Abstract
Background:
Returning to work can impact breastfeeding duration; limited data exist on how this may impact a lower income population.
Methods:
Data from U.S. Department of Agriculture’s longitudinal study WIC Infant and Toddler Feeding Practices Study-2 were used to assess breastfeeding duration (<12 versus ≥12 months) by age of the baby when women first returned to work and work status (full time and part time). Multivariable logistic regression was used to determine the association of the timing of return to work, work status, and the combination (timing and work status) with breastfeeding duration.
Results:
Among women who had worked prenatally and initiated breastfeeding, 20.2% breastfed for ≥12 months. Compared to women who did not return to work, fewer women breastfed for ≥12 months if they returned full time or part time (34.1%, 12.0%, and 20.0%, respectively, p < 0.0001). Work status negatively impacted breastfeeding for ≥12 months (full-time adjusted odds ratio [aOR]: 0.24; 95% confidence interval [CI]: 0.13, 0.44 and part-time aOR: 0.51; 95% CI: 0.31, 0.83). Compared to women who did not return, those who returned full time within 3 months or returned part time >1 to 3 months after birth had lower odds of breastfeeding ≥12 months.
Conclusions:
Returning to work within 3 months after birth had a negative impact on breastfeeding for ≥12 months, particularly for those who returned full time. Efforts to support maternity leave and flexible work schedules could prolong breastfeeding durations among a low-income population. This study was a registered study at clinicaltrials.gov (NCT02031978).
Keywords: breastfeeding, employment, returning to work, breastfeeding duration, WIC
Introduction
In 2018, over half (57.1%) of women ≥16 years were in the workforce, and among those women, nearly three-quarters were 20–54 years.1 Approximately two-thirds of women who had their first birth in 2006–2008 worked during pregnancy (56.1% full time and 9.5% part time) and two-thirds of these women were still working less than a month before their child’s birth.2 More than half of women who had worked during pregnancy and had their first birth in 2005–2007 returned to work within 3 months and approximately three-quarters returned within 6 months of birth.2
The American Academy of Pediatrics recommends infants are exclusively breastfed during their first 6 months followed by introduction to complementary foods with continued breastfeeding for at least 12 months and then as long as mom and baby desire.3 However, returning to work, and even the plan to return to work, can impact infant feeding. Mirkovic et al. found that women who planned to go back to work before 12 weeks or those who planned to return full time were less likely to plan to exclusively breastfeed.4 Returning to work also impacted the ability to achieve breastfeeding intentions and breastfeed for longer durations.5,6 While national breastfeeding rates have increased over the past decade,7 disparities remain with infants less likely to be breastfed if they live in households below the poverty level, are enrolled in the U.S. Department of Agriculture’s (USDA) Special Supplemental Nutrition Program for Women, Infants, and Children (WIC*) or are eligible to receive WIC, or are non-Hispanic black.7 Women working in lower income jobs, or those in lower income households, may have less flexibility in their work schedule, may return to work earlier, and are also less likely to breastfeed.8
Research has assessed the impact of returning to work on breastfeeding duration in higher income populations5,9–11; however, limited longitudinal data exist among a lower income population, such as those receiving WIC services. We examined how returning to work among prenatally employed women, including the timing and work status (i.e., full time or part time), was associated with breastfeeding duration in a national sample of low-income women whose infants were enrolled in WIC. Understanding how timing of returning to work and work status impact infant feeding outcomes could help support working women to breastfeed and inform the development of workplace policies and practices that support breastfeeding.
Methods
USDA’s WIC Program began enrolling participants (July 1 through November 18, 2013) for a longitudinal study examining maternal and child feeding practices (WIC Infant and Toddler Feeding Practices Study-2 [ITFPS-2]). The study was designed to provide information on feeding practices and nutrition outcomes among women and children enrolled in WIC through the child’s 6th birthday and has plans to conduct an additional assessment on the child’s 9th birthday.12,13 Sampling was conducted using a two-stage stratified approach as described previously.12 Using a probability proportional to size sample design, sampling occurred within WIC sites projected to enroll ≥30 participants/month, resulting in a total of 80 WIC sites from 27 states that represent 37% of WIC sites and 87% of WIC participants.12
Within the selected sites, all women who were enrolling in WIC for the first time for their current pregnancy or were enrolling their newborn (<2.5 months old) were invited to participate if they were ≥16 years of age and spoke English or Spanish.12 Women completed an in-person screener to determine eligibility. Eligible women then completed followup surveys, which were conducted through telephone once prenatally, and then every other month through their child’s first 13 months. Women provided written informed consent and were provided incentives for enrolling and completing each survey.12
A total of 6,775 women were invited to participate in the study; 987 did not complete a screener, 1,299 were screened and ineligible, and the remaining women (4,489) were screened and eligible to enroll. Of those screened and eligible, 4,367 enrolled (97.3%); 3,398 completed a month 1 interview (77.8%) in which data on prenatal work status were collected.12 Response rates, among those enrolled, ranged from 65.9% to 71.7% for month 3, 7, and 13, in which information on postnatal work status was available.12 Detailed study methodology has been published.12
Analytic sample
We limited our analyses to women who had worked ≥1 month during pregnancy (n = 2,025) as women eligible for this study must have worked at some time during pregnancy. In addition, analyses were restricted to those who had initiated breastfeeding and had breastfeeding duration information (n = 1,555). Women were excluded if they were 16–19 years of age (n = 128) or returned only to school (n = 111) as accommodations for supporting breastfeeding at schools or teenage mothers may differ from those available in the workplace. We excluded women with a birth before 32 weeks of age (n = 19) or those with multiples (n = 14) as breastfeeding practices among these women may differ.14 Finally, we excluded women missing both baby’s age when they first returned and their postnatal work status (n = 51) or women who had two answers on baby’s age when they first returned to work (n = 2). Final sample size was n = 1,230 (weighted n = 163,049).
