Abstract
Background
Various reduction techniques exist to treat traumatic shoulder dislocation, but best management remains unclear.
Aims
To investigate the reduction rate of traumatic anteroinferior shoulder dislocations using two sedation-free techniques and success rates of subgroups.
Methods
A single-center study was performed analysing shoulder dislocations in a two-year period. Adult patients with anteroinferior shoulder dislocation were included. Two sedation-free reduction techniques were used: the Davos self-reduction technique and the Arlt-chair technique. Two attempts were performed before sedation. All patients gave informed consent to study participation.
Results
The investigated 106 patients (106 shoulder dislocations) had a mean age of 48 ± 18 years (74% male patients). The majority occurred during winter sports (76%). The overall success rate for both sedation-free reduction techniques was 82% (87 reduced shoulders, two attempts). A significantly increased success rate was found in patients without greater tuberosity fracture (86% without vs. 68% with fracture, p = 0.002) and for patients with repeated dislocation (93% vs. 80% for primary dislocation, p = 0.004). Time for reduction was 5 minutes (Davos technique) and 1 minute (Arlt-chair-technique). Associated injuries were mostly Hill Sachs lesions (78%). There was no major complication and no new-onset sensory deficit.
Conclusion
Davos and Arlt reduction techniques allowed sedation-free and fast treatment for anteroinferior shoulder dislocation during winter sports.
Keywords: shoulder dislocation, shoulder reduction, Davos method, Arlt method, chair method
Introduction
The treatment of an acute shoulder dislocation should be performed in a timely manner. A delay of the first reduction attempt in anterior shoulder dislocation is associated with a higher failure rate. 1 Management algorithms without delaying the time to the first reduction attempt are, therefore, important because shoulder dislocations are the most frequent joint dislocations. 2 Up to 97% are anteroinferior dislocations that occur mostly during sports in young patients. 3 Repeated dislocations often lead to shoulder instability, associated glenohumeral bone and cartilage lesions.4,5 The reported incidence rate for young males is up to 98 per 100,000 person-years 6 and can affect even 14-to 16-year-old adolescent patients. 7 Treatment of anterior shoulder instability includes conservative management 8 or surgery. 9
The best management strategy for acute shoulder dislocations is yet unknown. There is a wide variety of management strategies, according to surveys in the Netherlands and the United Kingdom.10,11 In addition, there is a debate about the optimal immobilization position in patients with shoulder instability.8,12–14 The main controversies are the method of analgesia and the reduction technique for shoulder reduction. There are plenty of reduction techniques with various advantages and disadvantages. 15 One disadvantage of most reduction methods is the time needed, medication and the resources used and especially medical personnel (e.g., emergency doctors and nurses). One potential advantage of reduction with procedural sedation is the facilitated reduction needing less power and effort by the physician and a theoretically lower risk of iatrogenic fracture. A recent systematic review reported cumulative success rates of shoulder reduction for different methods that ranged from 73% to 97%. 16 But the number of patients was relatively small and the use of procedural sedation and analgesics ranged from 0% to 100%. 16 Some methods for closed shoulder reduction are analgesia-free, some use systemic analgesia, intra-articular lidocaine and/or procedural sedation. 17 Known negative consequences of intra-articular analgesia and procedural sedation are: delay of the first reduction attempt, a longer stay in the emergency department (ED) and potential septic arthritis. 18 Major complications of procedural sedation are laryngospasm, need for intubation and aspiration.17,19 A potential strategy to avoid these complications is the use of sedation-free techniques. These techniques (Figure 1) are reportedly nontraumatic, safe and simple, with a considerable success rate. 20
Figure 1.
Shoulder reduction methods: (a) Davos self-reduction technique (above), (b) Arlt chair technique (below).
Most acute shoulder dislocations that are encountered in the ED are associated with winter sports. These patients were managed without routine use of sedatives and their treatment analysed. The aim of this study was to analyse the reduction rate of traumatic anteroinferior shoulder dislocations of an algorithm without primary sedation. A secondary aim was to describe the success rates of different reduction techniques and subgroups, predictive factors for a successful reduction and associated injuries.
