Abstract
A vertical root fracture (VRF) is a complex condition in which the fracture lines can be partial or complete and extend along the long axis of the tooth. Considering the nature of the damage and the low likelihood of a successful outcome, such fractures can be difficult to manage. Their management typically involves complex endodontic or surgical procedures, which can be technically challenging for general dentists.
Recent advancements introduce promising techniques, such as intentional replantation, adhesive methodologies, and regenerative procedures, showcasing potential in salvaging teeth affected by VRFs. Nonetheless, the imprecise nature of symptoms necessitates meticulous case evaluation by clinicians. Comprehensive patient counseling regarding diverse treatment options and potential ramifications remains crucial to preserving the affected tooth. Preserving a vertically fractured tooth aids in improving both function and aesthetics while safeguarding the arch’s integrity by maintaining the height of the alveolar bone. It is important to note that the success of the treatment procedures depends on the extent and location of the fracture, the condition of the tooth and fragment, and the skill of the dental professional performing the treatment.
This review highlights the complexity of VRF management, emphasizing the necessity for precise evaluation, patient education, and the exploration of innovative techniques. It aims to review the treatment of VRFs, ranging from classical to contemporary methods, with a focus on tooth preservation.
The establishment of standardized protocols and conduct of further research to ascertain long-term efficacy are imperative in optimizing outcomes and retaining natural dentition in cases of VRFs.
Keywords: Fracture Healing, Tooth Replantation, Vertical Dimension
Background
Among the 5 types of tooth fractures, a vertical root fracture (VRF) begins as a rupture in the root that extends coronally from the apex in an oblique or longitudinal manner [1,2]. This fracture can develop after root canal therapy, leading to tooth or root extraction [3,4]. Although VRFs have various etiologies, important clinical factors include the patient’s age and the type of tooth involved [5]. There are also known risk factors, such as excessive removal of healthy dentin during root canal treatment, prolonged contact with intracanal disinfectants and medicaments, and improper placement of post-endodontic restorations [6]. Among teeth that have undergone root canal treatment, the incidence of VRFs ranges from 4% to 32% [6], and 80% of VRFs are typically detected within 2 years after the onset of initial symptoms [7].
Significant symptoms associated with VRFs include the presence of a sinus tract, increased probing depth, swelling/abscess formation, and tenderness to percussion [8]. In addition to clinical assessments, radiographic methods can facilitate the diagnosis of VRFs, although some fractures may not be visible on radiographs. Periapical radiography is commonly used to diagnose root fractures, but its 2-dimensional nature can lead to anatomical noise and distortion. In contrast, cone-beam computed tomography provides 3-dimensional images with reduced noise and distortion, offering superior accuracy in the detection of VRFs, compared with periapical radiography [9].
Because VRFs constitute a major challenge for endodontists, there has been extensive debate regarding suitable treatment options. Although many studies have been conducted, the choice of VRF treatment method depends on the clinician’s experience and the clinical features in each case. Extraction is the typical course of action for teeth with VRFs; however, recent reports of alternative strategies have demonstrated short-term success regarding tooth preservation [10]. A multi-disciplinary approach involving endodontic, periodontic, orthodontic, prosthodontic, and surgical interventions can be required [1].
This article aims to review the treatment of VRFs, ranging from classical to contemporary methods, with a focus on tooth preservation. In many cases of VRFs, extraction is required; therefore, this too will be described.
VRF Treatment Approaches
There are diverse treatment approaches for VRFs. Table 1 describes these approaches, along with their advantages and disadvantages. In this review, we focus on 5 key aspects of the treatment approaches listed in Table 1: root amputation, root resection, or hemisection [11,12]; laser-mediated VRF fusion [13,14]; whether calcium hydroxide dressing aids healing or causes damage [15]; fracture line bonding (with or without intentional replantation) [15–18]; and tooth extraction [6,19].
Table 1.
