Abstract
Background
To systematically review the literature to evaluate the outcomes following an open Latarjet (OL) procedure at a minimum 15-year follow-up.
Methods
Two independent reviewers performed a literature search using Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines using 3 databases. Only studies reporting outcomes of OL procedure with a minimum of 15 years of follow-up were included.
Results
Nine studies composed of 326 shoulders (78.2% males) in 313 patients were included (average age 26.9 ± 3.2 years (15–58)), with a mean follow-up of 271.9 ± 69.2 months (180–420) At a minimum 15-year follow-up, 93.5% (286 of 306) patients reported being satisfied with their OL procedure, whilst 86.8% (177 of 204) reported good/excellent outcomes at final follow-up. All nine of the included studies reported an overall rate of recurrent instability was 7.7%, with re-dislocations and subluxation at 3.4% and 5.8%, respectively. The rate of surgical revision was 5.15%; 3.5% of cases were revised for recurrent instability. Instability arthropathy was reported across all included studies as 41.0%.
Conclusion
The OL procedure results in satisfactory clinical outcomes, low rates of recurrent instability and surgical revision at a minimum 15-year follow-up. Although high levels of radiological instability arthropathy and residual pain are found over the same period, these appear stable from a minimum of 10-year follow-up data.
Level of Evidence
IV; a systematic review of all levels of evidence
Keywords: Long-term, 15 years, systematic review, latarjet, anterior shoulder instability
Introduction
Anterior shoulder instability is a common condition, affecting approximately 1% to 2% of the general population and up to 15% of collision athletes.1–4 Recurrent instability is not without morbidity, with each dislocation episode resulting in increasing glenoid bone loss.5,6 Although a myriad of management options exist, the open Latarjet (OL) procedure has emerged as the procedure of choice for many, with recent consensus guidelines recommending its use in cases of recurrent shoulder instability in patients with >15% glenoid bone loss.7–11
The OL procedure has previously been reported to result in excellent clinical outcomes in the short term, with high rates of return to play (RTP) and low recurrence rates at medium-term follow-up,10,12–17 with the procedure being increasingly performed using an arthroscopic technique.18–21 Furthermore, a systematic review of 845 shoulders by Hurley et al. 22 reported excellent clinical outcomes at a 10-year follow-up post-OL procedure. This study found rates of radiological instability arthropathy, recurrent instability and surgical revisions to be 40%, 8% and 3%, respectively, at 10-year follow-up.
As the literature continues to expand on this topic, further studies of outcomes are increasingly reported at ever-longer follow-up, with much literature focusing on patient outcomes after 10-year follow-up. Therefore, the purpose of this study was to systematically review the literature to evaluate the outcomes following the OL procedure at a minimum 15-year follow-up. We hypothesised that when compared to the 10-year outcomes reported by Hurley et al., 22 the OL procedure would result in (1) similarly satisfactory clinical outcomes, (2) higher radiological rates of instability arthropathy, (3) stable rates of recurrence, and (4) stable rates of surgical revisions at a minimum 15-year follow-up post-operatively.
Materials and methods
Search strategy
Whilst referencing the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines, two independent reviewers performed a literature search. In April 2022, the Pubmed, Embase and Scopus databases were used for the search using the following search terms: ((anterior shoulder instability or shoulder instability) AND (Latarjet OR open latarjet OR arthroscopic latarjet OR latarjet procedure OR bristow OR open bristow OR bristow procedure OR bristow-latarjet OR coracoid transfer) AND (long term OR long-term OR minimum 15 year OR 15 year outcomes)). It was pre-determined by all investigators that no time limit would be applied to the search. After duplicated studies were manually removed, both reviewers manually screened the titles and abstracts of all studies from the initial search whilst applying our exclusion criteria, with the senior author acting as an arbitrator in the instance of discrepancies in opinion between the reviewers. Thereafter, a pre-determined inclusion criterion was utilized by both independent reviewers for the evaluation of the full texts of all potentially eligible studies by both reviewers.
Eligibility criteria
Prior to the commencement of the study, all authors agreed on the pre-determined inclusion, exclusion criteria and data collection sheet for this study. The inclusion criteria for this study included the following parameters: (1) any study reporting outcomes of the OL procedure, (2) outcomes reported at a minimum 15-year follow-up, (3) published in English, and (4) published in a peer-reviewed journal. The exclusion criteria included: (1) studies focusing on revision procedures only, (2) abstract-only studies, (3) biomechanical studies, (3) cadaveric studies, and (5) case reports.
