Abstract
Objectives
To investigate whether there is a window of opportunity for psoriatic arthritis (PsA) patients and to assess which patient characteristics are associated with a longer diagnostic delay.
Methods
All newly diagnosed, disease-modifying antirheumatic drug-naïve PsA patients who participated in the Dutch southwest Early PsA cohoRt and had ≥3 years of follow-up were studied. First, total delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist and then split into patient and physician delays. The total delay was categorised into short (<12 weeks), intermediate (12 weeks to 1 year) or long (>1 year). These groups were compared on clinical (Minimal Disease Activity (MDA) and Disease Activity index for PSoriatic Arthritis (DAPSA) remission) and patient-reported outcomes during 3 years follow-up.
Results
708 PsA patients were studied of whom 136 (19%), 237 (33%) and 335 (47%) had a short, intermediate and long total delay, respectively. Patient delay was 1.0 month and physician delay was 4.5 months. Patients with a short delay were more likely to achieve MDA (OR 2.55, p=0.003) and DAPSA remission (OR 2.35,p=0.004) compared with PsA patients with a long delay. Patient-reported outcomes showed numerical but non-significant differences between the short and long delay groups. Female patients and those presenting with enthesitis, chronic back pain or normal C-reactive protein (CRP) had a longer delay.
Conclusions
In PsA, referral and diagnosis within 1 year is associated with better clinical outcomes, suggesting the presence of a window of opportunity. The most gain in referral could be obtained in physician delay and in females, patients with enthesitis, chronic back pain or normal CRP.
Keywords: Patient Reported Outcome Measures; Arthritis, Psoriatic; Outcome Assessment, Health Care
WHAT IS ALREADY KNOWN ON THIS TOPIC
A diagnostic delay in patients with psoriatic arthritis (PsA) is associated with more joint erosions and functional impairment. However, it is unknown whether a ‘window of opportunity’, as defined by <12 weeks, exists in PsA.
WHAT THIS STUDY ADDS
Patients with PsA with a diagnostic delay of <1 year are more likely to achieve Disease Activity index for PSoriatic Arthritis remission and Minimal Disease Activity compared with those with a delay of >1 year.
PsA patients with a delay of <12 weeks have better outcomes in the first year than those with a delay of 12 weeks to 1 year, but this effect is not sustained over time.
Female sex, having enthesitis, chronic back pain and lower C-reactive protein levels are associated with a longer diagnostic delay.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This is the first study in PsA that explores timing of referral and diagnosis, which shows that there is a window of opportunity. However, the current data suggest the window of opportunity to be the first year rather than the first 12 weeks after symptom onset.
Introduction
Diagnosing psoriatic arthritis (PsA) can be challenging due to the heterogeneous nature of the disease. A meta-analysis of several psoriasis cohorts has shown that 15.5% of psoriasis patients have undiagnosed PsA.1 In addition, a diagnostic delay of 1–2 years is common in PsA.2 3 The reasons why cases of established PsA remain unidentified have not been elucidated, but possible causes are the absence of antibodies and the lack of musculoskeletal expertise regarding enthesitis and dactylitis among primary care physicians and treating dermatologists. This high prevalence of late and undiagnosed PsA is alarming because early diagnosis and treatment of PsA are likely to be beneficial for long-term patient outcomes.4
A few studies have investigated symptom duration or diagnostic delay in relation to treatment outcomes.2 3 5 One of them has shown that PsA patients with a diagnostic delay of >2 years have more joint damage than patients with a delay of <2 years.5 In addition, Tillett et al demonstrated that a diagnostic delay of >1 year is associated with poorer functional status.3 A shorter diagnostic delay of 6 months is associated with less radiological progression and functional impairment in the long term.2 These studies highlight the importance of prompt referral and treatment initiation.2
Treatment of PsA is aimed at achieving the lowest level of disease activity in all disease domains, to prevent structural damage and to optimise functional status.4 Two recommended treatment targets are remission, measured with the Disease Activity index for PSoriatic Arthritis (DAPSA) score, and Minimal Disease Activity (MDA), as they include different disease domains and are associated with long-term outcomes.6–10 Shortening the diagnostic delay is one of the potentially modifiable factors that can help achieve these treatment targets and thereby improve patient outcomes.
In rheumatoid arthritis (RA), the importance of prompt referral and treatment initiation after the onset of symptoms is well established. Starting treatment within the so-called ‘window of opportunity’, that is, within 12 weeks after symptom onset, results in higher remission rates, and less radiological progression and functional impairment.11–14 Whether a similar ‘window of opportunity’ exists in PsA is unclear.
Therefore, our aim is to first investigate whether a window of opportunity exists in PsA by comparing clinical (MDA and DAPSA) and patient-reported outcomes (PROs) in PsA patients with a short (<12 weeks), intermediate (12 weeks to 1 year) and long (>1 year) diagnostic delay. In addition, we examined which patient characteristics are associated with a longer diagnostic delay.
Methods
Patients
Disease-modifying antirheumatic drug (DMARD)-naïve, newly diagnosed PsA patients were included in the Dutch southwest Early Psoriatic Arthritis cohoRt (DEPAR) from August 2013 onwards. The PsA diagnosis was based on expert opinion of the rheumatologist. Written informed consent was obtained from all participants according to the declaration of Helsinki. Further details on the DEPAR study can be found elsewhere.15
For this analysis, data up to March 2023 were used from all consecutive patients who were included between 2013 and 2020 (n=720). For 708 (98%) of these PsA patients, diagnostic delay data were available.
