Abstract
Background:
Dietary pattern may be one of the determinants of cardiovascular health. This study aimed to examine the relationship between a heart-healthy diet, the phytochemical content of a diet, and Mediterranean diet and cardiovascular disease (CVD) risks.
Methods:
This study was conducted with healthy volunteers (n=1446) from Turkey between August 2022 and September 2022. As risk assessment systems to determine CVD risks, SCORE (Systematic Coronary Risk Evaluation) and ASCVD (Atherosclerotic Cardiovascular Disease) were used. We utilized MEDFICTS (Meats, Eggs, Dairy, Fried foods, Fat in Baked Goods, Convenience Foods, Fats Added at the Table, and Snacks) to establish the suitability of the current diet for heart health, and MEDAS (Mediterranean Diet Adherence Screener) to examine the Mediterranean diet characteristics of the current diet. The phytochemical content of the diet was determined using the Phytochemical Index method developed by McCarty.
Results:
The lifetime and 10-year risk scores of SCORE and ASCVD were positively correlated with the MEDFICTS score (r=0.12, P<0.001; r=0.06, P=0.020; r=0.10, P=0.001, respectively). Mediterranean diet characteristics were correlated with lower CVD risk as per the SCORE categories (r=−0.07, P=0.009). A one-unit increase in MEDFICTS scores increased high-to-very high CVD risk and 10-year moderate-to-high CVD risk by 1.01 times, while a one-unit increase in the Mediterranean diet score decreased high-to-very high CVD risk and 10-year moderate-to-high CVD risk by 0.91 times and 0.95 times, respectively. In addition, high values of body weight, body mass index, waist circumference, waist-height ratio, and neck circumference were associated with higher CVD risk (P<0.001).
Conclusion:
Adopting a Mediterranean diet and a heart-healthy diet may be a good strategy to reduce CVD risks.
Keywords: Dietary patterns, Cardiovascular risk, Mediterranean diet, Phytochemicals
Introduction
Cardiovascular diseases (CVD) are among major health problems and the leading causes of morbidity and mortality globally (1). Modifiable factors including smoking, inadequate physical activity, increased body mass index (BMI), and unhealthy dietary patterns are associated with CVD and related deaths (1). Unhealthy dietary patterns take an active part in the development of CVD (2). Furthermore, WHO emphasizes that one of the most important risk factors for CVD is maintenance of unhealthy eating habits (3). A sedentary lifestyle, adopting an unhealthy diet pattern, and being overweight or obese are implicated in increased CVD risk (4).
Recently, studies investigating dietary patterns using dietary guidelines and diet quality indices have revealed the relationship between the diet and CVD (5–7). Among adults without CVD, those with a healthy diet were less likely to be at high risk of developing CVD over the 10 years ahead (6). Some argue that reductions in excess energy intake and improved dietary patterns can prevent many primary and secondary cardiovascular events (8–10). Dietary fat and cholesterol intake is considered as a risk factor for CVD, and behaviour changes towards decreasing the excess intake of fat and cholesterol seem to be beneficial for the prevention of CVD (11). Meats, Eggs, Dairy, Fried foods, Fat in Baked Goods, Convenience Foods, Fats Added at the Table, and Snacks (MEDFICTS) questionnaire is a brief dietary assessment tool developed as part of the National Cholesterol Education Program Adult Treatment Panel guidelines, and it measures the adherence to Step 1 and Step 2 diets that are recommended for the prevention and treatment of CVD (11, 12).
Optimal, 10-year, and lifetime CVD risk is determined using the biochemical parameters, systolic blood pressure measurements, age, gender, statin or aspirin use, diabetes history, and smoking status. Both the Systematic Coronary Risk Evaluation (SCORE, developed by the European Society of Cardiology) and the Atherosclerotic Cardiovascular Disease (ASCVD) Risk Estimator Plus program (developed by the American College of Cardiology) are assessment models used to predict lifetime and 10-year cardiovascular disease risk (13).
Studies investigating the relation of dietary patterns and characteristics to CVD risks are limited. This study was conducted to reveal the relationship between a heart-healthy diet (MEDFICTS), the phytochemical content of a diet, and Mediterranean diet and CVD risks. Because a diet is much easier to modify compared to many other CVD risk factors, establishing the relations of diet and CVD risks through research will be an important step for the reduction of morbidity and mortality risks due to CVD.
