Abstract
Introduction
Pulmonary embolism (PE) is a significant global cause of mortality, ranking third after myocardial infarction and stroke. ECG findings may play a valuable role in the prognostication of patients with PE, with various ECG abnormalities proving to be reasonable predictors of haemodynamic decompensation, cardiogenic shock, and even mortality. This study aims to assess the value of electrocardiography in predicting inpatient mortality in patients with acute pulmonary embolism, as diagnosed with computed tomography pulmonary angiogram.
Method
This study was a cross sectional analysis based at Tygerberg Hospital, Cape Town, South Africa. Eligible patients were identified from all CT-PA performed between 1 January 2017 and 31 December 2019 (2 years). The ECGs were independently screened by two blinded emergency physicians for predetermined signs that are associated with right heart strain and higher pulmonary artery pressures, and these findings were analysed to in-hospital mortality.
Results
Of the included 81 patients, 61 (75 %) were female. Of the 41 (51 %) patients with submassive PE and 8 (10 %) with massive PE, 7 (17 %) and 3 (38 %) suffered inpatient mortality (p = 0.023) respectively. Univariate ECG analysis revealed that complete right bundle branch block (OR, 8.6; 95 % CI, 1.1 to 69.9; p = 0.044) and right axis deviation (OR, 5.6; 95 % CI, 1.4 to 22.4; p = 0.015) were significant predictors of inpatient mortality.
Conclusion
Early identification of patients with pulmonary embolism at higher risk of clinical deterioration and in-patient mortality remains a challenge. Even though no clinical finding or prediction tool in isolation can reliably predict outcomes in patients with pulmonary embolism, this study demonstrated two ECG findings at presentation that were associated with a higher likelihood of inpatient mortality. This single-centre observational study with a small sample precludes concrete conclusions and a large follow-up multi-centre study is advised.
Keywords: Pulmonary embolism, ECG/electrocardiography, Mortality, Emergency centre, LMIC
African Relevance
-
•
The burden of pulmonary embolism is increasing in low- and middle-income countries, likely because of the pro-thrombotic state of the prevalent HIV/TB co-infection.
-
•
Prognosticating pulmonary embolism is complex, especially in those patients where lysis or surgery is not indicated initially.
-
•
ECG is cheap, reasonably available, and easy to perform, and the findings in pulmonary embolism are dynamic and correlate with the degree of right heart strain.
-
•
Clinical predictors of deterioration, especially in patients with a submassive PE, may indicate that the benefits of closer monitoring or even lysis/surgery outweigh the risk.
Introduction
Pulmonary embolism represents the third leading cause of mortality globally after myocardial infarction with an overall mortality of 30 % [1] The burden of disability-adjusted life years from thromboembolism is significantly higher in low- and middle-income countries (LMICs) compared to high-income countries (HICs) [2]. The pro-thrombotic state associated with HIV and TB likely contributes to the higher incidence of PE in LMICs [3], [4], [5].
PE is classified into different categories based on the presence or absence of hypoperfusion/shock and right ventricular dysfunction (RVD), allowing for tailored medical and interventional therapies [6]. However, patients with submassive PE (haemodynamically stable but with RVD) are particularly at risk, as their condition can rapidly deteriorate, leading to overt right ventricular failure and death [7]. Clot burden on computed tomography (CT) scan poorly predicts adverse outcomes, but rather the physiological changes to the right ventricle as seen on CT scan or ultrasound [6].
Electrocardiographic (ECG) findings have shown potential in predicting the prognosis of patients with PE, including haemodynamic decompensation, cardiogenic shock, and mortality [8]. Certain ECG abnormalities such as precordial T-wave inversion (TWI) and the presence of a Qr pattern in V1, have been associated with poor outcomes and increased mortality rates [9]
Reliably predicting clinical deterioration or mortality in patients with acute PE would enable the identification of individuals who will require closer monitoring and may benefit from thrombolysis or thrombectomy procedures, specifically in the submassive category. This study aims to evaluate the value of electrocardiography in predicting inpatient mortality in patients with acute pulmonary embolism.
