Abstract
Background:
There are difficulties in the treatment of smoking cessation in elderly patients. However, elderly smokers who gave up smoking had lower rates of death from heart attack, stroke, and cancer, as well as improved cognitive function. This study aimed to investigate the affecting factors and the success of smoking cessation rate in patients aged 60 and over in Turkey.
Methods:
Six smoking cessation outpatient clinics from four provinces were included in the study. The records of 1,065 patients who applied to a smoking cessation outpatient clinic between 2016 and 2019 and who were 60 yr of age or older were scanned. Overall, 917 cases that could be reached after treatment were included in the study. Smoking cessation rates at the first month, 3rd month, 6th month, 9th month and 12th month were given.
Results:
Of the 917 cases, 65.1% were male and 34.9% were female. Smoking cessation rates were 45.6% on the first month, 39% on the third month, 35.1% on the sixth month, 31.2% on the ninth month, and 30.3% at the twelfth month. Smoking cessation success was higher in men than in women.
Conclusion:
Since the success of smoking cessation in the elderly was similar to that of adults. Since smoking is an independent risk factor for death in the elderly, there should be greater willingness to provide elderly patients with smoking cessation treatment to reduce physical function loss and promote healthier aging.
Keywords: Smoking cessation, Geriatrics, Smoking cessation rates, Side effects
Introduction
The world population for 2021 was 7,831,718,605 and that the elderly population was 764,321,142. According to these estimates, 9.8% of the world’s population is composed of the elderly (1). The elderly population is increasing throughout the world. By 2030, the percentage of the population over the age of 65 will reach 20% (2). Smoking is an independent risk factor for death in the elderly (3,4). In a 7,178 elderly cohort, the rates of all-cause cancer and cardiovascular death was approximately twice as high in current smokers aged 65 and over compared to their peers never smoked (5). There is high-quality evidence that smoking cessation significantly reduces the risk of coronary heart disease, various cancers, and chronic obstructive pulmonary disease (6). A study of smoking cessation in community-dwelling older adults showed that, within 5 years of quitting, the relative risk of death from all causes decreased compared to current smokers (7). A meta-analysis found that lowered mortality benefits of smoking cessation was demonstrable at any age, including for those aged 80 and over (8). Unfortunately, smoking cessation interventions are offered to older adults at insufficient rates. Older adults who smoke are less likely than younger individuals to be advised to quit by healthcare providers (9–11). This is because it may be thought that treatment management may be difficult due to physiological changes due to aging, accompanying chronic diseases, polypharmacy, drug interactions, and side effects. Although there are many studies on smoking cessation rates in adults and the factors affecting it, there are few studies on smoking cessation rates in the elderly. In the study investigating the effects of aging on the effectiveness of smoking cessation medication, the overall success of quitting smoking over the age of 60 was found to be 41% (12). In a multicenter study conducted in Turkey, the rate of smoking cessation over the age of 60 was reported as 38% (13).
We aimed to investigate the affecting factors and the success of smoking cessation rate in patients aged 60 and over in Turkey.
Materials and Methods
Six smoking cessation outpatient clinics from four provinces were included in the study. Six smoking cessation centers from four big cities (Aydın, Adana, Istanbul, and Bursa) participated in the study. In all centers participating in the study, smoking cessation outpatient clinics are carried out by chest diseases specialists certified by the Ministry of Health of the Republic of Turkey, a smoking cessation polyclinic. Behavioral cognitive therapy was provided to all cases in the centers. Treatment program includes Behavioral cognitive therapy and medical therapy (bupropion, varenicline, nicotine replacement therapy). In our country, in addition to cognitive behavioral therapy, varenicline, bupropion or nicotine replacement therapies (NRT) are given to eligible patients (according to their addiction levels, comorbidities, drugs used and drug interactions) in smoking cessation outpatient clinics. This study was accessed from the files of pharmacological treatments given to patients retrospectively.
