; single‐site; recruited from community settings; intervention delivered in an outpatient clinic. Inclusion criteria: parents with at least one child aged 6 to 11 years with evidence of ADHD in a wide range of situations; ADHD evident before the age of six. Exclusion criteria: a serious neurological difficulties; Conduct Disorder in the child with ADHD; a serious marital difficulties. Ethnicity: not stated. Baseline characteristics: not stated. |
|
| Interventions | Three conditions: Cognitive‐behavioural parenting programme; Individual‐based parent programme; wait‐list control. Duration of intervention: 12 weeks; two additional sessions delivered at three and six months after the termination of initial 12 sessions. Length of follow‐up: none. |
|
| Outcomes | Stress (Parenting Stress Index)*. | |
| Notes | *Insufficient data to calculate effect sizes. We requested clarification from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Review authors consider the design of study means personnel would be aware which groups had been assigned to two study conditions. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Investigators report that participants were "presented with a structured interview by a research assistant who is blind to the treatment status of the parent" (page 80). Review authors consider the outcome assessor was blinded and that the non‐blinding of others was unlikely to have introduced bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Investigators report that the data presented "were obtained during the first year of the project with 24 subjects (8 subjects in each of the three treatment conditions)" (page 81). There was no missing data. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Bradley 2003.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of preschoolers with behavioural problems, recruited through advertisements placed in community locations. Sex: 184 mothers; 14 fathers. Age of parents: mean 35.20 years (SD 5.51) intervention; mean 35.88 years (SD 5.73) control. Unit of allocation: individual participant. Number randomised: 198 (89 intervention; 109 control). Number used in analysis: number available for analysis n=174 (81 intervention; 93 control)*. Country & setting: Canada; multi‐site (number unclear); recruited from community settings; intervention delivered in the community. Inclusion criteria: parents experiencing problems managing the behaviour of their 3 or 4 year old children. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: described as largely middle‐class parents; >80% had post‐secondary education; significantly more boys (121) than girls (77); no significant differences between experimental and control groups on age of parents, age of child, or intactness of family. |
|
| Interventions | Two conditions: Psychoeducational programme with videotape modelling (behavioural parenting programme); wait‐list control. Duration of intervention: 7 weeks. Length of follow‐up: 12 months. |
|
| Outcomes | Depressive symptoms (Brief Symptom Inventory)*. Stress (Brief Symptom Inventory)*. |
|
| Notes | *Insufficient data to calculate effect sizes. Clarification was requested from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 8/89 (9%) missing from the intervention condition, and for 16/89 (15%) from the control condition. Reasons for dropout not given. Overall attrition was 11.8% at post‐intervention. Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | High risk | Investigators do not report endpoint / follow‐up data for depressive symptoms from the BSI subscale outcomes. Clarification has been requested, but the trial investigators (email from SJ Bradley to CB on 07/07/10) states that they "are unable to find the data". |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Chronis 2006.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: mothers of child aged 5 to 13 years with ADHD who were already enrolled in the Summer Treatment Program. Sex: all mothers. Age of parents: mean 43.2 years (SD 5.0) intervention; 40.6 years (SD 7.5) control. Unit of allocation: individual participant. Number randomised: 62 (33 intervention; 29 control). Number used in analysis: 51 (25 intervention; 26 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: mother of a child with ADHD who had recently completed 'an intensive behavioural program targeting their child behaviour' (the ADHD Summer Treatment Program). Exclusion criteria: not stated. Ethnicity: children Caucasian 100% intervention group; 92.3% control group. Baseline characteristics: (mothers): 21/62 (34%) lifetime history of major depressive disorder; 2/62 (3%) experiencing current major depressive episode at time of intake; mean HDRS score at intake 5.6 (SD 4.6) intervention and 5.2 (SD 4.4) controls; taking antidepressants 32% intervention and 19% controls; (children): 100% ADHD; adopted 4% intervention and 7.7% controls; IQ 107.4 (SD16.07) intervention and 99.0 (SD 28.7) controls; 11.8% Predominately Inattentive ADHD subtype, 3.9% Predominantly Hyperactive/Impulsive ADHD subtype, 30% oppositional defiant disorder, 58% conduct disorder. |
|
| Interventions | Two conditions: 'Maternal Stress and Coping Group' program, modified version of the 'Coping With Depression Course' (cognitive‐behavioural parenting programme); wait‐list control. Duration of intervention: 12 weeks. Duration of trial: 3 years. Length of follow up: 5 months post‐treatment (intervention group only). |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). Anxiety symptoms (Beck Anxiety Inventory). Stress (Perceived Stress Scale). Self‐esteem (Rosenberg Self‐Esteem). Partner satisfaction (Dyadic Adjustment Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Cunningham 1995.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: 150 volunteer parents of pre‐school children with behaviour problems. Sex: both mothers or fathers (no further information). Age of parents: mean 54.2 years, SD 4.4 (community); mean 52.3 years, SD 4.6 (clinic); mean 54.1 years, SD 4.5 (control). Unit of allocation: individual participant. Number randomised: 150 (48 group‐based; 46 individual‐based; 56 control). Number used in analysis: 78 (36 group‐based; 42 control). Country & setting: Canada; single‐site; recruited from community and outpatient settings; delivered in the community (group intervention) and in an outpatient clinic (individual intervention). Inclusion criteria: parents with children rated at least 1.5 standard deviations above the mean for age and sex on Home Situations Questionnaire. Exclusion criteria: not stated. Ethnicity: 83% Canadian born, 17% immigrants (group intervention); 82% Canadian born, 18% immigrants (control). Baseline characteristics: 83 % two parents, 50% boys (group intervention); 71.4% two parents, 46.4% boys (control). |
|
| Interventions | Three conditions: Cognitive‐behavioural parenting programme; wait‐list control; parent programme delivered on a individual basis. Duration of intervention: 11 to 12 weeks. Length of follow‐up: 6‐months. |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). Confidence (Parenting Sense of Competence Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report that "those returning questionnaires above 90th percentile were block randomly assigned to one of three treatment conditions" (Abstract). Sequence generation process was not described, but information from trial investigator (email from C.Cunningham to NH on 22 Oct 2010) indicates that a random numbers table was used. |
| Allocation concealment (selection bias) | Low risk | Trial investigators report that "sealed questionnaire were returned to the school and forwarded unopened to the research team" (page 1143). Review authors judged that allocation was probably adequately concealed. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Design of study means personnel would be aware which groups had been assigned to an intervention condition. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Trial investigators report "data were collected during home visits by research assistants who were uninformed of the family's condition" (page 1145). Review authors judge that outcome assessors were blind to allocation status of participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Trial investigators report "of the 150 participants beginning the trial, 36 (24%) failed to complete the 6 month follow‐up. The number of dropouts in the respective conditions did not differ significantly" (page 1148). Missing outcome data balanced in numbers across intervention groups. Information from trial investigator (email from C.Cunningham to NH on 22 Oct 2010) indicates that the missing data were balanced between conditions and reflected dropout from the study. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
DeGarmo 2004.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: separated single mothers and their sons aged 6 to 10 years recruited in the community and in divorce court record departments. Sex: all mothers. Age of parents: mean 34.8 years (SD 5.4; range 21.4 to 49.6). Unit of allocation: mother/child dyads. Number randomised: 238 (153 intervention; 85 control). Number used in analysis: 216 (137 intervention; 79 control) at short‐term follow‐up; 179 (116 intervention; 63 control) at long‐term follow‐up. Country & setting: USA; single‐site; recruited from community settings: intervention delivered in the community. Inclusion criteria: single mothers; separated from partner within the prior 3 to 24 months; residing with a biological son of school grade between 1 and 6 inclusive; not cohabiting with a new partner. Exclusion criteria: not stated. Ethnicity: 86% white, 1% African American, 2% Latino; 2% Native American, 9% other. Baseline characteristics: mean separation time 9.2 months; mean 2.1 children per family; 76% receiving public assistance; education: 76% mothers had some academic or vocational training beyond high school; 14% mothers had completed college degree or higher; 4% mothers had not completed high school; 49% mothers clinically depressed as assessed by cut‐off score of 16 on CES‐D. |
|
| Interventions | Two conditions: Parent management training (behavioural parenting programme); no‐treatment control. Duration of intervention: 14 weeks. Duration of trial: 30 months. Length of follow up: 12 months, 18 months, and 30 months. |
|
| Outcomes | Depressive symptoms (Center for Epidemiologic Studies Depression Scale). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from D.DeGarmo to CB on 14 Jul 2010) states "we used block randomisation and fixed allocation 3:2, families were first recruited in blocked cohorts; a data manager used a random number generator and probabilities adjusted for fixed allocation for that cohort". |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from DeGarmo to CB on) states "all assessors, interviewers, and coders were blind to participants assigned group status. Coders and interviewers were mismatched across waves so they were not exposed to the same families wherever possible". |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from D.DeGarmo to CB on 14 Jul 2010) states "all assessors, interviewers, and coders were blind to participants assigned group status. Coders and interviewers were mismatched across waves so they were not exposed to the same families wherever possible". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Fanning 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: families recruited across 15‐month period from four local Head Start preschools. Sex: both mothers and fathers (no further information). Age of parents: mean 31 years intervention; mean 27 years control. Unit of allocation: individual family. Number randomised: 40 families (18 intervention; 22 control). Number used in analysis: 19 families (10 intervention; 9 control). Country & setting: USA; multi‐site (n=4); recruited from community settings: intervention delivered in the community. Inclusion criteria: families with children attending local Head Start preschools; aged 3 to 5 years; from economically disadvantaged backgrounds; monolingual; right‐handed. Exclusion criteria: taking psychopharmacological medication for ADD, ADHD, seizures or depression. Ethnicity: not stated. Baseline characteristics: education: mean 13.29 years (intervention group) and 12.93 years (control group); maternal education: mean 13.21 years (intervention); mean 12.80 years (control). |
|
| Interventions | Two conditions: 'Success in Parenting Preschoolers' (SIP2); wait‐list control. Duration of intervention: 8 weeks. Length of follow‐up: no follow‐up. |
|
| Outcomes | Stress (Ability and Confidence Rating Questionnaire). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Trial investigators report that trial personnel were blind to allocation status of participants (page 69). |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Trial investigators report that outcome assessors were blind to allocation status of participants (page 69). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data for 4/18 (22.2%) were missing from the intervention condition (1 unwilling to attend in evenings; 1 needing to work in evenings, 1 evicted and moved to new area; 1 reason unknown), and for 8/22 (36.3%) from the control condition. Overall attrition was 19% at post‐intervention. Review authors considered the numbers of missing data not closely balanced between conditions. Since reasons for attrition not provided for control group, it is not possible to judge whether the reasons for the missing data differ substantially across the groups. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Fantuzzo 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of the Head Start children recruited from 10 central‐city Head Start centres. Sex: 111 mothers; 5 fathers. Age of parents: mean 30.8 years. Unit of allocation: individual participant. Number randomised: 116 (61 treatment; 55 control). Number used in analysis: 76 (39 treatment; 37 control). Country & setting: USA; multi‐site (n=10); recruited from community settings; intervention delivered in the community. Inclusion criteria: socially isolated parents, who were given a rating of 'low' engagement in term of their adult social interaction in Head Start activities by the teacher of their child. Exclusion criteria: not stated. Ethnicity: 100% African‐American. Baseline characteristics: 84% were the Head Start child's mother, 13% grandmothers or aunts, 3% fathers; 70% families headed by single mothers; average number of children per household 2.78; 40 parents (34.4%) had a history of maltreatment involving their Head Start child. |
|
| Interventions | Two conditions: Community outreach through parent empowerment (COPE); treatment as usual control. Duration of intervention: 10 sessions (duration not stated). Length of follow up: none. |
|
| Outcomes | Stress (Uplifts and Hassles Scales). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Trial investigators report that outcome assessors were blind to allocation status of participants (page 84, col 2). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no missing data. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other forms of bias. |
Farrar 2005.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: mothers of preschool children between 2 and 5 years of age recruited from child care centres, pre‐schools, and stay‐at‐home mothers groups. Sex: all mothers. Age of parents: mean 33 years (SD 6.1; range 20 to 52 years). Unit of allocation: individual participant. Number randomised: 62 (31 experimental; 31 control). Number used in analysis: 62 (31 intervention; 31 control) at post‐intervention; 54 (27 intervention; 27 control) at short‐term follow‐up*. Country & setting: USA; multi‐site (n=8); recruited from community settings; intervention delivered in the community. Inclusion criteria: mothers of pre‐school children aged 2 to 5 years. Exclusion criteria: mothers of children with serious chronic illnesses, special needs or psychiatric diagnoses. Ethnicity: 99.7% Caucasian, 1.6% African American, 3.2% Native American, 3.2% Asian, 3.2% Hispanic. Baseline characteristics: marital state: 85.5% married; 3.2% remarried; 8% separated or divorced; 1.6% widowed; individuals living in their household: mean 4.03 (SD 0.98); number of children: mean 2.13 (SD 0.9); a graduate degree completed: 12.9%; employment: 42.6% |
|
| Interventions | Two conditions: Cognitive parenting programme; attention‐placebo control. Duration of intervention: 30 minutes. Length of follow‐up: 1 month. |
|
| Outcomes | Stress (Parental Stress Scale). Confidence (Kansas Parental Satisfaction Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence allocation by use of random number tables (page 35). |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient to for a judgement to be made, but information from trial investigator (email from R Farrar to CB on 30 Aug 2010) states "the allocation sequence was placed in sealed opaque envelops". |
| Blinding (performance bias and detection bias) Participants | High risk | It is not possible to fully blind participants in this type of study. Additional measures had been taken to reduce the risk of bias that might result from differential behaviours by participants: "one assessor was assigned to each group (control and experimental) in order to ensure that participants did not have contact with members of the other group during pre‐test measurement, intervention and post‐test measurement" (page 44). |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient to for a judgement to be made, but information from trial investigator (email from R.Farrar to CB on 30 Aug 2010) indicates "the control group interventionist was blinded to participant's allocation and study hypotheses". However, the experimental group interventionist was not blind to allocation status of participants and study hypotheses (page 35). |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Trial investigators report "one assessor was assigned to each group (control and experimental) in order to ensure that participants did not have contact with members of the other group during pre‐test measurement, intervention and post‐test measurement’ (page 44). However, the outcome assessors were not blind to allocation status of participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 4/31 (13%) were missing from the intervention condition, and for 4/31 (13%) from the control condition. Reason for missing data not given. Review authors considered the numbers of missing data balanced across the treatment conditions. Overall attrition was 13% at post‐intervention. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Trial investigators report "various one‐way ANOVAs were conducted to evaluate possible differences in participants who completed follow‐up measures versus those who failed to complete such measures. There were no significant differences between completers and non‐completers on the following variables: age of mother, age of child, number of children in the family, number of hours worked per week, and socioeconomic status. Further, there were no significant differences between completers and non‐completers regarding scores on any dependent variables at pre‐test assessment" (page 48). The study appeared to be free of other sources of bias. |
Feliciana 2005.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: low‐to‐middle income Africa American mothers who have at least one child between 5‐12 years old were recruited through letters and flyers at two sites. Sex: all mothers. Age of parents: mean 27.8 years (SD 2.42; range 23 to 33). Unit of allocation: individual participant. Number randomised: 60 (30 intervention; 30 control). Number used in analysis: 60 (30 intervention; 30 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: African‐American mothers; low‐to‐middle income; at least one child aged 5 to 12; interest in participating in a parenting skills training program. Exclusion criteria: not stated. Ethnicity: all African‐American. Baseline characteristics: Intervention group: education: 12% at least 2 years post secondary education; 9% completed at least 4 years of college; marital status: 63% single; 30% married; 7% divorced; number of children: 27% only one child; 67% had 2 or 3 children; 7% 4 or more children. Control group: education: 15% at least 2 years post secondary education; 8% completed at least 4 years of college; marital status: 70% single; 27% married; 3% divorced; number of children: 37% had only one child; 60% had 2 or 3 children; 3% 4 or more children. |
|
| Interventions | Two conditions: Active Parenting Programme; wait‐list control. Duration of intervention: 5 weeks. Length of follow‐up: none. |
|
| Outcomes | Depressive symptoms (Parenting Stress Index). Stress (Parenting Stress Index). Confidence (Parenting Sense of Competence Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report "mothers were selected on first‐come, first‐served basis and randomly assigned to either the control group or the treatment group" (page 40). Insufficient information to make judgment. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Gallart 2005.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of children between the ages of 2 and 8 years, who were experiencing difficulties with their children’s disruptive behaviours. They were recruited following advertising of the Group Triple P program in community through newspapers, pre‐schools, schools, playgroups and health professionals. Sex: 46 mothers; 3 fathers. Age of parents: not stated. Unit of allocation: individual participant. Number randomised: 49 (16 full intervention; 17 modified intervention; 16 control). Number used in analysis: 32 (16 full intervention; 16 control) Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: parenting a child between 2 and 8 years old; experiencing difficulties with child's disruptive behaviours. Exclusion criteria: not stated. Ethnicity: English‐speaking background (56%); others from various backgrounds including Italian, Maltese, Serbo‐Croatian, Armenian, Vietnamese and Uruguayan; children were aged 3 to 8 years (mean 5.4, SD 1.5 years). Baseline characteristics: 100% scored above the clinical cut‐off on at least one of the measures at the commencement of the program; three quarters had left school prior to year 12. |
|
| Interventions | Three conditions: Group Triple‐P program; modified Group Triple‐P program (no phone contact); wait‐list control. Duration of intervention: 8 weeks full intervention; 4 weeks modified intervention (although endpoint measures at 8 weeks). Duration of trial: 8 weeks. Length of follow up: none. |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scales). Anxiety symptoms (Depression Anxiety Stress Scales). Stress (Depression Anxiety Stress Scales). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report "on registering, participants were randomly assigned to one of three conditions’ (page 75). Insufficient information to make judgment, but information from trial investigator (email from S Matthey to CB on 07 Nov 2010) states "randomisation was by out of the hat method". |
| Allocation concealment (selection bias) | High risk | The trial investigators confirmed that allocation was not concealed. |
| Blinding (performance bias and detection bias) Participants | High risk | Participants were not fully blinded to allocation. Trial investigators report “participants were kept blind to the fact that there were two different formats of the program. Those in the ‘4 only’ condition were informed that the program had been slightly modified and did not include the telephone sessions described in their workbook. Those in the control condition were sent the initial assessment package, and when this was returned were informed that the program was full, and that they would be allocated to the next available program (this was offered them when they were mailed their post‐assessments)” (page 75). |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from S Matthey to CB on 07 Nov 2010) states "personnel not blinded". |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from S Matthey to CB on 07 Nov 2010) states "personnel not blinded". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Overall, data from 5/54 (9%) of those randomised were missing and results given only for the 49 with pre‐post data. Breakdown of missing data by allocated group not given. Reasons for missing data not given. Insufficient information to judge whether missing data balances across treatment conditions or whether the reasons for the missing data differ substantially across the groups. We requested clarification from the trial investigators, but no further information was available (email from S Matthey to CB on 07 Nov 2010). |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Gammon 1991.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteers or professionally referred parents of children with a disability. Sex: all mothers. Age of parents: mean 38.8 years, intervention; mean 37.8 years, control. Unit of allocation: individual participant. Number randomised: 42 (24 intervention; 18 control). Number used in analysis: number available for analysis not stated. Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: the parents must have known about their child's disability for at least 6 months and have verbally indicated that they were currently having difficulties related to child's behaviour; the parents were available to participate for the 10‐week duration of the study. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: not stated. |
|
| Interventions | Two condition: Cognitive‐behavioural parenting programme; no‐treatment control. Duration of intervention: 10 weeks. Duration of trial: 10 weeks. Length of follow‐up: none. |
|
| Outcomes | Stress (Profile of Mood State)*. Stress (Questionnaire on Resources and Stress)*. |
|
| Notes | *Insufficient data to calculate effect sizes. Clarification was requested from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Trial investigators do not report the numbers of participants completing the study. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The review appeared free of other forms of bias although, as the trial investigators note, "the absence of a placebo control group suggest that the role of social desirability effects cannot be excluded in accounting for the results" (page 255). |
Gardner 2006.
