Abstract
Objective: This study aims to identify facilitators and barriers of Human Papillomavirus (HPV) vaccine acceptance, initiation, and completion among LGBTQ (lesbian, gay, bisexual, trans, and queer) individuals. Method: A systematic review of qualitative and quantitative studies on HPV vaccine acceptance, initiation, and completion from 2006 to June 15, 2020 was performed in each database. Results: Twenty-six studies focusing on HPV vaccination among LGBTQ individuals were reviewed. Conclusions: Knowledge of HPV vaccine and healthcare providers’ recommendations were identified as facilitators to receive HPV vaccinate, while high co-pay cost and concerns of the effectiveness and safety were identified as barriers.
Keywords: HPV vaccine acceptance, HPV vaccine initiation, HPV vaccine completion, LGBTQ community
Introduction
The Human Papillomavirus (HPV) is a sexually transmitted virus through contact with infected anogenital skin, mucous membranes, or bodily fluids and can be passed through sexual intercourse (oral, vaginal, or anal; Ribeiro et al., 2015). The HPV can even pass through digital-oral and digital-genital contacts (Martínez & Troconis, 2014). The infection may result in genital warts and various cancers and can also be asymptomatic (Boda et al., 2016). HPV infection has become a leading cause of cervical cancers and penile cancer, by which people suffer from long-term mental and physical distress and shoulder financial burdens for treatment (Cavazos, 2017; Cunningham-Erves & Talbott, 2015; McBride et al., 2020). As the most common sexually transmitted infection in the U.S., HPV causes ∼20,700 cases in women and 14,100 cases in men each year for HPV-related cancers (CDCP, 2019).
LGBTQ (lesbian, gay, bisexual, trans, and queer) individuals are disproportionately impacted by HPV (Quinn et al., 2015). Especially for gay men, they are more likely than heterosexual men to have oral, anal, and penile HPV infections, so that it is more than 17 times higher for them to suffer anal cancer (Daling et al., 2004; Yeung et al., 2019). LGBTQ individuals are more vulnerable to HPV infection than heterosexual counterparts due to relatively low socioeconomic status, sparse healthcare utilization, more lifetime sexual partners, and multiple and concurrent risky behaviors (such as unprotected anal sex; Quinn et al., 2015; Tamargo et al., 2017). These population characteristics make LGBTQ individuals liable to suffer more negative health outcomes induced by HPV infection compared with heterosexual individuals, like anal cancer among gay men and cervical cancer among lesbian women (Boehmer et al., 2011; Chin-Hong et al., 2005).
The negative health impacts resulting from HPV-related diseases have created multiple burdens that disparately affect LGBTQ individuals in the U.S. (Reiter, Gower, et al., 2020). Financial distress from related medical treatment greatly contributes to the avoidance or delay of seeking timely healthcare services (Quinn et al., 2015). Also, LGBTQ patients are more likely to lack regular checks with healthcare providers and experience stigmatization or discrimination from healthcare providers (Quinn et al., 2015), which may promote the delay and hesitancy of seeking timely treatment for HPV-related diseases (Ceres et al., 2018). Additionally, LGBTQ individuals may also experience mental disorders like depression and anxiety due to sexual or gender identity-based stigma, substance use, or lacking regular healthcare providers (Grant et al., 2011; Hughto et al., 2015; Meyer, 2003). All of these behavioral factors, economic factors, and social factors intensify the HPV-related health burden in the LGBTQ community.
People can go many years before becoming symptomatic with HPV, and cancers from HPV can take between years or even decades to emerge after infection (Moshiri et al., 2016). HPV vaccination, therefore, plays a critical role in the prevention of cancer-causing infections and precancers, and subsequent HPV-related diseases and death (Markowitz et al., 2013; Ribeiro et al., 2015). According to CDC’s Advisory Committee on Immunization Practices (ACIP) recommendations, routine HPV vaccination is recommended at age 11 or 12 years through age 26 years and can be started as early as age 9 (CDCP, 2016). HPV vaccination is recommended to be given as a series of either two or three doses, and the extant HPV vaccines only work for some of the strains of HPV viruses, such as types 6, 11, 16, 18, 31, 33, 45, 52, and 58 (Gallego et al., 2020). Due to potential HPV exposure, those aged 27–45 years are recommended to discuss vaccination with their healthcare provider since they may benefit less from the HPV vaccination (CDCP, 2016).
It is worth noting that HPV vaccine acceptance, initiation, and completion are much lower among LGBTQ individuals than heterosexual individuals (Bernat et al., 2013; Eaton et al., 2008; Power et al., 2009). Compared to lesbians, heterosexual females (56%) were 20% more likely to have received at least one dose (Charlton et al., 2017). Moreover, many men who have sex with men are generally less likely to be recommended with the HPV vaccine by their health care providers, as many healthcare professionals do not routinely assess sexual orientation or trans and non-binary identities and then do not recommend HPV vaccines (Nadarzynski et al., 2014; National Cancer Institute, 2014). The previous study suggests that the LGBTQ community is well-educated about the HPV vaccine compared to the general population (Ong et al., 2013). Unfortunately, the good awareness of the HPV vaccine did not translate into increased HPV vaccination rates in the LGBTQ community because LGBTQ individuals perceived greater barriers (i.e., vaccine availability and affordability) to getting vaccinated (Reiter et al., 2015).
Given the disparities of HPV infections and HPV vaccination among LGBTQ individuals, burgeoning research focuses on HPV among LGBTQ individuals, including LGBTQ individuals’ HPV vaccine acceptance, initiation, and completion. Understanding facilitators and barriers can support evidence-based practice to reduce barriers to access HPV vaccines among LGBTQ individuals and to develop effective interventions to promote HPV vaccination rates for LGBTQ individuals. In current literature, an array of reviews focused on cervical cancer prevention in minority populations, including LGBTQ individuals (Lott et al., 2020; Spencer et al., 2019). However, these reviews did not provide detailed information on HPV vaccination in the LGBTQ community. Therefore, a systematic review focusing on LGBTQ individuals’ HPV vaccine use is needed to explore possibilities of reducing the cervical cancer burden in the LGBTQ community. To our best knowledge, this is the first study that comprehensively reviews quantitative and qualitative studies on HPV vaccine acceptance, initiation, and completion, focusing on LGBTQ individuals. To promote cervical cancer care equality in the LGBTQ community, we aim to identify facilitators and barriers of HPV vaccine acceptance, initiation, and completion among the LGBTQ community. This study is to provide valuable implications for health care practitioners, researchers, and policymakers for better prevention of HPV and HPV-related diseases.
