Abstract
To identify key factors affecting all-cause mortality in the elderly aged 80 years and above. Data from Chinese Longitudinal Healthy Longevity Survey (2011-2018) were utilized (N = 3993). A healthy lifestyle score was obtained by assigning 8 factors: smoking, drinking, exercise, sleep duration, social activity, waist circumference, BMI, and healthful plant-based diet index. Cox regression and decision tree model were used to identify factors influencing the mortality risk. Lifestyle and activities of daily living (ADL) were 2 of the most important modifiable factors influencing the mortality risk of the oldest seniors. A higher healthy lifestyle score was associated with lower mortality risk. The HR (95% CI) of death risk in Q2, Q3, and Q4 groups were 0.91 (0.81-1.01), 0.78 (0.71-0.86), and 0.64 (0.58-0.71), respectively, when compared with the Q1 group of healthy lifestyle score. Elderly with ADL disability had a higher mortality rate than those without ADL disability. When the elderly already have ADL disability, the healthier the lifestyle, the lower the mortality rate. Among individuals aged 80 to 89 years with ADL disability, the mortality rate was higher in the healthy lifestyle score Q1-Q2 groups (92.1%) than that in the Q3-Q4 groups (71.6%). Similar results were observed among subjects aged 90 to 99 years with ADL disability (Q1-Q2: 97.9%, Q3-Q4: 92.1%). For centenarians without ADL disability, maintaining a healthy lifestyle significantly reduced mortality (Q1-Q3: 90.5%, Q4: 75.5%). Caregivers should prioritize the consideration of lifestyle and ADL in their healthcare practices of the oldest old.
Keywords: lifestyle, activities of daily living, mortality, oldest old, healthcare
What do we already know about this topic?
As we know, the results of many studies have shown that there are various factors that affect the mortality risk of older adults, including lifestyle, ADL.
How does your research contribute to the field?
Identify key influences on all-cause mortality in the oldest old, evaluate their prioritization, to inform the development of health care for primary caregivers of the oldest old.
What are your research’s implications toward theory, practice, or policy?
To provide a research basis for the future development of health care policies and health monitoring programs for the elderly in China.
Introduction
Currently, there are about 190 million elderly people aged 65 and above in China, accounting for 13.5% of the total population, and elderly people aged 80 and above account for about 2.54 % of the total population, 1 life expectancy has reached 78.2 years. 2 A study 3 showed that by 2035, life expectancy per capita is expected to reach 81.3 years on the mainland, with female life expectancy reaching as high as 90 years in some areas.
With the gradual trend of advanced aging in China’s population, the care needs of the elderly are increasing rapidly. Focusing on the risk factors for adverse outcomes in the elderly will help improve their quality of life and prolong their healthy lifespan, which is of great significance in reducing the burden of disease and the overall economic burden on society, and realizing healthy aging. Numerous studies have shown that lifestyle, such as smoking, alcohol consumption, and diet, is closely related to the development of chronic diseases and the risk of death, and that a healthy lifestyle can reduce the risk of death in older people.4 -6 However, there are few large cohort studies on the relationship between overall lifestyle and mortality risk among Chinese seniors aged 80 years and older. Even fewer studies have been done on centenarians. More importantly, of the relevant factors affecting mortality in the elderly, which are the indicators that are more deserving of prioritized attention and monitoring by medical institution, nursing homes, and caregivers. These issues remain to be further studied, that is the contribution and innovation of this study.
Methods
Data Source
The data for this study were obtained from the “Peking University Open Research Data Platform” Chinese Longitudinal Healthy Longevity Survey (CLHLS) 2011 to 2018 tracking dataset. The CLHLS project, which is one of the world’s largest cohorts of the oldest old to date, randomly selected about half of the cities and counties in 23 provinces/municipalities/autonomous regions across the country and conducted 8 surveys from 1998 to 2018. The CLHLS adopted a targeted random-sample design, collected data of centenarians as much as possible within the sampled counties and cities, and matched for gender and age groups (nonagenarians, octogenarians, and young-old aged 65-79 years) living in the same area with the centenarians to ensure representativeness. More detailed information on the study population has been published previously. 7 Participants were interviewed by uniformly trained workers with a standard questionnaire (available online: https://opendata.pku.edu.cn/dataverse/CHADS). The quality of data in CLHLS has been systematically assessed for reliability, validity, and consistency.7,8 The project was reviewed by the Ethics Committee of Peking University (Grant No. IRB00001052-13074), and all research subjects or their proxies who participated in the investigation signed an informed consent form.