Data extraction
Independent evaluation of each of the published manuscripts of the included studies was carried out by the two reviewers independently with aim of gathering all relevant data. Study characteristics and patient demographics of interest included: (1) mean follow-up, (2) study design, (3) level of evidence (LOE), (4) methodological quality of evidence (MQOE), (5) number of patients included, (6) number of shoulders included, (7) mean patient age, (8) patient gender, and (9) whether the OL procedure was performed as a revision procedure. The criteria previously established by Robertson et al. 23 and Wright et al. 24 were utilized to evaluate each study's LOE and MQOE, respectively.
Outcomes of interest included: (1) reported pain levels, (2) patient-reported outcome measures, (3) RTP metrics, (4) dislocations and subluxations, (5) infection rates, (6) instability arthropathy, (7) radiological outcomes, and (8) subsequent revision surgeries. Classification of instability arthropathy was performed utilizing the criteria previously described by Samilson and Prieto, 25 which is a standardized metric for assessing degenerative changes secondary to shoulder instability. In cases where studies reported outcomes at various time points in follow-up, only outcomes that were specifically recorded at a minimum 15-year follow-up were included in this review.
Statistics
Quantitative statistical analysis was performed using SPSS version 22.0 (IBM Corp., Released 2013. IBM SPSS Statistics for Windows, Version 22.0; Armonk, NY: IBM Corp.) Categorical variables were analysed using Fisher's exact or chi-squared test. A p-value of <0.05 was deemed to be statistically significant.
Results
Literature search
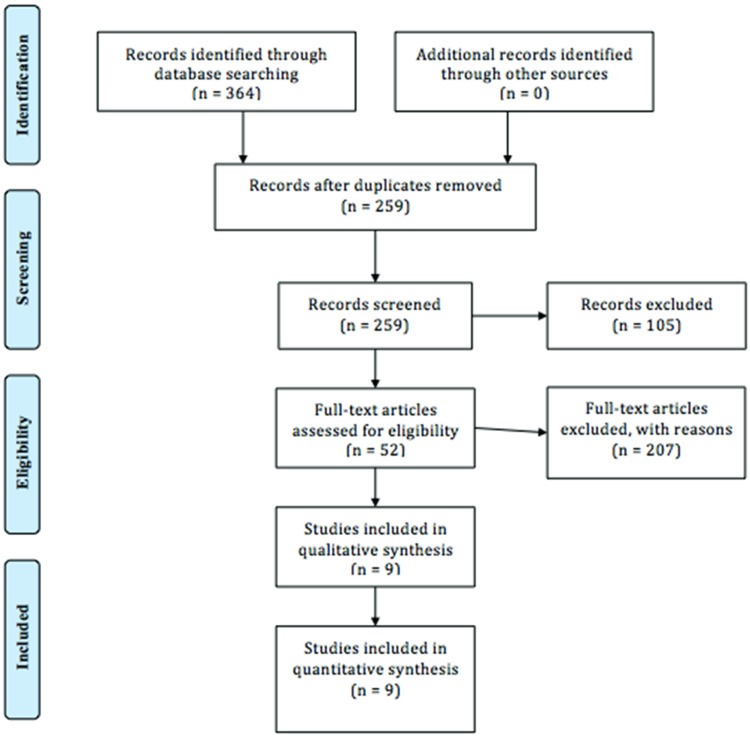
The initial literature search yielded an overall total of 364 studies. After the removal of 105 duplicated studies by both independent reviewers, the remaining 259 studies were screened using our exclusion criteria. Thereafter, the remaining full texts of 259 studies were screened for eligibility using our pre-determined inclusion criteria. A total of nine clinical studies including 326 shoulders were included in this study.26–34 A PRISMA Flow Chart is further illustrated in Figure 1.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flowchart.
Study characteristics and patient demographics
The nine included studies composed of 326 shoulders (78.2% males) in 313 patients who underwent the OL procedure in the setting of anterior shoulder instability. There were two level III studies and seven level IV studies, with a mean MQOE of 50.8 ± 10.9 (38–66). Overall, the mean age of the 313 included patients was 26.9 ± 3.2 years (15–58), with a mean follow-up of 271.9 ± 69.2 months (180–420). A summary of study characteristics and patient demographics is further illustrated in Table 1.
