Abstract
A large number of older people encounter both objective and subjective types of social isolation and sleep disorders. Social isolation increases a person’s risk of a wide range of adverse health outcomes and premature death. Social isolation can cause poor sleep quality that has been proposed as one of the possible mechanisms by which social isolation affects people’s health and quality of life. The present study was conducted to determine the relationship between objective and subjective social isolation with sleep difficulties among older adults. All articles in PubMed, Web of Science, Scopus, Embase, PsycInfo, and Social care online databases published by December 2020 were systematically searched for relevant published articles. Two authors separately checked the acceptability and quality of the studies using the Newcastle Ottawa checklist. Any disagreement was resolved by consulting the third author. According to the inclusion criteria, 11 studies were systematically reviewed, of which five were cross-sectional, and six were longitudinal studies. No meta-analysis was performed due to the high heterogeneity of the studies. Based on the present study results, both objective and subjective social isolation are related to sleep disturbance in older people. This systematic review showed that objective and subjective social isolation are associated with low sleep quality. It is recommended to investigate the causal relationships and possible pathways that affect the studied variables in future studies.
Keywords: Social isolation, Loneliness, Sleep disturbance, Older adults, Systematic review
Introduction
Social isolation is a common complaint in old age with numerous negative consequences on various aspects of health [1]. Although it frequently occurs among different age groups [2], older adults are at a higher risk compared to other age groups [3, 4]. It is predicted that the prevalence of social isolation in older people will increase in the coming years [5, 6]. Moreover, social isolation is a serious risk factor for the health status of older adults [7–9] leading to significant adverse effects on quality of life [10, 11], as well as physical and mental health [7, 12, 13].
Social isolation is divided into objective and subjective types. Objective isolation is the quantifiable and tangible lack of communication and contact with other people or members of an individual's network. In contrast, subjective isolation is the perceived lack of companionship and closeness between individuals and their social network members [14]. While objective isolation has been characterized as the “lack of contact with others due to situational factors, such as the small size of a social network, infrequent social interaction, or lack of participation in social activity”, subjective isolation has been described as the “perceived shortage in one’s social resources, such as companionship or social support” [8]. Both types of social isolation are considered essential components in determining the health status of individuals, and they might be a risk factor for obesity, inactivity, smoking, and high blood pressure [15].
Sleep disturbances are also another common problem with a reported prevalence of over 71% among older adults [16], and they have been assumed to be one of the possible mechanisms by which social isolation affects health conditions [17]. Both types of social isolation can be associated with low sleep quality [18, 19]. According to some evidence, people who live alone have worse sleep quality than those who are not alone, so they repeatedly wake up after falling asleep [20]. Long-term sleep problems have been linked to cardiovascular disease (CVD) risk factors, such as obesity, dyslipidemia, hypertension, diabetes, and metabolic syndrome [21].
With the increase in the number and proportion of older adults globally, the importance of perceiving their regular complaints and the possible relationships have been more emphasized [22]. Although the relationship between objective and subjective social isolation with low sleep quality is reported in older people [23–26], there are some inconsistent results [26, 27] that necessitate a comprehensive systematic review in this regard. Hence, the present study purposed to systematically review the literature on the association between objective and subjective social isolation with sleep disturbances in older adults. It is hoped that the study results would shed some light on reducing the complaints and problems of older adults.
Materials and methods
The review protocol was registered and published on the international Prospective Register of Systematic Reviews (PROSPERO) (registration number: CRD42020163341).
Search strategy
To retrieve the related data published before December 2020, a literature search was conducted on databases, including PubMed, Web of Science, Scopus, Embase, PsycInfo, and Social Care Online using the following keywords separately or in combination: ‘social isolation’, ‘loneliness’, ‘social withdrawal’, ‘social network’, ‘sleep disorder’, ‘sleep disturbance’, ‘sleepless’, ‘insomnia’, ‘sleep quality’, ‘aged people’, ‘older adults’, or ‘older people’. Moreover, the references of retrieved studies were checked to avoid any missing data. Then, to remove the duplicates, all the extracted studies were imported to Endnote X8.
Inclusion criteria
In this systematic review, we included all observational studies investigating the association between social isolation and loneliness (as the independent variables) with low sleep quality (as the dependent variables) in people aged over 60 years.
Exclusion criteria
The exclusion criteria were: different target populations, interventional or review studies, lack of access to the full text of articles, and no response from the authors of the included articles after sending an email.
Study selection
Two authors separately reviewed the titles and abstracts of the articles to find the related studies. If any disagreement arised, it was resolved by the third author's opinion.
Assessment of methodological quality
The quality of cross-sectional and longitudinal studies was assessed separately by two authors using the Newcastle–Ottawa Scale (NOS), which is a tool to evaluate the quality of nonrandomized studies included in a systematic review and/or meta-analyses [28].
