Key Points
Question
Is female sex associated with increased mortality risk in patients with Staphylococcus aureus bacteremia?
Findings
In this systematic review and meta-analysis that included 132 582 patients from 89 studies, female sex was associated with increased mortality. Female patients with S aureus bacteremia had 18% increased odds of death compared with male patients.
Meaning
These results suggest that female patients with S aureus bacteremia have higher mortality risk than male patients; further research is needed to study the potential underlying mechanisms.
This systematic review and meta-analysis of studies on outcomes for patients hospitalized with Staphylococcus aureus examines the association of mortality with female sex.
Abstract
Importance
Staphylococcus aureus is the leading cause of death due to bacterial bloodstream infection. Female sex has been identified as a risk factor for mortality in S aureus bacteremia (SAB) in some studies, but not in others.
Objective
To determine whether female sex is associated with increased mortality risk in SAB.
Data Sources
MEDLINE, Embase, and Web of Science were searched from inception to April 26, 2023.
Study Selection
Included studies met the following criteria: (1) randomized or observational studies evaluating adults with SAB, (2) included 200 or more patients, (3) reported mortality at or before 90 days following SAB, and (4) reported mortality stratified by sex. Studies on specific subpopulations (eg, dialysis, intensive care units, cancer patients) and studies that included patients with bacteremia by various microorganisms that did not report SAB-specific data were excluded.
Data Extraction and Synthesis
Data extraction and quality assessment were performed by 1 reviewer and verified by a second reviewer. Risk of bias and quality were assessed with the Newcastle-Ottawa Quality Assessment Scale. Mortality data were combined as odds ratios (ORs).
Main Outcome and Measures
Mortality at or before 90-day following SAB, stratified by sex.
Results
From 5339 studies retrieved, 89 were included (132 582 patients; 50 258 female [37.9%], 82 324 male [62.1%]). Unadjusted mortality data were available from 81 studies (109 828 patients) and showed increased mortality in female patients compared with male patients (pooled OR, 1.12; 95% CI, 1.06-1.18). Adjusted mortality data accounting for additional patient characteristics and treatment variables were available from 32 studies (95 469 patients) and revealed a similarly increased mortality risk in female relative to male patients (pooled adjusted OR, 1.18; 95% CI, 1.11-1.27). No evidence of publication bias was encountered.
Conclusions and Relevance
In this systematic review and meta-analysis, female patients with SAB had higher mortality risk than males in both unadjusted and adjusted analyses. Further research is needed to study the potential underlying mechanisms.
Introduction
Staphylococcus aureus is the leading cause of death due to bacterial bloodstream infection.1 Previously identified risk factors for mortality in patients with Staphylococcus aureus bacteremia (SAB) have included increasing age, infective endocarditis, hemodialysis dependence, and persistent bacteremia, among others.2 Female sex has been suggested as risk factor for mortality in SAB in several studies, with an increase of mortality of up to 30% relative to male patients.3,4,5 However, other studies found no gender inequality in outcome of SAB,6,7 or even a higher mortality in male individuals in a subgroup of patients with a higher comorbidity score.8 Thus, the impact of female sex in SAB remains unclear. The aim of this systematic review and meta-analysis was to determine whether female sex is associated with mortality in SAB.
Methods
The key question of this systematic review was: is female sex associated with increased mortality risk in patients with SAB? The study protocol was registered on Prospero (CRD42022373176). We followed the meta-analysis of observational studies in epidemiology Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guideline as the included studies involved observational data.
Search Strategy
We conducted a literature search of MEDLINE via PubMed, Embase via Elsevier, and Web of Science Core Collection (1900 to present) via Clarivate from inception to October 31, 2022, using a combination of key words to capture S aureus, bacteremia, mortality, and sex (eAppendix 1 in Supplement 1). An experienced medical librarian (S.K.) devised, developed, and executed the search with input from the entire team. The search was peer reviewed by a second medical librarian according to a modified Peer Review of Electronic Search Strategies (PRESS) checklist.9 No limitations were placed on language in the initial search, but studies published in languages other than English were excluded in the full-text review phase. A search update was conducted on April 26, 2023, to identify newly published studies. In addition, we hand-searched key references to identify citations not captured in the electronic database searches. All results were compiled in EndNote and imported into Covidence, a web-based data synthesis software program,10 for deduplication and screening.
Study Selection, Data Extraction, and Quality Assessment
We included studies that met the following conditions: (1) randomized or observational study evaluating outcomes in adults with SAB, (2) included 200 or more patients, (3) reported mortality at or before 90 days following SAB, and (4) reported mortality stratified by sex. Exclusion criteria were studies on specific subpopulations (eg, dialysis, intensive care unit, hematological or oncological patients), studies that included SAB patients as a subgroup (eg, patients with bacteremia by any microorganism) that did not report SAB-specific data, and studies using (partially) the same cohort as another study included in this review. In this latter scenario, the study with the largest cohort was included. Titles and abstracts of articles (with authors and institutions visible) identified through our primary search were screened independently by 2 reviewers (A.W. reviewed all; R.K., M.W., J.K., F.R., J.P., S.M., S.K., M.L., V.F., and J.T. were second reviewers). Conflicts at this stage were resolved by a third person. Articles marked for full-text review underwent full-text screening by 2 independent reviewers. Conflicts at this stage were resolved by consensus or by obtaining a third reviewer’s opinion when consensus could not be reached. Data extraction and quality assessment was done by 1 reviewer and verified by a second reviewer. Extracted variables included lead author, journal, year of publication, start and end year of inclusion, country, aim of study, study design, number of hospitals, number of patients, population description, and whether methicillin-resistant S aureus (MRSA), methicillin-susceptible S aureus (MSSA), or both were addressed. Unadjusted mortality stratified by sex was extracted, as well as adjusted mortality when reported, the statistical model and the covariates for which mortality was adjusted. If a study described mortality for 2 subgroups (eg, for MSSA and MRSA bacteremia separately), both were included. Risk of bias and quality were assessed with the Newcastle-Ottawa Quality Assessment Scale11 (eAppendix 2 in Supplement 1) because only observational studies were identified.
Statistical Analysis
Mortality data were combined as odds ratios (ORs). If ORs were not reported in a study, we calculated ORs from raw mortality by sex if such data was available. If raw data was not available either, then ORs were calculated from the provided risk ratio (RR) or hazard ratio (HR) values based on previously published methods.12,13 In the single study that reported a rate ratio,14 this rate ratio was used to estimate the OR.15 Sensitivity analyses involving only studies that directly reported an OR (as opposed to estimating OR based on HR or RR) were conducted. ORs were combined using inverse variance with random effects models. We used the Knapp and Hartung method to adjust the standard errors of the estimated coefficients.16,17 Robustness of findings were assessed through influence and sensitivity analyses as detailed in the text. We evaluated statistical heterogeneity with the Cochran Q and I2 statistics. To explore potential sources of heterogeneity, we performed meta-analyses on subsets of studies to determine if variation in factors such as mortality time point (eg, 30-day vs 90-day mortality), bacterial groups (eg, MSSA only, MRSA only, both MSSA and MRSA), or geographic location between studies could be contributing. Statistical analyses were performed with RStudio version 2022.02.0 (R Project for Statistical Computing). Publication bias was assessed using funnel plots with the Egger test18 when 10 or more studies were included in the analysis. We used the Evidence-based Practice Center (EPC) model from the US Agency for Healthcare Research and Quality (AHRQ) to grade overall strength of evidence.19 A full description of the EPC approach is detailed in eAppendix 3 in Supplement 1.