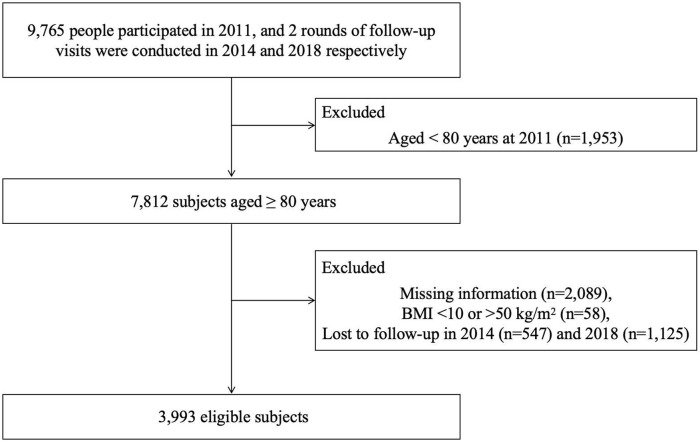
In total, 9765 people participated in the 2011 wave, and 2 rounds of follow-up visits were conducted in 2014 and 2018 respectively. Those who were younger than 80 years of age at the time of the 2011 survey (1953), those with missing information (2089), those with a BMI <10 or >50 kg/m2 (58), and those who were lost to follow-up in 2014 (547) and 2018 (1125) were excluded, and a final total of 3993 participants were included for analysis (See Figure 1).
Figure 1.
Flow chart for subject identification.
Measures
Based on the results of the questionnaire, relevant data were collected from the study participants in 2011, including age, gender, knee height, weight, waist circumference, region (city, town, rural), presence of cohabitants (with family, living alone, living in a nursing home), education level (0, 1-5, 6-9, ≥10 years), economic level (rated as poor, average, or rich based on the self-rating of the study participants), main occupation before 60 years old (institutional & professional and technical, industrial and commercial services, agriculture& forestry& fishery, unemployed or other), marital status (not in marriage, in marriage or cohabiting), sleep duration (<6 h/d, 6-10 h/d, ≥10 h/d), smoking (never, ever, now), drinking (never, ever, now), exercise (never, ever, now), social activities, dietary intake, disease status, and ability to perform activities of daily living. Information on outcome (death or survival) in the study population was obtained from follow-up surveys in 2014 and 2018.
BMI and waist circumference (WC)
Considering that the elderly usually have a hunched back and cannot be measured upright, height (cm) is indirectly estimated by knee height (cm) 9 : Male height = 67.78 + 2.01 × knee height, female height = 74.08 + 1.81 × knee height. BMI=weight (kg)/height2 (m2), BMI is categorized according to the latest published range of appropriate body weight for the elderly in China 9 : low (BMI < 22.0 kg/m2), appropriate (22.0 ≤ BMI<26.9 kg/m2), high (BMI ≥ 26.9 kg/m2). WC≥85cm for men and ≥80cm for women is defined as excess waist circumference. 10
Chronic diseases or disorders
These include hypertension, diabetes mellitus, dyslipidemia, cardiovascular and cerebrovascular disease, pulmonary disease, ophthalmic disease, cancer, gastrointestinal ulcers, Parkinson’s disease, decubitus ulcers, arthritis, cognitive impairment, epilepsy, gallbladder disease, rheumatism or rheumatoid rheumatism, chronic nephritis, hepatitis, visual and auditory impairments, and teeth loss, with the disease determinations being based on the self-reporting of the respondents and the diagnosis of the disease by the hospitals. Of which cognitive impairment: self-reported and diagnosed dementia or a score of < 18 on the Mini-mental State Examination (MMSE) 11 (Total score 30). Multimorbidity was defined as the number of chronic diseases (NCD) ≥2 in the study population. Activities of daily living (ADL) disability is recognized as requiring assistance in any of the 6 categories: bathing, eating, dressing, transfers, toileting, and continence. 12
Social activities
The frequency of the 8 types of activities “housework (cooking, taking care of kids), outdoor activities (Tai Ji, square dance, visit friends, etc.), garden work, reading newspapers/books, raising domestic animals, playing cards and/or mahjong, watching TV and/ or listening to the radio, and organized social activities” was assigned a score of 7 for “almost every day,” 3 for “sometimes,” and 0 for “never,” A total score of all these 8 activities was created (range from 0 to 56) and grouped by quartiles Q1 (0-2), Q2 (3-9), Q3 (10-19), and Q4 (20-56).
Healthy plant-based diet index (hPDI)
The foods in the questionnaire were categorized into healthful plant foods (grains, fruits, vegetables, nuts, soy products, mushrooms and algae, garlic, tea, and vegetable oils), less-healthful plant foods (pickles or kimchi, white sugar or candies, and refined grains), and animal products (dairy, meat, fish and other aquatic products, eggs, and animal fat), and each item was assigned a score ranging from 1 to 5 points based on intake to obtain the hPDI.13,14 Among them, healthful plant foods were positively scored according to the frequency of intake from high to low, with higher frequency of intake resulting in larger scores, while less-healthful plant foods and animal products were negatively scored according to the frequency of intake from high to low, with higher frequency of intake resulting in smaller scores (See Table 1). The total score ranges from 15 to 75 and is grouped by quartiles Q1(0-42), Q2(43-45), Q3(46-48), and Q4(≥49).
