Abstract
Pulmonary hypertension (PH) is highly prevalent in patients with left heart disease (LHD) and negatively impacts prognosis. The most common causes of PH associated with LHD (PH-LHD) are left heart failure and valvular heart disease. In LHD, passive backward transmission of increased left-sided filling pressures leads to isolated post-capillary PH. Additional pulmonary vasoconstriction and remodelling lead to a higher vascular load and combined pre- and post-capillary PH. The increased afterload leads to right ventricular dysfunction and failure. Multimodality imaging of the heart plays a central role in the diagnostic work-up and follow-up of patients with PH-LHD. Echocardiography provides information about the estimated pulmonary artery pressure, morphology and function of the left and right side of the heart, and valvular abnormalities. Cardiac magnetic resonance imaging is the gold standard for volumetric measurements and provides myocardial tissue characterisation. Computed tomography of the thorax may show general features of PH and/or LHD and is helpful in excluding other PH causes. Histopathology reveals a spectrum of pre- and post-capillary vasculopathy, including intimal fibrosis, media smooth muscle cell hyperplasia, adventitial fibrosis and capillary congestion. In this paper, we provide an overview of clinical, imaging and histopathological findings in PH-LHD based on three clinical cases.
Tweetable abstract
This review provides an overview of the clinical and imaging findings and the histopathological abnormalities in patients with pulmonary hypertension associated with left heart disease based on three clinical cases. https://bit.ly/3T5JDUV
Introduction
Pulmonary hypertension (PH) is defined by increased pressures in the pulmonary vasculature. Among the various PH subgroups, PH associated with left heart disease (PH-LHD) is the most common form and probably affects 5–10% of individuals aged >65 years [1, 2]. The most important causes of PH-LHD in current clinical practice are left heart failure (LHF) and valvular heart disease (VHD). The development of PH in patients with LHD marks an important event since it doubles the mortality risk [2, 3].
Irrespective of the origin of LHD, a progressive decline in left ventricular (LV) (systolic and/or diastolic) function leads to an increase in left atrial (LA) pressure (LAP). Passive backward transmission of raised LAP to the pulmonary veins results in PH. Disturbed function and compliance of the LA add a pulsatile load on the pulmonary circulation [4]. In addition, pulmonary vasoconstriction and intrinsic vascular remodelling may occur, leading to an even stronger increase in pulmonary pressures. The increased afterload results in right ventricular (RV) dysfunction and failure [5].
PH-LHD is haemodynamically defined as an elevated mean pulmonary artery pressure (mPAP) >20 mmHg and an increased pulmonary arterial wedge pressure (PAWP) >15 mmHg at rest [1, 6]. PAWP reflects the health of the LA and represents what pressures the pulmonary capillary bed sees over time [7]. PH-LHD is defined in two forms [1]: isolated post-capillary PH (IpcPH) which is characterised by a low pulmonary vascular resistance (PVR) ≤2 Wood units (WU). In IpcPH, the rise in LAP is followed by an increase in pulmonary pressures and intrinsic pulmonary vascular remodelling is limited; combined pre- and post-capillary PH (CpcPH) is characterised by a high PVR >2 WU. The transition into this stage marks potentially irreversible damage to the lung vasculature [8]. CpcPH is associated with a greater risk of RV failure and poorer prognosis compared to IpcPH [9].
Imaging of the heart plays a central role in the evaluation of patients with suspected PH-LHD and requires a multimodality approach. Echocardiography is the most universal imaging tool used to assess cardiac abnormalities. It plays a vital role in assessing the probability of PH by enabling the estimation of pulmonary pressures and assessing RV function. Cardiac magnetic resonance imaging (MRI) is complementary to echocardiography. It is considered the gold standard for ventricular dimension and function evaluations and provides cardiac tissue characterisation [10, 11]. High-resolution computed tomography (HRCT) and computed tomography pulmonary angiography (CTPA) provide information about the lung parenchyma and perfusion of the pulmonary blood vessels, respectively, and may be used to exclude other types of PH [1].
In this article, based on three case presentations, we describe the clinical features, diagnostic process, imaging and pathological characteristics of patients with PH-LHD.
Methods
The three clinical cases were presented at the Amsterdam UMC Center of Expertise for Pulmonary Hypertension in the Netherlands. Lung tissue samples (autopsy specimens) of the PH patients were stored as part of the Amsterdam UMC PH biobank after obtaining informed consent. In cases of autopsy samples, permission was obtained from the first legal representative.
For the literature search, publications after 2010 were mostly consulted. However, because recent literature about histopathological findings in PH associated with LHD is limited, we consulted histopathological publications from the 1980s.
Case 1
A 74-year-old male presented with progressive dyspnoea over 2 years (New York Heart Association (NYHA) functional class III). His medical history included systemic hypertension, paroxysmal atrial fibrillation and a bradycardia–tachycardia syndrome for which a two-chamber pacemaker had been implanted. He was a former smoker (25 pack-years). There was no history of venous thromboembolism and no exposure to drugs or toxins associated with PH development. He used diuretics, a vitamin K antagonist, a betablocker and antihypertensive drugs. On physical examination, blood pressure was 110/70 mmHg, pulse 82 bpm, peripheral oxygen saturation 90% on room air and body mass index (BMI) 27.5 kg·m−2. He showed clinical signs of RV decompensation with distended jugular veins and oedema in the lower legs. There were no signs of connective tissue disease (CTD). Laboratory testing showed renal insufficiency (creatinine 200 µmol·L−1 (normal <113 µmol·L−1)) and elevated N-terminal pro-brain natriuretic peptide (NT-proBNP) of 845 ng·L−1 (normal <300 ng·L−1). Blood count, thyroid function and liver function tests were normal. Auto-immune serology and an HIV test were negative. Arterial blood gas showed an arterial carbon dioxide tension (PaCO2) of 4.1 kPa (normal PaCO2 5.1–5.6 kPa) and an arterial oxygen tension (PaO2) of 8.4 kPa (normal PaO2 10.5–13.5 kPa). Electrocardiography (ECG) showed atrial fibrillation with ventricular pacing. Transthoracic echocardiography revealed preserved LV systolic function (LV ejection fraction (LVEF) 50%), but severely impaired LV diastolic function. There was RV dilatation with depressed RV function. Both atria were severely enlarged. Tricuspid regurgitation was mild. Peak tricuspid regurgitation velocity (TRV) was 3.4 m·s–1, corresponding to an estimated pulmonary artery (PA) pressure of 46 mmHg, so a high estimated PH probability (figure 1a–f). The vena cava was dilated and had a reduced collapse during respiration. There were no valvular abnormalities.
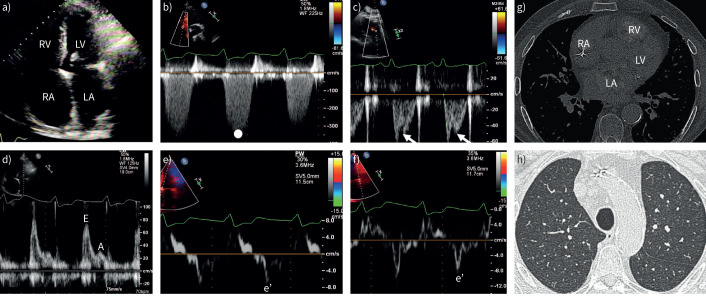
FIGURE 1.
Case 1. Pulmonary hypertension associated with heart failure with preserved ejection fraction: echocardiography and computed tomography (CT). a) Transthoracic echocardiography shows right atrial (RA) and right ventricular (RV) dilatation. In addition, the left atrium (LA) is dilated. Left ventricular (LV) dimensions and systolic function are preserved. b) Maximum tricuspid regurgitation velocity measured by continuous-wave Doppler over the tricuspid valve indicates elevated pulmonary pressures. c) Pulsed-wave (PW) Doppler over the RV outflow tract demonstrates a short acceleration time and a mid-systolic notch (arrows). d) LV diastolic function is severely impaired as illustrated by an increased E:A ratio measured by PW Doppler over the mitral valve inflow. Tissue doppler imaging demonstrates reduced e′ velocity over the e) septal wall and f) lateral LV wall. g) CT of the thorax shows a dilated LA. h) CT shows no signs of parenchymal lung disease.
Pulmonary function test showed no obstruction and minor restriction (forced vital capacity (FVC) 3.4 L (76% pred), forced expiratory volume in 1 s (FEV1) 2.7 L (81% pred), Tiffeneau index 78%, TLC 5.2 L (68% pred). Diffusing capacity for carbon monoxide (DLCO) was decreased (38% pred). However, HRCT did not show signs of emphysema or other (fibrosing) parenchymal lung disease. There was bi-atrial enlargement suggesting LHD (figure 1g and h). Ventilation/perfusion scintigraphy ruled out (chronic) pulmonary embolism. Right heart catheterisation (RHC) revealed CpcPH with an increased mPAP of 50 mmHg, PAWP of 20 mmHg and a PVR of 7.7 WU. In addition, right atrial pressure (RAP) was 20 mmHg (normal RAP <7 mmHg), cardiac output (CO) was 3.9 L·min−1 (thermodilution) and the mixed venous oxygen saturation (SvO2) was 44% (normal SvO2 60–75%). The diagnosis of group 2 PH associated with heart failure with preserved ejection fraction (HFpEF) was made. Best supportive care but not PH-specific therapy was initiated. A few months later, the patient died of progressive RV failure despite a high dose of diuretics.