Results
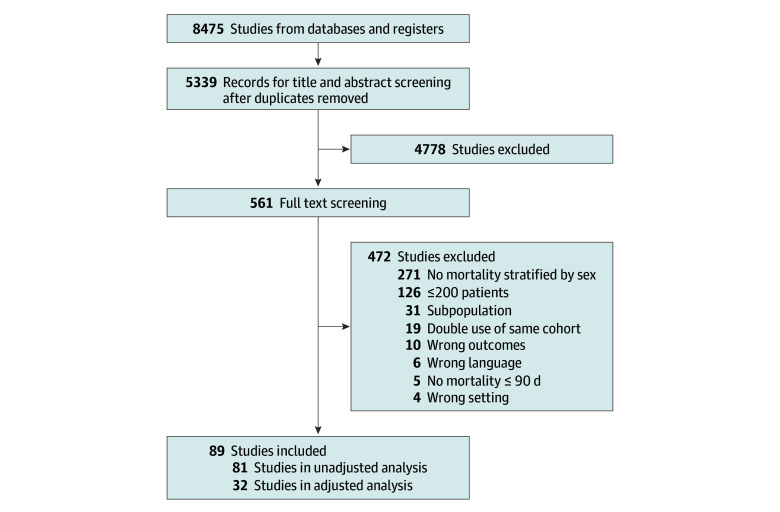
We screened the title and abstract of 5339 studies, and 4778 were deemed irrelevant (Figure 1). A full-text assessment was performed on 561 studies, and 472 of these were excluded. We included 89 studies in the analysis, with a total of 132 582 patients (50 258 female [37.9%], 82 324 male [62.1%]) (Table).3,4,5,6,7,8,14,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101 All data on mortality by sex were from observational studies: 88 of 89 cohort studies and 1 post hoc analysis of a randomized clinical trial. Mortality was most frequently assessed at 28 to 30 days (54 of 89 studies [61%]). The majority of studies were conducted in Europe (36 [40%]), Asia (24 [28%]) and North America (20 [22%]). The majority of studies were published after 2010 (68 [76%]). Thirty-two studies (36%) were rated as having low risk of bias, and 57 studies (64%) as having high risk of bias (detailed quality assessment of each study in eTable 1 in Supplement 1).
Figure 1. Search Flow Diagram of Systematic Review.
Table. Description of Studies Included in Systematic Review.
| Study characteristics | Studies, No. (%) (N = 89) |
|---|---|
| Publication year | |
| 2000-2010 | 21 (24) |
| 2011-2023 | 68 (76) |
| Study design | |
| Cohort study | 88 (99) |
| Post hoc analysis randomized trial | 1 (1) |
| Continent | |
| Europe | 36 (40) |
| Asia | 24 (27) |
| North America | 20 (22) |
| Oceania | 5 (6) |
| South America | 1 (1) |
| Africa | 1 (1) |
| Multiple | 2 (2) |
| No. of hospitals included | |
| 1 | 44 (49) |
| 2-20 | 33 (37) |
| >20 | 13 (15) |
| No. of patients included | |
| 200-1000 | 69 (78) |
| 1000-10 000 | 15 (17) |
| >10 000 | 4 (4) |
| Population | |
| All SAB patients | 82 (92) |
| Health care/hospital-associated SAB | 3 (3) |
| Community-acquired SAB | 4 (4) |
| Outcome measure | |
| 7-d mortality | 1 (1) |
| 14-d mortality | 4 (4) |
| 28-30–d mortality | 54 (61) |
| 90-d mortality | 9 (10) |
| In-hospital mortality | 16 (18) |
| Attributable mortality | 5 (6) |
| MRSA vs MSSA | |
| Both MRSA and MSSA | 59 (66) |
| Only MRSA | 20 (22) |
| Only MSSA | 10 (11) |
Abbreviations: MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-susceptible Staphylococcus aureus; SAB, Staphylococcus aureus bacteremia.
Mortality by Sex
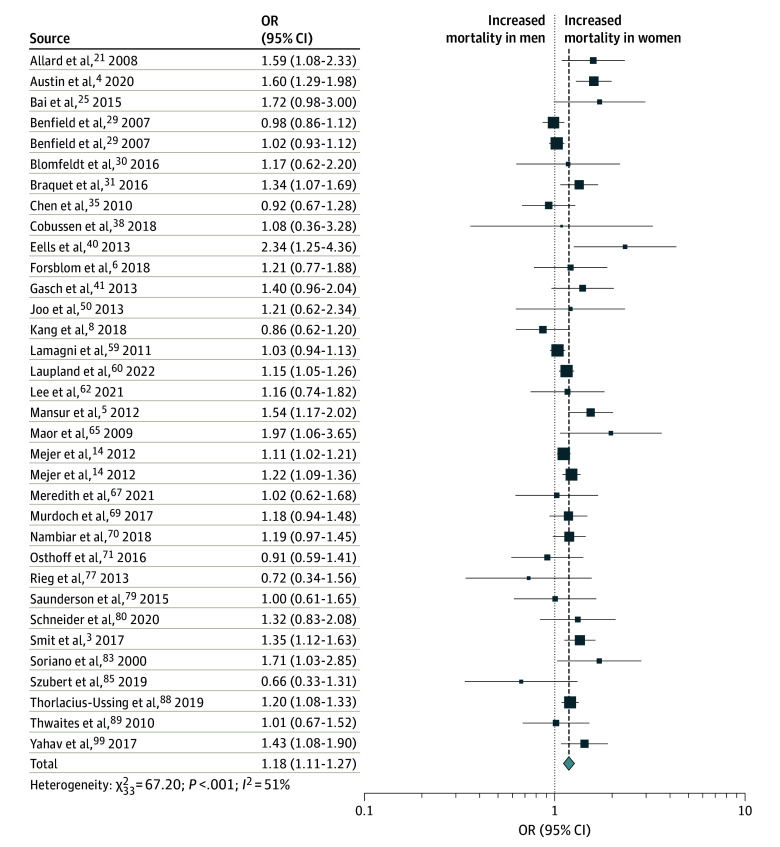
Unadjusted mortality data was available from 81 studies (109 828 patients) and revealed an increased mortality risk in female compared with male patients (pooled OR, 1.12; 95% CI, 1.06-1.18) (Figure 2). Moderate heterogeneity was observed in this analysis (Q = 130.17; P < .001; I2 = 37%). An influence analysis revealed that exclusion of any single study did not significantly alter the findings from the overall cohort (eAppendix 4 in Supplement 1). A sensitivity analysis with only studies that had an OR that was either reported or could be directly calculated (ie, excluding 14 studies in which RR or HR were reported) similarly did not change the overall findings (eFigure 1 in Supplement 1). Exclusion of single-center studies did not change the overall findings. No funnel plot asymmetry was found (eFigure 2 in Supplement 1).
Figure 2. Forest Plot of Unadjusted Mortality in Female vs Male Patients With Staphylococcus aureus Bacteremia.