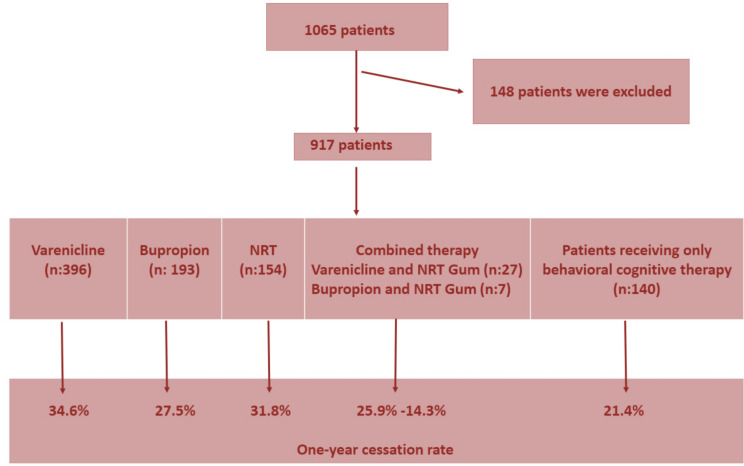
The files of 1,065 patients aged 60 and over who applied to the smoking cessation outpatient clinic between 2016 and 2019 were scanned and included in the treatment program. Overall, 917 cases that could be reached after treatment were included in the study (Fig.1).
Fig.1:
Overall study design flowchart.
The inclusion criteria included the following
All patients aged 60 and over who were smokers and whose files could be accessed were included.
The exclusion criteria included the following
Patients under the age of 60 and patients whose information could not be obtained from the files. The files of the cases were scanned retrospectively, and smoking behaviors, addiction levels, comorbidities, treatments used, and side effects were recorded. Factors affecting quitting success were investigated.
The Fagerstrom Nicotine Dependence Test (FTND) was used to assess nicotine addiction (14). The Fagerstrom Nicotine Dependence Test, widely used in smoking cessation outpatient clinics, is used to measure nicotine dependence. The Fagerstrom Nicotine Dependence Test consists of 6 questions. The level of addiction is determined according to the score totals of the answers. Total FTND score: Possible range: 0–10. Higher scores indicate higher nicotine dependence. 0–2 Very low; 3–4 Low; 5 Medium; 6–7 High; 8–10 Very high (Supplement 1).
The smoking cessation status of the patients was questioned and recorded by the staff of the smoking cessation outpatient clinic, either face-to-face or by telephone. The cases were divided into two subgroups 60–64 yr old and 65 yr old and over and analyzed. Smoking cessation rates at the first month, 3rd month, 6th month, 9th month and 12th month were given.
Smoker: A person who smokes one or more cigarettes per day is defined as a smoker.
Pack-years: It is calculated as the number of cigarettes smoked per day (number of packs) × the number of years smoked.
Ethical approval
Ethics committee approval was received from the Institutional Review Board (IRB) of Cukurova University Faculty of Medicine on 12-11.03.2020/52-757.
Statistical analysis
Data were evaluated using the (SPSS) 20.0 package program (IBM Corp., Armonk, NY, USA). Among the descriptive data, mean and standard deviation were used for continuous variables, and percentiles were used for categorical variables. The normal distribution suitability of the data was evaluated using the Kolmogorov-Smirnov test. The independent sample t-test was used for the relationship between treatment durations and the success of quitting after 12 months, and chi-square tests were used to analyze categorical data. The significance level was taken as P<0.05.
Results
We enrolled 917 cases; 65.1% were male and 34.9% were female. The mean age was 64.55 ± 4.30 (60–87) yr (Table 1). The mean pack-year of smoking was 49.27 ± 24.97. The mean Fager-strom addiction score was 6.16 ± 2.30. The mean age of starting smoking was 19.45 ± 6.91 (5–64) yr. Of the patients, 65.1% had comorbidities (Table 2). Varenicline was given to 43.2%, bupropion to 21%, and nicotine replacement therapy (NRT) to 16.2% of the cases. No pharmacological treatment was administered to 15.3% of the cases. The treatments received by the patients are shown in Table 3.
