While drafting a follow-up manuscript to this article – in which the mediation analysis will be validated using data from a randomised controlled trial – the authors noted an error in the research article as originally published in the European Respiratory Journal. The error pertains to the spline model used in calculating the odds ratio for age-related mortality, as illustrated in figures 2b and c of the manuscript. Notably, the error is unrelated to all other analyses, and correcting the mistake strengthens the conclusion already present in the relevant section of the published article.
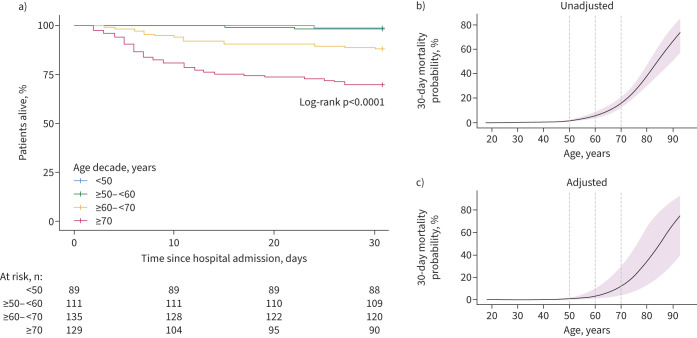
FIGURE 2.
Mortality analysis of COVID-19 patients admitted to the general ward stratified by age decade. a) Kaplan–Meier plot of patients stratified by age decade. b) Risk of 30-day mortality with age modelled as a continuous variable. The 30-day mortality probability was derived from a logistic regression. The shading represents the 95% confidence interval. c) The same method as b), but now the 30-day mortality probability is adjusted for demographics (inclusion hospital, sex and inclusion wave), age-related comorbidities (hypertension, diabetes, malignancies, immunosuppression, and chronic cardiac, neurological, respiratory and kidney disease), age-related chronic medication (antiplatelet and anticoagulant drugs), and COVID-19-related treatments both before and after sampling (corticosteroids including dexamethasone, anti-interleukin-6, imatinib, remdesivir and antibiotics).
In the very first part of the paper, the authors confirmed the already established association between ageing and mortality using a Kaplan–Meier analysis (figure 2a) and two spline plots (figure 2b and c). Upon re-examination of the data, it was found that the mortality probability and the accompanying odds ratios for mortality associated with ageing were underestimated due to an error in the spline model used to plot figures 2b and c. The mortality odds associated with ageing derived from a correct logistic regression model are higher. For example, it was initially reported that an increase in age from 60 to 70 years was associated with an increased 30-day mortality with odds ratio 1.15 (95% CI 1.12–1.18). In light of the authors’ re-analysis, the stated odds ratio should be changed to OR 3.29 (95% CI 2.41–4.48).
The corrected figure 2 and accompanying caption is presented below.
Additionally, the text in the “Results: Patients, presentation and outcome” section that originally stated:
“Mortality rates increased with age in a nonlinear fashion (table 2 and figure 2). For example, an increase in age from 60 to 70 years was associated with an increased 30-day mortality (OR 1.15, 95% CI 1.12–1.18) (figure 2b), which was independent of demographics, age-related comorbidities and COVID-related treatments (adjusted OR 1.14, 95% CI 1.11–1.17) (figure 2c). In pneumonia patients with pathogens other than SARS-CoV-2 (supplementary table S5), a similar increase in age (from 60 to 70 years) was not associated with an increase in 30-day mortality odds (OR 1.01, 95% CI 0.996–1.025).”
Should be changed to:
“Mortality rates increased with age (table 2 and figure 2). For example, an increase in age from 60 to 70 years was associated with an increased 30-day mortality (OR 3.29, 95% CI 2.41–4.48) (figure 2b), which was independent of demographics, age-related comorbidities and COVID-related treatments (adjusted OR 3.88, 95% CI 2.59–5.81) (figure 2c). In pneumonia patients with pathogens other than SARS-CoV-2 (supplementary table S5), a similar increase in age (from 60 to 70 years) was not associated with an increase in 30-day mortality odds (OR 1.62, 95% CI 0.89–2.91).”
Notably, the conclusion of the section – that ageing is associated with increased mortality in COVID-19 – remains unchanged. Additionally, the incorrect model was not used for any other analyses or figure 2a, so the rest of the findings presented in the article remain unchanged.