In nonrandomized studies, the checklist examines the quality of studies in three parts, including selection (four items, one star for each; maximum stars: four), comparability (one item, one to two star(s) for the item; maximum stars: two), and outcome/exposure (three items, one star for each; maximum stars: three) [28]. Accordingly, the quality of nonrandomized studies was measured as follows:
Good quality: three or four stars in selection domain AND one or two stars in comparability domain AND two or three stars in outcome/exposure domain;
Fair quality: two stars in selection domain AND one or two stars in comparability domain AND two or three stars in outcome/exposure domain;
Poor quality: zero or one star in selection domain OR zero star in comparability domain OR zero or one star in outcome/exposure domain.
Any disagreement between the authors was resolved by seeking the third author's opinion.
Data extraction
Two authors separately extracted the articles’ information, including the first author's name, publication year, study design, country, the number of participants, age, gender percentages, outcomes, instruments, quality score, and results. All the collected information was recorded in a checklist.
Data synthesis
Due to the high heterogeneity of the tools used to measure loneliness, social isolation, and sleep quality in the included studies, we did not conduct a meta-analysis. Out of 11 studies included in this systematic review, only two used the same tools to measure exposure and outcome variables [29, 30].
Results
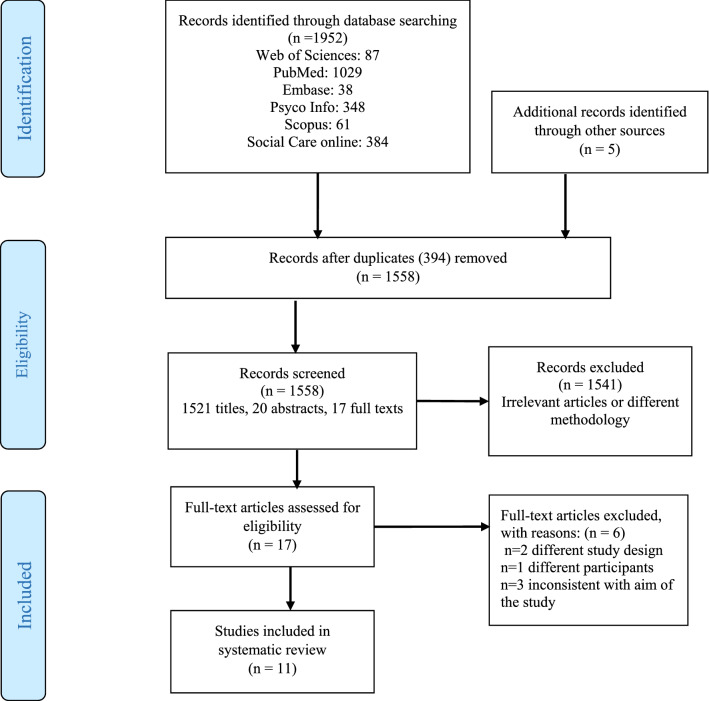
Our search strategy resulted in the retrieval of a total of 1952 papers, 394 of which were removed due to duplication. Then, 1521 titles, 20 abstracts, and 17 full texts were reviewed. After reading the full texts of 17 studies, two articles were eliminated due to different methodologies, three articles due to inconsistency with our study aims, and one article due to differences in the target population. Finally, 11 studies were systematically reviewed (Fig. 1).
Fig. 1.
PRISMA flow diagram
Characteristics of the included studies
Out of 11 papers included in this review study, six were cross-sectional [23, 27, 29–32] and five were longitudinal [24–26, 33, 34] studies. Three studies had been conducted in the United States [23, 27, 34], two in Taiwan [26, 32], and one in Iran [30], the United Kingdom [25], Singapore [33], Ireland [24], China [29], and Malaysia [31].
In the included studies, the number of participants varied from 80 to 5698, average age varied from 65.0 to 86.4 years, and the proportion of females was higher than males. In addition, two studies did not mention the age range, and one study did not mention the gender percentages.
In different studies, various instruments had been used to measure objective and subjective social isolation. The studies examining objective social isolation had used the following tools: the Lubben Social Network Scale (LSNS) in two studies [31, 33]; the Social Disconnectedness Scale in one study[27]; the researcher-made tool consisting of the social network, social structure, and functioning in one study [32]; and social network size in one study [23]. Also, Yu et al. used four items about different social network aspects to assess social isolation [26].
Subjective isolation (feeling lonely) had also been assessed using various tools. Of the eight studies, the 20-item UCLA Loneliness Scale [35] had been used in two studies [29, 30]; the four-item questionnaire [36] consisting of ‘feeling lonely, being cared for, wishing someone for comfort, and wishing for more close friends in one study [23]; the three-item UCLA Loneliness Scale [37] in three studies [25, 27, 34]; items of the Center for Epidemiological Studies Depression scale (CES-D) in one study [26]; and the De Jong Gierveld Loneliness Scale in one study [24].
For analyzing sleep quality, the Pittsburgh Sleep Quality Index (PSQI), including seven components, was used in six studies [23, 24, 26, 29, 30, 32]; the Jenkins Sleep Scale (JSS) in two studies [25, 34]; the CES-D in one study [33]; a self-reported sleep measure in two studies [25, 27]; and a four-item questionnaire in one study [26]. In addition, some studies had used more than one instrument (see Table 1).
Table 1.
