Abstract
Background
Young adult cancer survivors face medical financial hardships that may lead to delaying or forgoing medical care. This study describes the medical financial difficulties young adult cancer survivors in the United States experience in the post–Patient Protection and Affordable Care Act period.
Method
We identified 1009 cancer survivors aged 18 to 39 years from the National Health Interview Survey (2015-2022) and matched 963 (95%) cancer survivors to 2733 control individuals using nearest-neighbor matching. We used conditional logistic regression to examine the association between cancer history and medical financial hardship and to assess whether this association varied by age, sex, race and ethnicity, and region of residence.
Results
Compared with those who did not have a history of cancer, young adult cancer survivors were more likely to report material financial hardship (22.8% vs 15.2%; odds ratio = 1.65, 95% confidence interval = 1.50 to 1.81) and behavior-related financial hardship (34.3% vs 24.4%; odds ratio = 1.62, 95% confidence interval = 1.49 to 1.76) but not psychological financial hardship (52.6% vs 50.9%; odds ratio = 1.07, 95% confidence interval = 0.99 to 1.16). Young adult cancer survivors who were Hispanic or lived in the Midwest and South were more likely to report psychological financial hardship than their counterparts.
Conclusions
We found that young adult cancer survivors were more likely to experience material and behavior-related financial hardship than young adults without a history of cancer. We also identified specific subgroups of young adult cancer survivors that may benefit from targeted policies and interventions to alleviate medical financial hardship.
Many people in the United States face financial difficulties and stress resulting from the high costs of medical care (1,2). Medical financial hardship, or “financial toxicity,” is an ongoing concern; approximately 137.1 million adults have reported some medical financial hardship in the past year (1). The prevalence of medical financial hardship varies across sociodemographic groups and populations (3); people with lower educational attainment or multiple health conditions or who live in rural areas are more likely to experience medical financial hardship (1,4-6). Among patients with cancer, the adverse consequences of medical financial hardship are more drastic, with approximately 50% of these patients facing personal financial burden associated with the disease and its treatment (7,8). Compared with individuals with no history of cancer, cancer survivors are more likely to face substantial out-of-pocket health-care expenditures and experience difficulties paying medical bills, endure financial distress, and delay or forgo medical care (3,5,9-12).
Many life-saving treatments and medications prescribed for patients with cancer are costly. For example, treatment for breast cancer, the most prevalent type of cancer among women in the United States, costs an average of $198 400 over 5 years for patients younger than 65 years of age and an average of $116 800 for patients 65 years of age and older (13). Cancer survivors incur additional expenses as a result of follow-up treatments or checkups. The accumulation of these cancer-related health-care expenditures imposes an enormous financial burden on both cancer survivors and their families, which often results in the depletion of family assets, increased stress on household finances, reduced adherence to needed medical care, and increased mortality (3,14,15).
Cancer survivors, regardless of age, are at higher risk of experiencing financial hardship for multiple reasons, such as impaired work ability (16,17), productivity losses (18,19), and decreased income (20,21) resulting from cancer treatment and its long-term effects. The impact of financial hardship, however, could be particularly challenging for cancer survivors during their young adulthood (18-39 years of age) (10,22) because this is the time when these young cancer survivors experience the transition from adolescence into adulthood and from being cancer patients into cancer survivors. Cancer diagnosis from childhood or during young adulthood could lead to disruptions in education and in work and family planning (23,24); these disruptions could further result in decreased earnings, financial struggles, change in health-care–seeking behaviors, and reductions in needed medical care (12). Also, young adults lack a long employment history and, as a result, are likely to have limited financial assets.
Nonetheless, existing literature has largely focused on either all-age adult cancer survivors together or separated by the age cutoff of 65 years (4,5,9,25-27) or adult survivors of adolescent and young adult cancer (a cancer diagnosis at 15-39 years of age) (10,28,29). The disruptive financial influence of a cancer diagnosis, treatment, and continued care on young adults (ie, those aged 18-39 years)—who are more vulnerable to medical financial hardship than other age groups—has yet to be examined. Using nationally representative data from the National Health Interview Survey (NHIS), we studied material, psychological, and behavioral financial hardships among young adult cancer survivors.
Methods
Data sources and study population
We used publicly available data from NHIS 2015-2020. The NHIS is an ongoing nationally representative cross-sectional survey that samples approximately 87 500 individuals from 35 000 households annually. Using a multistage probability design, the NHIS sample is designed to be representative of the civilian, noninstitutionalized population living in the 50 states and the District of Columbia (30). The survey provides information about the socioeconomic status, demographics, health conditions, and health-care access and utilization of the respondents.