Materials and methods
Study design, inclusion and exclusion criteria
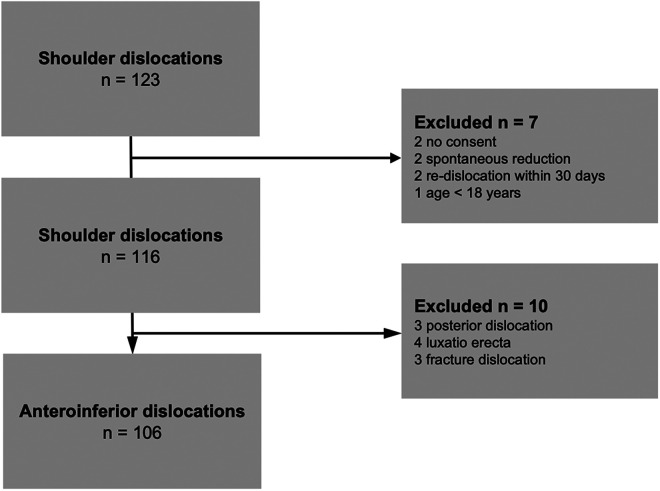
A single-center observational study of patients with shoulder dislocation was performed over a two-year period. All patients >18 years with a radiologically diagnosed anteroinferior shoulder dislocation were prospectively included. Patients with fractures of the glenoid rim, the greater tuberosity and with Hill Sachs lesions were included. Three patients with fracture dislocations of the proximal humerus, three patients with posterior dislocations and four patients with a “luxatio erecta” were excluded (Figure 2). Patients with a recurrent dislocation within 30 days were only included in their first ED attendance. This resulted in 106 patients (Figure 2), and all gave informed consent to participation in the study, and the data were analysed in an anonymized fashion. This study was observational, because patient management was not changed, and it was performed in accordance with the ethical standards of the Declaration of Helsinki.
Figure 2.
Flow chart shows excluded patients.
Management algorithm
All patients with shoulder dislocations were treated in the ED. This includes the acquisition of the patient's history and physical examination, especially evaluating the sensory and motor function and pulse deficits. All patients suspected of a shoulder dislocation were examined with an anteroposterior radiograph of the shoulder. A Neer view was added if there was a concern about the dislocation type. Every doctor working in the ED was instructed on the management algorithm. The methods that were instructed were the Arlt-chair and the Davos self-reduction technique. The doctors could choose the reduction method. Two attempts to reduce the dislocated shoulder were performed before sedation. Sedation was used if the first two attempts were not successful or if the patient was unable to participate in a reduction attempt or if the treating physician deemed primary sedation as the best medical treatment. The physicians could use the same method twice or change after a failed attempt. After two failed attempts, a procedural sedation was performed by a board-certified anaesthetist. No additional sedatives, intra-articular or regional anaesthesia was applied for the first two attempts of reduction.
Techniques of shoulder reduction
Davos self-reduction technique
This technique is also known as the Aronen or Boss–Holzach–Matter technique. The technique was first described in 1986. 21 The first systematic description of the technique and report of clinical results was published by Boss, Holzach and Matter from Davos in Switzerland in 1993. 22 They reported on a series of 51 patients with a primary success rate of 57%. In short, the patient is seated, leans forward and put his hands together to lock his hands on the injured upper extremity around the ipsilateral knee (Figure 1). For this self-reduction technique, a special bandage helps to fixate the wrists together. Alternatively, this can be provided with a knotted sheet. Because this is a self-reduction method, the physician's job is to instruct the patient, help with setup and provide mental support (details are provided in supplementary material).
Arlt chair technique
The Arlt-chair-technique is also known as the technique according to von Arlt, chair technique or Oxford chair technique, which was first mentioned (1941) by “Benno Ritter von Arlt” in Germany. 23 The original technical description with a picture can be found in a review reporting the development of shoulder reduction techniques. 24 The patient is placed on a chair with the armpit placed on the padded straight backrest. The physician assists the reduction while pulling the arm downwards as shown in Figure 1B. Additionally, adduction and a slight external rotation can help for a successful reduction. A combined success rate of 78% (108 patients) was described previously. 16
Follow-up treatment
The shoulder is immediately immobilized with a sling in an internal rotation position of the arm after successful reduction. Perfusion, sensory and motor function were assessed again. An anteroposterior and Neer radiograph are performed after reduction for documentation of the reduced shoulder joint. A follow-up visit was scheduled for all shoulder dislocations the day after to reassess pain and the neurovascular status. Day tourists occasionally did their follow-up visits at their place of residence.