Diagnostic delay
Total delay was calculated as the time period between symptom onset and PsA diagnosis made by a rheumatologist. Patients were categorised into three groups based on their total delay, namely (1) short delay of <12 weeks, (2) intermediate delay of 12 weeks to 1 year and (3) long delay of >1 year. There is no consensus yet on the definition of an early PsA patient.16 Therefore, the threshold for short delay was set equal to the ‘window of opportunity’ in RA, which is <12 weeks.11–13 The threshold between the intermediate and long delay groups was set at 1 year, which is based on previous literature, but it is also close to the median delay of our cohort.2 17 This ensured that there were enough patients in each group for valid comparisons. The total delay was studied at two levels. The first level is the ‘patient delay’, which consists of the time period between PsA-related symptoms onset and the first visit to the general practitioner (GP). The second level is the ‘physician delay’ that spans the period between the first assessment by the GP and the PsA diagnosis made by a rheumatologist. The total delay is the sum of patient and physician delay. In the Netherlands, the GP is the first contact point for patients with acute or chronic symptoms. Therefore, most patients were referred to a rheumatologist by their GP. However, some patients were referred by their dermatologist or another specialist, but those patients often also visited their GP for their PsA-related symptoms. For this reason, we did not distinguish between patients referred by their GP or by a specialist.
PsA phenotypes
We examined whether total delay differed between PsA phenotypes at diagnosis. The PsA phenotype categorisation, which is based on the predominant clinical symptoms, was done by the treating rheumatologist and includes monarthritis, oligoarthritis, polyarthritis, enthesitis, axial disease and dactylitis.
Data collection
Patients were assessed at 3-month intervals in the first year, 6-month intervals in the second year and each year thereafter. At baseline, data on diagnostic delay were collected through online questionnaires. Clinical outcomes, blood samples including C-reactive protein (CRP) and PROs were collected at each visit.
Clinical outcomes included swollen joint count (SJC 66), tender joint count (TJC 68), psoriasis (Body Surface Area; BSA), enthesitis (Leeds Enthesitis Index; LEI), dactylitis count and nail involvement.18 19
At each visit, patients filled out online questionnaires, capturing the following PROs: pain, general health, functional ability and disease impact. Pain and general health were measured on a 0–100 mm Visual Analogue Scale (VAS), where higher scores indicate poorer health status.20 The Health Assessment Questionnaire (HAQ) was used to measure functional ability.21 The HAQ consists of eight domains and the total score ranges from 0 to 3. Higher scores represent more functional impairment. Disease impact was measured with the Psoriatic Arthritis Impact of Disease (PsAID-12) questionnaire. The PsAID-12 measures 12 health domains concerning PsA-related symptoms, and physical and psychosocial difficulties that the patient experienced in the last week. Each domain is measured on a 0–10 Numeric Rating Scale. Using a formula, a sum score is calculated ranging from 0 to 10. Higher scores indicate a greater disease impact. A score <4 is considered to be an acceptable symptom state.22
Composite outcomes
Clinical outcomes and PROs were used to calculate the composite outcomes MDA and DAPSA. Patients were in MDA when they achieved ≥5 out of the following 7 criteria: TJC68 ≤1, SJC66 ≤1, BSA ≤3%, VAS pain ≤15 mm, VAS patient general health ≤20 mm, HAQ ≤0.5 and LEI ≤1.23 The DAPSA was calculated by taking the sum of TJC68, SJC66, CRP (mg/dL), general health (VAS divided by 10) and pain (VAS divided by 10). The DAPSA threshold for remission is ≤4.
Statistical analysis
Baseline characteristics of patients with a short, intermediate and long delay were compared using an analysis of variance, Kruskal-Wallis test or χ2 test, when appropriate. Patient and physician delay were compared using Wilcoxon’s signed-rank test.
Mixed effects logistic regression models were used to compare the proportion of patients reaching MDA or DAPSA remission over the course of 3 years between the aforementioned delay groups. The models were adjusted for sex and age. An interaction term between time and delay group was used to account for differences in the effect of time between groups. Time was modelled using linear spline functions with knots at 3 months, 1 and 2 years. To assess differences between delay groups in HAQ and PsAID-12 linear mixed effects models were used with an unstructured covariance matrix and a random person and time effect. The model was again adjusted with aforementioned covariates and also included the spline functions. We also provided crude estimates of the outcomes after 1 and 3 years to ensure validity of our results.
Due to missing data on some of the MDA criteria, not all patients could be categorised into achieving or not achieving MDA, which was solved in the following ways: if five MDA criteria were met and two were missing, MDA was considered achieved since missing information could not alter MDA status. Likewise, if three MDA criteria were not met, MDA was considered not achieved, regardless of missing data for the remaining four criteria. If MDA status could be changed by missing information, MDA status was found missing.
Logistic regression models were used to find associations between baseline characteristics and total, patient and physician delay. The median total delay (10.8), physician delay (4.5) and patient delay (1.0) were used as dependent variables. Univariately associated variables (p<0.20) were entered in a multivariate logistic regression model with a backward selection procedure until all remaining variables were significant (p≤0.05).
Drop-out rates were 25%, 31% and 29% in the short, intermediate and long delay group, respectively. We, therefore, compared baseline characteristics between patients who completed the 3 years of follow-up and those who dropped out. To ensure that enthesitis and axial disease were not the main driving factors of the effect of delay on outcomes we performed a sensitivity analysis in which we only included PsA patients with an oligoarthritis or polyarthritis.
All analyses were performed in Stata V.17.0. A p≤0.05 was considered statistically significant.