A total of 73 059 adults 18 to 39 years of age participated in the survey from 2015 to 2022. We excluded 27 participants who did not answer the question, “Have you EVER been told by a doctor or other health professional that you had …[c]ancer or a malignancy of any kind?” or responded “Don’t know” or “Refused” to the question. We then excluded 163 participants who had nonmelanoma or unknown skin cancer only. We further excluded 1266 participants who had missing values on the financial hardship outcome variables and 2891 participants who had missing values on key covariates and survey design elements (eg, survey strata, clusters, weights). Our final study sample consisted of 68 712 participants, out of which 1009 were cancer survivors, defined as individuals who had been diagnosed with cancer (Supplementary Figure 1, available online).
Outcome variables
Medical financial hardship was categorized into 3 domains: material conditions, psychological responses, and coping behaviors. This framework provides a multidimensional measure of medical financial hardship by capturing material conditions resulting from increased health-care expenses and reduced income (eg, difficulties in paying medical bills), psychological responses to treatment and care cost (eg, financial worry and distress), and consequent health-care–seeking behaviors (eg, delaying or forgoing care because of cost) (1,31,32). This approach has been adopted in previous studies, particularly in survey studies, with the benefit of summarizing information from multiple measures within the same domain of hardship (26,33). Material financial hardship was measured by the survey question, “In the past 12 months did you or anyone (in household) have problems paying or were unable to pay any medical bills?” It was categorized as a binary variable (Yes or No), with those who answered “Yes” considered to have material financial hardship. Psychological financial hardship was measured by the question, “If you get sick or have an accident, how worried are you that you will be able to pay your medical bills?” Those who answered “very worried” or “somewhat worried” were considered to have psychological financial hardship. Behavior-related financial hardship was measured by 5 binary variable (Yes or No) questions asking the respondents if they, in the past 12 months 1) had ever delayed medical care due to worry about cost, 2) had ever forgone medical care due to worry about cost, 3) were unable to afford prescription medicines when they needed them, 4) were unable to afford counseling or therapy when they needed it, and 5) were unable to afford dental care when they needed it (except for the year 2021). Those who answered “Yes” to any of the 5 questions were considered to have behavior-related financial hardship.
Exposure variable
The exposure variable was having a history of cancer. We defined those who answered “Yes” to the survey question, “Have you EVER been told by a doctor or other health professional that you had …[c]ancer or a malignancy of any kind?” as cancer survivors and those who answered “No” as controls without a history of cancer.
Covariates
We selected the following variables as potential confounders, based on the domain knowledge and existing literature (5,10,26,27). Individual-level demographic and clinical characteristics included age category at the time of the survey; self-reported sex; race and ethnicity; educational attainment; marital status; employment status; family income level as a percentage of the federal poverty level (FPL); health insurance coverage; residential region; and disease burden, calculated as the total number of 6 common chronic disease conditions. These conditions were based on a “Yes” response to the questions asking if they were ever told by a doctor that they had asthma, arthritis, cardiovascular disease (coronary heart disease, stroke, myocardial infarction, or angina pectoris), diabetes, respiratory disease (chronic obstructive pulmonary disease, emphysema, or chronic bronchitis), and hypertension.
Statistical analysis
To account for confounding and reduce bias, we used nearest-neighbor matching without replacement to match between 1 and 3 controls without a history of cancer to each cancer survivor, based on the following variables: age category, sex, race and ethnicity, education, marital status, employment status, family income level as a percentage of FPL, health insurance coverage, residential region, and disease burden. The matching approach is often preferred over commonly applied regression analyses because it provides more robust estimates by allowing one to assess the systematic difference in observed characteristics between groups (34,35). We performed descriptive analyses to compare the distribution of baseline characteristics between cancer survivors and controls before and after matching. We reported standardized mean differences in baseline characteristics between cancer survivors and controls; differences of 10% or less were considered meaningfully balanced.
Considering the correlation of individuals in the matched sets, we then used conditional logistic regressions to estimate the association between having a history of cancer and financial hardship. The matched individuals retained their natural sampling weights for better balance and lower bias (36). In addition, to investigate whether this association varied according to sociodemographic factors, we conducted similar regression analyses for stratified groups by age, sex, race and ethnicity, and residential region. All the analyses, unless specified, accounted for survey design elements, including survey strata, clusters, and sampling weights to generate population-level estimates. We used SAS, version 9.4, statistical analysis software (SAS Institute LP, Cary, NC) to perform all analyses and R, version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria) and Excel, version 2016 (Microsoft Corp, Redmond, WA) to create the figures. All tests were 2-sided, with P less than .05 considered statistically significant.