Breastfeeding duration
Breastfeeding duration was determined by current feeding practices at each survey (breast milk, infant formula, or both). Breastfeeding cessation was determined the first time any breast milk (breast or bottle) was not reported; age of the baby was recorded. Breastfeeding duration was categorized as <12 or ≥12 months.
Employment variables: age of baby when returning to work and work status
In the month 3, 7, or 13 survey, women provided baby’s age when women first started going to school or work (“How old was your child when you started going to school or working?”). Once an answer was provided, this question was no longer asked on future surveys. Baby’s age when women first returned to work was reported as (1) ≤1 month, (2) >1 month and ≤2 months, (3) >2 months and ≤3 months, (4) >3 months, and (5) no age provided and reported not returning to work by 13 months (henceforth, referred to as did not return to work).
Postnatal work status was assessed at month 3, 7, and 13 by asking, “Are you currently working for pay?” with response options of full time (≥35 hours per week), part time, or not at all. The work status at the time a woman first indicated she was currently working full time or part time and provided baby’s age when she returned was used (henceforth, referred to as postnatal work status). A variable combining baby’s age when women first returned and postnatal work status was created and categorized as (1) full time and baby ≤1 month, (2) full time and baby >1 to ≤2 months, (3) full time and baby >2 to ≤3 months, (4) full time and baby >3 months, (5) part time and baby ≤1 month, (6) part time and baby >1 to ≤2 months, (7) part time and baby >2 to ≤3 months, (8) part time and baby >3 months, and (9) did not return to work.
Covariates
Maternal covariates include age at birth (20–25 years or ≥26 years), race/ethnicity (non-Hispanic white, non-Hispanic black or African American [referred to as non-Hispanic black], Hispanic, or women of other race/ethnicities), education status at birth (≤high school or >high school), and breastfeeding history (any or none [defined as either did not have children or did not breastfeed children from previous pregnancies]). Infant characteristics include preterm status (baby born >3 weeks before due date) and type of delivery15 (vaginal or cesarean). Work characteristic includes number of months worked during pregnancy (1–3 months, 4–6 months, or 7–9 months, assessed in the month 1 survey).
Household characteristics include status of mother and father living in the same household at birth (yes or no), poverty level at the time of enrollment (≤75%, 76–130%, and >130% of the 2013 poverty guidelines16), consistent WIC participation during the study (yes/no), and prior WIC participation (yes/no). Current WIC participation was assessed at months 1, 3, 7, and 13. If participants indicated currently receiving WIC for themselves or their child at three or more time points, they were categorized as consistent WIC participation. For those who indicated currently receiving WIC for themselves or their child at two or fewer time points, they were categorized as inconsistent WIC participation. Prior WIC participation was defined as reporting ever receiving WIC benefits before this pregnancy or the birth of this child, assessed either prenatally or at month 1 or 3.
Statistical analyses
Among our analytic population, we describe sociodemographic characteristics by breastfeeding duration status. Differences in proportions were assessed using Chi-square tests (p < 0.05). Differences in proportions of breastfeeding ≥12 months by postnatal work status and corresponding baby’s age when women first returned to work were assessed using a t-test (p < 0.05). Multivariable logistic regression models were done to assess the association of postnatal work status (model 1), the association of baby’s age when women first returned (model 2), and the combined association of postnatal work status and baby’s age when women first returned (model 3) with breastfeeding duration ≥12 months. Odds ratios were adjusted for all covariates.
SPSS Complex Samples version 25.0 (IBM SPSS, Inc., Chicago, IL) was used to account for the study’s complex sample design. Analyses were weighted using the month 1 interview core weight, which adjusts for differential probability of selection and nonresponse. This weight was selected because prenatal employment status was collected in month 1, a criterion for analytic eligibility. Analyses are representative of the WIC population enrolled in WIC sites with ≥30 participants/month. The Centers for Disease Control and Prevention determined that this secondary analysis of de-identified data was not human subjects research and did not require IRB review.
Results
Among women who had worked prenatally and had initiated breastfeeding, 20.2% breastfed for ≥12 months. Table 1 describes the demographic characteristics of the analytic sample by breastfeeding duration. Compared to women who had breastfed for <12 months, a significantly higher proportion of women who had breastfed for ≥12 months were ≥26 years of age at the time of birth (51.5% and 67.2%, respectively, Chi-square p = 0.001). About two-thirds of women who had worked prenatally worked 7–9 months of their pregnancy (breastfed for <12 months: 69.1% and breastfed for ≥12 months: 63.4%). Among women who breastfed for <12 months, 42.9% returned to work full time, 37.6% returned part time, and 19.5% did not return to work within 13 months after birth. Comparatively, among women who breastfed for ≥12 months, 23.1% returned to work full time, 37.2% returned part time, and 39.7% did not return to work within 13 months after birth (breastfed for <12 months versus breastfed for ≥12 months, Chi-square p = 0.0001). Women who breastfed for ≥12 months were more likely to report both mom and dad were living in the same household than women who breastfed for <12 months (69.5% and 54.2%, respectively; Chi-square p = 0.001).