Method
Searching strategy
Since Gardasil, the first-generation HPV vaccine, was first approved by the FDA in 2006, PubMed, Web of Science, PsycINFO, and CINAHL were searched by three researchers (Y.G., Z.H., and M.L.) for articles ranging from 2006 to June 15, 2020. Furthermore, we expanded the search by consulting other sources, including references of related articles and other reviews on the HPV vaccination, to identify potential studies. According to the Cochrane Handbook, the searching terms were comprised of a combination of thesaurus with a wide range of free-text terms. Two researchers (Y.G. and M.L.) conducted a scoping search before the main search to identify keywords to index HPV vaccine utilization among LGBTQ individuals. Then, a discussion was conducted among the three authors to resolve any disagreements. The search terms were built up by a scoping search and after the agreement reached: (papillomavirus infections OR human papillomavirus OR HPV) AND (vaccines OR papillomavirus vaccines) AND (LGBTQ OR gay* OR lesbian* OR bisexual OR transgender* OR men who have sex with men OR MSM OR women have sex with women OR WSW) AND (accept* OR aware* OR attitude* OR belief* OR behave* OR decision OR decide OR intent* OR know* OR perceived* OR percept* OR risk* OR uptake* OR coverage OR vaccination OR mass vaccination OR decision making). The search terms listed above and the electronic search strategy are the same in each database.
Inclusion and exclusion criteria
The inclusion criteria of this review are studies that: (1) reported data on HPV vaccination coverage among LGBTQ individuals; (2) reported in the English language; (3) reported at least one of the factors associated with HPV vaccination; (4) include data collected from surveys, clinical trial studies and/or qualitative data; (5) focus on the U.S. healthcare system; (6) focus on LGBTQ individuals. Using Rayyan (Ouzzani et al., 2016), a software for systematic review, the three authors read all the titles, abstracts, and full text with applying the inclusion criteria to determine full-text eligibility. Modeling studies, cost-effectiveness studies, reviews, and opinion pieces were excluded. We also excluded studies that mainly focused on HPV vaccination in heterosexual people or cisgender individuals as well as studies that mainly focused on cervical cancer screening and not HPV vaccination.
Coding strategy
The data were analyzed from the included studies. Two investigators (Z.H. and Y.G.) identified and coded facilitators and barriers of (1) HPV vaccine acceptance; (2) HPV vaccine initiation; and (3) HPV vaccine completion among LGBTQ individuals. Results reported in the included studies were coded into two categories: facilitators and barriers. The initial agreement rate in the research team ranged from 85 to 90%. All disagreements were discussed and solved through weekly research meetings. Finally, we have successfully achieved an agreement rate of 100%.
Risk of bias
Included studies were critically appraised. According to Cochran’s quality of evidence guidelines (Higgins & Thomas, 2020), the included quantitative studies were assessed with the following potential biases for low risk, moderate risk, and high risk: selection biases, performance biases, detection biases, attrition biases, and reporting biases. Each item was scored as follows: 0 = Weak, 1 = Moderate, and 2 = Strong (range: 0–10). All items were summed to represent the potential biases: low risk ≤ 3, moderate risk: 4–7, and high risk ≥ 8.
The included qualitative studies’ trustworthiness was assessed by the “Rationale and standards for the systematic review of qualitative literature in health services research” (Popay et al., 1998). Five items were used to represent potential threats for low risk, moderate risk, and high risk: theoretical basis, sampling strategy, the scope of data collection, description of data collection, and concern with generalizability or typicality. The risk of bias was scored as follows: (1) High risk: two or more weak ratings; (2) Moderate risk: one weak rating; and (3) Low risk: no weak ratings.
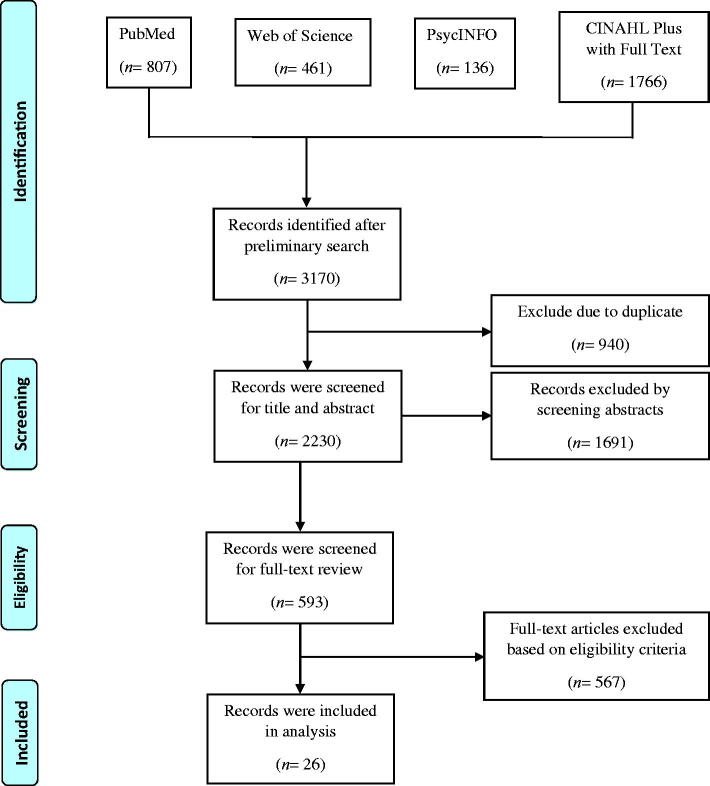
As a review of extant study reports, this review was deemed by the Institutional Review Board of the local university to be exempt from ethical approval (Figure 1).
Results
The present review identified 26 studies that met the inclusion criteria conducted from 2010 to 2020 in the U.S., no studies met the inclusion criteria between 2006 and 2009. Among these studies, there were 21 studies of men who have sex with men (MSM), 12 studies of bisexual men and bisexual women, and seven studies of women who have sex with women (WSW). Since only four studies were conducted among trans and queer individuals in total, we grouped them for the discussion. There were 21 quantitative studies and most of them had a low risk of bias (n = 13), the remainder of studies had a moderate risk of bias (n = 8). There were five qualitative studies that all had a low risk of bias.
Facilitators and barriers of HPV vaccine were identified respectively for acceptance, initiation, and completion of HPV vaccination in each subpopulation based on identity, including men who have sex with men (MSM), bisexual men and bisexual women, women who have sex with women (WSW), and trans and queer individuals (Supplementary Tables 1–4). Detailed information of each included study is shown in Tables 1.
Table 1.