| Methods | Parallel randomised control trial. | |
| Participants |
Participants: parents (main carers) of child aged 2‐9 years, who was referred for help with conduct problems. Sex (main carers): 72 mothers; 4 fathers. Age of parents: 31 years (SD 6.7) intervention; 30 years (SD 4.7) control. Unit of allocation: individual participant. Number randomised: 76 families (44 intervention; 32 control) Number used in analysis: 67 (39 intervention; 28 control) for 'depressive symptoms' outcome; 65 (37 intervention; 28 control) for 'confidence' outcome. Country & setting: UK; multi‐site (n=9); recruited from community settings; intervention delivered in the community. Inclusion criteria: parents (main carers) of child aged 2‐9 years, who was referred for help with conduct problems, and who scored above clinical cut‐off (>10 problems) on Eyberg ‘problem scale. Parent had to be able to attend group and communicate in English. Exclusion criteria: child severely disabled; child in temporary care; parent drug addicted; previous attendance at Family Nurturing Network, the charity in which the intervention took place. Ethnicity: not stated. Baseline characteristics: 47% headed by single parent; 29% moderate‐severe depression; 14% severe depression. Conduct problem scores were high: mean 21 on Eyberg problem scale compared to clinical cut‐off of 11 and population average of 4‐5; children: female 26; male 74%. |
|
| Interventions | Two conditions: Webster‐Stratton ‘Incredible Years'; wait‐list control. Duration of intervention: 14 weeks. Length of follow up: 18 months post‐recruitment |
|
| Outcomes | Depressive symptoms (Back Depression Inventory). Confidence (Parenting Sense of Competence Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report “a computer‐generated list was used for random allocation of families" (page 1125, col 2). The allocation sequence was adequately generated. |
| Allocation concealment (selection bias) | Low risk | Trial investigators report "the administrator, therapists and researchers were unaware of the randomisation sequence. The sequence was stored in numbered, opaque, tamper‐proof envelopes, held by an administrator who was not involved with recruitment, therapy or evaluation. Following research assessments, names of newly recruited families were passed to the administrator who allocated families in strict order of recruitment according to the next envelope in the sequence" (page 1125, col 2). Review authors judge that concealment through use of central administrator is an acceptable method of minimising risk of bias. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge it is not possible to blind participants in this type of study. In order to enhance blindness of outcome assessors, the parents were asked not to reveal intervention status to them (they were reminded about it by letter, phone, and at each visit) |
| Blinding (performance bias and detection bias) Personnel | Low risk | Trial investigators report "the administrator, therapists and researchers were unaware of the randomisation sequence’ (page 1125, col 2). Several strategies were used to enhance blindness of researchers: families were reminded by letter, phone and at each visit not to reveal intervention status. Researchers did not administer consumer satisfaction questionnaires; these were mailed to a different researcher for analysis. Wherever possible, staff coded observation tapes of families they had not themselves visited" (page 1126, col 1). Review authors judge personnel were adequately blinded. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Trial investigators report “all assessments were conducted in the home by researchers who were unaware of families’ allocation” (page 1125). Review authors judge knowledge of the allocated interventions was adequately prevented regarding the outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At post‐intervention point (6 months), 5/44 (11%) dropped out from treatment group and none dropped out from the control group. Investigators report that "families lost to follow‐up did not differ significantly from those retained’ (page 1127, col 2), although reasons for missing data not given. However, number given for ANCOVAs at post‐intervention was 66 (37 intervention and 29 control) suggesting 7/44 (16%) missing data from intervention group and 3/32 (9%) missing from control group. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Study appeared to be free of other forms of bias. Investigators note that the study was originally designed as a 3‐arm trial but was effectively reconfigured as a 2‐arm design due to poor recruitment. They describe how they used the same allocation list throughout to ensure families had the same probability of allocation to an intervention condition as in the original protocol, and the 11 families allocated to the third arm (‘Veritas’ programme) were not included in the analysis. |
Greaves 1997.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: mothers of pre‐school children attending a centre for children with Down's syndrome. Sex: all mothers. Age of parents: not stated. Unit of allocation: individual participant. Number randomised: 54 (21 intervention; 17 comparative‐treatment; 16 control). Number used in analysis: 37 (21 intervention; 16 control). Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: mothers of pre school children attending a centre for children with Down syndrome. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: not stated. |
|
| Interventions | Three condition: Rational Emotive parent education (cognitive‐behavioural parenting programme); Applied Behaviour Analysis programme; no‐treatment control. Duration of intervention: 8 weeks. Length of follow‐up: none. |
|
| Outcomes | Depressive symptoms (Parenting Stress Index). Stress (Parenting Stress Index). Anger (Berger Feeling Scale). Guilt (Berger Feeling Scale). Partner Satisfaction (Parenting Stress Index). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Trial investigators do not report any missing data for change scores at endpoint. They note that participants did not complete measures at 6‐month follow up, and present no follow up data. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Gross 1995.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteer parents of toddlers with behaviour difficulties. Sex: 46 mothers and fathers (no further information). Age of parents: mean 33 years (SD 4.8) mothers; 33 years (SD 4.9) fathers. Unit of allocation: individual family. Number randomised: 24 (18 intervention; 6 control). Number used in analysis: 16 (10 intervention; 6 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: both parents of child aged between 24 and 36 months who met criteria for behavioural difficulties; parent willing to participate in a 10‐week intervention and complete a serious of questionnaires and observations. Exclusion criteria: not stated. Ethnicity: 80% Caucasian mothers; 75% Caucasian fathers. Baseline characteristics: median education among both parents was some college; unemployment: 9 (37.5%) mothers; 1 (4%) father; 20 (83%) boys. |
|
| Interventions | Two conditions: Webster‐Stratton parenting programme; no‐treatment control. Duration of intervention: 10 weeks. Length of follow‐up: 3‐months. |
|
| Outcomes | Depressive symptoms (Center for Epidemiological Studies Depression Scale). Stress (Parenting Stress Index). Confidence (Toddler Care Questionnaire). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report "the 24 families were randomly assigned to the intervention group (n=18) or control group (n=6)" (page 490). Information reported insufficient for a judgement to be made, but information from trial investigator (email from D Gross to NH on 22 Oct 2010) indicates that a random numbers table was used. |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from D Gross to NH on 22 Oct 2010) indicates that concealment was achieved by use of a third party (a statistician). |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from D Gross to NH on 22 Oct 2010) states that trial personnel could not be blinded "because we were running the intervention". |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Information reported insufficient for a judgement to be made. Information from trial investigator (email from D Gross to NH on 22 Oct 2010) states "research assistants collecting parent report data were not told which conditions parents were in, but parents may have shared the information. Research assistants coding the parent‐child interactions only had access to video recorded parent‐child data and were fully blinded to parent condition". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | At post‐intervention, 7/18 (39%) missing from treatment group and 0/6 missing from control group. Numbers do not appear to be balanced between conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Gross 2003.
| Methods | Cluster randomised controlled trial. | |
| Participants |
Participants: parents of multiethnic toddlers two to three years of age in day care in low‐income urban communities, recruited from the general population of day care attenders. Sex: 238 (90%) mothers; 13 (4.9%) fathers; 4 (1.5%) foster parents; 9 (3.6%) grandparents or other relatives. Age of parents: mean 27.9 years (SD 6.8). Unit of allocation: a day centre (4 PT+TT; 4TT; 3C; three control centres became 3 PT centres with newly recruited participants). Number randomised: 11 centres (4 PT+TT; 4TT; 3C; three control centres became 3 PT centres with newly recruited participants); 264 participants (75 parent condition; 78 combined parent and teacher condition; 52 teacher condition; 59 control condition). Number used in analysis: 6 centres (3 PT; 3C); 134 participants (75 parent condition; 59 control). Country & setting: USA; multi‐site (n=11); recruited from community settings; intervention delivered in the community. Inclusion criteria: parents: legal guardian of a 2 to 3 year old child (if more than one in this age range, the younger child was selected for inclusion); enrolled in a day centre in Chicago that serves low‐income families; completed all baseline assessments; centres: with 90% of enrolled families meeting income‐eligibility requirements for subsidised child care; licensed by the Dept of Child and Family Services; serving families of 2‐3 year olds. Exclusion criteria: not stated. Ethnicity: African‐American 57%, Latino 29%, white 3%, multiethnic 4%, other 6%. Baseline characteristics: ; education: 28.4% high school diploma; 14.4% left before completing high school; employment: 56.7 full time employment; 13% part‐time employment; 4.3% unemployed; marital status: 36.1% married; 30.8% single; 8.2% partnered. |
|
| Interventions | Four conditions: Webster‐Stratton parent training (PT), parent and teacher training (PT plus TT); teacher training (TT), wait‐list control. Intervention consists of Incredible Years BASIC parenting programme. Duration of intervention: 12 weeks. Length of follow‐up: 6 months; 12 months. |
|
| Outcomes | Depressive symptoms (Center for Epidemiological Studies Depression Scale). Stress (Everyday Stress Index). Confidence (Toddler Care Questionnaire). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigators report "centres were assigned to groups of centres so that the grouped centres were matched on day care size, ethnic composition, percentage of single‐parent families, median income, and day care centre quality. These grouped centres were than randomly assigned to one of three conditions: PT + TT (n=4), TT (n=4) or C (n=3) conditions. C centres received no intervention for at least 1 years, after which new parents were recruited and these centres became PT centres" (page 263). Information reported insufficient for a judgement to be made, but information from trial investigator (email from D Gross to CB on 11 Oct 2010) indicates that a random numbers table was used. |
| Allocation concealment (selection bias) | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from D Gross to CB on 11 Oct 2010) indicates that sealed opaque envelopes were not used. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from D Gross to CB on 11 Oct 2010) state that "the research assistant collecting the surveys from parents could not be blinded". |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Trial investigators report "videotaped play sessions were later coded by European American observers (in Seattle) who were blind to study hypotheses and participant's group assignment" (page 265). Outcome assessors were blinded for the 'observer rated child behaviour problems' outcome. However, no information for parent self‐report measures. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Trial investigators do not supply a full breakdown of missing data by allocation condition due to dropouts. They state that 47 were missing from the PT+TT condition and 9 missing from the TT and C conditions. Reasons for attrition given for the sample overall and not by allocation condition: 20 lack of time; 17 schedule conflicts; 12 too much stress; 4 child left day centre; 3 failed to attend; 3 staff unable to locate. Additionally "the growth care models presented in this article are based on 208 participants who remained in the study. To assess the effects of dropouts on the results on these analyses, we also run the final growth curve on the initial sample of 246 participants. The pattern of significant parameters remained unchanged as a result of using the larger sample. This indicate that participants attrition did not modify the interpretation of results" (pages 266‐277). |
| Selective reporting (reporting bias) | Low risk | All prospectively stated outcomes were reported. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Gross 2009.
| Methods | Cluster randomised controlled trial. | |
| Participants |
Participants: parents or legal guardians of a 2‐4 year old child enrolled at the day care participating centre. Sex: 225 mothers, 17 fathers, 4 foster parent, 5 grandparents, and 2 other (sex of participants reported only on 253 participants who were included in analysis). Age of parents: not stated. Unit of allocation: a day care centre. Number randomised: 7 day centres (3 intervention; 4 control); 292 participants (156 intervention; 136 control). Number used in analysis: 7 day centres (3 intervention; 4 control); 253 participants (135 intervention; 118 control); number used in analysis for the 'depressive symptoms', 'stress' and 'confidence' outcomes: 247 (133 intervention; 114 control). Country & setting: USA; multi‐site (n=7); recruited from community settings; intervention delivered in the community. Inclusion criteria: Day care centre: had over 90% of enrolled families meeting income‐eligibility requirements for subsidised child care; was licensed by the Dept of Child and Family Services; provided full‐day child care; enrolled at least 60 children in the target age group; had a space on site to run a weekly parent group, and the director was willing to allow the site to be randomised. Participant: a parent or a legal guardian of a 2 to 4 year old child (if more than one in this age range, the youngest child was selected for inclusion); should speak English. Exclusion criteria: not stated. Ethnicity: 149 African‐American, 83 Latino, 12 white (not Latino), 9 other (intervention group had more Latino parents than control group, P<0.01). Baseline characteristics: There were no differences between two groups on parent age, educational level, employment status, marital status, or child age; there were significant differences between these two groups on parent/race ethnicity and child gender. |
|
| Interventions | Two conditions: Webster‐Stratton parent programme; wait‐list control. Duration of intervention: 12 weeks. Length of follow‐up: 6 months; 12 months. |
|
| Outcomes | Depressive symptoms (Center for Epidemiological Studies Depression Scale). Stress (Everyday Stress Index). Confidence (Toddler Care Questionnaire). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report “The day care centres were matched on size, racial/ethnic composition, percentage single‐parent households, and median income and randomly assigned to an intervention or control condition” (page 56). Information reported insufficient for a judgment to be made, but information from trial investigator (email from D Gross to CB on 11 Oct 2010) indicates that a random numbers table was used. |
| Allocation concealment (selection bias) | High risk | Information reported insufficient for a judgment to be made, but information from trial investigator (email from D Gross to CB on 11 Oct 2010) indicates that sealed opaque envelopes were not used. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgment to be made, but information from trial investigator (email from D Gross to CB on 11 Oct 2010) stated that "the research assistant collecting the surveys from parents could not be blinded". |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information from trial investigator (email from D Gross to CB on 11 Oct 2010) indicated that "the DPICS coders were blinded”. However, no information for parent self‐report measures. Information reported insufficient for a judgment to be made |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The trial investigators report that “Thirty nine (13%) participants dropped out of the study before their 1 year follow‐up. Attrition in the control condition was attributed to 17 parents (12.5%) who were lost to follow‐up and 1 parent (0.7%) who withdrew. Attrition in the intervention condition was attributed to 11 parents (7.1%) lost to follow‐up, 9 parents who withdrew, and 1 parents (5.8%) who withdrew, and 1 parent who was dropped from the study due to emotional problems that interfered with her ability to participate in group discussion” (page 59). For ‘depressive symptoms’, ‘stress’ and ‘confidence’ outcomes 23/156 participants (14.7%) dropped out from treatment group and 18/136 participants dropped out from the control group (13.2%). Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. Overall attrition was 14%. |
| Selective reporting (reporting bias) | High risk | The three outcomes, ‘depressive symptoms’ (CESD), ‘stress’ (ESI) and ‘confidence’ (TCQ) were not pre‐specified, nor reported, although they were measured. The authors provided the data (email from D Gross to CB on 27/12/10) stated “We did not include them in the 2009 paper because of (1) length and (2) their lack of association with the outcome variables, and therefore, did not contribute to the results”. |
| Other bias | Low risk | Trial investigators report “There were significant differences between intervention and control parents on parent race/ethnicity and child gender. To control for baseline differences, these variables were included as co‐variates in the analytic models (page 56). The study appears to be free of other sources of bias. |
Gutierrez 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: Hispanic Spanish speaking mothers of a school‐age child with behavioural and emotional difficulties. Sex: all mothers. Age of parents: mean 35.2 years. Unit of allocation: individual participant. Number randomised: 70 (number randomised to the four conditions; no further information). Number used in analysis: 34 (17 intervention; 17 wait‐list control). Country & setting: USA; single site; recruited from community settings; intervention delivered in the community. Inclusion criteria: mother; Hispanic and Spanish speaking; migrant farm workers; having a school‐age child (enrolled in Kindergarten to 5th grade) in Southern California; eligible to receive migrant education services; referred by the school districts Student Assistance Program for students experiencing behavioural and emotional problems. Exclusion criteria: past or present involvement in a parent training program. Ethnicity: 100% Spanish‐speaking Hispanic. Baseline characteristics: 74% married; 16% educated beyond 12th grade; mean 2.3 children in family; mean age of child = 8.0 years. |
|
| Interventions | Four conditions: Behavioural parenting program (BPP); STEP (a modified form of family therapy based on Adlerian therapy); wait‐list control; attention‐placebo control. Duration of intervention: 8 weeks. Length of follow‐up: 3 months. |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | We used data from the BPP arm only compared with wait‐list control to avoid double counting of participants in the control group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 68/70 randomised participants completed the study. The analyses were performed on the completers. The missing data did not differ substantially across the groups. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Hanisch 2010.
| Methods | Cluster randomised controlled trial. | |
| Participants |
Participants: parents of children aged between 3 and 6 years, who were attending kindergartens. Sex: both mothers and fathers (no further information). Age of parents: not stated. Unit of allocation: kindergarten. Number randomised: 58 kindergartens randomised (32 intervention; 26 control); 155 participants randomised (91 intervention group, 64 control). Number used in analysis: 54 kindergartens (31 intervention; 23 control); 121 families (75 intervention; 46 control). Country & setting: Germany; multi‐site (n=54); recruited from community settings; intervention delivered in the community. Inclusion criteria: families with children aged 3‐6 years; children with externalising behavioural problems indicated by scores above the 85th percentile for scores on a screening instrument derived from the Child Behaviour Checklist. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: mean CBCL scores: 43.14 (SD 20.99) and 39.72 (SD 19.35); mean mother‐assessed symptoms: 0.11 (SD 0.84) and ‐0.14 (SD 0.75). |
|
| Interventions | Two conditions: Prevention Programme for Externalising Problem behaviour (behavioural parenting programme); no‐treatment control. Duration of intervention: 10 weeks. Length of follow‐up: 8 weeks. |
|
| Outcomes | Depressive symptoms (Depressive Anxiety Stress Scale). Anxiety symptoms (Depressive Anxiety Stress Scale). Stress (Depressive Anxiety Stress Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report "each of the kindergartens was randomly assigned to either the intervention group of the control group so that any one teacher was not simultaneously teaching children in both groups" (page 98). Information reported insufficient for a judgement to be made. The trial investigator (e‐mail from C Hanisch to CB. on 19 Nov 2010) confirmed that states that lots corresponding to participating kindergartens were drawn manually. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | ‘Research assistants were blind to treatment group membership’ (page 99). However: ‘the blindness of the research assistants to the family’s group membership could not be fully guaranteed as a few families gave away their group membership during the home visit’ (page 107). |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Trial investigators report "research assistants were blind to treatment group membership’ (page 99). However, "the blindness of the research assistants to the family’s group membership could not be fully guaranteed as a few families gave away their group membership during the home visit" (page 107). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16/91 (18%) missing from experimental group (families declined to participate), and 18/64 (28%) missing from control group (families declined to participate). Trial investigators report "the pre‐test composite scores for families that dropped out of the study between the pre‐ and post‐tests did not differ from those that remained in the study. However, mothers who dropped out after the pre‐test assessment had a lower level of education than those who remained in the study (P<.001)" (page 103). |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared free of other forms of bias. "There were no significant differences between these groups for children’s age and gender, or symptom severity on the CBCL total, PCL, ADHD, or PCL ODD. Mothers and fathers of both groups reported similar levels of school education and vocational training". However, ". . . children in the intervention group were rated as more severely impaired than children in the control group" (page 103). |
Hiscock 2008.