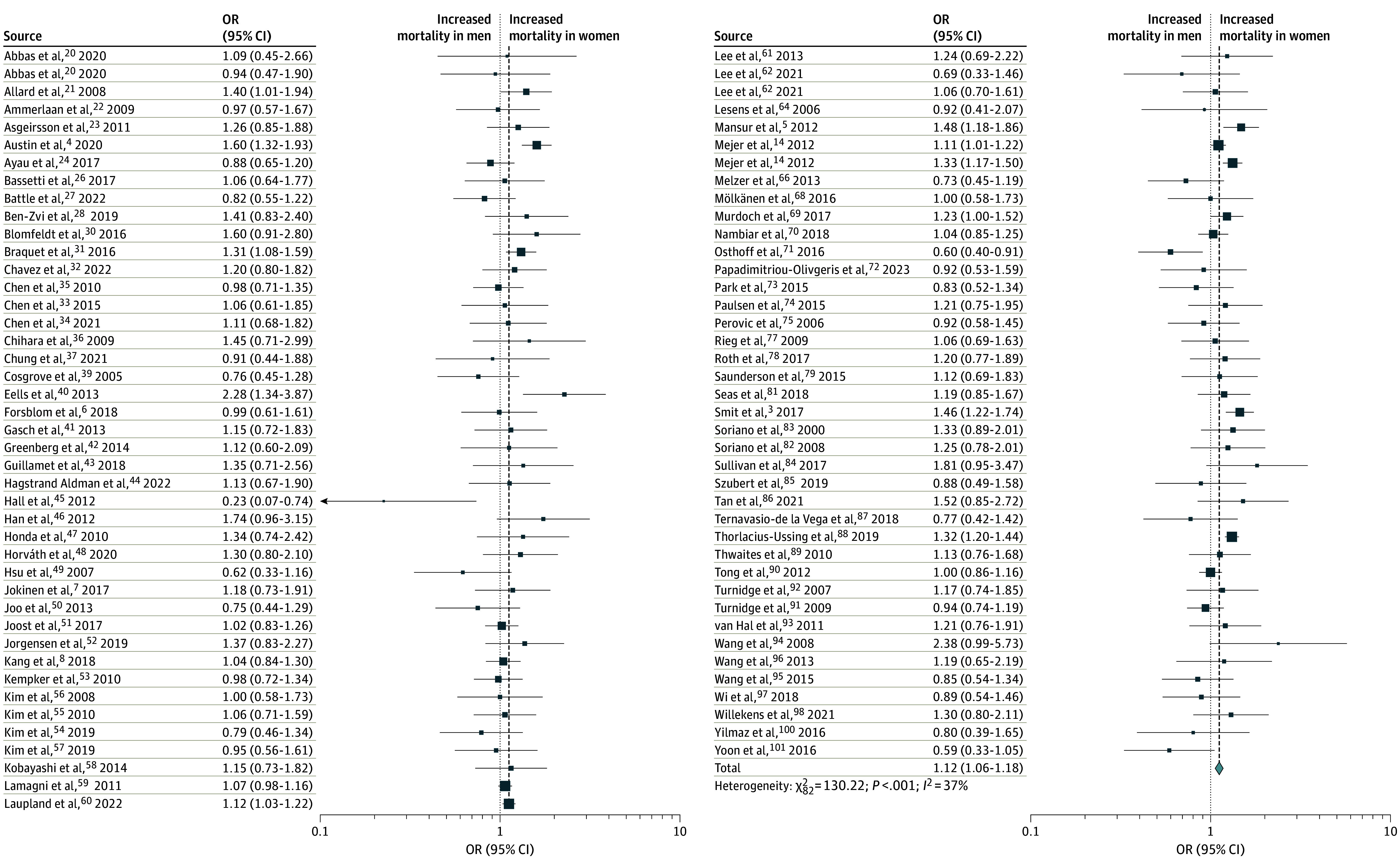
Adjusted mortality data that accounted for patient characteristics and treatment variables was available from 32 studies (95 469 patients) and revealed a similarly increased mortality risk in female relative to male patients (pooled adjusted OR [aOR], 1.18; 95% CI, 1.11-1.27) (Figure 3). An influence analysis revealed that exclusion of any single study did not significantly alter the findings from the overall cohort (eAppendix 5 in Supplement 1). A sensitivity analysis with only studies that had an OR that was either reported or could be directly calculated (ie, excluding 14 studies in which RR or HR were reported) similarly did not change the overall findings (eFigure 3 in Supplement 1). No funnel plot asymmetry was found (eFigure 4 in Supplement 1). Substantial heterogeneity was observed in this analysis of adjusted mortality data (Q = 66.98; P < .001; I2 = 51%). Meta-analyses on subsets of studies showed that variation in the geographic location of the study impacted heterogeneity. Meta-analyses of studies conducted in individual geographic regions all had lower observed heterogeneity than the overall cohort (overall I2 = 51%): Europe (19 studies; I2 = 41%), North America (5 studies; I2 = 12%), East Asia (4 studies; I2 = 0%), and Middle East (3 studies; I2 = 0%). The pooled aOR varied significantly based on geographic location of study and ranged from 0.96 (95% CI, 0.76-1.22) for studies conducted in East Asia to 1.57 (95% CI, 1.23-2.01) for studies conducted in North America. Stratification of studies by mortality time point or by methicillin resistance did not impact heterogeneity.
Figure 3. Forest Plot of Adjusted Mortality in Female vs Male Patients With Staphylococcus aureus Bacteremia.
Evaluation of the Evidence
Given that this systematic review contained observational studies that accounted for confounding through statistical adjustment (ie, the adjusted analysis), the baseline strength of evidence was moderate. The mortality effect estimate was downrated due to a serious risk of bias because studies without a sex-difference in a univariable analysis would likely not have included this variable in a multivariable analysis. We did not have serious concerns about inconsistency, indirectness, imprecision, or publication bias. Therefore, the overall strength of evidence for the association of female sex with increased mortality risk in patients with SAB was low (eTable 2 in Supplement 1).
Discussion
In this systematic review and meta-analysis, we addressed the question of whether female sex is associated with increased mortality risk in patients with SAB. The included studies involved over 130 000 patients and identified an association between female sex and increased mortality risk in both unadjusted and adjusted analyses. Heterogeneity was observed, but substantially decreased with stratification by geographic region. This may reflect the large practice variations for SAB throughout the world, as recently described in a global survey.102
This study sheds new light on sex differences in clinical outcomes of patients with SAB, which is an area of little clarity. Few studies have primarily focused on sex differences in outcome in SAB patients, and their results have been contradictory. Some studies reported higher mortality in female patients with SAB compared with male patients,3,5 while others did not report an overall sex-difference in mortality.6,8 In this meta-analysis we identified a relatively large (18%) increased odds of death in female patients compared with male patients. This association was significant in both the unadjusted analysis and in an adjusted analysis that accounted for patient co-morbidities and treatment variables. Beyond patients with SAB, excess mortality has been reported in female patients with hospital-acquired bloodstream infection,103 severe sepsis,104,105,106 and endocarditis107; however, conflicting evidence has been reported as well.108
The underlying causes of sex differences in clinical outcomes of patients with SAB were not addressed in this study. Sex-related differences in outcome may be due to a variety of social or biological factors. Firm data for a biological connection between sex differences in clinical outcomes from animal models has been elusive. Previous studies on sepsis have generally supported better outcomes in female patients relative to male.109 This has been hypothesized to stem from the positive immunomodulatory properties of sex hormones on cell-mediated immune responses and cardiovascular functions in female patients110,111 as well as the suppression of the anti-infective response by testosterone in male patients.112 Even an ongoing immunological advantage in postmenopausal septic women has been reported.113 In S aureus infections in particular, an animal study showed enhanced neutrophil bactericidal capacity in female mice.114 However, females were more susceptible to lethal toxic shock caused by S aureus enterotoxin B in another mouse model.115 Social factors could also be contributing to the observed differences in mortality between female and male patients with SAB. Analogous to acute myocardial infarction, where women waited longer before seeking treatment relative to men, gender-differences in health seeking behavior may exist in SAB patients.116 Gender bias in health care delivery can potentially contribute to the difference in outcome as well. Delays in antibiotic treatment and less invasive treatment have been reported in women with septic shock and critical illness,105,117,118,119 and women were less likely to receive the recommended quality of acute care compared with men in a US study on quality of care in sociodemographic subgroups.120 In a 2023 cohort study from our research group,121 women with SAB received shorter durations of antimicrobial treatment and were less likely to undergo transesophageal echocardiography compared to men. Regional or cultural differences in health care delivery could be impacting the observed sex-based difference in patient outcomes. The association between female sex and mortality varied to some degree by location of study, and we have previously shown that there is considerable global variation in SAB treatment factors.102 Finally, response to treatment can differ between female and male patients. Both pharmacokinetics and pharmacodynamics are generally subject to sex influences.122
Limitations
This study had several limitations. First, sex difference was not the primary outcome of interest in the majority of the included studies. Therefore, a number of studies did not include adjusted data for mortality by sex, and inclusion of this data could have influenced the results. Second, reporting bias can exist as studies may not report mortality stratified by sex if there was no significant difference in mortality. Third, heterogeneity exists not only in study methodology but also in the disease itself. The clinical presentation of SAB may vary from uncomplicated intravenous catheter-related bacteremia to complicated metastatic disease. Because all studies on SAB patients were included in our study, sex-based differences in outcome could not be stratified by infection severity. Lastly, whether reported sex represented sex assigned at birth or gender, was often not specified.
