Abstract
This comprehensive case report documents the treatment of a 37-year-old female patient who presented with anterior ST-elevation myocardial infarction (STEMI). The patient underwent percutaneous coronary intervention (PCI), followed by an innovative therapy - optimized supersaturated oxygen therapy (SSO2). This therapy was chosen due to its potential to enhance myocardial salvage, particularly in severe MI cases like the patient. The report meticulously details the patient's clinical course, including the diagnostic procedures and the rationale behind opting for SSO2 therapy. It highlights the significant improvements observed post-therapy: enhanced left ventricular (LV) function and a remarkable reduction in the size of the LV apical aneurysm. These outcomes suggest a direct benefit of SSO2 in reducing myocardial damage. Finally, the report discusses the broader implications of these findings. It underscores the potential of optimized SSO2 therapy in clinical settings, particularly for patients with anterior MI. The case exemplifies how advanced therapeutic interventions like SSO2 can play a pivotal role in improving clinical outcomes post-MI, thereby advocating for its consideration in similar clinical scenarios.
Keywords: st-elevation myocardial infarction (stemi), supersaturated oxygen therapy (sso2), infarct size reduction, post-pci for lad stemi, primary percutaneous coronary intervention (pci)
Introduction
For nearly three decades, the gold standard treatment for acute myocardial infarction (AMI) has been urgent revascularization, also known as primary percutaneous coronary intervention (PCI) [1]. When compared to conservative therapy, which includes thrombolysis, it reduces mortality and enhances cardiovascular outcomes [2]. One important factor influencing hospitalization for heart failure and one-year all-cause mortality is infarct size. In primary PCI, optimizing myocardial salvage and decreasing infarct size to minimize post-MI sequelae of heart failure and mortality continues to be a crucial objective [1,2]. Despite high rates of epicardial coronary flow restoration by PCI, myocardial salvage is frequently suboptimal in ST-elevation myocardial infarction (STEMI), even though early reperfusion therapy has decreased mortality over the past few decades [3]. Numerous mechanisms, including reperfusion injury, microcirculatory dysfunction or no-reflow, and late reperfusion, have been linked to this [4].
Supersaturated oxygen therapy (SSO2) infused into the left anterior descending coronary artery (LAD) was used to treat patients with anterior STEMI in the pivotal Acute Myocardial Infarction With Hyperoxemic Therapy II (AMIHOT II) trial. The results showed a significant reduction in infarct size at 14 days when compared with the control group [5]. However, because the SSO2 group required larger or more femoral arterial sheaths, hemorrhagic complications were more common. In addition, nonsignificant trends were observed for increased stent thrombosis and death at 30 days, which may have been caused by the SSO2 being delivered through an indwelling catheter in the stented area of the LAD [6].
This led to a modification of the intracoronary SSO2 delivery technique, resulting in "optimized" SSO2 delivery whereby, after PCI, hyperoxemic blood was infused into the left main coronary artery (LMCA) ostium via a diagnostic catheter. One of the systems that can provide optimized SSO2 therapy is ZOLL TherOx (ZOLL Medical Corporation, USA). We are presenting the case of a 37-year-old female patient who received SSO2 therapy following PCI for LAD STEMI.
Case presentation
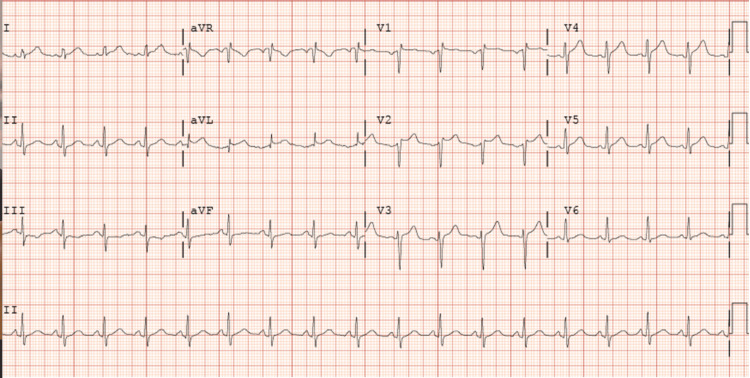
A 37-year-old female with a past medical history significant for nicotine dependence and uncontrolled diabetes presented to the emergency room with the chief complaint of chest pain. She described her chest pain as constant, severe, retrosternal, and radiating to her neck, which started around 40 minutes before presenting to the ER with no apparent aggravating or relieving factors. The pain was also associated with shortness of breath, nausea, and vomiting. In the emergency department, she was found to have dynamic EKG changes concerning for anterior STEMI (Figure 1).
Figure 1. EKG showed ST elevation in leads V2, V3, and V4 correlating with anterior STEMI with reciprocal changes in the inferior leads III and aVF.
EKG: electrocardiogram, STEMI: ST-elevation myocardial infarction, aVF: arteriovenous fistula
The patient was taken emergently to the cath lab. Catheterization was done after around 67 minutes from the onset of chest pain and revealed a thrombus in her LAD artery along with left ventricular (LV) dysfunction (Figure 2A). After reviewing the angiographic data, we proceeded with percutaneous transluminal coronary angioplasty (PTCA), primary PCI, and aspiration thrombectomy to the LAD artery (Figure 2B).