Treatment approaches for vertical root fractures.
| Treatment modality | Description | Advantages | Disadvantages |
|---|---|---|---|
| No treatment, just observation with monitoring | Following the actual clinical condition without taking any step in the treatment | Least invasive option, allows assessment of the fracture’s stability | Tooth may become symptomatic or fail. Typically leads to tooth loss due to infection or complications |
| Root resection and root amputation | Removing apex of a tooth’s root, or the whole root of multi-rooted teeth | Tooth preservation, maintains the bone density, restores the function and is an alternative to extraction | Complex procedure, risk of residual infection which leads to limited success. Requires surgical skills |
| Hemisection | The surgical removal of one-half of a tooth, typically in multi-rooted teeth | Can save one portion of the tooth, cost-effective, conservation of healthy roots | May result in a gap if one portion is extracted, also it is a complex procedure |
| Laser fusion of vertical root fracture | Sealing the fracture line while generating thermal energy | Better alternative than extraction and no treatment | Is not a widely recognized or established dental procedure |
| Re-cementing, bonding or sealing the fractured fragment | Closing the fracture line with different approaches, with the aim of saving the tooth and sealing the fracture line so the bacteria does not enter | Minimally invasive, compared with resection and hemisection, even though it is often combined with these procedures. Cost-effective and preserves the tooth | Complex procedure, Requires good surgical skills and healthy periradicular tissues, some bacteria can remain within the fracture lines |
| Intentional replantation | Tooth is intentionally removed from its socket, treated or repaired, and then replanted back into its original position in the patient’s mouth | Preservation of natural tooth, less invasive than dental implants and requires fewer dental appointments | Risk of complications, success rates vary, potential for reinfection, risk of root resorption, not suitable for all cases |
| Prosthodontic rehabilitation (partial denture or bridge) | Focused on restoring or replacing missing teeth and associated oral structures to enhance oral function, aesthetics, and overall well-being | Provides a functional and aesthetic replacement of the lost tooth as a result of vertical root fracture | Alteration of adjacent healthy teeth, not suitable for single-tooth replacements, potential for discomfort or instability |
| Tooth extraction and implant placement | The most common treatment in vertical root fracture cases | Removes the source of infection and brings back the tooth function | Loss of the natural tooth and extra cost for the implant |
Treatment is intended to preserve the health and function of teeth with VRF, primarily in cases of partial VRF. Two goals of optimal treatment are eliminating microbial invasion at the fracture line and preventing periodontal tissue loss [6]. However, the treatment of VRFs can be challenging, as shown in Figure 1.
Figure 1.
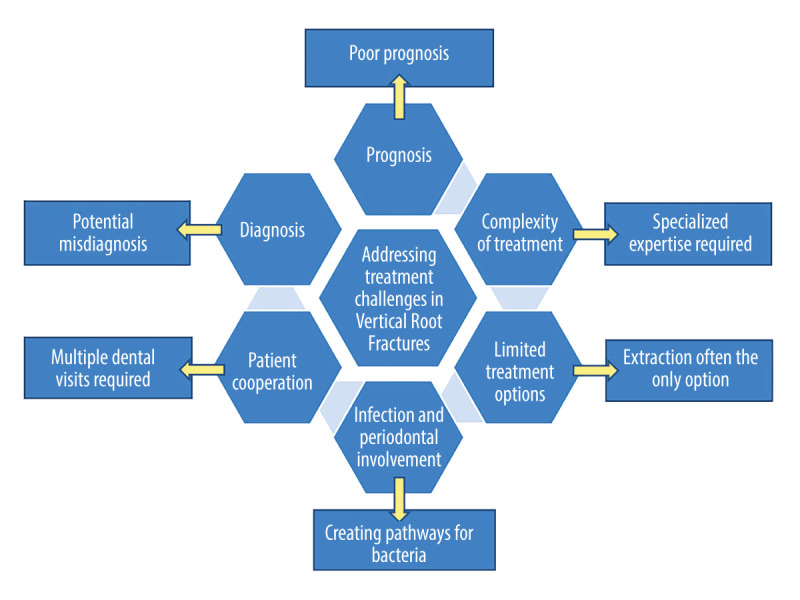
Chart illustrating the challenges encountered during vertical root fracture treatment.
Root Amputation, Root Resection, or Hemisection
Root amputation, usually involving maxillary molars, comprises removal of the root at its furcation or apex, without removing the crown. Root resection is generally regarded as removal of the root, regardless of crown treatment [20]. A multi-rooted tooth requires surgical division up to the furcation, which allows removal of the root and overlying anatomic crown. This procedure, known as root hemisection, is intended to preserve as much of the original tooth anatomy as possible [21].