Autopsy revealed a pulmonary pre- and post-capillary vasculopathy with important venous remodelling and arterialisation of septal veins and capillary congestion, to some point reminiscent of pulmonary veno-occlusive disease (PVOD). Detailed histology is presented in figure 2.
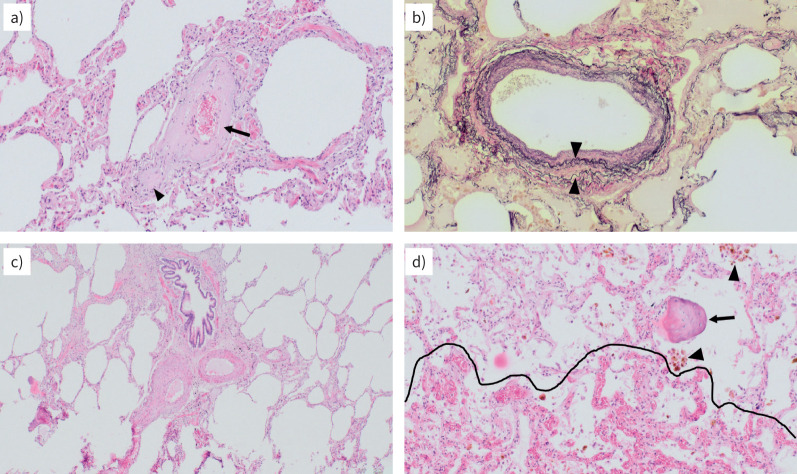
FIGURE 2.
Case 1. Pulmonary hypertension (PH) associated with heart failure with preserved ejection fraction: lung histopathology. a, c, d) Haematoxylin and eosin staining and b) Elastica van Gieson staining; magnification ×100 (all). a) Collagen-rich remodelling with constrictive intimal fibrosis of a septal vein; the small branch (arrowhead) beneath the larger vein (arrow) appears to be completely occluded. b) Arterialisation of a septal vein with duplication of the elastic lamina (arrowheads): these veins resemble arteries, but lack the adjacent bronchioles; note the beige oedema filling the alveoli in part. c) Two pulmonary arterial branches (and their adjacent bronchioles), with substantial intimal and medial thickening and representing the morphological correlate to the pre-capillary PH component. d) Capillary congestion with the beginning of haemangiomatosis-like changes (area below the dotted line); note the numerous haemosiderophages (arrowheads) and the ossified fragment (arrow), both typical in long-lasting congestion due to left heart failure.
PH associated with LHF
Clinics
In developed countries the prevalence of LHF is estimated to be 1–2% in the general adult population. LHF is a clinical syndrome consisting of typical cardiac symptoms and signs that are due to structural and/or functional cardiac abnormalities that result in reduced CO and/or increased left-sided filling pressures [12]. Signs of orthopnoea and paroxysmal nocturnal dyspnoea are generally not features of one of the other PH types [13].
LHF is categorised in three HF phenotypes based on LVEF measurements by echocardiography. LVEF <40% defines heart failure with reduced ejection fraction (HfrEF), LVEF 40–49% is defined as heart failure with mildly reduced ejection fraction (HfmrEF), LVEF ≥50% defines HfpEF [12]. In Western countries, coronary artery disease (CAD) and hypertension are the most common HfrEF causes [14]. HfpEF is frequently associated with obesity and the metabolic syndrome. Importantly, the heart failure (HF) phenotypes may have overlapping underlying pathophysiological causes and there can be a complex interplay between cardiac and noncardiac processes [15].
A normal ECG and/or low levels of laboratory brain natriuretic peptide (BNP) make the diagnosis of HfrEF unlikely. However, HfpEF patients may have a normal ECG and/or BNP levels in ∼33% cases [16, 17]. The prognosis of HfrEF patients has improved significantly since the advent of the four classes of HF drugs (i.e. angiotensin-converting enzyme inhibitors/angiotensin receptor-neprilysin inhibitors, mineralocorticoid receptor antagonists, betablockers and sodium-glucose co-transporter 2 inhibitors). Nevertheless, the prognosis remains poor, with estimated 5-year mortality rates of 43–78%. Most HF medical therapies have a limited impact on HfpEF and the risk of death is (nearly) as high as that for HfrEF patients [18]. HfmrEF is considered a milder form of HfrEF and HF medical therapies may improve HfmrEF [12, 19, 20].
At least 50% of HfrEF patients and ∼80% of HfpEF patients develop PH. In 20–30% of patients with LHF and post-capillary PH, CpcPH is found [2]. The development of PH in LHD increases the mortality risk [2, 3]. Drugs approved for pulmonary arterial hypertension (PAH) are currently not recommended as standard therapy for PH in LHD [1, 21].
Imaging
An echocardiographic probability-based approach for the assessment of PH is included in the work-up for all PH subgroups, including PH-LHD [1]. Peak TRV is the key parameter in determining PH probability. Other echo signs such as flattening/leftward bowing of the interventricular septum, RV and/or right atrium (RA) dilatation, enlarged PA dimensions and a dilated vena cava suggest PH. In addition, a short RV outflow tract acceleration time and a mid-systolic notch measured by pulsed-wave (PW) Doppler suggest PH (figure 1c). This “notch” is frequently seen in PAH but has a lower prevalence in IpcPH and CpcPH associated with LHD [22, 23].
In cases of an intermediate or high PH likelihood, this should prompt a careful assessment of LV function, atrial dimensions and valve diseases. Global systolic function is measured by LVEF, a hallmark parameter for outcome [24]. Regional LV function or myocardial deformation is measured by speckle-tracking derived global longitudinal strain (GLS) [25]. GLS is used for early detection of the subclinical alterations in LV longitudinal function that occur before LVEF impairment [26, 27]. The evaluation of LV diastolic dysfunction is based on echocardiography. Using PW Doppler measurements over the mitral valve inflow, the E-wave velocity during early diastole and A-wave velocity during late diastole are measured. A high E-wave indicates increased LV stiffness and an E/A ratio >2 suggests diastolic dysfunction. In addition, a low mitral annular early wall motion velocity (e′) measured at the mitral valve annulus by tissue Doppler imaging (TDI) indicates diastolic dysfunction. By combining the early diastolic transmitral flow velocity (E)/late diastolic velocity (A) ratio, E/e′ ratio, LA dimensions and an estimation of PH presence, LAP and the severity of LV diastolic dysfunction can be estimated [28].
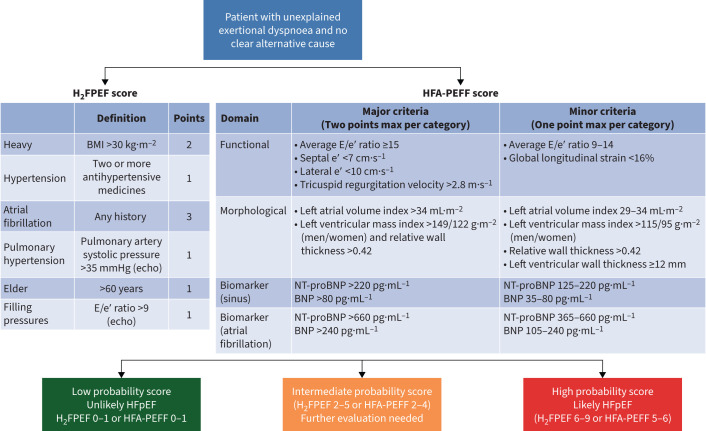
HFpEF diagnosis is complex. A helpful tool to establish the clinical likelihood of HFpEF is the H2FPEF score: a composite scoring system based on clinical, ECG and echocardiographic parameters (H2FPEF: Heavy, Hypertension, atrial Fibrillation, PH, Elder age, elevated Filling pressures) [29, 30]. The Heart Failure Association (HFA)-PEFF (pre-test assesment echocardiographic and natriuretic peptide score functional testing in case of uncertainty final aetiology) algorithm has also been validated but was shown to be less sensitive with lower overall accuracy than the H2FpEF score [31]. An overview of the diagnostic evaluation of patients with HFpEF is provided in figure 3 [17].
FIGURE 3.
An overview of the diagnostic evaluation of patients with heart failure with preserved ejection fraction (HfpEF). Reproduced from Borlaug et al. [17] with permission. BMI: body mass index; BNP: brain natriuretic peptide; echo: echocardiography; E/e′: early diastolic transmitral flow velocity/mitral annular early wall motion velocity ratio; NT-proBNP: N-terminal pro-brain natriuretic peptide; H2FPEF: heavy, hypertension, atrial fibrillation, pulmonary hypertension, elder age, elevated filling pressures.
LA dilation may indicate not only diastolic dysfunction but also serve as a marker of severity and chronicity of LHD [32]. LA enlargement can be used to distinguish between PAH and PH associated with LHD. In addition, adverse LA remodelling such as LA fibrosis, which can be identified by cardiac MRI (see below), is a predictor of LHF, PH, reduced quality of life and mortality [33]. Similarly, progressive LA dysfunction is associated with more severe HFpEF and advanced pulmonary vascular disease [34]. This so-called “LA myopathy” of adverse LA remodelling and/or dysfunction [35] contributes to more severe PH in HFpEF, independent of the increased LA pressures [36].