Table 1.
Demographic Characteristics of Prenatally Employed Women and Their Babies Who Are Enrolled in WIC and Initiated Breastfeeding by 12-Month Breastfeeding Duration,a U.S. Department of Agriculture’s WIC Infant and Toddler Feeding Practices Study-2
| Breastfeeding duration <12 months (unweighted n = 1,000)a | Breastfeeding duration ≥12 months (unweighted n = 230)a | Chi-square p-value | |
|---|---|---|---|
|
| |||
| % (95% CI) | |||
| Maternal characteristics | |||
| Age at child’s birth | 0.001 | ||
| 20–25 years | 48.5 (44.3–52.6) | 32.8 (25.3–41.3) | |
| ≥26 years | 51.5 (47.4–55.7) | 67.2 (58.7–74.7) | |
| Race and ethnicity | 0.100 | ||
| Non-Hispanic white | 27.3 (21.5–33.9) | 24.9 (17.4–34.2) | |
| Non-Hispanic black | 20.7 (15.9–26.4) | 15.1 (10.1–21.9) | |
| Hispanic | 47.0 (38.5–55.6) | 51.9 (41.3–62.3) | |
| Other | 5.1 (3.6–7.2) | 8.1 (4.3–14.8) | |
| Education status | 0.119 | ||
| High school or less | 50.9 (45.8–55.9) | 44.1 (36.4–52.1) | |
| More than high school | 49.1 (44.1–54.2) | 55.9 (47.9–63.6) | |
| Breastfeeding history | 0.194 | ||
| No breastfeeding history | 48.6 (44–53.2) | 43.9 (35.8–52.4) | |
| Any breastfeeding history | 51.4 (46.8–56.0) | 56.1 (47.6–64.2) | |
| Infant characteristics | |||
| Term status | 0.507 | ||
| Born >3 weeks before due date | 7.3 (5.6–9.5) | 8.6 (5.3–13.6) | |
| Born <3 weeks before due date | 92.7 (90.5–94.4) | 91.4 (86.4–94.7) | |
| Delivery type | 0.488 | ||
| Vaginal | 63.3 (58.7–67.6) | 66.1 (58.2–73.3) | |
| Caesarean | 36.7 (32.4–41.3) | 33.9 (26.7–41.8) | |
| Work characteristics | |||
| Months worked for pay during pregnancy | 0.337 | ||
| 1–3 months | 15.3 (12.4–18.7) | 17.7 (13.2–23.3) | |
| 4–6 months | 15.6 (12.7–19.2) | 18.9 (13.1–26.4) | |
| 7–9 months | 69.1 (64.1–73.6) | 63.4 (55.4–70.8) | |
| Postnatal work statusb | 0.0001 | ||
| Full time | 42.9 (39.3–46.7) | 23.1 (16.7–31.0) | |
| Part time | 37.6 (34.1–41.2) | 37.2 (29.2–46.0) | |
| Did not return to work | 19.5 (15.9–23.6) | 39.7 (31.8–48.3) | |
| Baby’s age when women first returned to work | 0.0001 | ||
| Baby is ≤1 month old | 9.3 (7.0–12.3) | 6.0 (2.8–12.2) | |
| Baby is >1 to ≤2 months old | 36.0 (32.3–39.8) | 19.0 (14.6–24.4) | |
| Baby is >2 to ≤3 months old | 14.9 (12.5–17.7) | 12.1 (8.7–16.6) | |
| Baby is >3 months old | 20.3 (17.3–23.7) | 23.2 (15.2–33.9) | |
| Did not return to work | 19.5 (15.9–23.6) | 39.7 (31.8–48.3) | |
| Baby’s age when women first returned to work and postnatal work statusb | 0.0001 | ||
| Full time | |||
| Baby is ≤1 month old | 4.6 (3.4–6.3) | 1.2 (0.3–4.1) | |
| Baby is >1 to ≤2 months old | 22.3 (19.3–25.7) | 7.6 (4.8–11.8) | |
| Baby is >2 to ≤3 months old | 7.5 (5.6–9.9) | 6.0 (3.4–10.3) | |
| Baby is >3 months old | 8.5 (6.8–10.5) | 8.3 (4.5–14.8) | |
| Part time | |||
| Baby is ≤1 month old | 4.7 (3.3–6.6) | 4.8 (2.0–10.9) | |
| Baby is >1 to ≤2 months old | 13.6 (10.9–16.9) | 11.4 (7.7–16.6) | |
| Baby is >2 to ≤3 months old | 7.4 (5.6–9.8) | 6.1 (3.6–10.1) | |
| Baby is >3 months old | 11.9 (9.6–14.5) | 14.9 (9.0–23.7) | |
| Did not return to work | 19.5 (15.9–23.6) | 39.7 (31.8–48.3) | |
| Household characteristics | |||
| Mom and Dad living in same household | 0.001 | ||
| Yes | 54.2 (50.0–58.4) | 69.5 (62.3–75.8) | |
| No | 45.8 (41.6–50.0) | 30.5 (24.2–37.7) | |
| Poverty levelc | 0.084 | ||
| ≤75% of poverty guideline | 52.5 (48.3–56.6) | 50.0 (41.4–58.6) | |
| 76–130% of poverty guideline | 35.2 (32.0–38.5) | 31.6 (24.7–39.4) | |
| >130% of poverty guideline | 12.4 (9.6–15.9) | 18.4 (13.3–25.0) | |
| WIC Participationd | 0.056 | ||
| Consistent participation | 81.1 (77.4–84.3) | 88.3 (80.5–93.2) | |
| Inconsistent participation | 18.9 (15.7–22.6) | 11.7 (6.8–19.5) | |
| Prior WIC receipte | 0.288 | ||
| Yes | 56.0 (51.8–60.1) | 60.7 (52.2–68.6) | |
| No | 44.0 (39.9–48.2) | 39.3 (31.4–47.8) | |
Weighted n is 130,079 for breastfeeding duration <12 months and 32,970 for breastfeeding duration ≥12 months.
