Abstract
Purpose
Endoscopic nipple-sparing mastectomy (E-NSM) is a minimally invasive surgical technique that shows good results in patients with breast cancer. The authors compared 3 different types of commercial energy devices to examine their efficacy and safety in E-NSM performed with breast reconstruction.
Methods
A total of 36 cases of E-NSM were conducted with either Sonicision (S group, n = 11), Harmonic (H group, n = 6), or Thunderbeat (T group, n = 19). The clinicopathologic factors and postoperative complications, including nipple or skin necrosis and surgical site seroma volume, were evaluated for 3 months after surgery.
Results
The surgical duration of E-NSM was significantly shorter in the S group than in the H group (P = 0.043) and T group (P = 0.037). However, the total surgical duration including E-NSM and breast reconstruction, and the total and daily drainage volume of postoperative seroma did not differ significantly among the 3 groups. Even when the energy devices were compared according to their working principle, i.e., ultrasonic (S and H) vs. hybrid (T), the total breast surgery duration and total and daily drainage volume of seroma showed no difference between the 2 groups. Although surgeon satisfaction did not significantly differ when using 3 devices for E-NSM (P = 0.428), surgeon’s fatigue was found to be lowest in the S group, though it was not significant (P = 0.064).
Conclusion
Any energy device can be safely used for E-NSM with breast reconstruction without causing any major complications. However, cordless ultrasonic energy devices allow greater mobility for the surgeon and, therefore, may shorten surgical time in breast surgery.
Keywords: Subcutaneous mastectomy, Surgical equipment, Wireless technology
INTRODUCTION
Minimally invasive breast surgery has become increasingly popular with the development of endoscopic or robotic surgery techniques [1,2]. Because minimally invasive surgery aims to provide a better cosmetic outcome with only a small incision, surgeons prefer using a robotic or an endoscopic instrument for this procedure. In particular, endoscopic nipple-sparing mastectomy (E-NSM) provides not only better cosmetic outcomes but also lower economic burden than robotic surgery because it only requires an endoscopic camera and energy device [3,4,5].
In E-NSM, an incision of 4–5 cm is made in the lateral or inframammary fold (IMF) with or without an axillary incision, which is also used for sentinel lymph node biopsy. Therefore, the lateral half of the breast can undergo open surgery without specific instruments. However, to perform surgery in the medial half of the breast, longer endoscopic or surgical instruments, an endoscopic camera, and energy devices are needed.
Commercial energy devices can be roughly classified into 3 types based on their working principles: ultrasonic, vessel sealing, and hybrid [6,7,8,9,10]. Because no large vessels are encountered in breast surgery except 1 or 2 internal thoracic arteries that run from the chest wall, the bipolar vessel sealer does not elicit a great advantage. Contrastingly, because the breast contains soft tissues including fat and parenchyma, an ultrasonic cutting energy device could be advantageous as it would cut through these tissues and reduce surgical time [11,12]. A hybrid energy device combines ultrasonic cutting with vessel sealing effects.
The authors compared 2 ultrasonic energy devices with a hybrid energy device to examine which device has superior safety and efficacy in breast surgery using E-NSM.
METHODS
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval for the study was obtained from the Institutional Review Board of the Kyungpook National University Chilgok Hospital (No. KNUCH 2020-12-002-002). Informed consent was obtained from all individual participants included in the study.
A total of 36 cases of breast reconstruction with E-NSM, performed between January 2017 and December 2021, were included in this study. The E-NSM was performed using 1 of the following 3 commercial energy devices: Sonicision (Medtronic; ultrasonic method; S group, n = 11), Harmonic (Ethicon Endo-Surgery, Inc.; ultrasonic method; H group, n = 6), and Thunderbeat (Olympus Corp.; hybrid method; T group, n = 19).