Table 1.
Study characteristics and patient demographics.
| Reference | N Shoulders | N Patients | LOE | MQOE | Male | Age (years) | F/U (Mo) | Prev surgery |
|---|---|---|---|---|---|---|---|---|
| Chillemi et al. 27 | 40 | 40 | III | 52 | 33/40 | 26.5 (18–35) | 307.4 (288–348) | 0/40 |
| Filho 28 | 27 | 27 | IV | 43 | 23/27 | 32 (17–59) | 240 | 0/27 |
| Gordins et al. 29 | 31 | 31 | IV | 58 | 23/31 | 26.7 | 408 (396–420) | 11/31 |
| Hovelius et al. 30 | 30 | 28 | III | 39 | 24/30 | 28.4 (15–45) | 181.3 (180–192) | 0/30 |
| Lalanne et al. 26 | 44 | 44 | IV | 38 | 35/44 | 28 | 264.3 | N/R |
| de å Escalopier et al. 31 | 20 | 20 | IV | 66 | 20/20 | 26.5 | 195.6 (180–288) | 0/20 |
| Mizuno et al. 32 | 68 | 60 | IV | 59 | 49/68 | 29.4 (16–58) | 240 (216–264) | 0/68 |
| Schroder et al. 33 | 52 | 49 | IV | 62 | 48/52 | 20.5 (18–22) | 316.8 (296.4–338.4) | N/R |
| Singer et al. 34 | 14 | 14 | IV | 40 | 8/14 | 25 (18–36) | 246 (240–270) | N/R |
F/U: follow-up; LOE: level of evidence; Mo: months; MQOE: methodological quality of evidence; N: number; Prev: previous; N/R: not reported; Yrs; years.
Functional outcomes
The most commonly reported functional outcome measure was patient-reported satisfaction, which was reported in eight studies (n = 306) overall. At a minimum 15-year follow-up, 93.5% (286 of 306) patients reported being satisfied with their OL procedure, whilst 86.8% (177 of 204) reported good or excellent outcomes at the final follow-up.
The most commonly utilized functional outcome score was the Rowe score, which was reported in six studies overall (n = 237). The mean Rowe score reported at a minimum 15-year follow-up post-OL procedure in 312 patients was 88.5 ± 5.5 (5–100). Additionally, the mean subjective shoulder values (SSV), constant and Walch-Duplay scores were reported at the final follow-up in three, two and two studies as 87.5 ± 6.4, 82.7 ± 2.5 (68–95) and 73.7 ± 8.4 (5–100), respectively.
Residual pain levels
Overall, a total of four studies reported the rates of residual pain as 33.3% (52 of 156) at a minimum of 15-year follow-up following the OL procedure. Furthermore, the rates of reported daily pain and occasional pain were 8.3% (13 of 156) and 26.3% (41 of 156), respectively.
Return to play
A total of three studies reported the rate of RTP as 96.1% (98 of 102) following the OL procedure. Additionally, two studies overall reported the rate of RTP at the same/higher level as 89.0% (73 of 82).
Recurrent instability and revision surgery
All nine of the included studies (n = 326) reported rates of recurrent instability post-OL procedure at the final follow-up. The overall rate of recurrent instability was 7.7% (25 of 326). This included rates of re-dislocations and subluxation at 3.4% (11 of 326) and 5.8% (25 of 326), respectively. The overall rate of apprehension at a minimum of 15 years post-OL was reported in five studies as 9.2% (13 of 142).
However, only seven of the included studies (n = 255) reported rates of overall surgical revisions and those revised for recurrent instability. The rate of surgical revision at a minimum 15-year follow-up following an OL procedure was 5.1% (13 of 255), of which 3.5% of cases (9 of 255) were revised for recurrent instability. A summary of clinical outcomes, recurrence rates and revision surgeries is further illustrated in Table 2.
Table 2.