Materials and Methods
Study Population
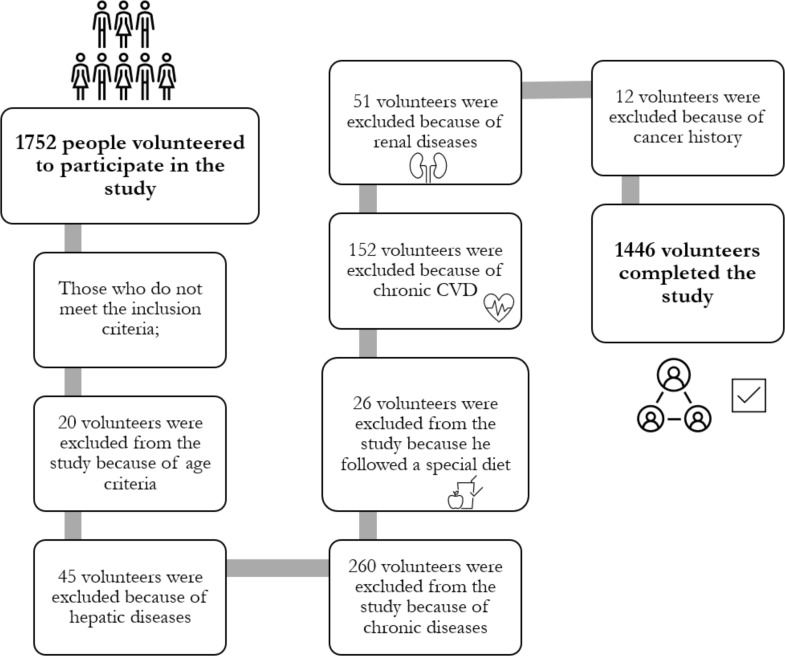
This study was carried out with 40–75-year-old healthy volunteers (n=1446) from community health centers (n=9) and family medicine clinics (n=9) in Turkey between August 2022 and September 2022. Patients with a history of chronic CVD such as stroke, myocardial infarction, coronary artery bypass surgery, percutaneous coronary intervention, coronary angiography, heart failure, or peripheral artery disease; patients with cancer, hepatic or renal disease; individuals following a special diet program, individuals younger than 40 yr of age or over the age of 75, and pregnant and breastfeeding women were excluded. Individuals in the age range of 40–75 yr, who agreed to participate in the study were included. Figure 1 shows the patient recruitment flowchart. The study protocol was approved by the Istanbul Medipol University, Non-Interventional Clinical Research Ethics Committee on July 26, 2022, with decision number 633.
Fig. 1:
Patient recruitment flow chart
Data collection and evaluation
Demographics and health information, dietary pattern, and physical activity status were obtained using a questionnaire form. The values for biochemical parameters were retrieved from patient files.
Assessment of cardiovascular risks
CVD risk was determined using SCORE, a risk assessment system developed by the European Society of Cardiology (https://www.heartscore.org/en_GB/). Based on SCORE assessments, the risk is categorized as low, moderate, high, and very high for scores of <1, 1–5, ≥5, <10, and ≥10, respectively (14). The ASCVD Risk Estimator Plus program was used to determine the optimal risk, 10-year risk, and lifetime risk (https://tools.acc.org/ascvd-risk-estimator-plus/#!/calculate/estimate/). A total score of <5 was considered low risk, scores of 5–7.4 borderline risk, scores of 7.5–19.9 intermediate risk, and scores of ≥20 high risk (15).
Determination of physical activity levels
A two-question physical activity assessment tool was used during face-to-face interviews in order to list the physical activity levels of subjects. Based on the total score of two questions, physical activity levels were listed as “inadequately active” or “adequately active” for scores of 0–3 or ≥4, respectively (16).
Measurement and assessment of anthropometric measurements
Body weight was measured using a calibrated scale and height was measured using a stadiometer. BMI was calculated by dividing body weight (kg) by the square of height (m2) (17). Waist and neck circumference was measured with a stretch-resistant tape, after obtaining the ideal position for the measurement (18, 19). The waist-height ratio, as an indicator of chronic disease risk, was calculated by dividing the waist circumference (cm) by the height (cm) (20).
Evaluation of the suitability of dietary patterns for heart health
Validated version of MEDFICTS questionnaire assessing the suitability of the individuals’ current diets for heart health (11, 21) was administered by the researcher during face-to-face interviews with participants. Scores of ≥ 70 indicate that the individual needs to make some dietary changes; scores of 40–70 indicate that the individual has healthy dietary habits for heart health, and scores of <40 indicate that the individual’s diet is considered compatible with the therapeutic lifestyle diet (22).