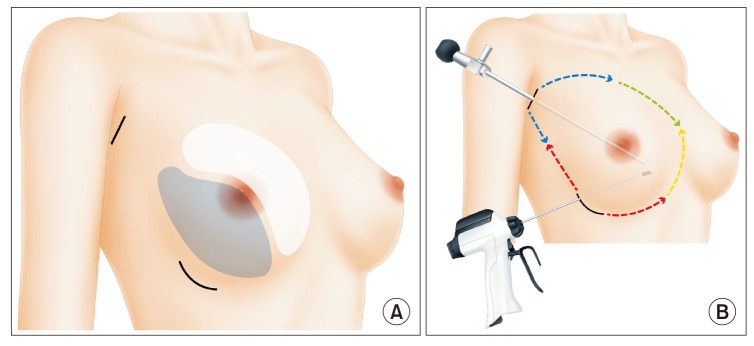
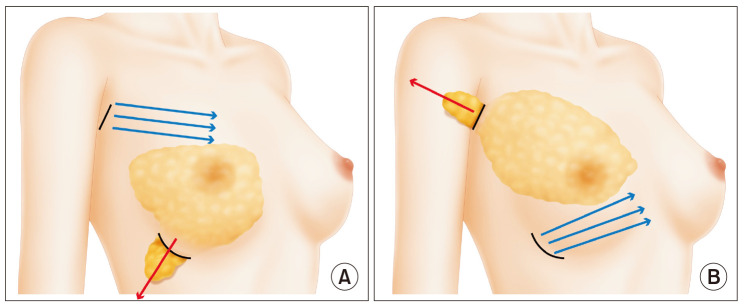
For E-NSM, a 5-cm incision was made in the IMF, and a 4-cm incision was made in the axillary line. Axillary surgery, such as a sentinel lymph node biopsy or axillary lymph node dissection, was performed according to the metastatic status of axillary lymph nodes. After axillary surgery was completed, the retromammary space was dissected using electrocautery or an energy device laterally to medially through both incisions. After the dissection of the retromammary space was completed, hydrodissection was performed along the superficial fascia layer of the breast with 300–400 mL of tumescent solution, which consists of normal saline (1,000 mL), 1% lidocaine (50 mL), and 1:1,000 epinephrine (1 mL), to prevent skin burn and bleeding. Thereafter, a blunt dissection with face-lifting scissors was performed according to the layer dissected using the tumescent solution. If necessary, the ductal tissue beneath the nipple was sent to a pathologist as a frozen section to evaluate whether the cancer involved the nipple. Both superficial and deep fasciae of the breast were separated from the skin and chest wall, and the lateral side was transected with electrocautery. When the transection along with breast parenchyma reached the medial side, where the specimen obscured the surgical field from the surgeon’s eyes, the endoscopic camera and energy device were employed. After completely separating the breast specimen from the skin and chest wall, the specimen was pulled out from the IMF incision, and the weight was calculated. Finally, the breast cavity was washed and any bleeding was checked and controlled with the energy device or a surgical tie (Figs. 1, 2).
Fig. 1. Surgical process of endoscopic nipple-sparing mastectomy (E-NSM). After dissection of the anterior and posterior aspects of the breast with tumescent solution and scissors, surgery was performed according to the red→blue→green→yellow process. (A) The incisions on the inframammary fold were 5 cm long, whereas those in the axillary area were 4 cm long. Although the inferior and lateral parts (blue area) of the breast can be removed by open surgery, the superior and medial parts (white area) of the breast require endoscopic surgery. (B) Green and yellow areas of the breast required visualization with the endoscopic camera and longer instruments for conducting E-NSM.
Fig. 2. Tips to secure a larger space in the breast cavity during endoscopic nipple-sparing mastectomy. The specimen can be pulled out through the opposite incision. (A) To create a larger space superiorly (blue arrows), the breast specimen can be pulled out (red arrow) through the inframammary fold incision (black line). (B) To secure a larger space inferiorly (blue arrows), the breast specimen can be pulled out (red arrow) through an axillary incision (black line).
After E-NSM with or without axillary surgery was completed, the plastic surgeon reconstructed the breast using an implant or an autologous latissimus dorsi muscle flap.
The patients’ medical records were reviewed and all clinical data, including the following, were collected: patient’s age, body mass index, bilaterality, location of breast cancer, clinical tumor stage, period of drainage tube placement in the breast, total and daily drainage volume, total and breast surgery time, postoperative complications, and additional treatment for breast cancer. Total drainage volume was calculated not only from the seroma that was obtained from the drainage bag but also from the seroma aspirated using a syringe in the outpatient clinic. The postoperative complications included nipple or skin necrosis and surgical site seroma; these were evaluated for 3 months after surgery. In addition, pathologic data including tumor type, pathologic tumor stage, and immunohistochemical staining results and subtypes were collated.