Reported postnatal work status is the current work status at the time a woman first indicated she was currently working full time or part time and provided baby’s age when she returned. Women were asked current work status at month 3, 7, and 13.
Poverty guideline is defined as the 2013 poverty guidelines.16
WIC participation is defined as currently receiving WIC for themselves or their child at three or more time points at months 1, 3, 7, or 13 (consistent participation) or ≤2 time points (inconsistent participation).
Prior WIC participation is defined as previously receiving WIC benefits before this pregnancy or birth of this child.
CI, confidence interval; USDA, U.S. Department of Agriculture; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Figure 1A and B show the proportion of women who worked prenatally and who breastfed for ≥12 months by postnatal work status (Fig. 1A) and baby’s age when women first returned (Fig. 1B). Compared to women who had not returned to work, a lower proportion of women who returned full time or part time breastfed for ≥12 months (34.1%, 12.0%, and 20.0%, respectively, p < 0.001 for each comparison) (Fig. 1A). A lower proportion of women who returned full time breastfed for ≥12 months compared to those who returned part time (p < 0.002) (Fig. 1A). Compared to women who returned to work >3 months after birth (22.5%), women who returned >1 to ≤2 months after birth were less likely to breastfed for ≥12 months (11.8%; p < 0.05); no difference was observed for those who returned ≤1 month or >2 to ≤3 months after birth (13.9% [p = 0.071] and 17.0% [p = 0.072]; respectively) (Fig. 1B).
FIG. 1.
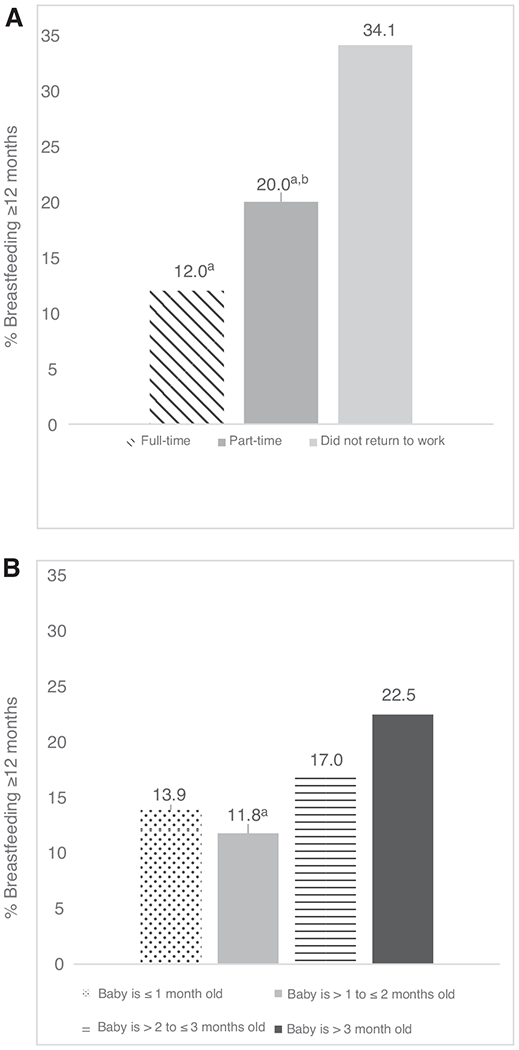
(A) Percentage of prenatally employed women who breastfed ≥12 months by postnatal work status,1 USDA’s WIC ITFPS-2.2 1Reported postnatal work status is the current work status at the time a woman first indicated she was currently working full time or part time and provided baby’s age when she returned. Women were asked current work status at month 3, 7, and 13. 2Unweighted n is full time = 58, part time = 93, and did not return to work = 79; weighted n is full time = 7,611, part time = 12,263, and did not return to work = 13,096. aIndicates results are significantly different from those who did not return to work (t-test, p < 0.05). bIndicates results are significantly different from those who first returned full time (t-test, p < 0.05). (B) Percentage of prenatally employed women who returned to work and breastfed ≥12 months by baby’s age when women first returned to work, USDA’s WIC ITFPS-2.1 1Unweighted n is baby is ≤1 month old = 15, baby is >1 to ≤2 months old = 52, baby is >2 to ≤3 months old = 32, and baby is >3 months old = 52; weighted n is baby is ≤1 month old = 1,963, baby is >1 to ≤2 months old = 6,267, baby is >2 to ≤3 months old = 3,985, and baby is >3 months old = 7,659. aIndicates results are significantly different from those who first returned when baby’s age was >3 months (t-test, p < 0.05). ITFPS-2, Infant and Toddler Feeding Practices Study-2; USDA, U.S. Department of Agriculture; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Figure 2 provides the proportion of women who worked prenatally and who breastfed for ≥12 months by the combination of postnatal work status and baby’s age when women first returned to work. Regardless of work status (full time or part time), there was generally a dose-response relationship between baby’s age when returning to work and breastfeeding for ≥12 months. Compared to women who did not return, a lower proportion breastfed for ≥12 months if they returned to work full time after birth (did not return: 34.1%; full time ≤1 month, >1 to ≤2 months, >2 to ≤3 months, or >3 months: 5.9%, 8.0%, 16.8%, and 20.0%, respectively; p < 0.010) or if they returned part time >1 to ≤2 months or >2 to ≤3 months (17.5% and 17.2%, respectively; p < 0.001).