For molars with periodontal, endodontic, restorative, or prosthetic problems, root resection therapy is a possible treatment option. Although the most common indications for root resection are periodontal-based, our discussion focuses on endodontic indications, such as an unfillable canal, root fracture, root perforation, root resorption, and root decay [22]. Root resection therapy can provide good outcomes in cases of incomplete fracture [23]. In a protocol for the treatment of incomplete VRFs, Taschieri [24] proposed removing the fractured apical segment of the root via resection. The residual fracture groove can then be prepared using a bur and sealed with mineral trioxide aggregate (MTA) [23,24]. According to Anitha and Rao [12], root resection involving removal of the entire fractured root fragment can facilitate retention of the remaining tooth. However, they note that long-term success requires careful case selection to ensure that the remaining root exhibits a robust periodontal status and can be sufficiently restored [12]. Other case selection approaches, based on a strict set of criteria [25], such as surgical performance, periodontal disease, endodontic therapy, oral hygiene, and high patient motivation, can ensure treatment success [12,21].
The surgical method of Anitha and Rao [12] led to a successful outcome in a patient with pain caused by vertical fracture of the mesial root in the lower right first molar. This result demonstrates that hemisection is an effective method of VRF treatment. In this instance, the 3-year follow-up visit revealed good oral hygiene and no patient concerns, indicating that hemisection can be an alternative to extraction for some patients with VRF who exhibit a suitable oral environment, along with the ability and desire to practice good oral hygiene.
It is important to consider the risk of surgical treatment for VRFs. After resection or hemisection of a fractured root, especially a resected root without root-end filling [26], the affected tooth may not tolerate pressure, leading to vertical fracture of the remaining root. Ayrancı et al [27] reported that apical resection does not reduce the fracture resistance of a tooth. However, the current literature supports the approach of allowing each patient to select the desired treatment option after they have received information regarding the advantages and disadvantages of surgical treatment for VRFs.
Laser-Mediated VRF Fusion
The effectiveness of laser treatment for VRFs has been investigated since the 1980s. Although successful outcomes have been reported, there are doubts about the efficiency of this technique and its influencing factors. Because the working principle of the carbon dioxide (CO2) laser is based on the short-term generation of intense heat, such a laser can sterilize and seal a vertical fracture that is a serious threat to the tooth. However, it remains unclear whether treatment success is the result of sterilization or the sealing effect [14]. There is some concern about the use of intense heat in pulp tissue [28]. In most cases, vertical fractures occur in non-vital teeth that have undergone endodontic treatment [29]. However, exposure of the vital pulp to intense heat should not be problematic if the remaining dentin thickness is at least 1 mm [30].
Factors that contribute to the success of this technique include a full-coverage cast crown restoration, which can promote mechanical stabilization of the fracture. Additionally, fractures that appear thin and well-approximated are more likely to be successfully fused with a CO2 laser, compared with fractures that exhibit large gaps [14]. Fractures with perpendicular access for the entire length are preferred [14], because proper laser beam exposure requires this type of access to the root surface [31]. Radiographic evidence of periapical bone loss is not required in endodontically treated teeth, implying the success of previous endodontic therapy [14].
Despite the questionable effect of the CO2 laser in VRF treatment, a 1996 study of the effects of CO2 and neodymium-doped yttrium aluminum garnet (Nd: YAG) lasers on 81 single-rooted teeth with induced root fracture revealed that the Nd: YAG laser was not effective in terms of fracture line fusion. The main finding in teeth treated with this laser was surface ablation, whereas the CO2 laser demonstrated greater effectiveness [32].
Whether Calcium Hydroxide Dressing Aids Healing or Causes Damage
A 1988 study by Stewart indicated that the intracanalicular use of calcium hydroxide dressing facilitates successful treatment of VRF over 9 to 12 months [33]. However, the results of in vitro studies suggested that teeth with long-term dressings can demonstrate an increased predisposition to root fracture [34]. For example, a 2006 study by Rosenberg et al revealed that dentin was weakened by 23% to 43.9% after root canal filling with calcium hydroxide [35]. Conversely, more recent studies have shown that calcium hydroxide products do not increase the predisposition to root fracture [36], and that thin and fragile roots can contribute to fracture [34]. Notably, calcium hydroxide dressings are effective in the management of horizontal root fractures [37], although such fractures are outside the scope of this review.
