Abstract
Introduction
Non-traumatic wrist disorders (NTWD) are commonly encountered yet sparse resources exist to aid management. This study aimed to produce a literature map regarding diagnosis, management, pathways of care and outcome measures for NTWDs in the United Kingdom.
Methods
An interdisciplinary team of clinicians and academic researchers used Joanna Briggs Institute guidelines and the PRISMA ScR checklist in this scoping review. A mixed stakeholder group of patients and healthcare professionals identified 16 questions of importance to which the literature was mapped. An a-priori search strategy of both published and non-published material from five electronic databases and grey literature resources identified records. Two reviewers independently screened records for inclusion using explicit eligibility criteria with oversight from a third. Data extraction through narrative synthesis, charting and summary was performed independently by two reviewers.
Results
Of 185 studies meeting eligibility criteria, diagnoses of wrist pain, De Quervain’s syndrome and ulna-sided pain were encountered most frequently, with uncontrolled non-randomised trial or cohort study being the most frequently used methodology. Diagnostic methods used included subjective questioning, self-reported pain, palpation and special tests. Best practice guidelines were found from three sources for two NTWD conditions. Seventeen types of conservative management, and 20 different patient-reported outcome measures were suggested for NTWD.
Conclusion
Substantial gaps in evidence exist in all parts of the patient journey for NTWD when mapped against an analytic framework (AF). Opportunities exist for future rigorous primary studies to address these gaps and the preliminary concerns about the quality of the literature regarding NTWD.
Keywords: Non-traumatic wrist disorder, wrist pain, wrist injury, clinical pathways, conservative management
Introduction
Wrist pain is commonly encountered with an annual consultation rate of 58 in 10,000 patients in primary care in the UK. 1 Its incidence increases in people who engage in physically demanding occupations and for sportspeople where 10% have been found to have short-term pain, and 24% have medium-term pain. 2 Non-modifiable associations with wrist pain include older age and female sex. 2 In the UK’s National Health Service (NHS), a typical clinical pathway for patients with wrist disorders would see initial diagnosis and management in primary care, with referral through a musculoskeletal service for further diagnostic assessment and treatment in secondary care based on clinical need.3,4
The main pathological causes of non-traumatic wrist disorders (NTWD) include carpal osteoarthritis (OA), tendinopathies (including De Quervain’s and intersection syndrome), ulnar-sided wrist pathologies (itself made up of sub-groups with poor diagnostic validity),5–11 and ganglion. NTWD are distinct from basal thumb and hand osteoarthritis based on the clinical burden, risk factor profile, clinical relevance of synovial inflammation and established therapeutic interventions, however there is a degree of overlap between pantrapezial and wrist OA.12,13 Other presentations considered distinct from NTWD due to established diagnostic criteria, and condition-specific care pathways and management strategies include rheumatoid arthritis, 14 carpal tunnel syndrome15–17 and complex regional pain syndrome, 18 and were excluded from this study.
Uncertainty in various parts of the journey of care for people with wrist and hand pain was highlighted in a James Lind Alliance Priority Setting Partnership.19,20 Specifically, stakeholders identified a need for more information on which surgical and conservative methods enable efficient return to function, and which patient-reported outcomes are most useful in measuring the effectiveness of management. Although this review is limited to non-surgical literature these findings were a motivating factor to assessing the literature regarding NTWD in this review. In order to set research questions that are derived from stakeholder and patient involvement, 21 this review convened a mixed stakeholder group to identify key areas for investigation.
The NHS Long Term Plan 22 recommends patient-centred models of care through ‘shared decision making’ over historic paternalistic models which emphasise expert opinion and passive care and states this is a pressing need as rates of non-communicable diseases rise and questions around musculoskeletal management are increasingly raised. 23 Lewis and O’Sullivan caution that trends toward an unwarranted specific musculoskeletal diagnosis in non-traumatic conditions are placing strain on health budgets and may divert resources from ‘high-value’ person-centred care, to the prioritisation of ‘low-value’ interventions targeted at uncertain diagnostic categories. 24 When evaluating musculoskeletal care for the shoulder, low back and knee, pathoanatomical diagnosis frequently fails to explain the sufferers’ pain experience and disability in non-traumatic disorders, nor improve outcomes, leading to recommendations for the use of grouped conditions to frame management.25–27 This viewpoint has synergy with The Management of Wrist Pain Group (MOWP) which suggests grouping specific non-traumatic wrist diagnoses into a broader category of non-traumatic wrist pain 28 to promote holistic rather than lesion-specific management. Through mapping the literature of all diagnoses making up NTWD, the areas of strength for particular categories can be identified.
This scoping review aims to identify the evidence for the diagnosis, management, pathways of care and outcome measures for both grouped and individual NTWD and produce a coherent and comprehensive map of key evidence gaps to direct future research.
Methods
A protocol for the review was registered on the Open Science Framework prior to conducting any searches: https://osf.io/mxz59/.
Study team composition
The review team of six comprised clinicians, academics, subject area specialists and a design-led expert.
Scoping review framework
Scoping review methodology allows a systematic approach to map evidence into poorly understood areas 29 and draws on evidence from both empirical research and grey literature sources. The current study adopted the academic standard Joanna Briggs Institute (JBI) methodology 29 for scoping reviews and the PRISMA-ScR checklist. 30
Developing a rationale and identifying the research questions
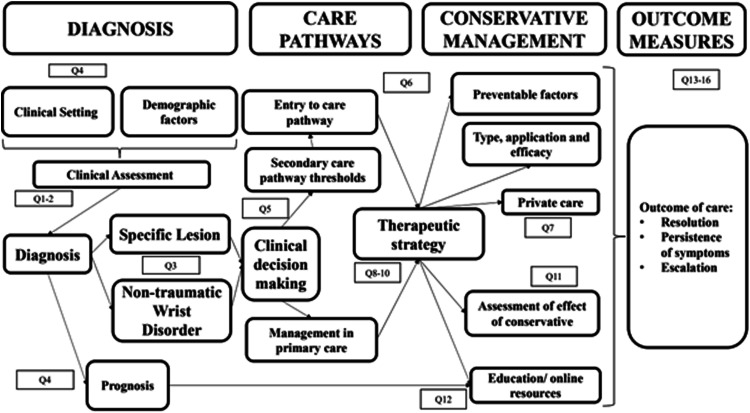
Although stakeholder involvement is not a requirement of scoping reviews, we considered that the engagement of both people suffering with NTWD, and providers of care was important to create a robust knowledge map. Individual interviews were conducted with three people diagnosed with NTWD, one primary care clinician, one secondary care clinician and one service commissioner. A video explaining the initial aims of the review and asking for their opinion about what questions are important to investigate in the field was shown to interviewees at the beginning of the consultation. A thematic narrative synthesis of interview transcripts, using an inductive approach,31,32 identified 16 research questions regarded as important by stakeholders. These questions were grouped into the four domains of interest (diagnosis, conservative management, pathways of care and outcomes) (Table 1) allowing an Analytic Framework (AF) to be produced which the literature was mapped against (Figure 1).
Table 1.
Research domains and questions identified from stakeholder interviews.
| Domain | |
|---|---|
| A | Diagnosis |
| Q1 | What elements comprise the diagnosis of non-traumatic wrist disorder and how are they staged? |
| Q2 | What is the performance of diagnostic methods for specific structural diagnosis? |
| Q3 | Does specific diagnosis alter management? |
| Q4 | Do diagnoses differ based on patient demographics, duration of symptoms clinical setting or the clinician’s role and experience? |
| B | Pathways of care |
| Q5 | What are the care pathways for non-traumatic wrist disorders, do they differ between settings and how are they compiled? |
| Q6 | What are the diagnostic criteria required for entry into care pathways and what features of wrist presentations inform escalation or removal from the pathway? |
| Q7 | How does private provision of care differ from National Health Service and how does it fit within care pathways. |
| C | Conservative management |
| Q8 | What conservative management is delivered for non-traumatic wrist disorder? |
| Q9 | Which interventions are most cost-effective and time efficient and does patient choice influence interventions selection? |
| Q10 | Does any clinical setting show superiority? |
| Q11 | Do pathways align with best use of interventions, and how do you know when an intervention has been effective and how does this feed into ongoing care? |
| Q12 | Where are the best patient resources held, and are the messages consistent with best practise? |
| Q13 | How long does it take to get better from non-traumatic wrist disorder? |
| D | Outcome measures |
| Q14 | Which measures are used and what are their reliability, validity, and responsiveness for non-traumatic wrist disorder? |
| Q15 | Is there a difference between outcomes of surgery, conservative care, and sham, and does more care equate with better outcome? |
| Q16 | How do outcome measures inform management, diagnosis or assess effectiveness of interventions? |
Figure 1.
Analytic framework based on clinical journey of NTWD with key domains and related research questions.
Identifying relevant studies
The three-step method recommended by the JBI guidelines for scoping reviews was followed. The search strategy was intended to be broad to identify both published and unpublished (grey) literature. Initially a narrow search of Google Scholar and MEDLINE database was used to identify key literature with additional studies identified through a snowballing technique using SCOPUS to identify related literature and citations from more recent work. The University of Tasmania guide to developing search terms 33 was applied, and we performed an analysis of the found studies to identify text words and key words relevant to the area. MeSh terms were collated via Medline to create the search strategy for Step 2 of the review (Supplementary section - 1). We applied this to MEDLINE then to PUBMED, OT Seeker, PeDRO and SPORTDiscus with minor adaptations made ad hoc to fit database requirements. Finally, a snowballing technique and citation search from key articles using SCOPUS was applied, combined with asking experts in the field for their recommended papers.
To allow non-journal and grey literature sources to be identified, we searched a variety of ‘grey literature’ databases and library catalogues via OpenGrey and Library Hub Discover (formally COPAC). Doctoral theses were identified via Ethos and ProQuest and clinical trial registers were screened via the World Health Organisation International Clinical Trials Registry Platform and the NIHR’s ‘Be Part of Research’ platform. Finally, clinical resources from BMJ Best Practice, NICE Evidence Standards Framework, the Cochrane Library and Trip were searched.
Study selection
The titles and abstracts of studies identified in the literature search were uploaded into Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) and duplicates removed.
Explicit a priori eligibility criteria (Supplementary Section 1) were applied at Level 1 (title and abstract) and Level 2 (full text) screening. A record was included if it provided an answer to at least one of the 16 research questions (Table 1) in the analytic framework (Figure 1) and did not meet any of the exclusion criteria. The Population, Concept and Context (PCC) method proposed by JBI were used to guide the identification and inclusion of published studies of all methodologies.