Clinical outcomes, recurrence and revision surgery.
| Outcome | N studies | Total | Range |
|---|---|---|---|
| Total (n) | 9 | 326 | – |
| Males (%) | 9 | 78.8% | – |
| Age (Yrs) | 9 | 26.9 ± 3.2 | 15–58 |
| Mean F/U (Mo) | 9 | 271.9 ± 69.2 | 180–420 |
| Constant | 2 | 82.7 ± 2.5 | 68–95 |
| Ex/good | 5 | 86.7% (177/204) | N/A |
| Rowe | 6 | 88.5 ± 5.4 | 5–100 |
| Satisfaction | 8 | 93.5% (286/306) | N/A |
| SSV | 3 | 87.5 ± 6.4 | N/R |
| Walch-Duplay | 2 | 73.8 ± 8.4 | 55–100 |
| Total pain | 4 | 33.3% (52/156) | N/A |
| Daily pain | 4 | 8.3% (13/156) | N/A |
| Occasional pain | 4 | 26.3% (41/156) | N/A |
| RTP | 3 | 96.1% (98/102) | N/A |
| RTP (S/H) | 2 | 89.0% (73/82) | N/A |
| Recurrence | 9 | 7.7% (25/326) | N/A |
| Dislocations | 9 | 3.4% (11/326) | N/A |
| Subluxations | 9 | 5.8% (19/326) | N/A |
| Apprehension | 5 | 9.2% (13/142) | N/A |
| Revisions | 7 | 5.1% (13/255) | N/A |
| Revision for recurrence | 7 | 3.6% (9/255) | N/A |
Ex: excellent; F/U: follow-up; Mo: months; N: number; N/A: not applicable; N/R: not reported; RTP: return to play; S/H: same or higher level; Yrs: years; SSV: subjective shoulder values; RTP: return to play.
Instability arthropathy
The overall rate of degenerative changes to the operated shoulder secondary to instability arthropathy was reported across all included studies as 41.0% (100 of 244). This included grade I (mild) instability arthropathy of 22.1% (54 of 244), grade II (moderate) instability arthropathy of 10.3% (25 of 244) and grade III (severe) instability arthropathy of 8.6% (21 of 244), respectively.
Radiological follow-up
A total of six studies (n = 132) reported the overall rate of radiological graft healing as 93.2% (23 of 132) at a minimum 15-year follow-up post-OL procedure. Additionally, three studies each reported the rates of fibrous union and non-union at the graft sites as 10.4% (12 of 115) and 7.7% (8 of 104), respectively. Radiological evidence of implanted screw breakage was reported in six studies as 4.5% (9 of 200), none of which required surgical revision. Screw migration was reported at a rate of 6.4% (7 of 109) in four studies, with no radiological bone block fractures (0 of 61) reported in three of the included studies. A summary of radiological findings is further illustrated in Table 3.
Table 3.
Radiological findings.
| Outcome | N studies | % | Total |
|---|---|---|---|
| Total OA | 9 | 41.0 | 100/244 |
| Normal | 9 | 59.0 | 144/244 |
| Mild (Grade I) | 9 | 22.1 | 54/244 |
| Moderate (Grade II) | 9 | 10.2 | 25/244 |
| Severe (Grade III) | 9 | 8.6 | 21/244 |
| Graft healing | 6 | 93.2 | 123/132 |
| Screw breakage | 6 | 4.5 | 9/200 |
| Graft resorption | 2 | 1.5 | Jan-67 |
| Fibrous union | 3 | 10.4 | 12/115 |
| Non-union | 3 | 7.7 | 8/104 |
| Migration | 4 | 6.4 | 7/109 |
| Pseudoarthrosis | 9 | 0.3 | 1/326 |
| Bone block fracture | 3 | 0.0 | 0/61 |
N: number; OA; osteoarthritis.
Discussion
The most important findings in this study are that when compared to the 10-year outcomes reported by Hurley et al., 22 the OL procedure resulted in similarly satisfactory clinical outcomes, similarly stable rates of recurrence and surgical revisions at a minimum 15-year follow-up. Additionally, although higher radiological rates of instability arthropathy were found at a minimum 15-year follow-up post-OL procedure, high rates of reported satisfaction and satisfactory clinical outcomes were reported in the longer term.