Assessment of the phytochemical content of the diet
A 24-hour retrospective food intake recall record was obtained from participants, showing total energy intake and energy intake from phytochemicals. The “Phytochemical Index (PI)” method developed by McCarty was used to determine the total dietary phytochemical intake of individuals (23). Dietary PI value was calculated in percentages as the ratio of energy from phytochemical-rich foods to the total daily energy intake (energy from phytochemical-rich foods (kcal)/total energy intake (kcal) *100). Foods rich in phytochemicals included fruits and vegetables, pulses, whole grains, oilseeds, soy products, olives, and olive oil.
Assessment of Mediterranean Diet Characteristics
Mediterranean diet characteristics were evaluated through face-to-face interviews, using the validated 14-item Mediterranean Diet Adherence Screener (MEDAS) (24, 25). MEDAS score of ≤5 was considered poor adherence, scores of 6–9 moderate adherence, and score of ≥10 good adherence (24).
Statistical Analysis
The collected study data were analyzed using the E-PICOS software (www.e-picos.com, New York) and the MedCalc statistical software package. Continuous variables from scales were described in mean and standard deviation. Categorical variables were described in frequency and percentage. The One-Way ANOVA test was used to compare the mean scale scores across more than two groups. Differences revealed by ANOVA were analyzed by the Tukey statistic as a post hoc test. Chi-square test statistics were utilized to evaluate the associations between categorical variables. Pearson’s correlation coefficient was used to examine associations between continuous variables. The exposure ratio (odds ratio) was obtained by Logistic Regression in order to estimate the exposure risk of factors affecting the cardiac risk status. In multivariable analysis, we adjusted for age, body mass index, physical activity, menopausal status and total energy intake.
Results
The characteristics of participants by adherence to MEDFICTS and Mediterranean diet adherence categories were presented in Table 1. Total cholesterol levels of subjects having dietary patterns compatible with the therapeutic lifestyle diet were statistically significantly lower compared to other groups (181.7±34.35 vs. 190.2±37.65 mg/dL, P=0.001; 181.7±34.35 vs. 196.6±38.53 mg/dL, P<0.001, respectively).
Table 1:
Characteristics of participants according to MEDFICTS, Mediterranean dietary patterns
| MEDFICTS | Mediterranean diet | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Compatible with the therapeutic life-style diet n (%) | Having healthy dietary habits for heart health n (%) | Need to make some dietary changes n (%) | P-value | Poor n (%) | Moderate n (%) | Good n (%) | P-value | |||
| Age (yr) | 40–44 | 142 (35.4) | 257 (34) | 101 (34.8) | 179 (41.5) | 271 (31.5) | 50 (32.1) | |||
| 45–64 | 226 (56.4) | 452 (59.9) | 179 (61.7) | 0.12 | 238 (55.2) | 524 (61) | 95 (60.9) | 0.001 | ||
| 65–75 | 33 (8.2) | 46 (6.1) | 10 (3.4) | 14 (3.2) | 64 (7.5) | 11 (7.1) | ||||
