Abstract
Background:
In theory, habitually exercising mindfulness skills can improve cognitive functioning abilities. However, no comprehensive quantitative reviews of the efficacy of mindfulness-based interventions (MBIs) on global and unique cognitive subdomains exist to date.
Method:
This meta-analysis examined the effects of MBIs on global cognition and 15 cognitive subdomains. Inclusion criteria: meditation naïve participants; participants randomly assigned to MBIs or no-treatment, waitlist, or active control; outcome measures included at least one behavioral cognitive assessment or subjective cognitive functioning measure; teaching mindfulness skills was the primary treatment focus. Exclusion criteria: inadequate data to calculate effect sizes; MBIs included only one session; control condition that contained any MBI form. Robust variance estimation and moderator analyses controlling for presence of reported treatment fidelity were conducted.
Results:
One-hundred-and-eleven randomized controlled trials (RCTs) (n = 9,538) met eligibility criteria. MBIs had small-to-moderate significant effects on global cognition, executive attention, WM accuracy, inhibition accuracy, shifting accuracy, sustained attention, and subjective cognitive functioning (vs. waitlist/no-treatment, average g = 0.257–0.643; vs. active controls, average g = 0.192–0.394). MBIs did not impact executive functioning (EF) latency indices, verbal fluency, processing speed, episodic memory, and cognitive error. Treatment effects were stronger for those with elevated psychiatric symptoms compared to healthy controls, and medical samples, studies with complete-case (vs. intention-to-treat) analysis, face-to-face (vs. self-guided) delivery, and use of non-standard mindfulness-based stress reduction or mindfulness-based cognitive therapy (vs. standard MBI).
Conclusion:
MBIs consistently yielded small-to-moderate yet practically meaningful effect sizes on global cognition and six cognitive subdomains that captured accuracy vs. latency-based indices of EF and sustained accuracy.
Keywords: mindfulness-based interventions, cognitive functioning, randomized controlled trials, meta-analysis, executive function
Mindfulness is described as the intentional practice of non-judgmentally focusing on experiences in the here and now in flexible, curious, and receptive ways (Bishop et al., 2004). Originating from Buddhist philosophies and meditative practices, abundant scientific evidence has shown that mindfulness-based interventions (MBIs) positively affect various health outcomes across diverse age groups, genders, and people living in different cultural contexts (Abbott et al., 2014; Black & Slavich, 2016; Flook et al., 2015; Kaunhoven & Dorjee, 2017; Wetherell et al., 2017). Advancing our understanding of potential mechanisms via which mindfulness confers benefits is thus essential.
Mindfulness can improve executive functioning (EF),1 which involves higher cognitive control functions. MBIs teach focused attention (FA) and open monitoring (OM) exercises to enhance EF abilities (Stein & Witkiewitz, 2020). FA training involves sustaining attention to a particular object or aspect of experience and continually re-focusing after distractions (Anālayo, 2019a). OM practices involve non-judgmental and non-elaborative awareness (Uusberg et al., 2016), cultivating non-reactivity to cognitive and emotional content (Anālayo, 2019b). These processes are plausible distinct mechanisms via which FA and OM may benefit EF domains.
Further, FA exercises might benefit working memory (WM; Corbetta & Shulman, 2002). Practicing FA and OM has been theorized to positively impact WM by continually updating information (Jha et al., 2019; Miyake et al., 2000; Vago et al., 2019). The positive influence of OM on emotion regulation abilities might also enhance WM capacity through meta-cognitive processes (Lutz et al., 2015; Raffone et al., 2019).
In addition, practicing FA could enhance the ability to shift between thinking modes and inhibit autopilot responses. Shifting involves fluently switching back and forth between different thinking modes (Berg, 1948; Chiu et al., 2018; Raffone & Srinivasan, 2017), whereas inhibition refers to the effortful refraining from autopilot responses (Jewsbury et al., 2016). These benefits of FA are especially evident when attention is directed away from unhelpful thoughts toward the present moment and task at hand (Wolkin, 2015).
On that note, mindfulness practices might enhance attentional control (Sorensen et al., 2018), a foundational precursor to EF (Vilgis et al., 2015). For instance, it has been proposed that MBIs can improve meta-cognition and attentional facets (Haigh et al., 2010), such as sustained attention accuracy (Esterman & Rothlein, 2019) and intra-individual coefficient of variation (Bellgrove et al., 2004; Cubillo et al., 2023). Sustained attention has also been defined as alerting (Prakash et al., 2020), and recurrently identifying distracting thoughts could buttress the salience attentional control subdomain linked to the identification of or goal-driven fixation on specific visual or physical cues (Awh et al., 2012; Seeley et al., 2007). Furthermore, mindfulness practices can improve orienting (or selective attention) ability by redirecting attention back to the task at hand (Ristic et al., 2007; Sood & Jones, 2013). Also, MBIs may enhance executive attention by managing conflicting thoughts, emotions, and responses (Petersen & Posner, 2012). Taken together, these theories propose that MBI skills may enhance attention domains through observation, discernment, psychological flexibility strategies, and increased awareness of influential factors (Cubillo et al., 2023; Garland et al., 2015).
MBIs could impact various cognitive functioning domains beyond EF and attentional constructs. For example, they might enhance verbal fluency by improving the ability to express internal experiences and external events using precise and expressive language (Baer et al., 2004). Relatedly, MBIs could reduce cognitive errors and distractions during task engagement by reducing repetitive negative thinking, such as worry and rumination (Gu et al., 2015; Lindsay & Creswell, 2017; Posner et al., 2015; Teper et al., 2013). Such processes could free up more cognitive resources to attend to and process incoming information, improving processing speed (Müller et al., 2021) and episodic memory (Allen & Fortin, 2013; Tulving, 2002). Additionally, increased acceptance, awareness, and quality of engagement through MBIs might enhance subjective cognitive functioning (Daglas-Georgiou et al., 2022; Hallion et al., 2019; Lindsay & Creswell, 2017) and objective cognitive functioning (Fisher et al., 2019; Teper & Inzlicht, 2013). Collectively, MBIs could refine specific cognitive subdomains and global cognition by freeing up limited resources and enabling effective and efficient use of them.
To date, only six meta-analyses focused solely on RCTs of MBIs on cognitive functioning. For example, across 13 RCTs (n = 1,112), MBIs had substantial, moderate effects on WM and inhibition but a negligible impact on shifting among adults (Cásedas et al., 2020). In children and adolescents, across 17 studies (n = 1,762), MBIs led to small but meaningful effects on attentional control and global EF (e.g., planning, WM; Dunning et al., 2019). Also, seven RCTs (n = 170) found positive impacts of MBIs (vs. control) on attention and episodic memory among persons with multiple sclerosis (Han, 2021). Relatedly, across 27 RCTs (n = 1,632), MBIs had small yet significant effects on attention and global EF, but not WM, among healthy adults ages 18–65 (Yakobi et al., 2021). However, these reviews did not consistently examine the effects of MBIs on EF facets and executive attention. Also, data synthesized across nine studies (n = 724) showed that MBIs did not notably impact attention, EF, memory, and global cognition in adults aged 60 years and above (Sanchez-Lara et al., 2021). Most recently, across 56 independent studies (n = 2,931), MBIs displayed superior effects on global cognition, EF, and WM, compared to no-treatment but not active controls (Whitfield et al., 2022).
Overall, previous reviews had several gaps that the current meta-analysis was designed to fill. First, beyond methodological limitations related to most of them, such as including uncontrolled or non-randomized studies, only two (Verhaeghen, 2021; Whitfield et al., 2022) tested if MBIs exerted differential effects on attentional control subdomains – alerting (or sustained attention), orienting, and executive attention. These attentional control domains should be examined separately as MBIs could influence them differently, given that they are neurologically dissociable despite their inter-connectedness (Posner & Rothbart, 2007). Further, prior MBI meta-analyses that examined moderators (Im et al., 2021; Verhaeghen, 2021) tended to test their effects only on global cognition. Since moderator effect sizes might be domain-specific, the current meta-analysis can provide more information by testing potential treatment and moderator effects on different cognitive domain outcomes. In addition, to our awareness, no reviews have investigated whether MBIs influenced processing speed, subjective cognitive functioning, and cognitive error, despite the theories above suggesting those possibilities. Also, it may be helpful to test the effects of MBIs on both objective (performance-based) cognitive functioning domains and subjective (self-reported) attentional control, as these aspects of cognitive functioning might not align (Vago et al., 2019; Van Dam et al., 2018). Doing so also permits examining if MBIs affected accuracy- more than latency-based markers of EF.
Additionally, no prior reviews have investigated whether instructor-led face-to-face (vs. self-guided) MBIs were more potent at changing cognitive outcomes. This question is becoming more important given the recent rise in mostly low-intensity self-help digital MBIs (Mrazek et al., 2019), highlighting the importance of determining the effectiveness of such MBIs in improving brain health on a broader scale. Relatedly, most prior meta-analyses of MBIs have not tested if gender, study quality, retention percentage, and complete-case (vs. intent-to-treat; ITT) analyses would moderate the impact of MBIs on cognitive functioning. Such efforts are necessary to determine under which conditions MBIs would be of benefit. Also, as lack of attention to treatment integrity is a field-wide major limitation concerning the state of science on this topic (Crane & Hecht, 2018a), our meta-analysis adds to prior ones by including the presence of reported treatment fidelity checks as a covariate. In addition, whereas most prior meta-analyses had restricted age ranges, we tested the main and interaction treatment effects of MBIs on cognitive functioning across the lifespan. Also, we examined only MBI RCTs and had 95 (Cásedas et al., 2020), 84 (Yakobi et al., 2021), and 55 (Whitfield et al., 2022) more studies than recent RCT-focused ones.
Most importantly, our efforts thus offer a more accurate, comprehensive, and up-to-date review, particularly by examining the impact of MBIs on pre-post global cognition and 15 cognitive functioning domains and its effects on pre-follow-up global cognition. These 15 cognitive subdomains are essential to study as separate MBI outcomes as they contribute to daily functioning, well-being, and task performance and could mitigate the risk for or target issues related to cognitive disorders (e.g., attention-deficit/hyperactivity disorder (ADHD), dementia), and improve clinical outcomes (Braenden et al., 2023; Lenze et al., 2022). The upshot is that understanding the potential and limits of MBIs to enhance these 15 cognitive subdomains may advance psychological sciences via positive cumulative personal and societal impacts.
Considering the above, an up-to-date systematic quantitative review was conducted to quantitatively synthesize 111 RCTs (n = 9,538) to assess the strength of the effect of MBIs on global cognition and the following unique cognitive subdomains: orienting, executive attention, WM accuracy and latency, inhibition accuracy and latency, shifting accuracy and latency, sustained attention (accuracy or intra-individual coefficient of variation), subjective cognitive functioning, processing speed, verbal fluency, episodic memory, and cognitive error. We selected these 15 subdomains because there was sufficient RCT literature to conduct a meta-analysis. Doing so can catalyze future efforts to advance the field on this topic by examining the effects of MBIs on other understudied cognitive subdomains, such as decision-making (Fernando et al., 2016; Kirk et al., 2016), inductive reasoning (Shapiro et al., 2012), language (Dickinson et al., 2016), and delay discounting (MacKillop et al., 2011). Moreover, as previous reviews arrived at varying conclusions, this systematic review tested factors that may have moderated the strength of the effect of MBIs on unique cognitive subdomains.
Method
Search
Search terms and databases.
This meta-analysis was carried out using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Moher et al., 2009) and was registered with the International Prospective Register of Systematic Reviews (PROSPERO; #CRD42020220576; https://tinyurl.com/5bhrmnub). We defined eligibility criteria and methods before the search and selection process and continually documented these steps in a study protocol. Relevant studies were identified by searching five databases (ScienceDirect, PubMed, PsycINFO, Google Scholar, and Cochrane Library). Search dates included all articles that met eligibility criteria from January 1989 to December 2022. We used the following keyword combinations: “mindful*,” or “mindful* training” or “meditation” and “cognition,” “attention,” “executive attention,” “cognitive control,” “shifting,” “switching,” “inhibition,” “inhibitory control,” “cognitive flexibility,” “working memory,” “verbal fluency” and “randomized controlled trial” or “RCT.” Further, we systematically searched through reference sections of articles pertinent to our research question and eligible studies. To reduce the odds of publication bias (i.e., file drawer problem; Rosenthal, 1979), we included unpublished master’s theses and doctoral dissertations that met eligibility criteria. Moreover, we searched for potentially eligible articles via PsyArXiv Preprints and requested eligible data from pertinent society listservs.
Screening process.
Eligibility criteria included: (1) sample comprised meditation naïve participants; (2) random assignment to MBIs vs. no-treatment, waitlist, or active control; (3) administration of at least one behavioral, cognitive assessment, or subjective cognitive functioning measure at baseline and post-treatment; (4) teaching mindfulness skills was the primary focus of treatment (Creswell, 2017). Specifically, MBIs had to include psychoeducation and FA and/or OM skills delivery. (5) MBIs had to include at least two sessions (note that number of sessions was also examined as a moderator). Also, homework was prescribed.
We excluded studies if: (1) data was inadequate to calculate effect sizes; (2) they used acceptance and commitment therapy, dialectical behavior therapy, integrative mind-body training, loving-kindness meditation, neurofeedback mindfulness training, mantra-based training, hatha yoga, or mindfulness-oriented yoga, self-compassion training, were augmented with aromatherapy or (3) a control condition contained any form of MBIs or MBI components (see Figure 1 for PRISMA flowchart).