Results
Patients
Of the 708 included PsA patients 136 (19%) had a short delay (<12 weeks), 237 (33%) had an intermediate delay (≥12 weeks and ≤1 year) and 335 (47%) had a long delay (>1 year). PsA patients with a long delay were more often female, had less swollen joints, more enthesitis, and more often experienced chronic back pain before the age of 45 years than those with a short or intermediate delay (table 1).
Table 1.
Baseline characteristics of study patients
| Symptom duration <12 weeks (n=136) | Symptom duration 12 weeks to 1 year (n=237) | Symptom duration >1 year (n=335) | P value | ||||
| Demographic characteristics | |||||||
| Symptom duration (months), median (IQR) | 1.5 | (1–2) | 5.8 | (4–8) | 34.8 | (21–84) | – |
| Age (years), mean (SD) | 51.4 | (14.6) | 50.6 | (13.7) | 48.8 | (13.0) | 0.12 |
| Sex (female), n (%) | 58 | (43) | 113 | (48) | 191 | (57) | 0.008 |
| Smoking, n (%) | 23 | (19) | 45 | (22) | 63 | (22) | 0.80 |
| Body mass index (kg/m2), mean (SD) | 27.9 | (4.9) | 27.7 | (5.0) | 28.6 | (5.1) | 0.074 |
| Low education level, n (%)* | 39 | (34) | 89 | (44) | 104 | (37) | 0.19 |
| Years psoriasis preceding PsA development, median (IQR) | 9.8 | (3–21) | 9.4 | (3–20) | 11.8 | (4–23) | 0.12 |
| Family history of psoriasis, n (%) | 74 | (54) | 117 | (49) | 165 | (49) | 0.56 |
| Chronic back pain <45 years, n (%) | 42 | (32) | 69 | (30) | 151 | (46) | <0.001 |
| Disease activity | |||||||
| Swollen joint count (66), median (IQR) | 2 | (1–5) | 2 | (1–5) | 2 | (0–4) | 0.013 |
| Tender joint count (68), median (IQR) | 2 | (1–7) | 3 | (1–7) | 4 | (1–8) | 0.15 |
| Psoriasis, n (%) | 119 | (88) | 198 | (84) | 275 | (83) | 0.42 |
| BSA (%) in case of psoriasis, median (IQR) | 3 | (1–5) | 3 | (1–5) | 3 | (1–5) | 0.61 |
| Enthesitis, n (%) | 46 | (34) | 87 | (37) | 165 | (49) | 0.001 |
| LEI in case of enthesitis, median (IQR) | 2 | (1–2) | 2 | (1–3) | 2 | (1–3) | 0.30 |
| Dactylitis, n (%) | 22 | (16) | 36 | (15) | 53 | (16) | 0.96 |
| Nail involvement, n (%) | 75 | (57) | 133 | (59) | 203 | (63) | 0.48 |
| Axial disease only, n (%) | 3 | (2) | 7 | (3) | 11 | (3) | 0.82 |
| CRP (mg/L), median (IQR) | 7 | (2–13) | 4 | (1–12) | 4 | (0–8) | 0.002 |
| HAQ, mean (SD) | 0.74 | (0.58) | 0.71 | (0.53) | 0.71 | (0.46) | 0.90 |
| General health (VAS), median (IQR) | 45 | (23–65) | 50 | (30–68) | 47 | (23–65) | 0.17 |
| Pain (VAS), median (IQR) | 48 | (19–68) | 49 | (29–71) | 47 | (27–66) | 0.29 |
A p<0.05 was considered significant and is shown in bold.
*Low education level was defined (according to the Organisation for Economic Co-operation and Development) as below secondary level.
BSA, body surface area; CRP, C-reactive protein; HAQ, Health Assessment Questionnaire; LEI, Leeds Enthesitis Index; VAS, Visual Analogue Scale.
Duration of delay
The overall median delay was 10.8 months (IQR 3.7–32.8), which can be subcategorised into a median physician delay (4.5 months, IQR 1.3–21.1) and patient delay (1.0 month, IQR 0.1–5.0). The overall physician delay was significantly longer than the patient delay (p<0.001).
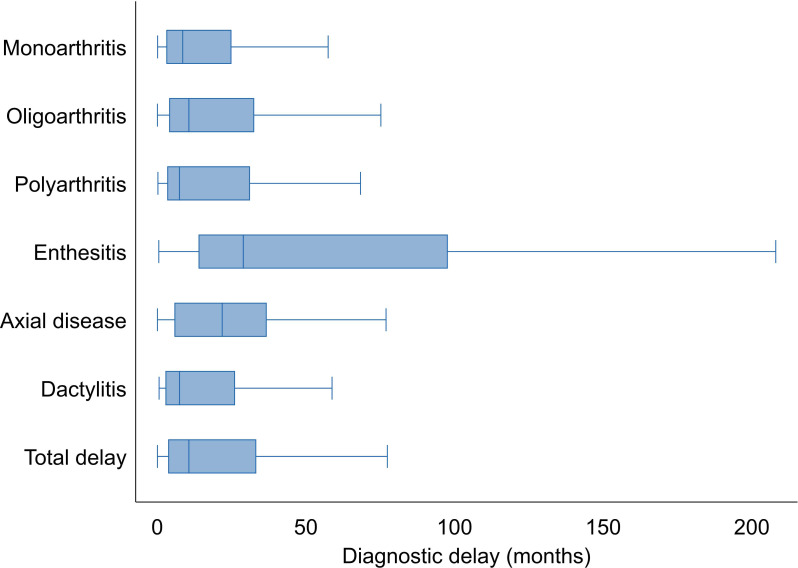
The total diagnostic delay differed between PsA phenotypes. Patients with enthesitis had the longest diagnostic delay (median 28.9 months, IQR 13.8–97.7), while patients with polyarthritis (median 7.4 months, IQR 3.3–31.1) and dactylitis (median 7.4 months, IQR 2.7–26.1) had the shortest delays (figure 1).