Fracture Line Bonding (With or Without Intentional Replantation)
There are several options for joining fractured fragments: solely inside the canal (intracanalicular); with external flap elevation; and through a combination of internal root canal preparation plus tooth extraction to allow external fracture line bonding and sealing, followed by intentional replantation [38]. Each bonding and sealing method requires various materials, including 4-methacryloxyethyl trimellitate anhydride in methyl methacrylate initiated by tri-n-butyl borane (4-META/MMA-TBB) resin cements [38,39], dual-curing resin cements [16], amalgam, ethoxy benzoic acid cement, MTA [40], and biodentine [41,42].
The intracanalicular approach of vertical fracture bonding is supported by many authors [43,44]. However, these authors have consistently stated that the entire fracture line cannot be reached; therefore, some bacteria can persistent within the fracture line, leading to treatment failure [38]. There have been various reports of successful VRF treatment with 4-META/MMA-TBB resin bonding through the root canal [43]. It is important to note that the prognosis of VRF treatment with intracanal access is better for vertical fractures detected at an early stage, prior to periodontal status disruption [38]. In a case report by Baranwal et al [44], the authors used universal dentin bonding and flowable composite to join the separated fragments in the crown region. After chemical and mechanical preparation of the canal, followed by drying, they placed biodentine in the apical part of the canal using a Lentulo spiral filler, then continued with other restorative procedures. The 24-month follow-up examination showed signs of successful treatment [44].
Regarding external treatment of fractured teeth, flap elevation without tooth extraction results in the inability to reach some fracture lines, leading to bacterial colonization in those lines [38]. Additionally, some portions of alveolar bone must be removed to access the fracture lines. Therefore, this removal of hard and soft periodontal tissues, which exposes the support apparatus of the fractured tooth, can reduce treatment success [45]. Intentional replantation is an ideal alternative treatment option that rarely compromises periodontal bone architecture [46].
The remaining option for vertical fracture management consists of tooth extraction, followed by external repair, and then intentional replantation. This method is advantageous in that it provides a 3-dimensional approach to the fractured tooth, enabling the removal of contaminated dentin and cement; all fractured surfaces can be cleaned and sealed with the selected material [38]. There have been multiple reports of successful VRF treatment with bonding and replantation involving frontal teeth [16,39,47]. Good results have also been achieved in posterior teeth, especially molars with 2 or more roots [38]. Substantial success was reported in the treatment of 6 teeth with VRFs (1 incisor, 1 canine, 1 premolar, and 3 molars) in 6 patients. In those teeth, the fracture lines were prepared and sealed with 4-META/MMA-TBB resin; the apical third was filled with MTA if necessary. When the fractured teeth exhibited roots that had been split in half, both fragments were extracted and carefully cleaned. The contaminated cement and dentin were removed with high-speed round burs or ultrasonic equipment with a water spraying system under a stereomicroscope. Subsequently, the root segments were cemented with 4-META/MMA-TBB resin. The attached tooth was then cleaned with saline. After removal of the periradicular granulation tissue, the tooth was carefully replanted into the alveolus [38].
It is important to mention the successful outcomes reported by Moradi Majd et al [16] during the treatment of vertical fracture in an upper left central incisor, with the aid of intentional replantation. Those authors performed careful tooth extraction, followed by minimal preparation of the fracture line and filling with dual-curing resin; next, they conducted root-end resection and prepared a retrograde cavity, which was then filled with calcium-enriched mixture cement. After this treatment, the tooth was replanted in its original position. The procedure duration was 18 min. After replantation, the tooth was immobilized for 10 days using a semirigid splint. At the 12-month follow-up visit, the tooth was asymptomatic, and periapical radiolucency was reduced [16].
Despite the reported success of intentional replantation in cases of VRF, many clinicians support extraction and subsequent replacement with an implant. Although the rate of implant survival is increasing, intentional replantation remains a more economical treatment approach. Therefore, intentional replantation should be the initial treatment option; if replantation fails, implant placement remains possible [48]. There is evidence that intentional replantation can preserve a fractured tooth through the incorporation of biomaterials, such as MTA and leukocyte-platelet rich fibrin [49]. However, root resorption is a persistent problem after intentional replantation [50].
Tooth Extraction
Discussion related to VRF refers to a crack that starts in the root of the tooth (Figure 2).
Figure 2.