The statistical analysis was performed using IBM SPSS Statistics ver. 25.0 (IBM Corp.) and a P-value less than 0.05 was considered statistically significant. The abbreviated one-way analysis of variance, Kruskal-Wallis test, and Mann-Whitney test were applied to compare the 3 independent groups. Additionally, the chi-square test and Student t-test were used to analyze categorical and continuous data, respectively.
RESULTS
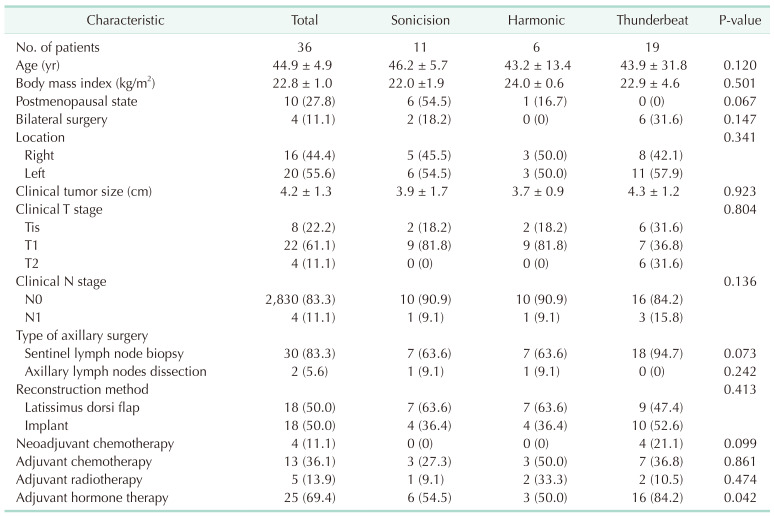
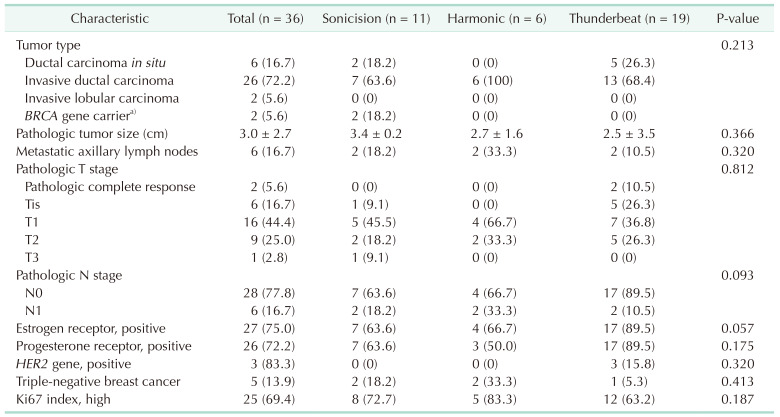
The mean age of the patients was 44.9 ± 4.9 years (mean ± standard deviation, for all subsequent data in the same format) and the mean body mass index was 22.8 ± 1.0 kg/m2. As noted in the methods, the patients were divided into 3 groups, namely S, H, and T groups, based on the energy device used in breast surgery. The 3 groups did not differ statistically in terms of clinical factors including the postmenopausal state, location of breast cancer, clinical tumor size and tumor stage, type of surgery, and additional treatments (Table 1). And there was no statistical difference in pathologic variables (Table 2).
Table 1. Clinical characteristics of breast cancer patients who received endoscopic nipple-sparing mastectomy using an energy device and immediate breast reconstruction.
Values are presented as number only, mean ± standard deviation, or number (%).
Sonicision, Medtronic; Harmonic, Ethicon Endo-Surgery, Inc.; Thunderbeat, Olympus Corp.
Table 2. Pathologic characteristics of breast cancer patients who received endoscopic nipple-sparing mastectomy using an energy device and immediate breast reconstruction.
Values are presented as number (%) or mean ± standard deviation.
Sonicision, Medtronic; Harmonic, Ethicon Endo-Surgery, Inc.; Thunderbeat, Olympus Corp.
a)Pathologic results were not available for BRCA gene carriers.