Characteristics of included studies
| References | Study design | Country | Sample size | Mean age (years) | Age range (years) | Male % | Female % | Outcome | Assessment method | Quality Score | Quality rating |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jia and Yuan [29] | Cross-sectional | China | 1658 | 70.4 | 60 years and older | 49.3 | 50.7 | Sleep quality |
Loneliness: UCLA Loneliness Scale; Sleep: PSQI |
7 | 75.0 |
| Benson [27] | Cross-sectional | USA | 759 | 72.6 | 62–90 | 56.8 | 53.2 | sleep problems |
Loneliness: UCLA Three-Item Loneliness Scale; Isolation: social disconnectedness scale; Sleep: Self-Reported Sleep Measures and Actigraphy |
6 | 66.6 |
| Shankar [25] | Longitudinal study | UK | 5698 | 65.0 | 50 and older | 44.8 | 55.2 | sleep problems |
Loneliness: UCLA Three-Item Loneliness Scale; Sleep: self-reported sleep measure and JSS |
5 | 55.5 |
| Griffin [34, 41] | Longitudinal study | USA | 5067 | 74.3 | 65–104 | 43.2 | 56.8 | Sleep disturbance |
Loneliness: UCLA Three-Item Loneliness Scale Sleep: a modified version of the JSS |
6 | 66.6 |
| Cho et al. [23] | Cross-sectional | USA | 2541 | 72.6 | 60–103 | 55.5 | 44.5 | Sleep disturbance |
Isolation: Social network size; Loneliness: 4-item questionnaire from (Seeman & Syme, 1987); Sleep: PSQI |
6 | 66.6 |
| Makarem and Naji [30] | Cross-sectional | Iran | 80 | 86.4 | 60 and older | 45.0 | 55.0 | Sleep quality |
Loneliness: UCLA Loneliness Scale Sleep: PSQI |
5 | 55.5 |
| Cheng et al. [33] | Longitudinal study | Singapore | 1417 | 70.0 | 60 and older | Not mentioned | Not mentioned | Sleep disturbance |
Isolation: LSNS; Sleep: The “my sleep was restless” item was extracted from (CES-D) |
6 | 66.6 |
| Yu et al. [26] | Longitudinal study | Taiwan | 1023 | 66.1 | Not mentioned | 56.6 | 53.4 | Sleep quality |
Loneliness: One single item from the CES-D; Isolation: Four items adapted from previous research; Sleep: PSQI |
6 | 66.6 |
| Eshkoor et al. [31] | Cross-sectional | Malaysian | 1210 | Not mentioned | 60 and older | Not mentioned | Not mentioned | Sleep disturbances |
Isolation: LSNS; Sleep: asking 1 question (feel fresh and relax after waking up) |
6 | 66.6 |
| McHugh and Lawlor [24] | Longitudinal study | Ireland | 447 | 73.3 | Not mentioned | 31.0 | 69.0 | Sleep quality |
Loneliness: De Jong Gierveld loneliness Scale; Sleep: PSQI |
7 | 77.7 |
| Yao et al. [32] | Cross-sectional | Taiwan | 187 | 72.1 | 65 and older | 51.3 | 48.7 | Sleep quality |
Social network: using a 6-item questionnaire; Sleep: PSQI |
5 | 55.5 |
UCLA University of California at Los Angeles, PSQI Pittsburgh Sleep Quality Index, LSNS Lubben’s social network scale, JSS Jenkins Sleep Scale, CES-D Center for Epidemiological Studies Depression Scale
Quality of included studies
Regarding the quality of studies, one cross-sectional study had a good quality, three studies had a moderate quality, and one study had a poor quality. Also, among the longitudinal studies, one study had a moderate quality, and other studies had a good quality (see Table 1).
Narrative results
Among the 11 studies included in this review, three studies investigated the relationship between objective social isolation and sleep quality [31–33], five studies addressed the relationship between the feeling of loneliness and sleep quality [24, 25, 29, 30, 34], and three studies examined the association of both objective and subjective social isolation with sleep quality [23, 26, 27]. The results of the included studies were inconsistent in some cases [26, 27].
While the study by Shankar in the UK [25] had the highest number of participants (n=5698), the survey by Makarem and Naji in Iran [30] had the lowest number of participants (n=80).
The relationship between objective social isolation and sleep quality
Three studies addressed the relationship between objective social isolation and sleep disturbances. Eshkoor et al., in a longitudinal study, found that the sleep disruption among respondents without a partner was more than those with a partner (OR 2.21, 95% CI 1.26–3.88). Moreover, sleep problems among isolated people were more than socialized people (OR 1.35, 95% CI 1.06–1.71). Also, they found that being single (OR=2.21) was the most decisive factor in increasing sleep disturbances [31]. In another study, Yao et al. reported a significant relationship between social networking and sleep quality. The study identified significant relationships between a social variable (relationships with relatives/friends) and sleep quality. The regression model showed that relationships with relatives/friends accounted for sleep quality variance [32]. Cheng et al. found that restricted social network was related to more restless sleep and a more depressed mood. Also, poor social relations and sleep disturbances could interact through depression [33].