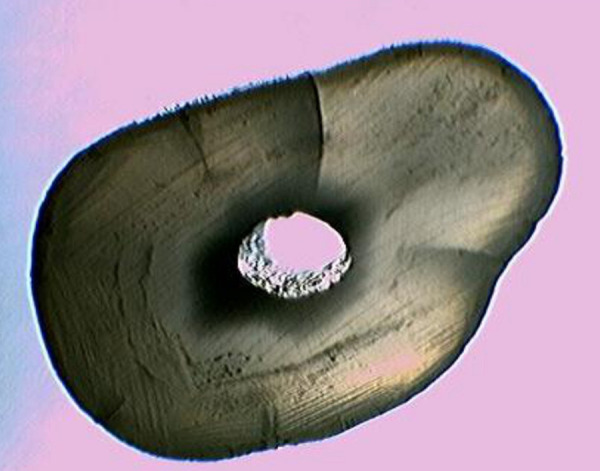
Cross sectional section of cracked root after stereomicroscopic observation.
In most cases, extraction remains the treatment of choice for VRF, especially in the context of complete fractures [6]. An intraosseous fracture with periodontal pain, often involving the mesial and distal aspects of the tooth, is an indication for extraction [1]. This treatment option is intended to prevent the destruction of the bone and periradicular tissue, which would hinder prosthetic or implant-based replacement of the lost tooth [6]. In some cases, VRF-induced periodontal bone destruction leads to the formation of a deep bone dehiscence. This situation is an indication for extraction and replacement with an implant, with increasing assistance from connective tissue grafts, which have demonstrated promising results in terms of periodontal defect replacement and implant therapy [51]. Because tooth extraction is the final treatment option, a correct diagnosis is essential before selecting this option. Vertical fractures are often included in the differential diagnosis for cemental tears; however, both of these conditions can cause extensive periodontal bone loss and serve as an indication for extraction [52].
Future Directions
Management of a tooth fracture requires an accurate diagnosis, treatment planning, and regular follow-up visits [53]. Therefore, preventing VRF of a tooth requires carefully assessing the occlusal scheme, avoiding deflective contacts, and determining parafunctional habits, as well as giving importance to access cavity design and endodontic and post-endodontic procedures [54]. Clinical detection of this condition by endodontists is becoming more common, whereas it is rather underestimated by general practitioners [55].
The future of VRF treatment is poised for advancements driven by technological innovations and a deeper understanding of dental biomechanics. However, more studies are required for exact VRF diagnosis and management.
Conclusions
Teeth with VRFs require treatments to alleviate pain, prevent infection, preserve function, maintain aesthetics, protect overall oral health, prevent complications, facilitate future alternative therapeutic options, and improve patient comfort and confidence. Individuals with such fractures should seek timely dental care to effectively address these concerns. Depending on the clinical picture, the management of VRFs can involve both options (treatment and no treatment), as discussed below.
Treatment can be considered in cases of incomplete fracture, involving cooperative patients who desire to preserve the natural tooth. A key consideration regarding the decision to treat VRFs is the patient’s periodontal status. Therefore, it is appropriate to treat VRFs in cases of intact periodontal status, in which the bone is preserved and the overall prognosis is good.
Extraction is suitable in cases of VRFs that approach a diagnosis of a split tooth, in which the bone and periodontal tissues do not suggest the natural tooth can be preserved, and no other treatment methods would lead to a good overall prognosis. Additionally, VRFs associated with severe chronic infections can be challenging to treat because of their tendency to erode bone surrounding the tooth, decreasing support for future dental implants. For patients with systemic health problems, considering the complexity of other surgical and non-surgical methods, along with their risk of infection, extraction remains the simplest choice.
Overall, the best treatment is prevention. Root fractures can be avoided by identifying susceptible teeth and roots, choosing appropriate dowels and cementing them properly, and avoiding the use of excessive force when removing tooth structures in endodontic and prosthetic procedures, as well as during gutta-percha condensation.
Acknowledgments
We thank Ryan Chastain-Gross, PhD, from Edanz (https://www.edanz.com/ac) for editing a draft of this manuscript.