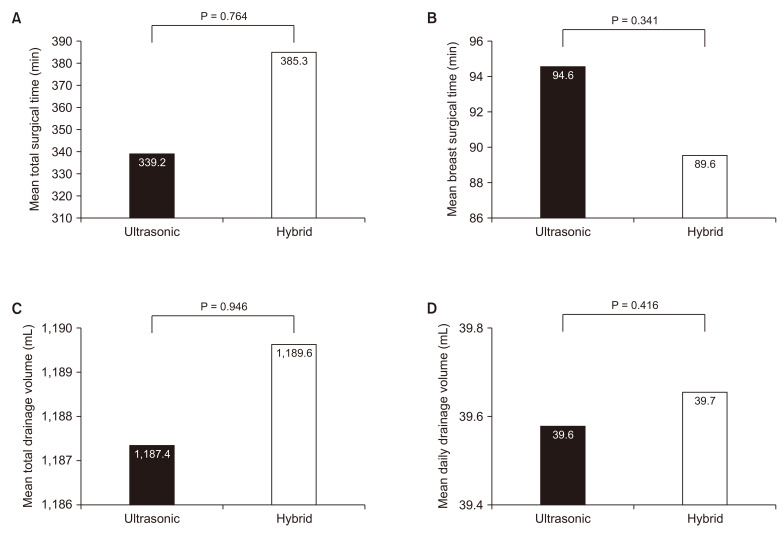
The mean period from surgery to the removal of the drainage tube was 9.4 ± 3.5 days, and the period was the shortest in the S group (8.9 ± 4.2 days) but did not differ significantly among the 3 groups (P = 0.512). The mean total drainage volume was 1,186.6 ± 1,411.4 mL, which included the seroma collected during hospital stay, after discharge, and in the outpatient clinic. The mean total and daily drainage volumes were comparable between the groups, and the mean total drainage volume did not differ significantly among 3 groups (P = 0.838). The mean total surgery duration including breast and reconstructive surgery was 363.5 ± 42.1 minutes, and there was no difference among the 3 groups in terms of the total surgical time (P = 0.867). The mean surgical time for breast surgery was 91.9 ± 36.8 minutes. Although the shortest time was noted in the S group (69.6 ± 9.9 minutes), the mean surgical duration for breast surgery did not differ significantly among the 3 groups (Table 3).
Table 3. Comparison of surgical parameters of breast cancer patients who received endoscopic nipple-sparing mastectomy using an energy device and immediate breast reconstruction.
Values are presented as mean ± standard deviation or number (%).
Sonicision, Medtronic; Harmonic, Ethicon Endo-Surgery, Inc.; Thunderbeat, Olympus Corp.
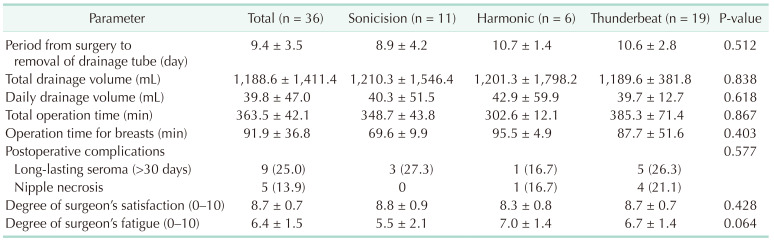
Thereafter, each group was compared with the other (S vs. H, H vs. T, S vs. T), and the results are shown in Fig. 1. The mean total surgical time did not differ significantly in any of the comparisons. Although the mean duration for breast surgery did not differ significantly in S vs. H and H vs. T, this duration was significantly shorter in the S group than in the H group (P = 0.043) and T group (P = 0.037). The mean total and daily drainage volumes of seroma did not show any statistical difference in the 2-by-2 comparisons of the S, H, and T groups (Fig. 3).
Fig. 3. The mean surgical duration and drainage volume of postoperative seroma. (A) The mean total surgical times among the Sonicision (S), Harmonic (H), and Thunderbeat (T) groups. (B) The mean breast surgery durations among the 3 groups. The S group showed a significantly shorter surgical duration than the other 2 groups (P = 0.043, P = 0.037). (C, D) The mean total drainage volume (C) and the mean daily drainage volume (D) of postoperative seroma among the 3 groups. Sonicision, Medtronic; Harmonic, Ethicon Endo-Surgery, Inc.; Thunderbeat, Olympus Corp.