Endpoints
The primary endpoint of this study was the rate of successful shoulder reduction without procedural sedation for two attempts of closed reduction. Secondary endpoints were the success rate of subgroups and reduction techniques, neurovascular complications, time in the ED and time used for a successful reduction. The overall success rate of all sedation-free reduction techniques was calculated by adding the successful reductions (first and second attempt) of different techniques.
Statistics
Descriptive statistics are reported as frequencies and percentages. Statistical evaluation was performed by one independent author, not involved in patient care. A normal distribution was present for all continuous parameters, which were confirmed with the Kolmogorov–Smirnov test. Normal distributed variables are displayed as mean and standard deviation (SD). Non-normal data are presented as median and minimum and maximum. Comparison of the reduction rate between the five subgroups (Table 1) was performed with the Fisher exact test and Chi-square test if applicable. Statistical significance was defined as p-value<0.01. Statistical analysis was performed with R (R Core Team (2018) and Winstat (R Fitch Software).
Table 1.
Sedation-free success rates in different subgroups of patients.
| Subgroup | No. of patients in subgroup | No. successful sedation-free reductions | Success rate |
|---|---|---|---|
| Overall | 106 | 87 | 82% |
| Male patients | 78 | 65 | 83% |
| Female patients | 28 | 22 | 79% |
| Without greater tuberosity fracture | 84 | 72 | 86%* |
| With greater tuberosity fracture | 22 | 15 | 68% |
| Patients with BMI<25 kg/m2 | 62 | 53 | 85% |
| Patients with BMI>25 kg/m2 | 40 | 30 | 75% |
| Primary dislocation | 92 | 74 | 80% |
| Repeated dislocation | 14 | 13 | 93%** |
| Age <30 years | 27 | 24 | 89% |
| Age >60 years | 35 | 28 | 80% |
| Male patients with repeated dislocation | 10 | 10 | 100% |
| Age <30 years with a BMI <25 kg/m2 | 20 | 19 | 95% |
*significant difference (p < 0.01) compared to patients with greater tuberosity fracture;
**significant difference (p < 0.01) compared to patients with primary dislocation; data for BMI calculation was available for 102 patients. Level of significance was adjusted with a Bonferroni correction for 5 subgroups (0.05 / 5 = 0.01).
Results
Demographics
Of 123 eligible patients, 106 patients were included in our analysis (Figure 2). The patients were mostly male (74%, Table 2) and had a mean age of 48 ± 18 years. Most injuries were primary shoulder dislocations (87%) and occurred during winter sports (76%), skiing was the most frequent winter sports.
Table 2.
Demographic and injury details for 106 patients.
| Parameter | Total |
|---|---|
| Age [years] | 48 ± 18 (18–84) |
| Male (% of all patients) | 78 (74%) |
| Primary dislocation | 92 (87%) |
| Height [cm]* | 175 ± 9 (152–194) |
| Weight [kg]* | 76 ± 14 (46–145) |
| Body mass index* | 25 ± 4 (18–42) |
| Patients with BMI <25kg/m2 (% of all patients) | 62 (61%) |
| Patients with BMI >25kg/m2 (% of all patients) | 40 (39%) |
| Previous shoulder surgery (% of all patients) | 5 (5%) |
| Left shoulder (% of all patients) | 54 (51%) |
| Time from accident to ED [min] | 60 (10–1560) |
| Mechanism of injury | |
| Winter sports injury (% of all patients) | 81 (76%) |
| Skiing | 62 (58%) |
| Snowboarding | 16 (15%) |
| Fall from standing height | 10 (9%) |
| Minor trauma | 6 (6%) |
| Biking | 5 (5%) |
| Other | 4 (4%) |
| Sledge riding | 3 (3%) |
*Data available for only 102 patients; Continuous variables are displayed as mean ± SD (min-max). Winter sports injury comprises skiing, snowboarding and sledge riding.
Primary endpoint success rate
Shoulder reduction without sedation was achieved in 82% of all patients with a shoulder dislocation (Figure 3).
Figure 3.
Flow chart shows the attempted and successful reductions of the patient series.