| Mean ± SD | 49.7±8.7 | 49.2±8.1 | 48.7±7.2 | 0.30 | 47.8±7.3 | 49.8±8.30 | 49.9±8.3 | <0.001 | ||
| Gender | Female | 266 (66.3) | 462 (61.2) | 138 (47.6) | <0.001 | 243 (56.4) | 523 (60.9) | 100 (64.1) | 0.16 | |
| Male | 135 (33.7) | 293 (38.8) | 152 (52.4) | 188 (43.6) | 336 (39.1) | 56 (35.9) | ||||
| Diabetes | Yes | 41 (10.2) | 71 (9.4) | 32 (11) | 0.72 | 43 (10) | 87 (10.1) | 14 (9) | 0.91 | |
| No | 360 (89.8) | 684 (90.6) | 258 (89) | 388 (90) | 772 (89.9) | 142 (91) | ||||
| Hypertension | Yes | 61 (15.2) | 90 (11.9) | 36 (12.4) | 0.27 | 49 (11.4) | 124 (14.4) | 14 (9) | 0.09 | |
| No | 340 (84.8) | 665 (88.1) | 254 (87.6) | 382 (88.6) | 735 (85.6) | 142 (91) | ||||
| Statin | Yes | 12 (3) | 25 (3.3) | 17 (5.9) | 0.10 | 19 (4.4) | 32 (3.7) | 3 (1.9) | 0.37 | |
| Medication | No | 389 (97) | 730 (96.7) | 273 (94.1) | 412 (95.6) | 827 (96.3) | 153 (98.1) | |||
| Hypertension | Yes | 60 (15) | 85 (11.3) | 36 (12.4) | 0.19 | 43 (10) | 125 (14.6) | 13 (8.3) | 0.02 | |
| No | 341 (85) | 670 (88.7) | 254 (87.6) | 388 (90) | 734 (85.4) | 143 (91.7) | ||||
| Physical activity | Inactive | 289 (72.1) | 616 (81.6) | 230 (79.3) | 0.001 | 360 (83.5) | 672 (78.2) | 103 (66) | <0.001 | |
| Adequate active | 112 (27.9) | 139 (18.4) | 60 (20.7) | 71 (16.5) | 187 (21.8) | 53 (34) | ||||
| Anthropometric measurement | BMI (kg/m2) | 26.3±4.75 | 27.2±4.71 | 27.8±5.12 | <0.001 | 27.6±5.52 | 27.0±4.58 | 26.0±3.89 | 0.001 | |
| Waist circumference (cm) | 87.2±14.42 | 89.8±13.86 | 91.6±15.21 | <0.001 | 90.0±4.83 | 90.0±15.27 | 89.7±14.03 | 0.07 | ||
| (Mean ± SD) | Waist height ratio | 0.53±0.09 | 0.53±0.08 | 0.53±0.09 | 0.07 | 0.53±0.1 | 0.53±0.09 | 0.5±0.08 | 0.03 | |
| Neck circumference (cm) | 35.0±4.56 | 35.9±4.71 | 36.9±5.21 | <0.001 | 35.9±5.07 | 35.9±4.64 | 35.6±4.98 | 0.84 | ||
| Lipid parameters | Total cholesterol | 181.7±34.35 | 190.2±37.65 | 196.6±38.53 | <0.001 | 190.7±37.94 | 190.5±37.57 | 177.1±31.47 | <0.001 | |
| (Mean±SD) (mg/dL) | LDL | 51.8±12.47 | 51.0±10.77 | 50.6±13.49 | 0.34 | 50.2±12.13 | 51.3±11.41 | 53.1±13.07 | 0.03 | |
| HDL | 107.5±28.09 | 115.9±32.48 | 122.1±33.2 | <0.001 | 116.6±32.52 | 111.9±32.43 | 104±24.04 | <0.001 | ||
One-Way ANOVA, PostHoc- Tukey, Chi square, P<0,05. BMI: body mass index, LDL: low density lipoprotein, HDL: high density lipoprotein
The cardiovascular risk scores of the participants by SCORE and ASCVD system assessments were presented in Table 2. Compared to subjects on the therapeutic lifestyle diet and those with healthy dietary patterns, subjects needing dietary changes had significantly higher ASCVD lifetime CVD risk scores (41.6±14.45 vs. 39.1±14.51, 39.3±13.73, P=0.04) and significantly higher SCORE risk scores (3.4±2.81 vs. 2.7±2.02, 2.64±1.91, P<0.001). CVD risk was significantly higher in subjects with poor adherence to the Mediterranean diet compared to those with good adherence (2.8±1.92 vs. 2.1±1.01, P=0.03), and subjects with moderate adherence compared to those with good adherence (2.9±2.41 vs. 2.1±1.01, P=0.007).