| Methods | Cluster randomised controlled trial. | |
| Participants |
Participants: English speaking mothers of 8 months old children attending primary care nursing centres. Sex: all mothers. Age of parents: mean 33 years (SD 4.8) intervention; 33.3 years (SD 4.7) control. Unit of allocation: centre. Number randomised: 40 cluster centres, 733 families (18 centres and 329 families intervention; 22 centres and 404 families control) Number used in analysis: 654‐671 families (291‐298 intervention; 363‐373 control). Country & setting: Australia; multi‐site (n=40); recruited from community settings; intervention delivered in the community. Inclusion criteria: English speaking mothers of 8 month‐old children attending well‐child appointments. Exclusion criteria: mothers with insufficient English to complete the questionnaires. Ethnicity: not stated. Baseline characteristics: married or cohabiting (96.7% intervention; 96.5% control); employment (25% intervention; 29.7% control); English spoken at home (96.4% intervention; 95.8% control); education: did not complete high school (19.8% intervention; 21% control); completed high school (34.5% intervention; 32.2% control); completed tertiary/postgraduate (45.7% intervention; 46.8% control). Mental health: depression score (mean=4.1, SD=5.4 intervention group; mean=3.5, SD=4.5 control); depressed (14% intervention group; 9.2% control); anxiety score (mean=2.2, SD=3.6 intervention group; mean=1.9, SD=3.1 control); anxious (9.8% intervention group; 6.7% control); stress score (mean=9.0, SD=6.5 intervention group; mean=8.8, SD=6.3 control); stressed (14% intervention group; 12.4% control). |
|
| Interventions | Two conditions: universal parenting (behavioural parenting) programme; treatment as usual control. Duration of intervention: 7 months. Duration of trial: 16 months. Length of follow‐up: 3 months; 9 months. |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scales). Anxiety symptoms (Depression Anxiety Stress Scales). Stress (Depression Anxiety Stress Scales). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigators report "as we considered balance on socioeconomic status to be important, randomisation was done with a computer generated allocation sequence by matching pairs of centres according to their closeness of their average socioeconomic disadvantage scores and then randomising one centre from each pair to the intervention arm" (page 3, col 2). Random sequence allocation by computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Investigators report "an independent statistician randomly allocated maternal and child health centres (and therefore their families), stratified by local government area, to intervention and control arms. Within each of the local government areas, a list of participating centres was created" (page 3, col 2). Concealment achieved by use of central allocation (an independent statistician) such that participants and any investigator enrolling participants could not foresee assignment. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgement to be made but information from trial investigator (e‐mail from H Hiscock to CB on 11 Oct 2010) states "the trial personnel were not blinded to the family group (intervention or control) status as we coordinated the bookings of their group sessions". |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from H.Hiscock to CB on 11 Oct 2010) states "all outcomes were collected by questionnaire and we remained blinded to family group status during data collection and analyses. Analyses were done by a statistician who was independent of study recruitment and intervention delivery". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 31/329 (9.4%) missing from the intervention condition (failure to return questionnaires in each case), and for 30/404 (7.4%) from the control condition (by 18 month evaluation point). Data for 37/329 (11.2%) missing from the intervention condition (failure to return questionnaires in each case), and for 40/404 (9.9%) from the control condition (by 24 month evaluation point). Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. Overall attrition was 9.5%. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Hutchings 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents from socially disadvantaged families, recruited from 11 Sure Start areas. Sex: both mothers and fathers (no further information). Age: not reported for parents; children: control group, mean 46.2 (SD 4.2) months; intervention group, mean 46.4 (SD 6.6) months. Unit of allocation: parent‐index child pair. Number randomised: 153 (104 intervention; 49 control). Number used in analysis: 153 (104 intervention; 49 control). Country & setting: UK; multi‐site (n=11); recruited from community settings; intervention delivered in the community. Inclusion criteria: socially disadvantaged families with a child aged 3 or 4 years; child living with primary carer; child scoring above the clinical cut‐off on either the Eyberg problem or the Eyberg intensity scale (11 or 127); primary carer able to attend at group times. Exclusion criteria: none reported. Ethnicity: 14% of children were Welsh speaking; 41% single parents; mean age of mother at birth of first child 20.5 (control) and 21.4 years (intervention). Baseline characteristics: target child: 57% boys intervention; 66% boys control. |
|
| Interventions | Two conditions: Webster‐Stratton ‘Incredible Years’ parenting programme; wait‐list control. Duration of intervention: 12 weeks. Length of follow up: 6 months. |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). Stress (Parenting Stress Index). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report that "participants were blocked randomised by area after stratification by sex and age, using a random number generator" (p.3, col 2). Random sequence allocation by computer‐generated random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Trial investigators report “researchers blind to allocation carried out interviews and observations” (p.3, col 2). Review authors judge that personnel were blinded. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Trial investigators report “observers were blind to allocation” (p.3, col 1). No specific details given on blinding of those who scored the self‐report (questionnaire) outcome measures used in this review. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 18/104 (17%) were missing from the intervention condition (9 formally withdrew before intervention; 9 could not be contacted), and for 2/49 (4%) from the control condition (1 formally withdrew before follow up; 1 could not be contacted). Thus although numbers of missing data do not balance between condition, the reasons for the missing data do not appear to differ substantially across the groups. Review authors judge incomplete data were adequately addressed. Overall attrition was 10.5%. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Investigators report “Competing interests: JH is paid by Incredible Years for running occasional training courses in the delivery of the parent programme . . .” (page 7600). This study appears to be free of other forms of bias. |
Irvine 1999.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: families of at‐risk middle school students. Sex: both mothers and fathers (no further information). Age of parents: intervention: 36.6 years (SD 5.4) mothers; 39.3 years (SD 7.1) fathers; control: 37.7 years (SD 6.97) mothers; 39.7 years (SD 7.07) fathers. Unit of allocation: individual family. Number randomised: 303 (151 intervention; 152 control). Number used in analysis: 241 (106 intervention; 135 control) at post‐intervention; 161 (67 intervention; 94 control) at 6 month follow‐up; 109 (51 intervention; 58 control) at 12 month follow‐up. Country & setting: USA; multi‐site (n=8); recruited from community settings; intervention delivered in the community. Inclusion criteria: students with more than three risk factors referred by school or by social service agency staff; the risk factors were: behavioural, externalising, substance use, deviant peer associations, academic deficiencies, and family stress. Exclusion criteria: families currently receiving other treatment. Ethnicity: 88% Caucasian. Baseline characteristics: there were no significant differences between conditions on family status, education, cultural background or target child's gender. |
|
| Interventions | Two condition: adolescent transition programme (behavioural parenting programme); wait‐list control. Duration of intervention: 12 weeks. Duration of trial: 4 years. Length of follow‐up: 3 months, 6 months; 12 months. |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report that families "were randomly assigned to a condition immediately following their recruitment" (page 813). Information from trial investigator (email from B Irvine to NH on 22 Oct 2010) indicates that a random numbers table was used. |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made. Information from trial investigator (e‐mail from B Irvine to NH on 22 Oct 2010) indicates that allocation concealment was achieved through use of a central allocation facility. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgement to be made. Information from trial investigator (email from B Irvine to NH on 22 Oct 2010) indicates that personnel were not blinded. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Information reported insufficient for a judgement to be made. Information from trial investigator (email from B Irvine to NH on 22 Oct 2010) states that the term 'outcome assessors' was not generally relevant to this study but that "most data were collected via mailed parent surveys". Phone interviewers "did know the allocation status" but "coders of the phone interview recordings did not know the allocation status". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Rates of attrition at post‐treatment were 45/151 (30%) in the treatment group and 17/152 (11%) in the control group, and at 6‐month follow up were 84/151 (56%) in the treatment group and 58/152 (38%) in the control group. Although numbers of missing data were not balanced between conditions, trial investigators conducted a comparison on each of the dependent variables, looking for a main effect between study drop out and the remaining participants across all of the subsequent time points and found that the study dropouts and the parents who remained differed on only one variable (the laxness scale of the PSA that measures parental limit setting). |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Joachim 2010.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of 2 to 6 year old children showing problem behaviour during shopping trips. Sex: 44 mothers; 2 fathers. Age of parents: mean 33.78 years (SD 5.21). Unit of allocation: individual participant. Number randomised: 46 (26 intervention; 20 control). Number used in analysis: 40 (22 intervention; 18 control). Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: parents of 2 to 6 year old children showing problem behaviour during shopping trips; residing within Brisbane metropolitan area. Data gathered from one parent only, usually the mother (or the father if he was the primary caregiver). Exclusion criteria: child had a disability; child had a chronic illness; parents currently consulting a professional for child behaviour difficulties or other personal problems Ethnicity: 91% Australian ethnic background. Baseline characteristics: 52% employed; 78.3% of children lived with parent who were married; target child: 54.3% boys; 45.7% girls. |
|
| Interventions | Two conditions: brief parent discussion programme (Triple‐P parenting programme); wait‐list control. Duration of intervention: two hours. Length of follow‐up: 6 months. |
|
| Outcomes | Depressive (Depression Anxiety Stress Scales). Anxiety symptoms (Depression Anxiety Stress Scales). Stress (Depression Anxiety Stress Scales). Confidence (Parenting Task Checklist). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from S Joachim to CB on 27 Oct 2010) indicates that computer generated random numbers were used. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. but information from trial investigator (email from S Joachim to CB on 27 Oct 2010) states "families were assigned sequentially to condition according to the list". |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from S Joachim to CB on 27 Oct 2010) states "the discussion groups were run with participants from both intervention and wait‐list group participating at the same time and practitioners running the groups were blinded to condition". |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 4/26 (15.4%) were missing from the intervention condition (lack of time, problems with childcare, and family illness), and for 2/20 (10%) from the control condition (lack of time, problems with childcare, and family illness). Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. Overall attrition was 13%. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | |
Joyce 1995.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteer parents with elementary school aged children. Sex: 35 (73%) mothers; (27%) 13 fathers. 12/48 (25%) were parents from one family. Age of participants: not stated. Unit of allocation: individual participant. Number randomised: 48 (32 intervention; 16 control). Number used in analysis: 48 (32 intervention; 16 control). Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: non‐clinical parent population of elementary school aged children in a private school in Melbourne. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: marital status: no single or divorced parents; one widow; sample was heterogeneous with respect to educational level. |
|
| Interventions | Two conditions: Rational Emotive parent education (cognitive‐behavioural parenting programme); wait‐list control. Duration of intervention: 9 sessions (assumed 9 weeks). Length of follow‐up: no follow‐up. |
|
| Outcomes | Anxiety symptoms (State‐Trait Anxiety Inventory). Anger (Berger Feeling Scale). Guilt (Berger Feeling Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report that parents "were randomly assigned to four experimental and two control groups; the two group leaders were then randomly assigned to the experimental groups" (page 58). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear whether there was missing data. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Larsson 2009.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of 4 to 8 year old children with oppositional or conduct problems. Sex: both mothers and fathers (no further information). Age of parents: mothers: mean 33.7 years (SD 6.3) intervention; mean 34.9 years (SD 6.8) control; fathers: mean 35.2 years (SD 5.7) intervention; mean 37.0 years (SD 8.0). Unit of allocation: individual family. Number randomised: 127 (47 parent training group; 52 parent plus child training group; 28 control group). Number used in analysis: 71 (43 parent training group; 28 control). Country & setting: Norway; multi‐site (n=2); recruited from outpatient settings; intervention delivered in an outpatient clinic. Inclusion criteria: parents of 4 to 8 year old children with sub‐threshold or clinical diagnosis of oppositional defiant disorder and/or conduct disorder according to DSM‐IV criteria. Exclusion criteria: parents of children with gross physical impairment; sensory deprivation; intellectual deficit; autism; receiving another psychotherapeutic intervention; receiving medication for ADHD unless this initiated >6 months prior to study entry. Ethnicity: 80 families were native Norwegians. Baseline characteristics: one parent families: mean 16 (SD 37.2) intervention; mean 8 (SD=32.0) control; mothers not completing high school: mean 11 (SD 23.9) intervention; mean 8 (SD=33.3) control; fathers not completing high school: mean 9 (SD 25.0) intervention; mean 6 (SD=31.6) control; target child: 60 (80%) boys. |
|
| Interventions | Three conditions: Basic Webster‐Stratton Incredible Years parenting program; Basic Incredible Years Parenting Program plus child treatment; wait‐list control. Duration of intervention: 12 to 14 weeks. Length of follow‐up: 12 months (the design resulted in loss of control group to follow‐up). |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 6/51 (12%) were missing from the intervention condition (4 never started, 2 dropped out; reasons not given), and for 2/30 (7%) from the control condition (2 withdrew; reasons not given). Review authors considered the numbers of missing data reasonably likely to be balanced across the treatment conditions. ITT analysis performed. Overall attrition 9.5%. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Investigators report “the allocation of the participants did not differ significantly in regard to demographic variables, diagnostic status or use of medication because of ADHD” (page 43, col 2). The study appeared to be free of other sources of bias |
Lipman 2005.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: single mothers of children aged 3 to 9 years who were recruited through advertisements in community flyers at various locations. Sex: all mothers. Age of parents: mean 32.4 years (SD 6.7) intervention. mean 32.3 years (SD 6.1) control. Unit of allocation: individual participant. Number randomised: 116 (59 intervention; 57 control) Number used in analysis: 101 (53 intervention; 48 control) at short‐term follow‐up; 83 (50 intervention; 33 control) at long‐term follow‐up. Country & setting: Canada; multi‐site (number unclear); recruited from community settings; intervention delivered in the community. Inclusion criteria: single mothers; at least one child aged 3 to 9 years; able to speak English. Exclusion criteria: acute psychiatric crisis (for example: psychotic or suicidal behaviour); threat of violence. Ethnicity: not reported; difference between groups significant at P<0.05 in terms of maternal education, employment in last year, income, financial pressure and sources of financial support in past year. Baseline characteristics: difference between groups significant at P<0.05in terms of treated for 'nerves' or nervous condition in last 6 months (70% in intervention; 46% in control). |
|
| Interventions | Two conditions: Social support and education (cognitive‐behavioural parenting programme); wait‐list control. Duration of intervention: 10 weeks. Length of follow‐up: 4 months; 10 months; 17 months. |
|
| Outcomes | Depressive symptoms (Center for Epidemiologic Studies Depression Scale). Self‐esteem (Rosenberg Self‐Esteem Scale). |
|
| Notes | In this study, all outcomes were scored to reflect poor functioning (high score is worse). We therefore input data as given in the paper without multiplying by ‐1 to correct for scale direction. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report "randomisation was done in blocks of 4, with numbers generated by a random‐numbers table and sealed in opaque envelopes. Random sequence generation by a random numbers table. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. The published report states it was not possible to conceal the group allocation from the participating mothers” (page 1452, col 2). |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Trial investigators report “assessment data were collected from all participants by interviewers working in pairs; at least one of the interviewers was blind to the mothers’ group allocation” (page 1452, col 2). Review authors judged that not having both of the pair of interviewers blind to allocation is inadequate. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data for 6 of 59 (10%) were missing from the intervention condition (reasons not given), and for 9 of 57 (16%) from the control condition (reasons not given) at post‐intervention. Review authors judged numbers of missing data appear approximately balanced. Although reasons for missing data were not given, the risk of bias was judged to be acceptable at this time point. Overall attrition rate was 8%. Data for 8 of 59 (14%) were missing from the intervention condition (reasons not given), and for 16 of 57 (28%) from the control condition (reasons not given) at 3 month follow‐up. Overall attrition rate was 21%. Data for 9 of 59 (15%) were missing from the intervention condition (reasons not given), and for 24 of 57 (42%) from the control condition (reasons not given) at 6 month follow‐up. Overall attrition rate was 28.5%. Review authors considered the numbers of missing data were not balanced across the treatment conditions at 3 month and 6 month follow‐up. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Martin 2003.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of children with the behavioural problems. Sex: both mothers or fathers (no further information). Age of parents: (for completers) mean 37.25 years (SD 5.26) intervention; 39.57 years (SD 3.91) control; (range 27 to 46 years). Unit of allocation: individual participant. Number randomised: 45 (23 intervention; 22 control). Number used in analysis: 27 (16 intervention; 11 control). Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: member of academic or general staff at University of Queensland; employed for at least 20 hours/week; experiencing a significant level of distress juggling the demands of work and home; having child aged 2 to 9 years; child having behavioural problems in the clinical range on the Strengths & Difficulties Questionnaire. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: marital status: 25 (81%) married; 1 (3%) divorced; 4(13%) separated; education: 27 (87%) tertiary education level; employment: 21 (68%) general employment at University; 10 (32%) academic employment at University. |
|
| Interventions | Two conditions: Work‐Place Triple‐P parent programme; wait‐list control. Duration of intervention: 8 weeks. Length of follow up: 4‐month follow‐up for intervention condition only. |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scale). Anxiety symptoms (Depression Anxiety Stress Scale)*. Stress (Depression Anxiety Stress Scale)*. Confidence (Problem Setting and Behaviour Checklist). |
|
| Notes | *DASS total score only available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data for 7/23 (30%) were missing from the intervention condition (reasons not given), and for 11/22 (50%) from the control condition (reasons not given). Review authors considered the numbers of a missing data were not balanced across the treatment conditions. Overall attrition rate was 40%. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Matsumoto 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: families with Japanese parents, where children had received support to learn and maintain Japanese culture. Sex: both mothers and fathers (no further information). Age of parents: not stated. Unit of allocation: individual family. Number randomised: 50 (25 intervention, 25 control). Number used in analysis: 50 (25 intervention, 25 control). Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: Japanese origin; resident in Gold Coast area of Queensland, Australia; with child or children aged 2 to 10 years. Exclusion criteria: not stated. Ethnicity: mothers: 48 (96%) Japanese, 2 (4%) Australian; fathers: 15 (30%) Japanese, 30 (60%) Australian, 5 (10%) other. Baseline characteristics: marital status: 45 (90%) married; 2 (4%) divorced; education: 27 (54%) mothers had University education; 33 (66%) fathers had University education; employment: 40 (80%) mothers unemployed; 6 (12%) fathers unemployed; 25 (50%) families receiving parenting support; language at home Japanese only, 17 (34%), English only, 1 (2%), Japanese and English, 32 (64%); children: 27 boys; 23 girls; children: mean 4.9 years. |
|
| Interventions | Two conditions: Group Triple‐P Positive Parenting Program; wait‐list control. Duration of intervention: 8 weeks. Length of follow up: 3 months. |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scale). Anxiety symptoms (Depression Anxiety Stress Scale). Stress (Depression Anxiety Stress Scale). Confidence (Problem Setting and Behaviour Checklist). Partner satisfaction (Relationship Quality Index). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from K Sofronoff to CB on 21 Oct 2010) states "participants were allocated ID numbers and randomisation was done using the ID numbers". |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from K Sofronoff to CB on 20 Oct 2010) indicates that personnel were not blinded. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from K Sofronoff to CB on 20 Oct 2010) indicates that outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no attrition from either condition and no missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Matsumoto 2010.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: Japanese families living in a Tokyo metropolitan area with the target child aged between 2 and 10 years old. Sex: both mothers and fathers (no further information). Age of parents: not stated. Unit of allocation: individual family. Number randomised: 54 (28 intervention; 26 control). Number used in analysis: 51 (25 intervention; 26 control). Country & setting: Japan; single site; recruited from community settings; intervention delivered in the community. Inclusion criteria: Japanese parents living in a Tokyo metropolitan area. Exclusion criteria: parents who were suffering from major psychopathology were excluded; parents whose child met clinical criteria for diagnosis of a pervasive developmental disorder were also excluded. Ethnicity: all Japanese. Baseline characteristics: all the parents were married; education level of both parents was mainly college or university; employment: all mothers were unemployed; all fathers were in full time employment. |
|
| Interventions | Two conditions: Triple P‐Positive Parenting Programme (PPP); wait‐list control. Duration of intervention: not stated; it is assumed that duration was 8 weeks as in the Matsumoto 2007 study. Length of follow‐up: none stated. |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scale). Anxiety symptoms (Depression Anxiety Stress Scale). Stress (Depression Anxiety Stress Scale). Confidence (Problem Setting and Behaviour Checklist). Partner satisfaction (Relation Quality Index). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report that “the participants were 54 families who were randomly assigned to a treatment group (28 families) or a wait‐list group (26 families). Information reported insufficient for a judgment to be made. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgment to be made. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgment to be made. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgment to be made. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 3/28 (4%) were missing from the intervention condition (reasons not given), and there were no missing data from the control condition. Attrition rate was 4%. Review authors considered the number of missing data were small, and it is unlikely that this would introduce bias. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
McGillicuddy 2001.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of substance abusing adolescents. Sex: both mothers and fathers (no further information). Age of parents: mean 44.9 years (SD 5.52) intervention; 45.4 (SD 4.41) control. Unit of allocation: individual family. Number randomised: 22 (14 intervention; 8 control). Number used in analysis: 22 (14 intervention; 8 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: a parent/legal guardian of a child aged 12‐21 who have lived in the same household as the child at least 30 of the previous 90 days; parent reporting that the child was actively involved in substance use over the previous six months, and not receiving any alcohol/drug treatment. Exclusion criteria: parent's involvement in another form of treatment in relation to their child's substance use; severe psychiatric disorder; involvement in alcohol/drug use; not living within commuting distance of the research site. Ethnicity: 86% white intervention; 100% white control. Baseline characteristics: employed: 13 (93%) intervention; 5 (63%) control; years of education: mean 9.7 intervention; 9.1 (2.3) control married: 7 (50%) intervention; 2 (25%) control. |
|
| Interventions | Two condition: Cognitive‐behavioural parenting programme; wait‐list control. Duration of intervention: 8 weeks. Length of follow‐up: none. |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). Anxiety symptoms (Brief Symptom Inventory). Anger (State‐Trait Anger Expression Inventory). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report "individuals eligible for participation were told that their group would be assigned randomly to receive treatment immediately (i.e. skill training) or following an 8‐week delay (i.e. wait list)” (page 63). Information from trial investigator (e‐mail from N McGillicuddy to NH on 25 Oct 2010) indicates that a random numbers table was used. |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (e‐mail from B Irvine to NH on 22 Oct 2010) indicates that sufficient care was taken to ensure that therapists and research staff (including those who had pre‐treatment contacts with participants) had no knowledge of whether a group's treatment would be immediate intervention or delayed treatment control. Random allocation was done separately and centrally for treatment condition and for treatment therapist. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Review authors judge that treatment and research staff were kept blind to the cohort randomisation scheme and to the pending treatment assignment of the next cohort. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Review authors judge that treatment and research staff were kept blind to the cohort randomisation scheme and to the pending treatment assignment of the next cohort. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data reported. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared free of other sources of bias. |
Morawska 2009.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents with child aged 3 to 10 years, reporting concerns about their child's behaviour or their parenting. Sex: 68 mothers; 7 fathers. Age: mothers: mean 39.28 years (SD 5.50; range: 27‐54 years); fathers: mean 41.77 years (SD 6.01; range: 35‐56 years). Unit of allocation: individual participant. Number randomised: 75 (37 intervention; 38 control). Number used in analysis: 60‐70 (29‐33 intervention; 31‐37 control). Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: family living within Brisbane metropolitan area; parents reporting concerns about their child's behaviour or their parenting; child aged 3 to 10 years; child identified as 'gifted' by school or as result of formal cognitive assessment. Exclusion criteria: parents currently seeing a professional about their child's behaviour difficulties. Ethnicity: Australian (85.3%), Asian (5.3%); Maori (1.3%), other (8%). Baseline characteristics: 86.7% children lived in their original family, 8% children lived in a single parent family, and 4% lived in a step family; mean family size 2.23 children; education: 77.3% of mothers and 65.3% of fathers had a university degree; employment: 60% of mothers and 86.7% of fathers were employed. |
|
| Interventions | Two conditions: Gifted and Talented Group Triple‐P program; wait‐list control. Duration of intervention: 9 weeks. Length of follow‐up: 6 months for the intervention group only. |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scale). Anxiety symptoms (Depression Anxiety Stress Scale). Stress (Depression Anxiety Stress Scale). Confidence (Parenting Task Checklist). Partner satisfaction (Relation Quality Index). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence allocation by computer‐generated random numbers. |
| Allocation concealment (selection bias) | High risk | Information from trial investigator (email from A Morawska to CB on 26/10/10) states that a research assistant not associated with the project used a list to allocate participants, but there is no indication that complete concealment of allocation was attempted. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | There is no indication either from the published report, or from the trial investigator that personal were blinded to the intervention (email from A Morawska to CB on 26/10/10). |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | The outcome assessment was self report by the parents so there were no judgements made by the assessors in relation to diagnostic status, however the parents were not blinded to the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | On page 468 there was missing data for 8/37 from the intervention group and 7/38 from the control group. Data for 4/37 (10.8%) were missing from the intervention condition, and for 1/38 (2.6%) from the control condition. Reasons for the 5 missing given as: 1 moved area, 1 had a new baby; 1 had insufficient time to attend, 1 had received a recent diagnosis of LD for their child and 1 was undergoing chemotherapy (page 466, col 2). Further information from trial investigator provided some details about the pairwise exclusion of missing data in the report (email from A Morawska to CB on 26/10/10). |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Investigators report "no between‐group differences on demographic variables were found on preliminary analysis. There were also no significant differences across the majority of outcome variables. Pre‐intervention scores were used as co‐variates in subsequent analyses to control for any differences’ (page 466, col 2). The study appeared to be free of other sources of bias. |
Niccols 2009.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: mothers of child aged 12 to 36 months. Sex: all mothers. Age of parents: mean 31.0 years (SD 5.7; range 18 to 45 years). Unit of allocation: individual participant. Number randomised: 79 (49 intervention; 30 control). Number used in analysis: 74 (45 intervention; 29 control) at post‐intervention; 71 (45 intervention; 26 control) at short‐term follow‐up. Country & setting: Canada; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: able to complete questionnaires in English; having a child of 12 to 36 months. Exclusion criteria: previous attendance at any portion of CWTB programme. Ethnicity: a range of ethnic backgrounds. Baseline characteristics: mothers: married/cohabiting: 82.3%; education: 84.8% completed high school; children: 39.2% children had no siblings; 22% scored above clinical cut‐off on the child behaviour problems questionnaire. The two study conditions did not differ significantly on pre‐test maternal age, education, socioeconomic status, marital status, infant age, infant gender, family size, family risk factors, number of the services used, or child behaviour problems. |