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Kahler W. The cracked tooth conundrum: terminology, classification, diagnosis, and management. Am J Dent. 2008;21(5):275–82. [PubMed] [Google Scholar]
- 2.Tamse A, Fuss Z, Lustig J, Kaplavi J. An evaluation of endodontically treated vertically fractured teeth. J Endod. 1999;25(7):506–8. doi: 10.1016/S0099-2399(99)80292-1. [DOI] [PubMed] [Google Scholar]
- 3.Haueisen H, Gärtner K, Kaiser L, et al. Vertical root fracture: Prevalence, etiology, and diagnosis. Quintessence Int. 2013;44(7):467–74. doi: 10.3290/j.qi.a29715. [DOI] [PubMed] [Google Scholar]
- 4.Tamse A. Vertical root fractures in endodontically treated teeth: diagnostic signs and clinical management. Endod Topics. 2006;13:84–94. [Google Scholar]
- 5.Hsiao LT, Ho JC, Huang CF, et al. Analysis of clinical associated factors of vertical root fracture cases found in endodontic surgery. J Dent Sci. 2020;15(2):200–6. doi: 10.1016/j.jds.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel S, Bhuva B, Bose R. Present status and future directions: Vertical root fractures in root filled teeth. Int Endod J. 2022;55(Suppl 3):804–26. doi: 10.1111/iej.13737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshino K, Ito K, Kuroda M, Sugihara N. Duration from initial symptoms to diagnosis of vertical root fracture in dental offices. Bull Tokyo Dent Coll. 2018;59(1):59–61. doi: 10.2209/tdcpublication.2016-0049. [DOI] [PubMed] [Google Scholar]
- 8.Haupt F, Wiegand A, Kanzow P. Risk factors for and clinical presentations indicative of vertical root fracture in endodontically treated teeth: A systematic review and meta-analysis. J Endod. 2023;49(8):940–52. doi: 10.1016/j.joen.2023.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Mizuhashi F, Watarai Y, Ogura I. Diagnosis of vertical root fractures in endodontically treated teeth by cone-beam computed tomography. J Imaging. 2022;8(3):51. doi: 10.3390/jimaging8030051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen S, Arola D, Ricucci D, et al. Biomechanical perspectives on dentine cracks and fractures: Implications in their clinical management. J Dent. 2023;130:104424. doi: 10.1016/j.jdent.2023.104424. [DOI] [PubMed] [Google Scholar]
- 11.Setzer FC, Shou H, Kulwattanaporn P, et al. Outcome of crown and root resection: A systematic review and meta-analysis of the literature. J Endod. 2019;45(1):6–19. doi: 10.1016/j.joen.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Anitha S, Rao DS. Hemisection: A treatment option for an endodontically treated molar with vertical root fracture. J Contemp Dent Pract. 2015;16(2):163–65. doi: 10.5005/jp-journals-10024-1654. [DOI] [PubMed] [Google Scholar]
- 13.Khallaf ME, Saadony DM. Comparative study of diode lasers used for two time intervals for the treatment of teeth with vertical root fractures. J Arab Soc Med Res. 2019;14:57–61. [Google Scholar]
- 14.Dederich DN. CO2 laser fusion of a vertical root fracture. J Am Dent Assoc. 1999;130(8):1195–99. doi: 10.14219/jada.archive.1999.0374. [DOI] [PubMed] [Google Scholar]
- 15.Liao WC, Chen CH, Pan YH, et al. Vertical root fracture in non-endodontically and endodontically treated teeth: Current understanding and future challenge. J Pers Med. 2021;11(12):1375. doi: 10.3390/jpm11121375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moradi Majd N, Akhtari F, Araghi S, Homayouni H. Treatment of a vertical root fracture using dual-curing resin cement: A case report. Case Rep Dent. 2012;2012:985215. doi: 10.1155/2012/985215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakagawa K, Saita M, Ikeda T, et al. Biocompatibility of 4-META/MMA-TBB resin used as a dental luting agent. J Prosthet Dent. 2015;114(1):114–21. doi: 10.1016/j.prosdent.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 18.von Arx T, Bosshardt D. Vertical root fractures of endodontically treated posterior teeth: A histologic analysis with clinical and radiographic correlates. Swiss Dent J. 2017;127(1):14–23. doi: 10.61872/sdj-2017-01-233. [DOI] [PubMed] [Google Scholar]
- 19.Berman LH, Hargreaves KM, Rotstein I. Cohen’s pathways of the pulp. 12th edition. Elsevier; 2021. [Google Scholar]