Table 1.
Healthy Plant-based Diet Index Scoring Scale.
| Type of food | Frequency of intake (assigned points) |
|---|---|
| Healthful plant foods | |
| °Vegetable oils, miscellaneous grain crops | Frequent (5), infrequent (1) |
| °Fruits, vegetables | Daily/almost daily (5), often (4), sometimes (2), rarely or never (1) |
| °Nuts, soybean products, mushrooms, garlic, tea | Almost daily (5), ≥1 time per week (4), ≥1 time per month (3), sometimes (2), rarely or never (1) |
| Less-healthful plant foods | |
| °Sugar, refined cereals, pickles or sauerkraut | Almost daily (1), ≥1 time per week (2), ≥1 time per month (3), sometimes (4), rarely or never (5) |
| Animal products | |
| °Dairy products, eggs, fish and other aquatic products, meat | Almost daily (1), ≥1 time per week (2), ≥1 time per month (3), sometimes (4), rarely or never (5) |
| °Animal fat | Frequent (1), infrequent (5) |
Healthy lifestyle score
Eight factors including smoking, drinking, exercise, sleep duration, social activities, BMI, WC, and hPDI were assigned to obtain a healthy lifestyle score. The total score was 2 to 17, grouped by quartiles Q1 (0-8), Q2 (9), Q3 (10-11), and Q4 (≥12), with higher scores indicating a healthier combined lifestyles. The specific scoring criteria are shown in Table 2.
Table 2.
Definitions of Healthy Lifestyle Score.
| Factors | Level (assigned points) |
|---|---|
| Smoking15,16 | Never (2), ever (1), now (0) |
| Drinking17 -19 | Never (2), ever (1), now (0) |
| Exercise 20 | Now (2), ever (1), never (0) |
| Sleep duration21,22 | 6-10 h/d (1), < 6 h/d (0), ≥10 h/d (0) |
| Social activities23,24 | Q4 (4), Q3 (3), Q2 (2), Q1 (1) |
| BMI 25 | Appropriate (1), high (0), low (0) |
| WC 26 | Normal (1), excessive (0) |
| hPDI13,27,28 | Q4 (4), Q3 (3), Q2 (2), Q1 (1) |
Statistical Analysis
SPSS 23.0 was used for data analysis, with p-values < .05 being considered statistically significant. Measurements were expressed as (x̄±s), and comparisons between groups were analyzed by ANOVA. Count data were expressed as n (%), and comparisons between groups were analyzed by χ2.
To investigate the association between healthy lifestyle score and all-cause mortality, we used Cox proportional regression models to estimate HRs and 95% CIs. Model 1 adjusted for age and gender. Model 2 further adjusted for region, education, occupation before age 60, economic level, marital status, ADL disability, and multimorbidity. Model 3 excludes subjects who died within 1 year of enrollment as sensitivity analyses. The CHAID decision tree model used outcome (death or survival) as the dependent variable, and the 7 factors screened by Cox multivariate regression, namely age, gender, region, marital status, ADL disability, multimorbidity, and healthy lifestyle score, as the independent variables. The maximum depth of the CHAID decision tree was set to 3 levels, the minimum number of cases for parent nodes was 100, and the minimum number of cases for child nodes was 50. Split-sample validation was set up, where 70% of the randomly selected study population was used as a training set to construct the model, and the remaining 30% was used as a test set to examine the accuracy of the constructed model.
Results
Sample Characteristics
A total of 3993 study participants were finally included in this study for analysis, including 1634 (40.9%) males and 2359 (59.1%) females. Age was 92.1 ± 7.6 years, of which 1622 (40.6%) were 80 to 89 years old, 1512 (37.9%) were 90 to 99 years old, and 859 (21.5%) were ≥ 100 years old. Study subjects were followed up for an average of 3.5 ± 2.4 years, with a cumulative total of 13 919 person-years of follow-up. There were 3117 (78.1%) deaths and 876 (21.9%) survivors during the follow-up period.
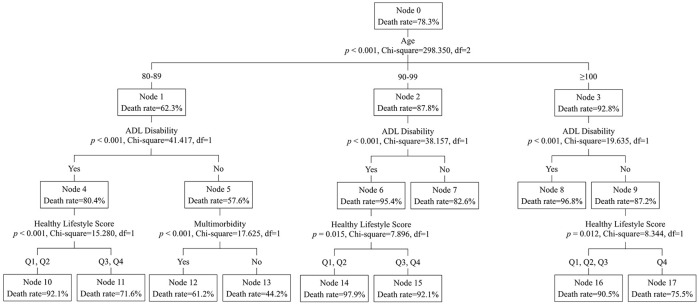
The participants were divided into 4 groups Q1-Q4 according to the quartiles of the healthy lifestyle score. The 4 groups were statistically different (P < .05) in age, region, marital status, education, economic level, occupation before age 60, smoking, drinking, exercise, hPDI, sleep duration, social activities, BMI, WC, ADL disability, NCD, and outcomes (Table 3). Figure 2 showed a significant difference in the proportion of survival among the 4 groups (P < .001).