Cardiac cine MRI plays an important role in identifying the underlying aetiology in HFrEF and HFpEF in the context of PH [37–39]. In addition, myocardial tissue characterisation can be performed through parametric mapping and the acquisition of late gadolinium enhanced (LGE) images [11, 40, 41]. Myocardial alterations due to oedema and inflammation, hyperaemia, capillary leak, haemorrhage, thrombosis, necrosis and fibrosis can be visualised. T1 and T2 (and T2*) mappings allow pixel-wise quantification of the changes in the myocardium and permit both visualisation and quantification of focal or diffuse disease processes. These changes may be related to intracellular disturbances of the cardiomyocyte, extracellular disturbances in the myocardial interstitium or both [42]. LGE imaging is widely used and is the gold standard for identifying regional myocardial infarction/replacement fibrosis. LGE images show a typically subendocardial to transmural enhancement in ischaemic heart disease [43]. Infarct assessment predicts outcomes [44, 45] and guides revascularisation strategies [46, 47]. In contrast, non-ischaemic cardiomyopathies show mid-wall or epicardial enhancement in a non-coronary distribution [42, 48].
Cardiac MRI is not used as a PH-screening tool. Instead, MRI is the gold standard for LV and RV volumetric quantification and is therefore used to monitor therapeutic effects during follow-up [10].
The RV plays an important role in the setting of PH-LHD. RV dysfunction may develop as a consequence of the increased pulmonary load associated with LHF or via direct interventricular interactions [49]. RV dysfunction predicts prognosis in patients with HFpEF and HFrEF [50–52] and in both ischaemic and nonischaemic cardiomyopathies [53, 54]. Even though the overall prevalence of PH is estimated to be higher in HFpEF compared to HFrEF, RV dysfunction is more pronounced in HFrEF for any given degree of PH [55, 56].
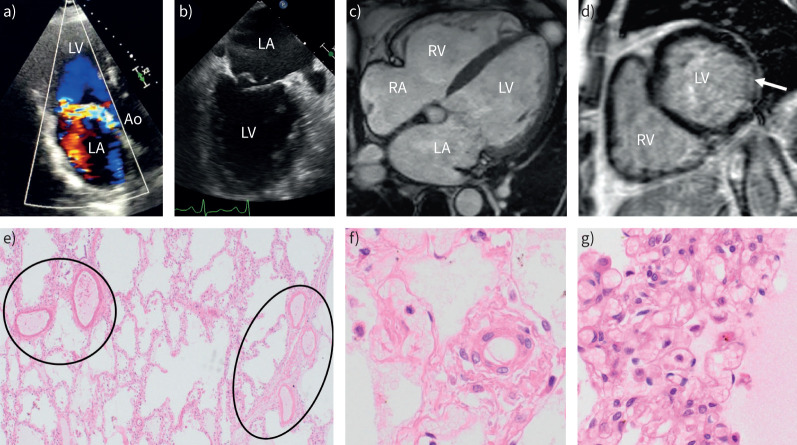
Recent studies show that echocardiographic RV GLS may provide a better estimation of RV systolic function than RV tricuspid annular plane systolic excursion or RV Sʹ (systolic wave prime) [57, 58]. In addition, adverse RV remodelling is a prognostic marker. In patients with Ph-HFpEF and in PAH, the RV shows diffuse fibrosis in comparison to controls [48]. Focal fibrosis is typically seen at the RV insertion points and may extend to the interventricular septum in PH (figure 4d). In mixed groups of PH aetiologies, there were conflicting results with respect to the prognostic value of fibrosis at the RV insertion points, but the presence of fibrosis in the interventricular septum predicted mortality [59, 60].
FIGURE 4.
Case 2. Pulmonary hypertension (PH) related to primary mitral valve regurgitation: echocardiography, cardiac magnetic resonance imaging (MRI) and lung histopathology. a) Transthoracic echocardiography illustrates severe mitral regurgitation. b) Transoesophageal echocardiography illustrates a prolapse of the mitral valve. c) Cardiac MRI shows bi-atrial and biventricular dilatation. d) Cardiac MRI with late-gadolinium enhancement demonstrates fibrosis of the left ventricular (LV) inferolateral wall (arrow). e) Lungs from the patient with PH due to mitral valve disease (autopsy). Haematoxylin and eosin staining (all); magnification: e) ×40 and f) and g) ×400. e) Pulmonary arteries (circle on the left) and pulmonary septal veins (circle on the right) are almost indistinguishable due to venous arterialisation; note the thickened alveolar septa in between that are magnified in g). f) Microvessel, either arteriole or venule, of about 30 µm in diameter; note the perfectly round, single-layered muscularisation of this vessel that is under normal conditions totally devoid of smooth muscle cells. g) Alveolar septa are thickened due to congestion and clear capillary haemangiomatosis, similar to capillary changes in pulmonary veno-occlusive disease; note multiple layers of capillaries in a single septum and expanded alveolus to the left and eosinophil fluid within the alveolus on the right side of the alveolar wall (oedema). Ao: aorta; LA: left atrium; RA: right atrium; RV: right ventricle.
Chest radiography or computed tomography (CT) may show signs of pulmonary vascular congestion and pleural effusion that suggest PH-LHD. With (HR)CT and CTPA, other causes of PH such as parenchymal disease, pulmonary embolism and arteriovenous malformations may be excluded. General CT signs of PH are an enlarged PA, increased main PA/aorta diameter ratio (>1), PA calcification and tortuosity, and tapering of smaller PAs. Additional findings are RV dilatation and hypertrophy, leftward septum bowing, reflux of contrast into the vena cava or hepatic veins and hypertrophy of the bronchial arteries.
Histopathology
Histopathological analyses of patients with PH associated with LHD reveal pulmonary vascular remodelling at the level of the PAs, veins and capillary bed [61–64], but no plexiform lesions. Remodelling of the different vascular compartments, including the intima (fibrosis), media (smooth muscle cell hyperplasia) and adventitia (fibrosis) may occur. Especially in HFrEF and HFpEF, duplication of the elastic lamina is seen in the pulmonary veins (so-called venous arterialisation) [61, 62, 65], making it sometimes difficult to morphologically differentiate arteries from veins.
It is suggested that remodelling of the arteries occurs secondary to remodelling of the veins, corroborating the long-term downstream effects of high cardiac filling pressures [61]. Pulmonary veins may show obstruction due to lose fibrosis and hyalinosis. The latter has been previously called “oedematous” remodelling and it is thought to be reversible after effective decongestion [66].
In addition, stress of the lung capillaries and disruption of the capillary endothelium [67] may induce fluid and protein subtraction from the capillary lumen to the alveolar interstitium, causing oedema. This “alveolar capillary stress failure” is reversible in the acute phase but persistent pressure overload may trigger a pro-inflammatory state leading to vascular remodelling, marking a critical stage in the development of CpcPH [68].
Case 2
A 67-year-old male patient was referred because of progressive dyspnoea over 6 months (NYHA III) related to severe mitral regurgitation and estimated severe PH based on echocardiography. He had a medical history of hypertension, hypercholesterolaemia and mild primary mitral regurgitation. He was treated with antihypertensive drugs and a statin. He has no chest pain, palpitations, orthopnoea or peripheral oedema. He was a nonsmoker, had no history of venous thromboembolisms, no signs of CTD and no toxin/drugs exposure associated with PH development. Physical examination revealed a blood pressure 104/70 mmHg, a pulse of 72 bpm and a peripheral oxygen saturation of 94% at room air. His jugular veins were distended. Auscultation revealed an accentuated pulmonary component of the second heart sound and a holosystolic murmur at the cardiac apex. Lung sounds were normal. Laboratory testing showed normal blood count, kidney function, thyroid function and liver function tests but elevated NT-proBNP of 678 ng·L−1. Auto-immune serology and an HIV test were negative. His ECG showed sinus rhythm with a first-degree atrioventricular block, rightward heart axis, RA dilatation, a tall R-wave in V2 and negative T values in III and AVF. These ECG abnormalities are typical for PH. Lung function tests did not show relevant abnormalities and pulmonary embolism was ruled out by CTPA. Echocardiography showed mild LV dilatation with mildly reduced LV systolic function; LV diastolic function was preserved. There was severe bi-atrial dilatation. The mitral valve showed severe eccentric mitral regurgitation due to a prolapse of posterior valve leaflet 2. There was a moderate tricuspid valve regurgitation due to annular dilatation (figure 4a and b). Maximum TRV was 3.2 m·s–1 corresponding to 41 mmHg. The vena cava was dilated with a reduced collapse during respiration. Coronary angiography ruled out CAD. RHC showed an mPAP of 32 mmHg. The mean PAWP was 21 mmHg and showed a high rise of the V-wave. CO was 3.1 L·min−1 and PVR was 3.5 WU. Cardiac MRI was acquired to better characterise RV function, mitral regurgitation severity and myocardial fibrosis. MRI showed that RV function was severely depressed (RV ejection fraction 25%; normal RV ejection fraction >45%). A severe mitral regurgitation fraction of 63% was found (normal: 0%). In addition, MRI showed myocardial fibrosis of the LV inferolateral wall and RV insertion points (figure 4c and d). The LA was severely dilated and there was a high amount of LA fibrosis of 19% (normal: 0%).
This patient was diagnosed with CpcPH secondary to severe primary mitral regurgitation. Despite mildly elevated pulmonary pressures, RV dysfunction was significant. The patient underwent mitral valve repair and tricuspid valve repair. Unfortunately, he had multiple post-operative complications including severe RV failure and was treated with vasopressors, inotropes and PH-lowering medicines. Despite optimal medical care, the patient ultimately died.