|
| Interventions | Two conditions: COPEing with toddler behaviour (behavioural parenting programme); wait‐list control. Duration of intervention: 8 weeks. Length of follow‐up: 1 month. |
|
| Outcomes | Depressive symptoms (Centre for Epidemiological Studies Depression Scale). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence allocation by use of random number tables. |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from A.Niccols to CB on 20 Oct 2010) indicates that sealed opaque envelopes were used. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from a.Niccols to CB on 20 Oct 2010) indicates that personnel were blind. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Investigators report that outcome assessors were blind to allocation status of participants and the method of randomisation (page 619, col 2). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 4/49 (8%) were missing from the intervention condition (failed to reach), and for 1/30 (3%) from the control condition (failed to reach) at post‐intervention. Data for 4/49 (8%) were missing from the intervention condition (failed to reach), and for 4/30 (13%) from the control condition (failed to reach) at post‐intervention at follow‐up. Overall attrition rate was 8%. Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Investigators report the two groups did not differ significantly on baseline characteristics. The study appeared to be free of other sources of bias. |
Nicholson 2002.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of low socioeconomic status who made excessive use of verbal and corporal punishment. Sex (main carer): 25 mothers or grandmothers (23 mothers; 2 grandmothers), 1 father. Age of parents: mean 31 years (SD 11.97). Unit of allocation: individual participant. Number randomised: 26 (13 intervention; 13 control). Number used in analysis: 26 (13 intervention; 13 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: families with one child between 1 and 5 years who reported frequent use of verbal or corporal punishment. Exclusion criteria: families with children who had psychiatric diagnoses or who were receiving special education services in school. Ethnicity: 14 (54%) African American; 6 (23%) Hispanic; 4 (15%) white; 2 (8%) other. Baseline characteristics: education: 7 (27%) not completed high school, 8 (30%) high school graduate, 11 (42%) completed some post‐high‐school education; 16 (62%) single, 10 (38%) married. |
|
| Interventions | Two conditions: STAR parenting programme (cognitive‐behavioural parenting programme); wait‐list control. Duration of intervention: 10 weeks. Length of follow‐up: 1 month. |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information from trial investigator (email from RA Fox to NH on 26 Oct 2010) indicates that random allocation was by computer‐generated random numbers. |
| Allocation concealment (selection bias) | High risk | Information from trial investigator (email from RA Fox to NH on 26 Oct 2010) indicates that the allocation sequence was known to one of the six individuals who also delivered some of the treatment services. This raises the possibility of bias. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information from trial investigator (email from RA Fox to NH on 26 Oct 2010) indicates that five of the six trial personnel/outcome assessors were blinded, but one was not. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information from trial investigator (email from RA Fox to NH on 26 Oct 2010) indicates that five of the six trial personnel/outcome assessors were blinded, but one was not. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyses were performed on all randomised participants. No missing data reported and “missed sessions were rescheduled to ensure that each parent consistently received the entire psychoeducational parenting program” (page 366). |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Nixon 1993.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteer parents of children with severe developmental disabilities attending special schools. Sex: both mothers and fathers (no further information). Age of participants: not stated. Unit of allocation: individual family. Number randomised: 58 (breakdown by group not given). Number used in analysis: 34 (18 intervention, 16 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: parents of children with severe developmental disabilities attending special schools. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: not stated. |
|
| Interventions | Two conditions: Cognitive‐behavioural parenting programme; wait‐list control. Duration of intervention: 5 weeks. Length of follow‐up: none. |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). Guilt (Situational Guilt Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report "fifty‐eight subjects were randomly assigned to treatment or waiting list control groups" (page 668). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Trial investigators report "at the time of the initial phone call, parents were randomly assigned to treatment and control groups and were informed of their assignment" (page 667). Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8 of 29 (26%) in the treatment group and 10 of 29 (34%) in the control group did not complete post‐tests, and a further 3 of 29 (10%) in the treatment group and 3 of 29 (10%) in the control group were excluded because the independence of husband's and wife's scores could not be demonstrated. Review authors considered that numbers of and reasons for missing data were approximately balanced between conditions. Attrition 41%. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Odom 1996.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteer parents of children with ADHD. Sex: all mothers. Age of parents: mean 32.7 years (range=24 to 47). Unit of allocation: individual participant. Number randomised: 25 (13 intervention; 12 control). Number used in analysis: 20 (10 intervention; 10 control). Country & setting: USA; recruited from community settings; intervention delivered in the community. Inclusion criteria: low socioeconomic status mothers who had a male child between the ages of 5 and 11 with ADHD, who had been taking methylphenidate, and who met noncompliant behavioural criteria. Exclusion criteria: not stated. Ethnicity: 75% African American. Baseline characteristics: 85% biological mothers; 70% single mothers; average educational level was 12 years (range 8‐15). |
|
| Interventions | Two conditions: Educational parent training (behavioural parenting programme); wait‐list control. Duration of intervention: 5 weeks. Length of follow‐up: none. |
|
| Outcomes | Confidence (Parenting Sense of Competence Scale). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information from trial investigator (email from S Odom to NH on 26 Oct 2010) indicates that random allocation was by drawing lots from a hat. |
| Allocation concealment (selection bias) | Low risk | Information from trial investigator (email from S Odom to NH on 26 Oct 2010) indicates that names of participants were placed on pieces of paper which here then drawn from a hat "first one to the control group and then one to the intervention group until there were 15 in each". Review authors consider this process is unlikely to have introduced a risk of bias. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Information from trial investigator (email from S Odom to NH on 26 Oct 2010) indicates that "all involved parties were blinded to allocation status". |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Information from trial investigator (email from S Odom to NH on 26 Oct 2010) indicates that "all involved parties were blinded to allocation status". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 5 weeks, 3/13 (23%) were missing from intervention group (due to non‐compliance or inability to participate in the educational sessions) and 2/12 (17%) were missing from control group (one due to her husband disagreeing that their male child receive the stimulant medication; reason not given for the other). Review authors judge that missing outcome data were balanced in numbers across conditions, even though the reasons for the missing data differed slightly. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Patterson 2002.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of children aged 2‐8 years registered at three GP practices in Oxford. Sex: both mothers or fathers (no further information). Age of parents: not stated. Unit of allocation: individual participant. Number randomised: 116 (60 intervention; 56 control). Number used in analysis: 95‐96 (45‐46 intervention; 50 control). Country & setting: UK; multi‐site (number not stated); recruited from primary care settings; intervention delivered in primary care. Inclusion criteria: scoring above 100 on the Eyberg Child Behaviour Inventory (ECBI). Exclusion criteria: not stated. Ethnicity: 91.4% white, 4.8% Asian, 2.9% mixed race, 1% Black. Baseline characteristics: 14.7% single parents. 13.3% social class I, 39.0% social class II, 22.9% social class III N, 13.3% social class III M, 5.7% social class IV, 5.7% social class V. |
|
| Interventions | Two conditions: Webster‐Stratton parenting program; no‐treatment control. Duration of Intervention: 10 weeks. Length of follow‐up: 3 months; 6 months. |
|
| Outcomes | Depressive symptoms (General Health Questionnaire). Anxiety symptoms (General Health Questionnaire). Stress (Parenting Stress Index‐total). Self‐esteem (Rosenberg Self‐Esteem Scale). |
|
| Notes | Includes follow up data from Stewart‐Brown 2004. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report that randomisation was "by tossing a coin in the presence of an independent witness, to treatment or control" (page 473). Review authors judge that the allocation sequence was adequately generated. |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from J Patterson to NH on 23 Oct 2010) indicates that central allocation was used involving a third party not otherwise involved in the trial. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from J Patterson to NH on 23 Oct 2010) indicates that personnel involved in data handling were blind to allocation until after all quantitative data had been collected. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from J Patterson to NH on 23 Oct 2010) indicates that outcome assessors were blinded during collection and analysis of quantitative data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At 6 months follow up, 4/60 (7%) were missing from intervention group and 4/56 (7%) were missing from the control group. At 12 months follow up, 16/60 (27%) were missing from intervention group and 13/56 (23%) were missing from the control group. Reasons for missing data not broken down by condition but included increased work commitment, moving away from the area, depression, other life stress, and holiday falling at start of group sessions. Trial investigators report no difference in the proportion of attenders or non‐attenders returning questionnaires at follow up. Review authors judge the numbers of missing data were balanced between conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Pisterman 1992a.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of preschoolers aged 3‐6 years who were clinically diagnosed with ADHD. Sex: both mothers and fathers (no further details); assessment was performed only on the target parents (88 mothers, 3 fathers). Age of parents: not stated. Unit of allocation: individual family. Number randomised: 91 (46 in Study 1: 23 intervention; 23 control; 45 in Study 2: 23 intervention; 22 control). Number used in analysis: 91 (46 intervention; 45 control) at post‐intervention; 46 (23 intervention; 23 control) at follow‐up. Country & setting: Canada; single‐site; recruited from community and outpatient settings: intervention delivered in an outpatient clinic. Inclusion criteria: parents of preschoolers aged 3‐6 years, who were clinically diagnosed with ADHD. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: not stated. |
|
| Interventions | Two conditions: Behavioural parenting programme; wait‐list control. Duration of intervention: 12 weeks. Length of follow‐up: 3 months. |
|
| Outcomes | Depressive symptoms (Parenting Stress Index). Stress (Parenting Stress Index). Confidence (Parenting Stress Index). Partner satisfaction (Parenting Stress Index). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Investigators report that "families of eligible children were randomly assigned to an immediate treatment group (experimental group) or a delayed treatment group (control group)" (pages 46‐47). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Trial investigators report an overall dropout rate of 8% in Study 1 and 21% in Study 2 with no significant difference between conditions. Breakdown by condition not provided. Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Study appeared free of other form of bias although, as the investigators noted, "the present study did not include an attention control group...therefore, it is possible that reported improvements were a function of demand characteristics" (page 55). |
Pisterman 1992b.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of preschoolers aged 3‐6 years who were clinically diagnosed with ADHD. Sex: both mothers and fathers (no further information). Age of participants: not stated. Unit of allocation: individual family. Number randomised: 57 (28 intervention; 29 control). Number used in analysis: number available for analysis n=45 (23 intervention; 22 control).* Country & setting: Canada; single‐site; recruited from community and outpatient settings; intervention delivered in an outpatient clinic. Inclusion criteria: parents of pre‐schoolers aged 3‐6 years who were clinically diagnosed with ADHD. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: not stated. |
|
| Interventions | Two conditions: Behavioural parenting programme; wait‐list control. Duration of intervention: 12 weeks. Length of follow‐up: 3 months. |
|
| Outcomes | Stress (Parenting Stress Index). Confidence (Parenting Stress Index). |
|
| Notes | *Insufficient data to calculate effect sizes. Clarification was requested from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data missing for 5 of 28 (18%) in the treatment condition and for 7 of 29 (24%) in the control condition due to participants dropping out of the study. The overall dropout rate was 21.1%. Review authors judge the numbers of missing data and reasons for missing data were balanced between conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Schultz 1993.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: mother‐father dyads of children or young adults with intellectual disabilities. Sex: 54 mothers; 54 fathers. Age of parents: mean 41.5 years intervention; 39.4 years control. Unit of allocation: individual family. Number randomised: 54 (15 intervention; 39 control). Number used in analysis: number available for analysis n=54 (15 intervention; 39 control).* Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: biological parents of children or young adults with intellectual disabilities. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: participants in the two conditions did not differ with respect to age, religion, education or occupation of parents. |
|
| Interventions | Two conditions: Caring for Parent caregivers; no‐treatment control. Duration of intervention: 6 weeks. Length of follow‐up: 12 months. |
|
| Outcomes | Partner satisfaction (Marital Adjustment Inventory). | |
| Notes | *Insufficient data to calculate effect sizes. Clarification was requested from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Sirbu 1978.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteer mothers of preschool children. Sex: all mothers. Age of parents: not stated. Unit of allocation: individual participant. Number randomised: 60 (number randomised to the four conditions; no further information). Number used in analysis: number available in analysis not stated*. Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: mothers of preschool children. Exclusion criteria: not stated. Ethnicity: all Caucasian. Baseline characteristics: no significant differences between the four conditions in the mother's level of education, occupation, number of children, or significant medical problems. |
|
| Interventions | Four conditions: three behavioural parenting training groups (course & programmed text; course alone; programmed text alone); attention‐placebo control. Duration of intervention: 5 weeks. Length of follow‐up: none. |
|
| Outcomes | Stress (Parent Stress Satisfaction Questionnaire)*. | |
| Notes | *Insufficient data to calculate effect sizes. Clarification was requested from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report that mothers "were randomly assigned to one of four treatment groups" (page164). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Trial investigators report that "instructions were given to each groups about the course, and in the case of Groups 2 and 4, not to look at a copy of Becker's book" (page 165), thus attempting to ensure participants were unaware of the type of intervention they were receiving. However, there is no information whether the instructions given were followed. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Spaccerelli 1992.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: volunteer parents concerned about their child behaviour problem. Sex: (completers) 47 mothers; 6 fathers. Age of parents: mean 35.5 years. Unit of allocation: individual participant. Number randomised: 126 (number randomised to the three conditions; no further information; 81 participated in the pre‐test assessment). Number used in analysis: number available for analysis n=53 (no further information)*. Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: parents concerned about their child behaviour problems. Exclusion criteria: not stated. Ethnicity: (81participants): 35 white; 28 Hispanic; 14 Black; 4 others. Baseline characteristics: (81 participants): 27 single/divorced, 47 married, 7 missing data; 21 high school, 32 some college education, 27 graduates, 1 missing data. |
|
| Interventions | Three conditions: behavioral (Webster‐Stratton) parent programme & problem‐solving skills training; behavioral parent training and discussion; wait‐list control. Duration of intervention: 16 hours (10 hours behavioral parent programme & 6 hours problem solving skills training). Length of follow‐up: 4 to 5 months. |
|
| Outcomes | Stress (Parenting Stress Index).* | |
| Notes | *Insufficient data to calculate effect sizes. Clarification was requested from the trial investigators but no further information was available at the time this review was prepared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report that "the 126 parents expressing interest in participating were randomly assigned" (page 5). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rates and numbers of missing data not provided, although effects of attrition were analysed by the trial investigators who found rates of attrition not significantly different between the three experimental groups. In terms of demographics, there was a significant main effect for attrition status on parent education, indicating that less educated parents were more likely to drop out. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Two measures in the study were newly devised (page 15). This raises the possibility of bias. |
Taylor 1998.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: families of 3 to 8 year old children with conduct problems. Sex: 107 mothers, 70 fathers. Age of parents: mean 33 years, mothers; mean 37 years, fathers. Unit of allocation: individual family. Number randomised: 110* (46 'Parents and Children Series' parent programme; 46 Eclectic programme; 18 wait‐list control). Number used in analysis: n=32 (15 intervention; 17 control) for 'depressive' symptoms; n=17 (7 intervention; 10 control) for 'partner satisfaction'. Country & setting: USA; single‐site; recruited from community settings; intervention delivered in an outpatient clinic. Inclusion criteria: families who contacted the Regional Family Centre for assistance related to conduct problems of 3 to 8 year old children, or to difficulties in parenting a child of this age. Exclusion criteria: not stated. Ethnicity: not stated. Baseline characteristics: (108 participants): 69 married or common‐law couples, 38 single mothers; 1 father. |
|
| Interventions | Three conditions: 'Parents and Children Series' (Webster‐Stratton) parent programme; Eclectic Programme (delivered individually); wait‐list control. Duration of intervention: 11 to 14 weeks. Length of follow‐up: 4 months. |
|
| Outcomes | Depressive symptoms (Back Depression Inventory). Partner satisfaction (Dyadic Adjustment Scale). |
|
| Notes | *Some families served initially as wait list controls and then were randomly assigned to either of the two interventions, based on need. We analysed results from 15 families who received the PACS intervention and were directly compared to the 17 families who were assigned to the wait list control group and did not receive the intervention at any stage (p. 288 'Assignment to treatment conditions and Table 1 p. 233). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report "families who were potential wait‐list candidates were randomly assigned to either of the two treatments or to the wait‐list control group, while families who had no possibility of wait‐list were randomly assigned between the two treatments" (page 228). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Review authors judge that the design of the study means personnel would be aware which participants had been assigned to the immediate intervention conditions. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Trial investigators report" research assistants who collected post‐test assessment measures were not informed of treatment assignment, although on occasion families revealed which treatment they received" (page 230). Review authors considered that the blinding of the outcome assessors was therefore compromised. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intention to treat analyses were performed for those families who attended at least one treatment session. Two participants of 46 (4%) in the PACS group and 2 of 46 (4%) in the eclectic treatment group attended no treatment sessions. Investigators report that "the design of the study did not allow for all comparison to be done simultaneously in a single analysis because the wait‐list control group was comparable only to a sub‐sample of each of the two treatments. For this reason, each hypothesis was tested separately, using only those participants relevant to hypothesis" (page 231). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Treacy 2005.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of children diagnosed with DSM‐IV ADHD recruited through an ADHD research clinic and the paediatric outpatient department of a local hospital. Sex: 40 mothers (including 3 step mothers and 1 foster mothers) ; 23 fathers (including 2 step fathers). Age of parents: mean 36.3 years mothers (SD 5.5; range 28‐49 years); mean 38.8 years (SD 6.6; range; 26‐53). Unit of allocation: individual family. Number randomised: 42 families and 63 participants (breakdown by group not given). Number used in analysis: 21‐32 (12‐16 intervention; 9‐17 control). Country & setting: New Zealand; single‐site; recruited from outpatient and research clinic settings; intervention delivered in an outpatient clinic. Inclusion criteria: families with at least one child diagnosed with DSM‐IV ADHD. Exclusion criteria: severe relationship difficulties between parents who both wished to participate; major psychiatric disorder. Ethnicity: not stated. Baseline characteristics: mean family socioeconomic status on SES scale, 4.2 (SD 1.7); 88.1% of children prescribed methylphenidate for their ADHD; 27/42 (64.3%) families were 2‐parent families; 47.4% children had delinquent behaviour problems; 56.1% children had aggressive behaviour problems; 37 (88.1%) boys. |
|
| Interventions | Two conditions: Parent stress management parenting program; wait‐list control. Duration of intervention: 9 weeks. Length of follow‐up: no follow‐up. |
|
| Outcomes | Depressive symptoms (Beck Depression Inventory). Stress (Parenting Stress Index). Partner satisfaction (Locke‐Wallace Marital Adjustment test). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | After randomisation, but prior to the beginning of treatment, 3 withdrew from the control group and 1 withdrew for the intervention group. One parent completed only 7 out of 9 treatment sessions. Investigators report overall 98.4% completion of outcome measures at baseline and 84.1% at post‐treatment, but with no breakdown by treatment condition. Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appeared to be free of other sources of bias. |
Turner 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: indigenous families of the children 1 to 13 years of age presenting to four South‐East Queensland Community Health sites. Sex: 45 mothers; 6 fathers. Age of parents: mean 34.52 years (SD 10.54), intervention; mean 30.87 years (SD 7.65), control. Unit of allocation: individual participant. Number randomised: 51 (26 intervention; 25 control). Number used in analysis: 38 (20 intervention; 18 control). Country & setting: Australia; multi‐site (n=4); recruited from community settings; intervention delivered in the community. Inclusion criteria: indigenous families with target child aged between 1 and 13 years; primary caregiver had concerns about their child’s behaviour or their own parenting skills. Exclusion criteria: developmental delay; major physical difficulty; severe chronic illness; developmental disorder (for example: autism); current medication or contact with another professional for behavioural problems. Ethnicity: all indigenous ethnicity. Baseline characteristics: mean 2.5 children per family; 11 (22%) in full time employment; 32 (63%) unemployed; 35 (68%) two‐parent family; target child: 33 (65%) boys; 34 (67.3%) mothers, 3 (6.1%) fathers, 9 (16.3%) grandmothers, 3 (6.1%) aunts and 2 (4.0%) guardians. |
|
| Interventions | Two conditions: 'Group Triple P' parent programme; wait‐list control. Duration of intervention: 8 weeks. Length of follow‐up: 6 months (intervention group only). |
|
| Outcomes | Depressive symptoms (Depression Anxiety Stress Scale). Stress (Depression Anxiety Stress Scale). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from K Turner to CB on 28 Oct 2010) states "the research officer used a computer program for random number generation for each site". |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made. Information from trial investigators (email from K Turner to CB on 28 Oct 2010) states that "there were sealed envelopes". |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judged that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Investigators report that trial personnel were blind to allocation status of participants. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | Investigators report that outcome assessors were blind to allocation status of participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 6/26 (23%) missing from the intervention condition (2 new baby; 1 decided not to participate; 1 illness in family; 1 illness; 1 too busy with work), and for 7/25 (28%) from the control condition (3 unknown; 1 death in family; 1 illness in family; 1 premature baby; 1 family crisis). Overall attrition was 25.5% at post‐intervention. Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | High risk | Investigators do not report on the anxiety scale of the DASS. A 42 item questionnaire was chosen but this was reduced to only 14 items(depression and stress) on the request of the local medical board to reduce the assessment burden on parents. |
| Other bias | Low risk | The study appears to be free of other sources of bias. Investigators report "there were no significant differences between those who completed post‐assessment and those who did not on any demographic or outcome measure at pre‐test" (page 433, col 1). |
van den Hoofdakker 2007.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: parents of children between 4 and 12 years of age with ADHD who were referred to an outpatient mental health clinic by their GP. Sex: both mothers and fathers (no further information). Age of parents: not stated. Unit of allocation: individual family. Number randomised: 96 (48 intervention; 48 control). Number used in analysis: 94 (47 intervention; 47 control). Country & setting: Netherlands; single‐site; recruited from an outpatient setting; intervention delivered in an outpatient clinic. Inclusion criteria: DSM‐IV criteria for ADHD; IQ > 80; child aged between 4 and 12 years; both parents (if present) willing to participate in the parent program. Exclusion criteria: families who had already received intensive behavioural parent training the year before; problems with the child/or family that required immediate intervention (for example: crisis in the family). Ethnicity: 94.7% white, 2.1% African, 2.1% Asian, 1.1% unknown. Baseline characteristics: marital status: 73 (77.7%) two biological parents; 10 (10.6%) single parent; 11 (11.7%) one biological, one step‐parent; no statistically significant differences in child or family characteristics between two conditions, with the exception of tics (significantly higher frequency in the control group). |
|
| Interventions | Two conditions: Behavioural parent programme plus treatment as usual; treatment as usual control. Duration of intervention: 12 sessions over 5‐month period. Length of follow‐up: 6 months (intervention group only). |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from B van den Hoofdakker to CB on 24 Nov) states "the randomisation sequence of family id‐numbers was computer generated". |
| Allocation concealment (selection bias) | Low risk | Information reported insufficient for a judgement to be made, but information from trial investigator (email from B van den Hoofdakker to CB on 24 Nov) states ""an external researcher generated the allocation sequence and preserved the list of randomised family id‐numbers. This researcher did not work in the outpatient mental health clinic where the study was conducted, was not involved in assessment or treatment, and did not determine eligibility for the study or entry of patients". |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for 1/48 (2%) missing from the intervention condition (urgent problems requiring immediate treatment), and for 1/48 (2%) from the control condition. Overall attrition was 2% at post‐intervention. Investigators report that an additional 5 discontinued (for personal reasons or because immediate treatment was required) with the missing endpoint data replaced with LOCF values. Review authors considered the numbers of and reasons for missing data reasonably likely to be balanced across the treatment conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Investigators report: a) there were no statistically significant differences between conditions at baseline on demographic or outcome measures with the exception of the presence of tics (a comorbid condition) which had a significantly higher frequency in the control group (P=.006). b) investigators carried out repeated‐measures ANOVAs to examine for interaction effects between time, treatment, and medication status and parenting stress. Results (F(2,91) = 0.010, P=.990) indicate that medication status at study entry did not affect treatment effects. c) there were no statistical differences (Chi2 tests) in the proportion of children who were taking medication between the two conditions at baseline and at post‐treatment. The study appeared free of other sources of bias. |
Wang 2005.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: families of children with autism. Sex: both mothers and fathers (no further information). Age of parents: biological mothers: mean 33.4 years intervention; 33.5 years control; biological fathers: mean 34.5 years intervention; 34.9 years control. Unit of allocation: individual family. Number randomised: 34 (17 intervention; 17 control). Number used in analysis: 27 Parental stress (15 intervention; 12 control) from Wang 2005 (thesis data). Country & setting: China; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: child <10 years old; formal diagnosis of autism by professionals or agencies not affiliated with the project. Exclusion criteria: not stated. Ethnicity: all Chinese. Baseline characteristics: 33% parents had no previous training on autism; the other 66% had received some form of training from an education service centre that included behaviour management, language instruction and applied behaviour analysis. |
|
| Interventions | Two conditions: Interactive skills of parents programme (behavioural parenting programme); wait‐list control. Duration of intervention: 4 weeks. Duration of trial: 5 weeks. Length of follow‐up: none. |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information from trial investigator (e‐mail from P Wang to CB on 31 Oct 2010) states "randomisation was completed via coin flipping". |
| Allocation concealment (selection bias) | High risk | No allocation concealment was attempted. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | High risk | Principal investigator delivered the training and also assessed the outcomes. |
| Blinding (performance bias and detection bias) Outcome assessors | High risk | Principal investigator delivered the training and also assessed the outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was missing outcome data: "after commencement of the study, two families dropped out of the training group and five dropped out of the control group, leaving 15 families remaining in the training group and 12 in the control group. One of the families in the training group, after completing the entire training program, dropped out during the posttest data collection phase because of a prescheduled family vacation.’ (p.97, col 2)." |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Webster Stratton 1988.