Population
Studies of people diagnosed with wrist disorders without traumatic origin were identified as the population. Those with clear history or radiological evidence of substantial trauma were excluded (i.e., scaphoid fracture/distal radius fracture/fracture clinic patients). Those with a history of less substantial minor trauma were not excluded. People who have had surgical management for their non-traumatic wrist disorder were excluded as were athletes.
Concept
The concept of interest in this review included the means of assessment for non-traumatic wrist disorders, conservative/non-operative interventions commonly administered, and the pathways of care and outcome measures used in primary and secondary care.
Context
This review considered both primary and secondary healthcare settings as each are part of the continuum of care for non-traumatic wrist disorders in the UK. The research questions arose from the consultation exercise to allow a broad approach considering the patient journey, clinician input and wider management structures.
Screening
Material that appeared to meet the initial screen of title and abstract was retrieved as complete reports and matched against the inclusion criteria leading to acceptance or discard by two reviewers (TM & SR), followed by a review of the full texts (TM & SR). Disagreements that arose between the reviewers were resolved through discussion, or consulting with a third reviewer (BD).
Data extraction and synthesis
The two primary researchers (TM & SR) extracted the following data for each included article:
• Authors, year of publication, country of origin.
• Research question, aims and domains selected by study authors.
• Methods: study design.
• Participants: number of participants included, eligibility criteria, sociodemographic data (sex and age).
• Non-traumatic wrist disorder diagnostic method.
• Pathways of care.
• Management modality administered including its parameters.
• Outcome measures and indications for escalation discharge or self-management.
Literature was appraised using qualitative synthesis and related to the analytic framework and its key domains and research questions. A knowledge map assessing the extent to which the analytic framework met by the literature was formed and used to identify gaps in the literature and research priorities in future clinical research.
Results
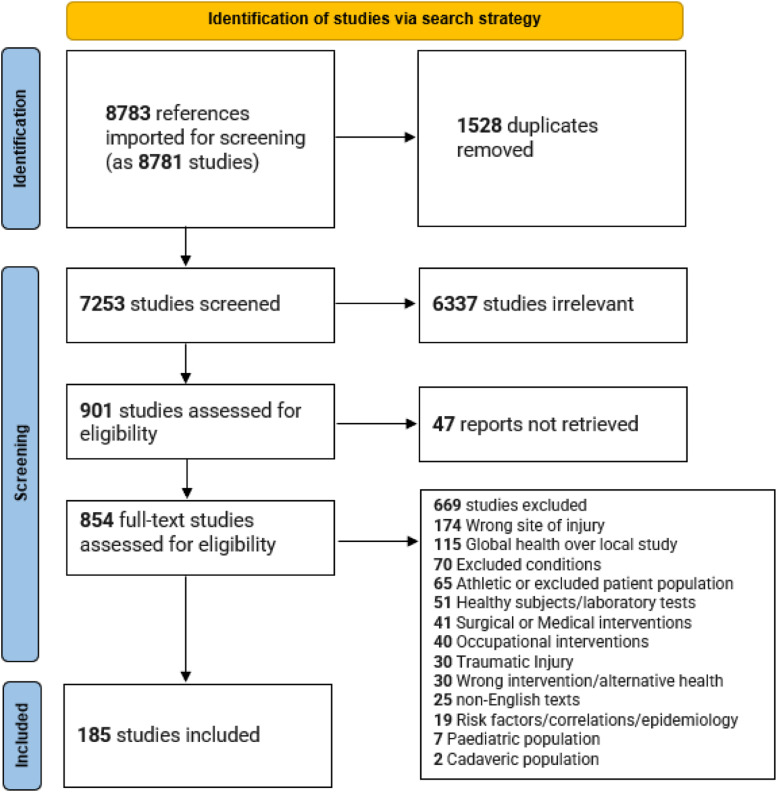
The initial search strategy identified 8767 documents, with 16 added from a search of cited references giving a total of 8783 sources (Figure 2). 1528 duplicates were removed, and screening of titles and abstracts resulted in 901 documents selected for full-text assessment. There were 47 instances where full text was unavailable, 669 did not meet the eligibility criteria, leaving 185 suitable for inclusion (Supplementary Section 2).
Figure 2.
PRISMA flow diagram for NTWD scoping review.
The general study characteristics (Table 2) of the sample identified the most common conditions referenced were wrist pain (44 studies, 23.8%), de Quervain’s (38 studies, 20.5%) and grouped ulna-sided diagnoses were represented in 22 articles (11.9%). Where the setting was recorded, secondary care was present in 107 texts (57.8%), primary care in 11 texts (5.9%), community services in nine texts (4.9%), private practice in six texts (3.2) and mixed settings in 10 texts (5.4%). Uncontrolled nonrandomized trials (71/38.4%) were the most common study design, of which 11 (5.9%) were prospective studies, 33 (17.8%) were retrospective cross-sectional studies and 24 were case series (13.0%). Case reports accounted for 27 sources (14.6%). There were 16 systematic reviews (8.1%) of which 7 focused on de Quervain's and regarding wrist pain and ganglion respectively, seven literature reviews (3.8%) and a single scoping review (0.5%). 17 ‘clinician guides’ which uncritically describe how-to perform assessment or treatment (9.2%) were identified, and opinion pieces made up eight texts (4.3%).
Table 2.
General study characteristics.
| Study characteristics. | Studies N = 185 | (%) | |
|---|---|---|---|
| Geographic origin. | |||
| USA | 7,8,34–71 | 40 | 21.6 |
| UK | 72–94 | 22 | 11.9 |
| Australia | 10,95–103 | 13 | 7.0 |
| Netherlands | 6,104–115 | 12 | 6.5 |
| Italy | 116–124 | 8 | 4.3 |
| Other | 90 | 48.6 | |
| Main presentation of interest. | |||
| Wrist pain | 5,10,34,38–40,45,50–52,54,55,62,63,65,67,68,71,76,80,88–90,99,102,103,106,109–111,114,125–141 | 44 | 23.8 |
| De Quervain’s | 36,42–44,46,47,59,72,74,77,78,85,93,97,97,105,108,119,122,131,142–161 | 38 | 20.5 |
| Ulna-sided | 8,9,48,58,66,87,94,113,118,162–175 | 22 | 11.9 |
| Carpal instabilities | 35–37,57,64,69,95,100,104,107,176–181 | 14 | 7.6 |
| Intersection syndrome | 49,53,60,61,121,124,182 | 7 | 3.8 |
| Ganglion | 44,56,73,82,115,183 | 6 | 3.2 |
| Nerve entrapment | 56,120,184–186 | 5 | 2.7 |
| Wrist OA | 75,186–188 | 4 | 2.2 |
| Other tendinopathy/paratendon | 92,123,189 | 3 | 1.6 |
| Dorsal-sided pain | 74,122,190 | 3 | 1.6 |
| Radial-sided pain | 70,191 | 2 | 1.1 |
| Red flags | 64,83,91,192–194 | 6 | 3.2 |
| Volar-sided pain | 7,116 | 2 | 1.1 |
| Care setting. | |||
| Secondary care | 6,7,9,10,36,38,40,43–45,48–50,53,56–58,61,63,67,70–72,77,80,85–87,89,90,92,94,95,97,99,103,105–107,108–111,113,116,118,120,124,125,127,129,131,133,137,139,143–145,149–155,159,161,163–165,169–174,176–178,181–183,185,187,189,191–193,195,196,199–205 | 107 | 57.8 |
| Primary care | 3,13,31,41,62,65,79,118,125,135,175 | 11 | 5.9 |
| Community service | 34,65,102,130,138,140,165,206,207 | 8 | 4.3 |
| Private practice | 47,78,126,160,190,198 | 6 | 3.2 |
| Mixed | 45,72,77,92,97,105,149,159,197 | 10 | 5.4 |
| Study design | |||
| Systematic review | 2,8,44,44,45,72,75,97,98,105,115,117,119,149,159,197 | 16 | 8.4 |
| DeQuervain’s | 72,97,98,105,149,159,197 | 7 | 3.8 |
| Ganglion | 44,115 | 2 | 0.6 |
| Ulna-sided | 8 | 1 | 0.3 |
| Wrist pain | 45,138 | 2 | 0.3 |
| Wrist OA | 75 | 1 | 0.3 |
| Neuropathy | 117 | 1 | 0.3 |
| Tenosynovitis (all) | 119 | ||
| Randomised controlled trial | 55,65,103,108,131,150,151,154,161,198,199 | 11 | 5.9 |
| Scoping review | 37 | 1 | 0.5 |
| Literature review | 77,79,114,123,164,192 | 7 | 3.8 |
| Delphi | 156 | 1 | 0.5 |
| Case control study | 99,109,110,142 | 4 | 2.2 |
| Best practice g’line | 73,92,115 | 3 | 1.6 |
| Non-randomised experimental study | 67,140,144,152,153,157,178,204 | 8 | 4.3 |
| Uncontrolled nonrandomized trial or cohort with one or more groups | 5–7,9,10,38,40,43,49,57,58,66,76,89,101,104,107,111,127,128,132–134,137,146,167,171,172,174,181,182,195, 46,48,51,70,71,74,85,95,113,121,124,125,163,173,176,177,180,183,187–191,201,202 | 71 | 38.4 |
| Prospective cohort study | 50,93,96,129,143,147,158,162,168,185,208 | 11 | 5.9 |
| Retrospective cross sectional study | 5–7,9,10,38,40,43,49,57,58,66,76,89,101,104,107,111,127,128,132–134,137,146,167,171,172,174,181,182,195 | 33 | 17.8 |
| Case series | 46,48,51,70,71,74,85,95,113,121,124,125,163,173,176,177,180,183,187–191,201,202 | 24 | 13.0 |
| Case report | 36,47,53,56,60–64,78,91,94,118,120,122,130,139,145,148,160,165,179,184,193,194,200,206 | 27 | 14.6 |
| Opinion pieces | 35,42,54,59,69,106,141,209 | 8 | 4.3 |
| Clinician guides | 39,41,52,68,80,81,83,84,86–88,116,129,169,175,196,210 | 17 | 9.2 |
| Qualitative research | 100,102,135 | 3 | 1.6 |
| Demographics of study sample subjects. | |||
| Sex | |||
| Mixed/not sex selected | 36,41–44,46,47,49,53,56,58–61,66,70,72,74,77–79,82,85–87,91,93,94,97,108,115,119–122,124,124,129,142–146,148–156,156–166,168,182,183,185,187,190–193,196,197,199,204 | 77 | 41.6 |
| Female only | 36,78,99,102,142,145,153,160,165,178,198 | 11 | 5.9 |
| Male only | 47,62,91,122,194 | 5 | 2.7 |
| Sex unclear or not reported | 5–7,9,10,34,38,40,45,50–52,54,55,63,65,67,68,71,73,76,80,81,83,84,88–90,96,98,99,101–103,106,109–111,113,114,116–118,125–137,139–141,167–175,186–188,194,195,200–206,208–211 | 84 | 45.4 |
| Age | |||
| Mixed age groups | 37,38,46,48,50,57,72,75,85,86,93,95,97,97,103,109–111,113,119,124,125,127,129–131,136,137,143,144,149,153,156,157,163,171,181,188–190,202 | 40 | 21.6 |
| 18–34 | 63,76,99,102,126,134,139,142,160,165,176,177,183,194,198 | 15 | 8.1 |
| 35–54 | 7,40,47,49,51,61,62,67,71,90,122,128,133,145,150–155,158,159,161,162,187,191,195,199,201 | 29 | 15.7 |
| 55–70 | 36,65 | 2 | 1.1 |
| 70+ | 34 | 1 | 0.5 |
Studies that addressed research questions in domain A: diagnosis
Methods of diagnosis (Supplementary Section 3) were commonly stated (Q1) with subjective questioning, (36, 19.5%), self-reported pain (35, 18.9%) and heat maps (1, 0.5%) representing patient-described symptoms. The use of special tests (51, 27.9%), palpation (33, 17.8%), range of motion assessment (28, 15.1%), manual accessory motion (20, 10.8), grip (7, 3.8), weighing scale and push-off tests (2, 1.1%), and laterality assessment (1, 0.5%) represent clinician-dependent examination methods stated. The range of individual special tests referred to in the literature numbered 25. Finklestein’s was the most commonly mentioned special test, however divergence in how this was described and confusion between this and Modified Eichoff was noted.157,158 Six studies (3.2%) described algorithms for the staging of the methods of assessment. MRI/MRA scans (35, 18.9%), X-ray (30, 16.2%), ultrasound scan (24, 13.0) nerve conduction studies (5, 2.7%), CT scans (3, 1.6%), and arthroscopy (11, 5.9%) were the most common advanced diagnostic methods found.