Conclusions
In this systematic review and meta-analysis, observational cohort studies demonstrated an association between female sex and increased mortality risk in adult patients with SAB. This association remained significant after including only studies that adjusted for patient clinical and treatment variables. Future research should focus on understanding the underlying causes and on promoting better outcomes in female patients with SAB. Fundamental research on biological sex differences in immune response or pharmacology, examinations of sex-based differences in management of SAB, and better reporting of sex-specific outcomes in randomized clinical trials are necessary to better understand the observed sex-specific differences in mortality among patients with SAB.
eAppendix 1. Search Strategies
eAppendix 2. Newcastle-Ottawa Quality Assessment Scale for Assessing Risk of Bias in Observational Studies
eAppendix 3. Description of EPC Approach
eAppendix 4. Influence Analysis Unadjusted Mortality
eAppendix 5. Influence Analysis Adjusted Mortality
eTable 1. Newcastle-Ottawa Quality Assessment of Individual Studies
eFigure 1. Sensitivity Analysis Unadjusted Mortality
eFigure 2. Funnel Plot Unadjusted Mortality
eFigure 3. Sensitivity Analysis Adjusted Mortality
eFigure 4. Funnel Plot Adjusted Mortality
eTable 2. Evidence Profile for Association of Female Sex and Mortality in Patients With Staphylococcus Aureus Bacteremia
Data Sharing Statement
References
- 1.GBD 2019 Antimicrobial Resistance Collaborators . Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10369):2221-2248. doi: 10.1016/S0140-6736(22)02185-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB. Predictors of mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev. 2012;25(2):362-386. doi: 10.1128/CMR.05022-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smit J, López-Cortés LE, Kaasch AJ, et al. Gender differences in the outcome of community-acquired Staphylococcus aureus bacteraemia: a historical population-based cohort study. Clin Microbiol Infect. 2017;23(1):27-32. doi: 10.1016/j.cmi.2016.06.002 [DOI] [PubMed] [Google Scholar]
- 4.Austin ED, Sullivan SS, Macesic N, et al. Reduced mortality of staphylococcus aureus bacteremia in a retrospective cohort study of 2139 patients: 2007-2015. Clin Infect Dis. 2020;70(8):1666-1674. doi: 10.1093/cid/ciz498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mansur N, Hazzan R, Paul M, Bishara J, Leibovici L. Does sex affect 30-day mortality in Staphylococcus aureus bacteremia? Gend Med. 2012;9(6):463-470. doi: 10.1016/j.genm.2012.10.009 [DOI] [PubMed] [Google Scholar]
- 6.Forsblom E, Kakriainen A, Ruotsalainen E, Järvinen A. Comparison of patient characteristics, clinical management, infectious specialist consultation, and outcome in men and women with methicillin-sensitive Staphylococcus aureus bacteremia: a propensity-score adjusted retrospective study. Infection. 2018;46(6):837-845. doi: 10.1007/s15010-018-1216-3 [DOI] [PubMed] [Google Scholar]
- 7.Jokinen E, Laine J, Huttunen R, et al. Comparison of outcome and clinical characteristics of bacteremia caused by methicillin-resistant, penicillin-resistant and penicillin-susceptible Staphylococcus aureus strains. Infect Dis (Lond). 2017;49(7):493-500. doi: 10.1080/23744235.2017.1292046 [DOI] [PubMed] [Google Scholar]
- 8.Kang CK, Kwak YG, Park Y, et al. ; Korea INfectious Diseases (KIND) study group . Gender affects prognosis of methicillin-resistant Staphylococcus aureus bacteremia differently depending on the severity of underlying disease. Eur J Clin Microbiol Infect Dis. 2018;37(6):1119-1123. doi: 10.1007/s10096-018-3226-6 [DOI] [PubMed] [Google Scholar]
- 9.McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40-46. doi: 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 10.Covidence . Covidence systematic review software, Veritas Health Innovation. Accessed October 31, 2022. http://www.covidence.org
- 11.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomised studies in meta-analyses. Ottawa Hospital Research Institute website. Accessed January 10, 2023. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 12.Shor E, Roelfs D, Vang ZM. The “Hispanic mortality paradox” revisited: meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants’ mortality. Soc Sci Med. 2017;186:20-33. doi: 10.1016/j.socscimed.2017.05.049 [DOI] [PubMed] [Google Scholar]
- 13.Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ. 2014;348:f7450. doi: 10.1136/bmj.f7450 [DOI] [PubMed] [Google Scholar]
- 14.Mejer N, Westh H, Schønheyder HC, et al. ; Danish Staphylococcal Bacteraemia Study Group . Stable incidence and continued improvement in short term mortality of Staphylococcus aureus bacteraemia between 1995 and 2008. BMC Infect Dis. 2012;12:260. doi: 10.1186/1471-2334-12-260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Appendix C: The Odds Ratio as an Estimator of the Incidence Rate Ratio. In: Greenberg RS, Daniels SR, Flanders W, et al. Medical Epidemiology, 4th Edition. McGraw-Hill Companies; 2005. [Google Scholar]
- 16.Hartung J, Knapp G. On tests of the overall treatment effect in meta-analysis with normally distributed responses. Stat Med. 2001;20(12):1771-1782. doi: 10.1002/sim.791 [DOI] [PubMed] [Google Scholar]
- 17.Hartung J, Knapp G. A refined method for the meta-analysis of controlled clinical trials with binary outcome. Stat Med. 2001;20(24):3875-3889. doi: 10.1002/sim.1009 [DOI] [PubMed] [Google Scholar]
- 18.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkman ND, Lohr KN, Ansari MT, et al. Grading the strength of a body of evidence when assessing health care interventions: an EPC update. J Clin Epidemiol. 2015;68(11):1312-1324. doi: 10.1016/j.jclinepi.2014.11.023 [DOI] [PubMed] [Google Scholar]
- 20.Abbas M, Rossel A, de Kraker MEA, et al. Association between treatment duration and mortality or relapse in adult patients with Staphylococcus aureus bacteraemia: a retrospective cohort study. Clin Microbiol Infect. 2020;26(5):626-631. doi: 10.1016/j.cmi.2019.07.019 [DOI] [PubMed] [Google Scholar]
- 21.Allard C, Carignan A, Bergevin M, et al. Secular changes in incidence and mortality associated with Staphylococcus aureus bacteraemia in Quebec, Canada, 1991-2005. Clin Microbiol Infect. 2008;14(5):421-428. doi: 10.1111/j.1469-0691.2008.01965.x [DOI] [PubMed] [Google Scholar]
- 22.Ammerlaan H, Seifert H, Harbarth S, et al. ; European Practices of Infections with Staphylococcus aureus (SEPIA) Study Group . Adequacy of antimicrobial treatment and outcome of Staphylococcus aureus bacteremia in 9 Western European countries. Clin Infect Dis. 2009;49(7):997-1005. doi: 10.1086/605555 [DOI] [PubMed] [Google Scholar]
- 23.Asgeirsson H, Gudlaugsson O, Kristinsson KG, Heiddal S, Kristjansson M. Staphylococcus aureus bacteraemia in Iceland, 1995-2008: changing incidence and mortality. Clin Microbiol Infect. 2011;17(4):513-518. doi: 10.1111/j.1469-0691.2010.03265.x [DOI] [PubMed] [Google Scholar]
- 24.Ayau P, Bardossy AC, Sanchez G, et al. Risk factors for 30-day mortality in patients with methicillin-resistant Staphylococcus aureus bloodstream infections. Int J Infect Dis. 2017;61:3-6. doi: 10.1016/j.ijid.2017.05.010 [DOI] [PubMed] [Google Scholar]