Figure 1. PRISMA flowchart summarizing the study identification, screening, and selection process.
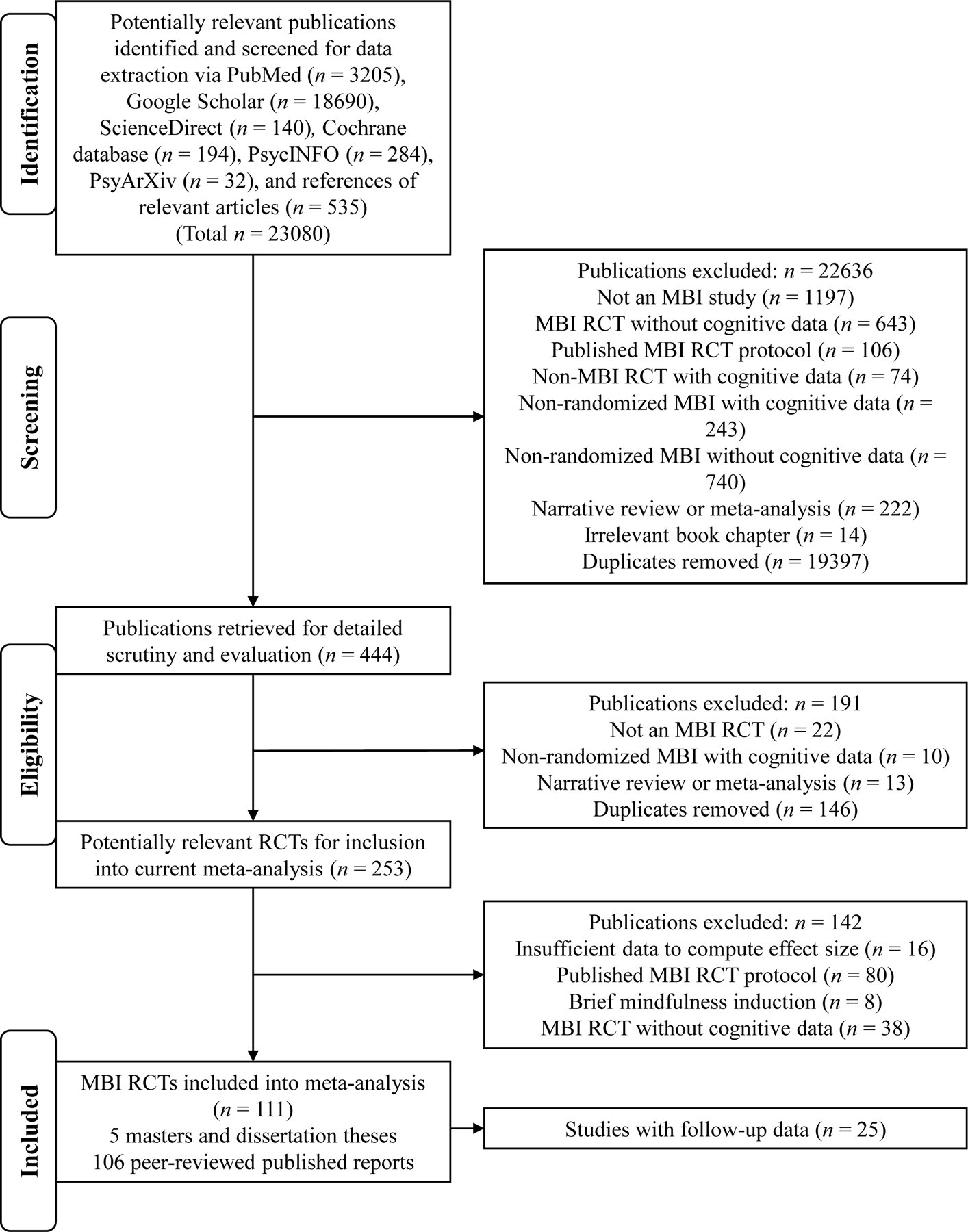
Note. MBI = mindfulness-based intervention; PRISMA = preferred reporting items for systematic reviews and meta-analyses; RCT = randomized controlled trial.
Coding procedures
We double-coded studies (k = 111) for participant attributes (e.g., age, percentage of female), clinical status (i.e., healthy control (HC), participants with elevated psychiatric symptoms (PSY) or medical/physical illness symptoms (MED)), treatment attributes (e.g., number of sessions, number of session hours), active (cognitive-behavioral therapy (CBT), cognitive training, psychoeducation-only, or treatment-as-usual (TAU) that involved some intervention) vs. no treatment or waitlist control condition, self-guided vs. teacher-led, standard (defined as MBSR or MBCT) vs. non-standard MBI, study attributes (study quality, presence of fidelity checks, retention percentage), and cognitive function outcome attributes. The first author coded and extracted data from all studies. A second coder from a research team of 16 members also independently coded for reliability. All coders underwent a standardized and rigorous training protocol that involved a mixture of didactics, regular meetings, consultations, and literature reviews. Discrepancies were resolved via regular discussion, and coders reached an agreement regarding a final set of codes.
Study quality.
We evaluated study quality based on an adapted version of the Delphi criteria (Verhagen et al., 1998). The modified criteria were: (1) randomization conducted, (2) individuals in both conditions were demographically alike, (3) eligibility criteria defined, (4) experimenters who administered cognitive function measures were uninformed of treatment allocation, (5) sufficient descriptive statistics (e.g., mean and standard deviations at all periods) were reported or available upon request to compute effect sizes for pre-to-post treatment changes, (6) ITT analysis used. Fulfilling each criterion received one point (vs. a zero). The Delphi score thus ranged from 0 to 6. In addition, this Delphi score study quality rating was used in the moderator analysis. We also assessed study quality using the Cochrane Collaboration risk of bias instrument (Higgins et al., 2011).
Measurement properties
Cognitive data were coded for global cognition and 15 cognitive subdomains: orienting, executive attention, WM accuracy or latency, inhibition accuracy or latency, shifting accuracy or latency, sustained attention (accuracy or intra-individual coefficient of variation), subjective cognitive functioning, processing speed, verbal fluency, episodic memory, and cognitive error. Table 1 in the main manuscript and Table S1 in the online supplemental materials (OSM) provide information on the definitions of global cognition, the 15 cognitive subdomains examined in the current meta-analysis, and the different types of tests classified in each cognitive subdomain. The OSM also details the specific measures used for each cognitive subdomain and its psychometric properties.
Table 1.
Definition of unique cognitive functioning subdomains and their specific tests
| Episodic Memory: Capacity to correctly recall previous events, facts, and information with their situational context (Allen & Fortin, 2013; Tulving, 2002). |
| CVLT-LDFR (Delis et al., 2017): Participants received instructions to listen and recall words on a 16-item list following each of the five learning trials. Following a distractor list, participants were again instructed to retrieve words verbally spontaneously (short delay-free recall) (SDFR) and with categorical cues. After the longer delay, participants underwent a yes/no recognition trial that required them to differentiate between the target words in the prior 16-item list and 32 distractor list. The CVLT-LDFR score could range from 0 to 16. |
|
|
| Attentional Control: Basic ability to regulate mental focus on tasks consistent with a desired aim (Sorensen et al., 2018). |
|
|
| Attentional Control – Executive Attention: Ability to skillfully manage responses in the face of conflicting thoughts, emotions, and responses or conflict monitoring (Petersen & Posner, 2012). |
|
|
| ANT – Executive attention (Fan et al., 2002; Posner et al., 2015): Participants had to classify as rapidly and accurately as possible if the central (target) arrow pointed left or right on double cue trials where flanker arrows pointed in the same direction (congruent trials) or opposite direction (incongruent trials). Executive control was computed by subtracting the average RT of congruent trials from the average RT of incongruent trials such that large positive scores signified poorer executive attention. |
|
|
| Attentional Control – Orienting: Honing focus on an object amid diverse sensory input or selective attention (Ristic et al., 2007; Sood & Jones, 2013). |
| ANT – Orienting (Fan et al., 2002; Posner et al., 2015): Refer to the description above. Orienting was computed by subtracting the average RT on spatial cue trials from the average RT on center cue trials (both trials informed participants on target onset, but they received cues of spatial orienting only on spatial-cue trials). |
|
|
| Executive Functioning (EF): Higher complex cognitive control functions responsible for governing cognitive and behavioral processes. |
|
|
| Inhibitory Control: Ability to refrain from autopilot response tendencies effortfully (Jewsbury et al., 2016). |
| Stroop test (Stroop, 1935): Participants viewed matrices of color-words printed in blue, red, and green ink that was either congruent (e.g., “red” word with red ink) or incongruent (e.g., “red” word with blue ink) and were asked to name the ink color as rapidly and accurately as possible. RT and task accuracy were documented for this test. |
|
|
| Set-Shifting: Capacity to switch back and forth between distinct thinking modes fluently (Berg, 1948; Chiu et al., 2018). |
| WCST (Grant & Berg, 1948): Participants were given four stimulus cards (mixture of shapes, colors, and numbers) across up to 64 or 128 trials for 10 to 20 minutes. Per the instructions, they sorted the cards based on specific rules (i.e., shape, color, or number) across trials and received feedback during each trial on whether their choice was correct or wrong. |
|
|
| Working Memory (WM): Adeptness to continually monitor environmental input and replace out-of-date information with new information (Jha et al., 2019; Miyake et al., 2000; Vago et al., 2019). |
| N-Back Task (Kane et al., 2007; Owen et al., 2005): Participants were instructed to retain information for a specific stimulus. Further, when a new stimulus substitutes the most prior one, the WM should update the information. The count of accurate responses and RT were indicators of WM performance. Similar variants of the n-back tasks used in previous MBIs RCTs exist (e.g., NIH-EXAMINER) (Kramer et al., 2014). |
|
|
| Verbal Fluency: Capacity to generate as many relevant words based on a cue (e.g., semantic category, letter) within a time limit (Henry & Crawford, 2004; Raucher-Chéné et al., 2017). |
| COWAT – Phonemic (Benton & Hampsher, 1978): Participants had to name as many unique words within 1 minute based on a phonemic cue (e.g., the letter “F,” “A,” or “S.”). |
|
|
| Subjective Cognitive Functioning: Perception of the degree one believes in their capacity to stay focused on task, process information, memorize facts, and exercise other cognitive functioning faculties (Daglas-Georgiou et al., 2022; Hallion et al., 2019). |
| ACS (Derryberry & Reed, 2002; Judah et al., 2014): Participants rated their perception of how well they could generally focus on the task at hand and flexibly shift attention between different tasks. |
|
|
| Sustained Attention Accuracy: Degree of correctness and consistency with staying on-task (Esterman & Rothlein, 2019). Sustained attention has also been defined as alerting (essential arousal or awareness of objects) (Prakash et al., 2020). |
| CPT (Corbett et al., 2009; MacLean et al., 2010): Participants received instructions to focus on the screen, saw one integer appear on the screen at a time, and had to press the spacebar when a specific number (e.g., the integer “6”) or letter (e.g., “K” or “X”) appeared. In the AX-CPT version (Braver, 2012; Servan-Schreiber et al., 1996), participants were told to offer a target response to an “X” probe after an “A” cue and to offer a non-target response for other kinds of non-target trials: cue “A” and subsequently a “non-X” probe letter (i.e., “AY” trial); a “non-A” and subsequently an “X” probe letter (i.e., BX trial); and a “non-A” cue and subsequently a “non-X” probe letter (i.e., “BY” trial). Higher number of accurate responses indicated better sustained attention ability. |
|
|
| Intra-Individual Coefficient of Variation: Degree of variability in offering accurate responses on sustained attention tasks (Bellgrove et al., 2004; Cubillo et al., 2023). |
| DART (Dockree et al., 2006; Robertson et al., 1997): Participants underwent procedures similar to the SART with the addition of a CPT to enhance the sensitivity of capturing sustained attention in healthy adults. Higher RT coefficient of variation (CV) for white integers denoted poorer overall DART performance. |
|
|
| Processing Speed: Degree of task completion efficiency (Muller et al., 2021). |
| LDST (Lezak et al., 2012; Smith, 1982; van der Elst et al., 2006): This assessment was adapted from earlier substitution tests, i.e., the Symbol Digit Modalities Test (SDMT) and the Digit Symbol Substitution Test (DSST). The DSST required participants to attend to a symbol-letter key and to write down the matching symbol beneath each digit in a blank space. In contrast, the instructions for SDMT were reversed (i.e., participants received instructions to write down the matching number). Simultaneously, participants could also verbalize answers for the DSST. The LDST differed from the earlier versions by including “over-learned” symbols, i.e., letters and numbers. Therefore, participants received instructions to learn the digit-letter connections, whereas other substitution tests required participants to acquire abstract symbols. |
|
|
| Cognitive Errors: Mistakes by commission or omission (Fetterman & Robinson, 2011). |
| d2 Test of Attention (Brickenkamp, 2002): Higher total error rate (i.e., commission errors and omission errors divided by total possible accurate responses), the error percentage (total errors divided by total processed responses multiplied by 100), and the error distribution (i.e., error sums for the three assessment sections – lines 1–5, lines 5–10, and lines 11–14) indicated more cognitive errors. |
|
|
| Global Cognition: Composite of all said cognitive subdomains herein. |
| MOCA (Nasreddine et al., 2005): A brief clinician-administered neurocognitive assessment that includes abstract reasoning, attention, language, orientation to time and place, short-term memory, and visuospatial function. |
Note. ACS = attention control scale; ANT = attention network test; COWAT = controlled oral word association task; CPT = continuous performance test; CVLT-LDFR = California verbal learning test-long delay-free recall; DART = dual attention response task; DCCS = dimensional change card sort task; DEX = dysexecutive questionnaire; DSB = digit span backward; DSF = digit span forward; LDST = letter-digit substitution task; MBI = mindfulness-based intervention; MOCA = Montreal cognitive assessment; RCT = randomized controlled trial; RT = response time; SART = sustained attention response task; SDMT = symbol digit modalities test; WCST = Wisconsin card sorting test.