| Methods | Parallel randomised controlled trial. | |
| Participants |
Participants: professionally referred parents of 3 to 8 year old children with conduct disorder. Sex: 114 mothers; 80 fathers. Age of parents: mean 32.8 years, mothers; mean 35.1 years, fathers. Unit of allocation: individual family. Number randomised: 114 (29 GDVM; 28 IVM; 28 GD; 29 control). Number used in analysis: 54 (27 intervention; 27 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: parents of the child aged 3 to 8 years; parents had rated their child as having a clinically significant number of behavioural problems according to the Eyberg Child Behaviour Inventory; primary referral problem of child misconduct that had been occurring for more than 6 months. Exclusion criteria: parents of children with debilitating physical impairment, intellectual deficit, or history of psychosis. Ethnicity: not stated. Baseline characteristics: 69.3% married, 30.7% single. |
|
| Interventions | Four conditions: Group discussion videotape modelling (Webster‐Stratton parenting programme) (GDVM); Individual videotape modelling (IVM); Group discussion (GD); wait‐list control. Duration of intervention: 10‐12 weeks. Length of follow‐up: none. |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | We used data from the GDVM arm only compared with wait‐list control to avoid double counting of participants in the control group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial investigators report that parents "were randomly assigned to one of four groups" (Abstract). Information from trial investigator (e‐mail from C Webster‐Stratton to NH on 22 Oct 2010) indicates that randomisation was achieved by the drawing of lots (i.e. names on folded pieces of paper drawn blindly from a hat). |
| Allocation concealment (selection bias) | Low risk | "Once subjects were accepted for entry, a randomly selected sealed envelope was opened that designated each family's parent training condition" (page 560). Review authors judged that allocation was probably adequately concealed. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Low risk | Information reported insufficient for a judgement to be made. Information from trial investigator (e‐mail from C Webster‐Stratton to NH on 22 Oct 2010) indicates that all personnel were blind to allocation status. |
| Blinding (performance bias and detection bias) Outcome assessors | Low risk | "Home observations were made by eight extensively trained observers who were blind to the hypothesis and the group membership of the subjects" (page 560). Independent assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | For mothers, 2/29 (7%) missing from GDVN condition, 1/28 (4%) missing from IVM condition, 4/28 (14%) missing from GD condition and 2/29 (7%) missing from control condition. Review authors judge that missing outcome data approximately balanced in numbers across conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Wolfe 2003.
| Methods | Parallel randomised controlled trial (study 1). | |
| Participants |
Participants: mothers of at least one child younger than five years of age recruited from parents who attended lectures on discipline at day care and family support centres. Sex: all mothers. Age of parents: mean 37.6 years. Unit of allocation: individual participant. Number randomised: 25 (11 intervention; 14 control) Number used in analysis: n=25 (11 intervention; 14 control)*. Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: mothers with at least one child younger than five years. Exclusion criteria: fathers (because of their small number). Ethnicity: 23 (92%) European American; 2 (8%) Asian American; 25 (100%) married; mean yearly family income $60,000 to $70,000. Baseline characteristics: Two study conditions were comparable with respect to most demographic characteristics; all participants married; mean number of children 1.9; 14 mothers employed. |
|
| Interventions | Two conditions: Listening to Children (LTC) parent education program; wait‐list control. Duration of intervention: 8 weeks. Length of follow‐up: 3 months. |
|
| Outcomes | Stress (Parenting Stress Index). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no attrition in either group. |
| Selective reporting (reporting bias) | High risk | Investigators do not report endpoint and follow‐up data for the parent‐child dysfunction interaction subscale of the PSI. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Wolfson 1992.
| Methods | Cluster randomised controlled trial | |
| Participants |
Participants: first‐time parent couples recruited from childbirth classes. Sex: 60 mothers; 60 fathers. Age of parents: mean 28.7 years. Unit of allocation: childbirth class. Number randomised: 25 classes (no further information); 60 couples (29 intervention; 31 control). Number used in analysis: 53 couples (26 intervention; 27 control). Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community. Inclusion criteria: parents who were expected their first child; mothers and near end of their 7th month of pregnancy; both parents between 21 and 40 years of age; married; gestational age should at least 38 weeks; birth weight 5 lb or more. Exclusion criteria: infant with gross congenital abnormality or serious health problem. Ethnicity: not stated. Baseline characteristics: education: mean 15 years (SD 2.2) mothers; mean 29.2 years (SD 3.9) fathers; duration of marriage: mean 3.6 years (SD 2.2). |
|
| Interventions | Two conditions: Behavioural parent programme; wait‐list control. Duration of intervention: 4 weeks (2 pre‐natal weekly group sessions & 2 post‐birth weekly sessions). Length of follow‐up: 10 to 11 weeks. |
|
| Outcomes | Stress (modified Uplifts & Hassles Scale). Confidence (Parental Efficacy measure). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Trial investigators report that "study used a randomised parallel group design; a) each of 25 Lamaze classes was randomly assigned to either training or control condition; b) husbands and wives where then recruited together as couples from these assigned classes; c) to minimise group process effect and group homogeneity related to Lamaze classes, couples from the same Lamaze classes were assigned to different training group sessions and filled out forms individually; training group(n=29) and control group (n=31)” (page 43). Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Participants | High risk | Review authors judge that it would not be possible to fully blind participants in this type of study, and found no indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants. |
| Blinding (performance bias and detection bias) Personnel | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Blinding (performance bias and detection bias) Outcome assessors | Unclear risk | Information reported insufficient for a judgement to be made. We requested clarification from the trial investigators, but no further information was available at the time this review was prepared. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no missing data at treatment endpoint. At follow up, 3/29 (10%) in the intervention condition and 4/31 (13%) in the control condition did not return to complete assessments. Review authors judge that numbers of and reasons for missing data were balanced between conditions. |
| Selective reporting (reporting bias) | Low risk | Review authors judge that the published report includes all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Al‐Hassan 2011 | RCT, but excluded because no standardised outcome measures. |
| Anastopoulos 1993 | Not randomised or quasi‐randomised; pre‐post test design; previously classified as a quasi‐RCT using a broad definition, which no longer meets criteria. |
| Atherton 2007 | This paper summarises findings from the Hutchings 2007a paper, which we have included. |
| Azrin 2001 | Randomised; participants did not meet the inclusion criteria (participants are adult parents and their children between 12‐17 years old); no control group (two interventions were compared); the study does not focus on psychosocial health; absence of required outcomes. |
| Barkby 2011 | Not an RCT. |
| Barkley 2001 | Quasi‐randomised; participants met the inclusion criteria; no control group (two family therapies were compared); intervention was group‐based; absence of psychosocial outcomes. |
| Barlow 2007 | This paper summarises findings from the Gardner 2006 paper, which we have included. |
| Barlow 2008 | Randomised; participants met the inclusion criterion; a wait‐list control group; intervention was not group‐based (intervention was delivered on an individual basis). |
| Baydar 2003 | RCT; participants met the inclusion criteria; a treatment as usual control group; intervention was group‐based; no data are provided on mental health measures at trial points ‐ the investigators measured depressive symptoms and anger/aggression at baseline, but than used the scores as indicators of risk in subsequent analysis ‐ they provide data on the effects of these risk factors on program results, but not data on the effect of the program on mental health. |
| Berry 2007 | Randomised; participants met the inclusion criteria; control group did not meet the inclusion criteria as they were attending a weight loss programme at the same time; intervention was group‐based; absence of psychosocial outcomes. |
| Bodenmann 2008 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; outcomes assessed: the study focuses on improving parenting and child behaviour rather than parental psychosocial health. |
| Bogle 2007 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was not solely group‐based: (i) significant individual component involved; ii) some participants received only individual component; absence of parental psychosocial outcomes. |
| Bradley 2010 | RCT, but excluded because intervention involved direct work with children. |
| Brunk 1987 | Randomised; participants were parents who had been investigated for abuse or neglect; no control group (two interventions were compared; intervention was group‐based. |
| Camp 1997 | "Quasi‐experimental" design; participants pregnant or parenting chemically‐dependent women; no control group (two interventions were compared); the interventions were delivered both in the groups, and on the individual basis. |
| Chacko 2006 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based, but involved direct work with children. |
| Chacko 2009 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based, but involved direct work with children. |
| Chazan‐Cohen 2007 | This paper presents recent findings from the follow‐up study, where 17 programmes with a random‐assignment were evaluated. Participants did not meet inclusion criteria: 39% of mothers were under 20 years old, and the results of those 20 years and older are not presented separately. |
| Coard 2007 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; outcomes assessed: parenting skills; the study did not focus on parental psychosocial health. |
| Connell 1997 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was not group‐based (a telephone counselling programme). |
| Cooper 2009 | Randomised; participants did not meet the inclusion criteria; a wait‐list control group; intervention was not group‐based. |
| Cummings 2000 | Randomised; intervention was not group‐based (delivered on individual basis in the home). |
| Dadds 1992 | Randomised; participants met the inclusion criteria; no control group (two interventions were compared); the study compared outcomes in 22 mothers of diagnosed oppositional/conduct disordered children. Two groups received parent training and one received additional social support. |
| Davidson 2011 | Pre‐post methodology. Not an RCT. |
| Dekovic 2010 | Not randomised. Intervention (Home Start) involved home visits. |
| DeRosier 2007 | RCT; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; outcomes assessed: social skills knowledge and assertive social problem‐solving; the study did not focus on parental psychosocial health. |
| Dionne 2009 | RCT; participants met the inclusion criteria; a wait‐list control group; intervention was not group‐based. |
| Doherty 2006 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based after the first session; absence of psychosocial outcomes outcomes; the focuses on the quality of father‐child interaction. |
| Drew 2002 | Randomised; the participants met the inclusion criteria; a treatment as usual control group; intervention was not a standard parenting programme ‐ it consists of different category of intervention, specific to parents of children with autistic spectrum disorders. |
| Duch 2011 | Not randomised. |
| Dumas 2010 | RCT, but excluded because of no relevant control condition. |
| Faircloth 2008 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based. The focus of the study is marital conflict rather than psychosocial health. |
| Feinberg 2008 | RCT; participants were pregnant women; the intervention was not a parenting programme for improving psychosocial health; the study focuses on couple relationship and preparing parents for parenthood. |
| Feinfield 2004 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was delivered both in a group, and individually; children participated in the study and received intervention. |
| Florsheim 2007 | Randomised controlled trial in adolescent preganant teenagers for improving co‐parenting alliance. |
| Forehand 2011 | RCT, but excluded because no relevant outcomes. |
| Forgatch 1999 | Randomised; participants were divorcing mothers with sons in Grades 1‐3; intervention was group‐based; the study did not focus on parental psychosocial health. |
| Fossum 2009 | Randomised; participants met the inclusion criteria; a no‐treatment control group; the intervention was group‐based; outcomes assessed: parent discipline and confidence in parenting . The study focuses on the parent discipline strategies rather than parental psychosocial health. |
| Hahlweg 2010 | RCT, but excluded because no relevant outcomes. |
| Harrison 1997 | Randomised controlled trial. Programme offered to fathers only. Control group had videotape intervention so did not meet the inclusion criteria. |
| Havighurst 2009 | Randomised; participants met the inclusion criteria; a wait‐list control group; the intervention was group‐based; absence of relevant parent psychosocial health primary outcomes; focuses on improving child behaviour. |
| Hawkins 2006 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was self‐guided, focusing on parenthood during the first year; the study did not focus on parental psychosocial health. |
| Hayes 2008 | Randomised; participants met the inclusion criteria; an 'enhanced' wait‐list control group; the intervention was a combination of group and individual sessions. |
| Heinrichs 2010 | RCT, but excluded because of no relevant control condition. |
| Helfenbaum 2007 | Randomised; participants met the inclusion criteria; a no‐treatment control; intervention was group‐based; the study focuses on child behaviour. |
| Hoff 2005 | Randomised: participants met the inclusion criteria; a treatment as usual control group; intervention was group‐based but did not primarily focus on improving parental psychosocial health; intervention was "specifically designed to decrease parental distress by teaching parents (of children with newly diagnosed diabetes) about the construct of uncertainty as well as uncertainty management techniques" (page 331, col 1). |
| Hughes 2004 | Randomised; participants met the inclusion criteria; a wait‐list control group; the intervention was group‐based; the study focuses on parenting skills of maltreating mothers and on autonomy rather than parental psychosocial outcomes. |
| Hutchings 2002 | Not fully randomised; "initially, referrals were randomly assigned to each treatment group. Unfortunately, there were not quite as many potential participants as had been predicted by the pilot study to complete the study in the allocated time slot, treatment was allocated to the next intensive treatment slot as it became available group based intervention" (page 284); intervention was not group‐based. |
| Kaaresen 2008 | Randomised; participants met the inclusion criteria; a treatment as usual control group; the intervention was not group‐based. |
| Kacir 1999 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was not group‐based; the study did not focus on parental psychosocial health. |
| Kalinauskiene 2009 | Randomised; participants met the inclusion criteria; a no‐treatment control group; the intervention was not group‐based. |
| Kazdin 1992 | Randomised; participants did not meet the inclusion criteria: in addition to parents, children were also active participants; interventions were group based, but involved direct work with children; no control group (three interventions were compared). |
| Kazdin 2003 | Randomised; participants met the inclusion criteria; unclear whether treatment received by the control group qualifies as treatment as usual; intervention was not group‐based. |
| Kiebert 2005 | Randomised; participants did not meet the inclusion criteria ‐ they were students not adult parents; a wait‐list control group; intervention was group‐based; the study did not focus on parental psychosocial health. |
| Kim 2008 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; the study focuses on parenting skills rather than parental psychosocial health. |
| Lagges 1999 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was not group‐based; absence of parental psychosocial health outcomes. |
| Lamb 2007 | Not randomised, although the Abstract states that participants were "randomly assigned to treatment or a wait‐list control group''; the control group was self‐selected; the participants met the inclusion criteria; WLC group; intervention was group‐based. |
| Landy 2006 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based. The study focuses on parenting skills rather than parental psychosocial health. |
| Lavigne 2008 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was group‐based; the study focuses on treating early childhood Oppositional Defiant Disorder rather than parental psychosocial health. |
| Leung 2003 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; outcomes assessed: parenting strategies. Tthe study focuses on parenting skills and strategies rather than parental psychosocial health. |
| Lim 2005 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; outcomes assessed: parenting strategies; the study focuses on parenting skills and strategies rather than parental psychosocial health. |
| Linares 2006 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention comprises of a similar number of group‐based and individually‐based sessions; the individual sessions involved children. |
| Martinez 2001 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; the study did not focus on parenting psychosocial outcomes. |
| Martinez 2005 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; outcomes assessed: parenting practices, parenting skills, and general parenting; the study focuses on parenting skills rather than parental psychosocial health. |
| Matos 2009 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was not group‐based. |
| Matthey 2004 | Cluster‐randomised; participants did not meet inclusion criteria: participants were couples who were expected their first child; a treatment as usual control group; intervention was group‐based; the study focuses on preparation for parenthood rather than parental psychosocial health. |
| McCabe 2009 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was not group‐based. |
| McIntyre 2008 | Randomised; participants met the inclusion criteria; control condition appeared to be a 'treatment as usual' plus special education and therapeutic services with a family focused orientation. Study focused on prevention of severe behaviour problem in children and was not not focused on parental psychosocial health, there fore no parental psychosocial outcomes were obtained or reported. |
| Melnyk 2007 | Randomised; participants met the inclusion criteria; control condition appeared to be a 'placebo group'; intervention was not group‐based. |
| Mendelsohn 2007 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was not group‐based. |
| Miller‐Heyl 1998 | Randomised; participants did not meet the inclusion criteria: joint intervention directed at parents and their children; a no‐treatment control group; intervention was group‐based. |
| Mullin 1994 | Not randomised or quasi‐randomised: pre‐post test design; previously classified as a quasi‐RCT using a broad definition, which no longer meets criteria. |
| NCT00183365 | RCT, but excluded because of no relevant control condition. |
| Nixon 2004 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was not group‐based. |
| Ogden 2008 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was not group‐based. |
| Olivares 1997 | Randomised controlled study, but no comparison of some outcomes in the control group. |
| Openden 2005 | Randomised; participants a control group met the inclusion criteria; intervention was not group‐based; absence of parental psychosocial outcomes. |
| Orrell‐Valente 1999 | Randomised; participants met the inclusion criteria; no information about the control condition given; intervention included a home visiting component which might confound the results of the parenting programme. |
| Ostergren 2003 | Design: the first treatment group was not randomised, while the second and third treatment groups, and the control group were randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was not group‐based. |
| Plant 2007 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was not group‐based. |
| Rahman 2009 | Randomised; participants did not meet the inclusion criteria; some pregnant women were included; a no‐treatment control group; intervention comprises of both group‐based and individually‐based sessions. |
| Rapee 2005 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; The study focuses on preventing the development of anxiety in preschool children rather than parental psychosocial health. |
| Reid 2001 | Randomised controlled trial, participants met the inclusion criteria. Combination of results from two Incredible Years Parenting Programs. Control group did not meet the inclusion criteria (the studies compare two treatment conditions). Focusses on parenting skills. |
| Reid 2004 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was group‐based; absence of parental psychosocial health outcomes; the study focuses on engagement in the program and parenting. |
| Ruffolo 2005 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was group‐based; outcomes assessed: parental attitudes towards family functioning (F‐COPES; PLOC); the study did not focus on parental psychosocial health. |
| Sanders 2000 | Randomised; participants met the inclusion criteria; a wait‐list control group; interventions were not group‐based. |
| Sanford 2003 | Randomised; participants did not meet the inclusion criteria: the study focuses solely on families with a parent with clinical depression; WLC group; intervention was group‐based. |
| Sawasdipanich 2010 | RCT but excluded because intervention involved home visits and the lack of any relevant outcome measures. |
| Scott 1987 | Allocation by group alternation. |
| Scott 2002 | Randomised; a multi‐faceted programme, including child literacy; the study did not focus on improving parental psychosocial health. |
| Scott 2005 | This study is follow‐up of an original trial (Scott 2001) that was RCT. Follow‐up was only attempted on those allocated to the intervention condition. Participants in the control condition received the same group parenting training at this time point. |
| Scott 2009 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; outcomes assessed: positive involvement, appropriate discipline, inconsistent parenting, and harsh discipline. The study focuses on parenting strategies rather than parental psychosocial health. |
| Sheeber 1994 | Partially randomised trial. |
| Shifflett 1999 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group based; the study focuses on parenting behaviour only rather than on parental psychosocial health. |
| Singer 1999 | Randomised; intervention was not group‐based. |
| Sonuga‐Barke 2001 | Randomised; a wait‐list control group; intervention was not group‐based (an individually‐based intervention). |
| Sonuga‐Barke 2002 | Randomised; intervention was not group‐based (an individually‐based intervention). |
| St James Roberts 2001 | Randomised; intervention was not group‐based (a leaflet programme). |
| Steiman 2005 | This dissertation is a retrospective analysis of three experimental studies (randomised design). |
| Suchman 2004 | Randomised; participants did not meet the inclusion criteria: participants were mother who had a specific psychiatric disorder and were receiving methadone therapy; control group did not meet the inclusion criteria; intervention was group‐based. |
| Suess 2005 | Randomised; participants met the inclusion criteria; unclear control group condition; intervention was not group‐based (be‐weekly home visits). |
| Sutton 1992 | Randomised; comparisons between three treatment modes and a control group; outcomes assessed: stress; outcome measure was not validated (an 'ad hoc' measure used). |
| Sutton 1995 | Randomised; a wait‐list control group; intervention was not group‐based: telephone based parent training intervention. |
| Thompson 2009 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was not group‐based. |
| Thompson 2010 | RCT, but excluded because intervention involved home visits and direct work with children. |
| Thorell 2009 | Not all participants were randomised: "at each one of the locations, maximum of 26 parents could be accepted to the programme, and if the number who applied was higher than 26, parent were randomly assigned to either the parent training group or to a wait‐list control group. However, in 8 out of 10 areas, all interested parents could be admitted to the programme. A total of 275 families attended the first introductory session" (page 376). |
| Tonge 2006 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention consisted of 10 group‐based and 10 individual sessions. Individual sessions play equal role as group sessions in the intervention. |
| Trost 2007 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; absence of required outcomes; the study focuses on the role of parenting involvement in Eating Disorder prevention of their children, rather than parental psychosocial health. |
| Turner 2006a | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; outcomes assessed: post‐natal depression; outcome measure (a qualitative outcome measure used) was not standardised. |
| Uslu 2006 | Randomised; participants met the inclusion criteria; a treatment as usual control group; intervention was group‐based; the study focuses on parental expressed emotion towards children with learning disorders rather than parental psychosocial health. |
| Van Wyk 1983 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; outcome assessed: personality outcomes; not focussed on improving parental mental health or parenting. Previously classified as included study. |
| Webster‐Stratton 2001 | Randomised; participants did not meet the inclusion criteria: in addition to parents, teachers and social workers were also involved in the programme; intervention was group‐based; the study did not focus on parental psychosocial health. |
| Webster‐Stratton 2004 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; the study focuses on parenting skills rather than parental psychosocial health. |
| Wheatley 2003 | Randomised; participants met the inclusion criteria; unclear whether the control group met the inclusion criteria; intervention was group‐based; the study focuses on preparing for parenthood rather than parental psychosocial health. |
| Whitehurst 2008 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; the study focuses on conflict between divorced and separated parents rather than parental psychosocial health. |
| Whittingham 2009a | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention included some individual sessions with parents; outcomes assessed: parenting skills and perception of parenting skills; the study focuses on parenting skills strategies rather than parental psychosocial health. |
| Whittingham 2009b | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention included some individual sessions with parents; outcomes assessed: parenting skills and perception of parenting skills; the study focuses on parenting skills strategies rather than parental psychosocial health. |
| Wiggins 2009 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention included some individual sessions with parents; outcomes assessed: parenting skills; the study focuses on parenting skills strategies and promoting positive parent‐child relationship rather than parental psychosocial health. |
| Wissow 2008 | Randomised; participants met the inclusion criteria: participants were service providers; a wait‐list control group; intervention was group‐based; the study focuses on impact of brief provider communication training with respect to mental health of parents and children. |
| Wolkchik 1993 | Randomised; participants met the inclusion criteria; a wait‐list control group; intervention was group‐based; the study focuses on parenting skills strategies, mother‐child relationship and negative divorce events rather than parental psychosocial health. |
| Zimmerman 1996 | Randomised; participants met the inclusion criteria; a no‐treatment control group; intervention was group‐based; outcomes assessed: parenting skills scales and family strengths ; previously classified as included study; now excluded on the basis that the study focuses on the influence of parenting skills strategies on family functioning and has no measures of parental psychosocial health. |
Characteristics of studies awaiting assessment [ordered by study ID]
Bayer 2010.