Figure 1.
Total diagnostic delay for different psoriatic arthritis phenotypes.Outliers are not shown for readability purposes.
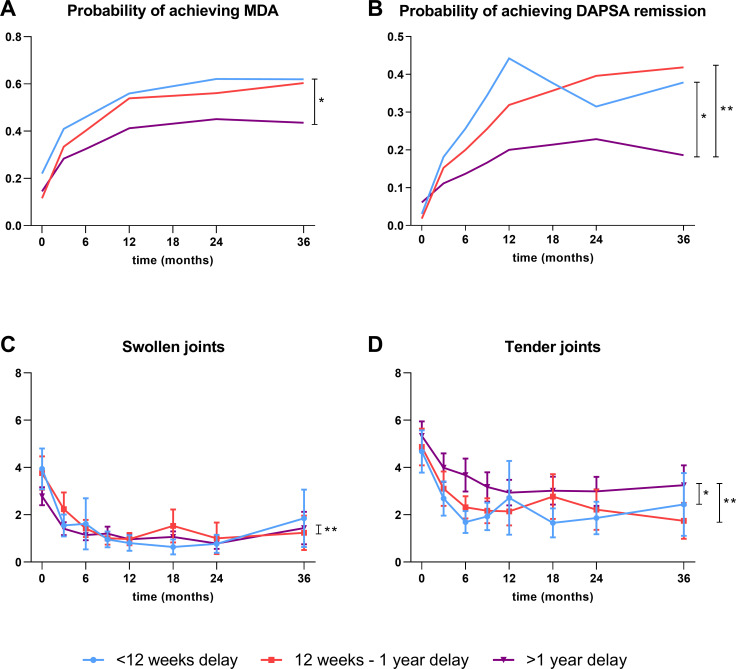
Delay and clinical outcomes
Patients with a short delay (<12 weeks) had a higher probability of achieving MDA than patients with a long delay (>1 year) over 3 years (OR 2.55 (95% CI 1.37 to 4.76), p=0.003) (figure 2A). Both the short and intermediate delay group were more likely to achieve DAPSA remission compared with the long delay group (OR 2.35 (95% CI 1.32 to 4.19), p=0.004 for short delay; OR 1.94 (95% CI 1.19 to 3.15), p=0.007 for intermediate delay) (figure 2B). Patients with a short delay were more likely to achieve DAPSA remission in the first year compared with those with an intermediate delay, but these differences diminished after 1 year of follow-up. No significant differences were found between the short and intermediate delay groups. SJCs were significantly higher in the intermediate delay group compared with the long delay group over 3 years, although the numerical difference was minimal (estimated mean difference 0.35 (95% CI 0.01 to 0.69) (figure 2C). Patients with a short or intermediate delay had slightly less tender joints during follow-up compared with the long delay group (estimated mean differences −1.09 (95% CI −1.88 to –0.30) for short vs long and −0.85 (95% CI −1.50 to –0.19) for intermediate vs long) (figure 2D). In conclusion, patients with a diagnostic delay of >1 year were less likely to achieve remission during 3 years of follow-up than patients with a delay ≤1 year.
Figure 2.
Clinical outcomes for delay groups over 3 years of follow-up. (A) Probability of achieving MDA, (B) probability of achieving DAPSA remission, (C) mean swollen joint count and (D) mean tender joint count in psoriatic arthritis patients stratified for the delay groups short (<12 weeks), intermediate (12 weeks to 1 year) and long (>1 year). (A, B) The predicted response after correcting for age and sex, while figure (C, D) the mean with 95% CI. *A significant difference between the short delay group and the long delay group. **A significant difference between the intermediate delay group and the long delay group. DAPSA, Disease Activity index for PSoriatic Arthritis; MDA, Minimal Disease Activity.