Summary of included studies
| Studies | Participants and Design | Facilitators/ Barriers | HPV Vaccine Outcome | Type of Study/ Risk of Bias |
|---|---|---|---|---|
| Agénor et al. (2020) |
|
Facilitators
|
Initiation |
|
| Gerend et al. (2019) |
|
Facilitators
|
|
|
| Loretan et al. (2019) |
|
Facilitators
|
Initiation |
|
| Koskan & Fernández- Pineda, (2018) |
|
Facilitators
|
|
|
| Bednarczyk et al. (2017) |
|
Facilitators
|
Initiation |
|
| Gorbach et al. (2017) |
|
Facilitators
|
Initiation |
|
| Oliver et al. (2017) |
|
Facilitators
|
Initiation |
|
| Polek & Hardie. (2017) |
|
Facilitators
|
Initiation |
|
| Wheldon et al. (2017) |
|
Facilitators
|
Initiation |
|
| Fontenot et al. (2016) |
|
Facilitators
|
|
|
| Gerend et al. (2016) |
|
Facilitators
|
Initiation |
|
| Jones et al. (2016) |
|
Facilitators
|
Acceptance |
|
| Makris et al. (2016) |
|
Facilitators
|
Initiation |
|
| Agénor et al., (2015) |
|
Facilitators
|
|
|
| Cummings et al. (2015) |
|
Facilitators
|
Acceptance Initiation |
|
| Onyeabor et al. (2015) |
|
Barriers
|
Acceptance |
|
| Reiter et al. (2015) |
|
Facilitators
|
|
|
| McRee et al. (2014) |
|
Facilitators
|
|
|
| Meites et al. (2014) |
|
Facilitators
|
Initiation |
|
| Ong et al. (2013) |
|
Facilitators
|
Acceptance |
|
| Gilbert et al. (2011) |
|
Facilitators
|
Acceptance |
|
| Gilbert et al. (2011) |
|
Facilitators
|
Acceptance |
|
| Thomas & Goldstone, (2011) |
|
Facilitators
|
Acceptance |
|
| Wheldon et al. (2011) |
|
Facilitators
|
Acceptance |
|
| Hollander (2010) |
|
Facilitators
|
Acceptance |
|
| Reiter et al. (2010) |
|
Facilitators
|
Acceptance |
|
For MSM, most of the identified facilitators affected whether they would initiate the HPV vaccine uptake. Among those, knowledge of HPV, medical diagnosis of any sexually transmitted diseases, access to healthcare, and sexual orientation disclosure were major facilitators. Other facilitators also influenced their HPV vaccine initiation, including having health insurance, perceived self-efficacy, affordable cost, age, education level, and urban setting. The number of sex partners influenced their HPV vaccine acceptance. For HPV vaccine completion, knowledge of HPV vaccine and healthcare providers' recommendations played a vital role. Most of the identified barriers affected whether MSM would complete their HPV vaccine uptake. Among those, high co-pay cost, lack of knowledge of HPV vaccine, and concerns of the effectiveness and safety of HPV vaccine were major barriers. Other barriers also impeded their HPV vaccine completion, including lack of recommendation from the health care providers, lack of health insurance, lack of vaccine accessibility, sexual orientation-related stigma, and inconvenience of vaccine uptake. The medical diagnosis of any sexually transmitted diseases hindered their HPV vaccine acceptance, and lack of HPV knowledge impeded whether they would initiate the HPV vaccination.
For bisexual men and bisexual women, identified facilitators like the number of sex partners and perceived self-efficacy affected whether they would accept the HPV vaccination. Access to healthcare, bisexual behaviors, and having health insurance influenced their HPV vaccine initiation. Knowledge of HPV, knowledge of the HPV vaccine, and healthcare providers' recommendations were major facilitators for their HPV vaccine completion. Other facilitators also affected their HPV vaccine completion, including education level and social support. The identified barriers all focused on the HPV vaccine completion. Among those, concerns of the effectiveness and safety of the HPV vaccine and high co-pay cost are major barriers. The remainder barriers also impeded their HPV vaccine completion, including lack of vaccine accessibility, lack of knowledge of HPV vaccine, lack of recommendations from the health care providers, inconvenience of vaccine uptake, and sexual orientation-related stigma.
For WSW, the most commonly identified facilitators affecting whether they would complete the HPV vaccination, including knowledge of the HPV vaccine, education level, knowledge of HPV, and recommendations from the health care providers. Having sex with different genders of partners and have health insurance influence their HPV vaccine initiation. The identified barriers all focused on the HPV vaccine initiation, including concerns about the effectiveness and safety of the HPV vaccine and lack of vaccine accessibility.
For trans and queer individuals, in terms of facilitators, knowledge of HPV affected their HPV vaccine acceptance. Education level, medical diagnosis of any sexually transmitted diseases, and have health insurance influenced their HPV vaccine initiation. Recommendations from the health care providers, knowledge of HPV vaccine, and social support affected whether they would complete their HPV vaccination. The identified barriers all focused on the HPV vaccine completion, including concerns of the effectiveness and safety of HPV vaccine, inconvenience of vaccine uptake, lack of knowledge of HPV vaccine, lack of vaccine accessibility, gender identity-related stigma, and high co-pay cost.
Discussion
In this systematic review, the facilitators and barriers of acceptance, initiation, and completion of HPV vaccine were identified respectively among MSM, WSW, bisexual men and bisexual women, and trans and queer individuals. We found that facilitators that motivate HPV vaccination uptake and barriers to accessing or completing the vaccination are varied across LGBTQ groups.
Acceptance of HPV vaccine
MSM and bisexual men and bisexual women reported the number of sex partners affected HPV vaccine acceptance. Higher numbers of sexual partners increased the likelihood of individuals being willing to get vaccinated (Hollander, 2010). Having multiple sex partners increases the likelihood of exposure to sexually transmitted infections and drastically increases the possibility of HPV infection (McPartland et al., 2005). Being aware of this fact, LGBTQ individuals may seek approaches to protect themselves and their sexual partners from the infection, such as the HPV vaccine (Jiamton et al., 2014).
Bisexual men and bisexual women also reported perceived self-efficacy plays a role in their decision to accept the HPV vaccine. Self-efficacy beliefs are cognitions that determine whether health-seeking behaviors will be initiated and how high the health goals will be set (Zimmerman, 2018). Especially for bisexual men, anal sex increases the possibility of getting sexually transmitted viruses like HIV and HPV (Donà et al., 2012). In addressing this stressful situation, people often exhibit negative mental health symptoms like fear, anxiety, and depression (Pachankis, 2014). Self-efficacy facilitates bisexual men not only reducing mental health disorders but also protecting themselves from being infected (Fallin-Bennett et al., 2016). When bisexual men have multiple relationships, including secret relationships or behaviors, self-efficacy can greatly motivate them to find ways to protect themselves and to protect their partners concurrently, such as through HPV vaccination (Wheldon, 2015).
