Abstract
Background:
The authors report their experience of the transanal endorectal pull through technique as described by De la Torre Mondragon in the treatment of Hirschsprung’s disease (HD).
Materials and Methods:
It was a retro prospective, observational and descriptive hospital based study involving all proven cases of HD managed within a time frame of 8 years.
Results:
Fifty two patients with a mean age of 18 months at the time of surgery. The male pre dominance was remarkable. The mean duration of the surgery was 2 h and a half hours. The surgical indication was based on the history, clinical findings and on the contrast enema (transition zone) with a 24 h film (prolonged contrast evacuation) and calculation of the rectosigmoid index (<1). With a mean follow up of 16 months, the morbidity was dominated by soiling, anastomotic strictures and enterocolitis. The mortality in one case was related to a post operative enterocolitis that was not amenable to resuscitation.
Conclusion:
Soiling, anastomotic strictures and enterocolitis are the main post operative complications of TEPT in the treatment of HD in our practice.
Keywords: Cameroon, child, De la Torre-Mondragon, Hirschsprung disease, Yaoundé
INTRODUCTION
The various techniques described for the surgical correction of Hirschsprung’s disease (HD) have evolved overtime, and currently, all techniques can be performed with either open abdominal incisions, laparoscopic or robot assisted. The classic pull-through procedures initially described by an abdominoperineal approach can be performed completely from a perineal approach. In 1998, De la Torre-Mondragón and Ortega-Salgado[1] described pull-through using the transanal approach without the need for laparotomy. The most prominent advantage of this procedure is that it avoids the septic complications associated with traditional laparotomy. In addition, it seems best suited to our resource-poor setting given that it is performed as a single-stage procedure. Since 2014, totally transanal endorectal pull-through (TEPT) has been routinely performed at our paediatric surgical department.
This study aimed at evaluating the results of TEPT in the management of HD in the context of a developing country.
MATERIALS AND METHODS
Our study was observational, retrospective, descriptive and analytical over 8 years. The specified time bracket spanned between 1 January 2014 and 1 January 2022. The medical records of all children who had undergone surgical correction of HD with TEPT and were followed up at our centre were included. HD was diagnosed based on the findings of contrast enema and confirmed by histology of the resected bowel segment.
We excluded patients operated using other techniques, as well as those lost to follow-up.
This study was approved by the Institutional Ethical Committee for medical research.
The variables collected included: demographic data (sex and age at surgery); clinical data (surgical indications and approach); operative data (length of the excised specimen, duration of the surgery), timing of the first passage of stool and beginning of oral feeding; post-operative complications, mortality and duration of follow-up.
Surgical procedure
For each patient, the surgical indication was based on specific radiologic signs of HD on a contrast enema including rectosigmoid ratio <1 and prolonged contrast evacuation seen on radiographs obtained 24 h after a contrast enema in neonates [Figures 1 and 2]. Patients were admitted 72 h before surgery and pre-operative bowel preparation was initiated. Our protocol includes both mechanical (rectal irrigation using normal saline and enema) and oral bowel preparation using an antibiotic regimen consisting of erythromycin suspension 4 mg/kg/day bd and metronidazole suspension 30 mg/kg/day tid). The day before the procedure only clear fluids were authorised. For all cases, a pint of packed red blood cells was reserved pre-operatively.
Figure 1.

A frontal radiograph of contrast enema of a patient shows the transition zone at the rectum radiograph showing
Figure 2.

A radiograph showing delayed retention of contrast at 24 h
Patients were operated on in the lithotomy or prone position under general anaesthesia. A nasogastric tube and a bladder catheter were mandatory. Undercast padding was wrapped around the limbs to reduce intraoperative heat loss. This is an alternative heat preventive measure used in our setting due to non-availability of circulating air heating blankets. Skin preparation using chlorhexidine or povidone-iodine and thorough cleaning of the anal canal was done before drapping. We used Lone Star Retractor and surgical loupes to optimise visibility [Figure 3]. Xylocaine with 1:2,00,000 adrenaline (doses adapted to weight) was used for pre-surgical submucosal infiltration 1 cm above the dentate line, taking care not to infiltrate it next to the posterior urethra. The incision of the rectal mucosa began 1 cm above the dentate line and continued step-by-step circumferentially towards the serosa using 4/0 Vicryl traction sutures [Figure 4]. Mucosectomy was performed up to the peritoneal reflection with opening of the posterior muscle cuff using monopolar diathermy circumferentially which made it possible to distinguish a dilated zone, a transition zone and a narrowed zone. Mobilisation of the rectosigmoid was done without tension by ligating the mesocolon close to the serosa [Figures 5 and 6]. The extent of resection was determined by intraoperative visualisation of the transition zone by the surgeon. Dilated bowel above the transition zone was resected as much as possible until normal caliber bowel was reached [Figure 7]. Coloanal anastomosis started by placing four cardinal sutures with Vicryl 3/0 which were reinforced by interrupted Vicryl 4/0 sutures [Figure 8]. A piece of vaseline gauze was left in the anal canal to be evacuated spontaneously during the first bowel movements. The length of the resected bowel segment was measured, and a suture was placed on the proximal resection margin. The entire length of the bowel that was resected was sent for histologic analysis. Proximal resection margins were analysed for the presence of ganglionic cells. Oral feeds were authorised as soon as the bowel movements resumed. The patients were systematically reviewed at the outpatient clinic on day 10, 1 month, 3 months, 6 months and 1 year post-operatively. The anastomosis was assessed with a finger or with dilatators 10 days after the surgery. Dilatation was not routinely performed but was reserved for anastomoses that were observed to be narrow because of a stricture. The Clavien-Dindo classification was used to assess post-operative surgical complications.[2]
Figure 3.