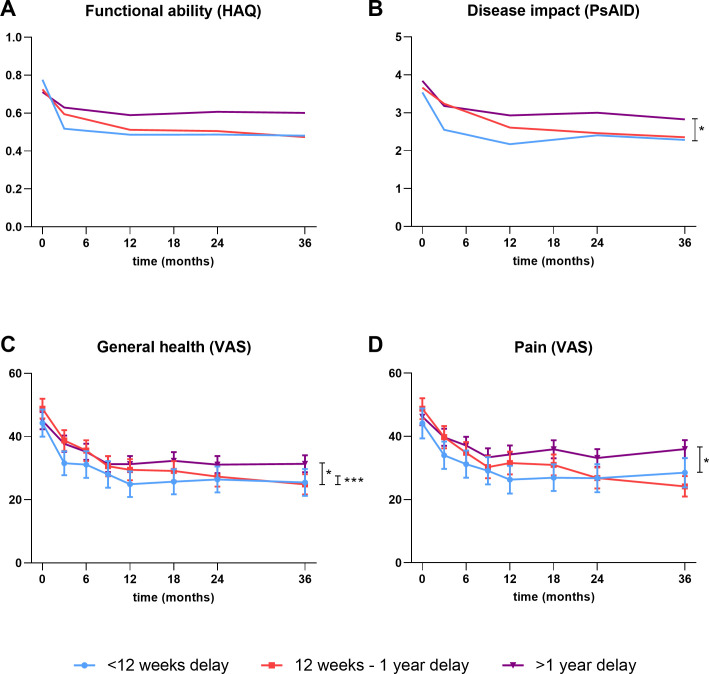
Delay and PROs
The PsA patients with a long delay experienced more functional limitations than the short and intermediate delay groups, but these differences were not statistically significant over 3 years (estimated mean difference −0.05 (95% CI −0.14 to 0.05) for short vs long and −0.03 (95% CI −0.11 to 0.05) for intermediate vs long) (figure 3A). The disease impact was slightly lower in the short delay group compared with the long delay group during follow-up (estimated mean difference −0.42 (95% CI −0.84 to –0.01)) (figure 3B). For all groups, the mean PsAID-12 score over time was <4, which is considered an acceptable symptom state. Patients with a short delay seemed to improve more quickly on their PROs in the first year compared with the intermediate and long delay groups (figure 3A,B). Mean general health was significantly better in the short delay group compared with the other two groups (estimated mean difference with long delay group −4.68 (95% CI −8.69 to –0.67) and estimated mean difference with intermediate delay group −4.26 (95% CI −8.47 to –0.04)) (figure 3C). Pain was on average 5.58 units lower (95% CI −9.98 to –1.18) in the short delay group compared with the long delay group over the course of 3 years (figure 3D). Overall, patients with a delay of >1 year had worse PROs over the course of 3 years compared with patients with a delay of ≤1 year, although differences were small.
Figure 3.
Patient-reported outcomes for delay groups over 3 years of follow-up. (A) Functional ability measured with the HAQ, (B) disease impact measured with the PsAID-12, (C) mean general health and (D) mean pain in psoriatic arthritis patients stratified for the delay groups short (<12 weeks), intermediate (12 weeks to 1 year) and long (>1 year). (A, B) The predicted response after correcting for age and sex, while figure (C, D) the mean with 95% CI. *A significant difference between the short delay group and the long delay group. ***A significant difference between the short delay group and the intermediate delay group. HAQ, Health Assessment Questionnaire; PsAID-12, Psoriatic Arthritis Impact of Disease; VAS, Visual Analogue Scale.
Patient characteristics associated with delay
The following baseline characteristics were significantly associated with a longer total delay by multivariate analysis: female sex, chronic back pain <45 years, enthesitis and lower CRP levels (table 2). For physician delay female sex and lower CRP levels were multivariately associated (online supplemental table S1). With respect to patient delay, only a lower CRP level was found to be significantly associated (online supplemental table S2).
Table 2.
Baseline characteristics of early PsA patients associated by univariate and multivariate analysis with total delay
| Total delay | Univariate model | Multivariate model | ||
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Female sex | 1.57 (1.17 to 2.12) | 0.003 | 1.44 (1.03 to 2.02) | 0.034 |
| Chronic back pain <45 years | 1.90 (1.39 to 2.60) | <0.001 | 1.71 (1.21 to 2.42) | 0.003 |
| Swollen joint count | 0.95 (0.91 to 0.98) | 0.005 | ||
| Enthesitis | 1.75 (1.30 to 2.37) | <0.001 | 1.53 (1.08 to 2.17) | 0.016 |
| CRP | 0.98 (0.96 to 0.99) | 0.002 | 0.98 (0.97 to 0.99) | 0.006 |
Patient characteristics associated with total delay were analysed using logistic regression by creating two groups based on the median value of total delay.
CRP, C-reactive protein; PsA, psoriatic arthritis.
rmdopen-2023-004062supp001.pdf (244.1KB, pdf)
Sensitivity analyses
To check for attrition bias, baseline characteristics of drop-outs were compared with those who completed follow-up. Those who dropped out were slightly younger, had more often enthesitis and had somewhat higher baseline pain scores (online supplemental table S3). Crude estimates of clinical outcomes and PROs after 1 and 3 years showed similar results as our main analysis (online supplemental table S4).
In the sensitivity analysis in which we only included oligoarthritis and polyarthritis patients (n=417) to exclude enthesitis and axial disease as the only driving factors, similar results were found for the probability of achieving MDA and DAPSA remission as well as for functional limitations and disease impact (online supplemental figure S1).
Discussion
It is unclear whether a diagnostic ‘window of opportunity’ exists in PsA and what the duration of such a window would be. We have shown that those presenting late are less likely to achieve remission. More specifically, a delay of >1 year is associated with worse clinical outcomes, which includes almost 50% of the PsA population. This is the first study suggesting some sort of window of opportunity in PsA. For good long-term outcomes, it is important that PsA patients are diagnosed by a rheumatologist within 1 year after symptom onset.
The total diagnostic delay is determined by the patient delay and the physician delay. In our study the physician delay (4.5 months) was significantly longer than the patient delay (1.0 month). Thus, the most progress to shorten the delay can be made in reducing physician delay. Dutch GP arthritis guidelines recommend referral to a rheumatologist in patients with a persistent arthritis of >3 weeks, patients with a suspected RA, and patients with a suspected peripheral arthritis related to spondyloarthritis.24 The 3-week mark is based on the EULAR recommendation that arthritis patients should be seen by a rheumatologist within 6 weeks after symptom onset.24 25 Although the GP guideline includes some important extra-articular PsA-related symptoms such as psoriasis and inflammatory back pain, it does not cover enthesitis. This means that mainly patients who have RA-like symptoms, that is an oligoarthritis or polyarthritis, or axial spondyloarthritis-like symptoms, that is, arthritis with inflammatory back pain, would be referred quickly. This was also visible in our study. Among the PsA phenotypes, patients with enthesitis had the longest delays, while patients with polyarthritis and dactylitis had the shortest delays. A study in the USA found similar results; those with a shorter time to PsA diagnosis more often had swollen joints and dactylitis, while those with a longer time to diagnosis more often reported enthesitis and back pain.26 It is not surprising that the more obvious symptoms (arthritis, dactylitis) are easier recognised by GPs than more vague complaints (enthesitis) or very common symptoms (back pain). It might, therefore, be beneficial to educate GPs on the most common tendon complaints related to PsA.