The lungs from this patient were assessed after autopsy. The most prominent changes were within the post-capillary vasculature with characteristic arterialisation of pulmonary septal veins to a degree, where discrimination from PAs was difficult, with the false impression of numerous “orphan arteries” lacking their adjacent airway and thereby topographically identified as veins. Pulmonary capillary haemangiomatosis (PCH) foci, reminiscent of PVOD/PCH, were present. For a detailed description of this histological findings see figure 4.
PH due to left-sided valvular heart disease
Clinics
In previous decades, rheumatic mitral valve stenosis was the most important cause for PH-LHD, but its prevalence in Western counties is decreasing [69]. PH is currently predominantly related to primary mitral regurgitation (estimated prevalence 20–64%) [70–74] and aortic stenosis (AOS) (estimated prevalence 20–53%) [75–78]. Data on PH prevalence in aortic regurgitation are scare (estimated prevalence of 16–44%) and its relationship with prognosis is controversial [79, 80]. The prevalence of PH varies over studies according to patient selection criteria and different cut-off values for PH. In most patients with PH related to VHD, IpcPH will develop and CpcPH may occur in ∼12–20% of cases [81–83]. It is important to notice that PH may also develop in patients with moderate–severe VHD [84].
The presence of PH is a strong and independent predictor of mortality in VHD. Even mild elevations in pulmonary pressures translate into a rise in the risk of death [84]. Patients with moderate–severe or severe VHD should be referred for surgical or transcatheter interventions according to the algorithms of the guidelines [85]. In patients with primary severe mitral regurgitation, severe PH (sPAP >50 mmHg) is a criterion for surgical intervention, regardless of the symptomatic stage [85, 86]. In addition, surgery should be considered in patients with severe PH associated with asymptomatic severe mitral stenosis [85].
Interestingly, PH is reversible in most patients with VHD after surgical or percutaneous interventions. Traditionally, pulmonary vasoconstriction was considered to be the most important underlying PH mechanism [87]. However, recent data show that PH may persist in up to ∼20% of patients despite successful surgery and this was associated with poor prognosis, emphasising the importance of early interventions [71, 86, 88]. Persistent post-operative PH was predicted by older age and higher pre-operative pulmonary pressures [71, 74]. Currently, no benefit is demonstrated of initiating PAH-specific therapy.
Imaging
Echocardiography has a central role in the evaluation of VHD and the criteria are described in the guidelines [85]. Importantly, the presence of PH and RV dysfunction may lead to a decrease in RV stroke volume, potentially leading to underestimation of the severity of left-sided VHD. Echocardiographic evaluation specifically includes evaluation of the tricuspid valve since concomitant tricuspid regurgitation is common [89]. When surgery or invasive intervention is planned for VHD, tricuspid regurgitation severity and RV dilatation determine whether concurrent tricuspid valve surgery should be performed [85]. In addition, estimation of pulmonary pressures during echocardiography is mandatory. In the specific setting of PH due to VHD, invasive RHC could be debated. However, RHC may be used to confirm PH diagnosis, measure its severity and measure PAWP [1].
Echocardiographic predictors for the presence of PH in mitral regurgitation are a higher LA size, LV end-systolic dimensions and E/e′, and a shorter mitral deceleration time [71, 86, 90]. In AOS, PH was predicted by more severe AOS and lower LVEF but is also related to LV diastolic dysfunction, LA dilatation, atrial fibrillation, concomitant mitral regurgitation and comorbidities [83, 91, 92].
Cardiac MRI provides “added” value to echocardiography in VHD. Using MRI phase-contrast velocity mapping, flows can be measured and are useful for the precise calculation of the regurgitant volume and the velocity of blood flow within the plane of a stenotic valve [93]. In addition, myocardial tissue characterisation provides prognostic information in VHD patients [94]. In mitral regurgitation, regional replacement fibrosis is commonly seen in segments adjacent to the posteromedial papillary muscle and indicates an arrhythmic risk (figure 4d) [95]. In addition, an increased extracellular volume measured by T1 mapping was found and possibly reflects reactive interstitial fibrosis that was reduced after surgery [96]. In patients with AOS, patchy LGE accumulates over time and is associated with more severe valve stenosis and LV dysfunction [97]. The extent of LV myocardial fibrosis measured by MRI and validated by endomyocardial biopsy in AOS patients correlated with PH severity [98].
Histopathology
A pre- and post-capillary pulmonary vasculopathy involving arteries and veins is initially described in PH patients with severe mitral valve stenosis [99]. Various combinations of arteriolar medial hypertrophy, intimal proliferation, adventitial thickening, microthrombi, medial hypertrophy and intimal fibrosis of veins, capillary congestion with haemosiderosis, thickened alveolar–capillary membranes and dilated lymphatics have been demonstrated [99–101].
Case 3
A 77-year-old male was referred because of suspected PH based on echocardiography. He has a medical history of obstructive sleep apnoea syndrome (OSAS), which was well controlled with continuous positive airway pressure, and multiple risk factors for LHD, namely obesity, hypertension and CAD. He had received a percutaneous coronary intervention of the left ascending coronary artery. He was treated with diuretics, dual antiplatelet therapy and antihypertensive drugs. During the last months, he experienced progressive dyspnoea (NYHA functional class III). He was a previous smoker (40 pack-years). No use of drugs or toxin exposure. Physical examination showed a high BMI of 37 kg·m−2, blood pressure 110/70 mmHg, pulse 82 bpm and peripheral oxygen saturation of 89% at room air. Pulmonary auscultation revealed bilateral crackles. There were no signs of ascites, but lower leg oedema was present. Laboratory testing showed normal blood count, liver function tests and thyroid function. There was mild renal impairment and NT-proBNP was increased (2302 ng·L−1). Auto-immune serology and an HIV test were negative. Arterial blood gas showed a PaCO2 5.2 kPA, PaO2 8.8 kPA and oxygen saturation of 92% on 5 L supplemental oxygen.
Echocardiography showed preserved LV systolic function, grade II (i.e. moderate) diastolic dysfunction, RV dilatation and dysfunction with leftward septum bowing. There was bi-atrial dilatation (figure 5a and b). Tricuspid regurgitation was mild and revealed an estimated TRV of 71 mmHg. Pulmonary function test was slightly obstructive (FVC 2.8 L (75% pred), FEV1 1.9 L (75% pred, Tiffeneau index 65%)) and DLCO was severely reduced (32% pred).
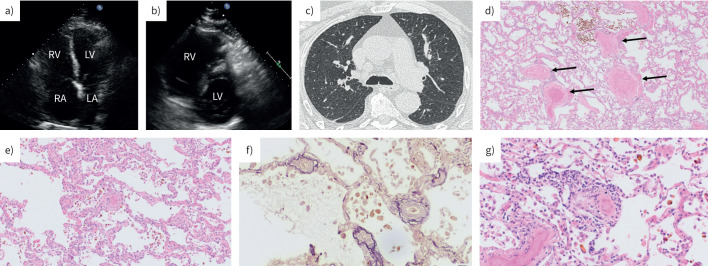
FIGURE 5.
Case 3. Pulmonary (arterial) hypertension (P(A)H) with cardiopulmonary comorbidities: echocardiography, computed tomography (CT) and histopathology. a, b) Transthoracic echocardiography shows bi-atrial and right ventricular (RV) dilatation. There is flattening of the interventricular septum. c) High-resolution CT showing minimal parenchymal emphysema, some septal lines, but no (fibrotic) interstitial lung disease. d) Lungs from the patient classified as P(A)H with cardiopulmonary comorbidities (autopsy) d, e, g). Haematoxylin and eosin staining and f) Elastica van Gieson staining; magnification: d) ×40, e) ×100, and f) and g) ×200. d) Pulmonary arteries (arrows) display important medial hyperplasia; congestion is present on every slide, with thick alveolar septa and enlarged capillaries; note the brownish haemosiderophages (top). e) and f) Microvessels are muscularised throughout the lung, down to the smallest pre- and post-capillary level, with near-occlusive remodelling. g) Chronic inflammatory infiltrate can be observed within the interstitium and in the vicinity of remodelled microvessels. LA: left atrium; LV: left ventricle; RA: right atrium.
CTPA showed general features of PH but no pulmonary embolism. The lung parenchyma on HRCT was mildly emphysematous and showed some subtle septal lines, but there was no (fibrotic) interstitial lung disease (figure 5c). RHC showed PH based on an elevated mPAP of 58 mmHg and a PVR of 9 WU. Resting PAWP was in the borderline range (13 mmHg) and CO was relatively preserved (4.8 L·min−1, thermodilution). An additional invasive LV end-diastolic pressure (LVEDP) measurement was 11 mmHg (normal LVEDP <12 mmHg).
Based on the invasive haemodynamic measurements, the patient was classified as group 1 idopathic PAH (IPAH) with cardiopulmonary comorbidities. He was treated with diuretics and careful initiation of PAH-specific therapy (phosphodiesterase inhibitor and an endothelin receptor antagonist). A few months later, he died of progressive RV failure.
Autopsy revealed pulmonary vascular disease at the pre-capillary and- post-capillary level. In addition to typical medial thickening in muscular-type PAs a prominent microvasculopathy with severe and near-occlusive remodelling of pre- and post-capillary vessels (arterioles and venules) down to 40–50 µm in diameter. Congestion and PCH-like areas with important thickening of alveolar septa was present, as well as moderate chronic inflammatory interstitial infiltrates, involving microvessels, too. For a detailed description of the cases histology see figure 5d–g.