Subgroup analysis
The success rate with the Davos self-reduction technique was 58% (first attempt) and 61% using two attempts. The success rate of the Arlt chair technique was 72% (first attempt) and 71% (two attempts). A significantly increased success rate of sedation-free techniques was found in patients without a greater tuberosity fracture (86% without versus 68% with a fracture, p = 0.002). A significantly increased success rate was found for patients with a repeated dislocation (93% vs. 80% for primary dislocation, p = 0.004, Table 1). High success rates were found for male patients with a repeated dislocation (100%), for patients <30 years of age with a BMI < 25 kg/m2 (95%) and for male patients (83%). In the first attempt, 59% could be reduced (Figure 3). In the second attempt of reduction, additional 24 patients could be reduced. The remaining 10 patients were reduced with procedural sedation (Figure 3). In total, 19 patients received a procedural sedation (Figure 3).
Time, analgesia and associated injuries
Successful reduction with the Davos self-reduction technique was achieved in 5 minutes (median, range 10 s to 15 minutes). The reduction with the Arlt-chair-technique took one minute (median, range 4 s to 14 min). Patients with a short time interval from accident to reduction (<90 min) had a significantly (p = 0.007) higher sedation-free reduction rate (93%) compared to patient with a longer interval (73%).
Sensory and motor assessment before and after reduction showed no new-onset motor deficit after reduction (Supplementary Table). The most common medication used for analgesia was fentanyl (44%, Table 3). Medication used for analgesia is listed in Table 3, and 14% of the patients did not use medication for analgesia (Table 3).
Table 3.
Analgesia regimen until reduction.
| Analgesic regimen | Frequency | Percentage of all patients |
|---|---|---|
| No analgesia | 15 / 106 | 14% |
| Metamizole | 36 / 106 | 34% |
| Fentanyl (Opiate) | 47 / 106 | 44% |
| Tilidin (Opiate) | 16 / 106 | 15% |
| NSAID | 6 / 106 | 6% |
| Ketamine | 13 / 106 | 12% |
| Benzodiazepine | 16 / 106 | 15% |
| Tramadol (Opiate) | 2 / 106 | 2% |
NSAID: non-steroidal anti-inflammatory drug.
Note: Medication used for procedural sedation is not included. Percentages add up to more than one-hundred percent due to combination of pain medication.
Discussion
In this case series, two sedation-free reduction techniques for anteroinferior shoulder dislocations were investigated. Most importantly, we found that both the Davos and the Arlt techniques are fast-reduction methods for patients with winter sport accidents. These techniques could be applied successfully for male patients with repeated dislocations (Table 1). No complications associated with the Davos self-reduction technique were noted. This study demonstrates that eight out of ten mainly winter sports–associated anteroinferior shoulder dislocations can be reduced without sedation. In six patients, a new-onset sensory nerve palsy after the reduction was observed, and in all of them, the Arlt-chair-technique was used (Supplementary Table). As there were five nerve palsies in the innervation field of the axillary nerve, this might be a result from the pressure between the armpit and the padded straight backrest of the chair. Neurological assessment of sensory and motor function before and after reduction showed no new-onset motor deficit after reduction (Supplementary Table).
Comparing the success rate of sedation-free reduction techniques, few studies investigating these techniques were found. A systematic review 16 reported success rates of different techniques for shoulder reduction ranging from 28% to 97%. The found success rate (82%) in the current study was comparable to the Milch (83%) 25 and Kocher technique (81%). 26 For other techniques such as the “scapular manipulation” and “traction counter-traction” slightly higher success rates were described. 16 However, 100% of the patients that underwent scapular manipulation received opioid analgesics, 27 and 37% of the patients that underwent traction counter-traction received intravenous sedation. 16 In addition, the previous studies investigating these two techniques 27 had a lower sample size. 28 Other studies reported lower success rates using different methods for reduction (Stimson or Hippocratic method). Unfortunately, the application of intravenous sedation was not reported in all studies 16 ; therefore, comparison to the methods used in the current study is limited.