FIG. 2.
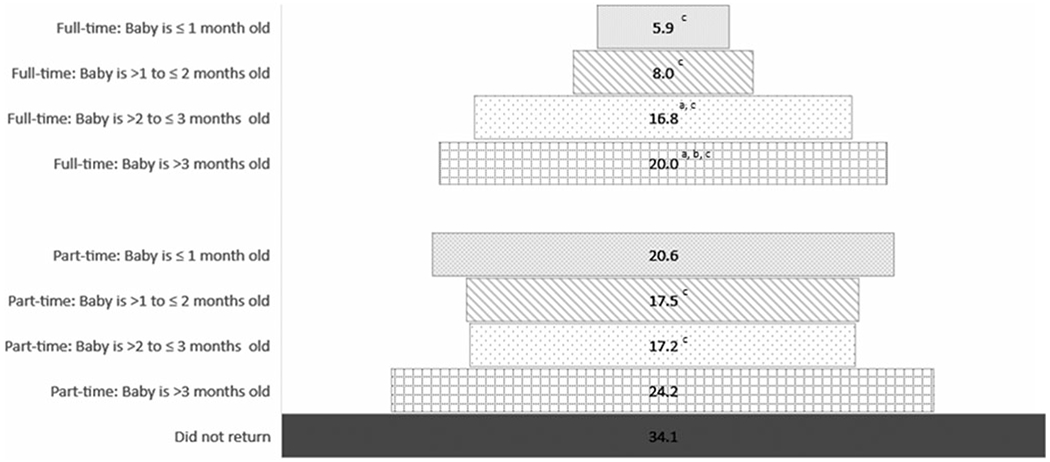
Percentage of prenatally employed women who breastfed ≥12 months by postnatal work status1 and baby’s age when women first returned to work, USDA’s WIC ITFPS-22. 1Reported postnatal work status is the current work status at the time a woman first indicated she was currently working full time or part time and provided baby’s age when she returned. Women were asked current work status at month 3, 7, and 13. 2Unweighted n is full time: baby is ≤1 month old = 3, baby is >1 to ≤2 months old = 22, baby is >2 to ≤3 months old = 13, and baby is >3 months old = 20; weighted n is full time: baby is ≤1 month old = 380, baby is >1 to ≤2 months old = 2,515, baby is >2 to ≤3 months old = 1,971, and baby is >3 months old = 2,744. Unweighted n is part time: baby is ≤1 month old = 12, baby is >1 to ≤2 months old = 30, baby is >2 to ≤3 months old = 19, and baby is >3 months old = 32; weighted n is part time: baby is ≤1 month old = 1,583, baby is >1 to ≤2 months old = 3,751, baby is >2 to ≤3 months old = 2,014, and baby is >3 months old = 4,915. Unweighted n is did not return = 79; weighted n is did not return = 13,096. aIndicates results are significantly different from those who first returned when baby’s age was ≤1 month within each work status strata. bIndicates results are significantly different from those who first returned when baby’s age was >1 to ≤2 months within each work status strata. cIndicates results are significantly different from those who did not return to work (t-test, p < 0.05). ITFPS-2, Infant and Toddler Feeding Practices Study-2; USDA, U.S. Department of Agriculture’s; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Table 2 shows that compared to women who did not return to work, those who returned either full time or part time had lower odds of breastfeeding for ≥12 months (adjusted odds ratio [aOR]: 0.24; 95% confidence interval [CI]: 0.13 and 0.44; aOR: 0.51; 95% CI: 0.31 and 0.83; respectively) (model 1). Compared to women who returned part time, those who returned full time had lower odds of breastfeeding for ≥12 months (aOR: 0.47; 95% CI: 0.28 and 0.80) (data not shown). Model 2 indicates that compared to those who did not return to work, women who returned within 3 months after birth had significantly lower odds of breastfeeding ≥12 months. However, this difference was not seen among women returning >3 months after birth. Women who returned full time within 3 months after birth had lower odds of breastfeeding ≥12 months compared to those who did not return (aORs: 0.13, 0.15, and 0.28 for ≤1 month, >1 to ≤2 months, and >2 to ≤3 months, respectively), but this association was no longer significant >3 months after birth (Model 3). Among women who returned part time, if they returned ≤1 month or >3 months after birth, there was no statistical difference in the odds of breastfeeding ≥12 months compared to women who had not returned to work. However, those who returned part time >1 to ≤3 months after birth had significantly lower odds of breastfeeding ≥12 months compared to women who had not returned to work.