- 20.Pal M, Kumar S, Pratibha G. Root resection – exploring ways beyond extraction. Indian J Dent Res. 2020;31(5):819–23. doi: 10.4103/ijdr.IJDR_91_18. [DOI] [PubMed] [Google Scholar]
- 21.Hanafi L. An approach of preserving a mandibular primary second molar by a hemisection procedure: A case report with 36-month follow up. Heliyon. 2022;8(9):e10655. doi: 10.1016/j.heliyon.2022.e10655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pai AV, Khosla M. Root resection under the surgical field employed for extraction of impacted tooth and management of external resorption. J Conserv Dent. 2012;15(3):298–302. doi: 10.4103/0972-0707.97966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taschieri S, Del Fabbro M, El Kabbaney A, et al. Microsurgical re-treatment of an endodontically treated tooth with an apically located incomplete vertical root fracture: A clinical case report. Restor Dent Endod. 2016;41(4):316–21. doi: 10.5395/rde.2016.41.4.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taschieri S, Tamse A, Del Fabbro M, et al. A new surgical technique for preservation of endodontically treated teeth with coronally located vertical root fractures: A prospective case series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(6):e45–52. doi: 10.1016/j.tripleo.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 25.Kurtzman GM, Silverstein LH, Shatz PC. Hemisection as an alternative treatment for vertically fractured mandibular molars. Compend Contin Educ Dent. 2006;27(2):126–29. [PubMed] [Google Scholar]
- 26.Penmatsa P, Boddeda M, Mandava J, et al. An in-vitro fracture strength assessment of endodontically treated teeth with different root-end materials. Eur Endod J. 2021;6(3):319–24. doi: 10.14744/eej.2021.55265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ayrancı F, Ayrancı LB, Özdoğan A, et al. Resistance to vertical root fracture of apicoected teeth using different devices during two root canal irrigation procedures. Lasers Med Sci. 2018;33(8):1685–91. doi: 10.1007/s10103-018-2517-6. [DOI] [PubMed] [Google Scholar]
- 28.Anagnostaki E, Mylona V, Parker S, et al. Systematic review on the role of lasers in endodontic therapy: valuable adjunct treatment? Dent J (Basel) 2020;8(3):63. doi: 10.3390/dj8030063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim MJ, Kim JA, Choi Y, et al. Differentiating spontaneous vertical root fracture in endodontically treated tooth. Eur J Dent. 2017;11(1):122–25. doi: 10.4103/ejd.ejd_160_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Umana M, Heysselaer D, Tielemans M, et al. Dentinal tubules sealing by means of diode lasers (810 and 980 nm): A preliminary in vitro study. Photomed Laser Surg. 2013;31(7):307–14. doi: 10.1089/pho.2012.3443. [DOI] [PubMed] [Google Scholar]
- 31.Teo CY, George R, Walsh LJ. Dispersion of near-infrared laser energy through radicular dentine when using plain or conical tips. Lasers Med Sci. 2018;33:251–55. doi: 10.1007/s10103-017-2352-1. [DOI] [PubMed] [Google Scholar]
- 32.Arakawa S, Cobb CM, Rapley JW, et al. Treatment of root fracture by CO2 and Nd: YAG lasers: An in vitro study. J Endod. 1996;22(12):662–67. doi: 10.1016/S0099-2399(96)80060-4. [DOI] [PubMed] [Google Scholar]
- 33.Stewart GG. The detection and treatment of vertical root fractures. J Endod. 1988;14(1):47–53. doi: 10.1016/S0099-2399(88)80242-5. [DOI] [PubMed] [Google Scholar]
- 34.Kahler SL, Shetty S, Andreasen FM, Kahler B. The effect of long-term dressing with calcium hydroxide on the fracture susceptibility of teeth. J Endod. 2018;44(3):464–69. doi: 10.1016/j.joen.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 35.Rosenberg B, Murray PE, Namerow K. The effect of calcium hydroxide root filling on dentin fracture strength. Dent Traumatol. 2007;23(1):26–29. doi: 10.1111/j.1600-9657.2006.00453.x. [DOI] [PubMed] [Google Scholar]
- 36.Karapinar-Kazandag M, Basrani B, Tom-Kun Yamagishi V, et al. Fracture resistance of simulated immature tooth roots reinforced with MTA or restorative materials. Dent Traumatol. 2016;32(2):146–52. doi: 10.1111/edt.12230. [DOI] [PubMed] [Google Scholar]
- 37.Aguiar CM, Mendes D, Camara AC. Horizontal root fracture in a maxillary central incisor: A case report. Gen Dent. 2013;61(2):12–14. [PubMed] [Google Scholar]