- 25.Bai AD, Showler A, Burry L, et al. Comparative effectiveness of cefazolin versus cloxacillin as definitive antibiotic therapy for MSSA bacteraemia: results from a large multicentre cohort study. J Antimicrob Chemother. 2015;70(5):1539-1546. doi: 10.1093/jac/dku560 [DOI] [PubMed] [Google Scholar]
- 26.Bassetti M, Peghin M, Trecarichi EM, et al. Characteristics of Staphylococcus aureus bacteraemia and predictors of early and late mortality. PLoS One. 2017;12(2):e0170236. doi: 10.1371/journal.pone.0170236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Battle SE, Shuping M, Withers S, Justo JA, Bookstaver PB, Al-Hasan MN. Prediction of mortality in Staphylococcus aureus bloodstream infection using quick Pitt bacteremia score. J Infect. 2022;84(2):131-135. doi: 10.1016/j.jinf.2021.12.002 [DOI] [PubMed] [Google Scholar]
- 28.Ben-Zvi H, Drozdinsky G, Kushnir S, et al. Influence of GeneXpert MRSA/SA test implementation on clinical outcomes of Staphylococcus aureus bacteremia—a before-after retrospective study. Diagn Microbiol Infect Dis. 2019;93(2):120-124. doi: 10.1016/j.diagmicrobio.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 29.Benfield T, Espersen F, Frimodt-Møller N, et al. Increasing incidence but decreasing in-hospital mortality of adult Staphylococcus aureus bacteraemia between 1981 and 2000. Clin Microbiol Infect. 2007;13(3):257-263. doi: 10.1111/j.1469-0691.2006.01589.x [DOI] [PubMed] [Google Scholar]
- 30.Blomfeldt A, Eskesen AN, Aamot HV, Leegaard TM, Bjørnholt JV. Population-based epidemiology of Staphylococcus aureus bloodstream infection: clonal complex 30 genotype is associated with mortality. Eur J Clin Microbiol Infect Dis. 2016;35(5):803-813. doi: 10.1007/s10096-016-2601-4 [DOI] [PubMed] [Google Scholar]
- 31.Braquet P, Alla F, Cornu C, et al. ; VIRSTA-AEPEI study group . Factors associated with 12 week case-fatality in Staphylococcus aureus bacteraemia: a prospective cohort study. Clin Microbiol Infect. 2016;22(11):948.e1-948.e7. doi: 10.1016/j.cmi.2016.07.034 [DOI] [PubMed] [Google Scholar]
- 32.Chavez MA, Munigala S, Burnham CD, Yarbrough ML, Warren DK. The impact of implementing the virtuo blood culture system on the characteristics and management of patients with Staphylococcus aureus bacteremia. J Clin Microbiol. 2022;60(4):e0226121. doi: 10.1128/jcm.02261-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen PY, Chuang YC, Wang JT, Chang SC. Impact of prior healthcare-associated exposure on clinical and molecular characterization of methicillin-susceptible Staphylococcus aureus bacteremia: results from a retrospective cohort study. Medicine (Baltimore). 2015;94(5):e474. doi: 10.1097/MD.0000000000000474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen PY, Chuang YC, Wang JT, Sheng WH, Chen YC, Chang SC. Sequence type 8 as an emerging clone of methicillin-resistant Staphylococcus aureus causing bloodstream infections in Taiwan. Emerg Microbes Infect. 2021;10(1):1908-1918. doi: 10.1080/22221751.2021.1981158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen SY, Wang JT, Chen TH, et al. Impact of traditional hospital strain of methicillin-resistant Staphylococcus aureus (MRSA) and community strain of MRSA on mortality in patients with community-onset S aureus bacteremia. Medicine (Baltimore). 2010;89(5):285-294. doi: 10.1097/MD.0b013e3181f1851e [DOI] [PubMed] [Google Scholar]
- 36.Chihara S, et al. Staphylococcus aureus bacteriuria as a prognosticator for outcome of Staphylococcus aureus bacteremia: A case-control study. BMC Infect Dis. 2009;10:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chung H, Kim E, Yang E, et al. C-reactive protein predicts persistent bacteremia caused by community-acquired methicillin-resistant Staphylococcus aureus strain. Eur J Clin Microbiol Infect Dis. 2021;40(12):2497-2504. doi: 10.1007/s10096-021-04303-5 [DOI] [PubMed] [Google Scholar]
- 38.Cobussen M, van Tiel FH, Oude Lashof AML. Management of S. aureus bacteraemia in the Netherlands; infectious diseases consultation improves outcome. Neth J Med. 2018;76(7):322-329. [PubMed] [Google Scholar]
- 39.Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y. The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: mortality, length of stay, and hospital charges. Infect Control Hosp Epidemiol. 2005;26(2):166-174. doi: 10.1086/502522 [DOI] [PubMed] [Google Scholar]
- 40.Eells SJ, McKinnell JA, Wang AA, et al. A comparison of clinical outcomes between healthcare-associated infections due to community-associated methicillin-resistant Staphylococcus aureus strains and healthcare-associated methicillin-resistant S. aureus strains. Epidemiol Infect. 2013;141(10):2140-2148. doi: 10.1017/S0950268812002634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gasch O, Camoez M, Dominguez MA, et al. ; REIPI/GEIH Study Groups . Predictive factors for mortality in patients with methicillin-resistant Staphylococcus aureus bloodstream infection: impact on outcome of host, microorganism and therapy. Clin Microbiol Infect. 2013;19(11):1049-1057. doi: 10.1111/1469-0691.12108 [DOI] [PubMed] [Google Scholar]
- 42.Greenberg JA, David MZ, Hall JB, Kress JP. Immune dysfunction prior to Staphylococcus aureus bacteremia is a determinant of long-term mortality. PLoS One. 2014;9(2):e88197. doi: 10.1371/journal.pone.0088197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guillamet MCV, Vazquez R, Deaton B, Shroba J, Vazquez L, Mercier RC. Host-pathogen-treatment triad: host factors matter most in methicillin-resistant Staphylococcus aureus bacteremia outcomes. Antimicrob Agents Chemother. 2018;62(2):e01902-17. doi: 10.1128/AAC.01902-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hagstrand Aldman M, Kavyani R, Kahn F, Påhlman LI. Treatment outcome with penicillin G or cloxacillin in penicillin-susceptible Staphylococcus aureus bacteraemia: a retrospective cohort study. Int J Antimicrob Agents. 2022;59(4):106567. doi: 10.1016/j.ijantimicag.2022.106567 [DOI] [PubMed] [Google Scholar]
- 45.Hall RG II, Giuliano CA, Haase KK, et al. Empiric guideline-recommended weight-based vancomycin dosing and mortality in methicillin-resistant Staphylococcus aureus bacteremia: a retrospective cohort study. BMC Infect Dis. 2012;12:104. doi: 10.1186/1471-2334-12-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Han JH, Mascitti KB, Edelstein PH, Bilker WB, Lautenbach E. Effect of reduced vancomycin susceptibility on clinical and economic outcomes in Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2012;56(10):5164-5170. doi: 10.1128/AAC.00757-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Honda H, Krauss MJ, Jones JC, Olsen MA, Warren DK. The value of infectious diseases consultation in Staphylococcus aureus bacteremia. Am J Med. 2010;123(7):631-637. doi: 10.1016/j.amjmed.2010.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Horváth A, Dobay O, Sahin-Tóth J, et al. Characterisation of antibiotic resistance, virulence, clonality and mortality in MRSA and MSSA bloodstream infections at a tertiary-level hospital in Hungary: a 6-year retrospective study. Ann Clin Microbiol Antimicrob. 