Trans and queer individuals reported that the knowledge of HPV facilitated their decision-making in accepting the HPV vaccine. Being aware of how HPV transmits, the severity of infection, and how the infection affects their life increases HPV-related health literacy (Reiter, Bustamante, et al., 2020). In turn, higher HPV-related health literacy contributes to greater HPV vaccine acceptance (Wigfall et al., 2020).
MSM reported that a medical diagnosis of any sexually transmitted infection (STI) was a barrier to HPV vaccine acceptance. As the HPV vaccine serves as a prevention measure and does not treat any existing HPV-related diseases or infections, this may impede people who are already infected with HPV to accept the HPV vaccine (Vorsters et al., 2015). People may also reject the HPV vaccine if they have another STI and do not have knowledge of HPV and the HPV vaccine (Rosenbloom & Killian, 2014). Therefore, HPV-related education is indispensable to promote HPV-related health literacy and the HPV vaccine and self-efficacy among LGBTQ individuals (Gaspar et al., 2018; Wigfall et al., 2020).
Initiation of HPV vaccine
MSM reported that affordable cost played a vital role in facilitating their initiation of the HPV vaccine. The total direct medical expenditure for prevention, management, and treatment of HPV-related diseases or infections is ∼$1.7 billion (range from $800 million to $2.9 billion), which is the highest among all STIs in the U.S., causing a huge burden to patients and medical system (Mayeaux, 2008; Owusu-Edusei et al., 2013). Therefore, possible ways to reduce the financial burden are needed to provide LGBTQ individuals with substantial access to HPV-related healthcare (Carter, 2017). A feasible and necessary approach is to expand health insurance coverage to benefit more qualified LGBTQ individuals (Kaur, 2016). This will ease access to healthcare services, including HPV vaccination initiation. It further reduces the unnecessary financial burden for treatment among LGBTQ individuals and mitigates the stress of the healthcare system in providing advanced treatments (Wigfall et al., 2018). MSM, bisexual men, and bisexual women, WSW, and trans and queer individuals all reported that having health insurance contributes to their HPV vaccine initiation due to concerns of cost.
Education level is a preeminent facilitator for HPV vaccine initiation among MSM, trans, and queer individuals. Higher education level is related to higher HPV-related health literacy, and from which often comes with higher self-efficacy to gain more HPV-related knowledge (Gallardo et al., 2020). Specifically, when people get a diagnosis of any STI, self-efficacy influences their ability to acquire knowledge about how to treat, manage, or prevent subsequent transmission or outbreaks (Krawczyk et al., 2013). Also, those with higher self-efficacy tend to disclose sexual or gender identity to their healthcare providers to obtain proper recommendations and more related knowledge (Venetis et al., 2017). However, school-based sex education is commonly limited due to the organizational culture and LGBTQ individuals are often not mentioned in sexual health education programmes, materials, and policies (Leung et al., 2020; Reiter & McRee, 2017). This fact makes lack of knowledge a barrier for MSM specifically to initiate HPV vaccine. Prompt action is needed to offer follow-up education to facilitate them to gain more understanding and knowledge of whether they are eligible to be vaccinated, especially for those who have a lower education level.
WSW, bisexual men, and bisexual women reported that having sexual behaviors at the risk of HPV facilitated their HPV vaccine initiation. When they experience sexual debut or have multiple sex partners, they are more likely to recognize the risk of HPV infection (Dunne et al., 2007; Gerend & Magloire, 2008). This cognition may increase their self-efficacy to seek proper healthcare services to protect both themselves and their sex partners (Gerend et al., 2019).
Completion of HPV vaccine
The facilitators and barriers of completion of HPV vaccine were highly convergent for all subgroups in this systematic review. Similar to the facilitators of initiation of the HPV vaccine, education level, knowledge of HPV, and knowledge of HPV vaccine facilitate LGBTQ individuals to further complete their HPV vaccination. Therefore, enhancing HPV-related and HPV vaccine-related education for LGBTQ individuals is essential, especially for those who have a lower education level.
Obtaining recommendations from healthcare providers through healthcare utilization greatly motivated LGBTQ individuals to finish the HPV vaccination. Healthcare providers play an irreplaceable role in providing HPV-related and HPV vaccine-related education for LGBTQ individuals during their HPV vaccination decision-making process (Jaiswal et al., 2020). Education can alleviate possible concerns of the effectiveness and safety of HPV vaccine and offer recommendations for LGBTQ individuals in terms of HPV prevention and management (McRee et al., 2014). However, LGBTQ individuals may not disclose their sexual or gender identities when they perceive stigma from healthcare providers (Apaydin et al., 2018). It results in the lack of necessary communication between patients and healthcare providers and by which HPV-related and HPV vaccine-related education are more likely to be omitted (Jaiswal et al., 2020). This fact further impedes or limits access to HPV-related knowledge and services, especially for those who lack the knowledge to finish the HPV vaccination. Even worse, healthcare providers may not have related knowledge to initiate any education or question prompts for LGBTQ patients related to HPV (Gilbert et al., 2011a). As a result, healthcare providers should be trained on HPV-related and HPV vaccine-related knowledge specific to LGBTQ individuals so that effective education and recommendations can be offered to facilitate the LGBTQ community to gain related knowledge to complete all three-doses of the HPV vaccine.
Social support from friends, family members, and intimate partners encourage and facilitate HPV vaccine completion among the LGBTQ community. Social support aids in alleviating HPV-related stigma and provides necessary assistance in reducing vaccine uptake inconveniences, like transportation to healthcare centers (Richardson, 2016). Financial support also releases burdens in direct medical cost of HPV vaccine uptake (Rosenbloom & Killian, 2014). However, social support is limited in addressing high co-pay costs to complete HPV vaccination (Medder, 2016). Health insurance coverage needs to be expanded to benefit more LGBTQ individuals to cover medical expenditures (Wheldon et al., 2011).
This review conducts an assessment of the risk of bias to report the quality of the included studies, showing that among all the 26 included studies, eight are of moderate quality and are all quantitative studies. According to the assessment standard, factors contributing to the classification of being moderate risk specifically relate to the methodology of the study, such as selection biases and performance biases. This result may prompt researchers in the future to pay more attention to the methodology to conduct the study and also provide references for future meta-analysis studies to achieve deeper understandings of the HPV vaccine among LGBTQ individuals.