Planned analyses
All analyses were conducted in R Version 4.0.1. Inter-rater agreement was established with the irr package in R (Gamer et al., 2007). The R packages robumeta (Fisher et al., 2017), metafor (Viechtbauer, 2010), and ggplot2 (Wickham, 2016) were used to examine treatment effects, study heterogeneity, outliers, and publication bias and to create funnel and forest plots. R syntax of analyses is available on Open Science Framework.
Reliability.
We established inter-rater agreement by computing two-way intra-class correlation coefficients (ICCs) for continuous variables (Shrout & Fleiss, 1979) and unweighted Cohen’s kappa (κ) for all binary or nominal variables (Hallgren, 2012).
Effect sizes.
Due to the diversity of studies, such as the varying number of treatment comparators (1–2) and cognitive outcome measures, we applied a random effects model (Borenstein et al., 2009). Further, we used robust variance estimation (RVE) with small sample adjustments to account for the non-independence of effect sizes clustered within the same samples and for studies with multiple treatment comparators (Tanner-Smith et al., 2016). Moreover, these RVE approaches produced effect size and 95% confidence interval (CI) estimates that account for effect size dependency. Effect sizes were coded such that higher values signified better cognitive outcomes between the treatment and control groups.
Based on random-effects models using pre- and post-treatment data between groups, we computed Hedge’s g to obtain accurate and unbiased parameter estimates (e.g., correcting for biases due to small sample size) to calculate pre-post effect sizes. As the pre- and post- correlation were not obtainable, we used a conservative estimate (r = .50) representative of the retest reliability of cognitive functioning tasks reported in the literature to date (Dai et al., 2019; Hedge et al., 2018). A similar approach was used for global cognition to calculate pre-follow-up treatment effect sizes (MBIs vs. waitlist or no-treatment and MBIs vs. active controls).2 We controlled for the presence of reported treatment fidelity checks in all effect size analyses.
We also contacted 15 authors for these descriptive statistics. Of these, nine responded. When we could not obtain the descriptive statistics, other inferential statistics (e.g., p, t, F) that permitted computing effect sizes based on pre-and post-treatment values (i.e., condition × time interaction) were calculated following recommendations by the Cochrane Collaboration (Higgins & Green, 2011). Effect sizes based on change scores (vs. post-treatment scores) are less affected by possible baseline differences (Johnsen & Friborg, 2015). Sampling variance was computed as the sum of variances for the treatment group and control group (Morris & DeShon, 2002, p. 117).
Outliers.
Outliers were defined as effect sizes with studentized deleted residuals more than ± 1.96 and Cook’s distance greater than the 50th percentile (Viechtbauer & Cheung, 2010). Sensitivity analyses tested if results remained the same with and without outlier(s).3 All findings in the current manuscript excluded outliers, as outliers estimate the population average as distinct from the average calculated from the remaining effect sizes. In total, six outliers were deleted.
Study heterogeneity.
To assess effect size heterogeneity, we used the I2 and Q statistic. I2 represents the degree of heterogeneity of the true observed dispersion due to between-study variability instead of within-study sampling error. I2 values of 25%, 50%, and 75% were considered small, moderate, and large, respectively (Higgins et al., 2003). A statistically significant Q statistic suggests that variability around the average effect size is higher than would be solely predicted from sampling error (Cochran, 1954). Importantly, significant heterogeneity was required before conducting moderator analyses.
Publication bias.
We assessed publication bias using the p-uniform test (van Assen et al., 2015) and inspected the funnel plots. Funnel plots illustrate publication bias by mapping each study’s effect size with its standard error, such that more significant asymmetry indicates more risk of bias. Figures S3a to S19b in the OSM provide funnel plots for all cognitive outcomes.
Results
Inter-rater agreement
At the screening stage, high levels of inter-rater agreement were observed for both continuous (ICC = .983) and categorical outcomes (κ = .978–.992). Likewise, at the data extraction stage, we found strong levels of inter-rater agreement for continuous (ICC = .960–1.000) and categorical outcomes (κ = .939–1.000). All item scores thus showed an excellent level of agreement. Fidelity checks were present in 64% of studies comparing MBIs to waitlist and no-treatment and 65% of studies comparing MBIs with active controls.
Sample characteristics
Tables S2 and S3 present study characteristics. Collectively, they included 9,538 participants with an average age of 33.98 years (SD = 20.05, range = 3.92–80.61, and of which 57.85% were female). The sample size ranged from 14 to 424, and the mean sample size was 84. Number of sessions ranged from 2 to 90 (M = 57.85, SD = 19.81). RCTs were conducted across 22 nations, most in the United States (k = 46, 41.44%). Forty-one out of 111 studies (36.94%) reported ethnicity, and in these studies, 60.93% of participants identified as White. No studies reported sexual orientation/gender identity. Concerning socioeconomic status, six studies recruited participants with low income and three with low socioeconomic status. Across the five studies that reported income figures, mean annual income ranged from $50,000 to $124,000. Also, the number of effect sizes for each independent study sample ranged from 1 to 39, with a mean of 6 effect sizes per study.
Effect of MBIs on cognitive domains compared to no-treatment or waitlist control
Effect size heterogeneity.
Significant moderate-to-large effect size heterogeneity was observed for global cognition, WM accuracy, WM latency, inhibition accuracy, processing speed, and cognitive error (Table S4).
Cognitive outcome effect sizes.
Table S4 and Figure S2 show the effects of MBIs (vs. controls) after outlier removal. Compared to waitlist or no-treatment, MBIs had significant small-to-large positive effects on global cognition (g = 0.583), executive attention (g = 0.301), WM accuracy (g = 0.326), inhibition accuracy (g = 0.643), shifting accuracy (g = 0.272), sustained attention accuracy (g = 0.367), and subjective cognitive functioning (g = 0.257).
Pre-follow-up effect on global cognition.
MBIs (vs. controls) had a significant and robust pre-follow-up treatment effect on global cognition, with a large effect size (g = 0.808).
Publication bias analyses for MBIs vs. waitlist/ no treatment
Based on p-uniform tests, no publication bias was observed for all cognitive subdomains examined from pre- to post-treatment and pre- to follow-up (p-uniform values = −2.69–0.00, p = .571–.997). Visual inspection of all funnel plots showed no asymmetry indicative of publication bias (Figures S2–S18 Part a).
Moderator analyses for MBIs vs. waitlist/ no treatment
Table S5 displays moderator analyses for MBIs vs. active control effect for global cognition, WM accuracy and latency, inhibition accuracy, processing speed, and cognitive error domains that showed significant effect size heterogeneity for domains with mixed outcomes.4
Age.
Older (vs. younger) individuals evidenced significantly smaller effects of MBIs (vs. waitlist or no-treatment) on WM accuracy (g = −0.502).
Percentage female.
More females led to a significantly weaker effect of MBIs (vs. waitlist or no-treatment) on processing speed (g = −3.122).
Study quality.
Higher study quality led to a significantly stronger effect of MBIs (vs. waitlist or no-treatment) on processing speed (g = 1.936).
Number of sessions.
Number of sessions did not significantly moderate the effect of MBIs (vs. waitlist or no-treatment) on any cognitive outcomes.
Treatment duration.
Total number of hours spent on treatment did not significantly moderate the effect of MBIs (vs. waitlist or no-treatment) on any cognitive outcomes.
Retention percentage.
Retention percentage did not significantly moderate the effect of MBIs (vs. waitlist or no-treatment) on any cognitive outcomes.
Complete-case analysis.
Complete-case (vs. ITT) analysis yielded a significantly stronger effect of MBIs (vs. waitlist or no-treatment) for global cognition (g = 0.619 vs. 0.478) and WM accuracy (g = 0.365 vs. 0.000886). ITT (vs. complete-case) analysis generated a significantly larger effect on inhibition accuracy (g = 0.804 vs. 0.556).
Type of MBI.
Standard MBSR or MBCT (vs. other non-standard MBI) had significantly stronger treatment effects for global cognition (g = 0.796 vs. 0.468), WM accuracy (g = 0.404 vs. 0.246), inhibition accuracy (g = 1.213 vs. 0.467), and cognitive error (g = 0.412 vs. 0.031).
Treatment delivery.
Self-guided MBI apps had a statistically significantly stronger treatment effect size than face-to-face MBIs for global cognition (g = 0.588 vs. 0.583), but the effect size difference was too small to be practically significant.
Clinical status.
MBIs (vs. no-treatment or waitlist) had a significantly larger treatment effect for persons with (vs. without) elevated psychiatric symptoms concerning global cognition (PSY: g = 0.822; MED: g = 0.618; HC: g = 0.345), WM accuracy (PSY: g = 0.396; MED: g = −0.251; HC: g = 0.301), inhibition accuracy (PSY: g = 0.974; HC: g = 0.300), and cognitive errors (PSY: g = 0.557; HC: g = 0.040).
Risk-of-bias for MBIs vs. no treatment/ waitlist
No RCTs included in this meta-analysis had high randomization bias. Some concerns emerged for 10.91% of the studies due to deviations from the intended intervention due to the trial context, but none showed a high risk of bias. There were concerns due to missing outcome data in 21.82% of the studies, as they did not report the degree of missing data or if appropriate steps such as multiple imputation or other reasonable data replacement strategies (e.g., full information maximum likelihood) were taken. However, no studies showed a high risk of bias due to missing data. In addition, some concerns emerged in 3.64% of the studies wherein assessors were aware of the participant’s treatment allocation, but the remaining 96.36% of studies had a low risk of bias. Concerning selection bias risk, one study (1.82%) had a high bias, 10.91% of studies showed some concerns, but the remaining 87.27% had a low risk of bias.
Comparison of significant treatment effect sizes for MBIs vs. no treatment/ waitlist
Table S5 in the OSM compares all MBI (vs. no-treatment or waitlist) effects on various cognitive functioning domains tested herein. These significant treatment effect sizes were not statistically significantly different from one another.
Effect of MBIs vs. active controls
Effect size heterogeneity.
Significant moderate-to-large effect size heterogeneity was observed for global cognition, inhibition latency, sustained attention accuracy, and subjective cognitive functioning (Table 2).
Table 2.
Effects of MBIs on global cognition and unique cognitive subdomain in comparison to active controls
| Cognitive outcome | ES N | k | N | Hedge’s g | 95% CI | Q | I 2 | p-uniform |
|---|---|---|---|---|---|---|---|---|
| Global Cognition | 374 | 72 | 5847 | 0.208 *** | [ 0.118, 0.298] | Q(df = 373) = 528.83 *** | 40.62 | −2.60 |
| Orienting | 10 | 6 | 733 | 0.303 | [ −0.338, 0.944] | Q(df = 9) = 16.60 | 63.55 | −1.70 |
| Executive attention | 19 | 14 | 1686 | 0.192 *** | [ 0.078, 0.306] | Q(df = 18) = 18.39 | 0.00 | 0.11 |
| WM accuracy | 37 | 25 | 2658 | 0.296 ** | [ 0.101, 0.490] | Q(df = 37) = 113.27 | 66.04 | −0.69 |
| WM latency | 12 | 8 | 749 | 0.105 | [ −0.108, 0.317] | Q(df = 11) = 6.00 | 0.00 | 0.00 |
| Inhibition accuracy | 22 | 12 | 1221 | 0.192 ** | [ 0.076, 0.307] | Q(df = 21) = 16.99 | 0.00 | −0.95 |
| Inhibition latency | 20 | 12 | 1182 | 0.015 | [ −0.702, 0.731] | Q(df = 19) = 32.78 * | 65.20 | −2.28 |
| Shifting accuracy | 18 | 10 | 1007 | 0.200 ** | [ 0.058, 0.341] | Q(df = 17) = 26.50 | 47.94 | −0.30 |
| Shifting latency | 18 | 13 | 1034 | −0.028 | [ −0.176, 0.120] | Q(df = 17) = 26.10 | 7.15 | −1.76 |
| Sustained attention accuracy | 54 | 23 | 3083 | 0.212 *** | [ 0.100, 0.325] | Q(df = 53) = 108.62 *** | 61.67 | −0.29 |
| Intra-individual coefficient of variation | 12 | 9 | 660 | 0.337 ** | [ 0.184, 0.490] | Q(df = 11) = 17.67 | 38.32 | −1.34 |
| Subjective cognitive functioning | 72 | 28 | 4278 | 0.394 *** | [ 0.190, 0.597] | Q(df = 71) = 414.30 *** | 80.43 | −0.81 |
| Processing speed | 13 | 6 | 560 | 0.381 | [−0.741, 1.504] | Q(df = 12) = 17.91 | 50.20 | −0.82 |
| Verbal fluency | 11 | 7 | 852 | 0.119 | [ −2.300, 2.535] | Q(df = 10) = 9.17 | 28.07 | 0.00 |
| Episodic memory | 22 | 10 | 1401 | 0.073 | [ −0.273, 0.420] | Q(df = 21) = 13.65 | 0.00 | 0.00 |
| Cognitive error | 30 | 8 | 1228 | 0.094 | [ −2.219, 2.410] | Q(df = 29) = 19.12 | 2.10 | 0.85 |
Note.
p≤.05;
p≤.01;
p≤.001.