Table 2:
Cardiovascular risk scores and classification according to dietary characteristics of the participants
| MEDFICTS | Meditarrenean diet | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Compatible with the therapeutic lifestyle diet n (%) | Having healthy dietary habits for heart health n (%) | Need to make some dietary changes n (%) | P-value | Poor n (%) | Moderate n (%) | Good n (%) | P-value | |
| ASCVD classification | ||||||||
| Low | 294 (73.7) | 549 (73) | 197 (68.2) | 311 (72.3) | 614 (71.8) | 115 (74.2) | 0.19 | |
| Borderline | 40 (10) | 65 (8.6) | 32 (11.1) | 0.58 | 42 (9.8) | 74 (8.7) | 21 (13.5) | |
| Intermediate | 49 (12.3) | 103 (13.7) | 42 (14.5) | 60 (14) | 119 (13.9) | 15 (9.7) | ||
| High | 16 (4) | 35 (4.7) | 18 (6.2) | 17 (4) | 48 (5.6) | 4 (2.6) | ||
| 10-year | 4.7±7.93 | 4.7±6.64 | 5.4±7.91 | 0.34 | 4.7±6.97 | 5.14±7.76 | 3.8±4.85 | 0.12 |
| ASCVD | ||||||||
| risk score a | ||||||||
| Lifetime | 39.1±14.51 | 39.3±13.73 | 41.6±14.45 | 0.04 | 40.8±13.84 | 39.3±14.13 | 38.9±14.81 | 0.20 |
| ASCVD risk score a | ||||||||
| Optimal | 2.1±1.34 | 1.9±1.63 | 1.8±1.51 | 0.48 | 2.1±1.93 | 1.6±1.79 | 1.8±1.23 | 0.03 |
| ASCVD risk score a | ||||||||
| SCORE risk score a | 2.7±2.02 | 2.6±1.91 | 3.4±2.81 | <0.001 | 2.8±1.92 | 2.9±2.41 | 2.1±1.01 | 0.01 |
| SCORE classification | ||||||||
| Low | 20 (5) | 54 (7.2) | 25 (8.6) | 19 (4.4) | 60 (7) | 20 (12.8) | ||
| Moderate | 313 (78.1) | 580 (76.8) | 200 (69) | 0.04 | 334 (77.5) | 637 (74.2) | 122 (78.2) | 0.002 |
| High | 52 (13) | 95 (12.6) | 45 (15.5) | 61 (14.2) | 120 (14) | 11 (7.1) | ||
| Very high | 16 (4) | 26 (3.4) | 20 (6.9) | 17 (3.9) | 42 (4.9) | 3 (1.9) | ||
One-Way ANOVA, PostHoc- Tukey, Chi square, P<0,05
a Mean ± SD
The MEDFICTS categories, Mediterranean diet characteristics, and PI of participants were presented in Table 3. Based on the SCORE assessments, subjects with low CVD risk (7.4±2.24) had significantly higher MEDAS scores compared to those with moderate, high, and very high risk (6.7±2.23, 6.3±2.00, 6.5±1.71, respectively) (P=0.005, P<0.001, P=0.03, respectively).
Table 3:
MEDFICTS, Mediterranean diet characteristics and phytochemical index score according to CVD risk classifications of the participants
| Variables | SCORE | 10-year ASCVD risk | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Low | Moderate | High | Very high | P-value | Low | Border-line | Intermediate | High | P-value | |
| MEDFICTS score (Mean ± SD) | 57.8±25.06 | 52.2±21.28 | 56.6±27.54 | 60.1±27.37 | 0.001 | 52.5±21.94 | 54.5±23.15 | 56.4±25.98 | 57.9±24.81 | 0.04 |
| MEDAS score (Mean ± SD) | 7.4±2.24 | 6.7±2.23 | 6.3±2.00 | 6.5±1.71 | <0.001 | 6.7±2.21 | 6.9±2.35 | 6.4±2.12 | 6,5±1,87 | 0.25 |
| Phytochemical index score (Mean SD) | 30.3±13.68 | 28.9±16.78 | 30.0±17.15 | 28.3±14.56 | 0.69 | 28.9±16.43 | 31.4±17.56 | 28.6±17.34 | 29.6±13.89 | 0.39 |
One-Way ANOVA, PostHoc- Tukey, P<0.05.
Correlations of dietary characteristics, physical activity with SCORE and ASCVD risk scores were presented in Table 4. The effects of diet characteristics in the estimation of CVD risk were presented in Table 5. A one-unit increase in MEDFICTS scores increased high-very high CVD risk by 1.01 times, while a one-unit increase in Mediterranean diet scores reduced high-very high CVD by 0.91 times.
Table 4:
Relationship between dietary characteristics, physical activity and SCORE and ASCVD risk score
| Variable | 10-year ASCVD risk | Lifetime ASCVD risk | Optimal ASCVD risk | SCORE | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| r | P-value | r | P-value | r | P-value | r | P-value | |
| MEDFICTS | 0.06 | 0.020 | 0.10 | 0.001 | −0.02 | 0.40 | 0.12 | <0.001 |
| Meat score | 0.07 | 0.009 | 0.15 | <0.001 | 0.02 | 0.55 | 0.05 | 0.04 |
| Egg score | 0.01 | 0.67 | 0.08 | 0.008 | −0.01 | 0.59 | −0.006 | 0.82 |
| Dairy products score | 0.12 | <0.001 | 0.04 | 0.19 | 0.09 | 0.001 | 0.18 | <0.001 |
| MEDAS score | −0.04 | 0.11 | −0.04 | 0.18 | 0.02 | 0.40 | −0.07 | 0.009 |
| Phytochemical index score | −0.003 | 0.91 | −0.02 | 0.56 | 0.02 | 0.39 | −0.009 | 0.73 |
| Physical activity score | −0.09 | <0.001 | 0.06 | 0.06 | −0.07 | 0.01 | −0.12 | <0.001 |
Pearson Correlation, p<0.05.