PAH with cardiopulmonary comorbidities?
The demographics and clinical characteristics of patients with IPAH have changed considerably over the last 30 years [1, 102]. IPAH patients have become older, are more often male and have a higher frequency of cardiac and pulmonary comorbidities [103–108]. Recently, it was shown in a cluster analysis of 841 newly diagnosed patients with IPAH from the COMPERA registry that only 12.6% of patients had a classic phenotype (young, mostly female patients without cardiopulmonary comorbidities, never-smokers and a preserved DLCO), while 35.8% of patients presented with a left heart phenotype (primarily female patients, older age, cardiopulmonary comorbidities and preserved DLCO) and 51.6% with a so-called pulmonary phenotype (primarily male patients, older age, history of smoking, pulmonary comorbidities and decreased DLCO) [103]. Similar phenotypes have been described by the PVDOMICS study group [109]. These nonclassical phenotypes are referred to in the 2022 European Respiratory Society/European Society of Cardiology (ESC) PH guidelines as IPAH with cardiopulmonary comorbidities [1]. However, a clear definition is lacking and whether patients currently classified as “P(A)H with cardiopulmonary co-morbidities” should be recognised as a group within group 1 PAH or should rather be placed within group 2 or 3 PH is a subject of ongoing debate and research.
The patient in case 3 had multiple comorbidities and cardiac risk factors for LHD with grade II diastolic dysfunction on echocardiography. Histopathology of case 3 showed pulmonary vascular remodelling at the pre- and post-capillary level that might suggest LHD as the primary cause (group 2 PH). However, this patient had a haemodynamic pre-capillary profile with an LVEDP measurement of 11 mmHg, illustrating the current diagnostic and treatment challenges in this patient population. Interestingly, cardiac risk factors such as obesity (and the related obesity hypoventilation syndrome) may directly induce pulmonary hypertensive changes. Histopathology of lungs of obese patients (autopsy) showed signs of venous hypertension and capillary haemangiomatosis [110, 111].
In this case, passive leg-raise manoeuvre or exercise tests were not performed. It has been demonstrated that many patients with “occult” HFpEF may have normal resting PAWP but show a significant rise in PAWP during stress [112]. Another explanation for a normal PAWP despite LHD, may be that the PAWP is normalised after successful treatment of hypertension and CAD.
In addition, the patient in case 3 was a former heavy smoker (however, only had a mildly obstructive pulmonary function test and minimal emphysema on chest CT), which might indicate that this patient could have group 3 PH disease. Despite the fact that some experts might call this case PH secondary to group 2 or group 3 disease, whereas others might classify this case as IPAH with cardiopulmonary comorbidities, the outcome is poor, irrespective of the name of the disease. This group of P(A)H patients experienced less effective responses from mono or combination therapies compared to “classic” PAH patients without (cardiopulmonary) comorbidities [113, 114]. In addition, the first group of patients may experience higher rates of clinical failure [114]. Currently, there is no solid evidence available for treatment recommendations in these patients with cardiopulmonary comorbidities fulfilling the pre-capillary haemodynamic P(A)H criteria. According to the recent ESC guidelines, monotherapy of endothelin receptor antagonist or phosphodiesterase type 5 inhibitor may be initiated but careful follow-up is required [1].
Future studies are required to reveal the nature of this type of P(A)H disease and explore novel treatment options.
Points for clinical practice
PH is a frequent complication of LHD.
The most common causes are (systolic and diastolic) LHF and VHD.
The development of PH in LHD doubles the mortality risk.
Isolated post-capillary PH is haemodynamically defined as mPAP >20 mmHg, PAWP >15 mmHg and PVR ≤2 WU.
Combined pre- and post-capillary PH is defined as mPAP >20 mmHg, PAWP >15 mmHg and PVR >2 WU.
A multimodality imaging approach is required for an accurate diagnosis.
Echocardiography plays a vital role in PH evaluation though estimations of pulmonary pressures and assessments of biventricular and atrial morphology and function and valvular abnormalities.
The presence of LA enlargement in patients with PH is a diagnostic clue suggesting LHD.
Cardiac MRI provides noninvasive tissue characterisation and has an important role in identifying the underlying aetiology of LHD.
Histopathological analyses reveal that vascular remodelling occurs at the level of the PAs, veins and the capillary bed.
Summary and conclusions
PH has a high prevalence and is an in important predictor of mortality in patients with LHD. A multimodality imaging approach is required to accurately diagnose PH in LHD and reveal the underlying cardiac aetiology. Echocardiography is important in the assessment of cardiac morphology, ventricular function, valvular abnormalities and estimation of haemodynamic parameters. Chest X-ray or CT may show general features of PH and signs of LHD/pulmonary congestion. Cardiac MRI is complimentary to echocardiography, providing additional information on tissue characterisation. Furthermore, it is the gold standard for volumetric measurements, making it a useful tool for surveillance and therapeutic monitoring.
Histologically, PH-LHD is a good example of a vascular phenotype mix that is increasingly coming to our attention: PAH-typical pulmonary arterial changes are found next to post-capillary and capillary remodelling that is strongly reminiscent of PVOD. In addition, some LHD cases show more prominent remodelling of smallest microvessels beneath 40 µm in diameter and, here, mostly smooth muscle cell hyperplasia that can be reversible. In contrast to IPAH and hereditary PAH, plexiform lesions are never found in PH-LHD. Interestingly, they also do not appear in lungs from patients with PVOD, which proves that different aetiologies may display a similar pattern in morphology, perhaps due to a common pathophysiological denominator we still have to identify.
Footnotes
Provenance: Commissioned article, peer reviewed.
Previous articles in this series: No. 1: Condliffe R, Durrington C, Hameed A, et al. Clinical–radiological–pathological correlation in pulmonary arterial hypertension. Eur Respir Rev 2023; 32: 230138. No. 2: Lichtblau M, Mayer L, Gopalan D, et al. Clinical-radiological-pathological correlation in pulmonary hypertension with unclear and/or multifactorial mechanisms. Eur Respir Rev 2023; 32: 230119. No. 3: Verbelen T, Godinas L, Dorfmüller P, et al. Clinical–radiological–pathological correlation in chronic thromboembolic pulmonary hypertension. Eur Respir Rev 2023; 32: 230149. No. 4: Lechartier B, Boucly A, Solinas S, et al. Pulmonary veno-occlusive disease: illustrative cases and literature review. Eur Respir Rev 2024; 33: 230156.
Number 5 in the Series “Clinical–radiological–pathological correlation in pulmonary hypertension” Edited by Robin Condliffe, Anton Vonk Noordegraaf, Olivier Sitbon, Peter Dorfmüller and Deepa Gopalan
This article has an editorial commentary: https://doi.org/10.1183/16000617.0237-2023
Conflict of interest: E.J. Nossent and A. Vonk Noordegraaf have received speaker fees for lectures and educational events from Janssen, MSD and United Therapeutics/Ferrer. E.J. Nossent has received consulting fees from Janssen, MSD and United Therapeutics/Ferrer and A. Vonk Noordegraaf from Janssen, MSD and United Therapeutics/Ferrer. The other authors did not report any conflict of interest.