Limitations
It is important to note the limitations of this review to encourage future studies to improve HPV vaccination research among the LGBTQ community. Although we applied a comprehensive searching process, it is possible that some potentially eligible studies were missed due to the search terms used in this study. To reduce this risk, we applied several strategies like an extensive searching process and multiple screenings to verify eligible studies for this systematic review. Even so, studies not available in English or gray literature (e.g., unpublished studies, dissertations, and abstracts) were not included in this study due to authors’ language barriers and access limitations to the sources. Another limitation is this review focused on the U.S. only, exploring possible facilitators and barriers of HPV vaccination under U.S. policies. Future studies may broaden this criterion to focus on multiple countries and regions to offer a more comprehensive understanding or comparison of this topic from different social welfare systems and cultural backgrounds. Despite these limitations, our review provides an essential contribution to understanding facilitators and barriers of HPV vaccine acceptance, initiation, and completion among LGBTQ individuals.
Conclusion
This review critically examined and summarized 26 studies focusing on the facilitators and barriers of HPV vaccine acceptance, initiation, and completion among LGBTQ individuals. Among all identified facilitators and barriers, knowledge of HPV, knowledge of HPV vaccine, and recommendations from the healthcare providers are commonly reported facilitators. Lack of knowledge of HPV vaccine, high co-pay cost, and concerns of the effectiveness and safety of HPV vaccine are highly reported barriers. Therefore, enhancing and improving HPV-related and HPV vaccine-related education and follow-ups to LGBTQ individuals is essential, especially for those with lower levels of education. Besides, professional training for healthcare providers to improve their HPV-related and HPV vaccine-related knowledge is necessary so that effective education and recommendations can be offered to facilitate LGBTQ individuals to complete all three doses of the HPV vaccine. Health insurance coverage also needs to be expanded to benefit more LGBTQ individuals to release their financial burden in direct medical costs to provide more access to HPV-related healthcare. Considering inadequate health insurance coverage and financial constraints are major barriers to receive HPV vaccines in LGBTQ individuals (Qureshi et al., 2018), policymakers may provide more free vaccination programs, such as the Merck Patient Assistance Program, to offer vaccines free of charge to the uninsured but eligible individuals.
Figure 1.
The flow diagram of the study selection process.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Agénor, M., Murchison, G. R., Chen, J. T., Bowen, D. J., Rosenthal, M. B., Haneuse, S., & Austin, S. B. (2020). Impact of the Affordable Care Act on human papillomavirus vaccination initiation among lesbian, bisexual, and heterosexual US women. Health Services Research, 55(1), 18–25. 10.1111/1475-6773.13231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agénor, M., Peitzmeier, S., Gordon, A. R., Haneuse, S., Potter, J. E., & Austin, S. B. (2015). Sexual orientation identity disparities in awareness and initiation of the human papillomavirus vaccine among U.S. women and girls: A national survey. Annals of Internal Medicine, 163(2), 99–106. 10.7326/M14-2108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apaydin, K. Z., Fontenot, H. B., Shtasel, D., Dale, S. K., Borba, C. P., Lathan, C. S., Panther, L., Mayer, K. H., & Keuroghlian, A. S. (2018). Facilitators of and barriers to HPV vaccination among sexual and gender minority patients at a Boston community health center. Vaccine, 36(26), 3868–3875. 10.1016/j.vaccine.2018.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednarczyk, R. A., Whitehead, J. L., & Stephenson, R. (2017). Moving beyond sex: Assessing the impact of gender identity on human papillomavirus vaccine recommendations and uptake among a national sample of rural-residing LGBT young adults. Papillomavirus Research, 3, 121–125. 10.1016/j.pvr.2017.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernat, D. H., Gerend, M. A., Chevallier, K., Zimmerman, M. A., & Bauermeister, J. A. (2013). Characteristics associated with initiation of the human papillomavirus vaccine among a national sample of male and female young adults. The Journal of Adolescent Health, 53(5), 630–636. 10.1016/j.jadohealth.2013.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boda, D., Neagu, M., Constantin, C., Voinescu, R. N., Caruntu, C., Zurac, S., Spandidos, D. A., Drakoulis, N., Tsoukalas, D., & Tsatsakis, A. M. (2016). HPV strain distribution in patients with genital warts in a female population sample. Oncology Letters, 12(3), 1779–1782. 10.3892/ol.2016.4903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehmer, U., Miao, X., & Ozonoff, A. (2011). Cancer survivorship and sexual orientation. Cancer, 117(16), 3796–3804. 10.1002/cncr.25950 [DOI] [PubMed] [Google Scholar]
- Carter, G. A. (2017). Interplay of agency, community, and attitudinal factors related to HIV pre-exposure prophylaxis by advanced practice nurses in Indiana. Indiana University. [DOI] [PubMed] [Google Scholar]
- Cavazos, S. (2017). Initiating HPV co-testing for women aged 30–65 in an Ob/Gyn practice setting. [Google Scholar]
- Centers for Disease Control and Prevention (2016). Human papillomavirus (HPV) ACIP vaccine recommendations. Series. https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/hpv.html
- Centers for Disease Control and Prevention (2019, August). How many cancers are linked with HPV each year? [Google Scholar]