Results
Population characteristics
Of 1009 young adult cancer survivors, 963 (95%) were matched to 2733 controls. Table 1 provides the distributions of baseline characteristics between cancer survivors and controls before and after matching. Before matching, the 2 groups of participants differed systematically. After matching, the characteristics of cancer survivors and their controls were similar, with standardized differences less than 10% for all variables.
Table 1.
Baseline characteristics of young adults with and without a history of cancer, before and after matching
| Variable | Before matching |
After matching |
||||
|---|---|---|---|---|---|---|
| Cancer survivors (n = 1009) | Controls (n = 67 703) | Standardized mean difference | Cancer survivors (n = 963) | Controls (n = 2733) | Standardized mean difference | |
| Age, No. (weighted %), y | ||||||
| 18-25 | 111 (13.1) | 19 363 (35.8) | 0.45 | 102 (12.7) | 286 (13.9) | <0.01 |
| 26-39 | 898 (86.9) | 48 340 (64.2) | 0.45 | 861 (87.3) | 2447 (86.1) | <0.01 |
| Female sex, No. (weighted %) | 719 (66.5) | 35 813 (50.1) | 0.39 | 689 (66.5) | 1949 (68.6) | 0.01 |
| Race and ethnicity, No. (weighted %) | ||||||
| Non-Hispanic White | 742 (70.6) | 39 841 (56.3) | 0.31 | 718 (71.6) | 2062 (74.5) | 0.02 |
| Non-Hispanic Black | 74 (7.9) | 8048 (13.2) | 0.15 | 68 (7.4) | 188 (7.5) | 0.01 |
| Hispanic | 140 (16.8) | 13 133 (21.4) | 0.15 | 130 (16.4) | 359 (13.8) | 0.01 |
| Othera | 53 (4.7) | 6681 (9.1) | 0.18 | 47 (4.5) | 124 (4.1) | 0.02 |
| Education, No. (weighted %) | ||||||
| Less than high school | 127 (14.7) | 7171 (12.2) | 0.06 | 114 (13.7) | 300 (11.8) | 0.03 |
| High school graduate | 157 (17.3) | 13 601 (23.2) | 0.12 | 144 (16.7) | 399 (15.8) | 0.01 |
| College or higher | 725 (68.0) | 46 931 (64.6) | 0.06 | 705 (69.6) | 2034 (72.4) | 0.03 |
| Marital status, No. (weighted %) | ||||||
| Married/living with a partner | 556 (62.0) | 32 696 (49.8) | 0.14 | 525 (61.8) | 1499 (61.0) | 0.01 |
| Never married/others | 453 (38.0) | 35007 (50.2) | 0.14 | 438 (38.2) | 1234 (39.0) | 0.01 |
| Employment, No. (weighted %) | ||||||
| Full time | 539 (51.0) | 41 221 (57.5) | 0.15 | 522 (51.5) | 1618 (58.3) | 0.1 |
| Part-time | 184 (17.7) | 11 625 (18.4) | 0.03 | 175 (17.6) | 440 (17.0) | 0.06 |
| Unemployed | 286 (31.3) | 14 857 (24.1) | 0.15 | 266 (30.9) | 675 (24.7) | 0.07 |
| Family income level as a percentage of the federal poverty level, No. (weighted %) | ||||||
| <200% | 417 (41.0) | 23 563 (33.0) | 0.13 | 390 (39.9) | 1073 (35.9) | 0.03 |
| 200%-399% | 266 (25.7) | 20 179 (30.6) | 0.08 | 256 (26.0) | 733 (29.0) | 0.01 |
| ≥400% | 326 (33.3) | 23 961 (36.4) | 0.07 | 317 (34.0) | 927 (35.1) | 0.02 |
| Health insurance, No. (weighted %) | ||||||
| Private and other | 630 (62.5) | 48 089 (69.1) | 0.18 | 611 (63.4) | 1794 (65.1) | 0.05 |
| Medicaid and other public insurance | 248 (23.4) | 10 000 (15.7) | 0.25 | 231 (23.3) | 634 (23.2) | 0.02 |
| Uninsured | 131 (14.1) | 9614 (15.2) | 0.04 | 121 (13.3) | 305 (11.6) | 0.04 |
| Region of residence, No. (weighted %) | ||||||
| Northeast | 137 (13.4) | 10 170 (16.3) | 0.04 | 132 (13.2) | 379 (16.0) | <0.01 |
| Midwest | 260 (25.8) | 15 314 (21.8) | 0.07 | 246 (25.1) | 697 (25.7) | <0.01 |
| South | 331 (35.4) | 23 926 (36.9) | 0.05 | 319 (35.9) | 902 (34.1) | <0.01 |
| West | 281 (25.4) | 18 293 (25.0) | 0.02 | 266 (25.8) | 755 (24.2) | <0.01 |
| Disease burden,b No. (weighted %) | ||||||
| None | 526 (51.0) | 48 164 (71.8) | 0.4 | 526 (53.8) | 1561 (57.4) | 0.05 |
| 1 | 274 (28.0) | 15 584 (22.7) | 0.1 | 268 (29.0) | 775 (29.5) | 0.01 |
| 2 | 136 (14.0) | 3130 (4.3) | 0.31 | 119 (12.3) | 300 (10.1) | 0.04 |
| ≥3 | 73 (7.0) | 825 (1.1) | 0.3 | 50 (4.8) | 97 (3.0) | 0.08 |
| Time since diagnosis, weighted mean (SD), y | 10.0 (0.5) | 10.2 (0.3) | ||||
“Other” includes Asian, American Indian and Alaska Native, and other race or ethnicity.