2020;19(1):17. doi: 10.1186/s12941-020-00357-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hsu LY, Loomba-Chlebicka N, Koh TH, Kang ML, Tan BH, Tambyah PA. EMRSA-15 bacteremia is not associated with a worse outcome compared with bacteremia caused by multidrug-resistant MRSA. Int J Biomed Sci. 2007;3(2):97-103. doi: 10.59566/IJBS.2007.3098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Joo EJ, Peck KR, Ha YE, et al. Impact of acute kidney injury on mortality and medical costs in patients with meticillin-resistant Staphylococcus aureus bacteraemia: a retrospective, multicentre observational study. J Hosp Infect. 2013;83(4):300-306. doi: 10.1016/j.jhin.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 51.Joost I, Kaasch A, Pausch C, et al. Staphylococcus aureus bacteremia in patients with rheumatoid arthritis—data from the prospective INSTINCT cohort. J Infect. 2017;74(6):575-584. doi: 10.1016/j.jinf.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 52.Jorgensen SCJ, Lagnf AM, Bhatia S, Rybak MJ. A new simplified predictive model for mortality in methicillin-resistant Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis. 2019;38(5):843-850. doi: 10.1007/s10096-018-03464-0 [DOI] [PubMed] [Google Scholar]
- 53.Kempker RR, Farley MM, Ladson JL, Satola S, Ray SM. Association of methicillin-resistant Staphylococcus aureus (MRSA) USA300 genotype with mortality in MRSA bacteremia. J Infect. 2010;61(5):372-381. doi: 10.1016/j.jinf.2010.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim D, Hong JS, Yoon EJ, et al. Toxic shock syndrome toxin 1-producing methicillin-resistant Staphylococcus aureus of clonal complex 5, the New York/Japan epidemic clone, causing a high early-mortality rate in patients with bloodstream infections. Antimicrob Agents Chemother. 2019;63(11):e01362-19. doi: 10.1128/AAC.01362-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim J, Gregson DB, Ross T, Laupland KB. Time to blood culture positivity in Staphylococcus aureus bacteremia: association with 30-day mortality. J Infect. 2010;61(3):197-204. doi: 10.1016/j.jinf.2010.06.001 [DOI] [PubMed] [Google Scholar]
- 56.Kim SH, Kim KH, Kim HB, et al. Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2008;52(1):192-197. doi: 10.1128/AAC.00700-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim T, Chong YP, Park KH, et al. Clinical and microbiological factors associated with early patient mortality from methicillin-resistant Staphylococcus aureus bacteremia. Korean J Intern Med. 2019;34(1):184-194. doi: 10.3904/kjim.2016.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kobayashi D, Yokota K, Takahashi O, Arioka H, Fukui T. A predictive rule for mortality of inpatients with Staphylococcus aureus bacteraemia: a classification and regression tree analysis. Eur J Intern Med. 2014;25(10):914-918. doi: 10.1016/j.ejim.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 59.Lamagni TL, Potz N, Powell D, Pebody R, Wilson J, Duckworth G. Mortality in patients with meticillin-resistant Staphylococcus aureus bacteraemia, England 2004-2005. J Hosp Infect. 2011;77(1):16-20. doi: 10.1016/j.jhin.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 60.Laupland KB, Harris PNA, Stewart AG, Edwards F, Paterson DL. Culture-based determinants and outcome of Staphylococcus aureus bloodstream infections. Diagn Microbiol Infect Dis. 2022;104(3):115772. doi: 10.1016/j.diagmicrobio.2022.115772 [DOI] [PubMed] [Google Scholar]
- 61.Lee CH, Chien CC, Liu JW. Timing of initiating glycopeptide therapy for methicillin-resistant Staphylococcus aureus bacteremia: the impact on clinical outcome. ScientificWorldJournal. 2013;2013:457435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee JE, Lee S, Park S, Lee SO, Lee SH. Impact of agr functionality on the outcome of patients with methicillin-susceptible Staphylococcus aureus bacteremia. Microbiol Spectr. 2021;9(1):e0011621. doi: 10.1128/Spectrum.00116-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee YW, Bae S, Yang E, et al. Clinical and microbiological characteristics of hospital-acquired methicillin-resistant Staphylococcus aureus bacteremia caused by a community-associated PVL-negative strain. Open Forum Infect Dis. 2021;8(9):ofab424. doi: 10.1093/ofid/ofab424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lesens O, Brannigan E, Bergin C, Christmann D, Hansmann Y. Impact of the use of aminoglycosides in combination antibiotic therapy on septic shock and mortality due to Staphylococcus aureus bacteremia. Eur J Intern Med. 2006;17(4):276-280. doi: 10.1016/j.ejim.2005.12.004 [DOI] [PubMed] [Google Scholar]
- 65.Maor Y, Hagin M, Belausov N, Keller N, Ben-David D, Rahav G. Clinical features of heteroresistant vancomycin-intermediate Staphylococcus aureus bacteremia versus those of methicillin-resistant S. aureus bacteremia. J Infect Dis. 2009;199(5):619-624. doi: 10.1086/596629 [DOI] [PubMed] [Google Scholar]
- 66.Melzer M, Welch C. Thirty-day mortality in UK patients with community-onset and hospital-acquired meticillin-susceptible Staphylococcus aureus bacteraemia. J Hosp Infect. 2013;84(2):143-150. doi: 10.1016/j.jhin.2012.12.013 [DOI] [PubMed] [Google Scholar]
- 67.Meredith J, Onsrud J, Davidson L, et al. Successful use of telemedicine infectious diseases consultation with an antimicrobial stewardship-led Staphylococcus aureus bacteremia care bundle. Open Forum Infect Dis. 2021;8(6):ofab229. doi: 10.1093/ofid/ofab229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mölkänen T, Ruotsalainen E, Rintala EM, Järvinen A. Predictive value of C-reactive protein (CRP) in identifying fatal outcome and deep infections in Staphylococcus aureus bacteremia. PLoS One. 2016;11(5):e0155644. doi: 10.1371/journal.pone.0155644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Murdoch F, Danial J, Morris AK, et al. The Scottish enhanced Staphylococcus aureus bacteraemia surveillance programme: the first 18 months of data in adults. J Hosp Infect. 2017;97(2):133-139. doi: 10.1016/j.jhin.2017.06.008 [DOI] [PubMed] [Google Scholar]
- 70.Nambiar K, Seifert H, Rieg S, et al. ; International Staphylococcus aureus collaboration (ISAC) study group (with linked authorship to members in the Acknowledgements) and the ESCMID Study Group for Bloodstream Infections and Sepsis (ESGBIS) . Survival following Staphylococcus aureus bloodstream infection: a prospective multinational cohort study assessing the impact of place of care. J Infect. 2018;77(6):516-525. doi: 10.1016/j.jinf.2018.08.015 [DOI] [PubMed] [Google Scholar]
- 71.Osthoff M, Sidler JA, Lakatos B, et al. Low-dose acetylsalicylic acid treatment and impact on short-term mortality in Staphylococcus aureus bloodstream infection: a propensity score-matched cohort study. Crit Care Med. 2016;44(4):773-781. doi: 10.1097/CCM.0000000000001554 [DOI] [PubMed] [Google Scholar]
- 72.Papadimitriou-Olivgeris M, Caruana G, Senn L, Guery B. Predictors of mortality of Staphylococcus aureus bacteremia among patients hospitalized in a Swiss university hospital and the role of early source control; a retrospective cohort study. Eur J Clin Microbiol Infect Dis. 2023;42(3):347-357. doi: 10.1007/s10096-023-04557-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Park KH, Chong YP, Kim SH, et al. Community-associated MRSA strain ST72-SCCmecIV causing bloodstream infections: clinical outcomes and bacterial virulence factors. J Antimicrob Chemother. 2015;70(4):1185-1192. doi: 10.1093/jac/dku475 [DOI] [PubMed] [Google Scholar]