Table 2.
Among Prenatally Employed Women Who Initiated Breastfeeding, the Association of Baby’s Age When Mothers First Return to Work and Postnatal Work Status with Breastfeeding Duration ≥12 Months, U.S. Department of Agriculture’s WIC Infant and Toddler Feeding Practices Study-2
| Breastfeeding duration ≥12 months |
|||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
|
|
|||
| Adjusteda ORs (95% CIs) | |||
| Postnatal work statusb | |||
| Full time | 0.24 (0.13–0.44) | — | — |
| Part time | 0.51 (0.31–0.83) | — | — |
| Did not return to work | Referent | — | — |
| Baby’s age when women first returned | |||
| ≤1 month | — | 0.33 (0.14–0.82) | — |
| >1 to ≤2 months | — | 0.25 (0.16–0.40) | — |
| >2 to ≤3 months | — | 0.34 (0.22–0.53) | — |
| >3 months | — | 0.54 (0.26–1.12) | — |
| Did not return to work | — | Referent | — |
| Baby’s age when women first returned and postnatal work statusb | |||
| Full time | |||
| Baby is ≤1 month old | — | — | 0.13 (0.04–0.47) |
| Baby is >1 to ≤2 months old | — | — | 0.15 (0.07–0.33) |
| Baby is >2 to ≤3 months old | — | — | 0.28 (0.14–0.58) |
| Baby is >3 months old | — | — | 0.43 (0.18–1.04) |
| Part time | — | — | |
| Baby is ≤1 month old | — | — | 0.52 (0.19–1.42) |
| Baby is >1 to ≤2 months old | — | — | 0.41 (0.24–0.70) |
| Baby is >2 to ≤3 months old | — | — | 0.42 (0.22–0.79) |
| Baby is >3 months old | — | — | 0.62 (0.29–1.33) |
| Did not return to work | Referent | ||
Bold font indicates statistical significance.
Models are adjusted for maternal age at birth, maternal race and ethnicity, maternal education status, breastfeeding history, preterm status, delivery type, number of months worked for pay during pregnancy, mom and dad living in same household, poverty level, consistent WIC participation during the study period, and prior WIC participation.
Reported postnatal work status is the current work status at the time a woman first indicated she was currently working full time or part time and provided baby’s age when she returned. Women were asked current work status at month 3, 7, and 13.
OR, odds ratio; USDA, U.S. Department of Agriculture; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Discussion
We found both postnatal work status and baby’s age when women first returned were associated with breastfeeding duration ≥12 months among a lower income population of prenatally employed women, who initiated breastfeeding. In general, prenatally employed women who returned to work within 3 months after birth were less likely to breastfeed for ≥12 months. For women who returned full time within 3 months after birth, this finding was striking. For women who returned part time, a u-shaped relationship was observed with baby’s age when women first returned.
The timing of returning to work after birth is often determined by the availability of leave, both paid and unpaid. The Family and Medical Leave Act is a federal law requiring employers to allow for unpaid leave up to 12 weeks to care for a newborn or family member with a serious illness and ensures the return to a job with the same terms and conditions before taking leave.17 While this law provides important benefits, certain requirements† must be met for both the employer and employee.14 The ability to take unpaid leave may depend upon existing financial resources. Qualitative research suggests that having paid time off could alleviate some of the financial stress encountered when combining work and breastfeeding.18,19 Currently, out of 41 high- and middle-income countries, the United States is the only one without nationwide, federal paid maternity leave, paternity leave, or parental leave.20 Strides have been made in providing more families with paid family leave21; however, access to paid leave is not equitably distributed.22 The ability to have and take leave, especially paid leave, can impact breastfeeding outcomes.22–26 While we are unable to assess the access to, or use of, leave (paid or unpaid), our findings support the assertion that returning to work within 3 months after birth can have a negative impact on breastfeeding duration for ≥12 months among a lower income population of prenatally employed women.
Studies assessing the impact of work status, and/or hours worked, have generally found that full-time status and/or increasing hours worked per week has a negative impact on various measures of breastfeeding, including planning to exclusively breastfeed,4 meeting intentions,5 or breastfeeding for specific amounts of time.9,27 For women who return part time, additional flexibilities in work schedule or the ability to have more time at home are possible and could support longer breastfeeding durations. Our findings indicated a negative association of work status on longer breastfeeding durations, regardless of full- or part-time status. However, the finding was weaker for those who returned in a part-time status. Interestingly, when both the timing of returning to work and work status were combined, we found a u-shaped relationship with breastfeeding duration for parttime status. The reasons for this are not entirely clear and may be due to smaller sample sizes and less stable estimates among these groups. Our findings might have varied if we were able to stratify by occupation type (i.e., accommodation or retail services, professional or managerial, education, health care, or leisure and hospitality) as occupation has been shown to differentially impact breastfeeding duration.26,28 However, occupation was not assessed, and we were unable to account for it.