Table 3.
Distribution of Basic Characteristics of Participants.
| Healthy lifestyle score | F/χ2 | P | ||||
|---|---|---|---|---|---|---|
| Q1 (n = 991) | Q2 (n = 598) | Q3 (n = 1246) | Q4 (n = 1158) | |||
| Age, years | 94.4 ± 7.6 | 93.2 ± 7.4 | 92.1 ± 7.6 | 89.5 ± 7.1 | 83.224 | <0.001 |
| Male, n (%) | 432(26.4%) | 245(15.0%) | 479(29.3%) | 478(29.3%) | 6.152 | 0.104 |
| Married/cohabiting, n (%) | 166(19.4%) | 107(12.5%) | 276(32.3%) | 305(35.7%) | 34.330 | <0.001 |
| Years of education (0), n (%) | 738(26.8%) | 420(15.3%) | 889(32.3%) | 704(25.6%) | 67.567 | <0.001 |
| Rural areas, n (%) | 588(28.4%) | 307(14.8%) | 682(32.9%) | 497(24.0%) | 80.407 | <0.001 |
| Economic level (average), n (%) | 662(25.4%) | 409(15.7%) | 810(31.0%) | 730(28.0%) | 47.189 | <0.001 |
| Institutional/professional, n (%) | 26(12.3%) | 23(10.8%) | 52(24.5%) | 111(52.4%) | 94.549 | <0.001 |
| Smoking (now), n (%) | 250(41.5%) | 113(18.8%) | 165(27.4%) | 74(12.3%) | 197.247 | <0.001 |
| Drinking (now), n (%) | 290(45.4%) | 105(16.4%) | 168(26.3%) | 76(11.9%) | 296.414 | <0.001 |
| Exercise (now), n (%) | 49(4.1%) | 75(6.3%) | 310(26.1%) | 752(63.4%) | 1122.294 | <0.001 |
| Sleep duration (6-10 h/d), n (%) | 292(14.6%) | 269(13.5%) | 657(32.9%) | 778(39.0%) | 323.387 | <0.001 |
| Social activity score Q4, n (%) | 56(5.4%) | 72(7.0%) | 307(29.8%) | 596(57.8%) | 1397.758 | <0.001 |
| BMI (appropriate), n (%) | 85(14.8%) | 72(12.5%) | 156(27.2%) | 261(45.5%) | 107.631 | <0.001 |
| WC (normal), n (%) | 543(22.9%) | 365(15.4%) | 749(31.6%) | 711(30.0%) | 11.542 | 0.009 |
| ADL disability, n (%) | 532(38.1%) | 250(17.9%) | 411(29.4%) | 204(14.6%) | 320.323 | <0.001 |
| NCD (≥2), n (%) | 926(26.4%) | 543(15.5%) | 1092(31.1%) | 952(27.1%) | 74.866 | <0.001 |
| hPDI Q4, n (%) | 49(4.6%) | 81(7.5%) | 352(32.7%) | 594(55.2%) | 1148.856 | <0.001 |
| Deaths, n (%) | 882(28.3%) | 510(16.4%) | 952(30.5%) | 773(24.8%) | 175.937 | <0.001 |
Figure 2.
Kaplan-Meier survive curves by healthy lifestyle score.
Factors Affecting Mortality Risk in the Oldest Old
The results of multifactorial Cox regression showed that age, gender, region, marital status, ADL disability, multimorbidity, and healthy lifestyle score were the main influences on mortality in the elderly (Figure 3).
Figure 3.

Forest plot of factors influencing all-cause mortality among the oldest old.
Note. Adjusted for age, gender, region, education, occupation before age 60, economic level, marital status, ADL disability, and multimorbidity coexistence.
Among these factors, the risk of death in the elderly was significantly negatively correlated with the healthy lifestyle score (P for trend < 0.001), meaning that the higher the healthy lifestyle score, the lower the risk of death in the elderly. After multifactorial adjustment (Model 2), the HR (95% CI) of death risk in Q2, Q3, and Q4 groups were 0.91 (0.81-1.01), 0.78 (0.71-0.86), and 0.64 (0.58-0.71), respectively, when compared with the Q1 group of healthy lifestyle score. Similar results (Model 3) were obtained from the sensitivity analyses (Table 4).
Table 4.