The performance of various diagnostic methods (Q2) were assessed in 37 papers (20%), with six studies detailing how specificity of diagnosis informed management (3.2%, Q3), of which three were best-practice guidelines, with the remaining referring to the benefits of early diagnosis, 139 staged management of de Quervain’s 159 and ulnar-sided wrist pain. 169 The impact that individual patient related factors had on diagnosis was found in 17 studies (9.2%), specifically age, clinic setting and sociodemographic factors (4, 2.2%), and three for sex (1.6%) (Q4).
Studies that addressed research questions in domain B: pathways of care
Two care pathways from the British Medical Journal were found for ganglion and tenosynovitis of the wrist (Q5) and composed through literature reviews from area experts (Q6). Other care pathways involved a chronic wrist pain algorithm, management of ganglion and a consensus document on the treatment guidelines for De Quervain’s. The interaction between private and public health provision was not explored (Q7). All pathways identified are displayed in Supplementary Section 4.
Studies that addressed research questions in domain C: Conservative management
Seventeen different conservative/non-operative management adjuncts to manage NTWD were referenced (Q8) in (Supplementary Section 5). The most common being injection (25, 13.5%), splinting (23, 12.4%), local exercise and manual therapy (18, 9.7%), activity modification (20, 10.8%), global exercise (9 studies, 4.9%), manual therapy sensorimotor and proprioceptive training (8 studies, (4.3%).
Cost implications of investigations were raised in five studies (2.7%), one finding routine X-ray was not cost-effective, three cautioning against the costs of investigations when they rarely change management but without scaling of costs, and one suggesting ultrasound sonography represents best value in emergency departments (Q9). Cost assessment was found for the use of injection and splints as first-line treatment for de Quervain’s, but no assessment of time efficiency nor the impact of patient choice in conservative/non operative options (Q9) was found. The effect of the clinical setting was discussed in one article which found that Primary Care was as effective in the delivery of injection as secondary care (Q10). For Q13 there were three studies which looked at the expected natural history of NTWD, one related to de Quervain’s, one regarding primary care presentations and one on the expected recovery following surgical management of ulna-sided pain.
Studies that addressed research questions in domain D: Outcomes
The recommendation for the use of, or investigation of the validity of outcome measures of interventions (Q14) was common, with 20 different Patient Reported Outcome Measures (PROMs) found (Supplementary Section 6). The Disabilities of the Arm, Shoulder and Hand (DASH) or QuickDASH 212 (16, 8.6%) and Patient-related Wrist and Hand Evaluation 138 (8, 4.3%) were most frequently referenced. Other methods of assessing outcomes were self-reported pain (26, 15.1%), changes in range of motion (28, 15.1%), visual analogue scale (VAS) (16, 8.6%), patient reported numerical score (6, 3.2%), grip strength (7, 3.8%) and changes on investigation findings were used in four instances (2.2%). Six studies (3.2%) were found which addressed Q15 in creating a hierarchy superiority of management approaches. Two related to de Quervain’s and the case for injection of steroid as an effective alternative to surgery, and two related to ganglion where injecting cortisone was not indicated over conservative/non-operative management. No studies were identified which specifically looked at the how outcome measures inform management (Q16).
Mapping onto the analytic framework
Using recommended scoping review methods, the extracted data were mapped onto the research domains and key questions from the pre-specified AF (Table 3). The extent to which the questions had been addressed was appraised to make recommendations for future research opportunities.
Table 3.
Knowledge gaps of evidence matched to the AF with suggested research opportunities.
| Domain and research question | Gaps in evidence | Clinical/research opportunities | |
|---|---|---|---|
| A | Diagnosis | ||
| Q1 | What elements comprise the diagnosis of non-traumatic wrist disorders and how are they staged? | Investigate how clinicians choose and stage the elements of assessment. | The components of diagnosis are frequently described with clear commonality. The justification for the selection and staging of elements is under-investigated. |
| Attempt consensus on systematic assessment process and its staging. | |||
| Q2 | What is the performance of diagnostic methods for specific structural diagnosis? | Investigation of measurement properties of tests used to diagnose non-traumatic wrist disorders. | Limited and sometimes contradictory evidence found for some elements for the use of diagnostic methods. |
| Q3 | Does specific diagnosis alter management? | Investigation of reasoning for management and staging based on diagnostic category. | Although often claimed in opinion pieces and narrative reviews, no systematic investigation for this assertion found. |
| Q4 | Do diagnoses differ based on patient demographics, duration of symptoms clinical setting or the clinician’s role and experience? | Further examination of demographic impact on management strategies. | Minimal sources for some subgroups, but insufficient evidence to authoritatively comment. |
| B | Pathways of care | ||
| Q5 | What are the care pathways for non-traumatic wrist disorders, do they differ between settings and how are they compiled? | Collection and evaluation of national and international care pathways | Two non-traumatic wrist disorders subgroups have guidelines to inform care pathways. No care pathways for other subgroups or non-traumatic wrist disorders as a group, or between care settings identified. |
| Q6 | What are the diagnostic criteria required for entry into care pathways and what features of wrist presentations inform escalation or removal from the pathway? | Collection and evaluation of national and care pathways | Present in three guidelines for two subgroups. Insufficient evidence to comment for other subgroups or non-traumatic wrist disorders as a group. |
| Q7 | How does private provision of care fit within care pathways, and why do private clinicians offer different things? | Investigation of care commissioner’s and clinician’s experiences in private and public settings. | Insufficient evidence to comment. |
| C | Conservative management | ||
| Q8 | What conservative management is delivered for non-traumatic wrist disorders? | Investigate how clinicians choose and stage the elements of treatment. | Methods of treatment are frequently described. The justification for the selection and staging of elements is under-investigated. |
| Attempt consensus on systematic assessment process and its staging. | |||
| Q9 | Which interventions are most cost-effective and time efficient and does patient choice influence interventions selection? | Scaling of cost for interventions based on outcomes. | Insufficient evidence to comment. |
| Q10 | Does any clinical setting show superiority? | Examination of clinical setting on outcome. | Insufficient evidence to comment. |
| Q11 | Do pathways align with best use of interventions, and how do you know when an intervention has been effective and how does this feed into ongoing care? | Explore the reasoning behind decision-making and care pathways for non-traumatic wrist disorders. | Insufficient evidence to comment. |
| Q12 | Where are the best patient resources held, and are the messages consistent with best practise? | Evaluation of web-based resources. | Insufficient evidence to comment. |
| Q13 | How long does it take to get better from non-traumatic wrist disorders? | Warrants further investigation. | Some evidence for some subgroup, but insufficient evidence to comment for other subgroups or non-traumatic wrist disorders as a group. |
| D | Outcome measures | ||
| Q14 | Which measures are used and what are their reliability, validity, and responsiveness for non-traumatic wrist disorders? | Attempt consensus of clinicians on which outcome measures are recommended and the method of their utility. | No suggestion of gaps in use of objective markers. Partial evidence to comment on their validity and use. |
| Q15 | Is there a difference between outcomes of surgery, conservative care, and sham, and does more care equate with better outcome? | Large scale multi-disciplinary collaborations. | Insufficient evidence to comment. |
| Q16 | How do outcome measures inform management, diagnosis or assess effectiveness of interventions? | Further evaluation of the use of outcome measures. | Insufficient evidence to comment. |
Discussion
The general study characteristics revealed a substantial proportion of the included sources comprised of evidence such as clinician guides, opinion pieces and case reports (52 studies, 28.1%). There is a risk that the volume of poor-quality evidence may ‘wash out’ the evidence derived from more rigorously designed and conducted studies and suggests peer learning is prominent in this field. The predominance of secondary care settings may indicate higher concentrations of research-active clinicians in secondary care rather than revealing the extent of NTWD presenting in this setting. It is likely higher rates of presentation of NTWD occur in primary and community settings at earlier stages of the care pathway that do not progress to secondary care which may be relatively under-researched. It is notable that uncontrolled nonrandomized cohort trials (71, 38.4%) were more prevalent than RCTs or experimental studies (19, 10.3%). This is driven partly by the large number of evaluations investigating the performance of advanced diagnostic machines when compared to either consultant clinical diagnosis or arthroscopic findings. The appetite for investigating new forms of scanning equipment or to validate new clinical tests for biomechanical diagnosis is consistent, however it is interesting that some authors have questioned the reductionist premise that biomechanical lesions are the modifiable factors to target in assisting patients with NTWD.7,9,10,28,157,162,172,202 The other reviews (systematic, literature and scoping) represent well-conducted enquiries into the methods of conservative/non-operative management of wrist disorders and provide good information on the risk factors and epidemiology of wrist pain.