- Ceres, M., Quinn, G. P., Loscalzo, M., & Rice, D. (2018). Cancer screening considerations and cancer screening uptake for lesbian, gay, bisexual, and transgender persons. In Seminars in oncology nursing (Vol. 34, pp. 37–51). Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton, B. M., Reisner, S. L., Agenor, M., Gordon, A. R., Sarda, V., & Austin, S. B. (2017). Sexual orientation disparities in human papillomavirus vaccination in a longitudinal cohort of US males and females. LGBT Health, 4(3), 202–209. 10.1089/lgbt.2016.0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin-Hong, P. V., Vittinghoff, E., Cranston, R. D., Browne, L., Buchbinder, S., Colfax, G., Da Costa, M., Darragh, T., Benet, D. J., Judson, F., Koblin, B., Mayer, K. H., & Palefsky, J. M. (2005). Age-related prevalence of anal cancer precursors in homosexual men: The EXPLORE study. Journal of the National Cancer Institute, 97(12), 896–905. 10.1093/jnci/dji163 [DOI] [PubMed] [Google Scholar]
- Cummings, T., Kasting, M. L., Rosenberger, J. G., Rosenthal, S. L., Zimet, G. D., & Stupiansky, N. W. (2015). Catching up or missing out? Human papillomavirus vaccine acceptability among 18- to 26-year-old men who have sex with men in a US national sample. Sexually Transmitted Diseases, 42(11), 601–606. 10.1097/OLQ.0000000000000358 [DOI] [PubMed] [Google Scholar]
- Cunningham-Erves, J., & Talbott, L. L. (2015). HPV vaccination of college males: Strategizing against HPV infection in college students. College Student Journal, 49(4), 565–571. [Google Scholar]
- Daling, J. R., Madeleine, M. M., Johnson, L. G., Schwartz, S. M., Shera, K. A., Wurscher, M. A., Carter, J. J., Porter, P. L., Galloway, D. A., & McDougall, J. K. (2004). Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer, 101(2), 270–280. [DOI] [PubMed] [Google Scholar]
- Donà, M. G., Palamara, G., Di Carlo, A., Latini, A., Vocaturo, A., Benevolo, M., Pimpinelli, F., Giglio, A., Moretto, D., Impara, G., & Giuliani, M. (2012). Prevalence, genotype diversity and determinants of anal HPV infection in HIV-uninfected men having sex with men. Journal of Clinical Virology, 54(2), 185–189. [DOI] [PubMed] [Google Scholar]
- Dunne, E. F., Unger, E. R., Sternberg, M., McQuillan, G., Swan, D. C., Patel, S. S., & Markowitz, L. E. (2007). Prevalence of HPV infection among females in the United States. JAMA, 297(8), 813–912. 10.1001/jama.297.8.813 [DOI] [PubMed] [Google Scholar]
- Eaton, L., Kalichman, S., Cain, D., Cherry, C., Pope, H., Fuhrel, A., & Kaufman, M. (2008). Perceived prevalence and risks for human papillomavirus (HPV) infection among women who have sex with women. Journal of Women's Health, 17(1), 75–84. [DOI] [PubMed] [Google Scholar]
- Fallin-Bennett, K., Henderson, S. L., Nguyen, G. T., & Hyderi, A. (2016). Primary care, prevention, and coordination of care. In Lesbian, gay, bisexual, and transgender healthcare (pp. 95–114). Springer. [Google Scholar]
- Fontenot, H. B., Fantasia, H. C., Vetters, R., & Zimet, G. D. (2016). Increasing HPV vaccination and eliminating barriers: Recommendations from young men who have sex with men. Vaccine, 34(50), 6209–6216. 10.1016/j.vaccine.2016.10.075 [DOI] [PubMed] [Google Scholar]
- Gallardo, K. R., Santa Maria, D., Narendorf, S., Markham, C. M., Swartz, M. D., Hsu, H. T., Barman-Adhikari, A., Bender, K., Shelton, J., & Ferguson, K. (2020). Human papillomavirus vaccination initiation and completion among youth experiencing homelessness in seven US cities. Prevention Science, 21(7), 937–948. 10.1007/s11121-020-01131-5 [DOI] [PubMed] [Google Scholar]
- Gallego, L. S., Dominguez, A., & Parmar, M. (2020). Human papilloma virus (HPV) vaccine. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK562186/
- Gaspar, M., Grennan, T., Salit, I., & Grace, D. (2018). Confronting comorbidity risks within HIV biographies: Gay men’s integration of HPV-associated anal cancer risk into their narratives of living with HIV. Health, Risk & Society, 20(5–6), 276–296. 10.1080/13698575.2018.1519114 [DOI] [Google Scholar]
- Gerend, M. A., Madkins, K., Crosby, S., Korpak, A. K., Phillips, G., Bass, M., Houlberg, M., & Mustanski, B. (2019). A qualitative analysis of young sexual minority men's perspectives on human papillomavirus vaccination. LGBT Health, 6(7), 350–356. 10.1089/lgbt.2019.0086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend, M. A., Madkins, K., Gregory Phillips, I. I., & Mustanski, B. (2016). Predictors of human papillomavirus vaccination among young men who have sex with men. Sexually Transmitted Diseases, 43(3), 185–191. 10.1097/OLQ.0000000000000408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend, M. A., & Magloire, Z. F. (2008). Awareness, knowledge, and beliefs about human papillomavirus in a racially diverse sample of young adults. The Journal of Adolescent Health, 42(3), 237–242. 10.1016/j.jadohealth.2007.08.022 [DOI] [PubMed] [Google Scholar]
- Gilbert, P. A., Brewer, N. T., & Reiter, P. L. (2011a). Association of human papillomavirus-related knowledge, attitudes, and beliefs with HIV status: A national study of gay men. Journal of Lower Genital Tract Disease, 15(2), 83–88. 10.1097/LGT.0b013e3181f1a960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert, P. A., Brewer, N. T., Reiter, P. L., Ng, T. W., & Smith, J. S. (2011b). HPV vaccine acceptability in heterosexual, gay, and bisexual men. American Journal of Men's Health, 5(4), 297–305. 10.1177/1557988310372802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbach, P. M., Cook, R., Gratzer, B., Collins, T., Parrish, A., Moore, J., Kerndt, P. R., Crosby, R. A., Markowitz, L. E., & Meites, E. (2017). Human papillomavirus vaccination among young men who have sex with men and transgender women in 2 US cities, 2012–2014. Sexually Transmitted Diseases, 44(7), 436–441. 10.1097/OLQ.0000000000000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, J. M., Motter, L. A., & Tanis, J. (2011). Injustice at every turn: A report of the national transgender discrimination survey. [Google Scholar]
- Higgins, J. P. T., & Thomas, J. (2020). Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. Retrieved from www.training.cochrane.org/handbook.