MBI = mindfulness-based intervention; k = number of studies; ESN = number of effect size comparisons between mindfulness-based intervention and a comparison group; N = sample size pooled across various studies; CI = confidence interval around average parameter estimate; Q = a standardized indicator for the degree of homogeneity of effect sizes concerning the average effect size; I2 = a metric for the proportion of observed variability that indicates real effect size variability; WM = working memory.
Cognitive outcome effect sizes.
MBIs vs. active controls had significant effects on global cognition (g = 0.208), executive attention (g = 0.192), WM accuracy (g = 0.296), inhibition accuracy (g = 0.192), shifting accuracy (g = 0.200), sustained attention accuracy (g = 0.212), intra-individual coefficient of variation (g = 0.337), and subjective cognitive functioning (g = 0.394), with small-to-moderate effect sizes (Table 2 and Figure 2).
Figure 2. Forest plot of MBIs on global cognition and unique cognitive subdomain outcomes compared to active controls.
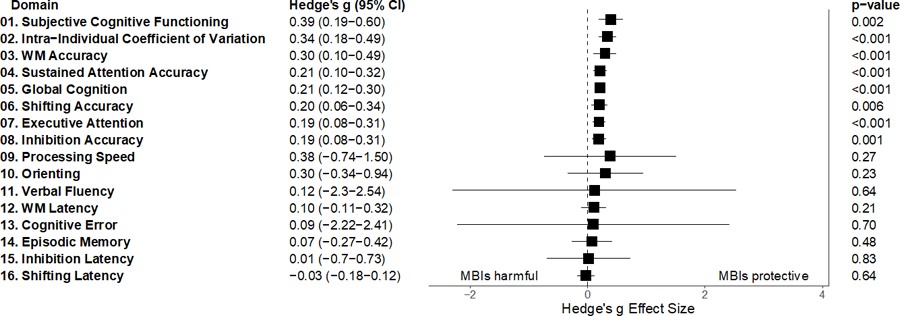
Note. MBI = mindfulness-based intervention; WM = working memory.
Pre-follow-up effect on global cognition.
There was a significant pre-follow-up effect of MBIs (vs. active controls) on global cognition, with a small effect size (g = 0.231).
Publication bias analyses for MBIs vs. active controls
The p-uniform tests found no publication bias for all cognitive subdomains inspected from pre- to post-treatment and pre- to follow-up. Visual inspection of all funnel plots showed no asymmetry suggesting publication bias (Figure S2–18 Part b).
Moderator analyses for MBIs vs. active controls
Table S6 displays moderator analyses for the effect of MBIs vs. active control effect for global cognition, inhibition latency, sustained attention accuracy, and subjective cognitive functioning domains that showed significant effect size heterogeneity.4
Age.
Age did not significantly moderate the effect of MBIs (vs. active controls) on any cognitive outcomes.
Percentage of females.
Percentage of females did not significantly moderate the effect of MBIs (vs. active controls) on any cognitive outcomes.
Study quality.
Study quality did not significantly moderate the effect of MBIs (vs. active controls) on any cognitive outcomes.
Number of sessions.
Number of sessions did not significantly moderate the effect of MBIs (vs. active controls) on any cognitive outcomes.
Treatment duration.
Total number of hours spent on treatment did not significantly moderate the effect of MBIs (vs. active controls) on any cognitive outcomes.
Retention percentage.
Retention percentage did not significantly moderate the effect of MBIs (vs. active controls) on any cognitive outcomes.
ITT (vs. Complete-case) analysis.
Complete-case (vs. ITT) analysis had a significantly smaller effect of MBIs (vs. active controls) on global cognition (g = 0.207 vs. 0.211), subjective cognitive functioning (g = 0.405 vs. 0.393), and sustained attention accuracy (g = 0.221 vs. 0.0672).
Type of MBI.
Non-standard MBIs (vs. standard MBSR or MBCT) had significantly stronger effects compared to active controls for global cognition (g = 0.229 vs. 0.171), sustained attention accuracy (g = 0.112 vs. −0.149), and subjective cognitive functioning (g = 0.475 vs. 0.276).
Treatment delivery.
Face-to-face MBIs had significantly larger treatment effects than self-guided MBIs compared to active controls for global cognition (g = 0.228 vs. 0.121), sustained attention accuracy (g = 0.115 vs. −0.00438), and subjective cognitive functioning (g = 0.413 vs. 0.312).
Clinical status.
The effect of MBIs (vs. active controls) on global cognition was significantly stronger for persons with elevated psychiatric symptoms and healthy controls than those with heightened medical symptoms (PSY: g = 0.211; HC: g = 0.222; MED: g = 0.130). Further, the impact of MBIs (vs. active controls) on sustained attention accuracy was significantly stronger for persons with elevated psychiatric symptoms than healthy controls and those with heightened medical symptoms (PSY: g = 0.201; MED: g = −0.0922; HC: g = 0.0911). For subjective cognitive functioning as the outcome, the effects of MBIs (vs. active controls) were significantly larger for persons with heightened medical and psychiatric symptoms than healthy controls (MED: g = 0.447; PSY: g = 0.307; HC: g = 0.436).
Risk-of-bias for MBIs vs. active controls
No studies (0%) showed a risk of randomization bias. Some concerns emerged for 19.72% of the studies regarding bias due to deviations from intended interventions, but none showed a high risk of bias. Some missing data bias concerns were identified for 24.66% of the studies, but none showed high risk of bias. Some measurement bias concerns arose for 9.59% of studies, but none showed high risk of bias. Some selection bias concerns were present for 12.33% of studies, but none had a high risk of bias.
Comparison of significant treatment effect sizes for MBIs vs. active controls
Table S9 compares all MBIs (vs. active controls) effects on various cognitive functioning domains examined herein. All treatment effect sizes did not significantly vary from one another.
Discussion
Overall effects of MBIs on global cognition and 15 cognitive subdomains
Our novel meta-analysis of 111 RCTs observed that MBIs had small-to-moderate effects on global cognition, executive attention, WM accuracy, inhibition accuracy, shifting accuracy, sustained attention, and subjective cognitive functioning. These findings were true compared to no-treatment and waitlist (average g = 0.249–0.644) and active controls (average g = 0.192–0.394), even after adjusting for treatment fidelity in all analyses. Here, we mainly focus on the comparative effects with active controls as comparators since these trials offer a more accurate and precise answer to the inquiry of whether MBIs improve cognitive functioning as compared to other treatments. Moreover, in interpreting the findings, we highlight that no evidence for a significant effect between MBIs and any control does not equal evidence for no effect. Also, we observed zero publication bias based on the p-uniform test and funnel plots, thus offering confidence in the validity of our findings and inferences drawn on how MBIs impact cognitive functioning, as detailed below.
Encouragingly, our results imply that in these domains, MBI-delivered skills were more potent than those imparted by active controls. However, as MBIs did not differ from controls in impacting nine out of 15 subdomains and significant effect sizes were small in the other domains, researchers and clinicians should exercise caution concerning MBIs’ beneficial effects on these nonsignificant domains, i.e., conclusions other researchers have drawn (e.g., Noone & Hogan, 2018; Van Dam et al., 2018). Meaningful inferences drawn from these findings include how the effect of MBIs on improved self-regulation (Tang et al., 2015) and reduced mind wandering (Mrazek et al., 2013) might be partly accounted for by the six specific cognitive domains serving as theoretical mechanisms of change. Potential policy and related applied implications based on these outcomes include the benefits of teaching mindfulness skills in primary care, specialist clinics (Elices et al., 2022), schools (Fulambarkar et al., 2023), and workplaces (Pérez-Fuentes et al., 2020) on specific cognitive domains for students, employees, and other stakeholders. Enhancements in specific cognitive functioning domains might also translate to better focus, resilience, and decision-making skills in governmental and related leadership settings (Oman, 2023).
Noteworthy is that the effect of MBIs on global cognition might be mainly attributable to significant effects on six specific cognitive subdomains. This possibility is based on evidence that substantial correlations exist between global cognition and these cognitive subdomains (Biagianti et al., 2019; Coors et al., 2022). Important implications and meaning of this finding are that targeting these six specific cognitive functioning domains via MBIs is probably more efficient than trying to enhance other cognitive functioning domains in various applied settings, such as clinics, government, schools, and workplaces.
Relatedly, the finding that MBIs’ impact on global cognition extended across time, in addition to evidence showing that MBIs had post-treatment effects that impacted cognition beyond attention measures (i.e., global cognition, executive attention, WM, inhibition accuracy, shifting accuracy), bolsters theoretical propositions that MBIs yield long-term persistent effects (Malinowski & Shalamanova, 2017), and lead to generalization of skills to tasks, objects, or contents beyond the ones practiced. Moreover, results that treatment effect sizes did not substantially differ between measures of attentional control and EF vs. other cognitive subdomains might provide more evidence for such viewpoints. Collectively, the topic of the benefit of MBIs on specific cognitive functioning subdomains over extended periods deserves more investigation. Our current meta-analysis was only well-powered to examine global cognition at follow-up, but not other unique cognitive subdomains. More importantly, these outcomes highlight the importance of relaying the long-term benefits of practicing mindfulness on global cognition when evaluating the policy impact of disseminating MBIs. For instance, any population-level long-term efficacy of MBIs on well-being, as evidenced by prior research (Grossman et al., 2007), might be due to improved global cognition.
Mixed effects of MBIs
Attentional control constructs.
Findings that MBIs improved executive attention, intra-individual coefficient of variation, and sustained attention accuracy concur with theories positing that MBIs boost unwavering focus and non-judgmental acceptance over time (Bishop et al., 2004). Assessing multiple sustained attention indices is essential to understand how MBIs enhance attentional stability. Moreover, our findings aligned with recent evidence that meditation practices enhanced accuracy instead of latency-based indices of attentional control components over time (Sumantry & Stewart, 2021). Essential clinical and educational implications include the potential to help youths and adults with ADHD and related attentional disorders via MBIs, as suggested by recent theories (Cairncross & Miller, 2020). The upshot is that MBIs promote attentional health aspects of mental well-being, i.e., the state of a person’s attentional capacity or functioning (Stark & Cimprich, 2003).
Intriguingly, MBIs (vs. active controls) improved executive attention but were not substantially different when targeting orienting aspects of attentional control. These findings support recent formulations (Prakash et al., 2020) about the specific effects of MBIs on different attentional control facets. Theories suggesting that MBIs promote executive attention by reducing mind wandering, attentional lapses, and emotional distractions (Good et al., 2015; Hölzel et al., 2011; Lin et al., 2019; Vago & Silbersweig, 2012) could account for these findings. Conversely, findings of no evidence of MBI (vs. control) effects on orienting were surprising since MBIs instruct selective attention for some exercises, such as body scans and focused imagery, and adopting a “decentered” stance for other exercises (e.g., nonjudgment; Bishop et al., 2004; Sumantry & Stewart, 2021; Verhaeghen, 2021). Note that the absence of evidence of an intervention effect does not imply evidence of the absence of such an intervention effect (Gelman & Stern, 2006; Harms & Lakens, 2018). An intervention effect of MBIs on orienting may exist but may require a long-term commitment to mindfulness practices (Isbel & Mahar, 2015; Lodha & Gupta, 2022) or other MBI modalities (Green & Bavelier, 2003) to enhance the orienting subdomain. Mixed prior findings of positive effects in one study (e.g., Jha et al., 2007) but null effects of MBIs on orienting in another (Felver et al., 2017) also possibly suggest heterogeneity of treatment effects (Kent et al., 2020) and the importance of discovering for whom MBIs confer beneficial effects on the orienting subdomain. However, these potential accounts require precise empirical testing, preferably by using experiments and random assignment among diverse groups.
EF constructs.
There was no evidence of MBI (vs. control) effects on WM, inhibition, shifting latencies, and processing speed. Overall, results suggest that MBIs primarily impacted cognitive processing effectiveness (captured by accuracy) more than efficiency (measured by latency) and offer only partial support for the viewpoint that MBIs promote both aspects of cognitive function (Jang et al., 2018; Raffone & Srinivasan, 2017). Nonsignificant difference on efficiency may be due to the calming and non-pressured nature of mindfulness practices. Thus, the delivery of MBIs might be optimized by emphasizing to participants the importance of focusing on the process instead of the outcome in goal-attainment endeavors. Construed clinically, such messages might particularly benefit those with anxiety and related disorders who usually self-reported struggles with racing and perseverative thoughts that compromise EF and associated capacities (Spinhoven et al., 2022; Zainal & Newman, 2022).
Non-significant effects: Episodic memory, verbal fluency, & cognitive error
Also, there was no evidence of MBI (vs. control) effects on episodic memory, verbal fluency, and cognitive error. Such results support hypotheses of null relations between trait mindfulness and declarative/episodic memory vs. emotionally-charged or personally-salient autobiographical memories (Levi & Rosenstreich, 2019; Whitfield et al., 2022). The findings also support hypotheses that MBIs likely do not assist with the storage and recall phases of verbal learning (Lueke & Lueke, 2019; Whitfield et al., 2022). Conversely, the outcomes differed from a recent qualitative review that indicated a beneficial effect of MBIs on verbal fluency (Hazlett-Stevens et al., 2019); however, that review focused on older adults and assessed verbal fluency solely with the controlled oral word association test. More importantly, the limitations of MBIs (i.e., what our research has shown it may not impact) should be explicitly communicated when delivering these interventions to improve cognitive functioning. Our nonsignificant results might also mean that the cognitive functioning measures of episodic memory, verbal fluency, and cognitive error must be sensitive to changes in RCTs. Such sensitive assessments are necessary to accurately detect changes over time and assess the efficacy of MBIs targeting cognitive improvement (Shields et al., 2023).