This study found that functional outcomes reported by patients following the OL procedure were excellent at a minimum 15-year follow-up. The outcomes found in this study are almost identical to those described by Hurley et al. 22 in 845 patients following OL at a minimum 10-year follow-up. 22 Therefore, it is fair to believe that functional outcomes of the OL procedure remain stable in the long-term post-10 years' minimum follow-up. The very high rates of patient-reported satisfaction as seen in the study by Hurley et al. 22 are further reflected in this study. This study echoes the patient satisfaction reported at a minimum 10-year follow-up, with over 93% of patients being satisfied with their OL procedure at least 15 years postoperatively. Despite these excellent rates of satisfaction, this study demonstrates that high rates of reported pain levels continue to exist 15 years after the OL procedure, with one-third of patients reporting pain on at least an occasional basis. However, these findings are in line with those suggested by Hurley et al., 22 suggesting that if residual pain is likely to occur in patients post-OL procedure, this seems to appear prior to long-term follow-up. Additionally, it may be postulated that in the patient with an inherently unstable shoulder, it appears stability, and not residual pain, is likely to represent the primary outcome of interest with respect to patient-reported satisfaction in the long term.
Varying rates of instability arthropathy are widely reported at long-term follow-up in the literature, with rates varying from 7% to 71% across studies with at least 10-year follow-up.34,35 However, one must consider instability arthropathy as a potential precipitator of residual pain following the OL procedure. Prior literature has found similar pain levels to rates of instability arthropathy in the cohort of patient included in this review. In their series of 177 patients, Lädermann et al. 36 reported rates of instability arthropathy and residual pain as 36% and 40%, respectively, at a mean 16-year follow-up post-OL procedure. Furthermore, the aforementioned study found satisfaction rates of >97% in the long-term, however, was excluded from inclusion in this review on the basis of our inclusion criteria, with a minimum 10-year follow-up reported overall. Similar to the rates of instability arthropathy reported by Hurley et al., 22 our study found rates of instability arthropathy of approximately 40% seem to plateau well into the second decade following the index OL procedure. In contrast, a similar systematic review by Murphy et al. 37 found instability arthropathy in 60% of patients undergoing arthroscopic Bankart repair at a minimum 10-year follow-up, which they attributed to a higher rate of recurrent instability.
This study found recurrence and revision rates of 7% and 6%, respectively, at a minimum of 15 years following the OL procedure, with rates of recurrent instability reported amongst included studies varying from 0% to 15% in the studies reporting outcomes at mean 20 years follow-up or less.27,28,32–34 With respect to these results as well as those reported by Hurley et al., 22 the rates of recurrent instability and revision surgeries are therefore likely fixed up to 20 years follow-up following the OL procedure. However, in their series of 31 shoulders at a minimum 33-year follow-up, Gordins et al. 29 reported a recurrent instability rate of 22.6% (1 dislocation, 6 subluxations) following OL procedures. Despite this, they found only one patient required surgical revision, and 87% of grafts had radiologically healed at 34 years mean follow-up. Although further longer-term follow-up studies may further inform surgeons on the topic, it is likely that based on the findings of Gordins et al. 29 that recurrent instability rates may potentially increase in the fourth decade following the OL procedure, however, potential revisions may potentially remain stable with respect to the findings of this study.
Limitations
As this study is a systematic review of all levels of evidence, it inherently suffers from the innate limitations of the included studies themselves. Furthermore, all of the included studies in this review represent retrospective studies, with seven of the nine included studies being therapeutic case series (level IV evidence). However, perhaps the largest limitation of this study is that when compared to the minimum 10-year outcomes reported by Hurley et al., 22 this study includes five of their previously included studies which account for over 20% of the patients included in their review (195 of 845). Of note, the four extra studies with over 15 years of minimum follow-up included in this study account for 131 patients, over 40% of the total included patients in this study. A further major potential bias in this study is that the search criterion was limited to English articles, which may have potentially excluded other foreign language articles on the long-term outcomes of the Latarjet procedure, further limiting results.