There was sufficient evidence to identify the range of assessment techniques, treatment techniques and outcome measures (Q1, Q8 & Q14), however all domains have evidence gaps related to the AF questions allowing ample opportunity for further investigation. The absence of care pathways returned from searches for subgroups and NTWD as a whole reveals a pressing requirement to understand what care is currently being delivered and how a person with NTWD navigates toward optimal management.
That a plethora of diagnosis methods, conservative/non-operative management types and means of assessing outcomes have been identified, indicates a lack of consensus in best practice for navigating the journey of care for people with NTWD. Future work should prioritise the calculation of the burden of cost and care, which NTWD represents, to give staging of research priorities.
Potential opportunities for further studies
There is a need for further enquiry amongst clinicians and patients to identify what meaningful assessment looks like and how outcomes are best contextualised. To this end, the development of best practice guides for assessment, conservative/non-operative management options and outcome measures for NTWD would be beneficial, with recommendations on their staging. Further investigation of patient information would be useful. The means of achieving this is likely to require a mix of methodologies.
Strengths and limitations of the review
The strengths of this review include its pre-registration on the Open Science Framework. The use of an interprofessional study team, rigorous search strategy, broad sources of literature, and engagement with a mixed stakeholder group of patients and healthcare professionals to create key questions, which were refined and expanded to form an AF based on the clinical journey of patients with NTWD in the UK, add to this strength. Limitations are in part related to the nature of scoping reviews as the broad search strategy and research question resulted in the inclusion of a large number of studies of great heterogeneity. At full-text-level review, 289 sources were excluded due to ‘wrong site of injury’ or ‘global disorders’ reflecting wrist and hand being used interchangeably. The restriction of studies selected to those of the English language was a further limitation.
Conclusion
Significant uncertainty exists across all domains of the NTWD patient journey. There is a need for knowledge synthesis to guide musculoskeletal practitioners to administer effective, evidence-based interventions at all points along the clinical care pathway. This scoping review’s findings will help guide further research and assist us in the long-term goal of generating knowledge synthesis.
Supplemental Material
Supplemental Material for A scoping review to map evidence regarding key domains and questions in the management of non-traumatic wrist disorders by Thomas Mitchell, Nick Hamilton, Ben Dean, Sarah Rodgers, Sally Fowler-Davis and Sionnadh McLean in Hand Therapy
Acknowledgements
We would like to thank Professor George Peat for his assistance as a contributor in this research.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was made possible through the funded Graduate Teaching Associate scheme which was awarded to TM from Sheffield Hallam University as part of his PhD programme.
Guarantor: SM.
Contributorship: TM, BD and SM conceived the study and developed the search strategy. TM, BD and SR reviewed the literature and TM wrote the initial manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Thomas Mitchell https://orcid.org/0009-0009-2876-628X
Nick Hamilton https://orcid.org/0000-0002-4807-3087
References
- 1.Jordan KP, Kadam UT, Hayward R, et al. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010; 11(1): 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferguson R, Riley ND, Wijendra A, et al. Wrist pain: a systematic review of prevalence and risk factors- what is the role of occupation and activity? BMC Musculoskelet Disord 2019; 20(1): 542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussenbux A, Morrissey D, Joseph C, et al. Intermediate Care pathways for musculoskeletal conditions – are they working? A systematic review. Physiotherapy 2015; 101(1): 13–24. [DOI] [PubMed] [Google Scholar]
- 4.Price AJ, Ogollah R, Kang S, et al. Determining responsiveness and meaningful changes for the Musculoskeletal Health Questionnaire (MSK-HQ) for use across musculoskeletal care pathways. BMJ Open 2019; 9(10): e025357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ratasvuori MS, Lindfors NC, Sormaala MJ. The clinical significance of magnetic resonance imaging of the hand: an analysis of 318 hand and wrist images referred by hand surgeons. J Plast Surg Hand Surg 2022; 56(2): 69–73. [DOI] [PubMed] [Google Scholar]
- 6.Luijkx T, Buckens CF, van Seeters T, et al. ECU tendon subluxation: a nonspecific MRI finding occurring in all wrist positions irrespective of ulnar-sided symptoms? Eur J Radiol 2019; 116: 192. [DOI] [PubMed] [Google Scholar]
- 7.Stoop N, van der Gronde BATD, Janssen SJ, et al. Incidental flexor carpi radialis tendinopathy on magnetic resonance imaging. Hand (N Y) 2019; 14(5): 632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan JJ, Teunis T, Ring D. Prevalence of triangular fibrocartilage complex abnormalities regardless of symptoms rise with age: systematic review and pooled analysis. Clin Orthop Relat Res 2014; 472(12): 3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ou Yang O, McCombe DB, Keating C, et al. Ulnar-sided wrist pain: a prospective analysis of diagnostic clinical tests. ANZ J Surg 2021; 91(10): 2159. [DOI] [PubMed] [Google Scholar]
- 10.Prosser R, Harvey L, Lastayo P, et al. Provocative wrist tests and MRI are of limited diagnostic value for suspected wrist ligament injuries: a cross-sectional study. J Physiother 2011; 57(4): 247. [DOI] [PubMed] [Google Scholar]
- 11.Morway GR, Miller A. Clinical and radiographic evaluation of ulnar-sided wrist pain. Curr Rev Musculoskelet Med 2022; 15(6): 590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kloppenburg M, van Beest S, Kroon FPB. Thumb base osteoarthritis: a hand osteoarthritis subset requiring a distinct approach. Osteoarthr Res Motion 2017; 31(5): 649. [DOI] [PubMed] [Google Scholar]
- 13.Normand M, Tang TS, Brismée JM, et al. Clinical evaluation of thumb base osteoarthritis: a scoping review. Hand Ther 2021; 26(2): 63–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heidari B. Rheumatoid Arthritis: early diagnosis and treatment outcomes. Casp J Intern Med 2011; 2(1): 161. [PMC free article] [PubMed] [Google Scholar]
- 15.Dabbagh A, MacDermid JC, Yong J, et al. Diagnosing carpal tunnel syndrome: diagnostic test accuracy of scales, questionnaires, and hand symptom diagrams—a systematic review. J Orthop Sports Phys Ther 2020; 50(11): 622. [DOI] [PubMed] [Google Scholar]
- 16.Kamal RN, Behal R. Clinical care redesign to improve value in carpal tunnel syndrome: a before-and-after implementation study. J Hand Surg 2019; 44(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 17.Osiak K, Elnazir P, Walocha J, et al. Carpal tunnel syndrome: state-of-the-art review. Folia Morphol 2021; 81: 851–862. DOI: 10.5603/FM.a2021.0121 [DOI] [PubMed] [Google Scholar]
- 18.Goebel A, Birklein F, Brunner F, et al. The Valencia consensus-based adaptation of the IASP complex regional pain syndrome diagnostic criteria. Pain 2021; 162(9): 2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karantana A, Davis T, Kennedy D, et al. Common hand and wrist conditions: creation of UK research priorities defined by a James Lind Alliance Priority Setting Partnership. BMJ Open 2021; 11(3): e044207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James Lind Alliance . Common conditions affecting the hand and wrist priority setting partnership . 2017 . Available from https://www.jla.nihr.ac.uk/priority-setting-partnerships/common-conditons-affecting-the-hand-and-wrist/downloads/JLA-Final-Summary.pdf (date last accessed 28 Jul 2023).