Table 5:
Evaluation of diet characteristics factor in predicting CVD risk status
| Variable | Model 1 Odds Ratio (95% CI) | P-value | Model 2 Odds Ratio (95% CI) | P-value |
|---|---|---|---|---|
| MEDFICTS score | 1.01 (1.01–1.02) | 0.002 | 1.01 (1.00–1.02) | <0.001 |
| MEDAS score | 0.91 (0.86–0.97) | 0.005 | 0.95 (0.89–1.01) | 0.09 |
| Phytochemical index score | 1.01 (0.99–1.01) | 0.56 | 0.98 (0.97–1.01) | 0.78 |
(Logistic Regression-Odds ratio), Model 1: SCORE risk (high-very high/low-moderate), Model 2: ASCVD-10-year risk (intermediate -high/low-borderline)
Discussion
Foods and dietary components are associated with CVD risk (26–28). Particularly healthy dietary patterns have been shown to reduce the incidence and mortality of CVD significantly (29, 30). A 25% increase in the healthy eating patterns was correlated with reduced CVD risk, which ranged from 10% to 20% (29). In Atherosclerosis Risk in Communities study (n=12 413), compared to participants in the lowest quintile of diet quality, the participants in the highest quintile had a 16% lower incidence of CVD (95% CI, P<0.001), 32% lower risk of CVD mortality (95% CI, P<0.001), and an 18% lower risk of all-cause mortality (95% CI, P<0.001) (30). Similarly, Zhang et al. (28) found that participants in the highest quartile of diet quality had lower 10-year CVD risk compared to participants in the lowest quartile (β = −2.37, 95% CI, P<0.0001) (28). In this study, a one-unit increase in MEDFICTS scores is associated with 1.01 times increases in high very high CVD risk and 10-year moderate-high CVD risk. Thus, consistent with the information in the literature, our study results highlight that healthy eating behavior can help reduce CVD risk.
The Mediterranean diet may help reduce CVD risk. Approximately one-third of CVD-related metabolites were significantly associated with adherence to the Mediterranean diet (31). Every 2 units increase in adherence to the Mediterranean diet was associated with a significant reduction of 15% in the risk of death from all causes and that the pooled HR for the risk of death from CVD was 0.91 (32). A meta-analysis study (n=29) emphasizes that the Mediterranean diet is protective against CVD risk, particularly against coronary heart disease and ischemic stroke; however, it does not help prevent a hemorrhagic stroke (33). In our study, a one-unit increase in Mediterranean diet scores reduces the risk of high-very high CVD by 0.91 times and 10-year moderate-to-high CVD risk by 0.95 times. A Mediterranean diet intervention may help prevent CVD by reducing high plasma concentrations of ceramides (34). Mediterranean diet can reduce CVD risk by increasing nitric oxide bioavailability and by alleviating triggering factors of CVD such as increased blood pressure, glucose as well as lipid levels, endothelial dysfunction, increased reactive oxygen species levels (35).
Phytochemicals may exhibit protective effects through their antioxidant activity by inhibiting reactive oxygen and nitrogen species, implicated in the pathogenesis of many chronic diseases (36). Phytochemicals may improve the lipid profile and alleviate inflammation by inhibiting prostaglandin synthesis, platelet aggregation and nuclear factor-κB activity, by enzyme inhibition, and by increasing cytokine production (37, 38). Furthermore, phenolic acids may be involved in the prevention of cardiovascular events by preventing the accumulation of vascular smooth muscle cells, which play a key role in the formation and development of atherosclerotic lesions (39). In addition, phytochemicals may promote the denovo expression of endogenous antioxidant defense genes such as glutathione peroxidase, superoxide dismutase, and heme oxygenase-1 (40). Despite these favorable effects of phytochemicals, the evidence showing their relation to CVD risk is inadequate. In this study, phytochemical intake alone was not associated with CVD risk, however, the Mediterranean diet, one of the best examples of a diet rich in phytochemicals, was associated with lower CVD risk. This might result from the adequacy of the diet, which contains cardioprotective components in addition to phytochemicals along with all nutrients, leading to the suggestion that the diet composition should be considered as a whole. However, the number of studies examining CVD risk and phytochemical intake is not adequate. Despite the striking results of the study, there are some limitations, including a lack of dietary intervention and the use of a recall-based assessment of current dietary patterns, diet characteristics, and the phytochemical intake. Such assessments depend on the subject’s memory and cognition. Furthermore, other non-dietary factors that might affect CVD risk need to be eliminated. It will be beneficial if future studies include the investigation of such factors such as age, gender, family history, and genetics. Long-term prospective studies with follow-up of subjects will be important for revealing the relationship between dietary patterns and CVD risk.