Workplace accommodations, including flexible schedules, allowing for paid breaks to pump, providing a private space that is not a bathroom for women to pump, or allowing babies at work, can support women to breastfeed when returning to work and are associated with increased breastfeeding rates.29–31 However, these accommodations may not be possible, or may be limited, based on occupation type.18,32 In this study, limited data were available on workplace accommodations to support breastfeeding and were only collected among women who reported breastfeeding and working postnatally. While our findings indicate that work status may impact breastfeeding durations, they need to be interpreted with caution, given the potential impact of unaccounted workplace characteristics such as occupation type and availability and use of workplace accommodations for breastfeeding.
This study has several strengths and limitations. This study was prospectively designed, which can minimize the recall bias for both the main exposure and outcome variables. These analyses are generalizable to WIC participants, who speak either English or Spanish, and who are enrolled in WIC sites that enroll ≥30 participants a month. However, results could be different among enrollees from smaller sites such as those in rural areas. Prenatal work status was only assessed in month 1; therefore, we could have missed women who were prenatally employed, but did not complete a month 1 survey. A sensitivity analysis was conducted that removed this criterion (i.e., prenatal employment) and the overall interpretation did not change (data not shown).
The questionnaire responses truncated baby’s age when women first returned at >3 months, reducing the ability to assess impacts at later returns. Postnatal work status was defined as the current work status at month 3, 7, or 13 (whichever of the three survey months women first reported returning to work) and may not be the same work status associated with the age of the baby when women first returned. However, we found limited changes in work status over time. Furthermore, a sensitivity analysis that excluded respondents who reported their first postnatal work status at either month 7 or 13, but reported baby’s age when returning to work as <3 months, did not change observed findings.
Misclassification could have occurred when determining when and if women returned to work. Respondents were included if they had a response on at least one of the three time points work status was assessed. Sensitivity analyses were run (1) among women with responses on all three survey time points and (2) among women with at least two responses on survey time points. Slightly stronger associations were found, and in general, the study’s overall interpretation did not change (data not shown). Therefore, our results include women with up to two missing responses. No information was available on the access to or use of leave, occupation type, or worksite accommodations. Finally, we do not address whether or not infants were in childcare and the associated breastfeeding policies and practices they experienced, which have been shown to impact breastfeeding duration.33
Conclusion
Among a sample of women and children enrolled in US-DA’s WIC ITFPS-2, we found that for women who were prenatally employed, returning to work within 3 months after birth had a negative association with breastfeeding for ≥12 months. This was particularly apparent among women who returned to work full time. Efforts to support access to and use of breastfeeding supportive leave policies, flexible work status options, and workplace accommodations may have positive impacts on longer breastfeeding durations among a low-income population.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Footnotes
US Department of Agriculture’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a federal program designed to support low-income (i.e., between 100% and185% of the federal poverty level; or participate in specific federal programs such as Medicaid) pregnant, breastfeeding, and non-breastfeeding women and infants and children with supplemental foods, health education, and health care referrals. Reference: US Department of Agriculture. WIC eligibility requirements. https://www.fns.usda.gov/wic/wic-eligibility-requirements. Published 2020. Accessed September 26, 2020.
According to the US Department of Labor, covered employers include a private sector employer with ≥50 employees in ≥20 weeks in the current or previous calendar year; a public agency, including a local, state, or Federal government agency, regardless of the number of employees it employs; or a public or private elementary or secondary school, regardless of the number of employees it employs. Eligible employees include those who work for a covered employer, have worked for at least 12 months, have at least 1,250 hours of service with such employer during the 12-month period preceding the leave, and work at a location where the employer has at least 50 employees within 75 miles. Reference: U.S. Department of Labor. (2012). Fact Sheet #28: The Family Medical Leave Act. Retrieved from https://www.dol.gov/sites/dolgov/files/WHD/legacy/files/whdfs28.pdf.
Disclosure Statement
No competing financial interests exist.
References
- 1.US Bureau of Labor Statistics. Women in the labor force: A databook (pgs. 1–149; Table 1 on pgs. 6–8). Report 1084. Available at https://www.bls.gov/opub/reports/womens-databook/2019/ (accessed September 20, 2019).
- 2.Laughlin L. Maternity leave and employment patterns of first-time mothers: 1961–2008 (Table 1 on pg. 4; Table 2 on pg. 5, and Table 8 on pg. 14). Current Population Report. Available at https://www.census.gov/content/census/en/library/publications/2011/demo/p70–128.html (accessed September 20, 2019).
- 3.Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–e841. [DOI] [PubMed] [Google Scholar]
- 4.Mirkovic KR, Perrine CG, Scanlon KS, et al. In the United States, a mother’s plans for infant feeding are associated with her plans for employment. J Hum Lact 2014;30:292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirkovic KR, Perrine CG, Scanlon KS, et al. Maternity leave duration and full-time/part-time work status are associated with US mother’s ability to meet breastfeeding intentions. J Hum Lact 2014;30:416–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogbuanu C, Glover S, Probst J, et al. The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics 2011;127:e1414–e1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Breastfeeding among U.S. children born 2009–2017, CDC National Immunization Survey. Results: Breastfeeding. Available at https://www.cdc.gov/breastfeeding/data/nis_data/results.html (accessed September 26, 2019).