Moderators to examine heterogeneity of treatment effects
Number of sessions and treatment duration.
There was no evidence that number of sessions and treatment duration were treatment moderators, contradicting the dose-response treatment effects hypothesis (Chiesa et al., 2011) and replicating recent quantitative reviews (Im et al., 2021; Verhaeghen, 2021). These nonsignificant findings are encouraging since brief MBIs might alleviate distress and enhance cognitive functioning (Schumer et al., 2018), which could have major clinical implications concerning scalability and dissemination. Practitioners delivering MBIs and seeking to shrink the implementation gap should thus accentuate the pragmatic cognitive benefits of brief mindfulness exercises daily, regardless of a busy schedule. On this note, low adherence has been touted as one of the reasons why the potential of MBIs on various health-related outcomes has been underrealized (Baydoun et al., 2021). Brief MBIs that are more actionable and easier to integrate into one’s lifestyle than lengthier ones thus bode well in efforts to improve specific cognitive functioning domains (Zainal & Newman, 2023).
Study quality.
There was no evidence that study quality moderated the effect of MBIs (vs. active controls) on global cognition, inhibition latency, sustained attention accuracy, and subjective cognitive functioning. Future RCTs should continue to exemplify high standards.
Socio-demographics.
We found no evidence that age moderated the effects of MBIs (vs. active controls) on global cognition, WM latency, inhibition accuracy and latency, processing speed, cognitive error, sustained attention accuracy, and subjective cognitive functioning. Findings align with theories that argue MBIs can benefit cognitive functioning equally for adults at various developmental stages (e.g., Berk et al., 2017). Further, no evidence that gender moderated the impact of MBIs (vs. active controls) on global cognition, inhibition latency, sustained attention accuracy, and subjective cognitive functioning emerged, supporting the idea that MBIs likely positively influence males and females equally (Katz & Toner, 2013). MBI instructors should spotlight these findings to foster diversity, equity, and inclusion when attempting to improve cognitive functioning via MBIs in various sociodemographic groups.
Clinical status.
MBIs (vs. active controls) had stronger effects on global cognition and sustained attention accuracy for those with elevated psychiatric symptoms and healthy controls than those with heightened medical symptoms. However, the impact of MBIs on subjective cognitive functioning was more pronounced for persons with heightened medical symptoms, followed by healthy controls and then those with elevated psychiatric symptoms. The reasons for these contradictory results remain unclear. Perhaps the stronger correlation between negative affective symptoms and the mindfulness describing skills in medical samples (Carpenter et al., 2019), coupled with higher distress levels and the motivating effect of physical illness stressors on mindfulness practices and related healthy behaviors, might explain these findings. Such factors could promote subjective cognitive functioning (Hodges et al., 2005; Sala et al., 2020). Future research is necessary to understand these results better. Overall, clinical implications from our findings include the possible therapeutic roles of MBIs in cognitive rehabilitation for cognitive impairments (e.g., ADHD, schizophrenia; Shen et al., 2023) and adjunctive benefits when offered in conjunction with other mental health treatments (Bursky et al., 2022). Other practical implications include the potential of MBIs in prevention and early intervention for non-clinical, albeit high-risk, subpopulations (Ma et al., 2019).
Treatment delivery.
Face-to-face MBIs (vs. active controls) than app- or Internet-delivered self-guided MBIs showed more potent effects on global cognition, sustained attention accuracy, and subjective cognitive functioning, but not inhibition latency. This pattern may be attributed to greater accountability and motivation with therapeutic support of face-to-face MBIs, concordant with literature on MBIs targeting depression, anxiety, and related mental health symptoms (French et al., 2017; Spijkerman et al., 2016), as proposed by the supportive accountability theory (Mohr et al., 2011) and efficiency model of support (Schueller et al., 2017). Future work should examine how the added benefits of the instructor-led format outweigh the gains of fully self-guided MBIs, such as scalability and reduced costs. If replicated, an essential policy implication is that self-guided MBIs should only be offered to subgroups that would benefit most from them (Benjet et al., 2023).
Type of MBI.
Non-standard MBIs (vs. standard MBSR or MBCT) showed stronger effects on global cognition, sustained attention accuracy, and subjective cognitive functioning. Studies comparing non-standard MBIs to active control tended to incorporate tailored treatments for specific populations (e.g., military cohorts; Jha et al., 2019). Adapting protocols to meet the needs of the target population might yield enhanced treatment effects compared to standard MBIs, a vital policy implication when developing and disseminating MBIs to specific subgroups. Achieving optimal efficacy in adapting MBIs necessitates thoughtful responses to unique cultural, organizational, or socio-political considerations (Oman, 2023). It is advisable to apply a meticulous “cost-benefit” analysis to discern which elements of MBIs necessitate adaptation, thereby ensuring the utmost suitability and effectiveness in optimizing cognitive functioning.
Study limitations and strengths
Study limitations should be considered. First, variations in the delivery of MBI protocols could not be fully accounted for (Cuijpers et al., 2008). Significant heterogeneity was observed for four domains (global cognition, inhibition latency, sustained attention accuracy, and subjective cognitive functioning) compared to active controls, indicating large irregularities in treatment structure and content (Van Dam et al., 2018; Whitfield et al., 2022). Future MBI RCTs should focus on standardizing MBI treatment protocol implementation to strengthen internal validity, construct validity, and replicability (Crane & Hecht, 2018b; Moncher & Prinz, 1991). Efforts should also address missing outcome data bias by employing the gold standard ITT analysis since complete-case analyses likely inflate effect sizes (McCoy, 2017). Additionally, the current meta-analysis cannot disambiguate the effects of specific MBIs techniques due to limited dismantling studies on cognitive outcomes (Britton et al., 2018).
Future efforts should isolate specific MBI components within RCTs via dismantling studies (Stein & Witkiewitz, 2020) and network meta-analyses (Furukawa et al., 2021) to better understand how MBIs enhance cognitive functions. Since stand-alone MBIs could yield comparable benefits to manualized MBI packages on psychological symptoms (Blanck et al., 2018), future studies could examine if this pattern extends to cognitive functioning. Moreover, testing the differential effects of unique mindfulness techniques, such as FA vs. OM, separate cognitive function subdomains (e.g., Britton et al., 2018) would advance the field.
Sample characteristics pose other shortcomings. Age range restrictions were observed in studies examining MBIs on orienting (ages 8–50), warranting investigations into treatment effects across older age groups. Ethnicity breakdown was not reported in 63% of studies, and virtually no studies reported the sexual orientation/gender identity of participants, highlighting severe shortcomings in the literature (Heck et al., 2017). Recruiting middle-class, White females with tertiary education and above was common (Mars & Abbey, 2010). It is essential to test MBIs’ impact on diverse populations, as outcomes may vary, such as weaker effects in older adults (Goldberg et al., 2021), children (Dunning et al., 2019), persons of color, and those with low income (Sun et al., 2022). Future studies should strive to include such information to reduce health disparities concerning the positive effects of MBIs on cognitive functioning.
Limitations notwithstanding, our meta-analysis has several strengths. We included unpublished theses and grey literature to address publication bias, including preprints (Lipsey & Wilson, 2001). Our dataset allowed us to test if age, gender, study quality, treatment duration, retention percentage, analysis approach, MBI type, delivery mode, clinical status, and fidelity checks moderated treatment effects. Further, this meta-analysis can catalyze future work on individual differences and treatment adaptations by synthesizing effect sizes to determine the impact of MBIs on various cognitive subdomains.
Conclusions
In summary, a comprehensive meta-analysis of 111 MBI RCTs suggested that MBIs benefitted global cognition and six cognitive subdomains (regardless of the control group and after adjusting for presence of fidelity checks). Specifically, MBIs showed positive effects on executive attention, inhibition accuracy, WM accuracy, shifting accuracy, sustained attention accuracy, intra-individual coefficient of variation, and subjective cognitive functioning. However, MBIs did not positively affect orienting, WM latency, inhibition latency, shifting latency, processing speed, verbal fluency, episodic memory, and cognitive error. Overall, MBIs improved EF and sustained attention accuracy-based rather than latency-based outcomes, likely because mindfulness practices promote present-moment awareness and effective goal attainment over efficiency (Hoge et al., 2021). These improvements in EF and sustained attention accuracy indices might contribute to why MBIs improve mood regulation (Gu et al., 2015) and physical immunity (Dunn & Dimolareva, 2022). Additionally, the enhancement of subjective cognitive functioning by MBIs might be one mechanism underlying improved flexible thinking and perspective-taking (Mediavilla et al., 2021).
Our extensive meta-analysis determined the effect of various moderators of MBIs on global cognition and 15 cognitive subdomains. Few significant moderator results emerged. Psychiatric and medical samples vs. healthy controls generally benefitted more from MBIs to target global cognition, some accuracy-based indices (inhibition, WM, sustained attention), and subjective cognitive functioning. Also, the absence of dose-response effects bodes well for the prospect of brief and scalable MBIs (e.g., Zainal & Newman, 2023) to enhance global cognition and the abovementioned six cognitive domains. Simultaneously, compared to self-guided MBIs, instructor-led face-to-face MBIs yielded more considerable impact on global cognition, sustained attention accuracy, and subjective cognitive functioning, highlighting the value of delivery by a qualified practitioner. Non-standard MBIs that tended to be highly tailored to specific target populations were better than standard MBIs in improving sustained attention accuracy and subjective cognitive functioning.
To conclude, our meta-analysis on the effect of MBIs on cognitive functioning adds to the extensive discourse that explored the potential advantages of mindfulness in clinical, education, workplace settings, and leadership roles, with a growing body of research actively examining these aspects (London et al., 2023). Our findings contribute to emerging narratives of policy implications of MBIs by augmenting a body of research showing that skills nurtured through MBIs encompassing compassion, mindfulness, and self-regulation (Bristow, 2019) could extend to specific cognitive functioning domains. Specifically, our findings suggest that MBIs can enhance cognitive functioning through the augmentation of executive attention, heightened WM, inhibition, set-shifting accuracy, sustained attention, and elevated subjective cognitive functioning. Hence, the integration of mindfulness in efforts to enhance specific cognitive functioning domains has the potential to play a critical role in shaping its future discourse and impact in the realms of research, policy, and practice.
Supplementary Material
Acknowledgments
We sincerely thank Drs. Nicole Anderson, Micela Balconi, Peter Malinowski, Michael Mrazek, Martin Prätzlich, Benjamin Schöne, Rob H.J. van der Lubbe, and Kathleen Walsh for providing descriptive data of the means and standard deviations of scores on all cognitive test(s) administered in their study at all time-points upon request. We also thank Dr. Mike Cheung at the National University of Singapore for offering statistical consultation to refine our Method section. We also wish to express gratitude to our 16 undergraduate research assistants – Ana Clever, Alexa Belnick, Armani Moore, Emma Win, Emily Forcht, Isabella Gonzalez, Jamie Gensbauer, Kathryn Miller, Madeline Lamonica, Madison Yeoman, Natalie Gottret, Natalie Suzette, Noor Lamba, Serena Chen, Shannon McGovern, and Vivian Nguyen – who served as reliability coders on the team and who regularly attended meta-analysis meetings to resolve any observed discrepancies between ratings.
Footnotes
This paper has not been peer-reviewed. Please do not copy or cite without the author’s permission.
Declarations of conflict of interest: none.
Due to space constraints, readers should refer to the definitions of italicized cognitive functioning constructs throughout the manuscript in Table 1 of the main manuscript and Table S1 in the online supplemental materials (OSM).
We calculated the pre-follow-up effect size only for global cognition because there were insufficient studies to synthesize effect sizes based on the 1 global cognition and 15 cognitive subdomains examined herein.
A similar pattern of results was attained when the analysis was carried out with and without the 6 outliers.
Due to space constraints, we only reported in text statistically significant results for all moderator analyses.