Relationship Between Healthy Lifestyle Score and All-Cause Mortality Risk Among the Oldest Old.
| Healthy lifestyle score | Deaths/person-years | Death density (/1000 person-years) | HR (95% CI) | ||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||
| Q1(0-8) | 882/2632 | 335.11 | 1.00(Ref) | 1.00(Ref) | 1.00(Ref) |
| Q2(9) | 510/1841 | 277.02 | 0.87(0.78-0.97) * | 0.91(0.81-1.01) | 0.95(0.84-1.08) |
| Q3(10-11) | 952/4425 | 215.14 | 0.72(0.66-0.79) ** | 0.78(0.71-0.86) ** | 0.81(0.73-0.90) ** |
| Q4(≥12) | 773/5021 | 153.95 | 0.56(0.51-0.62) ** | 0.64(0.58-0.71) ** | 0.67(0.59-0.75) ** |
| P for trend | - | - | <0.001 | <0.001 | <0.001 |
Note. Model 1 adjusted for age and sex; Model 2 adjusted for age, sex, region, education, occupation before age 60, economic level, marital status, ADL disability, and multimorbidity; Model 3 excludes subjects who died within 1 year of enrollment as sensitivity analyses.
P < .05 and **P < .001, which is statistically significant.
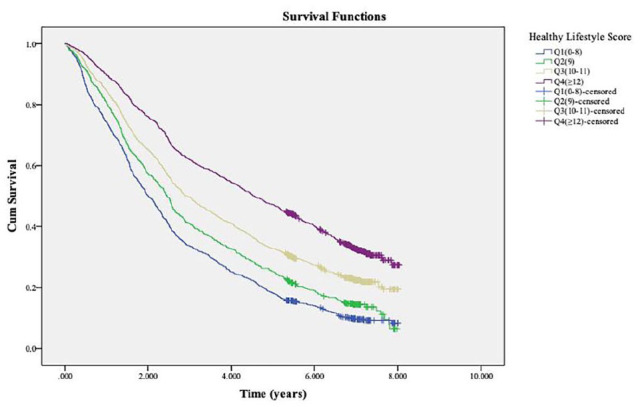
The 7 factors screened by Cox regression were used as independent variables and the outcome was used as the dependent variable in the CHAID decision tree model. The overall correctness of the model was 79.1%, with a good classification effect (Table 5). The results showed (Figure 4) that age, ADL disability, healthy lifestyle score, and multimorbidity may be more important (P < .05) in influencing the risk of mortality among the oldest old compared to the 3 factors of region, marital status, and gender. Among these, lifestyle and ADL were key modifiable factors. The mortality rate increased gradually with age (P < .001) and was 62.3%, 87.8%, and 92.8% in the 80 to 89, 90 to 99, and ≥ 100 age groups, respectively. Regardless of age, the mortality rate of the elderly with ADL disability was significantly higher than that of the elderly without ADL disability (P < .001). The mortality rates of the elderly with ADL disability in the 80 to 89, 90 to 99, and ≥ 100-year-old groups were 80.4%, 95.4%, and 96.8%, respectively. In contrast, the mortality rates of the elderly without ADL disability were 57.6%, 82.6%, and 87.2%, respectively.
Table 5.
Decision Tree Model Detection Correctness.
| Sample | Observed | Predicted | Percent correct (%) | |
|---|---|---|---|---|
| Survival | Death | |||
| Training | Survive | 106 | 490 | 17.8% |
| Death | 84 | 2067 | 96.1% | |
| Overall percentage | 6.9% | 93.1% | 79.1% | |
| Test | Survive | 55 | 225 | 19.6% |
| Death | 38 | 928 | 96.1% | |
| Overall percentage | 7.5% | 92.5% | 78.9% | |
Figure 4.
Decision tree model for all-cause mortality risk in the oldest old.
Healthy lifestyle score had an effect on mortality in all age groups of the elderly (P < .05). Among older adults aged 80 to 89 years with ADL disability, the mortality rate was higher in the healthy lifestyle score Q1 and Q2 groups (92.1%) than that in the Q3 and Q4 groups (71.6%); among older adults aged 80 to 89 years and without ADL disability, whether or not there was multimorbidity had a greater impact on mortality, with higher mortality rates among those who had multimorbidity (61.2%). Those with no chronic disease or only one chronic disease had lower mortality (44.2%).
Among older adults aged 90 to 99 years with ADL disability, those with lower healthy lifestyle scores in Q1 and Q2 had a higher mortality rate (97.9%) and those in the Q3 and Q4 groups had a lower mortality rate (92.1%), whereas among those ≥100 years old without ADL disability, the group with the highest healthy lifestyle scores (the Q4 group) had a lower mortality rate (75.5%), and the remaining 3 groups had a higher mortality rate (90.5%).
Discussion
Lifestyle and Mortality Risk
This study discovered a significant inverse relationship between combined healthy lifestyles and the risk of all-cause mortality in the oldest old. Compared with the lowest lifestyle score group (Q1), the risk of death decreased by 9%, 22%, and 36% in groups Q2, Q3, and Q4, respectively. However, the difference between groups Q2 and Q1 did not reach statistical significance. Possible explanations for this lack of significance include potential confounding factors such as advanced age, falls, and other accidents, as well as the relatively small sample size of the Q2 group. The results of the decision tree analysis also suggested that in the 80 to 89 and 90 to 99 age groups, older adults who already had ADL disability were at less risk of death if they lived in healthier lifestyles (Q3, Q4). For centenarians who already had a very high risk of death themselves, mortality was significantly reduced if they had unlimited ADL mobility and adopted a relatively healthier lifestyle (Q4). Numerous studies have demonstrated the importance of single or combined lifestyle interventions, such as a balanced diet, smoking cessation and alcohol restriction, and regular exercise, for managing body weight, 29 regulating metabolic markers,4,30 improving prognosis, 31 and decreasing the risk of death5,28,32 in older adults.