- 21.Welshman J, Terry R, Burchmore H. A Brief Guide to Patient and Public Involvement and Qualitative Methods within Health and Social Care Research [Internet]. National Insitute of Health Research; [cited 2023 Jul 23]. Available from: https://www.rds-se.nihr.ac.uk/wp-content/uploads/RDS_Guide_to_PPI.pdf [Google Scholar]
- 22.Alderwick H, Dixon J, NHS England . The NHS Long Term Plan. BMJ, 2019, 364, pp. 1–136. https://www.bmj.com/content/364/bmj.l84, In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bennett JE, Stevens GA, Mathers CD. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet; 392(10152): 1072–1088. North American ed. [DOI] [PubMed] [Google Scholar]
- 24.Lewis JS, Stokes EK, Gojanovic B, et al. Reframing how we care for people with persistent non-traumatic musculoskeletal pain. Suggestions for the rehabilitation community. Physiotherapy 2021; 112: 143. [DOI] [PubMed] [Google Scholar]
- 25.Bunzli S, Smith A, Schütze R, et al. Making sense of low back pain and pain-related fear. J Orthop Sports Phys Ther 2017; 47(9): 628. [DOI] [PubMed] [Google Scholar]
- 26.Beard DJ, Rees JL, Cook JA, et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. The Lancet 2018; 391(10118): 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 2002; 347(2): 81. [DOI] [PubMed] [Google Scholar]
- 28.The MOWP study group . The presentation, diagnosis and management of non-traumatic wrist pain: an evaluation of current practice in secondary care in the UK NHS. Rheumatol Adv Pract 2020; 4(2): rkaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Munn Z, Aromataris E, Tufanaru C, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute system for the unified management, assessment and review of information (JBI SUMARI). JBI Evid Implement [Internet]. 2019;17(1): 36–43. Available from: https://journals.lww.com/ijebh/Fulltext/2019/03000/The_development_of_software_to_support_multiple.5.aspx [DOI] [PubMed] [Google Scholar]
- 30.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169(7): 467. [DOI] [PubMed] [Google Scholar]
- 31.Lisy K, Porritt K. Narrative synthesis: considerations and challenges. JBI Evid Implement. 2016; 14(4): 201. Available from: https://journals.lww.com/ijebh/Fulltext/2016/12000/Narrative_Synthesis__Considerations_and_challenges.33.aspx [Google Scholar]
- 32.Caulfield J. How to Do Thematic Analysis | Step-by-step Guide & Examples. Scribbr, 2023. [cited 2023 Jul 23]. Available from: https://www.scribbr.com/methodology/thematic-analysis/
- 33.Systematic Reviews for Health : Building Search Strategies [Internet]. Univeristy of Tasmania, 2022. [cited 2023 Jul 23]. Available from: https://utas.libguides.com/SystematicReviews/SearchStrategies
- 34.Baptista M, Kugel J, Javaherian H, et al. Functional outcomes of a community occupation-based hand therapy class for older adults. Phys Occup Ther Geriatr 2018; 36(4): 380. [Google Scholar]
- 35.Andersson JK. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev 2017; 2(9): 382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Backstrom KM. Mobilization with movement as an adjunct intervention in a patient with complicated de Quervain’s tenosynovitis: a case report. J Orthop Sports Phys Ther 2002; 32(3): 86–94. [DOI] [PubMed] [Google Scholar]
- 37.Bergner JL, Farrar JQ, Coronado RA. Dart thrower’s motion and the injured scapholunate interosseous ligament: a scoping review of studies examining motion, orthoses, and rehabilitation. J Hand Ther 2020; 33(1): 45–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Billig JI, Sterbenz JM, Zhong L, et al. Gender disparities in preoperative resource use for wrist arthroscopy. Plast Reconstr Surg 2018; 142(5): 1267–1274. Available from: https://journals.lww.com/plasreconsurg/Fulltext/2018/11000/Gender_Disparities_in_Preoperative_Resource_Use.29.aspx [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Daun M, Rudd A, Cheng K, et al. Magnetic resonance imaging of the triangular fibrocartilage complex. Top Magn Reson Imaging TMRI 2020; 29(5): 237. [DOI] [PubMed] [Google Scholar]
- 40.Dreckmann SC, von Schroeder HP, Novak CB, et al. Utility of specialized imaging for diagnosis of chronic wrist pain. Journal of Wrist Surgery 2019; 8(6): 497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Forman TA, Forman SK, Rose NE. A clinical approach to diagnosing wrist pain. Am Fam Physician 2005; 72(9): 1753. [PubMed] [Google Scholar]
- 42.Goel R, Abzug JM. De quervain’s tenosynovitis: a review of the rehabilitative options. Hand (N Y) 2015; 10(1): 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hassan K, Sohn A, Shi L, et al. De quervain tenosynovitis: an evaluation of the epidemiology and utility of multiple injections using a national database. J Hand Surg 2022; 47(3): 284.e1. [DOI] [PubMed] [Google Scholar]
- 44.Head L, Gencarelli JR, Allen M, et al. Wrist ganglion treatment: systematic review and meta-analysis. J Hand Surg 2015; 40(3): 546. [DOI] [PubMed] [Google Scholar]
- 45.Heiser R, O’Brien VH, Schwartz DA. The use of joint mobilization to improve clinical outcomes in hand therapy: a systematic review of the literature. J Hand Ther 2013; 26(4): 297–311. [DOI] [PubMed] [Google Scholar]
- 46.Henry TW, Tulipan JE, Beredjiklian PK, et al. Are Plain X-rays necessary in the diagnosis of de quervain’s tenosynovitis? J Wrist Surg 2021; 10(1): 48–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Howell ER. Conservative care of De Quervain’s tenosynovitis/tendinopathy in a warehouse worker and recreational cyclist: a case report. J Can Chiropr Assoc 2012; 56(2): 121. [PMC free article] [PubMed] [Google Scholar]
- 48.LaStayo P, Weiss S. The GRIT: a quantitative measure of ulnar impaction syndrome. J Hand Ther 2001; 14(3): 173. [DOI] [PubMed] [Google Scholar]
- 49.Lee RP, Hatem SF, Recht MP. Extended MRI findings of intersection syndrome. Skeletal Radiol 2009; 38(2): 157. [DOI] [PubMed] [Google Scholar]
- 50.Lee C, Langford PN, Sullivan GE, et al. The radial synergy test: an aid to diagnose de Quervain’s tenosynovitis. HAND (N Y) 2021; 18: 15589447211057297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maccio JR, Carlton L, Fink S, et al. Directional preference of the wrist: a preliminary investigation. J Man Manip Ther Taylor Francis Ltd 2017; 25(5): 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matthews GS, Kiani B, Wuertzer SD, et al. MRI of the wrist: algorithmic approach for evaluating wrist pain. Radiographics 2019; 39(2): 447. [DOI] [PubMed] [Google Scholar]
- 53.Mattox R, Battaglia PJ, Scali F, et al. Distal intersection syndrome progressing to extensor pollicis longus tendon rupture: a case report with sonographic findings. J Ultrasound 2017; 20(3): 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Merkle SL, Sluka KA, Frey-Law LA. The interaction between pain and movement. J Hand Ther 2020; 33(1): 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Michlovitz S, Hun L, Erasala GN, et al. Continuous low-level heat wrap therapy is effective for treating wrist pain. Arch Phys Med Rehabil 2004; 85(9): 1409–1416. [DOI] [PubMed] [Google Scholar]
- 56.Nico B, Waclawik AJ. Ganglion cysts as a cause of ulnar neuropathy at the wrist. WMJ 2021; 120(4): 325. [PubMed] [Google Scholar]
- 57.Peach C, Wain R, Woodruff M. The kirk watson test predicts increasing instability at the scapholunate joint when compared with an arthroscopic classification. Orthop Proc 2012; 94-B(SUPP_XXXVII): 383. [Google Scholar]
- 58.Ruland RT, Hogan CJ. The ECU synergy test: an aid to diagnose ECU tendonitis. J Hand Surg 2008; 33(10): 1777. [DOI] [PubMed] [Google Scholar]
- 59.Satteson E, Tannan SC. De Quervain Tenosynovitis [Internet]. Treasure Island (FL): StatPearls Publishing, 2021. Available from: https://europepmc.org/abstract/MED/28723034 [PubMed] [Google Scholar]
- 60.Schmidt E, Kobayashi Y, Gottschalk AW. It’s not de quervain tenosynovitis – a diagnosis to consider in persistent wrist pain. Ochsner J 2021; 21(2): 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Servi JT. Wrist pain from overuse: detecting and relieving intersection syndrome. Phys Sportsmed 1997; 25(12): 41. [DOI] [PubMed] [Google Scholar]
- 62.Seymour CK, Griffin C, Holmes SM, et al. Structural differential - a 32-year-old man with persistent wrist pain. N Engl J Med 2018; 379(25): 2385. [DOI] [PubMed] [Google Scholar]
- 63.Skinner TM. Intersection syndrome: the subtle squeak of an overused wrist. J Am Board Fam Med 2017; 30(4): 547. [DOI] [PubMed] [Google Scholar]
- 64.Streitz M, Simon E. When rest, ice, compression, and elevation fail: a case of chronic wrist pain. J Emerg Med 2019; 56(5): 566. [DOI] [PubMed] [Google Scholar]
- 65.Toci GR, Green A, Mubin N, et al. Patient adherence with at-home hand and wrist exercises: a randomized controlled trial of video versus handout format. HAND (N Y) 2021; 18(4): 680–685. Ahead Print. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Verhiel SHWL, Blackburn J, Ritt MJPF, et al. MRI findings in patients undergoing triangular fibrocartilage complex repairs versus patients without ulnar-sided wrist pain. Hand (N Y) 2022; 17(3): 483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vincent JI, MacDermid JC, Michlovitz SL, et al. The push-off test: development of a simple, reliable test of upper extremity weight-bearing capability. J Hand Ther 2014; 27(3): 185. [DOI] [PubMed] [Google Scholar]
- 68.Watanabe A, Souza F, Vezeridis PS, et al. Ulnar-sided wrist pain. II. Clinical imaging and treatment. Skeletal Radiol 2010; 39(9): 837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wolff AL, Wolfe SW. Rehabilitation for scapholunate injury: application of scientific and clinical evidence to practice. Spec Issue Wrist 2016; 29(2): 146. [DOI] [PubMed] [Google Scholar]
- 70.Wollstein R, Kirk Watson H, Poultsides G, et al. Range of movement in the wrist as a diagnostic tool in radial-sided wrist pain. Scand J Plast Reconstr Surg Hand Surg 2006; 40(4): 230. [DOI] [PubMed] [Google Scholar]
- 71.Zlatkin MB, Chao PC, Osterman AL, et al. Chronic wrist pain: evaluation with high-resolution MR imaging. Radiology 1989; 173(3): 723. [DOI] [PubMed] [Google Scholar]