Figure 2. (A) A thrombus in her left anterior descending artery. (B) Same lesion after PTCA, primary PCI, and aspiration thrombectomy to the left anterior descending artery.
PTCA: percutaneous transluminal coronary angioplasty, PCI: percutaneous coronary intervention
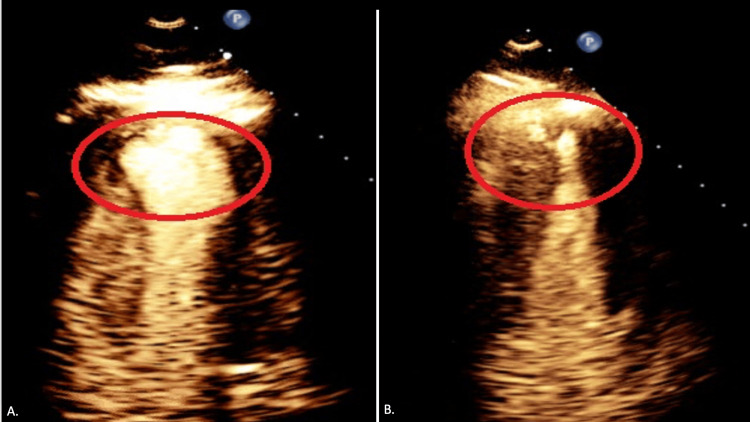
After successfully treating the culprit lesion, we decided to proceed with SSO2 TherOx treatment for anterior STEMI. Right femoral access was obtained, and a 6 French sheath was placed. We then used the JL 4.0 catheter and engaged the left coronary system. The sheath was sutured in place. The TherOx system blood draw line was connected to the sheath, and re-infusion was done from the JL 4.0 catheter that was left in place to infuse supersaturated oxygen into the left coronary system for a total of 60 minutes. Initial EKG revealed hypokinetic apical and apical septal LV segment. There was a 3 cm-wide apical ballooning (Figure 3A). The LV ejection fraction was estimated to be 50%. The rest of her hospital stay was uneventful. The patient was started on goal-directed medical therapy for coronary artery disease. The patient was discharged with a one-month follow-up from the hospital.
Figure 3. A. Aneurysmal dilation of the LV apex post-procedure (red oval). B. LV aneurysm that became smaller at one-month follow-up (red oval).
LV: left ventricular
On follow-up, the patient did not have any complaints. She had a repeat EKG, which showed that she only had a small remnant LV ballooning (Figure 3B). It measured 1.8 cm wide, a biplane LV ejection fraction of 59.8%, and recovery of the apical septal hypokinesia.
Discussion
Several pharmacologic techniques, such as intracoronary adenosine, nitroprusside, and abciximab infusions [7], have been used in the past to enhance microcirculatory function, avoid reperfusion injury, and decrease infarct size in patients with STEMI [8]. Nevertheless, there is no evidence that any of these therapies enhance clinical results. In patients with large anterior STEMI, the intracoronary delivery of SSO2 significantly decreased infarct size following primary PCI, a parameter strongly predictive of subsequent death and heart failure rehospitalizations [9]. Thus, SSO2 became the first medication to be shown to improve myocardial salvage and decrease infarct size in a pivotal, suitably powered, randomized trial [5,6,9].
SSO2 therapy proved safe and feasible for treating acute anterior STEMI in humans undergoing primary PCI. Larger clinical trials that can directly show a reduction in major adverse cardiovascular events are still lacking, but data from nearly 360 patients suggest that treating anterior STEMI within six hours of the onset of symptoms may be able to reduce infarct size. According to aggregate data from AMIHOT I, AMIHOT II, and IC-HOT, SSO2 therapy may help the infarct size of those patients decrease from roughly 25% to 27% of the LV to roughly 19% [5,6,10].
Although the primary composite safety endpoint of the AMIHOT II trial was met, bleeding complications were more common. In patients treated with SSO2, there were indications of increased 30-day rates of myocardial rupture, stent thrombosis, and mortality [9]. In the IC-HOT study, SSO2 delivery was "optimized" to be selectively infused to the origin of the left main coronary artery instead of the LAD at the stent site due to these concerns [11]. The IC-HOT study was an open-label, single-arm, prospective investigation. This instance demonstrates how SSO2 therapy helps patients. In the beginning, the patient had a sizable LV ballooning and mild LV dysfunction. Subsequent surveillance echocardiography, however, revealed improved LV function and a 1.8 cm versus 3.0 cm reduction in the size of the LV apical ballooning. In light of the results of this case, we recommend SSO2 therapy for patients suffering from LAD STEMI.
It will be interesting to observe in the future if the patient benefits more from a combination of different strategies for reducing infarct size in addition to primary PCI. However, for this to work, each of the individual interventions must be beneficial on its own. Appropriate clinical trials are either in the planning stages or currently underway [12].