- 38.Okaguchi M, Kuo T, Ho YC. Successful treatment of vertical root fracture through intentional replantation and root fragment bonding with 4-META/MMA-TBB resin. J Formos Med Assoc. 2019;118(3):671–78. doi: 10.1016/j.jfma.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 39.Nizam N, Kaval ME, Gürlek Ö, et al. Intentional replantation of adhesively reattached vertically fractured maxillary single-rooted teeth. Int Endod J. 2016;49(3):227–36. doi: 10.1111/iej.12444. [DOI] [PubMed] [Google Scholar]
- 40.Gurtu A, Roy S, Chandra P, Bansal R. Reattachment of complex fractures; A reality by advances in self-etch bonding systems. Indian J Dent Res. 2019;30(1):135–39. doi: 10.4103/ijdr.IJDR_643_16. [DOI] [PubMed] [Google Scholar]
- 41.Tang JJ, Shen ZS, Qin W, Lin Z. A comparison of the sealing abilities between Biodentine and MTA as root-end filling materials and their effects on bone healing in dogs after periradicular surgery. J Appl Oral Sci. 2019;27:e20180693. doi: 10.1590/1678-7757-2018-0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hadrossek PH, Dammaschke T. New treatment option for an incomplete vertical root fracture – a preliminary case report. Head Face Med. 2014;10:9. doi: 10.1186/1746-160X-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sugaya T, Natatsuka M, Motoki Y, et al. Sealing the gap of vertical root fracture through the root canal. Dentistry. 2016;6:354. [Google Scholar]
- 44.Baranwal HC, Singh N, Kumar N, et al. New approach in the management of vertical root fracture with the help of biodentine and CBCT. Case Rep Dent. 2020;2020:2806324. doi: 10.1155/2020/2806324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sugaya T, Tomita M, Motoki Y, et al. Periodontal tissue repair after sealing of the gap in vertical root fracture. Odontology. 2017;105:202–7. doi: 10.1007/s10266-016-0270-5. [DOI] [PubMed] [Google Scholar]
- 46.Yang Y, Zhang B, Huang C, Ye R. Intentional replantation of a second premolar with internal resorption and root fracture: A case report. J Contemp Dent Pract. 2021;22(5):562–67. [PubMed] [Google Scholar]
- 47.Arikan F, Franko M, Gürkan A. Replantation of a vertically fractured maxillary central incisor after repair with adhesive resin. Int Endod J. 2008;41(2):173–79. doi: 10.1111/j.1365-2591.2007.01334.x. [DOI] [PubMed] [Google Scholar]
- 48.Mainkar A. A systematic review of the survival of teeth intentionally replanted with a modern technique and cost-effectiveness compared with single-tooth implants. J Endod. 2017;43(12):1963–68. doi: 10.1016/j.joen.2017.08.019. [DOI] [PubMed] [Google Scholar]
- 49.Praveen Kumar V, Sadasiva K, Raj Kumar J, et al. Current trends in intentional replantation treatment among endodontists and postgraduate students in India, the United States of America, and the United Kingdom: A cross-sectional study. Cureus. 2023;15(5):e39742. doi: 10.7759/cureus.39742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Santos JM, Marques JA, Esteves M, et al. Intentional replantation as a starting approach for a multidisciplinary treatment of a mandibular second molar: A case report. J Clin Med. 2022;11(17):5111. doi: 10.3390/jcm11175111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tirone F, Genovesi F. Immediate implant placement and loading in the esthetic area when the buccal socket wall is significantly damaged. J Esthet Restor Dent. 2021;33(4):542–49. doi: 10.1111/jerd.12707. [DOI] [PubMed] [Google Scholar]
- 52.Pedercini A, Weitz DF, Heyse JD, Jr, et al. Cemental tear: An overlooked finding associated with rapid periodontal destruction. A case series. Aust Dent J. 2021;66(Suppl 1):S82–S87. doi: 10.1111/adj.12844. [DOI] [PubMed] [Google Scholar]
- 53.Patnana AK, Kanchan T. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2023. Tooth fracture. [PubMed] [Google Scholar]
- 54.Patel Sh, Bhuva B, Bose R. Present status and future directions: vertical root fractures in root filled teeth. Int Endod J. 2022;55(53):804–26. doi: 10.1111/iej.13737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khasnis SA, Kidiyoor KH, Patil AB, Kenganal SB. Vertical root fractures and their management. J Conserv Dent. 2014;17(2):103–10. doi: 10.4103/0972-0707.128034. [DOI] [PMC free article] [PubMed] [Google Scholar]