References
- 1.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2022; 43: 3618–3731. doi: 10.1093/eurheartj/ehac237 [DOI] [PubMed] [Google Scholar]
- 2.Hoeper MM, Humbert M, Souza R, et al. A global view of pulmonary hypertension. Lancet Respir Med 2016; 4: 306–322. doi: 10.1016/S2213-2600(15)00543-3 [DOI] [PubMed] [Google Scholar]
- 3.Bursi F, McNallan SM, Redfield MM, et al. Pulmonary pressures and death in heart failure: a community study. J Am Coll Cardiol 2012; 59: 222–231. doi: 10.1016/j.jacc.2011.06.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tedford RJ, Hassoun PM, Mathai SC, et al. Pulmonary capillary wedge pressure augments right ventricular pulsatile loading. Circulation 2012; 125: 289–297. doi: 10.1161/CIRCULATIONAHA.111.051540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol 2001; 37: 183–188. doi: 10.1016/S0735-1097(00)01102-5 [DOI] [PubMed] [Google Scholar]
- 6.Simonneau G, Hoeper MM. The revised definition of pulmonary hypertension: exploring the impact on patient management. Eur Heart J Suppl 2019; 21: Suppl. K, K4–K8. doi: 10.1093/eurheartj/suz211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huston JH, Shah SJ. Understanding the pathobiology of pulmonary hypertension due to left heart disease. Circ Res 2022; 130: 1382–1403. doi: 10.1161/CIRCRESAHA.122.319967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vanderpool RR, Saul M, Nouraie M, et al. Association between hemodynamic markers of pulmonary hypertension and outcomes in heart failure with preserved ejection fraction. JAMA Cardiol 2018; 3: 298–306. doi: 10.1001/jamacardio.2018.0128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenkranz S, Gibbs JS, Wachter R, et al. Left ventricular heart failure and pulmonary hypertension. Eur Heart J 2016; 37: 942–954. doi: 10.1093/eurheartj/ehv512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pennell DJ, Sechtem UP, Higgins CB, et al. Clinical indications for cardiovascular magnetic resonance (CMR): consensus panel report. Eur Heart J 2004; 25: 1940–1965. doi: 10.1016/j.ehj.2004.06.040 [DOI] [PubMed] [Google Scholar]
- 11.Haaf P, Garg P, Messroghli DR, et al. Cardiac T1 mapping and extracellular volume (ECV) in clinical practice: a comprehensive review. J Cardiovasc Magn Reson 2016; 18: 89. doi: 10.1186/s12968-016-0308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021; 42: 3599–3726. doi: 10.1093/eurheartj/ehab368 [DOI] [PubMed] [Google Scholar]
- 13.Guazzi M, Arena R. Pulmonary hypertension with left-sided heart disease. Nat Rev Cardiol 2010; 7: 648–659. doi: 10.1038/nrcardio.2010.144 [DOI] [PubMed] [Google Scholar]
- 14.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1789–1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gevaert AB, Kataria R, Zannad F, et al. Heart failure with preserved ejection fraction: recent concepts in diagnosis, mechanisms and management. Heart 2022; 108: 1342–1350. doi: 10.1136/heartjnl-2021-319605 [DOI] [PubMed] [Google Scholar]
- 16.Tromp J, van der Meer P, Tay WT, et al. Diagnostic accuracy of the electrocardiogram for heart failure with reduced or preserved ejection fraction. J Card Fail 2023; 29: 1104–1106. doi: 10.1016/j.cardfail.2023.03.014 [DOI] [PubMed] [Google Scholar]
- 17.Borlaug BA, Sharma K, Shah SJ, et al. Heart failure with preserved ejection fraction: JACC scientific statement. J Am Coll Cardiol 2023; 81: 1810–1834. doi: 10.1016/j.jacc.2023.01.049 [DOI] [PubMed] [Google Scholar]
- 18.Groenewegen A, Rutten FH, Mosterd A, et al. Epidemiology of heart failure. Eur J Heart Fail 2020; 22: 1342–1356. doi: 10.1002/ejhf.1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dewan P, Jackson A, Lam CSP, et al. Interactions between left ventricular ejection fraction, sex and effect of neurohumoral modulators in heart failure. Eur J Heart Fail 2020; 22: 898–901. doi: 10.1002/ejhf.1776 [DOI] [PubMed] [Google Scholar]
- 20.Cleland JGF, Bunting KV, Flather MD, et al. Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. Eur Heart J 2018; 39: 26–35. doi: 10.1093/eurheartj/ehx564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cao JY, Wales KM, Cordina R, et al. Pulmonary vasodilator therapies are of no benefit in pulmonary hypertension due to left heart disease: a meta-analysis. Int J Cardiol 2018; 273: 213–220. doi: 10.1016/j.ijcard.2018.09.043 [DOI] [PubMed] [Google Scholar]
- 22.Chiba Y, Iwano H, Murayama M, et al. Presence and relevance of midsystolic notching on right ventricular outflow tract flow velocity envelopes in pulmonary hypertension due to heart failure. J Am Soc Echocardiogr 2021; 34: 690–692.e1. doi: 10.1016/j.echo.2020.12.018 [DOI] [PubMed] [Google Scholar]
- 23.Arkles JS, Opotowsky AR, Ojeda J, et al. Shape of the right ventricular Doppler envelope predicts hemodynamics and right heart function in pulmonary hypertension. Am J Respir Crit Care Med 2011; 183: 268–276. doi: 10.1164/rccm.201004-0601OC [DOI] [PubMed] [Google Scholar]
- 24.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015; 16: 233–270. doi: 10.1093/ehjci/jev014 [DOI] [PubMed] [Google Scholar]
- 25.Voigt JU, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 2015; 16: 1–11. doi: 10.1093/ehjci/jeu184 [DOI] [PubMed] [Google Scholar]
- 26.Mor-Avi V, Lang RM, Badano LP, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Eur J Echocardiogr 2011; 12: 167–205. doi: 10.1093/ejechocard/jer021 [DOI] [PubMed] [Google Scholar]
- 27.Russo C, Jin Z, Elkind MS, et al. Prevalence and prognostic value of subclinical left ventricular systolic dysfunction by global longitudinal strain in a community-based cohort. Eur J Heart Fail 2014; 16: 1301–1309. doi: 10.1002/ejhf.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2016; 17: 1321–1360. doi: 10.1093/ehjci/jew082 [DOI] [PubMed] [Google Scholar]
- 29.Pieske B, Tschope C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J 2019; 40: 3297–3317. doi: 10.1093/eurheartj/ehz641 [DOI] [PubMed] [Google Scholar]
- 30.Reddy YNV, Carter RE, Obokata M, et al. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation 2018; 138: 861–870. doi: 10.1161/CIRCULATIONAHA.118.034646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reddy YNV, Kaye DM, Handoko ML, et al. Diagnosis of heart failure with preserved ejection fraction among patients with unexplained dyspnea. JAMA Cardiol 2022; 7: 891–899. doi: 10.1001/jamacardio.2022.1916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomas L, Marwick TH, Popescu BA, et al. Left atrial structure and function, and left ventricular diastolic dysfunction: JACC state-of-the-art review. J Am Coll Cardiol 2019; 73: 1961–1977. doi: 10.1016/j.jacc.2019.01.059 [DOI] [PubMed] [Google Scholar]
- 33.Mathari SE, Kluin J, Hopman L, et al. The role and implications of left atrial fibrosis in surgical mitral valve repair as assessed by CMR: the ALIVE study design and rationale. Front Cardiovasc Med 2023; 10: 1166703. doi: 10.3389/fcvm.2023.1166703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reddy YNV, Obokata M, Verbrugge FH, et al. Atrial dysfunction in patients with heart failure with preserved ejection fraction and atrial fibrillation. J Am Coll Cardiol 2020; 76: 1051–1064. doi: 10.1016/j.jacc.2020.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goette A, Kalman JM, Aguinaga L, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Europace 2016; 18: 1455–1490. doi: 10.1093/europace/euw161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gard EK, Beale AL, Telles F, et al. Left atrial enlargement is associated with pulmonary vascular disease in heart failure with preserved ejection fraction. Eur J Heart Fail 2023; 25: 806–814. doi: 10.1002/ejhf.2805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin K, Sarnari R, Pathrose A, et al. Cine MRI characterizes HfpEF and HfrEF in post-capillary pulmonary hypertension. Eur J Radiol 2021; 139: 109679. doi: 10.1016/j.ejrad.2021.109679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Wezenbeek J, Kianzad A, van de Bovenkamp A, et al. Right ventricular and right atrial function are less compromised in pulmonary hypertension secondary to heart failure with preserved ejection fraction: a comparison with pulmonary arterial hypertension with similar pressure overload. Circ Heart Fail 2022; 15: e008726. doi: 10.1161/CIRCHEARTFAILURE.121.008726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johns CS, Wild JM, Rajaram S, et al. Identifying at-risk patients with combined pre- and postcapillary pulmonary hypertension using interventricular septal angle at cardiac MRI. Radiology 2018; 289: 61–68. doi: 10.1148/radiol.2018180120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Robinson AA, Chow K, Salerno M. Myocardial T1 and ECV measurement: underlying concepts and technical considerations. JACC Cardiovasc Imaging 2019; 12: 2332–2344. doi: 10.1016/j.jcmg.2019.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brown LAE, Wahab A, Ikongo E, et al. Cardiovascular magnetic resonance phenotyping of heart failure with mildly reduced ejection fraction. Eur Heart J Cardiovasc Imaging 2022; 24: 38–45. doi: 10.1093/ehjci/jeac204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Messroghli DR, Moon JC, Ferreira VM, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson 2017; 19: 75. doi: 10.1186/s12968-017-0389-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Edelman RR. Contrast-enhanced MR imaging of the heart: overview of the literature. Radiology 2004; 232: 653–668. doi: 10.1148/radiol.2323031558 [DOI] [PubMed] [Google Scholar]