- 72.Ashraf MO, Devadoss VG. Systematic review and meta-analysis on steroid injection therapy for de Quervain’s tenosynovitis in adults. Eur J Orthop Surg Traumatol Orthop Traumatol 2014; 24(2): 149. [DOI] [PubMed] [Google Scholar]
- 73.Blazar P., BMJ Best Practice : Ganglion Cyst, 2021. [Cited 2023 Jul 23]. Available from: https://bestpractice.bmj.com/topics/en-gb/984/pdf/984/Ganglion/cyst.pdf
- 74.Brennan CM, Yong LY, Foley J, et al. The value of the distal radioulnar joint effusion in diagnosing triangular fibrocartilage complex tears on magnetic resonance imaging. Arch Bone Jt Surg 2021; 9(4): 423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dean B, Shwan H, Neal T, et al. Therapeutic Interventions for Osteoarthritis of the Wrist: A Systematic Review and Meta-Analysis. F1000Research, 2018, p. 7. Available from: https://www.proquest.com/scholarly-journals/therapeutic-interventions-osteoarthritis-wrist/docview/2174246898/se-2?accountid=13827 [DOI] [PMC free article] [PubMed]
- 76.Gatt I, Smith-Moore S, Steggles C, et al. The takei handheld dynamometer: an effective clinical outcome measure tool for hand and wrist function in boxing. HAND (N Y) 2017; 13(3): 319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Graham C. In adults with de Quervain tenosynovitis, are exercises more effective in reducing pain and improving function than usual care? 2016. [cited 2023 Jul 23] Available from: https://www.keele.ac.uk/media/k-web/k-research/iau/cats/ahpfullcats/ahr-38-de-quervain-tenosynovitis.pdf
- 78.Kaneko S, Takasaki H, May S. Application of mechanical diagnosis and therapy to a patient diagnosed with de Quervain’s disease: a case study. J Hand Ther 2009; 22(3): 278. [DOI] [PubMed] [Google Scholar]
- 79.Kluzek S, Dean B, Wartolowska KA. Patient-reported outcome measures (PROMs) as proof of treatment efficacy. BMJ Evid-Based Med 2022; 27(3): 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lauder J, Younis F, Khan SH. Imaging of ulnar-sided wrist pain. Br J Hosp Med Lond Engl 2019; 80(8): 461. [DOI] [PubMed] [Google Scholar]
- 81.Lindequist S, Marelli C. Modern imaging of the hand, wrist, and forearm. J Hand Ther 2007; 20(2): 119. [DOI] [PubMed] [Google Scholar]
- 82.Plonczak AM, Niruttan K, Jain A. Should we be imaging soft tissue masses of the hand and wrist? J Plast Reconstr Aesthet Surg 2019; 72(2): 335. [DOI] [PubMed] [Google Scholar]
- 83.Prasad G, Bhalli MJ. Assessing wrist pain: a simple guide. Br J Hosp Med 2020; 81(5): 1–7. [DOI] [PubMed] [Google Scholar]
- 84.Read J. Ulnar-sided wrist pain is not the only cause of TFCC injury: a clinical perspective on other diagnoses in the sport setting. Br J Sports Med 2013; 47(17): 1061. [DOI] [PubMed] [Google Scholar]
- 85.Redvers-Chubb K. De Quervain’s syndrome: it may not be an isolated pathology. Hand Ther 2016; 21(1): 25–32. [Google Scholar]
- 86.Saccomano SJ, Ferrara LR. Assessment and management of wrist pain. Nurse Pract 2017; 42(8): 15. [DOI] [PubMed] [Google Scholar]
- 87.Sevenoaks H, Khan SH, Younis F. Diagnosis of ulnar-sided wrist pain: a pragmatic approach for the non-specialist. Br J Hosp Med Lond Engl 2019; 80(8): 456. [DOI] [PubMed] [Google Scholar]
- 88.Seymour R, White PG. Magnetic resonance imaging of the painful wrist. Br J Radiol 1998; 71(852): 1323. [DOI] [PubMed] [Google Scholar]
- 89.Shirley RA, Dhawan RT, Rodrigues JN, et al. Bone SPECT-CT: an additional diagnostic tool for undiagnosed wrist pain. J Plast Reconstr Aesthetic Surg JPRAS 2016; 69(10): 1424. [DOI] [PubMed] [Google Scholar]
- 90.MOWP study group . The presentation, diagnosis and management of non-traumatic wrist pain: an evaluation of current practice in secondary care in the UK NHS. Rheumatol Adv Pract 2020; 4(2). rkaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tilden W, Lindsay D, Astrinakis E, et al. A 29-year-old male with a long history of atraumatic wrist pain. Skeletal Radiol 2021; 50(10): 2103. [DOI] [PubMed] [Google Scholar]
- 92.Wolf JM., BMJ Best Practice : Tenosynovitis of the Hand and Wrist. 2020. [cited 2023 Jul 23]. Available from: https://bestpractice.bmj.com/topics/en-gb/982/pdf/982/Tenosynovitis/of/the/hand/and/wrist.pdf
- 93.Wu F, Rajpura A, Sandher D. Finkelstein’s test is superior to eichhoff’s test in the investigation of de Quervain’s disease. J Hand Microsurg 2018; 10(2): 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shrier I, Morrison DR, Hawkes R. Looking further when symptoms are disproportionate to physical findings. Med Sci Sports Exerc 2019; 51(1): 1–3. [DOI] [PubMed] [Google Scholar]
- 95.Anderson H, Hoy G. Orthotic intervention incorporating the dart-thrower’s motion as part of conservative management guidelines for treatment of scapholunate injury. J Hand Ther 2016; 29(2): 199–204. [DOI] [PubMed] [Google Scholar]
- 96.Bialocerkowski A. Patient rated wrist evaluation. Aust J Physiother 2008; 54(3): 221. [DOI] [PubMed] [Google Scholar]
- 97.Cavaleri R, Schabrun SM, Te M, et al. Hand therapy versus corticosteroid injections in the treatment of de Quervain’s disease: a systematic review and meta-analysis. J Hand Ther 2016; 29(1): 3–11. [DOI] [PubMed] [Google Scholar]
- 98.McBain B, Rio E, Cook J, et al. Diagnostic accuracy of imaging modalities in the detection of clinically diagnosed de Quervain’s syndrome: a systematic review. Skeletal Radiol 2019; 48(11): 1715. [DOI] [PubMed] [Google Scholar]
- 99.Nitschke JE, McMeeken JM, Burry HC, et al. When is a change a genuine change? A clinically meaningful interpretation of grip strength measurements in healthy and disabled women. J Hand Ther 1999; 12(1): 25–30. [PubMed] [Google Scholar]
- 100.Prosser R, Herbert R, LaStayo PC. Current practice in the diagnosis and treatment of carpal instability--results of a survey of Australian hand therapists. J Hand Ther 2007; 20(3): 239. [DOI] [PubMed] [Google Scholar]
- 101.Reid M, Wood T, Montgomery AM, et al. MRI does not effectively diagnose ulnar-sided wrist pain in elite tennis players. J Sci Med Sport 2020; 23(6): 564. [DOI] [PubMed] [Google Scholar]
- 102.Ryley JP, Langstaff RJ, Barton NJ. The natural history of undiagnosed wrist pain in young women: a long-term fo11ow-up. J Hand Surg Br Eur 1992; 17(1): 51. [DOI] [PubMed] [Google Scholar]
- 103.Thiele J, Nimmo R, Rowell W, et al. A randomized single blind crossover trial comparing leather and commercial wrist splints for treating chronic wrist pain in adults. BMC Musculoskelet Disord 2009; 10: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cheriex KCAL, Sulkers GSI, Terra MP, et al. Scapholunate dissociation; diagnostics made easy. Eur J Radiol 2017; 92: 45–50. [DOI] [PubMed] [Google Scholar]
- 105.Huisstede BM, Gladdines S, Randsdorp MS, et al. Effectiveness of conservative, surgical, and postsurgical interventions for trigger finger, dupuytren disease, and de quervain disease: a systematic review. Arch Phys Med Rehabil 2018; 99(8): 1635. [DOI] [PubMed] [Google Scholar]
- 106.Lötters FJB, Schreuders TAR, Videler AJ. SMoC-Wrist: a sensorimotor control-based exercise program for patients with chronic wrist pain. J Hand Ther Off J Am Soc Hand Ther 2020; 33(4): 607. [DOI] [PubMed] [Google Scholar]
- 107.Mulders MAM, Sulkers GSI, Videler AJ, et al. Long-term functional results of a wrist exercise program for patients with palmar midcarpal instability. J Wrist Surg 2018; 7(3): 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Peters-Veluthamaningal C, van der Windt DAWM, Winters JC, et al. Corticosteroid injection for de Quervain’s tenosynovitis. Cochrane Database Syst Rev. 2009; 3: 1465–1858. doi: 10.1002/14651858.CD005616.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Smeulders MJC, Kreulen M, Bos KE. Fine motor assessment in chronic wrist pain: the role of adapted motor control. Clin Rehabil 2001; 15(2): 133. [DOI] [PubMed] [Google Scholar]
- 110.Smeulders MJC, Kreulen M, Hage JJ, et al. Motor control impairment of the contralateral wrist in patients with unilateral chronic wrist pain. Am J Phys Med Rehabil 2002; 81(3): 177. [DOI] [PubMed] [Google Scholar]
- 111.Spies-Dorgelo MN, van der Windt DAWM, van der Horst HE, et al. Hand and wrist problems in general practice–patient characteristics and factors related to symptom severity. Rheumatol Oxf Engl 2007; 46(11): 1723. [DOI] [PubMed] [Google Scholar]
- 112.Spies-Dorgelo MN, van der Windt DAWM, Prins APA, et al. Clinical course and prognosis of hand and wrist problems in primary care. Arthritis Rheum 2008; 59(9): 1349. [DOI] [PubMed] [Google Scholar]
- 113.Teunissen JS, van der Oest MJW, van Groeninghen DE, et al. The impact of psychosocial variables on initial presentation and surgical outcome for ulnar-sided wrist pathology: a cohort study with 1-year follow-up. BMC Musculoskelet Disord 2022; 23(1): 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.van Vugt RM, Bijlsma JW, van Vugt AC. Chronic wrist pain: diagnosis and management. Development and use of a new algorithm. Ann Rheum Dis 1999; 58(11): 665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Vroon P, Scholten RJ, van Weert H. Interventions for ganglion cysts in adults. Cochrane Database Syst Rev 2005; 2: 1465–1858. doi: 10.1002/14651858.CD005327 [DOI] [Google Scholar]
- 116.Becciolini A, Ariani A, Becciolini M. Pisotriquetral arthritis: ‘forgotten’ joint in ultrasound imaging of the wrist. Ann Rheum Dis 2022; 81(6): 1. [DOI] [PubMed] [Google Scholar]
- 117.Chiaramonte R, Pavone P, Musumeci G, et al. Preventive strategies, exercises and rehabilitation of hand neuropathy in cyclists: a systematic review [with consumer summary]. J Hand Ther 2021; 35: 164–173. Ahead Print. 2021. [DOI] [PubMed] [Google Scholar]
- 118.Draghi F, Gregoli B, Bortolotto C. Pisiform bursitis: a forgotten pathology. J Clin Ultrasound 2014; 42(9): 560. [DOI] [PubMed] [Google Scholar]
- 119.Ferrara PE, Codazza S, Cerulli S, et al. Physical modalities for the conservative treatment of wrist and hand’s tenosynovitis: a systematic review. Semin Arthritis Rheum 2020; 50(6): 1280. [DOI] [PubMed] [Google Scholar]