Comparing the two reduction techniques used in the current study, there was a slight difference between the primary success rate of the Arlt chair and the Davos self-reduction technique (72% vs. 58%, one attempt). The primary success rate of the Davos technique compares well to the first reported data in 1993 (57% success rate in 51 patients).22, 29 Marcano-Fernández et al. compared the Davos method (called Boss–Holzach–Matter method) and Spaso technique in their randomized controlled study in 2018 and randomized 30 patients to the Davos self-reduction method. 30 They reported a success rate of 77% (23/30) with a mean reduction time of 90 s (minimum 5 s and maximum 10 min). They had a higher primary success rate and a shorter reduction time compared to the current study. However, the number of excluded patients was high (378 patients screened for eligibility and 318 excluded). Therefore, a selection bias is possible in this randomized controlled study. The main exclusion criteria were age >60 years and associated fractures. The study population differs compared to the current study because only 60% were first episodes of shoulder dislocation and only 53% were sports-associated injuries in their study. In the current study, the mean age was 50 years (Table 2), and an associated greater tuberosity fracture seems to negatively influence the success rate (Table 1). This could explain partially the differences between the success rates. Stafylakis et al. reported a higher success rate of 86% (86/100) in a retrospective study of the Davos technique. 20 They treated mostly (62%, 62/100) recurrent shoulder dislocations and they performed no consecutive analysis because they excluded patients that were treated with another method. Comparing the rate of recurrent shoulder dislocations in the current study (13%), their rate seems to be much higher. This could probably explain the different results for the success rate of sedation-free techniques. To compare the success rate of the Davos method, previous studies were summarized in Figure 4.
Figure 4.
Studies that investigated the reduction rate of the Davos method are summarized. The bubble size indicates the sample size of the study.
This study has clinical implications. Based on our results, physicians and first-aiders working in the ED should be encouraged to use sedation-free techniques for shoulder reduction and to establish similar treatment algorithms. This could be beneficial for sportive patients and especially for young and male patients. An instruction of a self-reduction technique via smartphone may be an option for patients in areas 31 without a medical service. 32 For patients with a recurrent dislocation, it seems effective to teach them a self-reduction technique, such as the Davos (also called Boss–Holzach–Matter) technique. 33 Then they could probably treat themselves without seeing an emergency doctor. Sedation-free techniques could be very important for first-aiders, for athletes and for low-income countries, where medical care with anaesthesia is not always available. In addition, the use of sedation-free techniques could help to reduce complications associated with the use of sedation, such as laryngospasm, need for intubation and aspiration. 19 Self-reduction of shoulder dislocations demonstrates the art of medicine, after a quick history and physical examination, interpretation of the radiograph for assessment of the type of dislocation and associated injuries. The self-reduction is easy to learn and requires only minor guidance of the patient for reduction and could probably be applied by first aiders. 34
There are limitations and strengths to our study. First, the majority of the patients were male; therefore, the generalizability for female patients is limited. This was inherently given due to the higher incidence of shoulder dislocations in male patients. Second, most patients reported winter sports accidents, and this limits the generalizability of the results. Third, the individual performance (reduction rate) of physicians was not analysed. This is a potential bias because the experience could vary between physicians. But before the onset of this study, all physicians received standardized instructions and underwent training for the two sedation-free reduction methods. Fourth, there was a potential bias because doctors were free to choose the reduction method. They adapted the method to patient factors (e.g., compliance), for example, when a patient was not able to be instructed on the Davos self-reduction method because of language barrier or other causes. Patients were usually referred to a doctor at their place of residence for follow-up examination or to perform additional radiological examinations. One of the strengths of this study is the large sample size of more than 100 patients. Another strength is that the data were collected prospectively, all consecutive patients were screened for inclusion in the study, and several factors associated with a high success rate could be calculated. Furthermore, the current study represents real-world circumstances in an ED with winter sports–associated injuries, where different physicians treat the patients and different techniques are used.
Conclusion
The Davos and Arlt reduction techniques for anteroinferior shoulder dislocation were successful in four out of five patients allowing two attempts. These techniques are fast and favourable for winter sports injuries, for male patients, for recurrent dislocations and for dislocation without fracture. The Davos self-reduction and the Arlt-chair are sedation-free techniques and resulted in success rates of >90% for repeated dislocations and for young and male patients. This treatment approach could potentially accelerate patient management and could probably be applied in pre-hospital settings and by first aiders.
Supplemental Material
Supplemental material, sj-docx-1-sel-10.1177_17585732221145608 for Fast treatment of anterior shoulder dislocations with two sedation-free methods: The Davos self-reduction method and Arlt method by Lukas Werner Widmer, Till Dominic Lerch, Anna Genthner, Lara Pozzi, James Geiger and Hans-Curd Frei in Shoulder & Elbow
Footnotes
Contributorship: LW and TL researched literature. LW was involved in protocol development, gaining ethical approval, patient recruitment and data analysis. LW wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: The hospital does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article: This research received no specific grant from any funding agency in the public, commercial, or not for-profit sectors.