- 44.Aidi HE, Adams A, Moons KG, et al. Cardiac magnetic resonance imaging findings and the risk of cardiovascular events in patients with recent myocardial infarction or suspected or known coronary artery disease: a systematic review of prognostic studies. J Am Coll Cardiol 2014; 63: 1031–1045. doi: 10.1016/j.jacc.2013.11.048 [DOI] [PubMed] [Google Scholar]
- 45.Mather AN, Lockie T, Nagel E, et al. Appearance of microvascular obstruction on high resolution first-pass perfusion, early and late gadolinium enhancement CMR in patients with acute myocardial infarction. J Cardiovasc Magn Reson 2009; 11: 33. doi: 10.1186/1532-429X-11-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garcia MJ, Kwong RY, Scherrer-Crosbie M, et al. State of the art: imaging for myocardial viability: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging 2020; 13: e000053. doi: 10.1161/HCI.0000000000000053 [DOI] [PubMed] [Google Scholar]
- 47.Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 2000; 343: 1445–1453. doi: 10.1056/NEJM200011163432003 [DOI] [PubMed] [Google Scholar]
- 48.Patel RB, Li E, Benefield BC, et al. Diffuse right ventricular fibrosis in heart failure with preserved ejection fraction and pulmonary hypertension. ESC Heart Fail 2020; 7: 253–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Naeije R, Badagliacca R. The overloaded right heart and ventricular interdependence. Cardiovasc Res 2017; 113: 1474–1485. doi: 10.1093/cvr/cvx160 [DOI] [PubMed] [Google Scholar]
- 50.Aschauer S, Kammerlander AA, Zotter-Tufaro C, et al. The right heart in heart failure with preserved ejection fraction: insights from cardiac magnetic resonance imaging and invasive haemodynamics. Eur J Heart Fail 2016; 18: 71–80. doi: 10.1002/ejhf.418 [DOI] [PubMed] [Google Scholar]
- 51.Meyer P, Filippatos GS, Ahmed MI, et al. Effects of right ventricular ejection fraction on outcomes in chronic systolic heart failure. Circulation 2010; 121: 252–258. doi: 10.1161/CIRCULATIONAHA.109.887570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gorter TM, van Veldhuisen DJ, Voors AA, et al. Right ventricular–vascular coupling in heart failure with preserved ejection fraction and pre- vs. post-capillary pulmonary hypertension. Eur Heart J Cardiovasc Imaging 2018; 19: 425–432. doi: 10.1093/ehjci/jex133 [DOI] [PubMed] [Google Scholar]
- 53.Gulati A, Ismail TF, Jabbour A, et al. The prevalence and prognostic significance of right ventricular systolic dysfunction in nonischemic dilated cardiomyopathy. Circulation 2013; 128: 1623–1633. doi: 10.1161/CIRCULATIONAHA.113.002518 [DOI] [PubMed] [Google Scholar]
- 54.Larose E, Ganz P, Reynolds HG, et al. Right ventricular dysfunction assessed by cardiovascular magnetic resonance imaging predicts poor prognosis late after myocardial infarction. J Am Coll Cardiol 2007; 49: 855–862. doi: 10.1016/j.jacc.2006.10.056 [DOI] [PubMed] [Google Scholar]
- 55.Bosch L, Lam CSP, Gong L, et al. Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur J Heart Fail 2017; 19: 1664–1671. doi: 10.1002/ejhf.873 [DOI] [PubMed] [Google Scholar]
- 56.Ghio S, Guazzi M, Scardovi AB, et al. Different correlates but similar prognostic implications for right ventricular dysfunction in heart failure patients with reduced or preserved ejection fraction. Eur J Heart Fail 2017; 19: 873–879. doi: 10.1002/ejhf.664 [DOI] [PubMed] [Google Scholar]
- 57.Garcia-Martin A, Moya-Mur JL, Carbonell-San Roman SA, et al. Four chamber right ventricular longitudinal strain versus right free wall longitudinal strain. Prognostic value in patients with left heart disease. Cardiol J 2016; 23: 189–194. doi: 10.5603/CJ.a2015.0079 [DOI] [PubMed] [Google Scholar]
- 58.Cameli M, Bernazzali S, Lisi M, et al. Right ventricular longitudinal strain and right ventricular stroke work index in patients with severe heart failure: left ventricular assist device suitability for transplant candidates. Transplant Proc 2012; 44: 2013–2015. doi: 10.1016/j.transproceed.2012.06.018 [DOI] [PubMed] [Google Scholar]
- 59.Swift AJ, Rajaram S, Capener D, et al. LGE patterns in pulmonary hypertension do not impact overall mortality. JACC Cardiovasc Imaging 2014; 7: 1209–1217. doi: 10.1016/j.jcmg.2014.08.014 [DOI] [PubMed] [Google Scholar]
- 60.Freed BH, Gomberg-Maitland M, Chandra S, et al. Late gadolinium enhancement cardiovascular magnetic resonance predicts clinical worsening in patients with pulmonary hypertension. J Cardiovasc Magn Reson 2012; 14: 11. doi: 10.1186/1532-429X-14-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fayyaz AU, Edwards WD, Maleszewski JJ, et al. Global pulmonary vascular remodeling in pulmonary hypertension associated with heart failure and preserved or reduced ejection fraction. Circulation 2018; 137: 1796–1810. doi: 10.1161/CIRCULATIONAHA.117.031608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hunt JM, Bethea B, Liu X, et al. Pulmonary veins in the normal lung and pulmonary hypertension due to left heart disease. Am J Physiol Lung Cell Mol Physiol 2013; 305: L725–L736. doi: 10.1152/ajplung.00186.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Delgado JF, Conde E, Sanchez V, et al. Pulmonary vascular remodeling in pulmonary hypertension due to chronic heart failure. Eur J Heart Fail 2005; 7: 1011–1016. doi: 10.1016/j.ejheart.2004.10.021 [DOI] [PubMed] [Google Scholar]
- 64.Ghigna M-R, Dorfmüller P. Pulmonary vascular disease and pulmonary hypertension. Diagnostic Histopathology 2019; 25: 304–312. doi: 10.1016/j.mpdhp.2019.05.002 [DOI] [Google Scholar]
- 65.Wagenvoort CA. Lung biopsy specimens in the evaluation of pulmonary vascular disease. Chest 1980; 77: 614–625. doi: 10.1378/chest.77.5.614 [DOI] [PubMed] [Google Scholar]
- 66.Wagenvoort CA. Morphological substrate for the reversibility and irreversibility of pulmonary hypertension. Eur Heart J 1988; 9: Suppl. J, 7–12. doi: 10.1093/eurheartj/9.suppl_J.7 [DOI] [PubMed] [Google Scholar]
- 67.West JB, Mathieu-Costello O. Vulnerability of pulmonary capillaries in heart disease. Circulation 1995; 92: 622–631. doi: 10.1161/01.CIR.92.3.622 [DOI] [PubMed] [Google Scholar]
- 68.Guazzi M, Naeije R. Pulmonary hypertension in heart failure: pathophysiology, pathobiology, and emerging clinical perspectives. J Am Coll Cardiol 2017; 69: 1718–1734. doi: 10.1016/j.jacc.2017.01.051 [DOI] [PubMed] [Google Scholar]
- 69.Pasca I, Dang P, Tyagi G, et al. Survival in patients with degenerative mitral stenosis: results from a large retrospective cohort study. J Am Soc Echocardiogr 2016; 29: 461–469. doi: 10.1016/j.echo.2015.12.012 [DOI] [PubMed] [Google Scholar]
- 70.Weitsman T, Weisz G, Farkash R, et al. Pulmonary hypertension with left heart disease: prevalence, temporal shifts in etiologies and outcome. Am J Med 2017; 130: 1272–1279. doi: 10.1016/j.amjmed.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 71.Ghoreishi M, Evans CF, DeFilippi CR, et al. Pulmonary hypertension adversely affects short- and long-term survival after mitral valve operation for mitral regurgitation: implications for timing of surgery. J Thorac Cardiovasc Surg 2011; 142: 1439–1452. doi: 10.1016/j.jtcvs.2011.08.030 [DOI] [PubMed] [Google Scholar]
- 72.Le Tourneau T, Richardson M, Juthier F, et al. Echocardiography predictors and prognostic value of pulmonary artery systolic pressure in chronic organic mitral regurgitation. Heart 2010; 96: 1311–1317. doi: 10.1136/hrt.2009.186486 [DOI] [PubMed] [Google Scholar]
- 73.Magne J, Lancellotti P, Pierard LA. Exercise pulmonary hypertension in asymptomatic degenerative mitral regurgitation. Circulation 2010; 122: 33–41. doi: 10.1161/CIRCULATIONAHA.110.938241 [DOI] [PubMed] [Google Scholar]
- 74.Mentias A, Patel K, Patel H, et al. Effect of pulmonary vascular pressures on long-term outcome in patients with primary mitral regurgitation. J Am Coll Cardiol 2016; 67: 2952–2961. doi: 10.1016/j.jacc.2016.03.589 [DOI] [PubMed] [Google Scholar]
- 75.Ratwatte S, Stewart S, Strange G, et al. Prevalence of pulmonary hypertension in aortic stenosis and its influence on outcomes. Heart 2023; 109: 1319–1326. doi: 10.1136/heartjnl-2022-322184 [DOI] [PubMed] [Google Scholar]
- 76.Masri A, Abdelkarim I, Sharbaugh MS, et al. Outcomes of persistent pulmonary hypertension following transcatheter aortic valve replacement. Heart 2018; 104: 821–827. doi: 10.1136/heartjnl-2017-311978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Malouf JF, Enriquez-Sarano M, Pellikka PA, et al. Severe pulmonary hypertension in patients with severe aortic valve stenosis: clinical profile and prognostic implications. J Am Coll Cardiol 2002; 40: 789–795. doi: 10.1016/S0735-1097(02)02002-8 [DOI] [PubMed] [Google Scholar]