- 8.Kimbro RT. On-the-job moms: Work and breastfeeding initiation and duration for a sample of low-income women. Matern Child Health J 2006;10:19–26. [DOI] [PubMed] [Google Scholar]
- 9.Xiang N, Zadoroznyj M, Tomaszewski W, et al. Timing of return to work and breastfeeding in Australia. Pediatrics 2016;137:e20153883. [DOI] [PubMed] [Google Scholar]
- 10.Skafida V. Juggling work and motherhood: The impact of employment and maternity leave on breastfeeding duration: A survival analysis on Growing Up in Scotland data. Matern Child Health J 2012;16:519–527. [DOI] [PubMed] [Google Scholar]
- 11.Castetbon K, Boudet-Berquier J, Salanave B. Combining breastfeeding and work: Findings from the Epifane population-based birth cohort. BMC Pregnancy Childbirth 2020;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.May L, Borger C, Weinfield N, et al. WIC Infant and Toddler Feeding Practices Study-2: Infant Year Report. Alexandria, VA: Prepared by Westat, 2017. [Google Scholar]
- 13.US Department of Agriculture Food and Nutrition Service. Agency Information Collection Activities: Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Infant and Toddler Feeding Practices Study-2 (WIC ITFPS-2) Year 9 Extension. Vol 86: Federal Register; 2021:23914. [Google Scholar]
- 14.Chiang KV, Sharma AS, Nelson JN, et al. Receipt of breast milk by gestational age- United States 2017. MMWR 2019;68:489–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hobbs AJ, Mannion CA, McDonald SW, et al. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth 2016;16:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Health and Human Services. Annual update of the HHS Poverty Guidelines. Fed Regist 2013;78:5182–5183. [Google Scholar]
- 17.Family and Medical Leave Act of 1993, 29U.S.C, §2601–2654. [Google Scholar]
- 18.Rojjanasrirat W, Sousa VD. Perceptions of breastfeeding and planned return to work or school among low-income pregnant women in the USA. J Clin Nurs 2010;19:2014–2022. [DOI] [PubMed] [Google Scholar]
- 19.Johnson AM, Kirk R, Muzik M. Overcoming workplace barriers: A focus group study exploring African American mother’s needs for workplace breastfeeding support. J Hum Lact 2015;31:425–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chzhen Y, Gromada A, Rees G. Are the World’s Richest Countries Family Friendly? Policy in the OECD and EU. Florence, Italy: UNICEF Office of Research, 2019. [Google Scholar]
- 21.National Defense Reauthorization Act for Fiscal Year 2020. https://www.congress.gov/bill/116th-congress/senate-bill/1790 (accessed February 19, 2021).
- 22.Mirkovic KR, Perrine CG, Scanlon KS. Paid maternity leave and breastfeeding outcomes. Birth 2016;43:233–239. [DOI] [PubMed] [Google Scholar]
- 23.Sayres Van Niel MS, Bhatia R, Riano NS, et al. The impact of paid maternity leave on the mental and physical health of mothers and children: A review of the literature and policy implications. Harvard Rev Psychiatry 2020;28:113–126. [DOI] [PubMed] [Google Scholar]
- 24.Navarro-Rosenblatt D, Garmendia ML. Maternity leave and its impact on breastfeeding: A review of the literature. Breastfeed Med 2018;13:589–597. [DOI] [PubMed] [Google Scholar]
- 25.Dagher RK, McGovern PM, Schold JD, et al. Determinants of breastfeeding initiation and cessation among employed mothers: A prospective cohort study. BMC Pregnancy Childbirth 2016;16:194–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guendelman S, Kosa JL, Pearl M, et al. Juggling work and breastfeeding: Effects of maternity leave and occupational characteristics. Pediatrics 2009;123:e38–e46. [DOI] [PubMed] [Google Scholar]
- 27.Mandal B, Roe BE, Fein SB. The differential effects of full-time and part-time work status on breastfeeding. Health Policy 2010;97:79–86. [DOI] [PubMed] [Google Scholar]
- 28.Lauer EA, Armenti K, Henning M, et al. Identifying barriers and supports to breastfeeding in the workplace experienced by mothers in the New Hampshire Special Supplemental Nutrition Program for Women, Infants, and Children utilizing the Total Worker Health framework. Int J Environ Res Public Health 2019;16:529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barraza L, Lebedevitch C, Stuebe A. The Role of Law and Policy in Assisting Families to Reach Healthy People’s Maternal, Infant, and Child Health Breastfeeding Goals in the United States. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, 2020. [DOI] [PubMed] [Google Scholar]
- 30.Smith-Gagen J, Hollen R, Tashiro S, et al. The association of state law to breastfeeding practices in the US. Matern Child Health J 2014;18:2034–2043. [DOI] [PubMed] [Google Scholar]
- 31.Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues 2016;26:6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schindler-Ruswich J, Roess A, Robert RC, et al. Limitations of workplace lactation support: The case for DC WIC recipients. J Hum Lact 2020;36:59–63. [DOI] [PubMed] [Google Scholar]
- 33.Batan M, Li R, Scanlon KS. Association of child care providers breastfeeding support with breastfeeding duration at 6 months. Matern Child Health J 2013;17:708–713. [DOI] [PubMed] [Google Scholar]