Conclusion
A dietary pattern that includes balanced and healthy eating behaviors may help reduce the risk of CVD. Adopting a Mediterranean diet and a heart-healthy diet may be a good strategy to reduce CVD risks.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Footnotes
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.Shahdadian F, Saneei P, Milajerdi A, Esmaillzadeh A. (2019). Dietary glycemic index, glycemic load, and risk of mortality from all causes and cardiovascular diseases: a systematic review and dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr, 110(4):921–37. [DOI] [PubMed] [Google Scholar]
- 2.Denova-Gutiérrez E, Huitrón-Bravo G, Talavera JO, et al. (2010). Dietary glycemic index, dietary glycemic load, blood lipids, and coronary heart disease. J Nutr Metab, 2010:170680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. “-Fact Sheets-Cardiovascular diseases”, 2021. http://www.who.int/mediacentre/factsheets/fs317/en/ [accessed: 20 Apr 2022].
- 4.Lakka TA, Bouchard C. (2005). Physical activity, obesity and cardiovascular diseases. Handb Exp Pharmacol, (170):137–63. [DOI] [PubMed] [Google Scholar]
- 5.Milte CM, Thorpe MG, Crawford D, et al. (2015). Associations of diet quality with health-related quality of life in older Australian men and women. Exp Gerontol, 64:8–16. [DOI] [PubMed] [Google Scholar]
- 6.Edwards MK, Crush E, Loprinzi PD. (2018). Dietary behavior and predicted 10-year risk for a first atherosclerotic cardiovascular disease event using the pooled cohort risk equations among US adults. Am J Health Promot, 32(6):1447–51. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins DJA, Dehghan M, Mente A, et al. (2021). Glycemic index, glycemic load, and cardiovascular disease and mortality. N Engl J Med, 384(14):1312–22. [DOI] [PubMed] [Google Scholar]
- 8.Yu E, Malik VS, Hu FB. (2018). Cardiovascular disease prevention by diet modification: JACC Health Promotion Series. J Am Coll Cardiol, 72(8):914–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernstein AM, Sun Q, Hu FB, et al. (2010). Major dietary protein sources and risk of coronary heart disease in women. Circulation, 122(9):876–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.George SM, Ballard-Barbash R, Manson JE, et al. (2014). Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. Am J Epidemiol, 180(6):616–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Göktaş Z, Dikmen D, Rakıcıoğlu N. (2022). Validation of MEDFICTS dietary assessment questionnaire in Turkish population. Public Health Nutr, 25(1):13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kris-Etherton P, Eissenstat B, Jaax S, et al. (2001). Validation for MEDFICTS, a dietary assessment instrument for evaluating adherence to total and saturated fat recommendations of the National Cholesterol Education Program Step 1 and Step 2 diets. J Am Diet Assoc, 101(1): 81–6. [DOI] [PubMed] [Google Scholar]
- 13.Wong ND, Budoff MJ, Ferdinand K, et al. (2022). Atherosclerotic cardiovascular disease risk assessment: An American Society for Preventive Cardiology clinical practice statement. Am J Prev Cardiol, 10:100335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ural D. (2012). A perspective to lipid lowering therapy after ESC/EAS guidelines for the management of dyslipidaemias and the European guidelines on cardiovascular disease prevention in clinical practice. Turk Kardiyol Dern Ars, 40(4):293–7. [DOI] [PubMed] [Google Scholar]
- 15.Arnett DK, Blumenthal RS, Albert MA, et al. (2019). 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 140(11):e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall AL, Smith BJ, Bauman AE, Kaur S. (2005). Reliability and validity of a brief physical activity assessment for use by family doctors. Br J Sports Med, 39(5):294–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization (WHO) Global Database for Body Mass Index. The international classification of adult underweight, over-weight and obesity according to BMI. Web: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html [accessed: 06.06.2022].