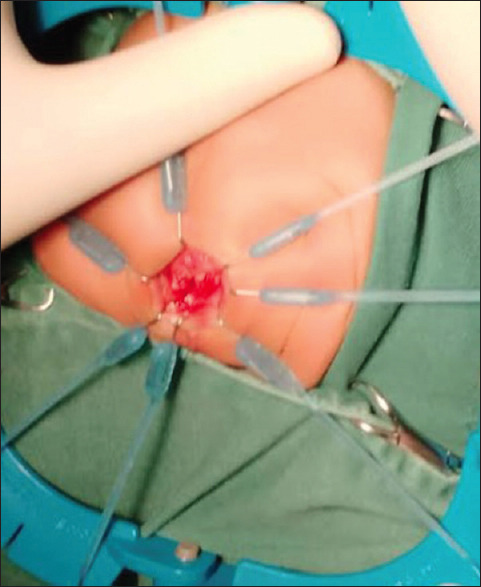
Exposition of the anal canal
Figure 4.
Placing traction sutures on the mucosa
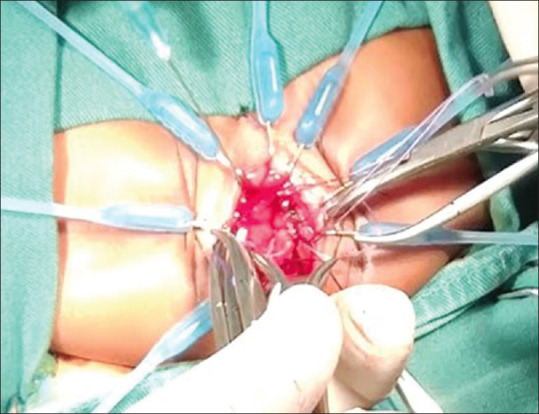
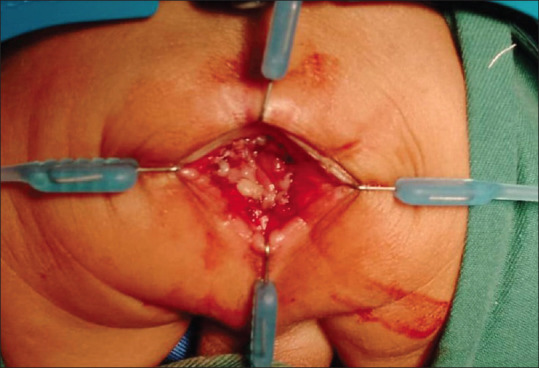
Figure 5.
Colon mobilisation
Figure 6.

Colon freed; macroscopic transition zone observed
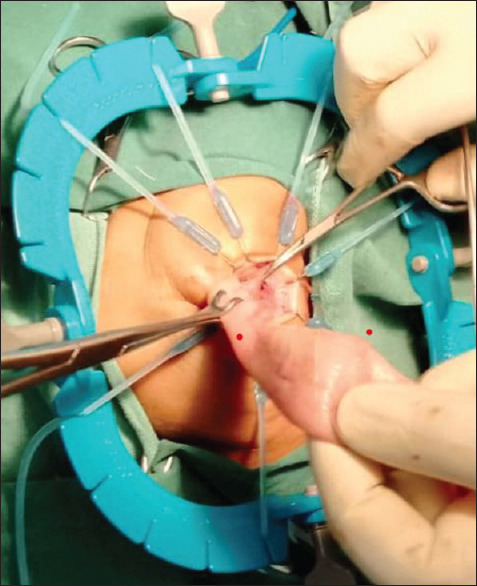
Figure 7.