Conclusion
This study established that the OL procedure results in satisfactory clinical outcomes, low rates of recurrent instability and surgical revision at a minimum 15-year follow-up. Although high levels of radiological instability arthropathy and residual pain are found over the same period, these appear stable from a minimum of 10-year follow-up data.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Martin S Davey https://orcid.org/0000-0002-3229-6032
Eoghan T Hurley https://orcid.org/0000-0002-7696-2981
References
- 1.Kirkley A, Litchfield R, Thain L, et al. Agreement between magnetic resonance imaging and arthroscopic evaluation of the shoulder joint in primary anterior dislocation of the shoulder. Clin J Sport Med 2003; 13: 148–151. [DOI] [PubMed] [Google Scholar]
- 2.Widjaja AB, Tran A, Bailey M, et al. Correlation between Bankart and Hill-Sachs lesions in anterior shoulder dislocation. ANZ J Surg 2006; 76: 436–438. [DOI] [PubMed] [Google Scholar]
- 3.Kawasaki T, Ota C, Urayama S, et al. Incidence of and risk factors for traumatic anterior shoulder dislocation: An epidemiologic study in high-school rugby players. J Shoulder Elbow Surg 2014; 23: 1624–1630. [DOI] [PubMed] [Google Scholar]
- 4.Hurley ET, Matache BA, Wong I, et al. Anterior shoulder instability part I – diagnosis, nonoperative management, and Bankart repair – an international consensus statement. Arthroscopy 2022; 38: 214–223. e7. [DOI] [PubMed] [Google Scholar]
- 5.Davey MS, Hurley ET, Hurley DJ, et al. Magnetic resonance arthrography in rugby players undergoing shoulder stabilization for glenohumeral instability: Professionals have higher frequencies of more pathologies. Arthrosc Sports Med Rehabil 2021; 3: e543–e547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hurley ET, Manjunath AK, Bloom DA, et al. Arthroscopic Bankart repair versus conservative management for first-time traumatic anterior shoulder instability – a systematic review and meta-analysis. Arthroscopy 2020; 36: 2526–2532. [DOI] [PubMed] [Google Scholar]
- 7.Shin S-J, Kim RG, Jeon YS, et al. Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic Bankart repair. Am J Sports Med 2017; 45: 1975–1981. [DOI] [PubMed] [Google Scholar]
- 8.Burkhart SS, De Beer JF, Barth JRH, et al. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007; 23: 1033–1041. [DOI] [PubMed] [Google Scholar]
- 9.Hurley ET, Matache BA, Wong I, et al. Anterior shoulder instability part II-Latarjet, remplissage, and glenoid bone-grafting: An international consensus statement. Arthroscopy 2022; 38: 224–233. e6. [DOI] [PubMed] [Google Scholar]
- 10.Hurley ET, Davey MS, Montgomery C, et al. Arthroscopic Bankart repair versus open Latarjet for recurrent shoulder instability in athletes. Orthop J Sports Med 2021; 9: 23259671211023801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedman LGM, Lafosse L, Garrigues GE. Global perspectives on management of shoulder instability: Decision making and treatment. Orthop Clin North Am 2020; 51: 241–258. [DOI] [PubMed] [Google Scholar]
- 12.Ialenti MN, Mulvihill JD, Feinstein M, et al. Return to play following shoulder stabilization: A systematic review and meta-analysis. Orthop J Sports Med 2017; 5: 2325967117726055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rossi LA, Gorodischer T, Brandariz R, et al. High rate of return to sports and low recurrences with the Latarjet procedure in high-Risk competitive athletes with glenohumeral instability and a glenoid bone loss <20. Arthrosc Sports Med Rehabil 2020; 2: e735–e742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davey MS, Hurley ET, O’Doherty R, et al. Open Latarjet procedure in athletes following failed prior instability surgery results in lower rates of return to play. Arthroscopy 2021; 37: 2412–2417. [DOI] [PubMed] [Google Scholar]
- 15.Davey MS, Hurley ET, Mullett H. Clinical outcomes of Gaelic Athletic Association athletes following surgical stabilization in the setting of anterior shoulder instability. JSES Int 2021; 6: 259–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hurley ET, Davey MS, Montgomery C, et al. Arthroscopic Bankart repair versus open Latarjet for first-time dislocators in athletes. Orthop J Sports Med 2021; 9: 23259671211023803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hurley ET, Davey MS, Montgomery C, et al. Analysis of athletes who did not return to play after open Latarjet. Orthop J Sports Med 2022; 10: 23259671211071082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boileau P, Saliken D, Gendre P, et al. Arthroscopic Latarjet: Suture-button fixation is a safe and reliable alternative to screw fixation. Arthroscopy 2019; 35: 1050–1061. [DOI] [PubMed] [Google Scholar]