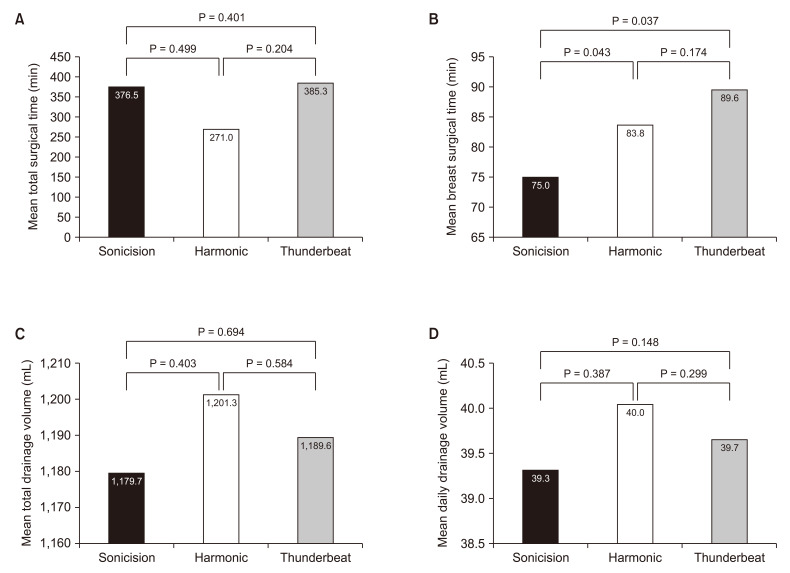
The mean total surgery and breast surgery durations did not differ significantly even when comparing groups based on the working principle of the energy devices (S and H vs. T). Furthermore, the mean total and daily drainage volumes of seroma did not differ between the groups wherein the ultrasonic energy device was used and the group wherein the hybrid energy device was used (Fig. 4).
Fig. 4. The mean surgical duration and drainage volume of postoperative seroma. There was no significant difference in these characteristics between ultrasonic and hybrid energy devices. Comparing the mean total surgical duration (A), mean breast surgical duration (B), mean total drainage volume of postoperative seroma (C), and mean daily drainage volume of postoperative seroma (D) between the 2 groups.
In surgeon’s satisfaction (score, 0–10) in the general process of surgery, there was no significant difference among 3 groups (S group: 8.8 ± 0.9, H group: 8.3 ± 0.8, and T group: 8.7 ± 0.7; P = 0.428). However, the surgeon’s fatigue was lowest in the S group (S group: 5.5 ± 2.1, H group: 7.0 ± 1.4, and T group: 6.7 ± 1.4; P = 0.064), even if there was no statistical significance (P = 0.064). There were no energy device-induced complications, such as skin burn injury or skin necrosis. Only long-lasting seroma (n = 9) and nipple necrosis (n = 5) were observed, and their incidence did not differ significantly among the 3 groups (Table 3).
DISCUSSION
Minimally invasive breast surgery is a trending topic in the field of breast cancer surgery [13,14]. Although the term “minimally invasive surgery” implies performing breast surgery with as small an incision as possible to obtain the best cosmetic outcome, it does not mean that the incisions are made so small that the conventional surgical objectives are compromised. Instead, the real objective of “minimally invasive breast surgery” is to use only small incisions and proper surgical instruments to maximize the cosmetic outcome and minimize harm, while improving the prognosis and reducing the surgical duration and complication risk in patients who undergo surgery for breast cancer.
Minimally invasive surgery is beneficial for the patient as well as the surgeon [15,16]. The conventional surgical techniques, though preferred by experts, could lead to the development of shoulder pain, neck pain, wrist pain, and fatigue in the surgeon. Minimally invasive surgery, however, employs endoscopic and robotic instruments and thus helps reduce the burden on the surgeon. This is why the development of minimally invasive breast surgery leads to the development of endoscopic and robotic instruments [1,2].