Colon resection
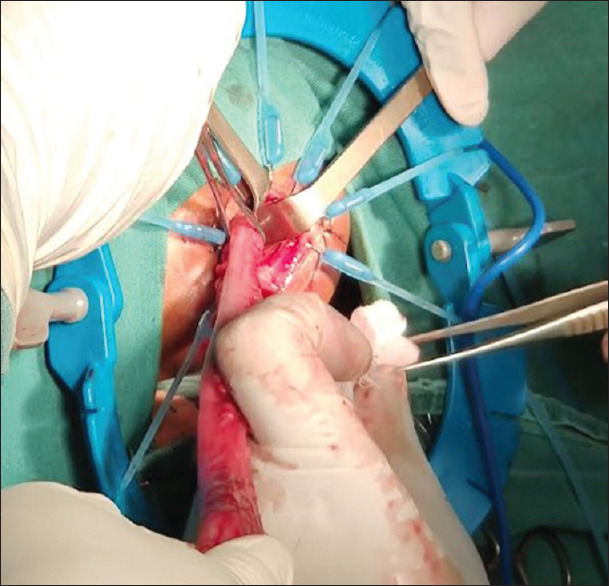
Figure 8.
Coloanal anastomosis
Statistical analysis
Qualitative categorical data were compared with Fisher’s exact test when the sum of each categorical data was <5 and the Chi-square test when this sum was >5. A P < 0.05 was considered to indicate statistical significance.
RESULTS
Fifty-two cases of HD underwent TEPT during the study period. The mean age of patients at the time of surgery was 18 months (range 14 days–12 years). The male pre-dominance was remarkable with a sex ratio of four. HD was diagnosed in all patients based on barium enema. The transition zone was present in the rectosigmoid in most cases. Contrast retention for more than 24 h was found in 40 cases. Regarding the surgical strategy, 82.5% of patients were operated without prior colostomy (n = 43). The operating time ranged from 2 h to 4 h and 15 min (mean 2 h and 30 min). The mean length of the resected bowel was 20 cm (range 15–35 cm). Bowel movements resumed at post-operative one in all cases and oral feeding started at post-operative day 2. Patients were discharged on post-operative days 7–12 (mean 9 days). Eleven patients (21.2% of the cases) in our series presented post-operative complications. Morbidity included perianal excoriation (n = 12), soiling (n = 4), anastomotic strictures (n = 3), obstructive syndrome (n = 2) and enterocolitis (n = 2). No patient required a post-operative blood transfusion. These complications were classified as Grade I (n = 4), Grade IIIa (n = 4) and Grade IIIb (n = 3). Patients presenting with anastomotic strictures required repeated dilatations with Hegar dilators under local anaesthesia with a lubricant gel. The patients who had post-operative enterocolitis presented at 3 weeks and 2 months, respectively. All were treated as inpatients, and they underwent rectal irrigations with antibiotic therapy. One of those who had a severe enterocolitis died. Two patients required revision surgery secondary to post-operative obstruction. The average follow-up period in our series was 16 months (range 2 months–4 years). Statistical analysis (Fisher’s exact test) found no correlation between age at the time of surgery and the occurrence of post-operative complications (P = 0.3451). The incidence of post-operative complications was not influenced by age at time of surgery (P = 0.3451) nor the duration of surgery (P = 0.6071).