| Methods | Cluster‐randomised controlled trial |
| Participants | 40 primary care nursing centres; 733 English‐speaking mothers of 6 to 7 month old infants consecutively recruited from well‐child appointments of which 80% retained at age 3 years |
| Interventions | 'Toddlers Without Tears' parenting programme |
| Outcomes | Maternal mental health (Depression Anxiety Stress Scales), child externalising behaviour, parenting |
| Notes |
Bywater 2011.
| Methods | Randomised controlled trial |
| Participants | 46 foster carers |
| Interventions | Incredible Years programme |
| Outcomes | Depression, child behaviour, service use, parenting competency |
| Notes |
Cefai 2010.
| Methods | Randomised controlled trial (3 conditions) |
| Participants | 116 parents |
| Interventions | Group‐based programme (2 sessions); individual self‐administered intervention (2 sessions); wait‐list control |
| Outcomes | Sense of competence, parental satisfaction, child problem behaviour |
| Notes |
Eichelberger 2010.
| Methods | Randomised controlled study |
| Participants | 93 families of 3‐6 year old German pre‐school children |
| Interventions | Triple P parent group training |
| Outcomes | Psychological distress, child behaviour problems, parenting strategies and partnership satisfaction |
| Notes | Obtain full translation |
Franz 2007.
| Methods | Randomised controlled study |
| Participants | 61 single mothers suffering from medium grade psychosocial impairment |
| Interventions | An emotion oriented parent training programme, based on attachment theory |
| Outcomes | Psychological impairment, depression and emotional competence. Child behavioural problems |
| Notes | Obtain full translation |
Hampel 2010.
| Methods | Unclear; translation required; ? multicentre randomised trial |
| Participants | Unclear; translation required; ? families with a handicapped child |
| Interventions | Stepping Stones Triple P group parent training |
| Outcomes | Parental stress, dysfunctional parenting, and child behaviour problems |
| Notes | Obtain full translation |
Heinrichs 2006.
| Methods | Cluster‐randomised (by pre‐school) into parent training or control group |
| Participants | 219 two‐parent families |
| Interventions | Triple P parent group training |
| Outcomes | Parenting, child behaviour, psychological distress, relationship satisfaction |
| Notes | Obtain full translation |
Morawska 2011.
| Methods | Randomised controlled trial |
| Participants | 67 parents of children aged 2 to 5 years |
| Interventions | Single session discussion group on positive parenting plus two follow up telephone calls |
| Outcomes | Depressive symptoms; confidence; partner satisfaction |
| Notes |
Naumann 2007.
| Methods | Randomised controlled trial |
| Participants | 280 families |
| Interventions | Triple P parent training or control group |
| Outcomes | Parental competencies |
| Notes | Obtain full translation |
Reedtz 2011.
| Methods | Randomised controlled trial |
| Participants | 186 parents of children aged 2 to 8 years |
| Interventions | Short parenting programme (Incredible Years) |
| Outcomes | Sense of competence, parenting skills |
| Notes |
Sanders 2011.
| Methods | Randomised controlled trial |
| Participants | 121 working parents with children between 1 and 16 years |
| Interventions | Workplace Triple P group intervention |
| Outcomes | Personal distress, dysfunctional parenting, work commitment, work satisfaction and self‐efficacy |
| Notes |
Characteristics of ongoing studies [ordered by study ID]
NTR1338.
| Trial name or title | RCT of the positive parenting programme (Triple P) versus care as usual provided by the preventive child healthcare system |
| Methods | RCT |
| Participants | Parents of 9‐11 year old primary school children in the Netherlands with increased but subclinical levels of psychosocial problems |
| Interventions | Triple‐P (level 3) versus care‐as‐usual control |
| Outcomes | Child problem behaviour; parenting behaviour; parenting stress (including depression and anxiety symptoms) |
| Starting date | Registered in 2008; results available 2012 |
| Contact information | w.spijkers@med.umcg.nl |
| Notes | Trial registration: NTR1338 |
Differences between protocol and review
We changed the title from 'maternal' to 'parental'.
We updated the Background and Discussion text.
We clarified the participants, i.e. specified that parents with disabled children were included.
We clarified that we excluded studies that explicitly targeted and thereby focused solely on parents with a specific psychiatric disorder, including for example clinical depression. We also excluded studies that focused solely on child outcomes, or were focused on preparation for parenthood, or were studies with participants who were pregnant or parenting teenagers (below the age of 20), and studies with mixed age groups where data were not presented separately for adult and teenage parents. We excluded studies which did not focus on parental mental health or parenting. This is not a change but was not explicitly described in the previous published version of the review.
Outcomes change to primary and secondary. We clarified the types of outcomes included in the term 'parental psychosocial health'. In the previous published version of the review perception of parenting skills as an outcome was implied but not specified as such in the list of outcomes, this has now been clarified. No new outcomes other than adverse effects.
Quasi‐randomised trials were defined as those where the participants were assigned to treatment groups on the basis of alternate allocation (Higgins 2008) but not if they were described as quasi‐experimental and were of a pre‐ and post‐test design. In this updated version of the review we re‐assessed two studies (Anastopoulos 1993; Mullin 1994) that were previously categorised as quasi‐randomised and excluded them on the basis that they did not involve alternate allocation.
We conducted analyses based on the duration of the interventions and the type of intervention.
We updated the Methods section to take into account Risk of BIas assessments.
Criteria for considering studies for this review. We specified in more detail the types of participant, interventions and types of studies.
Unit of analysis issues. We updated the Methods section for dealing with cluster randomised trials. We added a section about dealing with multi‐arm trials.
Timing of outcome assessment. We clarified the time points in the Methods section. Although these were implied in the previous published versions of the review, it was not clearly stated that these time points were prospectively applied to data extraction. Data were extracted for the following time points, post‐intervention assessment: any time from immediate post intervention to up to 4 weeks post‐intervention; short‐term follow‐up assessment: one to six months post‐intervention; long‐term assessment: > six months post‐intervention.
Contributions of authors
JB updated and wrote the background and discussion sections, edited the methods, wrote up results, gave advice about the set up of the analyses, overall responsibility for ensuring data in the review are correct.
NS reviewed the draft and scope of the review with the contact author of the review (JB). Searched for potential included studies from searches run by the CDPLP Group, identified included studies, checked the old excluded studies and excluded newly found studies that did not fit the inclusion criteria. Managed data extraction and entry. Completed the tables of characteristics of studies, extracted data, competed 'Risk of bias' tables (RoB), extracted data for use in analysis, constructed outcomes tables, checked the existing included studies data, entered data into the analysis table, set up meta‐analyses, wrote up methods and results section, inserted analysis results into text, entered and checked references, attended progress meetings, responsible for working collaboratively with other authors to meet publication deadlines.
CB worked with all review authors to ensure that the review met publication deadlines. Contributed to the methods section, analyses, recorded outcomes for drafts of the additional tables, excluded studies table. General review and publication support.
NH identified potential included studies, jointly finalised list of included studies with NS, data extraction, entry of RoB data for new included studies checking data entry, tables of characteristics of studies, extracted data, contributed to 'Risk of bias' tables (RoB), extracted data for use in analysis, entered data into analysis table, set up meta‐analyses, wrote up results section, inserted analysis results into text.
VR contributed the investigation of cluster effects, contributed to the analysis plan and advised about the set up of analyses.
Sources of support
Internal sources
UK Cochrane Centre, UK.
Health Services Research Unit at the University of Warwick, UK.
Institute of Mental Health, Nottinghamshire Healthcare NHS Trust, UK.
External sources
NHS Cochrane Collaboration Programme Grant Scheme (NIHR), UK.
Declarations of interest
Jane Barlow ‐ none known.
Nadja Smailagic ‐ none known.
Nick Huband ‐ none known.
Verena Roloff ‐ none known.
Cathy Bennett ‐ I am employed by Systematic Research Ltd and I received a consultancy fee for my contributions to this review.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Blakemore 1993 {published data only}
- Blakemore B, Shindler S, Conte R. A problem solving training program for parents of children with attention deficit hyperactivity disorder. Canadian Journal of School Psychology 1993;9(1):66‐85. [Google Scholar]
Bradley 2003 {published data only}
Chronis 2006 {published data only}
- Chronis A. The addition of the "coping with depression course" to behavioral parent training for mothers of children with attention deficit hyperactivity disorder. Dissertation Abstracts International 2003; Vol. 63, issue 8‐B:3907. [MEDLINE: ; CN‐00462983]
- Chronis AM, Gamble SA, Roberts JE, Pelham WE. Cognitive‐behavioral depression treatment for mothers of children with attention‐deficit/hyperactivity disorder. BehaviorTherapy 2006; Vol. 37:143‐58. [MEDLINE: ] [DOI] [PubMed]
Cunningham 1995 {published data only}
- Cunningham CE, Bremner R, Boyle M. Large group community‐based parenting programs for families of preschoolers at risk for disruptive behaviour disorders: utilization, cost‐effectiveness, and outcome. Journal of Child Psychology and Psychiatry and Allied Disciplines 1995;36(7):1141‐59. [DOI] [PubMed] [Google Scholar]
DeGarmo 2004 {published data only}
Fanning 2007 {published data only}
- Fanning JL. Parent Training for Caregivers of Typically Developing, Economically Disadvantaged Preschoolers: An Initial Study in Enhancing Language Development, Avoiding Behavior Problems, and Regulating Family Stress (PhD thesis). Oregon: University of Oregon, 2007. [Google Scholar]
Fantuzzo 2007 {published data only}
- Fantuzzo J, Stevenson H, Abdul Kabir S, Perry MA. An investigation of a community‐based Intervention for socially isolated parents with a history of child maltreatment. Journal of Family Violence 2007; Vol. 22:81‐9. [MEDLINE: ; 0885‐7482]
Farrar 2005 {published data only}
- Farrar RLE. The Effect of a Cognitively Based Parent Training Intervention on Parental Stress. Tulsa, OK: The University of Tulsa, 2005. [MEDLINE: ] [Google Scholar]
Feliciana 2005 {published data only}
- Feliciana JB. The Impact of Participation in a Parent Training Program on Maternal Sense of Competency and Stress in Urban African‐American Mothers. Washington, DC: Howard University, 2005. [Google Scholar]
Gallart 2005 {published data only}
- Gallart SC Matthey S. The effectiveness of group Triple P and the impact of the four telephone contacts. Behaviour Change 2005; Vol. 22, issue 2:71‐80. [MEDLINE: ; CN‐00569669]
Gammon 1991 {published data only}
- Gammon EA, Rose SD. The coping skills training program for parents of children with developmental disabilities: an experimental evaluation. Research on Social Work Practice 1991;1(3):244‐56. [Google Scholar]
Gardner 2006 {published data only}
- Gardner F Burton J, Klimes I. Randomised controlled trial of a parenting intervention in the voluntary sector for reducing child conduct problems: outcomes and mechanisms of change. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2006; Vol. 47, issue 11:1123‐32. [MEDLINE: ; CN‐00573306] [DOI] [PubMed]
Greaves 1997 {published data only}
- Greaves D. The effect of rational‐emotive parent education on the stress of mothers of children with Down Syndrome. Journal of Rational‐Emotive and Cognitive‐Behavior Therapy 1997;15(4):249‐67. [Google Scholar]
Gross 1995 {published data only}
- Gross D, Fogg L, Tucker S. The efficacy of parent training for promoting positive parent‐toddler relationships. Research in Nursing and Health 1995;18(6):489‐99. [DOI] [PubMed] [Google Scholar]
- Tucker S, Gross D, Fogg L, Delaney K, Lapporte R. The long‐term efficacy of a behavioural parent training intervention for families with 2‐year‐olds. Research in Nursing and Health 1998;21(3):199‐210. [DOI] [PubMed] [Google Scholar]
Gross 2003 {published data only}
Gross 2009 {published data only}
- Gross D, Garvey C, Julion W, Fogg L, Tucker S, Mokros H. Efficacy of the Chicago parent program with low‐income African American and Latino parents of young children. Prevention Science: the official journal of the Society for Prevention Research 2009; Vol. 10, issue 1:54‐65. [DOI] [PMC free article] [PubMed]
Gutierrez 2007 {published data only}
- Gutierrez SR. A Comparison of Two Parent Education Programs on the Reduction of Parent‐Child Stress in Mother‐Child Relationships of Hispanic Migrant Farmworkers. Tucson, AZ: The University of Arizona, 2007. [MEDLINE: ] [Google Scholar]
Hanisch 2010 {published data only}
- Hanisch C, Freund‐Braier I, Hautmann C, Janen N, Pluck J, Brix G, et al. Detecting effects of the indicated prevention programme for externalizing problem behaviour (PEP) on child symptoms, parenting, and parental quality of life in a randomized controlled trial. Behavioural and Cognitive Psychotherapy 2010;38(1):95‐112. [1469‐1833] [DOI] [PubMed] [Google Scholar]
Hiscock 2008 {published data only}
- Hiscock H, Bayer JK, Price A, Ukoumunne OC, Rogers S, Wake M. Universal parenting programme to prevent early childhood behavioural problems: cluster randomised trial. BMJ 2008;336(7639):318‐21. [MEDLINE: ; 0959‐535X] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchings J. A parenting programme does not affect behavioural problems in toddlers. Evidence‐Based Mental Health 2008;11(4):119. [1362‐0347] [DOI] [PubMed] [Google Scholar]
Hutchings 2007 {published data only}
- Bywater T, Hutchings J, Daley D, Whitaker C, Yeo ST, Jones K, et al. Long‐term effectiveness of a parenting intervention for children at risk of developing conduct disorder. British Journal of Psychiatry 2009;195(4):318‐24. [0007‐1250] [DOI] [PubMed] [Google Scholar]
- Eames C, Daley D, Hutchings J, Whitaker C, Bywater T, Jones K, Hughes J. The impact of group leaders' behaviour on parents acquisition of key parenting skills during parent training. Behaviour Research and Therapy 2010;48(12):1221‐6. [DOI] [PubMed] [Google Scholar]
- Hawkins‐Walsh E. A cognitive‐behavioural parenting intervention reduced problem behaviours in at‐risk preschool children and improved parenting skills in socially disadvantaged families. Evidence‐Based Nursing 2007;10(4):105. [MEDLINE: ; 1367‐6539] [DOI] [PubMed] [Google Scholar]
- Hutchings JGF, Bywater T, Daley D, Whitaker C, Jones K, Eames C, et al. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. BMJ 2007; Vol. 334, issue 7595:678. [MEDLINE: ; CN‐00579132] [DOI] [PMC free article] [PubMed]
Irvine 1999 {published data only}
- Irvine AB, Biglan A, Smolkowski K, Metzler CW, Ary DV. The effectiveness of a parenting skills program for parents of middle school students in small communities. Journal of Consulting and Clinical Psychology 1999;67(6):811‐25. [DOI] [PubMed] [Google Scholar]
Joachim 2010 {published data only}
Joyce 1995 {published data only}
- Joyce MR. Emotional relief for parents: is rational‐emotive parent education effective?. Journal of Rational‐Emotive and Cognitive‐Behavior Therapy 1995;13(1):55‐75. [Google Scholar]
Larsson 2009 {published data only}
- Larsson B, Fossum S, Clifford G, Drugli MB, Handegård BH, Mørch W. Treatment of oppositional defiant and conduct problems in young Norwegian children: results of a randomized controlled trial. European Child and Adolescent Psychiatry 2009;18(1):42‐52. [1018‐8827] [DOI] [PubMed] [Google Scholar]
Lipman 2005 {published data only}
- Lipman EL, Boyle MH. Social support and education groups for single mothers: a randomized controlled trial of a community‐based program. Canadian Medical Association Journal 2005; Vol. 173, issue 12:1451‐6. [MEDLINE: ; CN‐00553003] [DOI] [PMC free article] [PubMed]
Martin 2003 {published data only}
- Martin AJ, Sanders MR. Balancing work and family: A controlled evaluation of the Triple P‐Positive Parenting Program as a work‐site intervention. Child and Adolescent Mental Health 2003;8(4):161‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Matsumoto 2007 {published data only}
- Matsumoto Y, Sofronoff K, Sanders MR. The efficacy and acceptability of the Triple P‐positive parenting program with Japanese parents. Behaviour Change 2007;24(4):205‐18. [MEDLINE: ] [Google Scholar]
Matsumoto 2010 {published data only}
- Matsumoto Y, Sofronoff K, Sanders MR. Investigation of the effectiveness and social validity of the Triple P Positive Parenting Program in Japanese society. Journal of Family Psychology 2010;24(1):87‐91. [0893‐3200] [DOI] [PubMed] [Google Scholar]
McGillicuddy 2001 {published data only}
- McGillicuddy NB, Rychtarik RG, Duquette JA, Morsheimer T. Development of a skill training program for parents of substance‐abusing adolescents. Journal of Substance Abuse Treatment 2001;20(1):59‐68. [DOI] [PubMed] [Google Scholar]
Morawska 2009 {published data only}
Niccols 2009 {published data only}
Nicholson 2002 {published data only}
- Nicholson B, Anderson M, Fox R, Brenner V. One family at a time: a prevention program for at‐risk parents. Journal of Counseling & Development 2002;80(3):362‐71. [Google Scholar]
Nixon 1993 {published data only}
- Nixon CD, Singer GHS. Group cognitive‐behavioral treatment for excessive parental self‐blame and guilt. American Journal on Mental Retardation 1993;97(6):665‐72. [PubMed] [Google Scholar]
Odom 1996 {published data only}
- Odom SE. Effects of an educational intervention on mothers of male children with attention deficit hyperactivity disorder. Journal of Community Health Nursing 1996;13(4):207‐20. [DOI] [PubMed] [Google Scholar]
Patterson 2002 {published data only}
- Patterson J, Barlow J, Mockford C, Klimes I, Pyper C, Stewart‐Brown S. Improving mental health through parenting programmes: block randomised controlled trial. Archives of Disease in Childhood 2002;87:472‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reading R. Impact of a general practice based group parenting programme: quantitative and qualitative results from a controlled trial at 12 months. Child: Care, Health and Development 2004;30(5):560‐1. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart Brown SPJ, Mockford C, Barlow J, Klimes I, Pyper C. Impact of a general practice based group parenting programme: quantitative and qualitative results from a controlled trial at 12 months. Archives of Disease in Childhood 2004;89(6):519‐25. [MEDLINE: ; CN‐00469249] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pisterman 1992a {published data only}
- Pisterman S, Firestone P, McGrath P, Goodman JT, Webster I, Mallory R, et al. The effects of parent training on parenting stress and sense of competence. Canadian Journal of Behavioural Science 1992;24(1):41‐58. [Google Scholar]