- 18.World Health Organization. Waist circumference and waist-hip ratio. Report of a WHO Expert Consultation. Geneva.
- 19.Ben-Noun LL, Sohar E, Laor A. (2001). Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res, 9(8):470–7. [DOI] [PubMed] [Google Scholar]
- 20.Ashwell M, Gibson S. (2016). Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’based on BMI and waist circumference. BMJ Open, 6(3): e010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation, 106(25):3143–421. [PubMed] [Google Scholar]
- 22.Holmes AL, Sanderson B, Maisiak R, Brown A, Bittner V. (2005). Dietitian services are associated with improved patient outcomes and the MEDFICTS dietary assessment questionnaire is a suitable outcome measure in cardiac rehabilitation. J Am Diet Assoc, 105(10):1533–40. [DOI] [PubMed] [Google Scholar]
- 23.McCarty MF. (2004). Proposal for a dietary “phytochemical index. Med Hypotheses, 63(5):813–817. [DOI] [PubMed] [Google Scholar]
- 24.Martínez-González MA, García-Arellano A, Toledo E, et al. (2012). A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One, 7(8):e43134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Özkan Pehlivanoğlu EF, Balcıoğlu H, Ünlüoğlu İ. (2020). Turkish validation and reliability of Mediterranean Diet Adherence Screener. Osmangazi Journal of Medicine, 42(2):160–4. [Google Scholar]
- 26.Wang DD, Hu FB. (2017). Dietary fat and risk of cardiovascular disease: recent controversies and advances. Annu Rev Nutr, 37:423–46. [DOI] [PubMed] [Google Scholar]
- 27.Astrup A, Magkos F, Bier DM, et al. (2020). Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J Am Coll Cardiol, 76(7):844–57. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Lu C, Li X, et al. (2022). Healthy Eating Index-2015 and predicted 10-year cardiovascular disease risk, as well as heart age. Front Nutr, 9:888966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shan Z, Li Y, Baden MY, et al. (2020). Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med, 180(8):1090–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu EA, Steffen LM, Coresh J, et al. (2020). Adherence to the Healthy Eating Index-2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr, 150(2):312–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li J, Guasch-Ferré M, Chung W, et al. (2020). The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur Heart J, 41(28):2645–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang C, Wang X, Qin LQ, Dong JY. (2021). Mediterranean diet and mortality in people with cardiovascular disease: A meta-analysis of prospective cohort studies. Nutrients, 13(8):2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rosato V, Temple NJ, La Vecchia C, et al. (2019). Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr, 58(1):173–91. [DOI] [PubMed] [Google Scholar]
- 34.Wang DD, Toledo E, Hruby A, et al. (2019). Plasma ceramides, Mediterranean diet, and incident cardiovascular disease in the PREDIMED Trial (Prevención con Dieta Mediterránea) Circulation, 140(16):e726. [DOI] [PubMed] [Google Scholar]
- 35.Widmer RJ, Flammer AJ, Lerman LO, Lerman A. (2015). The Mediterranean diet, its components, and cardiovascular disease. Am J Med, 128(3):229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang YJ, Gan RY, Li S, Zhou Y, et al. (2015). Antioxidant phytochemicals for the prevention and treatment of chronic diseases. Molecules, 20(12):21138–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Costa A, Garcia-Diaz DF, Jimenez P, Silva PI. (2013). Bioactive compounds and health benefits of exotic tropical red-black berries. J Funct Food, 5(2):539–49. [Google Scholar]
- 38.Hutchins-Wolfbrandt A, Mistry AM. (2011). Dietary turmeric potentially reduces the risk of cancer. Asian Pac J Cancer Prev, 12(12):3169–73. [PubMed] [Google Scholar]
- 39.Xie CH, Kang J, Chen JR, et al. (2011). Phenolic acids are in vivo atheroprotective compounds appearing in the serum of rats after blueberry consumption. J Agric Food Chem, 59(18):10381–7. [DOI] [PubMed] [Google Scholar]
- 40.Ismaeel A, Greathouse KL, Newton N, Miserlis D, et al. (2021). Phytochemicals as therapeutic interventions in peripheral artery disease. Nutrients, 13(7):2143. [DOI] [PMC free article] [PubMed] [Google Scholar]