DISCUSSION
TEPT was described by De la Torre-Mondragon’s technique is suitable in our context for the definitive treatment of HD because it is a single-stage strategy that avoids specific morbidity related to the prior colostomy but also complications related to the natural history of the disease. The fact that it is performed even in neonates without prior colostomy in our setting, is sufficient proof of experience gathered in the management of HD. The average age of 18 months at the time of surgery in our series, if close to the 22 months reported by Ellahya and Saiad in Morocco,[3] is, however, quite far from the 62 days reported by Hoff et al. in Switzerland.[4] We must recognise the traditional delay in consultation in our underdeveloped countries compared to developed countries where HD is usually diagnosed at birth. This is due to some cultural practices that prevail in our context: evacuation enema at birth is a ritual in most regions leading to a delay in the diagnosis of patients as this often misleads the delayed passage of meconium at birth. The pre-dominance of the male sex found in our series has been previously reported by other authors.[5,6] The non-availability of rectal suction material in our centre does not permit pre-operative biopsy. These diagnostic constraints as well as the absence of intraoperative frozen section are major drawbacks to the management of children with HD disadvantaged settings. Nonetheless, we perform single-stage pull-through in patients despite the lack of these facilities. The mean operating time (2 h 30 min) which is close to that of Ellahya in Morocco which was 2 h 27 min is influenced by many factors such as the use of adequate retractors and surgical loupes that improve visibility but mainly acquired surgical expertise. Post-operative obstructive syndrome classified as Clavien-Dindo Grade IIIb justified redo pull-through in three patients for suspected aganglionic segment pull-through. Post-operative anastomotic strictures may be related to the number of stitches during the anastomosis but also to the use of inappropriate suture materials. A long rectal muscular cuff dissected and left for coloanal anastomosis, could sometimes explain post-operative obstructive symptoms and enterocolitis. Hence, most surgeons currently practice modified TEPT consisting of rectal mucosa dissection with a long cuff, coloanal anastomosis with a short cuff and a V-shaped partial resection in the posterior wall of the muscular cuff a muscle split before performing the coloanal anastomosis.[7,8,9] The risk of performing a coloanal anastomosis in an aganglionic segment is only possible in the absence of peroperative frozen section biopsy. In such cases, it is recommended to move back to the traditional surgical therapy for HD consisting of a proximal defunctioning colostomy that is followed months later by a definitive reconstructive pull-through procedure and then colostomy closure, hence subsequently four stages rather than one. TEPT seems to be an obvious choice given that HD is confined to the rectosigmoid region in 75%–80% of cases of HD.[10] In older children, TEPT can be performed after the initial colostomy and the same applies to cases of complications of the disease. With a mean follow-up of 16 months, the mortality reported in one case in our series was a late death (2 months after surgery) not directly related to the surgical technique but rather due to severe post-operative enterocolitis. The child developed multiorgan failure despite intravenous antibiotic therapy and died in the intensive care unit.
CONCLUSION
Soiling, anastomotic strictures and enterocolitis are the main post-operative complications of TEPT in the treatment of HD in our practice. Mortality is not exceptional, often related to post-operative enterocolitis. Our experience has demonstrated the feasibility of performing single-stage totally transanal pull-through as described by De la Torre-Mondragon, even in the neonatal period, in our context. It had outcomes comparable with those reported in literature.
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. All methods were performed in accordance with the declaration of Helsinki and approved by the Faculty of Medicine of the University of Yaoundé I. Written informed consent was obtained from all legal guardians/parents of participants included in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.De la Torre-Mondragón L, Ortega-Salgado JA. Transanal endorectal pull-through for Hirschsprung's disease. J Pediatr Surg. 1998;33:1283–6. doi: 10.1016/s0022-3468(98)90169-5. [DOI] [PubMed] [Google Scholar]
- 2.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The clavien-dindo classification of surgical complications: Five-year experience. Ann Surg. 2009;250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 3.Ellahya H. [Unpublished MD thesis] Cadi Ayyad University, Marrakech; 2011. Hirschsprung's disease in children. A study on 43 cases (N°43) [Google Scholar]
- 4.Hoff N, Wester T, Granström AL. Classification of short-term complications after transanal endorectal pullthrough for Hirschsprung's disease using the Clavien-Dindo-grading system. Pediatr Surg Int. 2019;35:1239–43. doi: 10.1007/s00383-019-04546-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bastard F, Podevin G. Hirschsprung disease, diagnosis and management. Colon Rectum. 2015;9:149–54. [Google Scholar]
- 6.Moulot MO, Yebouet E, Agbara S, Ehua M, Azakpa L, Kouame A, et al. Résultats de la prise en charge chirurgicale de la maladie de Hirschsprung dans le service de chirurgie pédiatrique du CHU de Treichville. J Afri Hépato Gastroentérologie. 2015;9:109–13. [Google Scholar]
- 7.Wester T, Rintala RJ. Early outcome of transanal endorectal pull-through with a short muscle cuff during the neonatal period. J Pediatr Surg. 2004;39:157–60. doi: 10.1016/j.jpedsurg.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Hadidi A, Bartoli F, Waag KL. Role of transanal endorectal pull-through in complicated Hirschsprung's disease: Experience in 18 patients. J Pediatr Surg. 2007;42:544–8. doi: 10.1016/j.jpedsurg.2006.10.047. [DOI] [PubMed] [Google Scholar]
- 9.Yang L, Tang ST, Cao GQ, Yang Y, Li S, Li SW, et al. Transanal endorectal pull-through for Hirschsprung's disease using long cuff dissection and short V-shaped partially resected cuff anastomosis: Early and late outcomes. Pediatr Surg Int. 2012;28:515–21. doi: 10.1007/s00383-012-3071-0. [DOI] [PubMed] [Google Scholar]
- 10.Butler Tjaden NE, Trainor PA. The developmental etiology and pathogenesis of Hirschsprung disease. Transl Res. 2013;162:1–15. doi: 10.1016/j.trsl.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