Conversely, healthier combined lifestyles mean that seniors tend to have good dietary habits, regular exercise, socialization, and are relatively more likely to have better nutritional status, cognitive function, muscle function, and muscular strength, leading to better physical health.33,34 In addition, some studies have shown that lifestyle is associated with factors such as an individual’s education, economic level, and whether or not he or she lives alone. 35 Therefore, a healthy lifestyle may also suggest that the individual is more capable to manage his or her health problems, afford health care, and is more likely to receive timely care, therefore has a relatively lower risk of death.
ADL and Mortality Risk
This study found that among the 7 factors affecting the death of the elderly, 4 factors, namely, age, ADL, lifestyle, and multimorbidity, were more important than gender, region, and marital status. Two modifiable factors among them, ADL disability and lower lifestyle score harmed the death of elderly people of all ages, suggesting that for elderly people aged 80 years and above, priority attention needs to be given to their ADL and if they are no longer able to perform activities of daily living independently, more attention needs to be paid to healthy lifestyles.
ADL is an individual’s ability to independently maintain basic life activities, and ADL dependence can lead to decreased quality of life, extra depletion of caregiving resources, increased disease burden and financial burden, and higher mortality risk in older adults.12,36 The main reasons are: (1) ADL is closely related to muscle strength, muscle mass, and function. 37 On the one hand, the rate of muscle attenuation accelerates significantly with age, especially after the age of 60 years, 38 which in turn leads to a reduction in muscle mass, a decrease in the level of muscle strength, a limitation of somatic mobility, and an increase in the risk of ADL disability. On the other hand, when ADL disability occurs, it tends to further exacerbate muscle decay due to limited physical activity, which increases the risk of falls, fractures, and death in the elderly. 39 (2) Some studies have found that ADL can be an important predictor of cognitive impairment in older adults, 40 and limited ADL ability in older adults may also be a sign of cognitive decline, diminished sensory abilities, or psychiatric problems such as depression, leading to an increased risk of incapacitation and death. (3) In addition, findings by Hyejin et al 41 , Kim et al 42 have shown that older adults with ADL dependence and activity limitations are more likely to have unmet healthcare needs than those with normal ADL ability. As a result, their quality of life, health status, and disease outcomes are compromised, and they are at higher risk of death.43,44
Strengths and Limitations
The data used in this study came from a large-sample long-term cohort, with a representative sample covering 23 provinces, municipalities, and autonomous regions across China, and the data collection process was professional and reliable. However, there are still limitations in the study itself, including (1) the information on various lifestyles was self-reported by the respondents or proxies, which may result in a certain degree of recall bias; (2) only baseline data on lifestyles were included, and there was no detailed analyses of changes during the follow-up period and their impact on the outcomes; (3) there is only qualitative information on the frequency of intake for diets and no quantitative data on nutrients intake; (4) no subdivision of the severity of disease and ADL disability was made, which may have different effects on the outcomes.
Conclusion
In conclusion, age, ADL, lifestyle, and multimorbidity are important factors affecting the risk of death in the elderly aged 80 years and older, of which lifestyle and ADL are 2 important modifiable factors. In caring for the elderly in the future, medical institutions and caregivers should, on the one hand, pay more attention to the improvement of indoor and outdoor facilities that are suitable for the elderly, to prevent the partial or complete loss of mobility as a result of accidents. On the other hand, they should recognize high-risk factors and carry out graded health management, so as to take early precautions. At this stage in China, the assessment of mobility, cognition, and other functions of the elderly is often done when patients visit the doctor for various disease reasons, such as recurrent fractures and memory loss. If health management records are established in the community and routine monitoring or intervention is piloted for those at high risk, such as those with ADL disability or with unhealthy life habits, and if detection, diagnosis and treatment are carried out as early as possible via regular nutritional assessment, screening for muscle decay (grip strength, walking speed, etc.), management of chronic diseases (reminding of medication taking and regular follow-ups), this will help to retard the progress of function loss in the elderly, and to minimize the occurrence of additional disease burdens, or serious adverse consequences such as disability and death caused by delayed diagnosis and treatment.