- 78.Weber L, Rickli H, Haager PK, et al. Haemodynamic mechanisms and long-term prognostic impact of pulmonary hypertension in patients with severe aortic stenosis undergoing valve replacement. Eur J Heart Fail 2019; 21: 172–181. doi: 10.1002/ejhf.1322 [DOI] [PubMed] [Google Scholar]
- 79.Ratwatte S, Playford D, Stewart S, et al. Prevalence of pulmonary hypertension in aortic regurgitation and its influence on outcomes. Heart 2023; 109: 1310–1318. doi: 10.1136/heartjnl-2022-322187 [DOI] [PubMed] [Google Scholar]
- 80.Khandhar S, Varadarajan P, Turk R, et al. Survival benefit of aortic valve replacement in patients with severe aortic regurgitation and pulmonary hypertension. Ann Thorac Surg 2009; 88: 752–756. doi: 10.1016/j.athoracsur.2009.05.025 [DOI] [PubMed] [Google Scholar]
- 81.Sultan I, Fukui M, Bianco V, et al. Impact of combined pre and postcapillary pulmonary hypertension on survival after transcatheter aortic valve implantation. Am J Cardiol 2020; 131: 60–66. doi: 10.1016/j.amjcard.2020.06.037 [DOI] [PubMed] [Google Scholar]
- 82.Martinez C, Tsugu T, Sugimoto T, et al. Pulmonary hypertension with valvular heart disease: when to treat the valve disease and when to treat the pulmonary hypertension. Curr Cardiol Rep 2019; 21: 151. doi: 10.1007/s11886-019-1240-7 [DOI] [PubMed] [Google Scholar]
- 83.Maeder MT, Weber L, Buser M, et al. Pulmonary hypertension in aortic and mitral valve disease. Front Cardiovasc Med 2018; 5: 40. doi: 10.3389/fcvm.2018.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Magne J, Pibarot P, Sengupta PP, et al. Pulmonary hypertension in valvular disease: a comprehensive review on pathophysiology to therapy from the HAVEC Group. JACC Cardiovasc Imaging 2015; 8: 83–99. doi: 10.1016/j.jcmg.2014.12.003 [DOI] [PubMed] [Google Scholar]
- 85.Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 2022; 43: 561–632. doi: 10.1093/eurheartj/ehab395 [DOI] [PubMed] [Google Scholar]
- 86.Barbieri A, Bursi F, Grigioni F, et al. Prognostic and therapeutic implications of pulmonary hypertension complicating degenerative mitral regurgitation due to flail leaflet: a multicenter long-term international study. Eur Heart J 2011; 32: 751–759. doi: 10.1093/eurheartj/ehq294 [DOI] [PubMed] [Google Scholar]
- 87.Zener JC, Hancock EW, Shumway NE, et al. Regression of extreme pulmonary hypertension after mitral valve surgery. Am J Cardiol 1972; 30: 820–826. doi: 10.1016/0002-9149(72)90005-7 [DOI] [PubMed] [Google Scholar]
- 88.Pai RG, Varadarajan P, Kapoor N, et al. Aortic valve replacement improves survival in severe aortic stenosis associated with severe pulmonary hypertension. Ann Thorac Surg 2007; 84: 80–85. doi: 10.1016/j.athoracsur.2007.02.094 [DOI] [PubMed] [Google Scholar]
- 89.Lancellotti P, Tribouilloy C, Hagendorff A, et al. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2013; 14: 611–644. doi: 10.1093/ehjci/jet105 [DOI] [PubMed] [Google Scholar]
- 90.Le Tourneau T, Deswarte G, Lamblin N, et al. Right ventricular systolic function in organic mitral regurgitation: impact of biventricular impairment. Circulation 2013; 127: 1597–1608. doi: 10.1161/CIRCULATIONAHA.112.000999 [DOI] [PubMed] [Google Scholar]
- 91.Sinning JM, Hammerstingl C, Chin D, et al. Decrease of pulmonary hypertension impacts on prognosis after transcatheter aortic valve replacement. EuroIntervention 2014; 9: 1042–1049. doi: 10.4244/EIJV9I9A177 [DOI] [PubMed] [Google Scholar]
- 92.Bishu K, Suri RM, Nkomo VT, et al. Prognostic impact of pulmonary artery systolic pressure in patients undergoing transcatheter aortic valve replacement for aortic stenosis. Am J Cardiol 2014; 114: 1562–1567. doi: 10.1016/j.amjcard.2014.08.019 [DOI] [PubMed] [Google Scholar]
- 93.Gatehouse PD, Keegan J, Crowe LA, et al. Applications of phase-contrast flow and velocity imaging in cardiovascular MRI. Eur Radiol 2005; 15: 2172–2184. doi: 10.1007/s00330-005-2829-3 [DOI] [PubMed] [Google Scholar]
- 94.Ajmone Marsan N, Delgado V, Shah DJ, et al. Valvular heart disease: shifting the focus to the myocardium. Eur Heart J 2023; 44: 28–40. doi: 10.1093/eurheartj/ehac504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Basso C, Perazzolo Marra M, Rizzo S, et al. Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation 2015; 132: 556–566. doi: 10.1161/CIRCULATIONAHA.115.016291 [DOI] [PubMed] [Google Scholar]
- 96.Liu B, Neil DAH, Bhabra M, et al. Reverse myocardial remodeling following valve repair in patients with chronic severe primary degenerative mitral regurgitation. JACC Cardiovasc Imaging 2022; 15: 224–236. doi: 10.1016/j.jcmg.2021.07.007 [DOI] [PubMed] [Google Scholar]
- 97.Everett RJ, Tastet L, Clavel MA, et al. Progression of hypertrophy and myocardial fibrosis in aortic stenosis: a multicenter cardiac magnetic resonance study. Circ Cardiovasc Imaging 2018; 11: e007451. doi: 10.1161/CIRCIMAGING.117.007451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gumauskiene B, Drebickaite E, Pangonyte D, et al. The association of left ventricular histologically verified myocardial fibrosis with pulmonary hypertension in severe aortic stenosis. Perfusion 2023; 38: 165–171. doi: 10.1177/02676591211042733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Goodale F Jr, Sanchez G, Friedlich AL, et al. Correlation of pulmonary arteriolar resistance with pulmonary vascular changes in patients with mitral stenosis before and after valvulotomy. N Engl J Med 1955; 252: 979–983. doi: 10.1056/NEJM195506092522303 [DOI] [PubMed] [Google Scholar]
- 100.Tandon HD, Kasturi J. Pulmonary vascular changes associated with isolated mitral stenosis in India. Br Heart J 1975; 37: 26–36. doi: 10.1136/hrt.37.1.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Evans W, Short DS. Pulmonary hypertension in mitral stenosis. Br Heart J 1957; 19: 457–472. doi: 10.1136/hrt.19.4.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Robalino BD, Moodie DS. Primary pulmonary hypertension, then and now: 28 years of experience. Cleve Clin J Med 1992; 59: 411–417. doi: 10.3949/ccjm.59.4.411 [DOI] [PubMed] [Google Scholar]
- 103.Hoeper MM, Pausch C, Grunig E, et al. Idiopathic pulmonary arterial hypertension phenotypes determined by cluster analysis from the COMPERA registry. J Heart Lung Transplant 2020; 39: 1435–1444. doi: 10.1016/j.healun.2020.09.011 [DOI] [PubMed] [Google Scholar]
- 104.Hoeper MM, Huscher D, Ghofrani HA, et al. Elderly patients diagnosed with idiopathic pulmonary arterial hypertension: results from the COMPERA registry. Int J Cardiol 2013; 168: 871–880. doi: 10.1016/j.ijcard.2012.10.026 [DOI] [PubMed] [Google Scholar]
- 105.Badesch DB, Raskob GE, Elliott CG, et al. Pulmonary arterial hypertension: baseline characteristics from the REVEAL Registry. Chest 2010; 137: 376–387. doi: 10.1378/chest.09-1140 [DOI] [PubMed] [Google Scholar]
- 106.Trip P, Nossent EJ, de Man FS, et al. Severely reduced diffusion capacity in idiopathic pulmonary arterial hypertension: patient characteristics and treatment responses. Eur Respir J 2013; 42: 1575–1585. doi: 10.1183/09031936.00184412 [DOI] [PubMed] [Google Scholar]
- 107.Olsson KM, Fuge J, Meyer K, et al. More on idiopathic pulmonary arterial hypertension with a low diffusing capacity. Eur Respir J 2017; 50: 1700354. doi: 10.1183/13993003.00354-2017 [DOI] [PubMed] [Google Scholar]
- 108.Opitz CF, Hoeper MM, Gibbs JS, et al. Pre-capillary, combined, and post-capillary pulmonary hypertension: a pathophysiological continuum. J Am Coll Cardiol 2016; 68: 368–378. doi: 10.1016/j.jacc.2016.05.047 [DOI] [PubMed] [Google Scholar]
- 109.Hemnes AR, Leopold JA, Radeva MK, et al. Clinical characteristics and transplant-free survival across the spectrum of pulmonary vascular disease. J Am Coll Cardiol 2022; 80: 697–718. doi: 10.1016/j.jacc.2022.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Haque AK, Gadre S, Taylor J, et al. Pulmonary and cardiovascular complications of obesity: an autopsy study of 76 obese subjects. Arch Pathol Lab Med 2008; 132: 1397–1404. doi: 10.5858/2008-132-1397-PACCOO [DOI] [PubMed] [Google Scholar]
- 111.Ahmed Q, Chung-Park M, Tomashefski JF Jr. Cardiopulmonary pathology in patients with sleep apnea/obesity hypoventilation syndrome. Hum Pathol 1997; 28: 264–269. doi: 10.1016/S0046-8177(97)90122-2 [DOI] [PubMed] [Google Scholar]
- 112.van de Bovenkamp AA, Wijkstra N, Oosterveer FPT, et al. The value of passive leg raise during right heart catheterization in diagnosing heart failure with preserved ejection fraction. Circ Heart Fail 2022; 15: e008935. doi: 10.1161/CIRCHEARTFAILURE.121.008935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Badagliacca R, D'Alto M, Ghio S, et al. Relevance of comorbidities on initial combination therapy in pulmonary arterial hypertension. ERJ Open Res 2022; 8: 00298-2022. doi: 10.1183/23120541.00298-2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.McLaughlin VV, Vachiery JL, Oudiz RJ, et al. Patients with pulmonary arterial hypertension with and without cardiovascular risk factors: results from the AMBITION trial. J Heart Lung Transplant 2019; 38: 1286–1295. doi: 10.1016/j.healun.2019.09.010 [DOI] [PubMed] [Google Scholar]