E-NSM can be performed using any conventional endoscopic surgical instrument and an energy device with a similar length. In particular, the energy device should be able to cut as well as electrically cauterize dense tissue to appropriately control the bleeding during surgery. Of the 2 types of energy devices, namely vessel sealers and ultrasonic energy devices, the latter are more suitable for use in breast surgery because, with the exception of the internal thoracic artery and vein, large blood vessels that may need sealing are rarely encountered in breast surgery. Previous studies have already proven that ultrasonic energy devices shorten the duration of breast surgery [17,18,19,20]. In the present study, the authors compared 2 ultrasonic cutting energy devices with an integrated, hybrid energy device that combines ultrasonic cutting and vessel sealing functions of energy devices. We found that the ultrasonic energy devices were more suitable than the hybrid device for E-NSM. While there was no difference in surgeons' overall satisfaction with surgeries using the 3 instruments, the lowest fatigue was observed in the S group, albeit not statistically significant. Although confirming statistical significance was challenging due to the small number of subjects in this study, the use of the cordless ultrasonic energy device (S group) showed potential for reducing surgical time and surgeon’s fatigue.
The total surgical time was calculated as the sum of breast surgery duration and reconstructive surgery duration, owing to which it was difficult to accurately analyze the influence of various reconstructive techniques, such as autologous or implant-based reconstruction, on the total surgery duration. However, when only considering the duration of breast surgery, ultrasonic devices showed somewhat better results than the hybrid device. In particular, the cordless ultrasonic energy device (Sonicision Curved Jaw Cordless Ultrasonic Dissection System, Medtronic) significantly shortened the operation time owing to its unlimited mobility in E-NSM, which is a procedure that requires the surgeon to change their position several times.
E-NSM is a minimally invasive surgery practiced by many breast surgeons. However, repetitive, and continuous changes in position during E-NSM may cause fatigue. Thus, safer and more convenient techniques are essential to reduce the physical burden on the surgeon. Although both ultrasonic and hybrid energy devices could be safely used in E-NSM in our study, the cordless ultrasonic energy device was more effective in reducing surgical time.
The limitations of this study are its small sample size, retrospective nature of the analysis, and non-randomized selection of participants. Nonetheless, this study could assess and compare the potential efficacies of various types of energy devices for E-NSM. Further multicenter clinical trials with larger populations are needed to corroborate our study’s results.
In conclusion, using a cordless ultrasonic energy device for E-NSM led to a shorter breast surgery duration than using regular ultrasonic or hybrid energy devices. However, because the difference was very subtle, it could relate less to the difference in the working principle and more to the cordless feature in Sonicision, which allowed the surgeon to move freely while performing E-NSM. Thus, this cordless type of energy device can be an appropriate option over other devices for surgeries like E-NSM that require the surgeon to frequently change positions.
Footnotes
Fund/Grant Support: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (2014R1A5A2009242, 2022R1F1A1072458) and this research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Ministry of Science & ICT (2017M3A9G8083382) and this work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2022R1I1A1A01070224). This research was also supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HR22C1832).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: BK, JL.
- Formal Analysis, Methodology: All authors.
- Investigation: JHJ, WWK, HK.
- Writing – Original Draft: BK, JL.
- Writing – Review & Editing: JHJ, HYP.