Supplemental Material
Supplemental material, sj-pdf-1-inq-10.1177_00469580241235755 for Lifestyle and ADL Are Prioritized Factors Influencing All-Cause Mortality Risk Among Oldest Old: A Population-Based Cohort Study by Zhiwen Ge, Cheng Li, Yaru Li, Nan Wang and Zhongxin Hong in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-2-inq-10.1177_00469580241235755 for Lifestyle and ADL Are Prioritized Factors Influencing All-Cause Mortality Risk Among Oldest Old: A Population-Based Cohort Study by Zhiwen Ge, Cheng Li, Yaru Li, Nan Wang and Zhongxin Hong in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
We would like to acknowledge all the subjects who participated in the Chinese Longitudinal Healthy Longevity Survey (CLHLS).
Footnotes
Author Contributions: GE Zhi-wen: Conception and design of study, analysis and interpretation of data, and preparation of manuscript. LI Cheng: Constructive discussions. LI Ya-ru: Constructive discussions. WANG Nan: Constructive discussions. HONG Zhong-xin: Constructive discussions. All authors have read and approved the final manuscript.
Data Availability: The CLHLS questionnaires are available online at https://opendata.pku.edu.cn/dataverse/CHADS. The datasets analyzed in this study are available from the corresponding author upon reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Statement: The study was approved by the Ethics Committee of Peking University (Grant No. IRB00001052-13074). All research subjects or their proxies who participated in the investigation signed an informed consent form.
ORCID iD: Zhongxin Hong  https://orcid.org/0000-0002-9070-046X
https://orcid.org/0000-0002-9070-046X
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Statistics NBo. Seventh national census bulletin. China Information News. 2021;2021:002. [Google Scholar]
- 2. China NHCotPsRo. Statistical bulletin of China’s health development in 2021. Chin Pr J Rural Dr. 2022;29(9):1-11. [Google Scholar]
- 3. Bai R, Liu Y, Zhang L, et al. Projections of future life expectancy in China up to 2035: a modelling study. Lancet Public Health. 2023;8(12):e915-e922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in Type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753-2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Colpani V, Baena CP, Jaspers L, et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur J Epidemiol. 2018;33(9):831-845. [DOI] [PubMed] [Google Scholar]
- 6. Han H, Cao Y, Feng C, et al. Association of a healthy lifestyle with All-Cause and cause-specific mortality among individuals with type 2 diabetes: a prospective study in UK biobank. Diabetes Care. 2022;45(2):319-329. [DOI] [PubMed] [Google Scholar]
- 7. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. 2017;389(10079):1619-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu E, Feng Y, Yue Z, Zhang Q, Han T. Differences in the health behaviors of elderly individuals and influencing factors: evidence from the Chinese Longitudinal Healthy Longevity Survey. Int J Health Plann Manage. 2019;34(4):e1520-e1532. [DOI] [PubMed] [Google Scholar]
- 9. Chinese Nutrition Society. [Appropriate range of body mass index and body weight management guidelines for Chinese oldest old (T/CNSS 021-2023)]. Chin J Endemiol. 2023;44(9):1335-1337. [DOI] [PubMed] [Google Scholar]
- 10. Zhai Y, Zhao WH, Chen CM. [Verification on the cut-offs of waist circumference for defining central obesity in Chinese elderly and tall adults]. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31(6):621-625. [PubMed] [Google Scholar]
- 11. Gao M, Kuang W, Qiu P, et al. The time trends of cognitive impairment incidence among older Chinese people in the community: based on the CLHLS cohorts from 1998 to 2014. Age Ageing. 2017;46(5):787-793. [DOI] [PubMed] [Google Scholar]
- 12. Mlinac ME, Feng MC. Assessment of activities of daily living, self-care, and independence. Arch Clin Neuropsychol. 2016;31(6):506-516. [DOI] [PubMed] [Google Scholar]
- 13. Kim H, Caulfield LE, Rebholz CM. Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J Nutr. 2018;148(4):624-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhu A, Chen H, Shen J, et al. Interaction between plant-based dietary pattern and air pollution on cognitive function: a prospective cohort analysis of Chinese older adults. Lancet Reg Heal Pac. 2022;20:100372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hu Y, Zong G, Liu G, et al. Smoking cessation, weight change, type 2 diabetes, and mortality. New Engl J Med. 2018;379(7):623-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yang JJ, Yu D, Wen W, et al. Tobacco smoking and mortality in Asia: a pooled meta-analysis. JAMA Netw Open. 2019;2(3):e191474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burton R, Sheron N. No level of alcohol consumption improves health. Lancet. 2018;392(10152):987-988. [DOI] [PubMed] [Google Scholar]
- 18. GBDA Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10152):1015-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rumgay H, Shield K, Charvat H, et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22(8):1071-1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. Br Med J. 2019;366:l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Han H, Wang Y, Li T, et al. Sleep duration and risks of incident cardiovascular disease and mortality among people with type 2 diabetes. Diabetes Care. 2023;46(1):101-110. [DOI] [PubMed] [Google Scholar]