Conclusions
In addition to primary PCI, SSO2 therapy is a newly available treatment option for patients with anterior STEMI. The IC-HOT trial was the only one used to assess the effectiveness of the "optimized" SSO2 therapy; however, it was constrained by its single-arm, open-ended design. Therefore, additional clinical research is required to examine the practical effects of "optimized" SSO2 therapy. In this instance, we offer a very positive result for a patient who received "optimized SSO2 therapy."
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Shaden Daloub, Mohamed Suliman, Rameez Sayyed, Kamran Zaheer, Kanaan Mansoor
Acquisition, analysis, or interpretation of data: Shaden Daloub, Mohamed Suliman, Kamran Zaheer, Kanaan Mansoor
Drafting of the manuscript: Shaden Daloub, Mohamed Suliman, Kamran Zaheer, Kanaan Mansoor
Critical review of the manuscript for important intellectual content: Shaden Daloub, Mohamed Suliman, Rameez Sayyed, Kamran Zaheer, Kanaan Mansoor
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Novel therapeutic strategies to reduce reperfusion injury after acute myocardial infarction. Schäfer A, König T, Bauersachs J, Akin M. Curr Probl Cardiol. 2022;47 doi: 10.1016/j.cpcardiol.2022.101398. [DOI] [PubMed] [Google Scholar]
- 2.One-year outcomes of supersaturated oxygen therapy in acute anterior myocardial infarction: the IC-HOT study. Chen S, David SW, Khan ZA, et al. Catheter Cardiovasc Interv. 2021;97:1120–1126. doi: 10.1002/ccd.29090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Left ventricular remodeling after primary coronary angioplasty: patterns of left ventricular dilation and long-term prognostic implications. Bolognese L, Neskovic AN, Parodi G, Cerisano G, Buonamici P, Santoro GM, Antoniucci D. Circulation. 2002;106:2351–2357. doi: 10.1161/01.cir.0000036014.90197.fa. [DOI] [PubMed] [Google Scholar]
- 4.Impact and determinants of left ventricular function in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction. Halkin A, Stone GW, Dixon SR, et al. Am J Cardiol. 2005;96:325–331. doi: 10.1016/j.amjcard.2005.03.069. [DOI] [PubMed] [Google Scholar]
- 5.Effect of supersaturated oxygen delivery on infarct size after percutaneous coronary intervention in acute myocardial infarction. Stone GW, Martin JL, de Boer MJ, et al. Circ Cardiovasc Interv. 2009;2:366–375. doi: 10.1161/CIRCINTERVENTIONS.108.840066. [DOI] [PubMed] [Google Scholar]
- 6.Evaluation of intracoronary hyperoxemic oxygen therapy in acute anterior myocardial infarction: the IC-HOT study. David SW, Khan ZA, Patel NC, et al. Catheter Cardiovasc Interv. 2019;93:882–890. doi: 10.1002/ccd.27905. [DOI] [PubMed] [Google Scholar]
- 7.Strategies to attenuate micro-vascular obstruction during P-PCI: the randomized reperfusion facilitated by local adjunctive therapy in ST-elevation myocardial infarction trial. Nazir SA, McCann GP, Greenwood JP, et al. Eur Heart J. 2016;37:1910–1919. doi: 10.1093/eurheartj/ehw136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Intracoronary compared with intravenous bolus abciximab application during primary percutaneous coronary intervention in ST-segment elevation myocardial infarction: cardiac magnetic resonance substudy of the AIDA STEMI trial. Eitel I, Wöhrle J, Suenkel H, et al. J Am Coll Cardiol. 2013;61:1447–1454. doi: 10.1016/j.jacc.2013.01.048. [DOI] [PubMed] [Google Scholar]
- 9.Relationship between infarct size and outcomes following primary PCI: patient‐level analysis from 10 randomized trials. Stone GW, Selker HP, Thiele H, et al. J Am Coll Cardiol. 2016;67:1674–1683. doi: 10.1016/j.jacc.2016.01.069. [DOI] [PubMed] [Google Scholar]
- 10.Acute Myocardial Infarction with Hyperoxemic Therapy (AMIHOT): a prospective, randomized trial of intracoronary hyperoxemic reperfusion after percutaneous coronary intervention. O'Neill WW, Martin JL, Dixon SR, et al. J Am Coll Cardiol. 2007;50:397–405. doi: 10.1016/j.jacc.2007.01.099. [DOI] [PubMed] [Google Scholar]
- 11.Update on cardioprotective strategies for STEMI: focus on supersaturated oxygen delivery. Kloner RA, Creech JL, Stone GW, O'Neill WW, Burkhoff D, Spears JR. JACC Basic Transl Sci. 2021;6:1021–1033. doi: 10.1016/j.jacbts.2021.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Left ventricular unloading using an Impella CP improves coronary flow and infarct zone perfusion in ischemic heart failure. Watanabe S, Fish K, Kovacic JC, et al. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.006462. [DOI] [PMC free article] [PubMed] [Google Scholar]