The relationship between subjective social isolation and sleep quality
Five studies addressed the relationship between subjective social isolation and sleep quality. Two cross-sectional studies conducted in China [29] and Iran [30] showed a significant and inverse relationship between loneliness and PSQI total score (P<0.001). In addition, loneliness was found to be statistically associated with the following components of PSQI: (a) sleep latency, (b) subjective sleep quality, (c) sleep duration, (d) use of sleeping medication, and (e) daytime dysfunction [29]. The interaction between loneliness and sleep disturbances was also investigated in three longitudinal studies [24, 25, 34]. A longitudinal study by McHugh and Lawlor showed that loneliness could predict sleep quality at follow-up, controlling for demographic covariates and sleep quality at baseline. Also, the stress from loneliness mediated the effect of loneliness on sleep quality [24]. Griffin et al. evaluated 5067 participants (≥ 65 years) in three time periods (2006, 2010, and 2014). Their results revealed that high levels of loneliness at baseline were associated with high levels of sleep disturbance at baseline, as well as at 4-year and 8-year follow-up phases. Moreover, sleep disturbance was associated with high levels of loneliness at baseline and follow-up phases. Their study showed a bidirectional relationship between loneliness and sleep disturbance [34]. Another study also reported that baseline loneliness was associated with an increased prevalence of sleep problems (OR 1.30, 95% CI 1.03–1.63) during the 4-year follow-up period. Moreover, there was an association between feeling lonely and sleep disturbance, which significantly reduced sleep duration and led to sleep disturbance [25].
The relationship between objective and subjective social isolation with sleep quality
Among the 11 included studies, three cases evaluated the relationship between objective and subjective social isolation with sleep disturbance. According to Yu et al. [26], sleep quality was inversely associated with loneliness and social isolation in univariate analysis. Social isolation at baseline might be associated with low sleep quality even up to a 6-year follow-up period (P<0.001). Despite the significant relationship between loneliness and sleep quality at baseline (P<0.011), no significant difference was observed during follow-up (P=0.270) [26]. Another longitudinal study showed that objective social isolation and loneliness could be associated with poor sleep quality. According to Benson et al. [27], although loneliness and social isolation were associated with wake after sleep onset (WASO) and percent sleep [total sleep time (TST) divided by the duration of the first to the last epochs scored as sleep], none of them were associated with actigraphy-measured TST. Besides, increased loneliness was strongly associated with more insomnia symptoms and shorter sleep duration; however, this was not true for social isolation. In addition, isolated individuals spent a longer time in bed [27]. Finally, a cross-sectional study showed that objective and subjective social isolation were associated with sleep disturbance. In separate multivariate regression models, subjective social isolation and objective social isolation were associated with sleep disturbance (unadjusted beta 0.27, P<0.001 vs. − 0.12, P<0.001, respectively). These associations remained significant after adjusting for all covariates. Furthermore, isolated people were worse, mostly when people felt lonely [23]. The narrative results of included studies are summarized in Table 2.
Table 2.
Narrative summary of results of included studies
| References | Summary of results |
|---|---|
| Jia and Yuan [29] |
Older adults with higher levels of loneliness had poorer sleep quality Five dimensions of sleep quality, including subjective sleep quality, sleep latency, sleep duration, use of sleeping medication, and daytime dysfunction, were associated with loneliness |
| Benson [27] |
Loneliness and social isolation were associated with WASO and percent sleep (TST divided by the duration of the first to the last epochs scored as sleep). Neither was associated with TST -Sleep calculated duration, the calculated time in bed, and later wake times were significantly associated with social isolation in adjusted models Increased loneliness was strongly associated with more insomnia symptoms, but social isolation was not |
| Shankar [25] | Following adjustment for covariates, baseline loneliness score was associated with an increase in the odds of reporting more sleep problems at follow-up |
| Griffin [34, 41] |
Loneliness and sleep were bidirectionally related. Loneliness is a risk factor for sleep disturbance and vice versa Loneliness and sleep disturbance predicted each other over time, suggesting reciprocal causality between loneliness and sleep disturbance |
| Cho et al. [23] | The associations between subjective and objective social isolation with sleep disturbance remained significant after adjusting for all covariates |
| Makarem and Naji [30] | There was an inverse relationship between loneliness and quality of sleep |
| Cheng et al. [33] | Poor social networks and restless sleep reciprocally influence each other through depressed moods in older adults |
| Yu et al. [26] |
After controlling confounders, social isolation at the baseline predicted poor sleep quality 6 years later, while the association between loneliness and sleep quality was no longer significant There is an adverse effect of social isolation on sleep quality, but this effect is independent of loneliness It seems that loneliness and social isolation have distinct pathways in affecting the quality of sleep among older adults |
| Eshkoor et al. [31] | Social isolation and being single increased sleep disruption |
| McHugh and Lawlor [24] | After controlling for demographic factors and for sleep quality at baseline, loneliness at baseline predicted sleep quality at follow-up |
| Yao et al. [32] | There was a significant relationship between a social network (relationships with relatives/friends) and sleep quality |
WASO wake after sleep onset, TST total sleep time
Discussion
The current systematic review assessed the relationship between loneliness and social isolation with sleep quality in older adults. Among the 11 included studies, seven studies (four cross-sectional [23, 27, 29, 30] and three longitudinal [24, 25, 34]) had reported a statistically significant association between subjective isolation and low sleep quality. Also, five studies (three cross-sectional [23, 31, 32] and two longitudinal [26, 33]) had reported a statistically significant association between objective isolation and low sleep quality. Although loneliness and social isolation are often used interchangeably, they are two separate categories. Loneliness, also known as subjective isolation, denotes how people perceive their experience and whether or not they feel isolated. It is described as the perceived deficit in an individual’s social resources, such as social support and companionship [8]. On the other hand, social isolation is defined as a lack of relation with friends or family and a weak social network at the broader level [38].