Methods
This study was a cross sectional analysis that received ethical approval from the University of Cape Town Human Research Ethics Committee (HREC Ref: 722/2020).
This study was conducted at Tygerberg Hospital, a tertiary level hospital in Cape Town, South Africa. Patients with suspected PE were risk stratified according to their pre-test probabilities [10].
All adult patients (≥12 years old) with a confirmed PE as diagnosed by a radiologist reported CT scan during the study period of 3 years (1st of January 2017–31st of December 2019) were eligible for inclusion. Patients with missing or incomplete data, septic emboli, and chronic PE, were excluded. Convenience sampling included only diagnosis via CT scans as the proportion of diagnosis via scintigraphy were negligible and would have complicated data collection.
Data were collected in three phases. First, eligible cases were collated from the Picture Archiving and Communication System (PACS) database by exporting all CT-PA studies performed and reported on by a radiologist during the study period. CT outcome was then dichotomised as either positive or negative for pulmonary embolism. Phase 2 entailed the extraction of all clinical information, including all ECGs done at the time of diagnosis, and the demographic details of all CT-PA positive patient from the Enterprise Content Manager (ECM) database. Two emergency physicians, blinded to the clinical history, PE classification, and patient outcomes, independently analysed all ECGs in phase 3. ECGs were assessed for the presence or absence of pre-determined characteristics [9,11]. The definitions and measurements of ECG characteristics were standardised by the researchers prior to the initiation of phase 3 to minimise information bias (supplementary table). The only disagreements were due to differences in measurements, and this was resolved by consultation and joint remeasurement.
Categorical data were presented as frequencies and proportions (%) and continuous variables as median and inter- quantile ranges. Categorical data were assessed for non-random associations with the use of the Chi2 test. Continuous variables were assessed for significant differences with the Mann-Whitney U test. The prognostic value of electrocardiography to predict inpatient mortality was assessed univariately by calculating diagnostic odds ratios and p-values. Data were analysed with the help of IBM SPSS Statistics version 27 and statistical significance was defined as p < 0.05.
Results
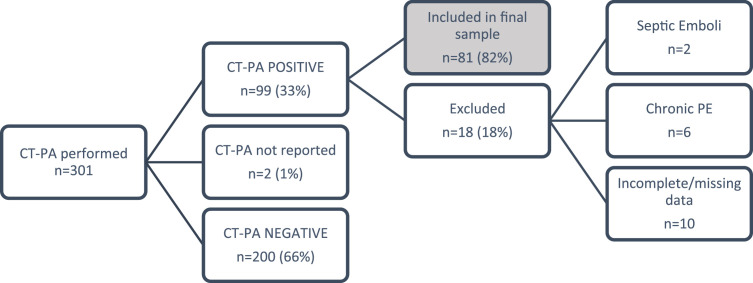
During the 36 month study period, 301 patients received a CT-PA for a suspected PE, of which 99 (33 %) were positive. Eighty-one (82 %) patients were included in the final sample (Fig. 1).
Fig. 1.
Flow of participants.
The median age of the sample was 43 years (Table 1), with a female preponderance (n = 61, 75 %). Ten (12 %) patients suffered inpatient mortality, of which nine (90 %) were females. The most prevalent co-morbidities included hypertension (n = 33, 41 %), HIV/AIDS (n = 24, 30 %), and cardiac failure (n = 10, 12 %). Risk factors for the development of a PE were similarly distributed between the two groups. There were no significant differences between the vital signs on presentation between the two groups: median systolic BP 116 vs 120 mmHg, p = 0.636; median diastolic BP 72 vs. 77 mmHg, p = 0.351; median HR 108 vs 110 bpm, p = 0.874 and SpO2 94% vs 95 %, p = 0.203.
Table 1.
Patient demographics and clinical characteristics for each patient outcome (n = 81).
 |
⁎ GP, general practitioner; WCRC, Western Cape Rehabilitation Centre; COPD, DVT, deep vein thrombosis; POCUS, point-of-care ultrasonography.
Statistically significant different variables are highlighted; Gender were self-reported; Percentages may not add to 100 % because of rounding.