Contributor Information
Nur Hani Zainal, Harvard Medical School
Michelle G. Newman, The Pennsylvania State University
References
- Abbott RA, Whear R, Rodgers LR, Bethel A, Thompson Coon J, Kuyken W, … Dickens C. (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research, 76(5), 341–351. 10.1016/j.jpsychores.2014.02.012 [DOI] [PubMed] [Google Scholar]
- Allen TA, & Fortin NJ (2013). The evolution of episodic memory. Proceedings of the National Academy of Sciences, 110(Suppl. 2), 10379–10386. 10.1073/pnas.1301199110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anālayo B (2019a). Meditation on the breath: Mindfulness and focused attention. Mindfulness, 10(8), 1684–1691. 10.1007/s12671-019-01169-9 [DOI] [Google Scholar]
- Anālayo B (2019b). Open monitoring and mindfulness. Mindfulness, 10(7), 1437–1442. 10.1007/s12671-019-01181-z [DOI] [Google Scholar]
- Awh E, Belopolsky AV, & Theeuwes J (2012). Top-down versus bottom-up attentional control: a failed theoretical dichotomy. Trends in Cognitive Sciences, 16(8), 437–443. 10.1016/j.tics.2012.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GT, & Allen KB (2004). Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment, 11(3), 191–206. 10.1177/1073191104268029 [DOI] [PubMed] [Google Scholar]
- Baydoun M, Moran C, McLennan A, Piedalue KL, Oberoi D, & Carlson LE (2021). Mindfulness-based interventions in cancer survivors: A systematic review of participants’ adherence to home practice. Patient Preference and Adherence, 15, 1225–1242. 10.2147/PPA.S267064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellgrove MA, Hester R, & Garavan H (2004). The functional neuroanatomical correlates of response variability: Evidence from a response inhibition task. Neuropsychologia, 42(14), 1910–1916. 10.1016/j.neuropsychologia.2004.05.007 [DOI] [PubMed] [Google Scholar]
- Benjet C, Zainal NH, Albor Y, Alvis-Barranco L, Carrasco-Tapias N, Contreras-Ibáñez CC, … Kessler RC (2023). A precision treatment model for internet-delivered cognitive behavioral therapy for anxiety and depression among university students: A secondary analysis of a randomized clinical trial. JAMA Psychiatry 10.1001/jamapsychiatry.2023.1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton A, & Hampsher K (1978). Multilingual aphasia examination University of Iowa. [Google Scholar]
- Berg EA (1948). A simple objective technique for measuring flexibility in thinking. Journal of General Psychology, 39(1), 15–22. 10.1080/00221309.1948.9918159 [DOI] [PubMed] [Google Scholar]
- Berk L, van Boxtel M, & van Os J (2017). Can mindfulness-based interventions influence cognitive functioning in older adults? A review and considerations for future research. Aging & Mental Health, 21(11), 1113–1120. 10.1080/13607863.2016.1247423 [DOI] [PubMed] [Google Scholar]
- Biagianti B, Fisher M, Brandrett B, Schlosser D, Loewy R, Nahum M, & Vinogradov S (2019). Development and testing of a web-based battery to remotely assess cognitive health in individuals with schizophrenia. Schizophrenia Research, 208, 250–257. 10.1016/j.schres.2019.01.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop S, Duncan J, Brett M, & Lawrence AD (2004). Prefrontal cortical function and anxiety: Controlling attention to threat-related stimuli. Nature Neuroscience, 7(2), 184–188. 10.1038/nn1173 [DOI] [PubMed] [Google Scholar]
- Black DS, & Slavich GM (2016). Mindfulness meditation and the immune system: A systematic review of randomized controlled trials. Annals of the New York Academy of Sciences, 1373(1), 13–24. 10.1111/nyas.12998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanck P, Perleth S, Heidenreich T, Kröger P, Ditzen B, Bents H, & Mander J (2018). Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: Systematic review and meta-analysis. Behaviour Research and Therapy, 102, 25–35. 10.1016/j.brat.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2009). Fixed-effect model. In Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (Eds.), Introduction to meta-analysis (pp. 63–68). John Wiley & Sons, Ltd. [Google Scholar]
- Braenden A, Coldevin M, Zeiner P, Stubberud J, & Melinder A (2023). Executive function in children with disruptive mood dysregulation disorder compared to attention-deficit/hyperactivity disorder and oppositional defiant disorder, and in children with different irritability levels. European Child & Adolescent Psychiatry, 1–11. 10.1007/s00787-023-02143-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braver TS (2012). The variable nature of cognitive control: A dual mechanisms framework. Trends in Cognitive Sciences, 16(2), 106–113. 10.1016/j.tics.2011.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brickenkamp R (2002). Afmerksamkeits-Belastungs-Test (Test d2) [The D2 Test of Attention] (9th ed.). Hogrefe. [Google Scholar]
- Bristow J (2019). Mindfulness in politics and public policy. Curr Opin Psychol, 28, 87–91. 10.1016/j.copsyc.2018.11.003 [DOI] [PubMed] [Google Scholar]
- Britton WB, Davis JH, Loucks EB, Peterson B, Cullen BH, Reuter L, … Lindahl JR. (2018). Dismantling mindfulness-based cognitive therapy: Creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behaviour Research and Therapy, 101, 92–107. 10.1016/j.brat.2017.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bursky M, Egglefield DA, Schiff SG, Premnath P, & Sneed JR (2022). Mindfulness-enhanced computerized cognitive training for depression: An integrative review and proposed model targeting the cognitive control and default-mode networks. Brain Sciences, 12(5). 10.3390/brainsci12050663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairncross M, & Miller CJ (2020). The effectiveness of mindfulness-based therapies for ADHD: A meta-analytic review. J Atten Disord, 24(5), 627–643. 10.1177/1087054715625301 [DOI] [PubMed] [Google Scholar]
- Carpenter JK, Conroy K, Gomez AF, Curren LC, & Hofmann SG (2019). The relationship between trait mindfulness and affective symptoms: A meta-analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clinical Psychology Review, 74, 101785. 10.1016/j.cpr.2019.101785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cásedas L, Pirruccio V, Vadillo MA, & Lupiáñez J (2020). Does mindfulness meditation training enhance executive control? A systematic review and meta-analysis of randomized controlled trials in adults. Mindfulness, 11(2), 411–424. 10.1007/s12671-019-01279-4 [DOI] [Google Scholar]
- Chiesa A, Calati R, & Serretti A (2011). Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clinical Psychology Review, 31(3), 449–464. 10.1016/j.cpr.2010.11.003 [DOI] [PubMed] [Google Scholar]
- Chiu HL, Chan PT, Kao CC, Chu H, Chang PC, Hsiao SS, … Chou KR (2018). Effectiveness of executive function training on mental set shifting, working memory and inhibition in healthy older adults: A double-blind randomized controlled trials. Journal of Advanced Nursing, 74(5), 1099–1113. 10.1111/jan.13519 [DOI] [PubMed] [Google Scholar]
- Cochran WG (1954). The combination of estimates from different experiments. Biometrics, 10(1), 101–129. 10.2307/3001666 [DOI] [Google Scholar]
- Coors A, Breteler MMB, & Ettinger U (2022). Processing speed, but not working memory or global cognition, is associated with pupil diameter during fixation. Psychophysiology, 59(11), e14089. 10.1111/psyp.14089 [DOI] [PubMed] [Google Scholar]
- Corbett BA, Constantine LJ, Hendren R, Rocke D, & Ozonoff S (2009). Examining executive functioning in children with autism spectrum disorder, attention deficit hyperactivity disorder and typical development. Psychiatry Research, 166(2–3), 210–222. 10.1016/j.psychres.2008.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbetta M, & Shulman GL (2002). Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews Neuroscience, 3(3), 201–215. 10.1038/nrn755 [DOI] [PubMed] [Google Scholar]
- Crane RS, & Hecht FM (2018a). Intervention integrity in mindfulness-based research. Mindfulness (N Y), 9(5), 1370–1380. 10.1007/s12671-018-0886-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane RS, & Hecht FM (2018b). Intervention integrity in mindfulness-based research. Mindfulness, 9(5), 1370–1380. 10.1007/s12671-018-0886-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD (2017). Mindfulness interventions. Annual Review of Psychology, 68(1), 491–516. 10.1146/annurev-psych-042716-051139 [DOI] [PubMed] [Google Scholar]
- Cubillo A, Hermes H, Berger E, Winkel K, Schunk D, Fehr E, & Hare TA (2023). Intra-individual variability in task performance after cognitive training is associated with long-term outcomes in children. Developmental Science, 26(1), e13252. 10.1111/desc.13252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Andersson G, & van Oppen P (2008). Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology, 76(6), 909–922. 10.1037/a0013075 [DOI] [PubMed] [Google Scholar]
- Daglas-Georgiou R, Bryce S, Smith G, Kaur M, Cheng N, De Rozario M, … Allott K. (2022). Treatments for objective and subjective cognitive functioning in young people with depression: Systematic review of current evidence. Early Intervention in Psychiatry, 16(10), 1057–1074. 10.1111/eip.13248 [DOI] [PubMed] [Google Scholar]
- Dai M, Li Y, Gan S, & Du F (2019). The reliability of estimating visual working memory capacity. Scientific Reports, 9(1), 1155. 10.1038/s41598-019-39044-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, & Ober BA (2017). California Verbal Learning Test-3 (3rd ed.). The Psychological Corporation. [Google Scholar]
- Derryberry D, & Reed MA (2002). Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology, 111(2), 225–236. 10.1037/0021-843X.111.2.225 [DOI] [PubMed] [Google Scholar]
- Dickinson J, Friary P, & McCann CM (2016). The influence of mindfulness meditation on communication and anxiety: A case study of a person with aphasia. Aphasiology, 31(9), 1044–1058. 10.1080/02687038.2016.1234582 [DOI] [Google Scholar]
- Dockree PM, Bellgrove MA, O’Keeffe FM, Moloney P, Aimola L, Carton S, & Robertson IH (2006). Sustained attention in traumatic brain injury (TBI) and healthy controls: Enhanced sensitivity with dual-task load. Experimental Brain Research, 168(1), 218–229. 10.1007/s00221-005-0079-x [DOI] [PubMed] [Google Scholar]
- Dunn TJ, & Dimolareva M (2022). The effect of mindfulness-based interventions on immunity-related biomarkers: A comprehensive meta-analysis of randomised controlled trials. Clinical Psychology Review, 92, 102124. 10.1016/j.cpr.2022.102124 [DOI] [PubMed] [Google Scholar]
- Dunning DL, Griffiths K, Kuyken W, Crane C, Foulkes L, Parker J, & Dalgleish T (2019). Research review: The effects of mindfulness-based interventions on cognition and mental health in children and adolescents – a meta-analysis of randomized controlled trials. Journal of Child Psychology and Psychiatry, 60(3), 244–258. 10.1111/jcpp.12980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elices M, Perez-Sola V, Perez-Aranda A, Colom F, Polo M, Martin-Lopez LM, & Garriz M (2022). The effectiveness of mindfulness-based cognitive therapy in primary care and the role of depression severity and treatment attendance. Mindfulness, 13(2), 362–372. 10.1007/s12671-021-01794-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esterman M, & Rothlein D (2019). Models of sustained attention. Current Opinion in Psychology, 29, 174–180. 10.1016/j.copsyc.2019.03.005 [DOI] [PubMed] [Google Scholar]
- Fan J, McCandliss BD, Sommer T, Raz A, & Posner MI (2002). Testing the efficiency and independence of attentional networks. Journal of Cognitive Neuroscience, 14(3), 340–347. 10.1162/089892902317361886 [DOI] [PubMed] [Google Scholar]
- Felver JC, Tipsord JM, Morris MJ, Racer KH, & Dishion TJ (2017). The effects of mindfulness-based intervention on children’s attention regulation. Journal of Attention Disorders, 21(10), 872–881. 10.1177/1087054714548032 [DOI] [PubMed] [Google Scholar]
- Fernando AT, Skinner K, & Consedine NS (2016). Increasing compassion in medical decision-making: Can a brief mindfulness intervention help? Mindfulness, 8(2), 276–285. 10.1007/s12671-016-0598-5 [DOI] [Google Scholar]
- Fetterman AK, & Robinson MD (2011). Routine cognitive errors: A trait-like predictor of individual differences in anxiety and distress. Cognition and Emotion, 25(2), 244–264. 10.1080/02699931.2010.486941 [DOI] [PubMed] [Google Scholar]
- Fisher GG, Chacon M, & Chaffee DS (2019). Theories of cognitive aging and work. In Work Across the Lifespan (pp. 17–45). 10.1016/b978-0-12-812756-8.00002-5 [DOI] [Google Scholar]
- Fisher Z, Tipton E, & Zhipeng H (2017). robumeta: Robust variance meta-regression [Google Scholar]
- Flook L, Goldberg SB, Pinger L, & Davidson RJ (2015). Promoting prosocial behavior and self-regulatory skills in preschool children through a mindfulness-based kindness curriculum. Developmental Psychology, 51(1), 44–51. 10.1037/a0038256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French K, Golijani-Moghaddam N, & Schröder T (2017). What is the evidence for the efficacy of self-help acceptance and commitment therapy? A systematic review and meta-analysis. Journal of Contextual Behavioral Science, 6(4), 360–374. 10.1016/j.jcbs.2017.08.002 [DOI] [Google Scholar]
- Fulambarkar N, Seo B, Testerman A, Rees M, Bausback K, & Bunge E (2023). Review: Meta-analysis on mindfulness-based interventions for adolescents’ stress, depression, and anxiety in school settings: a cautionary tale. Child and Adolescent Mental Health, 28(2), 307–317. 10.1111/camh.12572 [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Suganuma A, Ostinelli EG, Andersson G, Beevers CG, Shumake J, … Cuijpers P. (2021). Dismantling, optimising, and personalising internet cognitive behavioural therapy for depression: A systematic review and component network meta-analysis using individual participant data. The Lancet Psychiatry, 8(6), 500–511. 10.1016/s2215-0366(21)00077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamer M, Lemon J, Fellows I, & Singh P (2007). irr: Various coefficients of interrater reliability and agreement. R package http://www.r-project.org [Google Scholar]