Pisterman 1992b {published data only}
- Pisterman S, Firestone P, McGrath P, Goodman JT, Webster I, Mallory R, et al. The role of parent training in treatment of preschoolers with ADHD. American Journal of Orthopsychiatry 1992;62(3):397‐407. [DOI] [PubMed] [Google Scholar]
Schultz 1993 {published data only}
- Schultz CL, Schultz NC, Bruce EJ, Smyrnios KX, Carey LB, Carey CL. Psychoeducational support for parents of children with intellectual disability. International Journal of Disability, Development and Education 1993;40(3):205‐16. [Google Scholar]
Sirbu 1978 {published data only}
- Sirbu W, Cotler S, Jason LA. Primary prevention: teaching parents behavioral child rearing skills. Family Therapy 1978;5(2):163‐70. [Google Scholar]
Spaccerelli 1992 {published data only}
- Spaccarelli S, Cotler S, Penman D. Problem‐solving skills training as a supplement to behavioral parent training. Cognitive Therapy and Research 1992;16(1):1‐18. [Google Scholar]
Taylor 1998 {published data only}
- Taylor TK, Schmidt F, Pepler D, Hodgins C. A comparison of eclectic treatment with Webster‐Stratton's parents and children series in a children's mental health center: a randomised controlled trial. Behavior Therapy 1998;29(2):221‐40. [Google Scholar]
Treacy 2005 {published data only}
- Treacy L, Tripp G, Baird A. Parent stress management training for attention‐deficit/hyperactivity disorder. Behavior Therapy 2005; Vol. 36, issue 3:223‐33. [MEDLINE: ]
Turner 2007 {published data only}
- Turner KM, Richards M, Sanders MR. Randomised clinical trial of a group parent education programme for Australian Indigenous families. Journal of Paediatrics and Child Health 2007; Vol. 43, issue 6:429‐37. [MEDLINE: ; CN‐00615331] [DOI] [PubMed]
- Turner KMT, Sanders MR, Richards M, Arthur N. Tailoring and evaluating an evidence‐based group family intervention program for parents in indigenous communities. Australian Journal of Psychology; Proceedings The Abstracts of the Joint Conference of the Australian Psychological Society and the New Zealand Psychological Society. London: Taylor and Francis, 2006; Vol. 58:201. [MEDLINE: ]
van den Hoofdakker 2007 {published data only}
- Hoofdakker BJ, Veen‐Mulders LL, Sytema S, Emmelkamp PMG, Minderaa RB, Nauta MH. Effectiveness of behavioral parent training for children with ADHD in routine clinical practice: a randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry 2007; Vol. 46, issue 10:1263‐71. [MEDLINE: ] [DOI] [PubMed]
Wang 2005 {published data only}
- Wang P. Effects of a Parent Training Program for Teaching Children with Autism in the People's Republic of China (PhD thesis). New York, NY: Columbia University, 2005. [Google Scholar]
Webster Stratton 1988 {published data only}
- Webster‐Stratton C, Kolpacoff M, Hollinsworth T. Self‐administered videotape therapy for families with conduct‐problem children: comparison with two cost‐effective treatments and a control group. Journal of Consulting and Clinical Psychology 1988;56(4):558‐66. [DOI] [PubMed] [Google Scholar]
Wolfe 2003 {published data only}
- Wolfe RB, Hirsch BJ. Outcomes of parent education programs based on reevaluation counseling. Journal of Child and Family Studies 2003; Vol. 12, issue 1:61‐76. [MEDLINE: ; 1062‐1024]
Wolfson 1992 {published data only}
- Wolfson A, Lacks P, Futterman A. Effects of parent training on infant sleeping patterns, parents stress, and perceived parental competence. Journal of Consulting and Clinical Psychology 1992;60(1):41‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Al‐Hassan 2011 {published data only}
- Al‐Hassan SM, Lansford JE. Evaluation of the better parenting programme in Jordan. Early Child Development and Care 2011;181(5):587‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anastopoulos 1993 {published data only}
- Anastopoulos AD, Shelton TL, DuPaul GJ, Guevremont DC. Parent training for attention‐deficit hyperactivity disorder: its impact on parent functioning. Journal of Abnormal Child Psychology 1993;21(5):581‐96. [DOI] [PubMed] [Google Scholar]
Atherton 2007 {published data only}
- Atherton C. The Incredibles. Community Care 2007; Vol. 1673:32‐33. [MEDLINE: ; 0307‐5508]
Azrin 2001 {published data only}
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, Decato LA. A controlled evaluation and description of individual‐cognitive problem solving and family‐behavior therapies in dually‐diagnosed conduct‐disordered and substance‐dependent youth. Journal of Child & Adolescent Substance Abuse 2001;11(1):1‐43. [Google Scholar]
Barkby 2011 {published data only}
- Barkby H, Butterworth R, Davies J, Marsland L, O'Shaughnessy R. Bonding with baby: A pilot parent‐infant intervention programme in Liverpool. Clinical Psychology Forum 2011;224:17‐21. [Google Scholar]
Barkley 2001 {published data only}
- Barkley RA, Edwards G, Laneri M, Fletcher K, Metevia L. The efficacy of problem‐solving communication training alone, behavior management training alone, and their combination for parent‐adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology 2001;69(6):926‐41. [PubMed] [Google Scholar]
Barlow 2007 {published data only}
Barlow 2008 {published data only}
- Barlow JH, Powell LA, Gilchrist M, Fotiadou M. The effectiveness of the training and support program for parents of children with disabilities: a randomized controlled trial. Journal of Psychosomatic Research 2008;64(1):55‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Baydar 2003 {published data only}
- Baydar N, Reid MJ, Webster Stratton C. The role of mental health factors and program engagement in the effectiveness of a preventive parenting program for Head Start mothers. Child Development 2003;74(5):1433‐53. [MEDLINE: ; CN‐00458200] [DOI] [PubMed] [Google Scholar]
Berry 2007 {published data only}
- Berry D, Savoye M, Melkus G, Grey M. An intervention for multiethnic obese parents and overweight children. Applied Nursing Research 2007;20(2):63‐71. [MEDLINE: ; 0897‐1897] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodenmann 2008 {published data only}
Bogle 2007 {published data only}
- Bogle KE. Evaluation of a Brief Group Parent Training Intervention in the Context of an After‐School Program for Middle‐School Students. South Carolina: University of South Carolina, 2007. [Google Scholar]
Bradley 2010 {published data only}
- Bradley R, Whiteside‐Mansell L, Casey P, Barrett K. Impact of a two‐generation early education program on parenting processes at age 18. Journal of Family Psychology 2010;24(4):478‐84. [DOI] [PubMed] [Google Scholar]
Brunk 1987 {published data only}
- Brunk M, Henggeler SW, Whelan JP. Comparison of multisystemic therapy and parent training in the brief treatment of child abuse and neglect. Journal of Consulting and Clinical Psychology 1987;55(2):171‐8. [DOI] [PubMed] [Google Scholar]
Camp 1997 {published data only}
- Camp JM, Finkelstein N. Parenting training for women in residential substance abuse treatment. Journal of Substance Abuse Treatment 1997;14(5):411‐22. [DOI] [PubMed] [Google Scholar]
Chacko 2006 {published data only}
- Chacko A. Treatment for Single‐Mothers of Children Diagnosed with ADHD: A Comparison between a Traditional and an Enhanced Behavioral Parenting Program. New York: State University of New York at Buffalo, 2006. [MEDLINE: ] [Google Scholar]
Chacko 2009 {published data only}
Chazan‐Cohen 2007 {published data only}
Coard 2007 {published data only}
- Coard SI, Foy‐Watson S, Zimmer C, Wallace A. Considering culturally relevant parenting practices in intervention development and adaptation: a randomized controlled trial of the black parenting strengths and strategies (BPSS) program. The Counseling Psychologist 2007;35(6):797‐820. [MEDLINE: ] [Google Scholar]
Connell 1997 {published data only}
- Connell S, Sanders MR, Markie‐Dadds C. Self‐directed behavioral family intervention for parents of oppositional children in rural and remote areas. Behavior Modification 1997;21(4):379‐408. [DOI] [PubMed] [Google Scholar]
Cooper 2009 {published data only}
- Cooper PJ, Tomlinson M, Swartz L, Landman M, Molteno C, Stein A, et al. Improving quality of mother‐infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ 2009; Vol. 338, issue 7701:997. [0959‐8146] [DOI] [PMC free article] [PubMed]
Cummings 2000 {published data only}
- Cummings LL. Parent training: A Program for Parents of Two‐ and Three‐year‐olds (PhD thesis). Mount Pleasant, MI: Cental Michigan University, 2000. [Google Scholar]
Dadds 1992 {published data only}
- Dadds MR, McHugh TA. Social support and treatment outcome in behavioral family therapy for child conduct problems. Journal of Consulting and Clinical Psychology 1992;60(2):252‐9. [DOI] [PubMed] [Google Scholar]
Davidson 2011 {published data only}
- Davidson VL. A Parent Training Program for Caucasian and Latino Parents of Children with Developmental Delays or Behavioral Difficulties (Psy D dissertation). Chicago, Illinois: Chicago School of Professional Psychology, 2011. [Google Scholar]
Dekovic 2010 {published data only}
- Dekovic M, Asscher JJ, Hermanns J, Reitz E, Prinzie P, Akker AL. Tracing changes in families who participated in the home‐start parenting program: parental sense of competence as mechanism of change. Prevention Science 2010;11(3):263‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
DeRosier 2007 {published data only}
- DeRosier ME, Gilliom M. Effectiveness of a parent training program for improving children's social behavior. Journal of Child and Family Studies 2007;16(5):660‐70. [1062‐1024] [Google Scholar]
Dionne 2009 {published data only}
- Dionne R, Davis B, Sheeber L, Madrigal L. Initial evaluation of a cultural approach to implementation of evidence‐based parenting interventions in American Indian communities. Journal of Community Psychology 2009;37(7):911‐21. [0090‐4392] [Google Scholar]
Doherty 2006 {published data only}
Drew 2002 {published data only}
- Drew A, Baird G, Baron‐Cohen S, Cox A, Slonims V, Wheelwright S, et al. A pilot randomised control trial of a parent training intervention for pre‐school children with autism: preliminary findings and methodological challenges. European Child & Adolescent Psychiatry 2002;11(6):266‐72. [DOI] [PubMed] [Google Scholar]
Duch 2011 {published data only}
- Duch H, Rodriguez C. Strengthening families in Head Start: The impact of a parent education programme on the emotional well‐being of Latino families. Early Child Development and Care 2011;181(6):733‐48. [Google Scholar]
Dumas 2010 {published data only}
- Dumas J, Begle A, French B, Pearl A. Effects of monetary incentives on engagement in the PACE parenting program. Journal of Clinical Child and Adolescent Psychology 2010;39(3):302‐313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faircloth 2008 {published data only}
- Faircloth WB, Cummings EM. Evaluating a parent education program for preventing the negative effects of marital conflict. Journal of Applied Developmental Psychology 2008;29(2):141‐56. [MEDLINE: ; 0193‐3973] [Google Scholar]
Feinberg 2008 {published data only}
- Feinberg ME, Kan ML. Establishing family foundations: intervention effects on coparenting, parent/infant wellbeing, and parent‐child relations. Journal of Family Psychology 2008;22(2):253‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feinfield 2004 {published data only}
- Feinfield KA BB. Empirical support for a treatment program for families of young children with externalizing problems. Journal of Clinical Child and Adolescent Psychology 2004;33(1):182‐95. [MEDLINE: ; CN‐00468832] [DOI] [PubMed] [Google Scholar]
Florsheim 2007 {published data only}
- Florsheim P, Hall S, Gaskill M, McArthur L, McElligott K. The Young Parenthood Program: a preventive intervention to support positive coparenting among pregnant adolescents and their partners. Journal of Adolescent Health 2007;40 Suppl 1(2):14. [MEDLINE: ; 1054‐139x] [Google Scholar]
Forehand 2011 {published data only}
- Forehand RL, Merchant MJ, Parent J, Long N, Linnea K, Baer J. An examination of a group curriculum for parents of young children with disruptive behavior. Behavior Modification 2011;3:235‐51. [DOI] [PubMed] [Google Scholar]
Forgatch 1999 {published data only}
- Forgatch MS, DeGarmo DS. Parenting through change: an effective prevention program for single mothers. Journal of Consulting and Clinical Psychology 1999;67(5):711‐24. [DOI] [PubMed] [Google Scholar]
Fossum 2009 {published data only}
- Fossum S, Morch WT, Handegard BH, Drugli MB, Larsson B. Parent training for young Norwegian children with ODD and CD problems: predictors and mediators of treatment outcome. Scandinavian Journal of Psychology 2009;50(2):173‐81. [DOI] [PubMed] [Google Scholar]
Hahlweg 2010 {published data only}
- Hahlweg K, Heinrichs N, Kuschel A, Bertram H, Naumann S. Long‐term outcome of a randomized controlled universal prevention trial through a positive parenting program: is it worth the effort?. Child and Adolescent Psychiatry and Mental Health 2010;4:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrison 1997 {published data only}
- Harrison K. Parental training for incarcerated fathers: effects on attitudes, self‐esteem, and children's self‐perceptions. The Journal of Social Psychology 1997;137(5):588‐93. [DOI] [PubMed] [Google Scholar]
Havighurst 2009 {published data only}
- Havighurst SS, Wilson KR, Harley AE, Prior MR. Tuning in to kids: An emotion‐focused parenting program ‐ initial findings from a community trial. Journal of Community Psychology 2009;37(8):1008‐23. [0090‐4392] [Google Scholar]
Hawkins 2006 {published data only}
- Hawkins AJ, Fawcett EB, Carroll JS, Gilliland TT. The marriage moments program for couples transitioning to parenthood: divergent conclusions from formative and outcome evaluation data. Journal of Family Psychology 2006;20(4):561‐70. [MEDLINE: ; 0272‐4944] [DOI] [PubMed] [Google Scholar]
Hayes 2008 {published data only}
Heinrichs 2010 {published data only}
- Heinrichs N, Jensen‐Doss A. The effects of incentives on families' long‐term outcome in a parenting program. Journal of Clinical Child and Adolescent Psychology 2010;39(5):705‐12. [DOI] [PubMed] [Google Scholar]
Helfenbaum 2007 {published data only}
- Helfenbaum KED, Ortiz C. Parent‐training groups for fathers of Head Start Children: a pilot study of their feasibility and impact on child behavior and intra‐familial relationships. Child and Family Behavior Therapy 2007; Vol. 29, issue 2:47‐64. [0731‐7107]
Hoff 2005 {published data only}
- Hoff AL, Mullins LL, Gillaspy SR, Page MC, Pelt JC, Chaney JM. An intervention to decrease uncertainty and distress among parents of children newly diagnosed with diabetes: a pilot study. Families, Systems, & Health 2005; Vol. 23, issue 3:329‐42. [MEDLINE: ]
Hughes 2004 {published data only}
Hutchings 2002 {published data only}
- Hutchings J, Appleton P, Smith M, Lane E, Nash S. Evaluation of two treatments for children with severe behaviour problems: child behaviour and maternal mental health outcomes. Behavioural & Cognitive Psychotherapy 2002;30(3):279‐95. [Google Scholar]
Kaaresen 2008 {published data only}
Kacir 1999 {published data only}
- Kacir CD, Gordon DA. Parenting adolescents wisely: the effectiveness of an interactive videodisk parent training program in Appalachia. Child & Family Behavior Therapy 1999;21(4):1‐22. [Google Scholar]
Kalinauskiene 2009 {published data only}
- Kalinauskiene L, Cekuoliene D, Ijzendoorn MH, Bakermans‐Kranenburg MJ, Juffer F, Kusakovskaja I. Supporting insensitive mothers: the Vilnius randomized control trial of video‐feedback intervention to promote maternal sensitivity and infant attachment security. Child: Care, Health & Development 2009; Vol. 35, issue 5:613‐23. [0305‐1862] [DOI] [PubMed]
Kazdin 1992 {published data only}
- Kazdin AE, Siegel TC, Bass D. Cognitive problem‐solving skills training and parent management training in the treatment of antisocial behavior in children. Journal of Consulting and Clinical Psychology 1992;60(5):733‐47. [DOI] [PubMed] [Google Scholar]
Kazdin 2003 {published data only}
Kiebert 2005 {published data only}
- Kiebert BW. The Effect of Parenthood Education on Self‐efficacy, Parent Effectiveness, and the Parent‐Child Relationship in an Alternative High School Student Population. Hagerman, ID: University of Idaho, 2005. [MEDLINE: ] [Google Scholar]
Kim 2008 {published data only}
- Kim E, Cain KC, Webster‐Stratton C. The preliminary effect of a parenting program for Korean American mothers: a randomized controlled experimental study. International Journal of Nursing Studies 2008; Vol. 45, issue 9:1261‐73. [DOI] [PMC free article] [PubMed]
Lagges 1999 {published data only}
- Lagges AM, Gordon DA. Use of an interactive laserdisc parent training program with teenage parents. Child and Family Behavior Therapy 1999;21(1):19‐37. [Google Scholar]
Lamb 2007 {published data only}
- Lamb K. Addressing the challenges of parenting: parent training with parents of children with ADHD. Dissertation Abstracts International 2007; Vol. 67, issue 11. [MEDLINE: ; 0419‐4209]
Landy 2006 {published data only}
- Landy S, Menna R. An evaluation of a group intervention for parents with aggressive young children: improvements in child functioning, maternal confidence, parenting knowledge and attitudes. Early Child Development and Care 2006; Vol. 176, issue 6:605‐20. [MEDLINE: ]
Lavigne 2008 {published data only}
Leung 2003 {published data only}
Lim 2005 {published data only}
- Lim M, Stormshak EA, Dishion TJ. A one‐session intervention for parents of young adolescents: videotape modeling and motivational group discussion. Journal of Emotional and Behavioral Disorders 2005; Vol. 13, issue 4:194‐9. [MEDLINE: ; 1063‐4266]
Linares 2006 {published data only}
Martinez 2001 {published data only}
- Martinez CR, Forgatch MS. Preventing problems with boys' noncompliance: effects of a parent training intervention for divorcing mothers. Journal of Consulting and Clinical Psychology 2001;69(3):416‐28. [DOI] [PubMed] [Google Scholar]
Martinez 2005 {published data only}
Matos 2009 {published data only}
Matthey 2004 {published data only}
McCabe 2009 {published data only}
McIntyre 2008 {published data only}
- McIntyre LL. Parent training for young children with developmental disabilities: randomized controlled trial. American Journal of Mental Retardation 2008;113(5):356‐68. [PUBMED: 18702556] [DOI] [PMC free article] [PubMed] [Google Scholar]
Melnyk 2007 {published data only}
- Melnyk BM, Crean HF, Feinstein NF, Fairbanks E, Alpert Gillis LJ. Testing the theoretical framework of the COPE program for mothers of critically ill children: an integrative model of young children's post‐hospital adjustment behaviors. Journal of Pediatric Psychology 2007; Vol. 32, issue 4:463‐74. [MEDLINE: ] [DOI] [PubMed]
Mendelsohn 2007 {published data only}
- Mendelsohn AL, Valdez PT, Flynn V, Foley GM, Berkule SB, Tomopoulos S, et al. Use of videotaped interactions during pediatric well‐child care: Impact at 33 months on parenting and on child development. Journal of Developmental and Behavioral Pediatrics 2007; Vol. 28, issue 3:206‐12. [MEDLINE: ] [DOI] [PMC free article] [PubMed]
Miller‐Heyl 1998 {published data only}
- Miller‐Heyl J, MacPhee D, Fritz JJ. DARE to be You: A family‐support, early prevention program. The Journal of Primary Prevention 1998;18(3):257‐85. [Google Scholar]
Mullin 1994 {published data only}
- Mullin E, Quigley K, Glanville B. A controlled evaluation of the impact of a parent training programme on child behaviour and mothers' general wellbeing. Counselling Psychology Quarterly 1994;7(2):167‐79. [Google Scholar]
NCT00183365 {published data only}
- NCT00183365. Effect of family‐based prevention on children of depressed parents. http://clinicaltrials.gov/ct2/show/NCT00183365. Accessed 21 April 2011.