- 74.Paulsen J, Mehl A, Askim Å, Solligård E, Åsvold BO, Damås JK. Epidemiology and outcome of Staphylococcus aureus bloodstream infection and sepsis in a Norwegian county 1996-2011: an observational study. BMC Infect Dis. 2015;15(1):116. doi: 10.1186/s12879-015-0849-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Perovic O, Koornhof H, Black V, Moodley I, Duse A, Galpin J. Staphylococcus aureus bacteraemia at two academic hospitals in Johannesburg. S Afr Med J. 2006;96(8):714-717. [PubMed] [Google Scholar]
- 76.Rieg S, Jonas D, Kaasch AJ, et al. Microarray-based genotyping and clinical outcomes of Staphylococcus aureus bloodstream infection: an exploratory study. PLoS One. 2013;8(8):e71259. doi: 10.1371/journal.pone.0071259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rieg S, Peyerl-Hoffmann G, de With K, et al. Mortality of S. aureus bacteremia and infectious diseases specialist consultation–a study of 521 patients in Germany. J Infect. 2009;59(4):232-239. doi: 10.1016/j.jinf.2009.07.015 [DOI] [PubMed] [Google Scholar]
- 78.Roth JA, Widmer AF, Tschudin-Sutter S, et al. The Model for End-stage Liver Disease (MELD) as a predictor of short-term mortality in Staphylococcus aureus bloodstream infection: a single-centre observational study. PLoS One. 2017;12(4):e0175669. doi: 10.1371/journal.pone.0175669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Saunderson RB, Gouliouris T, Nickerson EK, et al. Impact of routine bedside infectious disease consultation on clinical management and outcome of Staphylococcus aureus bacteraemia in adults. Clin Microbiol Infect. 2015;21(8):779-785. doi: 10.1016/j.cmi.2015.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schneider SM, Schaeg M, Gärtner BC, Berger FK, Becker SL. Do written diagnosis-treatment recommendations on microbiological test reports improve the management of Staphylococcus aureus bacteremia? a single-center, retrospective, observational study. Diagn Microbiol Infect Dis. 2020;98(4):115170. doi: 10.1016/j.diagmicrobio.2020.115170 [DOI] [PubMed] [Google Scholar]
- 81.Seas C, Garcia C, Salles MJ, et al. ; Latin America Working Group on Bacterial Resistance . Staphylococcus aureus bloodstream infections in Latin America: results of a multinational prospective cohort study. J Antimicrob Chemother. 2018;73(1):212-222. doi: 10.1093/jac/dkx350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Soriano A, Marco F, Martínez JA, et al. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46(2):193-200. doi: 10.1086/524667 [DOI] [PubMed] [Google Scholar]
- 83.Soriano A, Martínez JA, Mensa J, et al. Pathogenic significance of methicillin resistance for patients with Staphylococcus aureus bacteremia. Clin Infect Dis. 2000;30(2):368-373. doi: 10.1086/313650 [DOI] [PubMed] [Google Scholar]
- 84.Sullivan SB, Austin ED, Stump S, et al. Reduced vancomycin susceptibility of methicillin-susceptible Staphylococcus aureus has no significant impact on mortality but results in an increase in complicated infection. Antimicrob Agents Chemother. 2017;61(7):e00316-17. doi: 10.1128/AAC.00316-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Szubert A, Bailey SL, Cooke GS, et al. ; United Kingdom Clinical Infection Research Group (UKCIRG) . Predictors of recurrence, early treatment failure and death from Staphylococcus aureus bacteraemia: Observational analyses within the ARREST trial. J Infect. 2019;79(4):332-340. doi: 10.1016/j.jinf.2019.08.001 [DOI] [PubMed] [Google Scholar]
- 86.Tan K, Minejima E, Lou M, Mack WJ, Nieberg P, Wong-Beringer A. Cytokine measurements add value to clinical variables in predicting outcomes for Staphylococcus aureus bacteremia. BMC Infect Dis. 2021;21(1):317. doi: 10.1186/s12879-021-06010-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ternavasio-de la Vega HG, Castaño-Romero F, Ragozzino S, et al. The updated Charlson comorbidity index is a useful predictor of mortality in patients with Staphylococcus aureus bacteraemia. Epidemiol Infect. 2018;146(16):2122-2130. doi: 10.1017/S0950268818002480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Thorlacius-Ussing L, Sandholdt H, Larsen AR, Petersen A, Benfield T. Age-dependent increase in incidence of Staphylococcus aureus bacteremia, Denmark, 2008-2015. Emerg Infect Dis. 2019;25(5):875-882. doi: 10.3201/eid2505.181733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Thwaites GE; United Kingdom Clinical Infection Research Group (UKCIRG) . The management of Staphylococcus aureus bacteremia in the United Kingdom and Vietnam: a multi-centre evaluation. PLoS One. 2010;5(12):e14170. doi: 10.1371/journal.pone.0014170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tong SY, van Hal SJ, Einsiedel L, Currie BJ, Turnidge JD; Australian New Zealand Cooperative on Outcomes in Staphylococcal Sepsis . Impact of ethnicity and socio-economic status on Staphylococcus aureus bacteremia incidence and mortality: a heavy burden in Indigenous Australians. BMC Infect Dis. 2012;12:249. doi: 10.1186/1471-2334-12-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Turnidge JD, Kotsanas D, Munckhof W, et al. ; Australia New Zealand Cooperative on Outcomes in Staphylococcal Sepsis . Staphylococcus aureus bacteraemia: a major cause of mortality in Australia and New Zealand. Med J Aust. 2009;191(7):368-373. doi: 10.5694/j.1326-5377.2009.tb02841.x [DOI] [PubMed] [Google Scholar]
- 92.Turnidge JD, Nimmo GR, Pearson J, Gottlieb T, Collignon PJ; Australian Group on Antimicrobial Resistance . Epidemiology and outcomes for Staphylococcus aureus bacteraemia in Australian hospitals, 2005-06: report from the Australian Group on Antimicrobial Resistance. Commun Dis Intell Q Rep. 2007;31(4):398-403. [DOI] [PubMed] [Google Scholar]
- 93.van Hal SJ, Jones M, Gosbell IB, Paterson DL. Vancomycin heteroresistance is associated with reduced mortality in ST239 methicillin-resistant Staphylococcus aureus blood stream infections. PLoS One. 2011;6(6):e21217. doi: 10.1371/journal.pone.0021217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang JL, Chen SY, Wang JT, et al. Comparison of both clinical features and mortality risk associated with bacteremia due to community-acquired methicillin-resistant Staphylococcus aureus and methicillin-susceptible S. aureus. Clin Infect Dis. 2008;46(6):799-806. doi: 10.1086/527389 [DOI] [PubMed] [Google Scholar]
- 95.Wang JT, Hsu LY, Lauderdale TL, Fan WC, Wang FD. Comparison of outcomes among adult patients with nosocomial bacteremia caused by methicillin-susceptible and methicillin-resistant Staphylococcus aureus: a retrospective cohort study. PLoS One. 2015;10(12):e0144710. doi: 10.1371/journal.pone.0144710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang JT, Wu HS, Weng CM, Hsu LY, Wang FD. Prognosis of patients with methicillin-resistant Staphylococcus aureus bloodstream infection treated with teicoplanin: a retrospective cohort study investigating effect of teicoplanin minimum inhibitory concentrations. BMC Infect Dis. 2013;13:182. doi: 10.1186/1471-2334-13-182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wi YM, Rhee JY, Kang CI, Chung DR, Song JH, Peck KR. Clinical predictors of methicillin-resistance and their impact on mortality associated with Staphylococcus aureus bacteraemia. Epidemiol Infect. 2018;146(10):1326-1336. doi: 10.1017/S0950268818001255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Willekens R, Puig-Asensio M, Suanzes P, et al. Mortality in Staphylococcus aureus bacteraemia remains high despite adherence to quality indicators: secondary analysis of a prospective cohort study. J Infect. 2021;83(6):656-663. doi: 10.1016/j.jinf.2021.10.001 [DOI] [PubMed] [Google Scholar]