- Garland EL, Farb NA, Goldin P, & Fredrickson BL (2015). Mindfulness broadens awareness and builds eudaimonic meaning: A process model of mindful positive emotion regulation. Psychological Inquiry, 26(4), 293–314. 10.1080/1047840X.2015.1064294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman A, & Stern H (2006). The difference between “significant” and “not significant” is not itself statistically significant. The American Statistician, 60(4), 328–331. [DOI] [Google Scholar]
- Goldberg SB, Riordan KM, Sun S, & Davidson RJ (2021). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science, 17(1), 108–130. 10.1177/1745691620968771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good DJ, Lyddy CJ, Glomb TM, Bono JE, Brown KW, Duffy MK, … Lazar SW. (2015). Contemplating mindfulness at work. Journal of Management, 42(1), 114–142. 10.1177/0149206315617003 [DOI] [Google Scholar]
- Grant DA, & Berg EA (1948). A behavioral analysis of degree of reinforcement and ease of shifting to new responses in a Weigl-type card-sorting problem. Journal of Experimental Psychology: General, 38(4), 404–411. 10.1037/h0059831 [DOI] [PubMed] [Google Scholar]
- Green CS, & Bavelier D (2003). Action video game modifies visual selective attention. Nature, 423(6939), 534–537. 10.1038/nature01647 [DOI] [PubMed] [Google Scholar]
- Grossman P, Tiefenthaler-Gilmer U, Raysz A, & Kesper U (2007). Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and Psychosomatics, 76(4), 226–233. 10.1159/000101501 [DOI] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, & Cavanagh K (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. 10.1016/j.cpr.2015.01.006 [DOI] [PubMed] [Google Scholar]
- Haigh EAP, Moore MT, Kashdan TB, & Fresco DM (2010). Examination of the factor structure and concurrent validity of the Langer mindfulness/mindlessness scale. Assessment, 18(1), 11–26. 10.1177/1073191110386342 [DOI] [PubMed] [Google Scholar]
- Hallgren KA (2012). Computing inter-rater reliability for observational data: an overview and tutorial. Tutorials in quantitative methods for psychology, 8(1), 23–34. https://www.unboundmedicine.com/medline/citation/22833776/Computing_Inter_Rater_Reliability_for_Observational_Data:_An_Overview_and_Tutorial_https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/22833776/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion LS, Tolin DF, & Diefenbach GJ (2019). Enhanced cognitive control over task-irrelevant emotional distractors in generalized anxiety disorder versus obsessive-compulsive disorder. Journal of Anxiety Disorders, 64, 71–78. 10.1016/j.janxdis.2019.02.004 [DOI] [PubMed] [Google Scholar]
- Han A (2021). Effects of mindfulness-and acceptance-based interventions on quality of life, coping, cognition, and mindfulness of people with multiple sclerosis: A systematic review and meta-analysis. Psychology, Health & Medicine, 1–18. 10.1080/13548506.2021.1894345 [DOI] [PubMed] [Google Scholar]
- Harms C, & Lakens D (2018). Making ‘null effects’ informative: statistical techniques and inferential frameworks. Journal of Clinical and Translational Research, 3(Suppl 2), 382–393. 10.18053/jctres.03.2017S2.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazlett-Stevens H, Singer J, & Chong A (2019). Mindfulness-based stress reduction and mindfulness-based cognitive therapy with older adults: A qualitative review of randomized controlled outcome research. Clinical Gerontologist, 42(4), 347–358. 10.1080/07317115.2018.1518282 [DOI] [PubMed] [Google Scholar]
- Heck NC, Mirabito LA, LeMaire K, Livingston NA, & Flentje A (2017). Omitted data in randomized controlled trials for anxiety and depression: A systematic review of the inclusion of sexual orientation and gender identity. Journal of Consulting and Clinical Psychology, 85(1), 72–76. 10.1037/ccp0000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedge C, Powell G, & Sumner P (2018). The reliability paradox: Why robust cognitive tasks do not produce reliable individual differences. Behavior Research Methods, 50(3), 1166–1186. 10.3758/s13428-017-0935-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JD, & Crawford JR (2004). A meta-analytic review of verbal fluency performance following focal cortical lesions. Neuropsychology, 18(2), 284–295. 10.1037/0894-4105.18.2.284 [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. British Medical Journal, 327(7414), 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, … Sterne JAC. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 343, d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, & Green S (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Google Scholar]
- Hodges LJ, Humphris GM, & Macfarlane G (2005). A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Social Science & Medicine, 60(1), 1–12. 10.1016/j.socscimed.2004.04.018 [DOI] [PubMed] [Google Scholar]
- Hoge EA, Acabchuk RL, Kimmel H, Moitra E, Britton WB, Dumais T, … Fulwiler C. (2021). Emotion-related constructs engaged by mindfulness-based interventions: A systematic review and meta-analysis. Mindfulness, 12(5), 1041–1062. 10.1007/s12671-020-01561-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, & Ott U (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559. 10.1177/1745691611419671 [DOI] [PubMed] [Google Scholar]
- Im S, Stavas J, Lee J, Mir Z, Hazlett-Stevens H, & Caplovitz G (2021). Does mindfulness-based intervention improve cognitive function?: A meta-analysis of controlled studies. Clinical Psychology Review, 84, 101972. 10.1016/j.cpr.2021.101972 [DOI] [PubMed] [Google Scholar]
- Isbel B, & Mahar D (2015). Cognitive mechanisms of mindfulness: A test of current models. Consciousness and Cognition, 38, 50–59. 10.1016/j.concog.2015.10.005 [DOI] [PubMed] [Google Scholar]
- Jang JH, Kim J-H, Yun J-Y, Choi S-H, An SC, & Kang D-H (2018). Differences in functional connectivity of the insula between brain wave vibration in meditators and non-meditators. Mindfulness, 9(6), 1857–1866. 10.1007/s12671-018-0928-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewsbury PA, Bowden SC, & Strauss ME (2016). Integrating the switching, inhibition, and updating model of executive function with the Cattell-Horn-Carroll model. Journal of Experimental Psychology: General, 145(2), 220–245. 10.1037/xge0000119 [DOI] [PubMed] [Google Scholar]
- Jha AP, Denkova E, Zanesco AP, Witkin JE, Rooks J, & Rogers SL (2019). Does mindfulness training help working memory ‘work’ better? Current Opinion in Psychology, 28, 273–278. 10.1016/j.copsyc.2019.02.012 [DOI] [PubMed] [Google Scholar]
- Jha AP, Krompinger J, & Baime MJ (2007). Mindfulness training modifies subsystems of attention. Cognitive, Affective, & Behavioral Neuroscience, 7(2), 109–119. 10.3758/cabn.7.2.109 [DOI] [PubMed] [Google Scholar]
- Johnsen TJ, & Friborg O (2015). The effects of cognitive behavioral therapy as an anti-depressive treatment is falling: A meta-analysis. Psychological Bulletin, 141(4), 747–768. 10.1037/bul0000015 [DOI] [PubMed] [Google Scholar]
- Judah MR, Grant DM, Mills AC, & Lechner WV (2014). Factor structure and validation of the Attentional Control Scale. Cognition and Emotion, 28(3), 433–451. 10.1080/02699931.2013.835254 [DOI] [PubMed] [Google Scholar]
- Kane MJ, Conway ARA, Miura TK, & Colflesh GJH (2007). Working memory, attention control, and the N-back task: a question of construct validity. Journal of Experimental Psychology: Learning, Memory, and Cognition, 33(3), 615–622. 10.1037/0278-7393.33.3.615 [DOI] [PubMed] [Google Scholar]
- Katz D, & Toner B (2013). A systematic review of gender differences in the effectiveness of mindfulness-based treatments for substance use disorders. Mindfulness, 4(4), 318–331. 10.1007/s12671-012-0132-3 [DOI] [Google Scholar]
- Kaunhoven RJ, & Dorjee D (2017). How does mindfulness modulate self-regulation in pre-adolescent children? An integrative neurocognitive review. Neuroscience and Biobehavioral Reviews, 74(Pt A), 163–184. 10.1016/j.neubiorev.2017.01.007 [DOI] [PubMed] [Google Scholar]
- Kent DM, Paulus JK, van Klaveren D, D’Agostino R, Goodman S, Hayward R, … Steyerberg EW. (2020). The predictive approaches to treatment effect heterogeneity (path) statement. Annals of Internal Medicine, 172(1), 35–45. 10.7326/M18-3667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk U, Gu X, Sharp C, Hula A, Fonagy P, & Montague PR (2016). Mindfulness training increases cooperative decision making in economic exchanges: Evidence from fMRI. Neuroimage, 138, 274–283. 10.1016/j.neuroimage.2016.05.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer JH, Mungas D, Possin KL, Rankin KP, Boxer AL, Rosen HJ, … Widmeyer M. (2014). NIH EXAMINER: Conceptualization and development of an executive function battery. Journal of the International Neuropsychological Society, 20(1), 11–19. 10.1017/S1355617713001094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze EJ, Voegtle M, Miller JP, Ances BM, Balota DA, Barch D, … Wetherell JL. (2022). Effects of mindfulness training and exercise on cognitive function in older adults: A randomized clinical trial. JAMA, 328(22), 2218–2229. 10.1001/jama.2022.21680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levi U, & Rosenstreich E (2019). Mindfulness and memory: A review of findings and a potential model. Journal of Cognitive Enhancement, 3(3), 302–314. 10.1007/s41465-018-0099-7 [DOI] [Google Scholar]
- Lezak M, Howieson D, Bigler E, & Tranel D (2012). Neuropsychological assessment Oxford University Press. [Google Scholar]
- Lin Y, Fisher ME, & Moser JS (2019). Clarifying the relationship between mindfulness and executive attention: A combined behavioral and neurophysiological study. Social Cognitive and Affective Neuroscience, 14(2), 205–215. 10.1093/scan/nsy113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2017). Mechanisms of mindfulness training: Monitor and acceptance theory (MAT). Clinical Psychology Review, 51, 48–59. 10.1016/j.cpr.2016.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Applied social research methods series: Vol. 49. Practical meta-analysis Sage. [Google Scholar]
- Lodha S, & Gupta R (2022). Mindfulness, attentional networks, and executive functioning: A review of interventions and long-term meditation practice. Journal of Cognitive Enhancement, 6(4), 531–548. 10.1007/s41465-022-00254-7 [DOI] [Google Scholar]
- London M, Sessa VI, & Shelley LA (2023). Developing self-awareness: Learning processes for self- and interpersonal growth. Annual Review of Organizational Psychology and Organizational Behavior, 10(1), 261–288. 10.1146/annurev-orgpsych-120920-044531 [DOI] [Google Scholar]
- Lueke A, & Lueke N (2019). Mindfulness improves verbal learning and memory through enhanced encoding. Memory and Cognition, 47(8), 1531–1545. 10.3758/s13421-019-00947-z [DOI] [PubMed] [Google Scholar]
- Lutz A, Jha AP, Dunne JD, & Saron CD (2015). Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. American Psychologist, 70(7), 632–658. 10.1037/a0039585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L, Zhang Y, & Cui Z (2019). Mindfulness-based interventions for prevention of depressive symptoms in university students: a meta-analytic review. Mindfulness, 10(11), 2209–2224. 10.1007/s12671-019-01192-w [DOI] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, & Munafo MR (2011). Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology, 216(3), 305–321. 10.1007/s00213-011-2229-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean KA, Ferrer E, Aichele SR, Bridwell DA, Zanesco AP, Jacobs TL, … Saron CD. (2010). Intensive meditation training improves perceptual discrimination and sustained attention. Psychological Science, 21(6), 829–839. 10.1177/0956797610371339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malinowski P, & Shalamanova L (2017). Meditation and cognitive ageing: The role of mindfulness meditation in building cognitive reserve. Journal of Cognitive Enhancement, 1(2), 96–106. 10.1007/s41465-017-0022-7 [DOI] [Google Scholar]
- Mars TS, & Abbey H (2010). Mindfulness meditation practise as a healthcare intervention: A systematic review. International Journal of Osteopathic Medicine, 13(2), 56–66. 10.1016/j.ijosm.2009.07.005 [DOI] [Google Scholar]
- McCoy CE (2017). Understanding the intention-to-treat principle in randomized controlled trials. Western Journal of Emergency Medicine, 18(6), 1075–1078. 10.5811/westjem.2017.8.35985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mediavilla R, Muñoz-Sanjose A, Rodriguez-Vega B, Lahera G, Palao A, Bayon C, … Bravo-Ortiz MF. (2021). People with psychosis improve affective social cognition and self-care after a mindfulness-based social cognition training program (SocialMIND). Psychiatric Rehabilitation Journal, 44(4), 391–395. 10.1037/prj0000466 [DOI] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, & Wager TD (2000). The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology, 41(1), 49–100. 10.1006/cogp.1999.0734 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & The PG (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Cuijpers P, & Lehman K (2011). Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. Journal of Medical Internet Research, 13(1), e30. 10.2196/jmir.1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moncher FJ, & Prinz RJ (1991). Treatment fidelity in outcome studies. Clinical Psychology Review, 11(3), 247–266. 10.1016/0272-7358(91)90103-2 [DOI] [Google Scholar]
- Morris SB, & DeShon RP (2002). Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods, 7(1), 105–125. 10.1037/1082-989X.7.1.105 [DOI] [PubMed] [Google Scholar]
- Mrazek AJ, Mrazek MD, Cherolini CM, Cloughesy JN, Cynman DJ, Gougis LJ, … Schooler JW. (2019). The future of mindfulness training is digital, and the future is now. Current Opinion in Psychology, 28, 81–86. 10.1016/j.copsyc.2018.11.012 [DOI] [PubMed] [Google Scholar]
- Mrazek MD, Franklin MS, Phillips DT, Baird B, & Schooler JW (2013). Mindfulness training improves working memory capacity and GRE performance while reducing mind wandering. Psychological Science, 24(5), 776–781. 10.1177/0956797612459659 [DOI] [PubMed] [Google Scholar]