- Hollander, D. (2010). Gay and bisexual men are largely receptive to HPV vaccination. Perspectives on Sexual and Reproductive Health, 42(3), 218–218. 10.1363/4221810_1 [DOI] [Google Scholar]
- Hughto, J. M. W., Reisner, S. L., & Pachankis, J. E. (2015). Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Social Science & Medicine, 147, 222–231. 10.1016/j.socscimed.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaiswal, J., LoSchiavo, C., Maiolatesi, A., Kapadia, F., & Halkitis, P. N. (2020). Misinformation, gendered perceptions, and low healthcare provider communication around HPV and the HPV vaccine among young sexual minority men in New York City: The P18 cohort study. Journal of Community Health, 45(4), 702–711. 10.1007/s10900-019-00784-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiamton, S., Leeyaphan, C., Maneeprasopchoke, P., & Omcharoen, V. (2014). Prevalence and clinical manifestations of male patients with anogenital warts attending a sexually transmitted disease clinic prior HPV vaccine recommendation. The Southeast Asian Journal of Tropical Medicine and Public Health, 45(6), 1337–1343. [PubMed] [Google Scholar]
- Jones, J., Parrish, A., Collins, T., & Chang, P. (2016). HPV vaccine acceptance among a sample of Southern men who have sex with men: A comparison of younger and older men. Journal of Gay & Lesbian Social Services, 28(3), 245–254. 10.1080/10538720.2016.1191404 [DOI] [Google Scholar]
- Kaur, L. (2016). The development, implementation, and evaluation of a transgender health resource bundle. [Google Scholar]
- Koskan, A. M., & Fernández-Pineda, M. (2018). Human papillomavirus vaccine awareness among HIV-positive gay and bisexual men: A qualitative study. LGBT Health, 5(2), 145–149. 10.1089/lgbt.2017.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk, A., Stephenson, E., Perez, S., Lau, E., & Rosberger, Z. (2013). Deconstructing human papillomavirus (HPV) knowledge: Objective and perceived knowledge in males’ intentions to receive the HPV vaccine. American Journal of Health Education, 44(1), 26–31. 10.1080/19325037.2012.749714 [DOI] [Google Scholar]
- Leung, E., Wanner, K. J., Senter, L., Brown, A., & Middleton, D. (2020). What will it take? Using an implementation research framework to identify facilitators and barriers in implementing a school-based referral system for sexual health services. BMC Health Services Research, 20(1), 1–12. 10.1186/s12913-020-05147-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loretan, C., Chamberlain, A. T., Sanchez, T., Zlotorzynska, M., & Jones, J. (2019). Trends and characteristics associated with human papillomavirus vaccination uptake among men who have sex with men in the United States, 2014–2017. Sexually Transmitted Diseases, 46(7), 465–473. 10.1097/OLQ.0000000000001008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lott, B. E., Okusanya, B. O., Anderson, E. J., Kram, N. A., Rodriguez, M., Thomson, C. A., Rosales, C., & Ehiri, J. E. (2020). Interventions to increase uptake of human papillomavirus (HPV) vaccination in minority populations: A systematic review. Preventive Medicine Reports, 19, 101163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makris, N., Vena, C., & Paul, S. (2016). Rate and predictors of human papillomavirus vaccine uptake among women who have sex with women in the United States, the National Health and Nutrition Examination Survey, 2009–2012. Journal of Clinical Nursing, 25(23–24), 3619–3627. 10.1111/jocn.13491 [DOI] [PubMed] [Google Scholar]
- Markowitz, L. E., Hariri, S., Lin, C., Dunne, E. F., Steinau, M., McQuillan, G., & Unger, E. R. (2013). Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. The Journal of Infectious Diseases, 208(3), 385–393. 10.1093/infdis/jit192 [DOI] [PubMed] [Google Scholar]
- Martínez, G. G., & Troconis, J. N. (2014). Natural history of the infection for human papillomavirus: an actualization. Investigacion Clinica, 55(1), 82–91. [PubMed] [Google Scholar]
- Mayeaux, E. J. Jr. (2008). Reducing the economic burden of HPV-related diseases. Journal of the American Osteopathic Association, 108(4 Supplement 2), S2–S7. [PubMed] [Google Scholar]
- McBride, E., Marlow, L. A. V., Forster, A. S., Ridout, D., Kitchener, H., Patnick, J., & Waller, J. (2020). Anxiety and distress following receipt of results from routine HPV primary testing in cervical screening: The psychological impact of primary screening (PIPS) study. International Journal of Cancer, 146(8), 2113–2121. 10.1002/ijc.32540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPartland, T. S., Weaver, B. A., Lee, S.-K., & Koutsky, L. A. (2005). Men’s perceptions and knowledge of human papillomavirus (HPV) infection and cervical cancer. Journal of American College Health, 53(5), 225–230. [DOI] [PubMed] [Google Scholar]
- McRee, A.-L., Katz, M. L., Paskett, E. D., & Reiter, P. L. (2014). HPV vaccination among lesbian and bisexual women: Findings from a national survey of young adults. Vaccine, 32(37), 4736–4742. 10.1016/j.vaccine.2014.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medder, J. (2016). Caring for men who have sex with men. In Men’s health in primary care (pp. 283–300). Springer. [Google Scholar]
- Meites, E., Markowitz, L. E., Paz-Bailey, G., & Oster, A. M, NHBS Study Group (2014). HPV vaccine coverage among men who have sex with men – National HIV Behavioral Surveillance System, United States, 2011. Vaccine, 32(48), 6356–6359. 10.1016/j.vaccine.2014.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshiri, F., Siadati, S., Shokri-Shirvani, J., Haji-Ahmadi, M., Shafaei, S., & Yahyapour, Y. (2016). Detection of HPV infection in non-cancer oesophageal lesions and normal tissue by nested PCR. West Indian Medical Journal, 65(3), 496. [Google Scholar]
- Nadarzynski, T., Smith, H., Richardson, D., Jones, C. J., & Llewellyn, C. D. (2014). Human papillomavirus and vaccine-related perceptions among men who have sex with men: A systematic review. Sexually Transmitted Infections, 90(7), 515–523. 10.1136/sextrans-2013-051357 [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (2014). Vaccine uptake: Urgency for action to prevent cancer. A report to the President of the United States from the President’s Cancer Panel. National Cancer Institute. [Google Scholar]
- Oliver, S. E., Hoots, B. E., Paz-Bailey, G., Markowitz, L. E., Meites, E., & Grp, N. S., for the NHBS Study Group (2017). Increasing human papillomavirus vaccine coverage among men who have sex with men-national HIV behavioral surveillance, United States, 2014. Journal of Acquired Immune Deficiency Syndromes, 75(3), S370–S374. 10.1097/QAI.0000000000001413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong, C., Winer, J., Margolies, L., Dai, F., Patridge, E., & Chagpar, A. B. (2013). Awareness of HPV and its vaccine among lesbian, gay, bisexual, transgender, and queer (LGBTQ) populations. Journal of Clinical Oncology, 31(15_suppl), e17597. 10.1200/jco.2013.31.15_suppl.e17597 [DOI] [Google Scholar]
- Onyeabor, O. S., Martin, N., Orish, V. N., Sanyaolu, A. O., & Iriemenam, N. C. (2015). Awareness of human papillomavirus vaccine among adolescent African American males who have sex with males: A pilot study. Journal of Racial and Ethnic Health Disparities, 2(3), 290–294. 10.1007/s40615-014-0068-5 [DOI] [PubMed] [Google Scholar]