- 99.Yahav D, Schlesinger A, Shaked H, et al. Clinical presentation, management and outcomes of Staph aureus bacteremia (SAB) in older adults. Aging Clin Exp Res. 2017;29(2):127-133. doi: 10.1007/s40520-016-0543-4 [DOI] [PubMed] [Google Scholar]
- 100.Yilmaz M, Elaldi N, Balkan İİ, et al. Mortality predictors of Staphylococcus aureus bacteremia: a prospective multicenter study. Ann Clin Microbiol Antimicrob. 2016;15(1):7. doi: 10.1186/s12941-016-0122-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yoon YK, Park DW, Sohn JW, et al. Effects of inappropriate empirical antibiotic therapy on mortality in patients with healthcare-associated methicillin-resistant Staphylococcus aureus bacteremia: a propensity-matched analysis. BMC Infect Dis. 2016;16:331. doi: 10.1186/s12879-016-1650-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Westgeest AC, Buis DTP, Sigaloff KCE, Ruffin F, et al. Global differences in the management of Staphylococcus aureus bacteremia: no international standard of care. Clin Infect Dis. 2023;77(8):1092-1101. doi: 10.1093/cid/ciad363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Leibovici L, Paul M, Weinberger M, et al. Excess mortality in women with hospital-acquired bloodstream infection. Am J Med. 2001;111(2):120-125. doi: 10.1016/S0002-9343(01)00771-9 [DOI] [PubMed] [Google Scholar]
- 104.Sakr Y, Elia C, Mascia L, et al. The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care. 2013;17(2):R50. doi: 10.1186/cc12570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pietropaoli AP, Glance LG, Oakes D, Fisher SG. Gender differences in mortality in patients with severe sepsis or septic shock. Gend Med. 2010;7(5):422-437. doi: 10.1016/j.genm.2010.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vincent JL, Sakr Y, Sprung CL, et al. ; Sepsis Occurrence in Acutely Ill Patients Investigators . Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34(2):344-353. doi: 10.1097/01.CCM.0000194725.48928.3A [DOI] [PubMed] [Google Scholar]
- 107.Varela Barca L, Vidal-Bonnet L, Fariñas MC, et al. ; GAMES Investigators . Analysis of sex differences in the clinical presentation, management and prognosis of infective endocarditis in Spain. Heart. 2021;107(21):1717-1724. doi: 10.1136/heartjnl-2021-319254 [DOI] [PubMed] [Google Scholar]
- 108.Adrie C, Azoulay E, Francais A, et al. ; OutcomeRea Study Group . Influence of gender on the outcome of severe sepsis: a reappraisal. Chest. 2007;132(6):1786-1793. doi: 10.1378/chest.07-0420 [DOI] [PubMed] [Google Scholar]
- 109.Lakbar I, Einav S, Lalevée N, Martin-Loeches I, Pastene B, Leone M. Interactions between gender and sepsis-implications for the future. Microorganisms. 2023;11(3):746. doi: 10.3390/microorganisms11030746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Angele MK, Pratschke S, Hubbard WJ, Chaudry IH. Gender differences in sepsis: cardiovascular and immunological aspects. Virulence. 2014;5(1):12-19. doi: 10.4161/viru.26982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhang MQ, Macala KF, Fox-Robichaud A, Mendelson AA, Lalu MM; Sepsis Canada National Preclinical Sepsis Platform . Sex- and gender-dependent differences in clinical and preclinical sepsis. Shock. 2021;56(2):178-187. doi: 10.1097/SHK.0000000000001717 [DOI] [PubMed] [Google Scholar]
- 112.Gay L, Melenotte C, Lakbar I, et al. Sexual dimorphism and gender in infectious diseases. Front Immunol. 2021;12:698121. doi: 10.3389/fimmu.2021.698121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Thompson KJ, Finfer SR, Woodward M, Leong RNF, Liu B. Sex differences in sepsis hospitalisations and outcomes in older women and men: a prospective cohort study. J Infect. 2022;84(6):770-776. doi: 10.1016/j.jinf.2022.04.035 [DOI] [PubMed] [Google Scholar]
- 114.Castleman MJ, Pokhrel S, Triplett KD, et al. Innate sex bias of Staphylococcus aureus skin infection is driven by α-hemolysin. J Immunol. 2018;200(2):657-668. doi: 10.4049/jimmunol.1700810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Faulkner L, Altmann DM, Ellmerich S, Huhtaniemi I, Stamp G, Sriskandan S. Sexual dimorphism in superantigen shock involves elevated TNF-alpha and TNF-alpha induced hepatic apoptosis. Am J Respir Crit Care Med. 2007;176(5):473-482. doi: 10.1164/rccm.200611-1712OC [DOI] [PubMed] [Google Scholar]
- 116.Mnatzaganian G, Braitberg G, Hiller JE, Kuhn L, Chapman R. Sex differences in in-hospital mortality following a first acute myocardial infarction: symptomatology, delayed presentation, and hospital setting. BMC Cardiovasc Disord. 2016;16(1):109. doi: 10.1186/s12872-016-0276-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG. Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med. 2003;31(7):1901-1907. doi: 10.1097/01.CCM.0000069347.78151.50 [DOI] [PubMed] [Google Scholar]
- 118.Madsen TE, Napoli AM. The DISPARITY-II study: delays to antibiotic administration in women with severe sepsis or septic shock. Acad Emerg Med. 2014;21(12):1499-1502. doi: 10.1111/acem.12546 [DOI] [PubMed] [Google Scholar]
- 119.Fowler RA, Sabur N, Li P, et al. Sex-and age-based differences in the delivery and outcomes of critical care. CMAJ. 2007;177(12):1513-1519. doi: 10.1503/cmaj.071112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Asch SM, Kerr EA, Keesey J, et al. Who is at greatest risk for receiving poor-quality health care? N Engl J Med. 2006;354(11):1147-1156. doi: 10.1056/NEJMsa044464 [DOI] [PubMed] [Google Scholar]
- 121.Westgeest AC, Ruffin F, Kair JL, et al. The association of female sex with management and mortality in patients with Staphylococcus aureus bacteraemia. Clin Microbiol Infect. 2023;29(9):1182-1187. doi: 10.1016/j.cmi.2023.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Soldin OP, Mattison DR. Sex differences in pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 2009;48(3):143-157. doi: 10.2165/00003088-200948030-00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Search Strategies
eAppendix 2. Newcastle-Ottawa Quality Assessment Scale for Assessing Risk of Bias in Observational Studies
eAppendix 3. Description of EPC Approach
eAppendix 4. Influence Analysis Unadjusted Mortality
eAppendix 5. Influence Analysis Adjusted Mortality
eTable 1. Newcastle-Ottawa Quality Assessment of Individual Studies
eFigure 1. Sensitivity Analysis Unadjusted Mortality
eFigure 2. Funnel Plot Unadjusted Mortality
eFigure 3. Sensitivity Analysis Adjusted Mortality
eFigure 4. Funnel Plot Adjusted Mortality
eTable 2. Evidence Profile for Association of Female Sex and Mortality in Patients With Staphylococcus Aureus Bacteremia
Data Sharing Statement