Of the 41 (51 %) patients with submassive PE and eight (10 %) with massive PE, seven (17 %) and three (38 %) suffered inpatient mortality (p = 0.023) respectively. Two out of the seven (9 %) patients who received thrombolysis died and of the three patients who had embolectomies, all survived to hospital discharge. The cause of death was attributed to the PE in all non-survivors and no complications of thrombolysis were described.
Two emergency physicians assessed all ECGs individually (n = 81). Tachycardia (HR ≥100/minute) was the most common ECG feature (n = 59, 73 %) and the most sensitive (90 %) predictor of in-hospital death. Complete right bundle branch block (RBBB) and incomplete RBBB were the most specific predictors of in-hospital death, with a specificity of 97 % and 92 % respectively. TWI in leads V1-V4 (82 %), TWI in II (86 %), Q-wave in AvF (89 %) were reasonably specific changes that predicted in-hospital mortality. Unadjusted diagnostic odds ratios (OR) of ECG characteristics to predict in-hospital mortality (Table 2) found a complete RBBB (OR, 8.6; 95 % CI, 1.1 to 69.9; p = 0.044) and right axis deviation (RAD) (OR, 5.6; 95 % CI, 1.4 to 22.4; p = 0.015) to be significant predictors of in-hospital mortality.
Table 2.
Univariate analysis of ECG characteristics to predict in-hospital mortality.
 |
⁎ bpm, beats per minute.
Statistically significant values highlighted.
Discussion
Despite the high mortality and prevalence of PE in LMICs, predicting rapid clinical deterioration and death remains challenging. Limited availability of resources to diagnose and monitor RVD, as well as the lack of validated clinical decision and prediction rules in high HIV/TB settings, contribute to this difficulty. Nevertheless, this study, despite its small sample size, identified two ECG characteristics associated with a higher likelihood of inpatient mortality.
This study identified two ECG characteristics that were associated with an increased inpatient mortality: RAD and a complete RBBB with a 5.6- and 1.2-times higher odds respectively, in patients who did not survive to hospital discharge. However, the small sample size and low number of non-survivors resulted in wide confidence intervals. Sinus tachycardia was the most common and sensitive, while complete and incomplete RBBB were the most specific predictors of fatality. Although not statistically significant, TWI in V1-V4, TWI in lead II, and Q-wave in AvF were reasonably specific in predicting in-hospital death. A systemic review and meta-analysis conducted by Qaddoura et al. [12] found several ECG features predictive of in-hospital death, including S1Q3T3, complete RBBB, TWI, ST-depression in V4-V6, ST-elevation in V1 and lead III, Qr in V1, RAD, AF, and RV transmural ischaemic pattern. These ECG changes reflect RVD in patients with large clot load and have been shown to predict a poorer outcome when present [13]. Therefore, patients presenting with a suspected PE with any of these signs, may require more intensive monitoring and management. Clinical decision rules to predict outcomes often incorporate CT scan findings or point of care ultrasound findings, lowering their utility in LMICs where access to these modalities is limited [14].
The limited sample size reduced the likelihood of identifying significant findings and prevented robust multivariate regression analysis. The sampling strategy excluded younger patients and those who received lung scintigraphy, potentially introducing selection bias. All-cause mortality as the outcome measure requires a thorough analysis of confounders, yet confounders during hospital admission were not assessed (including the effect of conditions that contribute to chronic right heart strain). Future research should collect prospective data from multiple facilities and explore clinical outcomes in cases where clinical deterioration or death can be reliably predicted.
Conclusion
Identifying high-risk patients with pulmonary embolism and predicting their clinical deterioration and in-patient mortality is challenging. Although the sample size was small, this study suggests that complete RBBB and RAD may serve as predictors of mortality in pulmonary embolism patients. While no single finding or prediction tool can reliably determine outcomes, ECG findings hold promise. Due to the limitations of this single-centre observational study and small sample, further large-scale multi-centre research is recommended for conclusive results.
Dissemination of results
The findings of this study were presented at the Division of Emergency Medicine Cape Town, and at various forums to local emergency medicine clinicians.
Author contributions
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: NR 50 %, CH 35 %, SL 15 %. All authors approved the version to be published and agreed to be accountable for all aspects of work.