Table 1:
Demographic characteristics of the cases
| Specifications | N (%) | Specifications | N (%) |
|---|---|---|---|
| Gender | Working Status1 | ||
| Female | 320 (34.9) | retired | 497(54.2) |
| Male | 597(65.1) | working | 178(19.4) |
| not working | 210(22.9) | ||
| Age | Other Addiction Status1 | ||
| 60–64 age | 564(61.5) | yes (alcohol) | 8(0.9) |
| 65 age ≥ | 353(38.5) | no | 587(64.0) |
| Education Status1 | |||
| literate | 74(8.1) | Comorbidity | |
| Primary school | 370(40.3) | yes | 597(65.1) |
| Middle School | 138(15.0) | no | 320(34.9) |
| High school | 185(20.2) | ||
| University | 121(13.2) |
Table 2:
Comorbidity status of the cases
| Comorbidity | N(%) | Comorbidity | N(%) |
|---|---|---|---|
| COPD | 221(24.1) | Head injury | 2(0.2) |
| Hypertension | 267(29.1) | Kidney disease | 4(0.4) |
| Diabetes mellitus | 174(19.0) | Depressive Disorder | 130(14.2) |
| Asthma | 42(4.6) | Alcohol addiction | 2(0.2) |
| Allergic Diseases | 15(1.6) | Psychotic disorder | 1(0.1) |
| Coronary Artery Disease | 66(7.2) | Bipolar affective disorder | 1(0.1) |
| Heart failure | 2(0.2) | Cerebrovascular diseases | 3(0.3) |
| Cancer | 5(0.5) | Thyroid diseases | 2(0.2) |
| Hepatitis B | 2(0.2) | Prostate diseases | 1(0.1) |
Table 3:
Treatments given to 917 cases
| Pharmacological Treatment | N (917) | % |
|---|---|---|
| Varenicline | 396 | 43.2 |
| Bupropion | 193 | 21.0 |
| NRT (patch) | 149 | 16.2 |
| NRT (Gum) | 2 | 0.2 |
| NRT (Pacth and Gum) | 3 | 0.3 |
| Varenicline and NRT Gum | 27 | 2.9 |
| Bupropion and NRT Gum | 7 | 0.8 |
| No pharmacological treatment | 140 | 15.3 |
Smoking cessation rates were 45.6% in the first month, 39% in the third month, 35.1% in the six month, 31.2% in the ninth month, and 30.3% in the twelfth month. The mean duration of treatment for the cases was 34.74 d. The mean duration of treatment in cases who quit smoking after 1 year was 51 d, and the success of smoking cessation increased with the increase in treatment duration, and the difference was significant (P<0.001).
Smoking cessation success was higher in men than in women (P<0.010). No difference was found between education, occupation, comorbidity, and quitting success. The one-year cessation rate was 27.5% with bupropion, 34.6% with vareniclin, 31.8% with NRT, 14.3% with combined bupropion and NRT, and 25.9% with combined varenicline and NRT. However, the difference was not statistically significant. In this study, no severe side effects that required emergency service admission or hospitalization were detected during the treatment. After examining the smoking cessation success of 777 patients, results revealed that the success was higher after varenicline use in the 60–64 age group (P=0.021), and there was no significant difference between other treatments and age groups.
While the age of onset of smoking and the mean cigarette pack years were significantly higher in cases aged 65 and over (P=0.002 and P=0.007), the Fagerstrom Nicotine Dependence score was significantly higher in cases below the age of 65 (P=0.007) (Table 4).
Table 4:
Comparison of smoking characteristics of cases over and under 65 yr old
| Variable | Mean ± Standard deviation | P |
|---|---|---|
| Age of Initiation to Smoking (yr) | ||
| 60–64 age | 18.85±5.91 | 0.002 |
| 65 age ≥ | 20.42±8.21 | |
| Smoking amount (Pack-year) | ||
| 60–64 age | 47.51±24.30 | 0.007 |
| 65 age ≥ | 52.08±25.81 | |
| Fagerstrom Nicotine Addiction Score | ||
| 60–64 age | 6.32±2.21 | 0.007 |
| 65 age ≥ | 5.90±2.40 |
Discussion
In our study, the one-year smoking cessation rate of 917 patients over the age of 60 was 30.3%. This rate was similar to adult smoking cessation rates.
The 1-year quit success rate of 153 patients aged 60 yr and over was 49%, and quitting success was significantly higher than in the group under 60 (15). In our study, the 1-year smoking cessation rate was 30.3%. Again, in Turkey, in a multicenter study with 16,473 cases, a quit rate of 29.6% with varenicline and 25.1% with bupropion was found. In the same study, the rate of smoking cessation was 38% in patients aged 60 and over (13). In our study, Fagerstrom addiction, smoking duration, and smoking amount were higher in patients aged 65 and over. It is difficult for older smokers to become more dependent on smoking cessation treatments due to their long-term smoking, comorbidities, and multiple drug use (4).