- 19.Hurley ET, Ben Ari E, Lorentz NA, et al. Both open and arthroscopic Latarjet result in excellent outcomes and low recurrence rates for anterior shoulder instability. Arthrosc Sports Med Rehabil 2021; 3: e1955–e1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong SE, Friedman LGM, Garrigues GE. Arthroscopic Latarjet: Indications, techniques, and results. Arthroscopy 2020; 36: 2044–2046. [DOI] [PubMed] [Google Scholar]
- 21.Leuzinger J, Brzoska R, Metais P, et al. Learning curves in the arthroscopic Latarjet procedure: A multicenter analysis of the first 25 cases of 5 international surgeons. Arthroscopy 2019; 35: 2304–2311. [DOI] [PubMed] [Google Scholar]
- 22.Hurley ET, Jamal MS, Ali ZS, et al. Long-term outcomes of the Latarjet procedure for anterior shoulder instability: A systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg 2019; 28: e33–e39. [DOI] [PubMed] [Google Scholar]
- 23.Robertson C, Ramsay C, Gurung T, et al. Practicalities of using a modified version of the Cochrane Collaboration risk of bias tool for randomised and non-randomised study designs applied in a health technology assessment setting. Res Synth Methods 2014; 5: 200–211. [DOI] [PubMed] [Google Scholar]
- 24.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am 2003; 85: 1–3. [PubMed] [Google Scholar]
- 25.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 1983; 65: 456–460. [PubMed] [Google Scholar]
- 26.Lalanne C, Vervoort T, Cassagnaud X, et al. Long-term prevalence and impact of glenohumeral osteoarthritis after Latarjet-Patte procedure for anterior instability. Orthop Traumatol Surg Res 2022: 103050. [DOI] [PubMed] [Google Scholar]
- 27.Chillemi C, Guerrisi M, Paglialunga C, et al. Latarjet procedure for anterior shoulder instability: A 24-year follow-up study. Arch Orthop Trauma Surg 2021; 141: 189–196. [DOI] [PubMed] [Google Scholar]
- 28.Filho JG, Leite MC, Borges ACW, et al. Clinical and radiographic evaluation of patients operated by the Bristow-Latarjet technique with a minimum follow-up of 20 years. Revis Bras Ortop (Sao Paulo) 2020; 55: 455–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gordins V, Hovelius L, Sandström B, et al. Risk of arthropathy after the Bristow-Latarjet repair: A radiologic and clinical thirty-three to thirty-five years of follow-up of thirty-one shoulders. J Shoulder Elbow Surg 2015; 24: 691–699. [DOI] [PubMed] [Google Scholar]
- 30.Hovelius LK, Sandström BC, Rösmark DL, et al. Long-term results with the Bankart and Bristow-Latarjet procedures: Recurrent shoulder instability and arthropathy. J Shoulder Elbow Surg 2001; 10: 445–452. [DOI] [PubMed] [Google Scholar]
- 31.de å Escalopier N, Barbier O, Demoures T, et al. Long-Term results of a monocentric series of soldiers after Latarjet procedure for anterior shoulder instability. Implications for the assessment of soldiers’ medical ability. Mil Med 2018; 183: e134–e137. [DOI] [PubMed] [Google Scholar]
- 32.Mizuno N, Denard PJ, Raiss P, et al. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 2014; 23: 1691–1699. [DOI] [PubMed] [Google Scholar]
- 33.Schroder DT, Provencher MT, Mologne TS, et al. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen. Am J Sports Med 2006; 34: 778–786. [DOI] [PubMed] [Google Scholar]
- 34.Singer G, Kirkland P, Emery R. Coracoid transposition for recurrent anterior instability of the shoulder. A 20-year follow-up study. J Bone Joint Surg Br 1995; 77: 73–76. [PubMed] [Google Scholar]
- 35.Bouju Y, Gadéa F, Stanovici J, et al. Shoulder stabilization by modified Latarjet-Patte procedure: Results at a minimum 10 years’ follow-up, and role in the prevention of osteoarthritis. Orthop Traumatol Surg Res 2014; 100: S213–S218. [DOI] [PubMed] [Google Scholar]
- 36.Lädermann A, Lubbeke A, Stern R, et al. Risk factors for dislocation arthropathy after Latarjet procedure: A long-term study. Int Orthop 2013; 37: 1093–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murphy AI, Hurley ET, Hurley DJ, et al. Long-term outcomes of the arthroscopic Bankart repair: A systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg 2019; 28: 2084–2089. [DOI] [PubMed] [Google Scholar]