References
- 1.Schwartzberg BS, Goates JJ, Kelley WE. Minimal access breast surgery. Surg Clin North Am. 2000;80:1383–1398. doi: 10.1016/s0039-6109(05)70235-8. [DOI] [PubMed] [Google Scholar]
- 2.Mok CW, Lai HW. Evolution of minimal access breast surgery. Gland Surg. 2019;8:784–793. doi: 10.21037/gs.2019.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soybir G, Fukuma E. Endoscopy assisted oncoplastic breast surgery (EAOBS) J Breast Health. 2015;11:52–58. doi: 10.5152/tjbh.2015.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai HW, Chen ST, Tai CM, Lin SL, Lin YJ, Huang RH, et al. Robotic- versus endoscopic-assisted nipple-sparing mastectomy with immediate prosthesis breast reconstruction in the management of breast cancer: a case-control comparison study with analysis of clinical outcomes, learning curve, patient-reported aesthetic results, and medical cost. Ann Surg Oncol. 2020;27:2255–2268. doi: 10.1245/s10434-020-08223-0. [DOI] [PubMed] [Google Scholar]
- 5.Sakamoto N, Fukuma E, Higa K, Ozaki S, Sakamoto M, Abe S, et al. Early results of an endoscopic nipple-sparing mastectomy for breast cancer. Ann Surg Oncol. 2009;16:3406–3413. doi: 10.1245/s10434-009-0661-8. [DOI] [PubMed] [Google Scholar]
- 6.Cimino WW. Ultrasonic surgery: power quantification and efficiency optimization. Aesthet Surg J. 2001;21:233–241. doi: 10.1067/maj.2001.116006. [DOI] [PubMed] [Google Scholar]
- 7.Shabbir A, Dargan D. Advancement and benefit of energy sealing in minimally invasive surgery. Asian J Endosc Surg. 2014;7:95–101. doi: 10.1111/ases.12101. [DOI] [PubMed] [Google Scholar]
- 8.Sankaranarayanan G, Resapu RR, Jones DB, Schwaitzberg S, De S. Common uses and cited complications of energy in surgery. Surg Endosc. 2013;27:3056–3072. doi: 10.1007/s00464-013-2823-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang YW, Kim HS, Jung SP, Woo SU, Lee JB, Bae JW, et al. Comparison of skin-sparing mastectomy using LigaSure™ Small Jaw and electrocautery. World J Surg Oncol. 2017;15:129. doi: 10.1186/s12957-017-1199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrell AG, Kercher KW, Heniford BT. Energy sources in laparoscopy. Semin Laparosc Surg. 2004;11:201–209. doi: 10.1177/107155170401100310. [DOI] [PubMed] [Google Scholar]
- 11.Lee D, Jung BK, Roh TS, Kim YS. Ultrasonic dissection versus electrocautery for immediate prosthetic breast reconstruction. Arch Plast Surg. 2020;47:20–25. doi: 10.5999/aps.2019.00759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tupasi TE, Mangubat NV, Sunico ME, Magdangal DM, Navarro EE, Leonor ZA, et al. Malnutrition and acute respiratory tract infections in Filipino children. Rev Infect Dis. 1990;12 Suppl 8:S1047–S1054. doi: 10.1093/clinids/12.supplement_8.s1047. [DOI] [PubMed] [Google Scholar]
- 13.Lai HW, Chen ST, Lin YJ, Lin SL, Lin CM, Chen DR, et al. Minimal access (endoscopic and robotic) breast surgery in the surgical treatment of early breast cancer-trend and clinical outcome from a single-surgeon experience over 10 years. Front Oncol. 2021;11:739144. doi: 10.3389/fonc.2021.739144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kell MR, Sharma S. Minimally invasive, maximal outcomes in breast surgery. Surgeon. 2016;14:174–178. doi: 10.1016/j.surge.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Chang J, Rattner DW. History of minimally invasive surgical oncology. Surg Oncol Clin N Am. 2019;28:1–9. doi: 10.1016/j.soc.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Pawlik TM. Minimally invasive oncologic surgery, part II. Surg Oncol Clin N Am. 2019;28(Suppl 1):xiii–xxiv. doi: 10.1016/j.soc.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Patrone R, Gambardella C, Romano RM, Gugliemo C, Offi C, Andretta C, et al. The impact of the ultrasonic, bipolar and integrated energy devices in the adrenal gland surgery: literature review and our experience. BMC Surg. 2019;18(Suppl 1):123. doi: 10.1186/s12893-018-0457-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Back K, Hur N, Kim MJ, Choe JH, Kim JH, Kim JS. A prospective, randomized, controlled comparative study of three energy devices in open thyroid surgery: Thunderbeat, Harmonic, and Ligasure. J Endocr Surg. 2019;19:106–115. [Google Scholar]
- 19.Tou S, Malik AI, Wexner SD, Nelson RL. Energy source instruments for laparoscopic colectomy. Cochrane Database Syst Rev. 2011;(5):CD007886. doi: 10.1002/14651858.CD007886.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Harold KL, Pollinger H, Matthews BD, Kercher KW, Sing RF, Heniford BT. Comparison of ultrasonic energy, bipolar thermal energy, and vascular clips for the hemostasis of small-, medium-, and large-sized arteries. Surg Endosc. 2003;17:1228–1230. doi: 10.1007/s00464-002-8833-7. [DOI] [PubMed] [Google Scholar]