According to the results of the present review, social isolation and loneliness were related to sleep problems in older adults. Jia and Yuan found that the older adults with higher levels of loneliness had poorer sleep quality than those with moderate to less loneliness [29]. Although social isolation and loneliness are often correlated [39], some findings suggest that the relationship between objective and subjective social isolation with sleep quality is independent of each other. On the one hand, there is evidence that loneliness affects sleep quality regardless of social interaction. People who felt lonely, regardless of household size and whether living with others or alone, reported more sleep problems than those who were not lonely [40]. On the other hand in a longitudinal study, Yu et al. found that after controlling confounders, social isolation at the baseline could predict poor sleep quality in a 6-year follow-up period, while the association between loneliness and sleep quality was no longer significant. These findings indicate that the association between social isolation and loneliness with sleep quality is independent of each other [26]. Thus, it seems that loneliness and social isolation have distinct pathways in affecting the quality of sleep among older adults.
The findings of Benson et al. were in contrast with those reported by Yu et al. Benson et al. found that loneliness was associated with low sleep quality, but social isolation was not. In contrast, Yu et al. found that social isolation was associated with self-reported low sleep quality, but loneliness was not associated with a worse sleep quality [26, 27]. This inconsistent finding may be related to differences in how social isolation, loneliness, and sleep quality were measured. Benson et al. used the actigraph sleep metrics and four items about insomnia symptom scores. They used the three-item UCLA Loneliness Scale and the Social Disconnectedness Scale to measure subjective and objective social isolation. In contrast, Yu et al. used the PSQI to determine self-reported sleep quality and used less comprehensive social isolation and loneliness measures. Similar to the results of Benson et al., a systematic review [41] showed that loneliness increased sleep problems (poor sleep quality and insomnia symptoms), though it did not change sleep duration [29].
Some physiological functions may clarify the relationship between objective and subjective social isolation with sleep quality. Sleep problems are associated with tremendous stress and anxiety and may express emotional distress in lonely people [29, 42]. Depression and anxiety are probable, but not necessarily an exclusive path in which social isolation can affect sleep quality. The existing evidence has proposed several risk factors for depression and anxiety, of which social isolation is only one of the risk factors. In addition, the studies examining the relationship between social isolation, depression, and sleep quality showed that the relationship between both types of social isolation and poor sleep quality remains significant even after controlling for depression [25, 26, 34]. This finding indicates that there are also other pathways between loneliness and social isolation with sleep problems.
The effect of social isolation and loneliness on the older adults’ sleep quality was partly due to the stress caused by them [24]. Social isolation and loneliness are the primary sources of chronic stress in modern society [43] due to deprivation and social exclusion perceptions [24]. Also, it might have a negative impact on health. Stress poses the risk of CVD [24, 43], directly affects sympathetic neuronal function, and raises the danger of engaging in high-risk behaviors, such as smoking and alcohol abuse [24].
Besides, the relationship between objective and subjective social isolation with sleep quality can lead to a sense of security through sleeping together at night [44, 45]. Throughout the historical stages of human life evolution, security in general and sleeping security in particular—provided by sleeping together- have ever been one of the vital needs of humankind. The relationship between social isolation and loneliness with low-quality sleep can be due to insecurity from living alone and in isolation. The loneliness associated with it makes a person feel more threatened and vulnerable. Feelings of vulnerability lead to hypersensitivity to threatening stimuli, resulting in scattered sleep and poor sleep quality [26]. Given the mentioned discussions, it is crucial to address older adults’ sleep problems since sleep disturbances may detrimentally influence individuals’ physical and mental health [46]. Objective and subjective social isolation can increase sleep problems, depression, and fatigue in older adults, which means that people who feel lonely and have a weak social network suffer more sleep problems, depression, and fatigue. Social isolation can lead to sleep problems through depression or, conversely, sleep problems can lead to social isolation through depression [33]. As age increases, sleep problems increase with changes in the brain [47], increasing depressive symptoms [48]. In general, the feeling of isolation provokes neural activity and anxiety [49] and reduces sleep quality [50]. In a study, social support improved sleep quality in older adults with insomnia compared with the control group [51]. In another study, perceived social support was significantly associated with sleep problems [52]. Thus, the development of social services and the formation of support groups for older adults to prevent social isolation, loneliness, and ultimately sleep problems seem to be an excellent way to promote their health.