Declaration of competing interest
The authors declared no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.afjem.2024.01.004.
Appendix. Supplementary materials
References
- 1.Cugno M., Depetri F., Gnocchi L., Porro F., Bucciarelli P. Validation of the predictive model of the european society of cardiology for early mortality in acute pulmonary embolism. TH Open. 2018;2(3):e265–ee71. doi: 10.1055/s-0038-1669427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wendelboe A.M., Raskob G.E. Global burden of thrombosis: epidemiologic aspects. Circ Res. 2016;118(9):1340–1347. doi: 10.1161/CIRCRESAHA.115.306841. [DOI] [PubMed] [Google Scholar]
- 3.Mampuya F.K., Steinberg W.J., Raubenheimer J.E. Risk factors and HIV infection among patients diagnosed with deep vein thrombosis at a regional/tertiary hospital in Kimberley, South Africa. S Afr Fam Pract. 2018;60(4):107–113. [Google Scholar]
- 4.Bulajic B., Welzel T., Vallabh K. Clinical presentation and diagnostic work up of suspected pulmonary embolism in a district hospital emergency centre serving a high HIV/TB burden population. Afr J Emerg Med. 2019;9(3):134–139. doi: 10.1016/j.afjem.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meel S., Peter A., Menezes C. The clinical features and management of pulmonary embolism at Chris Hani baragwanath academic hospital. Afr J Thorac Crit Care Med. 2018;24(3):113–117. doi: 10.7196/AJTCCM.2018.v24i3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaff M.R., McMurtry M.S., Archer S.L., Cushman M., Goldenberg N., Goldhaber S.Z., et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American heart association. Circulation. 2011;123(16):1788–1830. doi: 10.1161/CIR.0b013e318214914f. [DOI] [PubMed] [Google Scholar]
- 7.Mohan B., Tandon R., Bansal R., Singh M., Singh B., Goyal A., et al. Determinants of in-hospital clinical outcome in patients with sub-massive pulmonary embolism. Indian Heart J. 2018;70:S90–SS5. doi: 10.1016/j.ihj.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Co I., Eilbert W., Chiganos T. New electrocardiographic changes in patients diagnosed with pulmonary embolism. J Emerg Med. 2017;52(3):280–285. doi: 10.1016/j.jemermed.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Choi B.Y., Park D.G. Normalization of negative T-Wave on electrocardiography and right ventricular dysfunction in patients with an acute pulmonary embolism. Korean J Intern Med. 2012;27(1):53–59. doi: 10.3904/kjim.2012.27.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fedullo P.F., Tapson V.F. The evaluation of suspected pulmonary embolism. N Engl J Med. 2003;349(13):1247–1256. doi: 10.1056/NEJMcp035442. [DOI] [PubMed] [Google Scholar]
- 11.Kucher N., Walpoth N., Wustmann K., Noveanu M., Gertsch M. QR in V1-an ECG sign associated with right ventricular strain and adverse clinical outcome in pulmonary embolism. Eur Heart J. 2003;24 doi: 10.1016/s0195-668x(03)00132-5. [DOI] [PubMed] [Google Scholar]
- 12.Qaddoura A., Digby G.C., Kabali C., Kukla P., Zhan Z.Q., Baranchuk A.M. The value of electrocardiography in prognosticating clinical deterioration and mortality in acute pulmonary embolism: a systematic review and meta-analysis. Clin Cardiol. 2017;40(10):814–824. doi: 10.1002/clc.22742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bolt L., Lauber S., Limacher A., Samim D., Lowe A., Tritschler T., et al. Prognostic value of electrocardiography in elderly patients with acute pulmonary embolism. Am J Med. 2019;132(12):e835–ee43. doi: 10.1016/j.amjmed.2019.05.041. [DOI] [PubMed] [Google Scholar]
- 14.Weekes A.J., Raper J.D., Lupez K., Thomas A.M., Cox C.A., Esener D., et al. Development and validation of a prognostic tool: pulmonary embolism short-term clinical outcomes risk estimation (PE-SCORE) PLoS One. 2021;16(11) doi: 10.1371/journal.pone.0260036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.