Guarantor: LW.
Informed Consent: Written informed consent was obtained from the patients for their anonymized information to be published in this article.
ORCID iDs: Till Dominic Lerch https://orcid.org/0000-0002-0475-0269
Lara Pozzi https://orcid.org/0000-0003-4618-045X
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Kanji A, Atkinson P, Fraser J, et al. Delays to initial reduction attempt are associated with higher failure rates in anterior shoulder dislocation: a retrospective analysis of factors affecting reduction failure. Emerg Med J 2016; 33: 130–133. [DOI] [PubMed] [Google Scholar]
- 2.Nabian M, Zadegan S, Zanjani L, et al. Epidemiology of joint dislocations and ligamentous/tendinous injuries among 2,700 patients: five-year trend of a tertiary center in Iran. Arch Bone Jt Surg 2017; 5: 426–434. [PMC free article] [PubMed] [Google Scholar]
- 3.Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg 1989; 108: 288–290. [DOI] [PubMed] [Google Scholar]
- 4.Duchman KR, Hettrich CM, Glass NA, et al. The incidence of glenohumeral bone and cartilage lesions at the time of anterior shoulder stabilization surgery: a comparison of patients undergoing primary and revision surgery. Am J Sports Med 2018; 46: 2449–2456. [DOI] [PubMed] [Google Scholar]
- 5.Longo UG, Candela V, Berton A, et al. Epidemiology of shoulder instability in Italy: a 14-years nationwide registry study. Injury 2021; 52: 862–868. [DOI] [PubMed] [Google Scholar]
- 6.Leroux T, Wasserstein D, Veillette C, et al. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med 2014; 42: 442–450. [DOI] [PubMed] [Google Scholar]
- 7.Leroux T, Ogilvie-Harris D, Veillette C, et al. The epidemiology of primary anterior shoulder dislocations in patients aged 10 to 16 years. Am J Sports Med 2015; 43: 2111–2117. [DOI] [PubMed] [Google Scholar]
- 8.Braun C, McRobert CJ. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst Rev 2019; 5: CD004962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng S, Song Y, Li H, et al. Outcomes for arthroscopic repair of combined Bankart/SLAP lesions in the treatment of anterior shoulder instability: a systematic review and meta-analysis. Orthop J Sports Med 2019; 7: 232596711987780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.te Slaa RL, Wijffels MPJM, Marti RK. Questionnaire reveals variations in the management of acute first-time shoulder dislocations in the Netherlands. Eur J Emerg Med 2003; 10: 58–61. [DOI] [PubMed] [Google Scholar]
- 11.Chong M, Karataglis D, Learmonth D. Survey of the management of acute traumatic first-time anterior shoulder dislocation among trauma clinicians in the UK. Ann R Coll Surg Eng 2006; 88: 454–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itoi E, Kitamura T, Hitachi S, et al. Arm abduction provides a better reduction of the Bankart lesion during immobilization in external rotation after an initial shoulder dislocation. Am J Sports Med 2015; 43: 1731–1736. [DOI] [PubMed] [Google Scholar]
- 13.Jordan RW, Saithna A, Old J, et al. Does external rotation bracing for anterior shoulder dislocation actually result in reduction of the labrum? Am J Sports Med 2015; 43: 2328–2333. [DOI] [PubMed] [Google Scholar]
- 14.Scheibel M, Kuke A, Nikulka C, et al. How long should acute anterior dislocations of the shoulder be immobilized in external rotation? Am J Sports Med 2009; 37: 1309–1316. [DOI] [PubMed] [Google Scholar]
- 15.Alkaduhimi H, van der Linde JA, Flipsen M, et al. A systematic and technical guide on how to reduce a shoulder dislocation. Turk J Emerg Med 2016; 16: 155–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alkaduhimi H, van der Linde JA, Willigenburg NW, et al. A systematic comparison of the closed shoulder reduction techniques. Arch Orthop Trauma Surg 2017; 137: 589–599. [DOI] [PubMed] [Google Scholar]
- 17.Fitch RW, Kuhn JE. Intraarticular lidocaine versus intravenous procedural sedation with narcotics and benzodiazepines for reduction of the dislocated shoulder: a systematic review. Acad Emerg Med 2008; 15: 703–708. [DOI] [PubMed] [Google Scholar]