The included studies used different tools to measure the variables. Different sleep assessment methods, from objective methods such as actigraphy [27] to subjective methods such as sleep questionnaires [23–26, 29, 30, 32, 34], from single item [31, 33] to scales with strong psychometric properties [23, 24, 26, 29, 30, 32], were used. Actigraphy is an objective and reliable method of sleep assessment. A previous review study showed that there is no perfect sleep assessment method [53]. Nevertheless, the accuracy of hardware devices is superior to that of questionnaires [53, 54]. This superiority, however, must be considered only in terms of precision, but not in terms of diagnostic usefulness. The most valid and widely used questionnaire to assess sleep quality is PSQI, which contains seven components as follows: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. The reliability of the scale was considered good. Also, the validity of PSQI was good, with a sensitivity of 89.6% and a specificity of 86.5% in patients versus control subjects [55]. The sleep questionnaires are easy to administer and very low-cost; so, they are ideal to be used as the first diagnostic test. They do not require a sleep center, can be self-administered at home, and most importantly, their accuracy is relatively high [54]. Furthermore, they summarize the participants’ perceptions about their sleep quality quantitatively. Because sleep questionnaires are primarily subjective, they can be influenced by the same sources of bias and inaccuracy as any other such reports. Also, they have been erroneously considered as unreliable. However, their subjectivity does not necessarily render questionnaires inaccurate [53]. Both discussed instruments (PSQI and actigraphy) were recommended for future studies [33].
In the same way, social isolation and loneliness measures varied across studies, ranging in quality from one single-item and researcher-made questionnaires to standard scales. The UCLA Loneliness Scale was the most used tool to measure loneliness. The three-item UCLA Loneliness Scale has several advantages, including easy-to-use nature in older adults, high reliability in terms of internal consistency and test-retest, and high convergent and construct validity [35] with the advantages of a shorter scale [56]. In addition, although De Jong Gierveld Loneliness Scale was used in only one study, it might be the preferred instrument on loneliness because it is a valid and reliable tool to measure emotional and social loneliness [57]. Due to the mentioned features and the benefits of a shorter scale, this tool is suitable for epidemiological surveys [56]. In the case of measuring objective social isolation, it seems that the abbreviated scales such as the LSNS-6 [58] with its more ‘objective’ style questions ascertaining the degree of perceived social support from friends and family might be the preferred instrument for use in primary health care settings or community-based screenings [56]. Further comparative studies on measuring instruments can be helpful and provide good indicators. However, choosing a specific instrument should be based on the characteristics of the target population and study resources.
Strengths and limitations
As far as the researchers investigated, this is the first systematic review evaluating the relationship between objective and subjective social isolation with sleep quality in older adults.
The strengths of the present study can be listed as the following: a large sample size; selecting the vulnerable and growing older adults as the target group; the simultaneous review of cross-sectional and longitudinal studies; the high quality of five studies out of the six longitudinal studies; and the inclusion of studies from different countries.
However, the main limitations of the present review were as follows: First, most of the included studies were cross-sectional [23, 27, 29–32] which was a barrier to inference on the causality and directionality of the relationship between objective and subjective social isolation with sleep quality in older adults. So, there was not sufficient evidence to conclude whether social isolation and loneliness precede sleep disturbances or vice versa. Therefore, prospective studies should be carried out to demonstrate the causal relationship between social isolation and loneliness with sleep quality. Second, summarizing the results and performing a meta-analysis were not possible due to not using common standard tools to examine the association of social isolation and loneliness with sleep quality in some of the included studies. Thirdly, in most of the studies, the assessment of sleep disturbances relied on subjective self-reported questionnaires, rather than standard objective measures such as actigraphy or polysomnography; hence, incorporating both objective and subjective instruments to measure sleep quality are highly suggested for future studies. Fourthly, among the studies using the PSQI [23, 24, 26, 29, 30, 32], only one study [29] assessed the association of PSQI components with loneliness, and PSQ total score has been used in the remaining. Analyzing the associations of social isolation and loneliness with the PSQI components could provide valuable information on different types of sleep problems. Finally, none of the included studies reported sleep disorders based on the ICD-10 codes, which avoids comprehensive assessment of the relationship between social isolation and loneliness by the components of sleep disorders.
Conclusion
According to our results, most of the included studies reported a significant association between objective and subjective social isolation with sleep quality. However, determining the causal relationships and the possible ways that these variables may affect each other requires further studies. It is recommended to focus more on the mechanisms and/or factors mediating the impact of isolation and/or loneliness on sleep problems and their interactions. Future longitudinal studies are required to establish a causal association between objective and subjective social isolation with sleep disturbances. Also, this review did not assess whether interventions targeting social isolation improve sleep quality. Future research should also determine the role of social isolation reduction interventions on sleep quality.
Acknowledgements
This study was financed by a grant from the Tabriz University of Medical Sciences. We would like to appreciate Clinical Research Development Unit, Imam Reza Hospital, Tabriz University of Medical Sciences, Tabriz, Iran.
Data availability
All data generated or analyzed during this study are included in this published article.
Declarations
Conflict of interest
There is no conflict of interest. The authors have no financial relationships relevant to this article. None of the authors received support for this work influencing the outcome.