Aging people are more likely to suffer from chronic diseases. Eighty percent have at least one chronic condition and 50% had at least two chronic conditions (2). In our study, 65.1% of the cases were accompanied by at least one comorbidity. Comorbidities, polypharmacy, and drug interactions are factors that complicate smoking cessation treatment in the elderly. Pharmacological treatment was started in 84.7% of our cases, and no side effects that required hospital admission or hospitalization were observed. In another study, 239 Brazilian patients over 60 were given pharmacological treatment for 12 wk and followed up for 52 wk. Being over the age of 60 was significantly associated with increased quit success among NRT users alone, while the efficacy of varenicline and bupropion did not differ significantly by age group (12). Again, varenicline was well tolerated; all reported adverse events were mild to moderate in severity. Therefore, no dose adjustments based solely on age were found to be necessary. This study showed that the pharmacokinetic trend of varenicline in elderly smokers with normal renal function was similar to that in young, healthy subjects and that varenicline was well tolerated in this population. No dose adjustment based on age alone is considered necessary (16).
78.3% of the cases were given NRT, and 21.7%, varenicline. Varenicline is preferred because of its comorbidities and less drug interaction with varenicline (17). In our study, the most preferred pharmacological treatment was varenicline with 43.2%. Varenicline has been reported to be effective and safe in the elderly. Bupropion can also be used in the elderly; however, dose adjustment may be required (once daily dose). In our study, 21.0% of cases were given bupropion at normal dosage, and no serious side effects were detected. NRT can be used safely in both the elderly and the young (18). In the current study, NRT was used safely in 16.7% of the cases.
Although various smoking cessation programs have been developed in China in the last decade, the rates of use in the elderly were low, and a mobile smoking cessation program was an appropriate approach to reach older smokers. A mobile application is a promising model for reaching the elderly and possibly other hard-to-reach smokers (19).
Both elderly smokers and healthcare providers may think that quitting smoking at an advanced age is too late or will not be beneficial. However, quitting smoking reduces the risk of cardiovascular disease, stroke, lung cancer, and COPD in patients aged 65 and over (4). Individuals who quit smoking in old age are able to maintain a higher level of functionality at later ages compared to those who continue to smoke. One explanation for this may be that smoking cessation improves cardiovascular function and pulmonary function, resulting in less fatigue during daily activities. In addition, smoking cessation has been shown to be associated with better physical performance in terms of increased muscle strength, better agility and coordination, and better gait and balance. Subjects who continue to smoke have decreased mobility, earlier loss of mobility, higher prevalence of chronic diseases, and lower quality of life scores compared to their smoking peers (9). Today, we have substantial evidence of the meaningful benefits in terms of physical and mental functions, overall health, and survival for older persons who quit smoking.
This study suggests that smoking cessation treatments are safe and effective in patients over 60 yr of age. As the duration of treatment increased (3 months), the success of quitting increased. Smoking cessation treatments in cases aged 60 and over are important in terms of both health gains and setting an example for young people.
Our study had some limitations. Since it was a retrospective study, our quit success rate was found to be lower than that of prospective studies with regular follow-ups. In addition, the death rates of nonsmokers due to comorbidities or the inability to be reached by phone may have changed. Another limitation of our study is the state of smoking cessation based on the patient’s statement.
Conclusion
The elderly population is increasing throughout the world. In this case, the number of patients aged 60 and over who apply to smoking cessation outpatient clinics will gradually increase. Older smokers should be encouraged to engage in smoking cessation programs that emphasize the health benefits of quitting and identify the risks they avoid.
Special attention should be paid to smoking cessation treatments in the elderly because of their longer smoking history, comorbidities, and the pharmacological treatments they use. Studies should be conducted in geriatric outpatient clinics and smoking cessation clinics on the factors that will affect the success of smoking cessation in the elderly and how to increase the success of smoking cessation.
Journalism Ethics considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
There was no financial source of the study
Footnotes
Conflict of interest
The authors declare that there is no conflict of interests.