- 120.Ginanneschi F, Filippou G, Milani P, et al. Ulnar nerve compression neuropathy at Guyon’s canal caused by crutch walking: case report with ultrasonographic nerve imaging. Arch Phys Med Rehabil 2009; 90(3): 522. [DOI] [PubMed] [Google Scholar]
- 121.Montechiarello S, Miozzi F, D’Ambrosio I, et al. The intersection syndrome: ultrasound findings and their diagnostic value. J Ultrasound 2010; 13(2): 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ricci V, Özçakar L. Ultrasound imaging for dorsal radiolunotriquetral ligament possibly causing wrist impingement. Am J Phys Med Rehabil 2019; 98(2): e17. [DOI] [PubMed] [Google Scholar]
- 123.Rosskopf AB, Martinoli C, Sconfienza LM, et al. Sonography of tendon pathology in the hand and wrist. J Ultrason 2021; 21(87): e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Giovagnorio F, Miozzi F. Ultrasound findings in intersection syndrome. J Med Ultrason 2012; 39(4): 217. [DOI] [PubMed] [Google Scholar]
- 125.Huellner MW, Bürkert A, Schleich FS, et al. SPECT/CT versus MRI in patients with nonspecific pain of the hand and wrist - a pilot study. Eur J Nucl Med Mol Imaging 2012; 39(5): 750. [DOI] [PubMed] [Google Scholar]
- 126.Landman DM, Maree JH, Peterson C. The effect of the powerball gyroscope as a treatment device for nonspecific wrist pain. J Manipulative Physiol Ther 2020; 43(5): 483. [DOI] [PubMed] [Google Scholar]
- 127.Elkhader BA. Sonography of the wrist joint: pathologic conditions. MSARR 2022; 4: 5–10. [Google Scholar]
- 128.Hampole AB, Jeevika MU, Nirnay KK, et al. Ultrasonography and MRI evaluation in wrist joint pain. Asian J Med Radiol Res 2021; 9(1): 17. [Google Scholar]
- 129.Spies-Dorgelo MN, van der Windt DAWM, Prins APA, et al. Diagnosis and management of patients with hand and wrist problems in general practice. Eur J Gen Pract 2009; 15(2): 84–94. [DOI] [PubMed] [Google Scholar]
- 130.Worboys T, Brassington M, Ward EC, et al. Delivering occupational therapy hand assessment and treatment sessions via telehealth. J Telemed Telecare 2018; 24(3): 185. [DOI] [PubMed] [Google Scholar]
- 131.Kim GS, Weon JH, Kim MH, et al. Effect of weight-bearing wrist movement with carpal-stabilizing taping on pain and range of motion in subjects with dorsal wrist pain: a randomized controlled trial. J Hand Ther 2020; 33(1): 25–33. [DOI] [PubMed] [Google Scholar]
- 132.Mehta NH, Garg B, Ansari T, et al. Comparison of magnetic resonance arthrography and wrist arthroscopy in the evaluation of chronic wrist pain in Indian population. Indian J Orthop 2019; 53(6): 769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Moellhoff N, Throner V, Frank K, et al. Visualization of the location and level of pain in common wrist pathologies using color-coded heatmaps. Arch Orthop Trauma Surg 2022; 143:1095–1102. DOI: 10.1007/s00402-022-04479-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.El-Deek AMF, Dawood EMAEHH, Mohammed AAM. Role of ultrasound versus magnetic resonance imaging in evaluation of non-osseous disorders causing wrist pain. Egypt J Radiol Nucl Med 2019; 50(1): 8. [Google Scholar]
- 135.MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther Off J Am Soc Hand Ther 1996; 9(2): 178. [DOI] [PubMed] [Google Scholar]
- 136.Pelletier R, Higgins J, Bourbonnais D. Laterality recognition of images, motor performance, and aspects related to pain in participants with and without wrist/hand disorders: an observational cross-sectional study. Musculoskelet Sci Pract 2018; 35: 18–24. [DOI] [PubMed] [Google Scholar]
- 137.Pelletier R, Paquette É, Bourbonnais D, et al. Bilateral sensory and motor as well as cognitive differences between persons with and without musculoskeletal disorders of the wrist and hand. Musculoskelet Sci Pract 2019; 44: 102058. [DOI] [PubMed] [Google Scholar]
- 138.Shafiee E, MacDermid J, Farzad M, et al. A systematic review and meta-analysis of Patient-Rated Wrist (and Hand) Evaluation (PRWE/PRWHE) measurement properties, translation, and/or cross-cultural adaptation. Disabil Rehabil 2021: 1–15. [DOI] [PubMed] [Google Scholar]
- 139.Talić Tanović A, Tanović E, Mekić M, et al. Effects of early diagnosis of the wrist over-use syndrome on the treatment. Med Glas Off Publ Med Assoc Zenica-Doboj Cant Bosnia Herzeg 2018; 15(2): 168. [DOI] [PubMed] [Google Scholar]
- 140.Staes FF, Banks KJ, De Smet L, et al. Reliability of accessory motion testing at the carpal joints. Man Ther 2009; 14(3): 292. [DOI] [PubMed] [Google Scholar]
- 141.Hagert E. Proprioception of the wrist joint: a review of current concepts and possible implications on the rehabilitation of the wrist. J Hand Ther 2010; 23(1): 2–17. [DOI] [PubMed] [Google Scholar]
- 142.Avci S, Yilmaz C, Sayli U. Comparison of nonsurgical treatment measures for de Quervain’s disease of pregnancy and lactation. J Hand Surg - Am 2002; 27(2): 322–324. [DOI] [PubMed] [Google Scholar]
- 143.Mandiroglu S, Alemdaroglu E. Idiopathic carpal tunnel syndrome and de Quervain’s tenosynovitis: is there an association? Somatosens Mot Res 2021; 38(4): 353. [DOI] [PubMed] [Google Scholar]
- 144.Jongprasitkul H, Suputtitada A, Kitisomprayoonkul W, et al. Elastic bandage vs. neoprene thumb stabilizer splint in acute De Quervain’s tenosynovitis. Asian Biomed 2017; 5(2): 263. [Google Scholar]
- 145.Allam AES, Al-Ashkar DS, Negm AA, et al. Ultrasound-guided methotrexate injection for De Quervain disease of the wrist: what lies beyond the horizon? J Pain Res 2017; 10: 2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yeom JW, Koh KH, Park MJ, et al. Modified staged finkelstein test for the identification of intracompartmental septum in patients with de quervain’s disease. J Hand Surg Asian-Pac 2021; 26(4): 555. [DOI] [PubMed] [Google Scholar]
- 147.Sato J, Ishii Y, Noguchi H. Clinical and ultrasound features in patients with intersection syndrome or de Quervain’s disease. J Hand Surg Eur 2016; 41(2): 220. [DOI] [PubMed] [Google Scholar]
- 148.Tamura H, Shikino K, Uchida S, et al. de Quervain’s tenosynovitis. BMJ Case Rep 2020; 13(12): e240129. Available from: https://hallam.idm.oclc.org/login?url=https://www.proquest.com/scholarly-journals/de-quervain-s-tenosynovitis/docview/2468944015/se-2?accountid=13827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rowland P, Phelan N, Gardiner S, et al. The effectiveness of corticosteroid injection for de quervain’s stenosing tenosynovitis (DQST): a systematic review and meta-analysis. Open Orthop J 2015; 9: 437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hadianfard M, Ashraf A, Fakheri M, et al. Efficacy of acupuncture versus local methylprednisolone acetate injection in de Quervain’s tenosynovitis: a randomized controlled trial. J Acupunct Meridian Stud 2014; 73: 115–121. [DOI] [PubMed] [Google Scholar]
- 151.Homayouni K, Zeynali L, Mianehsaz E. Comparison between kinesio taping and physiotherapy in the treatment of de quervain’s disease. J Musculoskelet Res 2013; 16(04): 1350019. [Google Scholar]
- 152.Mardani-Kivi M, Karimi Mobarakeh M, Bahrami F, et al. Corticosteroid injection with or without thumb spica cast for de Quervain tenosynovitis. J Hand Surg - Am 2014; 39(1): 37–41. [DOI] [PubMed] [Google Scholar]
- 153.Nemati Z, Javanshir MA, Saeedi H, et al. The effect of new dynamic splint in pinch strength in De Quervain syndrome: a comparative study. Disabil Rehabil Assist Technol 2017; 12(5): 457. [DOI] [PubMed] [Google Scholar]
- 154.Sharma R, Thukral A, Kumar S, et al. Effect of low level lasers in de Quervains tenosynovitis prospective study with ultrasonographic assessment [with consumer summary]. Physiother 2002: 88(12): 730–734. [Google Scholar]
- 155.Sharma R, Aggarwal AN, Bhatt S, et al. Outcome of low level lasers versus ultrasonic therapy in de Quervain’s tenosynovitis. Indian J Orthop 2015; 49(5): 542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Huisstede BMA, Coert JH, Fridén J, et al. Consensus on a multidisciplinary treatment guideline for de Quervain disease: results from the European handguide study. Phys Ther 2014; 94(8): 1095. [DOI] [PubMed] [Google Scholar]
- 157.Cheimonidou A, Lamnisos D, Lisacek-Kiosoglous A, et al. Validity and reliability of the finkelstein test. Trends Med 2019; 19(2): 1–7. [Google Scholar]
- 158.Lahiri A, Mckenzie G. Simple and Patient-Friendly Clinical Diagnostic Tests for de Quervain’s Disease. SunKrist Journal of Orthopedics and Musculoskeletal Disorders. 2020; 2(1): 1–5. [Google Scholar]
- 159.Abi-Rafeh J, Kazan R, Safran T, et al. Conservative management of de Quervain stenosing tenosynovitis: review and presentation of treatment algorithm. Plast Reconstr Surg. 2020;146(1): 105–126. Available from: https://journals.lww.com/plasreconsurg/Fulltext/2020/07000/Conservative_Management_of_de_Quervain_Stenosing.20.aspx [DOI] [PubMed] [Google Scholar]
- 160.Papa JA. Conservative management of De Quervain’s stenosing tenosynovitis: a case report. J Can Chiropr Assoc 2012; 56(2): 112. [PMC free article] [PubMed] [Google Scholar]
- 161.Karlibel IA, Aksoy MK, Alkan A. Paraffin bath therapy in de Quervain’s tenosynovitis: a single-blind randomized controlled trial. Int J Biometeorol 2021; 65(8): 1391–1398. [DOI] [PubMed] [Google Scholar]
- 162.Erpala F, Ozturk T. ‘Snapping’ of the extensor carpi ulnaris tendon in asymptomatic population. BMC Musculoskelet Disord 2021; 22(1): 387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Sahin G, Dogan BE, Demirtaş M. Virtual MR arthroscopy of the wrist joint: a new intraarticular perspective. Skeletal Radiol 2004; 33(1): 9–14. [DOI] [PubMed] [Google Scholar]
- 164.Wu WT, Chang KV, Mezian K, et al. Ulnar wrist pain revisited: ultrasound diagnosis and guided injection for triangular fibrocartilage complex injuries. J Clin Med 2019; 8(10): 1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Chen Z. A novel staged wrist sensorimotor rehabilitation program for a patient with triangular fibrocartilage complex injury: a case report. J Hand Ther 2019; 32(4): 525. [DOI] [PubMed] [Google Scholar]