- Muller C, Otto B, Sawitzki V, Kanagalingam P, Scherer JS, & Lindberg S (2021). Short breaks at school: effects of a physical activity and a mindfulness intervention on children’s attention, reading comprehension, and self-esteem. Trends in Neuroscience and Education, 25, 100160. 10.1016/j.tine.2021.100160 [DOI] [PubMed] [Google Scholar]
- Müller C, Otto B, Sawitzki V, Kanagalingam P, Scherer JS, & Lindberg S (2021). Short breaks at school: Effects of a physical activity and a mindfulness intervention on children’s attention, reading comprehension, and self-esteem. Trends in Neuroscience and Education, 25, 100160. 10.1016/j.tine.2021.100160 [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, … Chertkow H. (2005). The Montreal cognitive assessment (MoCA): a brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Noone C, & Hogan MJ (2018). A randomised active-controlled trial to examine the effects of an online mindfulness intervention on executive control, critical thinking and key thinking dispositions in a university student sample. BMC Psychology, 6(1), 13. 10.1186/s40359-018-0226-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oman D (2023). Mindfulness for global public health: Critical analysis and agenda. Mindfulness 10.1007/s12671-023-02089-5 [DOI] [Google Scholar]
- Owen AM, McMillan KM, Laird AR, & Bullmore E (2005). N-back working memory paradigm: A meta-analysis of normative functional neuroimaging studies. Human Brain Mapping, 25(1), 46–59. 10.1002/hbm.20131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Fuentes M. d. C., Molero Jurado M. d. M., Mercader Rubio I, Soriano Sánchez JG, & Gázquez Linares JJ (2020). Mindfulness for preventing psychosocial risks in the workplace: A systematic review and meta-analysis. Applied Sciences, 10(5). 10.3390/app10051851 [DOI] [Google Scholar]
- Petersen SE, & Posner MI (2012). The attention system of the human brain: 20 years after. Annual Review of Neuroscience, 35(1), 73–89. 10.1146/annurev-neuro-062111-150525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner MI, & Rothbart MK (2007). Research on attention networks as a model for the integration of psychological science. Annual Review of Psychology, 58(1), 1–23. 10.1146/annurev.psych.58.110405.085516 [DOI] [PubMed] [Google Scholar]
- Posner MI, Rothbart MK, & Tang Y-Y (2015). Enhancing attention through training. Current Opinion in Behavioral Sciences, 4, 1–5. 10.1016/j.cobeha.2014.12.008 [DOI] [Google Scholar]
- Prakash RS, Fountain-Zaragoza S, Kramer AF, Samimy S, & Wegman J (2020). Mindfulness and attention: Current state-of-affairs and future considerations. Journal of Cognitive Enhancement. 10.1007/s41465-019-00144-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffone A, Marzetti L, Del Gratta C, Perrucci MG, Romani GL, & Pizzella V (2019). Chapter 9 - Toward a brain theory of meditation. In Srinivasan N (Ed.), Progress in Brain Research (Vol. 244, pp. 207–232). Elsevier. 10.1016/bs.pbr.2018.10.028 [DOI] [PubMed] [Google Scholar]
- Raffone A, & Srinivasan N (2017). Mindfulness and cognitive functions: Toward a unifying neurocognitive framework. Mindfulness, 8(1), 1–9. 10.1007/s12671-016-0654-1 [DOI] [Google Scholar]
- Raucher-Chéné D, Achim AM, Kaladjian A, & Besche-Richard C (2017). Verbal fluency in bipolar disorders: A systematic review and meta-analysis. Journal of Affective Disorders, 207, 359–366. 10.1016/j.jad.2016.09.039 [DOI] [PubMed] [Google Scholar]
- Ristic J, Wright A, & Kingstone A (2007). Attentional control and reflexive orienting to gaze and arrow cues. Psychonomic Bulletin & Review, 14(5), 964–969. 10.3758/BF03194129 [DOI] [PubMed] [Google Scholar]
- Robertson IH, Manly T, Andrade J, Baddeley BT, & Yiend J (1997). Òops!’: Performance correlates of everyday attentional failures in traumatic brain injured and normal subjects. Neuropsychologia, 35(6), 747–758. 10.1016/S0028-3932(97)00015-8 [DOI] [PubMed] [Google Scholar]
- Rosenthal R (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Sala M, Rochefort C, Lui PP, & Baldwin AS (2020). Trait mindfulness and health behaviours: A meta-analysis. Health Psychology Review, 14(3), 345–393. 10.1080/17437199.2019.1650290 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lara E, Lozano-Ruiz A, Perez-Garcia M, & Caracuel A (2021). Efficacy of mindfulness-based interventions in cognitive function in the elderly people: a systematic review and meta-analysis. Aging and Mental Health, 1–11. 10.1080/13607863.2021.1976724 [DOI] [PubMed] [Google Scholar]
- Schueller SM, Tomasino KN, & Mohr DC (2017). Integrating human support into behavioral intervention technologies: The efficiency model of support. Clinical Psychology: Science and Practice, 24(1), 27–45. 10.1111/cpsp.12173 [DOI] [Google Scholar]
- Schumer MC, Lindsay EK, & Creswell JD (2018). Brief mindfulness training for negative affectivity: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 86(7), 569–583. 10.1037/ccp0000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, … Greicius MD. (2007). Dissociable intrinsic connectivity networks for salience processing and executive control. The Journal of Neuroscience, 27(9), 2349. 10.1523/jneurosci.5587-06.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servan-Schreiber D, Cohen JD, & Steingard S (1996). Schizophrenic deficits in the processing of context: A test of a theoretical model. Archives of General Psychiatry, 53(12), 1105–1112. 10.1001/archpsyc.1996.01830120037008 [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Jazaieri H, & Goldin PR (2012). Mindfulness-based stress reduction effects on moral reasoning and decision making. The Journal of Positive Psychology, 7(6), 504–515. 10.1080/17439760.2012.723732 [DOI] [Google Scholar]
- Shen H, Zhang L, Li Y, Zheng D, Du L, Xu F, … Cui D. (2023). Mindfulness-based intervention improves residual negative symptoms and cognitive impairment in schizophrenia: a randomized controlled follow-up study. Psychological Medicine, 53(4), 1390–1399. 10.1017/S0033291721002944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields RH, Kaat A, Sansone SM, Michalak C, Coleman J, Thompson T, … Hessl D. (2023). Sensitivity of the NIH toolbox to detect cognitive change in individuals with intellectual and developmental disability. Neurology, 100(8), e778–e789. 10.1212/WNL.0000000000201528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, & Fleiss JL (1979). Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428. 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- Smith A (1982). Symbol digit modalities test Western Psychological Services. [Google Scholar]
- Sood A, & Jones DT (2013). On mind wandering, attention, brain networks, and meditation. Explore, 9(3), 136–141. 10.1016/j.explore.2013.02.005 [DOI] [PubMed] [Google Scholar]
- Sorensen L, Osnes B, Visted E, Svendsen JL, Adolfsdottir S, Binder PE, & Schanche E (2018). Dispositional mindfulness and attentional control: The specific association between the mindfulness facets of non-judgment and describing with flexibility of early operating orienting in conflict detection. Frontiers in Psychology, 9, 2359. 10.3389/fpsyg.2018.02359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijkerman MPJ, Pots WTM, & Bohlmeijer ET (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 45, 102–114. 10.1016/j.cpr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Hoogerwerf E, van Giezen A, & Greeven A (2022). Mindfulness-based cognitive group therapy for treatment-refractory anxiety disorder: A pragmatic randomized controlled trial. Journal of Anxiety Disorders, 90, 102599. 10.1016/j.janxdis.2022.102599 [DOI] [PubMed] [Google Scholar]
- Stark MA, & Cimprich B (2003). Promoting attentional health: importance to women’s lives. Health Care for Women International, 24(2), 93–102. 10.1080/07399330390170079 [DOI] [PubMed] [Google Scholar]
- Stein E, & Witkiewitz K (2020). Dismantling mindfulness-based programs: A systematic review to identify active components of treatment. Mindfulness, 11(11), 2470–2485. 10.1007/s12671-020-01444-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroop JR (1935). Studies of interference in serial verbal reactions. Journal of Experimental Psychology, 18(6), 643–662. 10.1037/h0054651 [DOI] [Google Scholar]
- Sumantry D, & Stewart KE (2021). Meditation, mindfulness, and attention: A meta-analysis. Mindfulness 10.1007/s12671-021-01593-w [DOI] [Google Scholar]
- Sun S, Goldberg SB, Loucks EB, & Brewer JA (2022). Mindfulness-based interventions among people of color: A systematic review and meta-analysis. Psychotherapy Research, 32(3), 277–290. 10.1080/10503307.2021.1937369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y-Y, Hölzel BK, & Posner MI (2015). The neuroscience of mindfulness meditation. Nature Reviews Neuroscience, 16(4), 213–225. 10.1038/nrn3916 [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Tipton E, & Polanin JR (2016). Handling complex meta-analytic data structures using robust variance estimates: A tutorial in R. Journal of Developmental and Life-Course Criminology, 2(1), 85–112. 10.1007/s40865-016-0026-5 [DOI] [Google Scholar]
- Teper R, & Inzlicht M (2013). Meditation, mindfulness and executive control: The importance of emotional acceptance and brain-based performance monitoring. Social Cognitive and Affective Neuroscience, 8(1), 85–92. 10.1093/scan/nss045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teper R, Segal ZV, & Inzlicht M (2013). Inside the mindful mind: How mindfulness enhances emotion regulation through improvements in executive control. Current Directions in Psychological Science, 22(6), 449–454. 10.1177/0963721413495869 [DOI] [Google Scholar]
- Tulving E (2002). Episodic memory: From mind to brain. Annual Review of Psychology, 53, 1–25. 10.1146/annurev.psych.53.100901.135114 [DOI] [PubMed] [Google Scholar]
- Uusberg H, Uusberg A, Talpsep T, & Paaver M (2016). Mechanisms of mindfulness: The dynamics of affective adaptation during open monitoring. Biological Psychology, 118, 94–106. 10.1016/j.biopsycho.2016.05.004 [DOI] [PubMed] [Google Scholar]
- Vago D, & Silbersweig DA (2012). Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in Human Neuroscience, 6(296), 296. 10.3389/fnhum.2012.00296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vago DR, Gupta RS, & Lazar SW (2019). Measuring cognitive outcomes in mindfulness-based intervention research: a reflection on confounding factors and methodological limitations. Current Opinion in Psychology, 28, 143–150. 10.1016/j.copsyc.2018.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Assen MALM, van Aert RCM, & Wicherts JM (2015). Meta-analysis using effect size distributions of only statistically significant studies. Psychological Methods, 20(3), 293–309. 10.1037/met0000025 [DOI] [PubMed] [Google Scholar]
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, … Meyer DE (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Elst W, van Boxtel MP, van Breukelen GJ, & Jolles J (2006). The Letter Digit Substitution Test: normative data for 1,858 healthy participants aged 24–81 from the Maastricht Aging Study (MAAS): Influence of age, education, and sex. Journal of Clinical and Experimental Neuropsychology, 28(6), 998–1009. 10.1080/13803390591004428 [DOI] [PubMed] [Google Scholar]
- Verhaeghen P (2021). Mindfulness as attention training: Meta-analyses on the links between attention performance and mindfulness interventions, long-term meditation practice, and trait mindfulness. Mindfulness, 12(3), 564–581. 10.1007/s12671-020-01532-1 [DOI] [Google Scholar]
- Verhagen AP, de Vet HCW, de Bie RA, Kessels AGH, Boers M, Bouter LM, & Knipschild PG (1998). The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology, 51(12), 1235–1241. 10.1016/S0895-4356(98)00131-0 [DOI] [PubMed] [Google Scholar]
- Viechtbauer W (2010). metafor: Meta-Analysis Package for R. R package version, 2010, 1–0. [Google Scholar]
- Viechtbauer W, & Cheung MW-L (2010). Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods, 1(2), 112–125. 10.1002/jrsm.11 [DOI] [PubMed] [Google Scholar]
- Vilgis V, Silk TJ, & Vance A (2015). Executive function and attention in children and adolescents with depressive disorders: A systematic review. European Child and Adolescent Psychiatry, 24(4), 365–384. 10.1007/s00787-015-0675-7 [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Hershey T, Hickman S, Tate SR, Dixon D, Bower ES, & Lenze EJ (2017). Mindfulness-based stress reduction for older adults with stress disorders and neurocognitive difficulties: A randomized controlled trial. Journal of Clinical Psychiatry, 78(7), e734–e743. 10.4088/JCP.16m10947 [DOI] [PubMed] [Google Scholar]
- Whitfield T, Barnhofer T, Acabchuk R, Cohen A, Lee M, Schlosser M, … Marchant NL. (2022). The effect of mindfulness-based programs on cognitive function in adults: A systematic review and meta-analysis. Neuropsychology Review, 32(3), 677–702. 10.1007/s11065-021-09519-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H (2016). ggplot2: Elegant Graphics for Data Analysis Springer-Verlag. https://ggplot2.tidyverse.org [Google Scholar]
- Wolkin JR (2015). Cultivating multiple aspects of attention through mindfulness meditation accounts for psychological well-being through decreased rumination. Psychology Research and Behavior Management, 8, 171–180. 10.2147/PRBM.S31458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakobi O, Smilek D, & Danckert J (2021). The effects of mindfulness meditation on attention, executive control and working memory in healthy adults: A meta-analysis of randomized controlled trials. Cognitive Therapy and Research 10.1007/s10608-020-10177-2 [DOI] [Google Scholar]
- Zainal NH, & Newman MG (2022). Inflammation mediates depression and generalized anxiety symptoms predicting executive function impairment after 18 years. Journal of Affective Disorders, 296, 465–475. 10.1016/j.jad.2021.08.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainal NH, & Newman MG (2023). A randomized controlled trial of a 14-day mindfulness ecological momentary intervention (MEMI) for generalized anxiety disorder. European Psychiatry, 66(1), e12. 10.1192/j.eurpsy.2023.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