This study shows the negative effect of a longer diagnostic delay on clinical outcomes as well as PROs in PsA patients. This is in agreement with previous data showing an association of a longer diagnostic delay with more radiological damage and functional limitations, and less DMARD-free remission and MDA achievement.2 3 5 27 PsA patients with a shorter delay probably have a more modifiable disease course due to early treatment initiation, which leads to better outcomes. Although some data are available on this subject, this is the first longitudinal study analysing the effect of a very short delay (<12 weeks) on long-term outcomes in PsA.
Ideally, a randomised controlled trial with an early and a delayed intervention arm would be conducted to assess the effect of delayed treatment on long-term outcomes in PsA. Because such a trial would not be ethically feasible, a cohort design was used. However, a cohort design is subject to potential confounding if, for example, subgroups with a short delay are included that are themselves characterised by a better outcome. Indeed, there were some baseline imbalances between delay groups that were independently associated with total delay. Female patients and patients with enthesitis, chronic back pain and lower CRP levels had a longer diagnostic delay. Currently, there is no accepted definition for ‘difficult-to-treat’ PsA. However, it was recently proposed that four key factors may lead to treatment resistance in PsA, including the presence of comorbidities that sustain inflammation and comorbidities that increase pain and disability.28 Although we do not have data on all comorbidities that may sustain inflammation, we found no difference in smoking and BMI at baseline, which are known to negatively impact treatment response.29 30 Regarding comorbidities that increase pain and disability, depression, anxiety and chronic widespread pain are frequent in PsA and can lead to increased pain and poorer functional outcomes, resulting in lower remission rates as measured with composite scores, such as the DAPSA and MDA.31–33 In addition, previous literature has shown that female PsA patients have higher disease activity and poorer response to treatment than their male counterparts.34 We have attempted to account for these confounders by adjusting our results for sex and by performing a sensitivity analysis in which only patients with oligoarthritis or polyarthritis were included. However, we cannot be sure that there is no residual confounding in our study. Therefore, management of PsA patients should not only focus on early intervention, but should be tailored to the individual patient, taking into account comorbidities that may affect disease activity.
Although there might be a ‘window of opportunity’ in PsA, this window seems to be much larger than that in RA (<1 year vs <12 weeks). This difference may have several causes. First, PsA has a different pathophysiology than RA. Unlike RA, circulating autoantibodies and B-cell infiltration do not seem to play a role in the pathogenesis of PsA.35 Thus, PsA clearly is a different clinical entity from RA, which may naturally also lead to a different timing of diagnosis in PsA. Second, the majority of PsA patients have had psoriasis for ±10 years before PsA is diagnosed.36 37 Psoriasis is a systemic inflammatory disease in itself with elevated levels of proinflammatory cytokines in both skin lesions and the blood.38 These chronically elevated cytokine levels stimulate subclinical inflammation, which can already be present for many years before the diagnosis of PsA is made.39 40 This suggests that chronic systemic inflammation is present for a long period before musculoskeletal PsA symptoms become apparent, which makes very rapid referral somewhat less influential in comparison to RA. In summary, we appear to be fortunate to have more time to diagnose PsA than RA to minimise poor clinical outcomes.
A limitation of our study is the drop-out rate. Patients with a long delay might drop out because of dissatisfaction with their treatment, while patients with a short or intermediate delay might drop out due to inactive disease. Therefore, baseline characteristics of patients who dropped out were compared with those with a complete follow-up. Since only minor differences were present, we do not expect that this influenced our results. Furthermore, mixed models were used in the analysis, which account for missing data.
Strengths are the use of a large real-world, prospective cohort, which makes our data more generalisable than data from, for example, clinical trials. Moreover, clinical outcomes as well as PROs are reported and all outcomes were in concordance with each other, which makes our results more valid.
In conclusion, a shorter time to PsA diagnosis is associated with a greater likelihood of achieving MDA and DAPSA remission over time, suggesting the presence of a window of opportunity in PsA. This is an important finding because currently ~50% of PsA patients have a diagnostic delay of >1 year. Physician delay is modifiable and reduction of the physician delay is of utmost importance to improve long-term outcomes in PsA.
Acknowledgments
We gratefully thank all participating patients, rheumatologists and research nurses.
Footnotes
Contributors: SVJSH performed the statistical analysis and drafted the manuscript. PHPdJ and MV contributed to the analysis. All authors contributed to the design, revised the manuscript and read and approved the final manuscript. MV is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Medical research ethics committee of Erasmus Medical Center Rotterdam, the Netherlands (MEC-2012-549). Participants gave informed consent to participate in the study before taking part.