Nixon 2004 {published data only}
Ogden 2008 {published data only}
Olivares 1997 {published data only}
- Olivares J, Rosa AI, Garcia‐Lopez LJ. Video paper on the training of mothers: a comparative study [El papel del video en el entrenamiento a Madres: un estudio comparativo]. Psicologia Conductual 1997;5(2):237‐54. [Google Scholar]
Openden 2005 {published data only}
- Openden DA. Pivotal Response Treatment for Multiple Families of Children with Autism: Probable Efficacy and Effectiveness of a Group Parent Education Workshop. Santa Barbara, CA: University of California, 2005. [Google Scholar]
Orrell‐Valente 1999 {published data only}
- Orrell‐Valente JK, Pinderhughes EE, Valente E, Laird RD. If it's offered, will they come? Influences on parents' participation in a community‐based conduct problems prevention program. American Journal of Community Psychology 1999;27(6):753‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ostergren 2003 {published data only}
- Ostergren CS. Evaluation of a temperament‐based parenting program: factors affecting program usefulness, ease of understanding, preferred amount of materials and parental attitudes. Dissertation Abstracts International 2003; Vol. 64, issue 5:Nov 2003. [MEDLINE: ; 0419‐4209]
Plant 2007 {published data only}
Rahman 2009 {published data only}
Rapee 2005 {published data only}
Reid 2001 {published data only}
- Reid MJ, Webster‐Stratton C, Beauchaine TP. Parent training in head start: a comparison of program response among African American, Asian American, Caucasian, and Hispanic mothers. Prevention Science 2001;2(4):209‐27. [DOI] [PubMed] [Google Scholar]
Reid 2004 {published data only}
Ruffolo 2005 {published data only}
- Ruffolo MC, Kuhn MT, Evans ME. Support, empowerment, and education: a study of multiple family group psychoeducation. Journal of Emotional and Behavioral Disorders 2005; Vol. 13, issue 4:200‐12. [MEDLINE: ]
Sanders 2000 {published data only}
- Sanders MR, Markie‐Dadds C, Tully LA, Bor W. The Triple P‐Positive Parenting Program: a comparison of enhanced, standard, and self‐directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology 2000;68(4):624‐40. [PubMed] [Google Scholar]
Sanford 2003 {published data only}
Sawasdipanich 2010 {published data only}
- Sawasdipanich N, Srisuphan W, Yenbut J, Tiansawad S, Humphreys J. Effects of a cognitive adjustment program for Thai parents. Nursing & Health Sciences 2010;12(3):306‐13. [DOI] [PubMed] [Google Scholar]
Scott 1987 {published data only}
- Scott MJ, Stradling SG. Evaluation of a group programme for parents of problem children. Behavioral Psychotherapy 1987;15(3):224‐39. [Google Scholar]
Scott 2002 {unpublished data only}
- Scott S, Sylva K. The Spokes Project: supporting parents on kids' education. Department of Health Project Funded by the Parenting Initiative (UK) 2002.
Scott 2005 {published data only}
- Scott S. Do parenting programmes for severe child antisocial behaviour work over the longer term, and for whom? One year follow‐up of a multi‐centre controlled trial. Behavioural and Cognitive Psychotherapy 2005; Vol. 33, issue 4:403‐21. [MEDLINE: ; CN‐00605903]
Scott 2009 {published data only}
Sheeber 1994 {published data only}
- Sheeber LB, Johnson JH. Evaluation of a temperament‐focused, parent training program. Journal of Clinical Child Psychology 1994;23(3):249‐59. [Google Scholar]
Shifflett 1999 {published data only}
- Shifflett K, Cummings EM. A program for educating parents about the effects of divorce and conflict on children: an initial evaluation. Family Relations 1999;48(1):79‐89. [Google Scholar]
Singer 1999 {published data only}
- Singer GHS, Marquis J, Powers LK, Blanchard L, Divenere N, Santelli B, et al. A multi‐site evaluation of parent to parent programs for parents of children with disabilities. Journal of Early Intervention 1999;22(3):217‐29. [Google Scholar]
Sonuga‐Barke 2001 {published data only}
- Sonuga‐Barke EJS, Daley D, Thompson M, Laver‐Bradbury C, Weeks A. Parent‐based therapies for preschool attention‐deficit/hyperactivity disorder: A randomized, controlled trial with a community sample. Journal of the American Academy of Child & Adolescent Psychiatry 2001;40(4):402‐8. [DOI] [PubMed] [Google Scholar]
Sonuga‐Barke 2002 {published data only}
- Sonuga‐Barke EJ, Daley D, Thompson M. Does maternal ADHD reduce the effectiveness of parent training for preschool children's ADHD?. Journal of the American Academy of Child & Adolescent Psychiatry 2002;41(6):696‐702. [DOI] [PubMed] [Google Scholar]
Steiman 2005 {published data only}
- Steiman M. Parent training with children with conduct problems: the role of the marital relationship and parental adjustment. Washington, DC: University of Washington, 2005. [MEDLINE: ] [Google Scholar]
St James Roberts 2001 {published data only}
- James‐Roberts I, Sleep J, Morris S, Owen C, Gillham P. Use of a behavioural programme in the first 3 months to prevent infant crying and sleeping problems. Journal of Paediatrics and Child Health 2001;37(3):289‐97. [DOI] [PubMed] [Google Scholar]
Suchman 2004 {published data only}
Suess 2005 {published data only}
- Suess GJ, Kissgen R. STEEP‐an attachment‐ and research‐based early intervention program [STEEP‐ein bindungstheoretisch und empirisch fundiertes Fruhinterventionsprogramm]. Psychologie‐in‐Erziehung‐und‐Unterricht 2005. [MEDLINE: ]
Sutton 1992 {published data only}
- Sutton C. Training parents to manage difficult children: a comparison of methods. Behavioural Psychotherapy 1992;20(2):115‐39. [Google Scholar]
Sutton 1995 {published data only}
- Sutton C. Parent training by telephone: a partial replication. Behavioural and Cognitive Psychotherapy 1995;23(1):1‐24. [Google Scholar]
Thompson 2009 {published data only}
- Thompson MJ, Laver‐Bradbury C, Ayres M, Poidevin E, Mead S, Dodds C, et al. A small‐scale randomized controlled trial of the revised new forest parenting programme for preschoolers with attention deficit hyperactivity disorder. European Child and Adolescent Psychiatry 2009; Vol. 18, issue 10:605‐16. [1018‐8827] [DOI] [PubMed]
Thompson 2010 {published data only}
- Thompson MJJ, Ayres M, Poidevin E, Mead S, Dodds C. A small‐scale randomized controlled trial of the selfhelp version of the new forest parent training programme for children with ADHD. European Child and Adolescent Psychiatry 2010;18:605‐6. [Google Scholar]
Thorell 2009 {published data only}
Tonge 2006 {published data only}
- Tonge B, Brereton A, Kiomall M, MacKinnon A, King N, Rinehart N. Effects on parental mental health of an education and skills training program for parents of young children with autism: a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry 2006; Vol. 45, issue 5:561‐9. [MEDLINE: ; CN‐00564984] [DOI] [PubMed]
Trost 2007 {published data only}
- Trost AS. The Healthy Image Partnership (HIP) parents program: the role of parental involvement in eating disorder prevention (PhD Thesis). Austin, Texas: The University of Texas, 2007. [MEDLINE: ] [Google Scholar]
Turner 2006a {published data only}
- Turner KMT, Sanders MR. Help when it's needed first: a controlled evaluation of brief, preventive behavioral family intervention in a primary care setting. Behavior Therapy 2006;37(2):131‐42. [DOI] [PubMed] [Google Scholar]
Uslu 2006 {published data only}
Van Wyk 1983 {published data only}
- Wyk JD, Eloff ME, Heyns PM. The evaluation of an integrated parent training program. The Journal of Social Psychology 1983;121(2):273‐81. [Google Scholar]
Webster‐Stratton 2001 {published data only}
- Webster‐Stratton C, Reid MJ, Hammond M. Preventing conduct problems, promoting social competence: a parent and teacher training partnership in Head Start. Journal of Clinical Child Psychology 2001;30(3):283‐302. [DOI] [PubMed] [Google Scholar]
Webster‐Stratton 2004 {published data only}
Wheatley 2003 {published data only}
Whitehurst 2008 {published data only}
- Whitehurst DH, O'Keefe SL, Wilson RA. Divorced and separated parents in conflict: results from a true experiment effect of a court mandated parenting education program. Journal of Divorce and Remarriage 2008; Vol. 48, issue 3‐4:127‐44. [MEDLINE: ; 1050‐2556]
Whittingham 2009a {published data only}
Whittingham 2009b {published data only}
- Whittingham K, Sofronoff K, Sheffield J, Sanders MR. Do parental attributions affect treatment outcome in a parenting program? An exploration of the effects of parental attributions in an RCT of Stepping Stones Triple‐P for the ASD population. Research in Autism Spectrum Disorders 2009; Vol. 3, issue 1:129‐44. [1750‐9467]
Wiggins 2009 {published data only}
Wissow 2008 {published data only}
Wolkchik 1993 {published data only}
- Wolkchik SA, West SG, Westover S, Sandler IN, Martin A, Lustig J, et al. The children of divorce parenting intervention: outcome evaluation of an empirically based program. American Journal of Community Psychology 1993;21(3):293‐331. [DOI] [PubMed] [Google Scholar]
Zimmerman 1996 {published data only}
- Zimmerman TS, Jacobsen RB, MacIntyre M, Watson C. Solution‐focused parenting groups: an empirical study. Journal of Systemic Therapies 1996;15(4):12‐25. [Google Scholar]
References to studies awaiting assessment
Bayer 2010 {published data only}
- Bayer JK, Hiscock H, Ukoumunne OC, Scalzo K, Wake M. Three‐year‐old outcomes of a brief universal parenting intervention to prevent behaviour problems: randomised controlled trial. Archives of Disease in Childhood 2010;95:187‐92. [DOI] [PubMed] [Google Scholar]
Bywater 2011 {published data only}
- Bywater T, Hutchings J, Linck P, Whitaker C, Daley D, Yeo S, Edwards R. Incredible Years parent training support for foster carers in Wales: a multi‐centre feasibility study. Child: Care, Health and Development 2011;37(2):233‐43. [DOI] [PubMed] [Google Scholar]
Cefai 2010 {published data only}
- Cefai J, Smith D, Pushak RE. Parenting wisely: parent training via CD‐ROM with an Australian sample. Child & Family Behavior Therapy 2010;32(1):17‐33. [Google Scholar]
Eichelberger 2010 {published data only}
- Eichelberger I, Pluck J, Hanisch C, Hautmann C, Janen N, Dopfner M. Effects of the universal parent training program Triple P on child behavior problems, parenting strategies, and psychological distress. Zeitschrift fur Klinische Psychologie und Psychotherapie 2010;39(1):24‐32. [Google Scholar]
Franz 2007 {published data only}
- Franz M, Gertheinrichs T, Guttgemanns J, Haubold S, Rentsch D, Schafer R. Palme ‐ a structured attachment oriented parental training for depressive single mothers. First results of a controlled randomized intervention study in an urban community. Psychotherapie Psychosomatik Medizinische Psychologie 2007; Vol. 57, issue 2:84‐5. [MEDLINE: ]
Hampel 2010 {published data only}
- Hampel OA, Schaadt AK, Hasmann SE, Petermann F, Holl R, Hasmann R. Evaluation of Stepping Stones Triple P: Interims analysis of the Stepping‐Stones‐SPC‐Multicentric Study. Klinische Paediatrie 2010;222:18‐25. [DOI] [PubMed] [Google Scholar]
Heinrichs 2006 {published data only}
- Heinrichs N Hahlweg K, Bertram H, Kuschel A, Naumann S, Harstick S. The 1‐year efficacy of a parent training in the universal prevention of child‐behavior problems: results from mothers and fathers. Zeitschrift fur Klinische Psychologie und Psychotherapie 2006; Vol. 35, issue 2:82‐96. [MEDLINE: ; CN‐00615242]
- Heinrichs N, Bertram H, Kuschel A, Hahlweh K. Parent recruitment and retention in a universal prevention program for child behaviour and emotional problems: barriers to research and program participation. Prevention Science 2005;6(4):275‐86. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Hahlweg K, Naumann S, Kuschel A, Bertram H, Ständer D. Universal prevention of child behaviour problems with parent training programme: outcomes after three years. [Universelle Prävention kindlicherVerhaltensstörungen mithilfeeiner elternzentrierten MaßnahmeErgebnisse drei Jahre nach Teilnahme]. Zeitschrift für Klinische Psychologie und Psychotherapie 2009;38(2):79‐88. [Google Scholar]
Morawska 2011 {published data only}
- Morawska A, Haslam D, Milne D, Sanders MR. Evaluation of a brief parenting discussion group for parents of young children. Journal of Developmental and Behavioral Pediatrics 2011;2:136‐145. [DOI] [PubMed] [Google Scholar]
Naumann 2007 {published data only}
Reedtz 2011 {published data only}
- Reedtz C, Handegård BH, Mørch WT. Promoting positive parenting practices in primary pare: outcomes and mechanisms of change in a randomized controlled risk reduction trial. Scandinavian Journal of Psychology 2011;2:131‐7. [DOI] [PubMed] [Google Scholar]
Sanders 2011 {published data only}
- Sanders MR, Stallman HM, McHale M. Workplace Triple P: a controlled evaluation of a parenting intervention for working parents. Journal of Family Psychology 2011;25(4):581‐90. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NTR1338 {published data only}
- Spijkers W, Jansen D, Meer G, Reijneveld SA. Effectiveness of a parenting programme in a public health setting: a randomised controlled trial of the positive parenting programme (Triple P) level 3 versus care as usual provided by the preventive child healthcare (PCH). BMC Public Health 2010;10:131‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abidin 1983
- Abidin RR. The Parenting Stress Index. Charlottesville, VA: Pediatric Psychology Press, 1983. [Google Scholar]
Barlow 2010
- Barlow J, Smailagic N, Ferriter M, Bennett C, Jones H. Group‐based parent training programmes for improving emotional and behavioural adjustment in children from birth to three years old. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD003680] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barlow 2011
- Barlow J, Smailagic N, Bennett C, Huband N, Jones H, Coren E. Individual and group based parenting programmes for improving psychosocial outcomes for teenage parents and their children. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD002964] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beardslee 1998
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archive of General Psychiatry 1961;4(6):561‐71. [DOI] [PubMed] [Google Scholar]
Beck 1988
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1988;56:893‐7. [DOI] [PubMed] [Google Scholar]
Beebe 2011
- Beebe B, Steele M, Jaffe J, Buck KA, Chen H, Cohen P, et al. Maternal anxiety symptoms and mother‐infant self‐ and interactive contingency. Infant Mental Health Journal 2011;32(2):174‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cornish 2008
- Cornish AM, McMahon C, Ungerer JA. Postnatal depression and the quality of mother‐infant interactions during the second year of life. Australian Journal of Psychology 2008;60(3):142‐51. [Google Scholar]
Dawson 1997
- Dawson G, Frey K, Panagiotides H, Osterling J, HessI D. Infants of depressed mothers exhibit atypical frontal brain activity: a replication and extension of previous findings. Journal of Child Psychology and Psychiatry 1997;38(2):179‐86. [DOI] [PubMed] [Google Scholar]
Department of Health 2009
- Shribman S, Billingham K. Healthy Child Programme: Pregnancy and the First Five Years of Life. London: Department of Health, 2009. [Google Scholar]
Dretze 2005
- Dretzke J, Frew E, Davenport C, Barlow J, Stewart‐Brown S, Sandercock J, et al. The effectiveness and cost‐effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children. Health Technology Assessment 2005;9(50):1‐233. [DOI] [PubMed] [Google Scholar]
Fonagy 1997
- Fonagy P, Target M. Attachment and reflective function: their role in self‐organization. Development and Psychopathology 1997;9:679‐700. [DOI] [PubMed] [Google Scholar]
Grienenberger 2005
- Grienenberger J, Kelly K, Slade A. Maternal reflective functioning, mother‐infant affective communication and infant attachment: exploring the link between mental states and observed caregiving behavior in the intergenerational transmission of attachment. Attachment and Human Development 2005;7(3):299‐311. [DOI] [PubMed] [Google Scholar]
Gunnar 1994
- Gunnar M. Psychoendocrine studies of temperament and stress in early childhood: expanding current models.. In: Bates J, Wachs T editor(s). Temperament: Individual Differences at the Interface of Biology and Behavior. Washington, DC: American Psychological Association, 2003:131. [ISBN: 978‐1‐55798‐222‐3] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Jaffe 2001
- Jaffe J, Beebe B, Feldstein S, Crown CL, Jasnow MD. Rhythms of dialogue in infancy: coordinated timing in development. Monographs of the Society for Research in Child Development 2001;66(2):1‐132. [PubMed] [Google Scholar]
Johnston 1989
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. Journal of Clinical Child Psychology 1989;18:167‐75. [Google Scholar]
Kane 2003
- Kane G, Wood VA, Barlow J. Parenting programmes: a systematic review and synthesis of qualitative research. Child: Care, Health and Development 2003;33(6):784‐93. [DOI] [PubMed] [Google Scholar]
Kane 2004
- Kane P, Garber J. The relations among depression in fathers, children's psychopathology, and father‐child conflict: a meta‐analysis. Clinical Psychology Review 2004;24(3):339‐60. [DOI] [PubMed] [Google Scholar]
Klass 1987
- Klass ET. Situational approach to the assessment of guilt: development and validation of a self‐report measure. Journal of Psychopathology and Behavioral Assessment 1987;9:35‐48. [Google Scholar]
Maiuro 1987
- Maiuro RD, Vitaliano PP, Cahn TS. A brief measure for the assessment of anger and aggression. Journal of Interpersonal Violence 1987;2:166‐78. [Google Scholar]
Martin 2000
- Martin AJ, Linfoot K, Stephenson J. Exploring the cycle of mother‐child relations, maternal confidence and children's aggression. Australian Journal of Psychology 2000;52(1):34‐40. [Google Scholar]
McGuinn 2004
- McGuinn IBL. Adolescents' perceptions of typical inter‐parental conflict and quality of parenting: a path to depression and aggression. New Haven, CT: Yale University, 2003. [Google Scholar]
McMahon 2006
- McMahon CA, Barnett B, Kowalenko NM, Tennant CC. Maternal attachment state of mind moderates the impact of postnatal depression on infant attachment. Journal of Child Psychology and Psychiatry 2006;47(7):660‐9. [DOI] [PubMed] [Google Scholar]
Murray 1992
- Murray L. The Impact of postnatal depression on infant development. Journal of Child Psychology and Psychiatry 1992;33(3):543‐61. [DOI] [PubMed] [Google Scholar]
Murray 1996
- Murray L, Fiori‐Cowley A, Hooper, Cooper P. The impact of postnatal depression and associated adversity on early mother‐infant interactions and later infant outcome. Child Development 1996;67(5):2512‐26. [PubMed] [Google Scholar]
Parry‐Langdon 2008
- Parry‐Langdon N. Three years on: survey of the development and emotional wellbeing of children and young people. London: Office for National Statistics 2008.
Patterson 1992
- Patterson GR, Reid JB, Dishion TJ. Antisocial Boys. Eugene OR: CastaliaPress, 1992. [Google Scholar]
Pawlby 2008
- Pawlby S, Sharpe D, Hay D, O'Keane V. Postnatal depression and child outcome at 11 years: the importance of clinical diagnosis. Journal of Affective Disorders 2008;107:241‐5. [DOI] [PubMed] [Google Scholar]
Ramchandani 2008
- Ramchandani PG, O'Connor TG, Heron J, Murray L, Evans J. The effects of pre and postnatal depression in fathers: a natural experiment comparing the effects of exposure to depression on offspring. Journal of the American Academy of Child and Adolscent Psychiatry 2008;47(4):390‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Rosenberg 1965
- Rosenberg M. Society and the Adolescent Self‐Image. Princeton, NJ: Princeton University Press, 1965. [Google Scholar]
Schore 2005
- Schore AN. Back to basics: attachment, affect regulation, and the developing right brain: linking developmental neuroscience to pediatrics. Pediatrics in Review 2005;26(6):204‐17. [DOI] [PubMed] [Google Scholar]
Sharp 1995
- Sharp D, Hay DF, Pawlby S, Schmücker G, Allen H, Kumar R. The impact of postnatal depression on boys' intellectual development. Journal of Child Psychology and Psychiatry 1995;36(8):1315‐36. [DOI] [PubMed] [Google Scholar]
Shelton 2008
- Shelton K, Harold H, Gordon T. Interparental conflict, negative parenting, and children's adjustment: bridging links between parents' depression and children's psychological distress. Journal of Family Psychology 2008;22(5):712‐24. [DOI] [PubMed] [Google Scholar]
Spanier 1976
- Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family 1976;38:15‐28. [Google Scholar]
Todres 1993
- Todres R, Bunston T. Parent‐education programme evaluation: a review of the literature. Canadian Journal of Community Mental Health 1993;12(1):225‐57. [Google Scholar]
Van IJzendoorn 1995
- Van IJzendoorn. Adult attachment representations, parental responsiveness, and infant attachment: a meta‐analysis on the predictive validity of the adult attachment interview. Psychological Bulletin 1995;117(3):387‐403. [DOI] [PubMed] [Google Scholar]
Waylen 2010
- Waylen A, Stewart‐Brown S. Factors influencing parenting in early childhood: A prospective longitudinal study focusing on change. Child: Care, Health and Development 2010;36:198‐207. [DOI] [PubMed] [Google Scholar]
Wilson 2010
- Wilson SB, Durbin CE. Effects of paternal depression on fathers parenting behaviors: a meta‐analytic review. Clinical Psychology Review 2010;30(2):167‐80. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Barlow 2001
- Barlow J, Coren E. Parent‐training programmes for improving maternal psychosocial health. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD002020] [DOI] [PubMed] [Google Scholar]
Barlow 2003
- Barlow J, Coren E, Stewart‐Brown S. Parent‐training programmes for improving maternal psychosocial health. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD002020.pub2] [DOI] [PubMed] [Google Scholar]