- 166.Chen Z. Clinical evaluation of a wrist sensorimotor rehabilitation program for triangular fibrocartilage complex injuries. Hand Ther 2021; 26(4): 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Banjar M, Nor FEM, Singh P, et al. Comparison of visibility of ulnar sided triangular fibrocartilage complex (TFCC) ligaments between isotropic three-dimensional and two-dimensional high-resolution FSE MR images. Eur J Radiol 2021; 134: 109418. [DOI] [PubMed] [Google Scholar]
- 168.Sato J, Ishii Y, Noguchi H. Diagnostic performance of the extensor carpi ulnaris (ECU) synergy test to detect sonographic ECU abnormalities in chronic dorsal ulnar-sided wrist pain. J Ultrasound Med Off J Am Inst Ultrasound Med 2016; 35(1): 7–14. [DOI] [PubMed] [Google Scholar]
- 169.Jain DKA, Wahegaonkar AL. Ulnar-side wrist pain management guidelines: all that hurts is not the TFCC. Indian J Orthop 2021; 55(2): 310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Huflage H, Luetkens KS, Kunz AS, et al. Improved diagnostic accuracy for ulnar-sided TFCC lesions with radial reformation of 3D sequences in wrist MR arthrography. Eur Radiol 2021; 31(12): 9399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Spies CK, Unglaub F, Bruckner T, et al. Diagnostic accuracy of wrist MRI in comparison to wrist arthroscopy regarding TFCC lesions in clinical practice. Arch Orthop Trauma Surg 2022; 142(5): 879. [DOI] [PubMed] [Google Scholar]
- 172.Kuntz MT, Janssen SJ, Ring D. Incidental signal changes in the extensor carpi ulnaris on MRI. Hand (N Y) 2015; 10(4): 750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kaiser P, Kellermann F, Arora R, et al. Diagnosing extensor carpi ulnaris tendon dislocation with dynamic rotation MRI of the wrist. Clin Imaging 2018; 51: 323. [DOI] [PubMed] [Google Scholar]
- 174.Öztürk T, Burtaç Eren M. Is it really safe to evaluate symptomatic extensor carpi ulnaris tendon instability by magnetic resonance imaging (MRI)? Acta Orthop Belg 2021; 87(2): 227. [PubMed] [Google Scholar]
- 175.Porteous R, Harish S, Parasu N. Imaging of ulnar-sided wrist pain. J Assoc Can Radiol 2012; 63(1): 18–29. [DOI] [PubMed] [Google Scholar]
- 176.Ozçelik A, Günal I, Köse N. Stress views in the radiography of scapholunate instability. Eur J Radiol 2005; 56(3): 358. [DOI] [PubMed] [Google Scholar]
- 177.Holmes MK, Taylor S, Miller C, et al. Early outcomes of ‘The Birmingham Wrist Instability Programme’: a pragmatic intervention for stage one scapholunate instability. Hand Ther 2017; 22(3): 90–100. [Google Scholar]
- 178.van Andel CJ, Roescher WBM, Tromp MF, et al. Quantification of wrist joint laxity. J Hand Surg 2008; 33(5): 667. [DOI] [PubMed] [Google Scholar]
- 179.Ye BJ, Kim JI, Lee HJ, et al. A case of avascular necrosis of the capitate bone in a pallet car driver. J Occup Health 2009; 51(5): 451. [DOI] [PubMed] [Google Scholar]
- 180.Scheck RJ, Kubitzek C, Hierner R, et al. The scapholunate interosseous ligament in MR arthrography of the wrist: correlation with non-enhanced MRI and wrist arthroscopy. Skeletal Radiol 1997; 26(5): 263. [DOI] [PubMed] [Google Scholar]
- 181.Hollevoet N. Bilateral scapholunate widening may have a nontraumatic aetiology and progress to carpal instability and osteoarthritis with advancing age. J Hand Surg Eur 2019; 44(6): 566. [DOI] [PubMed] [Google Scholar]
- 182.Draghi F, Bortolotto C. Intersection syndrome: ultrasound imaging. Skeletal Radiol 2014; 43(3): 283. [DOI] [PubMed] [Google Scholar]
- 183.Grégoire C, Guigal V. Efficacy of corticosteroid injections in the treatment of 85 ganglion cysts of the dorsal aspect of the wrist. Orthop Traumatol Surg Res 2022; 108: 103198. [DOI] [PubMed] [Google Scholar]
- 184.Higashihara M, Sonoo M, Imafuku I, et al. Origin of ulnar compound muscle action potential investigated in patients with ulnar neuropathy at the wrist. Muscle Nerve 2010; 41(5): 704. [DOI] [PubMed] [Google Scholar]
- 185.Kollmer J, Bäumer P, Milford D, et al. T2-signal of ulnar nerve branches at the wrist in guyon’s canal syndrome. PloS One 2012; 7(10): e47295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Swärd E, Nennesmo I, Wilcke M. Structural changes in the posterior interosseous nerve from patients with wrist osteoarthritis and asymptomatic controls. J Wrist Surg 2020; 9(6): 481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Higashigaito K, Pfirrmann CWA, Koch S, et al. Ligaments of the scapho-trapezial-trapezoidal joint: MR anatomy in asymptomatic and symptomatic individuals. Skeletal Radiol 2022; 51(3): 637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Krag C. Osteoarthritis of the piso-triquetral articulation. The Hand 1974; 6(2): 181. [DOI] [PubMed] [Google Scholar]
- 189.Ahuja A, Lawande M, Daftary AR. Role of radiographs and ultrasound in diagnosing calcific tendinitis and periarthritis in the wrist and hand with ultrasound-guided barbotage as management tool. Indian J Radiol Imaging 2021; 31(3): 605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Choung SD, Kwon OY, Park KN, et al. Short-term effects of self-mobilization with a strap on pain and range of motion of the wrist joint in patients with dorsal wrist pain when weight bearing through the hand: a case series. Man Ther 2013; 18(6): 568. [DOI] [PubMed] [Google Scholar]
- 191.Abe Y, Katsube K, Tsue K, et al. Arthoscopic diagnosis of partial scapholunate ligament tears as a cause of radial sided wrist pain in patients with inconclusive X-ray and mri findings. J Hand Surg 2006; 31(4): 419. [DOI] [PubMed] [Google Scholar]
- 192.Khaled W, Drapé JL. MRI of wrist and hand masses. Diagn Interv Imaging 2015; 96(12): 1238. [DOI] [PubMed] [Google Scholar]
- 193.Ağırman M, Tolu S, Başkan Ö, et al. Brachial artery thrombosis mimicking De Quervain’s syndrome:a case report. Turk J Phys Med Rehabil 2017; 63(3): 272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Iwatsuki K, Yoneda H, Kurimoto S, et al. Osteoid osteoma of the wrist misdiagnosed as de Quervain’s tenosynovitis due to normal X-ray at the first visit: a case report. Int J Surg Case Rep 2020; 75: 469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Prosser R, Hancock MJ, Nicholson LL, et al. Prognosis and prognostic factors for patients with persistent wrist pain who proceed to wrist arthroscopy. J Hand Ther 2012; 25(3): 264. [DOI] [PubMed] [Google Scholar]
- 196.Liao JC, Liao AK, Tan DM. Causes and assessment of subacute and chronic wrist pain. Singapore Med J 2013; 54(10): 592. quiz 598. DOI: 10.11622/smedj.2013205 PMID: 24154586. [DOI] [PubMed] [Google Scholar]
- 197.Drapeza RC, Navasca SB, Dones V, et al. The effects of taping in de Quervain’s disease: a systematic review and meta-analysis. J Bodyw Mov Ther 2022; 32: 218–227. [DOI] [PubMed] [Google Scholar]
- 198.Jung K-S, Jung J-H, Shin H-S, et al. The effects of taping combined with wrist stabilization exercise on pain, disability, and quality of life in postpartum women with wrist pain: a randomized controlled pilot study. Int J Environ Res Public Health 2021; 18(7): 3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Awan WA, Babur MN, Masood T. Effectiveness of therapeutic ultrasound with or without thumb spica splint in the management of De Quervain’s disease. J Back Musculoskelet Rehabil 2017; 30(4): 691. [DOI] [PubMed] [Google Scholar]
- 200.Chang KE-V, Hung C-Y, Özçakar L. Snapping thumb and superficial radial nerve entrapment in de quervain disease: ultrasound imaging/guidance revisited. Pain Med 2015; 16(11): 2214. [DOI] [PubMed] [Google Scholar]
- 201.Schleich FS, Schürch M, Huellner MW, et al. Diagnostic and therapeutic impact of SPECT/CT in patients with unspecific pain of the hand and wrist. EJNMMI Res 2012; 2(1): 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Albastaki U, Sophocleous D, Göthlin J, et al. Magnetic resonance imaging of the triangular fibrocartilage complex lesions: a comprehensive clinicoradiologic approach and review of the literature. J Manipulative Physiol Ther 2007; 30(7): 522. [DOI] [PubMed] [Google Scholar]
- 203.Lee SH, Yun SJ. Point-of-care wrist ultrasonography in trauma patients with ulnar-sided pain and instability. Am J Emerg Med 2018; 36(5): 859. [DOI] [PubMed] [Google Scholar]
- 204.LaStayo P, Howell J. Clinical provocative tests used in evaluating wrist pain: a descriptive study. J Hand Ther 1995; 8(1): 10. [DOI] [PubMed] [Google Scholar]
- 205.Fu J, Zhang H, Wei K, et al. Design and performance analysis of a dynamic magnetic resonance imaging-compatible device for triangular fibrocartilage complex injury diagnosis. J Healthc Eng 2022; 2022: 9688441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Taniguchi S, Satow A. Objective measurement of pain in the wrist: analyses of basic factors for normative data and a case study. Percept Mot Skills 1988; 67(1): 37. [DOI] [PubMed] [Google Scholar]
- 207.Castarlenas E, de la Vega R, Jensen MP, et al. Self-Report measures of hand pain intensity: current evidence and recommendations. Hand Clin 2016; 32(1): 11. [DOI] [PubMed] [Google Scholar]
- 208.Burgess RA, Pavlosky WF, Thompson RT. MRI-identified abnormalities and wrist range of motion in asymptomatic versus symptomatic computer users. BMC Musculoskelet Disord 2010; 11(1): 273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Dharmshaktu G. ‘Selfie test’: the proposal of a new clinical test for diagnosing De Quervain’s tenosynovitis at primary care level. J Fam Med Prim Care 2020; 9(4): 2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Daenen B, Houben G, Bauduin E, et al. Sonography in wrist tendon pathology. J Clin Ultrasound JCU 2004; 32(9): 462. [DOI] [PubMed] [Google Scholar]
- 211.Kus S, van de Ven-Stevens LA, Coenen M, et al. What is our knowledge of functioning and disability in hand conditions based on? Arch Phys Med Rehabil 2011; 92(8): 1326. [DOI] [PubMed] [Google Scholar]
- 212.Beaton DE, Wright JG, Katz J. Development of the QuickDASH: comparison of three iten-reduction approaches. J Bone Joint Surg Am 2005; 87A: 1038–1104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for A scoping review to map evidence regarding key domains and questions in the management of non-traumatic wrist disorders by Thomas Mitchell, Nick Hamilton, Ben Dean, Sarah Rodgers, Sally Fowler-Davis and Sionnadh McLean in Hand Therapy