References
- 1. Villani AP, Rouzaud M, Sevrain M, et al. Prevalence of undiagnosed psoriatic arthritis among psoriasis patients: systematic review and meta-analysis. J Am Acad Dermatol 2015;73:242–8. 10.1016/j.jaad.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 2. Haroon M, Gallagher P, FitzGerald O. Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann Rheum Dis 2015;74:1045–50. 10.1136/annrheumdis-2013-204858 [DOI] [PubMed] [Google Scholar]
- 3. Tillett W, Jadon D, Shaddick G, et al. Smoking and delay to diagnosis are associated with poorer functional outcome in psoriatic arthritis. Ann Rheum Dis 2013;72:1358–61. 10.1136/annrheumdis-2012-202608 [DOI] [PubMed] [Google Scholar]
- 4. Coates LC, Soriano ER, Corp N, et al. Group for research and assessment of psoriasis and psoriatic arthritis (GRAPPA): updated treatment recommendations for Psoriatic arthritis 2021. Nat Rev Rheumatol 2022;18:465–79. 10.1038/s41584-022-00798-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gladman DD, Thavaneswaran A, Chandran V, et al. Do patients with Psoriatic arthritis who present early fare better than those presenting later in the disease Ann Rheum Dis 2011;70:2152–4. 10.1136/ard.2011.150938 [DOI] [PubMed] [Google Scholar]
- 6. Smolen JS, Schöls M, Braun J, et al. Treating axial Spondyloarthritis and peripheral Spondyloarthritis, especially Psoriatic arthritis, to target: 2017 update of recommendations by an international task force. Ann Rheum Dis 2018;77:3–17. 10.1136/annrheumdis-2017-211734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coates LC, FitzGerald O, Merola JF, et al. Group for research and assessment of psoriasis and Psoriatic arthritis/outcome measures in rheumatology consensus‐based recommendations and research agenda for use of composite measures and treatment targets in psoriatic arthritis. Arthritis Rheumatol 2018;70:345–55. 10.1002/art.40391 [DOI] [PubMed] [Google Scholar]
- 8. Aletaha D, Alasti F, Smolen JS. Disease activity States of the DAPSA, a psoriatic arthritis specific instrument, are valid against functional status and structural progression. Ann Rheum Dis 2017;76:418–21. 10.1136/annrheumdis-2016-209511 [DOI] [PubMed] [Google Scholar]
- 9. Snoeck Henkemans SVJ, de Jong PHP, Luime JJ, et al. Importance of quick attainment of minimal disease activity for a positive impact on lives of patients with psoriatic arthritis. RMD Open 2022;8:e002706. 10.1136/rmdopen-2022-002706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Coates LC, Nash P, Kvien TK, et al. Comparison of remission and low disease activity States with DAPSA, MDA and VLDA in a clinical trial setting in psoriatic arthritis patients: 2-year results from the FUTURE 2 study. Semin Arthritis Rheum 2020;50:709–18. 10.1016/j.semarthrit.2020.03.015 [DOI] [PubMed] [Google Scholar]
- 11. Quinn MA, Emery P. Window of opportunity in early rheumatoid arthritis: possibility of altering the disease process with early intervention. Clin Exp Rheumatol 2003;21(5 Suppl 31):S154–7. [PubMed] [Google Scholar]
- 12. Nell VPK, Machold KP, Eberl G, et al. Benefit of very early referral and very early therapy with disease-modifying anti-rheumatic drugs in patients with early rheumatoid arthritis. Rheumatology (Oxford) 2004;43:906–14. 10.1093/rheumatology/keh199 [DOI] [PubMed] [Google Scholar]
- 13. Möttönen T, Hannonen P, Korpela M, et al. Delay to institution of therapy and induction of remission using single-drug or combination-disease-modifying antirheumatic drug therapy in early rheumatoid arthritis. Arthritis Rheum 2002;46:894–8. 10.1002/art.10135 [DOI] [PubMed] [Google Scholar]
- 14. van der Linden MPM, le Cessie S, Raza K, et al. Long-term impact of delay in assessment of patients with early arthritis. Arthritis Rheum 2010;62:3537–46. 10.1002/art.27692 [DOI] [PubMed] [Google Scholar]
- 15. Kasiem FR, Luime JJ, Vis M, et al. Lessons learned from clinical phenotypes in early Psoriatic arthritis: the real-world Dutch South West early Psoriatic arthritis study. Scand J Rheumatol 2021;50:124–31. 10.1080/03009742.2020.1803398 [DOI] [PubMed] [Google Scholar]
- 16. Gladman DD. Early Psoriatic arthritis. Rheum Dis Clin North Am 2012;38:373–86. 10.1016/j.rdc.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 17. Bonifati C, Elia F, Francesconi F, et al. The diagnosis of early psoriatic arthritis in an outpatient dermatological centre for psoriasis. J Eur Acad Dermatol Venereol 2012;26:627–33. 10.1111/j.1468-3083.2011.04138.x [DOI] [PubMed] [Google Scholar]
- 18. Henseler T, Schmitt-Rau K. A comparison between BSA, PASI, PLASI and SAPASI as measures of disease severity and improvement by therapy in patients with psoriasis. Int J Dermatol 2008;47:1019–23. 10.1111/j.1365-4632.2008.03753.x [DOI] [PubMed] [Google Scholar]
- 19. Healy PJ, Helliwell PS. Measuring clinical enthesitis in psoriatic arthritis: assessment of existing measures and development of an instrument specific to psoriatic arthritis. Arthritis Rheum 2008;59:686–91. 10.1002/art.23568 [DOI] [PubMed] [Google Scholar]
- 20. Cauli A, Gladman DD, Mathieu A, et al. Patient global assessment in psoriatic arthritis: a multicenter GRAPPA and OMERACT study. J Rheumatol 2011;38:898–903. 10.3899/jrheum.100857 [DOI] [PubMed] [Google Scholar]
- 21. Bruce B, Fries JF. The health assessment questionnaire (HAQ). Clin Exp Rheumatol 2005;23(5 Suppl 39):S14–8. [PubMed] [Google Scholar]
- 22. Gossec L, de Wit M, Kiltz U, et al. A patient-derived and patient-reported outcome measure for assessing psoriatic arthritis: elaboration and preliminary validation of the Psoriatic arthritis impact of disease (Psaid) questionnaire, a 13-country EULAR initiative. Ann Rheum Dis 2014;73:1012–9. 10.1136/annrheumdis-2014-205207 [DOI] [PubMed] [Google Scholar]
- 23. Coates LC, Fransen J, Helliwell PS. Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis 2010;69:48–53. 10.1136/ard.2008.102053 [DOI] [PubMed] [Google Scholar]
- 24. Janssens H, Lopuhaä DE, Schaafstra A, et al. NHG Standaard Artritis. 2017.