- 18.Gulihar A, Robati S, Twaij H, et al. Articular cartilage and local anaesthetic: a systematic review of the current literature. J Orthop 2015; 12: S200–S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellolio MF, Gilani WI, Barrionuevo P, et al. Incidence of adverse events in adults undergoing procedural sedation in the emergency department: a systematic review and meta-analysis. Acad Emerg Med 2016; 23: 119–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stafylakis D, Abrassart S, Hoffmeyer P. Reducing a shoulder dislocation without sweating. The Davos technique and its results. Evaluation of a nontraumatic, safe, and simple technique for reducing anterior shoulder dislocations. J Emerg Med 2016; 50: 656–659. [DOI] [PubMed] [Google Scholar]
- 21.Aronen JG. Anterior shoulder dislocations in sports. Sports Med 1986; 3: 224–234. [DOI] [PubMed] [Google Scholar]
- 22.Boss A, Holzach P, Matter P. [Analgesic-free self-reduction of acute shoulder dislocation]. Z Unfallchir Versicherungsmed 1993; Suppl 1: 215–220. [PubMed] [Google Scholar]
- 23.von Arlt B. Erfahrungen bei Einrichtung der Schulterverrenkung. Chirurg 1941; 13: 416–418. [Google Scholar]
- 24.Sachs M. Die Entwicklung der Repositionsverfahren bei Patienten mit Schulter- luxationen seit der Antike. In: Geschichte konservativer Verfahren an den Bewegungsorganen. Heidelberg: Steinkopff, 2001, pp. 179–192. [Google Scholar]
- 25.Amar E, Maman E, Khashan M, et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J Shoulder Elbow Surg 2012; 21: 1443–1449. [DOI] [PubMed] [Google Scholar]
- 26.Uglow MG. Kocher’s painless reduction of anterior dislocation of the shoulder: a prospective randomised trial. Injury 1998; 29: 135–137. [DOI] [PubMed] [Google Scholar]
- 27.Sahin N, Oztürk A, Ozkan Y, et al. A comparison of the scapular manipulation and Kocher’s technique for acute anterior dislocation of the shoulder. Eklem Hastalik Cerrahisi 2011; 22: 28–32. [PubMed] [Google Scholar]
- 28.Guler O, Ekinci S, Akyildiz F, et al. Comparison of four different reduction methods for anterior dislocation of the shoulder. J Orthop Surg Res 2015; 10: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boss A, Holzach P and Matter P. A new self-repositioning technique for fresh, anterior-lower shoulder dislocation. Helv Chir Acta 1993; 60: 263–265. [PubMed]
- 30.Marcano-Fernández FA, Balaguer-Castro M, Fillat-Gomà F, et al. Teaching patients how to reduce a shoulder dislocation. J Bone Joint Surg Am 2018; 100: 375–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dudkiewicz I, Arzi H, Salai M, et al. Patients education of a self-reduction technique for anterior glenohumeral dislocation of shoulder. J Trauma 2010; 68: 620–623. [DOI] [PubMed] [Google Scholar]
- 32.Chechik O, Maman E, Kazum E, et al. Self-reduction techniques taught via smartphone are effective for anterior shoulder dislocation: prospective randomized study. Knee Surg Sports Traumatol Arthrosc 2021; 29: 2338–2341. [DOI] [PubMed] [Google Scholar]
- 33.Marcano-Fernández FA, Fillat-Gomà F, Balaguer-Castro M, et al. ‘Can patients learn how to reduce their shoulder dislocation?’ A one-year follow-up of the randomized clinical trial between the Boss-Holzach-matter self-assisted technique and the Spaso method. Acta Orthop Traumatol Turc 2020; 54: 516–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Durrer B, Allenspach U, Felgenhauer S, et al. Shoulder dislocations in and outside of the doctor's surgery. Ther Umsch 2015; 72: 52–54. DOI: 10.1024/0040-5930/a000639. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sel-10.1177_17585732221145608 for Fast treatment of anterior shoulder dislocations with two sedation-free methods: The Davos self-reduction method and Arlt method by Lukas Werner Widmer, Till Dominic Lerch, Anna Genthner, Lara Pozzi, James Geiger and Hans-Curd Frei in Shoulder & Elbow