Ethical approval
The present study was approved by the Ethics Committee of Tabriz University of Medical Sciences, Iran (code: IR.TBZMED.REC.1398.768).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nicholson NR., Jr Social isolation in older adults: an evolutionary concept analysis. J Adv Nurs. 2009;65(6):1342–1352. doi: 10.1111/j.1365-2648.2008.04959.x. [DOI] [PubMed] [Google Scholar]
- 2.Leigh-Hunt N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 3.Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community. 2017;25(3):799–812. doi: 10.1111/hsc.12311. [DOI] [PubMed] [Google Scholar]
- 4.Iliffe S, et al. Health risk appraisal in older people 2: the implications for clinicians and commissioners of social isolation risk in older people. Br J Gen Pract. 2007;57(537):277–82. [PMC free article] [PubMed] [Google Scholar]
- 5.Chan A, et al. Loneliness and all-cause mortality in community-dwelling elderly Singaporeans. Dem Res. 2015;32:1361–1382. doi: 10.4054/DemRes.2015.32.49. [DOI] [Google Scholar]
- 6.Chang Q, Chan CH, Yip PSF. A meta-analytic review on social relationships and suicidal ideation among older adults. Soc Sci Med. 2017;191:65–76. doi: 10.1016/j.socscimed.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Buffel T, Rémillard-Boilard S, Phillipson C. Social isolation among older people in urban areas: a review of the literature for the ambition for ageing programme in greater Manchester. Manchester: Manchester Institute for Collaborative Research on Ageing; 2015. [Google Scholar]
- 8.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seyfzadeh A, Hagighatian M, Mohajerani A. The relationship between social isolation and health among the tehranian elderly. J Edu Commun Health. 2017;4(3):19–25. doi: 10.21859/jech.4.3.19. [DOI] [Google Scholar]
- 10.Hawton A, et al. The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res. 2011;20(1):57–67. doi: 10.1007/s11136-010-9717-2. [DOI] [PubMed] [Google Scholar]
- 11.Weeks DJ. Sex for the mature adult: health, self-esteem and countering ageist stereotypes. Sex Relationsh Ther. 2002;17(3):231–240. doi: 10.1080/14681990220149031. [DOI] [Google Scholar]
- 12.Cotterell N, Buffel T, Phillipson C. Preventing social isolation in older people. Maturitas. 2018;113:80–84. doi: 10.1016/j.maturitas.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Nicholson NR. A review of social isolation: an important but underassessed condition in older adults. J Primary Prevent. 2012;33(2–3):137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen AW, et al. Objective and subjective social isolation and psychiatric disorders among African Americans. Clin Soc Work J. 2020;48(1):87–98. doi: 10.1007/s10615-019-00725-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 16.Dangol M, Shrestha S, Rai Koirala SK. Insomnia and its associated factors among older people of selected ward of Banepa municipality. Nepal Nurs Open. 2020;7(1):355–363. doi: 10.1002/nop2.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46(3):S39–S52. doi: 10.1353/pbm.2003.0049. [DOI] [PubMed] [Google Scholar]
- 18.Chen J-H, Lauderdale DS, Waite LJ. Social participation and older adults' sleep. Soc Sci Med. 2016;149:164–173. doi: 10.1016/j.socscimed.2015.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smagula SF, et al. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev. 2016;25:21–30. doi: 10.1016/j.smrv.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cacioppo JT, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychol Sci. 2002;13(4):384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- 21.Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nature Sci Sleep. 2017;9:151–161. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petersen N, König H-H, Hajek A. The link between falls, social isolation and loneliness: a systematic review. Arch Gerontol Geriatr. 2020;88:104020. doi: 10.1016/j.archger.2020.104020. [DOI] [PubMed] [Google Scholar]
- 23.Cho JH-J, et al. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging Mental Health. 2019;23(9):1130–1138. doi: 10.1080/13607863.2018.1481928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McHugh JE, Lawlor BA. Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. Br J Health Psychol. 2013;18(3):546–555. doi: 10.1111/j.2044-8287.2012.02101.x. [DOI] [PubMed] [Google Scholar]
- 25.Shankar A. Loneliness and sleep in older adults. Soc Psychiatry Psychiatr Epidemiol. 2020;55(2):269–272. doi: 10.1007/s00127-019-01805-8. [DOI] [PubMed] [Google Scholar]
- 26.Yu B, et al. Prospective associations of social isolation and loneliness with poor sleep quality in older adults. Qual Life Res. 2018;27(3):683–691. doi: 10.1007/s11136-017-1752-9. [DOI] [PubMed] [Google Scholar]
- 27.Benson JA, et al. Associations of loneliness and social isolation with actigraph and self-reported sleep quality in a national sample of older adults. Sleep. 2020 doi: 10.1093/sleep/zsaa140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peterson J, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 29.Jia G, Yuan P. The association between sleep quality and loneliness in rural elderly individuals: a cross-sectional study in Shandong Province China. BMC Geriatr. 2020 doi: 10.1186/s12877-020-01554-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Makarem Z, Naji A. Surveying the relationship between the social isolation and quality of sleep of the older adults in bam-based elderly care centers in 2017. World Family Med J. 2018;99(5833):1–5. doi: 10.5742/mewfm.2018.93379. [DOI] [Google Scholar]