- 25. Combe B, Landewe R, Daien CI, et al. Update of the EULAR recommendations for the management of early arthritis. Ann Rheum Dis 2017;76:948–59. 10.1136/annrheumdis-2016-210602 [DOI] [PubMed] [Google Scholar]
- 26. Ogdie A, Nowell WB, Applegate E, et al. Patient perspectives on the pathway to psoriatic arthritis diagnosis: results from a web-based survey of patients in the United States. BMC Rheumatol 2020;4:2. 10.1186/s41927-019-0102-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Theander E, Husmark T, Alenius G-M, et al. Early psoriatic arthritis: short symptom duration, male gender and preserved physical functioning at presentation predict favourable outcome at 5-year follow-up. Ann Rheum Dis 2014;73:407–13. 10.1136/annrheumdis-2012-201972 [DOI] [PubMed] [Google Scholar]
- 28. Fagni F, Motta F, Schett G, et al. Difficult-to-treat psoriatic arthritis: a conceptual approach. Arthritis Rheumatol December 18, 2023. 10.1002/art.42780 [DOI] [PubMed] [Google Scholar]
- 29. Højgaard P, Glintborg B, Hetland ML, et al. Association between tobacco smoking and response to tumour necrosis factor Α inhibitor treatment in psoriatic arthritis: results from the DANBIO Registry. Ann Rheum Dis 2015;74:2130–6. 10.1136/annrheumdis-2014-205389 [DOI] [PubMed] [Google Scholar]
- 30. Gialouri CG, Pappa M, Evangelatos G, et al. Effect of body mass index on treatment response of biologic/targeted-synthetic Dmards in patients with rheumatoid arthritis, psoriatic arthritis or axial spondyloarthritis. a systematic review. Autoimmun Rev 2023;22:103357. 10.1016/j.autrev.2023.103357 [DOI] [PubMed] [Google Scholar]
- 31. Wong A, Ye JY, Cook RJ, et al. Depression and anxiety reduce the probability of achieving a state of sustained minimal disease activity in patients with psoriatic arthritis. Arthritis Care Res (Hoboken) 2022;74:1430–4. 10.1002/acr.24593 [DOI] [PubMed] [Google Scholar]
- 32. Michelsen B, Kristianslund EK, Sexton J, et al. Do depression and anxiety reduce the likelihood of remission in rheumatoid arthritis and psoriatic arthritis? Data from the prospective multicentre NOR-DMARD study. Ann Rheum Dis 2017;76:1906–10. 10.1136/annrheumdis-2017-211284 [DOI] [PubMed] [Google Scholar]
- 33. Brikman S, Furer V, Wollman J, et al. The effect of the presence of fibromyalgia on common clinical disease activity indices in patients with psoriatic arthritis: a cross-sectional study. J Rheumatol 2016;43:1749–54. 10.3899/jrheum.151491 [DOI] [PubMed] [Google Scholar]
- 34. Tarannum S, Leung Y-Y, Johnson SR, et al. Sex- and gender-related differences in Psoriatic arthritis. Nat Rev Rheumatol 2022;18:513–26. 10.1038/s41584-022-00810-7 [DOI] [PubMed] [Google Scholar]
- 35. Fitzgerald O, Winchester R. Psoriatic arthritis: from pathogenesis to therapy. Arthritis Res Ther 2009;11:214. 10.1186/ar2580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Perez-Chada LM, Haberman RH, Chandran V, et al. Consensus terminology for preclinical phases of psoriatic arthritis for use in research studies: results from a Delphi consensus study. Nat Rev Rheumatol 2021;17:238–43. 10.1038/s41584-021-00578-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis 2005;64(Suppl 2):ii14–7. 10.1136/ard.2004.032482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Suárez-Fariñas M, Li K, Fuentes-Duculan J, et al. Expanding the psoriasis disease profile: interrogation of the skin and serum of patients with moderate-to-severe psoriasis. J Invest Dermatol 2012;132:2552–64. 10.1038/jid.2012.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Korman NJ. Management of psoriasis as a systemic disease: what is the evidence Br J Dermatol 2020;182:840–8. 10.1111/bjd.18245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pennington SR, FitzGerald O. Early origins of Psoriatic arthritis: clinical, genetic and molecular biomarkers of progression from psoriasis to Psoriatic arthritis. Front Med (Lausanne) 2021;8:723944. 10.3389/fmed.2021.723944 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2023-004062supp001.pdf (244.1KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data are available from the corresponding author on reasonable request.