References
- 1.TUIK, 2021. https://data.tuik.gov.tr/Bulten/Index?p=Istatistiklerle-Yaslilar-2021-45636#:~:text=T%C3%BCrkiye’de%202021%20y%C4%B1l%C4%B1nda%20toplam,bir%20ya%C5%9Fl%C4%B1%20fert%20ya%C5%9Fad%C4%B1%C4%9F%C4%B1%20g%C3%B6r%C3%BCld%C3%BC
- 2.Centers for Disease Control and Prevention and The Merck Company Foundation. The state of aging and health in America 2007. https://www.cdc.gov/aging/pdf/saha_2007.pdf
- 3.Müezzinler A, Mons U, Gellert C, et al. (2015). Smoking and all-cause mortality in older adults: Results from the CHANCES consortium. Am J Prev Med, 49(5):e53–63. [DOI] [PubMed] [Google Scholar]
- 4.Appel DW, Aldrich TK. (2003). Smoking cessation in the elderly. Clin Geriatr Med, 19(1):77–100. [DOI] [PubMed] [Google Scholar]
- 5.LaCroix AZ, Lang J, Scherr P, et al. (1991). Smoking and mortality among older men and women in three communities. N Engl J Med, 324(23):1619–25. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control. Health benefits of smoking cessation: A report of the Surgeon General Office on Smoking and Health; 1990. https://www.cdc.gov/mmwr/preview/mmwrhtml/00001801.htm
- 7.Russell MA, Wilson C, Taylor C, Baker CD. (1979). Effect of general practitioners’ advice against smoking. Br Med J, 2(6184):231–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gellert C, Schöttker B, Brenner H. (2012). Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Intern Med, 172(11):837–44. [DOI] [PubMed] [Google Scholar]
- 9.Doolan DM, Froelicher ES. (2008). Smoking cessation interventions and older adults. Prog Cardiovasc Nurs,23(3):119–27. [DOI] [PubMed] [Google Scholar]
- 10.Timmermans EJ, Huisman M, Kok AA, Kunst AE. (2018). Smoking cessation and 16-year trajectories of functional limitations among Dutch older adults: Results from the Longitudinal Aging Study Amsterdam. J Gerontol A Biol Sci Med Sci, 73(12):1722–8. [DOI] [PubMed] [Google Scholar]
- 11.Maguire CP, Ryan J, Kelly A, O’Neill DE, Coakley D, Walsh JB. (2000). Do patient age and medical condition influence medical advice to stop smoking? Age Ageing, 29(3):264–6. [DOI] [PubMed] [Google Scholar]
- 12.Scholz J, Santos PCJL, Buzo CG, et al. (2016). Effects of aging on the effectiveness of smoking cessation medication. Oncotarget, 7(21):30032–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Çelik İ, Yüce D, Hayran M, et al. (2015). Nationwide smoking cessation treatment support program–Turkey project. Health Policy,119(1):50–6. [DOI] [PubMed] [Google Scholar]
- 14.Fagerstrom KO, Schneider NG. (1989). Measuring nicotine dependence: a review of the Fagerstrom Tolerance Questionnaire. J Behav Med, 12(2):159–82. [DOI] [PubMed] [Google Scholar]
- 15.Gunay T, Pekel O, Simsek H, et al. (2014). Smoking habits and cessation success. Saudi Med J, 35(6):585–91. [PubMed] [Google Scholar]
- 16.Burstein AH, Fullerton T, Clark DJ, Faessel HM. (2006). Pharmacokinetics, safety, and tolerability after single and multiple oral doses of varenicline in elderly smokers. J Clin Pharmacol, 46(11):1234–40. [DOI] [PubMed] [Google Scholar]
- 17.Chang CP, Huang WH, You CH, Hwang LC, Lu IJ, Chan HL. (2019). Factors correlated with smoking cessation success in older adults: a retrospective cohort study in Taiwan. Int J Environ Res Public Health, 16(18):3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yüce GD, Duru S, Ulaşlı SS, Ardıç S. (2013). Sıgara Bırakma Tedavısının 65 Yaş Ve Üzeri Hastalardaki Etkinliği. Turkish Journal of Geriatrics,16(3):309–14. [Google Scholar]
- 19.Abdullah AS, Lam TH, Chan SK, et al. (2008). Effectiveness of a mobile smoking cessation service in reaching elderly smokers and predictors of quitting. BMC Geriatr, 8:25. [DOI] [PMC free article] [PubMed] [Google Scholar]