- 22. Svensson T, Saito E, Svensson AK, et al. Association of sleep duration with all- and major-cause mortality among adults in Japan, China, Singapore, and Korea. JAMA Netw Open. 2021;4(9):e2122837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lamar M, James BD, Glover CM, et al. Social engagement and all-cause mortality: a focus on participants of the minority aging research study. Am J Prev Med. 2022;63(5):700-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith RW, Barnes I, Green J, et al. Social isolation and risk of heart disease and stroke: analysis of two large UK prospective studies. Lancet Public Health. 2021;6(4):E232-E239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bhaskaran K, dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar S. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. Br Med J. 2020;370:m3324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sotos-Prieto M, Struijk EA, Fung TT, et al. Association between the quality of plant-based diets and risk of frailty. J Cachexia Sarcopenia Muscle. 2022;13(6):2854-2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shan Z, Wang F, Li Y, et al. Healthy eating patterns and risk of total and cause-specific mortality. JAMA Intern Med. 2023;183(2):142-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haywood C, Sumithran P. Treatment of obesity in older persons-a systematic review. Obes Rev. 2019;20(4):588-598. [DOI] [PubMed] [Google Scholar]
- 30. Moura A, Paz S, Frota K, Carvalho C. Lifestyle associated with risk of metabolic syndrome in adults and the elderly. Nutrition. 2022;99-100:111647. [DOI] [PubMed] [Google Scholar]
- 31. Rolandi E, Frisoni GB, Cavedo E. Efficacy of lifestyle interventions on clinical and neuroimaging outcomes in elderly. Ageing Res Rev. 2016;25:1-12. [DOI] [PubMed] [Google Scholar]
- 32. Zhang YB, Pan XF, Chen J, et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. J Epidemiol Community Health. 2021;75(1):92-99. [DOI] [PubMed] [Google Scholar]
- 33. Volpato S, Bianchi L, Cherubini A, et al. Prevalence and clinical correlates of sarcopenia in community-dwelling older people: application of the EWGSOP definition and diagnostic algorithm. J Gerontol A Biol Sci Med Sci. 2014;69(4):438-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gao Q, Hu K, Yan C, et al. Associated factors of sarcopenia in community-dwelling older adults: a systematic review and meta-analysis. Nutrients. 2021;13(12):4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ning Y, Li J, Yin Z, Xiao L. Study on prevalence of healthy lifestyle among Chinese elderly in 22 provinces and the health promotion strategy for the elderly. Chin J Heal Educ. 2022;38(3):240-243. [Google Scholar]
- 36. Millán-Calenti JC, Tubío J, Pita-Fernández S, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010;50(3):306-310. [DOI] [PubMed] [Google Scholar]
- 37. Wang DXM, JYao J, Zirek Y, ReijnierseEM EM, Maier AB. Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle. 2020;11(1):3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Xie WQ, Xiao GL, Fan YB, et al. Sarcopenic obesity: research advances in pathogenesis and diagnostic criteria. Aging Clin Exp Res. 2021;33(2):247-252. [DOI] [PubMed] [Google Scholar]
- 39. Zhou J, Liu B, Qin MZ, Liu JP. A prospective cohort study of the risk factors for new falls and fragility fractures in self-caring elderly patients aged 80 years and over. BMC Geriatr. 2021;21(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fauth EB, Schwartz S, Tschanz JT, et al. Baseline disability in activities of daily living predicts dementia risk even after controlling for baseline global cognitive ability and depressive symptoms. Int J Geriatr Psychiatry. 2013;28(6):597-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hyejin L, Bumjo O, Sunyoung K, Kiheon L. Adl/ IADL dependencies and unmet healthcare needs in older persons: a nationwide survey. Arch Gerontol Geriatr. 2021;96:104458. [DOI] [PubMed] [Google Scholar]
- 42. Kim YS, Lee J, Moon Y, et al. Unmet healthcare needs of elderly people in Korea. BMC Geriatr. 2018;18(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Musich S, Wang SS, Ruiz J, Hawkins K, Wicker E. The impact of mobility limitations on health outcomes among older adults. Geriatr Nurs. 2018;39(2):162-169. [DOI] [PubMed] [Google Scholar]
- 44. Lindström C, Rosvall M, Lindström M. Unmet health-care needs and mortality: a prospective cohort study from southern Sweden. Scand J Public Health. 2020;48(3):267-274.31405329 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-inq-10.1177_00469580241235755 for Lifestyle and ADL Are Prioritized Factors Influencing All-Cause Mortality Risk Among Oldest Old: A Population-Based Cohort Study by Zhiwen Ge, Cheng Li, Yaru Li, Nan Wang and Zhongxin Hong in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-pdf-2-inq-10.1177_00469580241235755 for Lifestyle and ADL Are Prioritized Factors Influencing All-Cause Mortality Risk Among Oldest Old: A Population-Based Cohort Study by Zhiwen Ge, Cheng Li, Yaru Li, Nan Wang and Zhongxin Hong in INQUIRY: The Journal of Health Care Organization, Provision, and Financing