- 31.Eshkoor SA, et al. The effects of social support and having a partner on sleep quality in dementia. Am J Alzheimers Dis Other Demen. 2013;28(3):253–257. doi: 10.1177/1533317513481098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yao K-W, et al. Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults. J Nurs Res. 2008 doi: 10.1097/01.jnr.0000387298.37419.ff. [DOI] [PubMed] [Google Scholar]
- 33.Cheng GHL, et al. Weak social networks and restless sleep interrelate through depressed mood among elderly. Qual Life Res. 2018;27(10):2517–2524. doi: 10.1007/s11136-018-1895-3. [DOI] [PubMed] [Google Scholar]
- 34.Griffin SC, et al. Reciprocal effects between loneliness and sleep disturbance in older Americans. J Aging Health. 2020;32(9):1156–1164. doi: 10.1177/0898264319894486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. J Pers Assess. 1978;42(3):290–4. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- 36.Seeman TE, Syme SL. Social networks and coronary artery disease: a comparison of the structure and function of social relations as predictors of disease. Psychosom Med. 1987;49(4):341–54. doi: 10.1097/00006842-198707000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Hughes ME, et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alspach JG. Loneliness and social isolation: risk factors long overdue for surveillance. Critical Care Nurse. 2013;33(6):8–13. doi: 10.4037/ccn2013377. [DOI] [PubMed] [Google Scholar]
- 39.Schrempft S, et al. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health. 2019;19(1):74. doi: 10.1186/s12889-019-6424-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McLay L, et al. Loneliness and social isolation is associated with sleep problems among older community dwelling women and men with complex needs. Scic Rep. 2021;11(1):4877. doi: 10.1038/s41598-021-83778-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Griffin SC, et al. Loneliness and sleep: a systematic review and meta-analysis. Health Psychol Open. 2020;7(1):2055102920913235. doi: 10.1177/2055102920913235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matthews T, et al. Sleeping with one eye open: loneliness and sleep quality in young adults. Psychol Med. 2017;47(12):2177–2186. doi: 10.1017/s0033291717000629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li H, Xia N. The role of oxidative stress in cardiovascular disease caused by social isolation and loneliness. Redox Biol. 2020;37:101585. doi: 10.1016/j.redox.2020.101585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hawkley LC, Preacher KJ, Cacioppo JT. Loneliness impairs daytime functioning but not sleep duration. Health Psychol. 2010;29(2):124–9. doi: 10.1037/a0018646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hawkley LC, et al. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychology and aging. 2010;25(1):132. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stone KL, Xiao Q. Impact of poor sleep on physical and mental health in older women. Sleep Med Clin. 2018;13(3):457–465. doi: 10.1016/j.jsmc.2018.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buckley TM, Schatzberg AF. Aging and the role of the HPA axis and rhythm in sleep and memory-consolidation. Am J Geriatr Psychiatry. 2005;13(5):344–352. doi: 10.1097/00019442-200505000-00002. [DOI] [PubMed] [Google Scholar]
- 48.BelvederiMurri M, et al. HPA axis and aging in depression: systematic review and meta-analysis. Psychoneuroendocrinology. 2014;41:46–62. doi: 10.1016/j.psyneuen.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 49.Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An fMRI study of social exclusion. Science. 2003;302(5643):290. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- 50.Cacioppo JT, et al. Lonely traits and concomitant physiological processes: the MacArthur social neuroscience studies. Int J Psychophysiol. 2000;35(2):143–154. doi: 10.1016/S0167-8760(99)00049-5. [DOI] [PubMed] [Google Scholar]
- 51.Troxel WM, et al. Does social support differentially affect sleep in older adults with versus without insomnia? J Psychosom Res. 2010;69(5):459–466. doi: 10.1016/j.jpsychores.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Costa SVD, Ceolim MF, Neri AL. Sleep problems and social support: frailty in a Brazilian elderly multicenter study. Rev Latino-Am Enfermagem. 2011;19:920–927. doi: 10.1590/S0104-11692011000400010. [DOI] [PubMed] [Google Scholar]
- 53.Ibáñez V, Silva J, Cauli O. A survey on sleep assessment methods. PeerJ. 2018;6:e4849–e4849. doi: 10.7717/peerj.4849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ibáñez V, Silva J, Cauli O. A survey on sleep questionnaires and diaries. Sleep Med. 2018;42:90–96. doi: 10.1016/j.sleep.2017.08.026. [DOI] [PubMed] [Google Scholar]
- 55.Buysse DJ, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 56.Sansoni J, Marosszeky N, Sansoni NG. Fleming, Final report: effective assessment of social isolation (Centre for Health Service Development, University of Wollongong, 2010). https://www.adhc.nsw.gov.au/__data/assets/file/0007/236329/24_Social_Isolation_Report.pdf.
- 57.De Jong Gierveld J, Van Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing. 2010;7(2):121–130. doi: 10.1007/s10433-010-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lubben J, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist. 2006;46(4):503–13. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.