- Owusu-Edusei, K. Jr., Chesson, H. W., Gift, T. L., Tao, G., Mahajan, R., Ocfemia, M. C. B., & Kent, C. K. (2013). The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sexually Transmitted Diseases, 40(3), 197–201. 10.1097/OLQ.0b013e318285c6d2 [DOI] [PubMed] [Google Scholar]
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 1–10. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis, J. E. (2014). Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology, 21(4), 313–330. 10.1111/cpsp.12078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polek, C., & Hardie, T. (2017). Changing HPV vaccination rates in bisexual and lesbian women. Journal of the American Association of Nurse Practitioners, 29(6), 333–339. 10.1002/2327-6924.12453 [DOI] [PubMed] [Google Scholar]
- Popay, J., Rogers, A., & Williams, G. (1998). Rationale and standards for the systematic review of qualitative literature in health services research. Qualitative Health Research, 8(3), 341–351. [DOI] [PubMed] [Google Scholar]
- Power, J., McNair, R., & Carr, S. (2009). Absent sexual scripts: Lesbian and bisexual women's knowledge, attitudes and action regarding safer sex and sexual health information. Culture, Health & Sexuality, 11(1), 67–81. 10.1080/13691050802541674 [DOI] [PubMed] [Google Scholar]
- Quinn, G. P., Sanchez, J. A., Sutton, S. K., Vadaparampil, S. T., Nguyen, G. T., Green, B. L., Kanetsky, P. A., & Schabath, M. B. (2015). Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA: A Cancer Journal for Clinicians, 65(5), 384–400. 10.3322/caac.21288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi, R. I., Zha, P., Kim, S., Hindin, P., Naqvi, Z., Holly, C., Dubbs, W., & Ritch, W. (2018). Health care needs and care utilization among lesbian, gay, bisexual, and transgender populations in New Jersey. Journal of Homosexuality, 65(2), 167–180. [DOI] [PubMed] [Google Scholar]
- Reiter, P. L., Brewer, N. T., McRee, A.-L., Gilbert, P., & Smith, J. S. (2010). Acceptability of HPV vaccine among a national sample of gay and bisexual men. Sexually Transmitted Diseases, 37(3), 197–203. 10.1097/OLQ.0b013e3181bf542c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter, P. L., Bustamante, G., & McRee, A.-L. (2020). HPV vaccine coverage and acceptability among a national sample of sexual minority women ages 18–45. Vaccine, 38(32), 4956–4963. 10.1016/j.vaccine.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter, P. L., Gower, A. L., Kiss, D. E., Malone, M. A., Katz, M. L., Bauermeister, J. A., Shoben, A. B., Paskett, E. D., & McRee, A. L. (2020). A web-based human papillomavirus vaccination intervention for young gay, bisexual, and other men who have sex with men: Protocol for a randomized controlled trial. JMIR Research Protocols, 9(2), e16294. 10.2196/16294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter, P. L., McRee, A.-L., Katz, M. L., & Paskett, E. D. (2015). Human papillomavirus vaccination among young adult gay and bisexual men in the United States. American Journal of Public Health, 105(1), 96–102. 10.2105/AJPH.2014.302095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter, P. L., & McRee, A.-L. (2017). HPV infection among a population-based sample of sexual minority women from USA. Sexually Transmitted Infections, 93(1), 25–31. 10.1136/sextrans-2016-052536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro, A. A., Costa, M. C., Alves, R. R. F., Villa, L. L., Saddi, V. A., Carneiro, M. A. D. S., Zeferino, L. C., & Rabelo-Santos, S. H. (2015). HPV infection and cervical neoplasia: Associated risk factors. Infectious Agents and Cancer, 10(1), 16. 10.1186/s13027-015-0011-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson, H. L. (2016). Preventative health test utilization among sexual minorities: A nationally representative population-based study. [Google Scholar]
- Rosenbloom, S. R., & Killian, C. (2014). What are they thinking? Findings for educators and practitioners on youths’ experience and knowledge of the HPV vaccine. American Journal of Sexuality Education, 9(1), 41–64. 10.1080/15546128.2013.860352 [DOI] [Google Scholar]
- Spencer, J. C., Calo, W. A., & Brewer, N. T. (2019). Disparities and reverse disparities in HPV vaccination: A systematic review and meta-analysis. Preventive Medicine, 123, 197–203. 10.1016/j.ypmed.2019.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamargo, C. L., Quinn, G. P., Sanchez, J. A., & Schabath, M. B. (2017). Cancer and the LGBTQ population: Quantitative and qualitative results from an oncology providers’ survey on knowledge, attitudes, and practice behaviors. Journal of Clinical Medicine, 6(10), 93. 10.3390/jcm6100093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, E. A., & Goldstone, S. E. (2011). Should I or shouldn’t I: Decision making, knowledge and behavioral effects of quadrivalent HPV vaccination in men who have sex with men. Vaccine, 29(3), 570–576. 10.1016/j.vaccine.2010.09.101 [DOI] [PubMed] [Google Scholar]
- Venetis, M. K., Meyerson, B. E., Friley, L. B., Gillespie, A., Ohmit, A., & Shields, C. G. (2017). Characterizing sexual orientation disclosure to health care providers: Lesbian, gay, and bisexual perspectives. Health Communication, 32(5), 578–586. [DOI] [PubMed] [Google Scholar]
- Vorsters, A., Van Keer, S., & Van Damme, P. (2015). The use of urine in the follow-up of HPV vaccine trials. Human Vaccines & Immunotherapeutics, 11(2), 350–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheldon, C. W. (2015). HPV vaccine decision-making among male sexual minorities: An integrative theoretical framework for vaccine promotion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheldon, C. W., Daley, E. M., Buhi, E. R., Baldwin, J. A., Nyitray, A. G., & Giuliano, A. R. (2017). HPV vaccine decision-making among young men who have sex with men. Health Education Journal, 76(1), 52–65. 10.1177/0017896916647988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheldon, C. W., Daley, E. M., Buhi, E. R., Nyitray, A. G., & Giuliano, A. R. (2011). Health beliefs and attitudes associated with HPV vaccine intention among young gay and bisexual men in the southeastern United States. Vaccine, 29(45), 8060–8065. 10.1016/j.vaccine.2011.08.045 [DOI] [PubMed] [Google Scholar]
- Wigfall, L. T., Bynum, S. A., Brandt, H. M., Sebastian, N., & Ory, M. G. (2018). HPV-related cancer prevention and control programs at community-based HIV/AIDS service organizations: Implications for future engagement. Frontiers in Oncology, 8, 422. 10.3389/fonc.2018.00422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigfall, L. T., Goodson, P., Cunningham, G. B., Harvey, I. S., Gilreath, T. D., Adair, M., Gaddist, B. W., Julious, C. H., & Friedman, D. B. (2020). Understanding community-based HIV/AIDS service organizations: An invaluable source of HPV-related cancer information for at-risk populations. Journal of Health Communication, 25(1), 23–32. 10.1080/10810730.2019.1697397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung, H., Luk, K. M., Chen, S. C., Ginsberg, B. A., & Katz, K. A. (2019). Dermatologic care for lesbian, gay, bisexual, and transgender persons: Epidemiology, screening, and disease prevention. Journal of the American Academy of Dermatology, 80(3), 591–602. 10.1016/j.jaad.2018.02.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman, M. S. (2018). Assessing the reproductive health-related information-seeking behavior of low-income women: Describing a two-step information-seeking process. Journal of Health Communication, 23(1), 72–79. 10.1080/10810730.2017.1411996 [DOI] [PubMed] [Google Scholar]