Disease burden was defined as the number of the following 6 common chronic conditions, based on whether they were ever told by a physician that they had asthma, arthritis, cardiovascular disease (coronary heart disease, stroke, myocardial infarction, or angina pectoris), diabetes, respiratory disease (chronic obstructive pulmonary disease, emphysema, or chronic bronchitis), and hypertension.
Association of a history of cancer with financial hardship
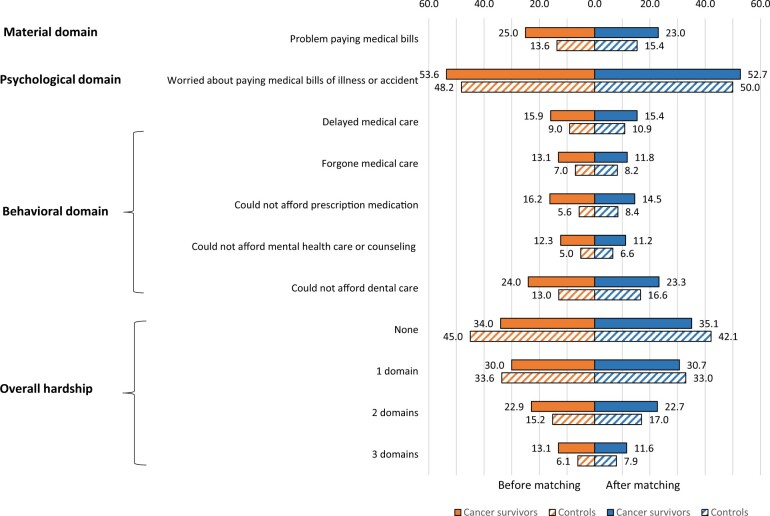
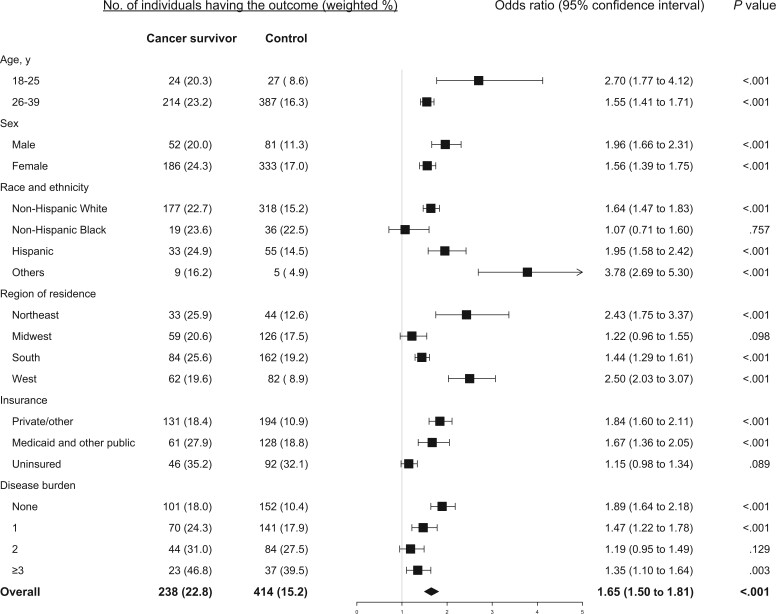
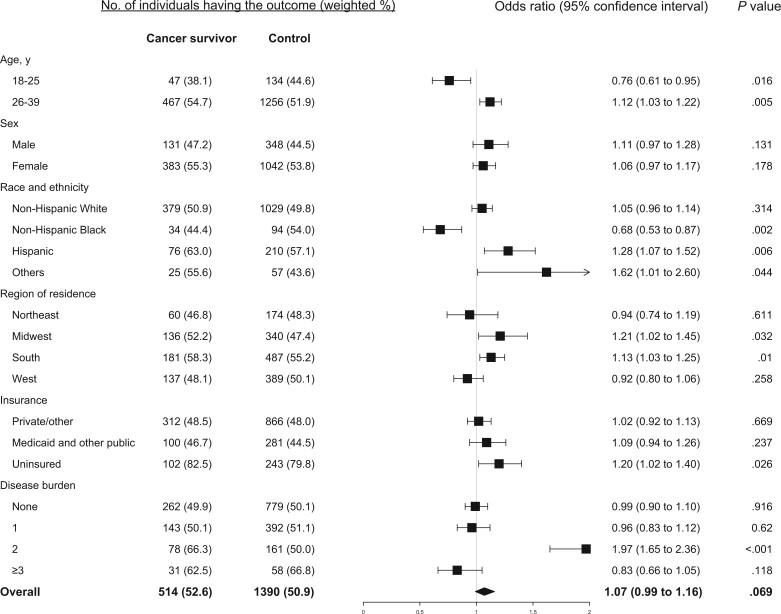
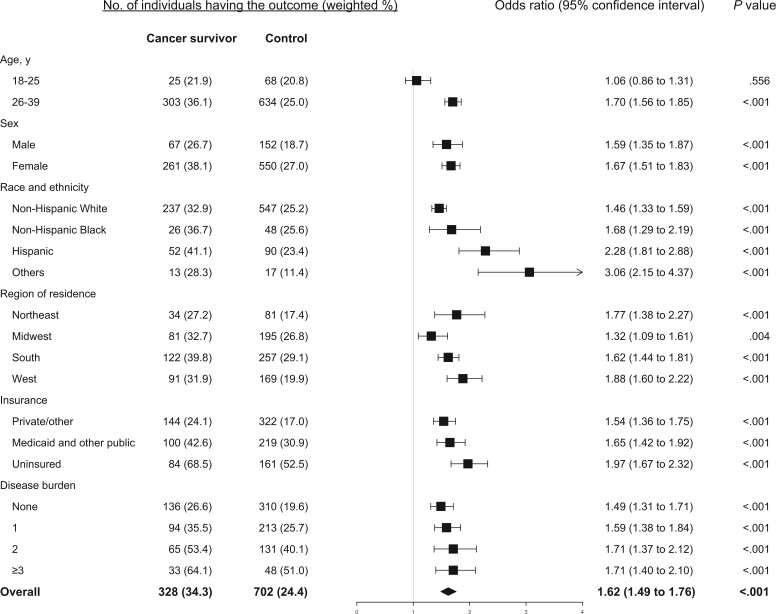
Among cancer survivors, 22.8%, 52.6%, and 34.3% reported having material, psychological and behavior-related financial hardship, respectively, compared with 15.2%, 50.9%, and 24.4% among the matched controls. Also compared with their counterparts, cancer survivors were more likely to report having financial hardship in 2 domains (21.8% vs 16.2%, P = .002) and in all 3 domains (11.7% vs 7.9%, P = .002). The detailed response to each measure in the 3 domains for cancer survivors and their controls is provided in Figure 1. Compared with those with no history of cancer, cancer survivors had significantly higher odds of material financial hardship (odds ratio [OR] = 1.65, 95% confidence interval [CI] = 1.50 to 1.81) and behavior-related financial hardship (OR = 1.62, 95% CI = 1.49 to 1.76) but not psychological financial hardship (OR = 1.07, 95% CI = 0.99 to 1.16) (Figures 2-4).
Figure 1.
Proportion of young adult cancer survivors and control individuals reporting material, psychological, and behavioral financial hardship before and after matching.
Figure 2.
Estimated association between history or cancer and material financial hardship overall and stratified by age, sex, race and ethnicity, residential region, health insurance coverage, and disease burden.
Association of a history of cancer with financial hardship, stratified by age, sex, race and ethnicity, residential region, health insurance status, disease burden, and cancer type
Compared with those who did not have a history of cancer, cancer survivors 26 to 39 years of age consistently had significantly increased odds of reporting material (Figure 2), psychological (Figure 3), and behavioral (Figure 4) financial hardship, while cancer survivors 18 to 25 years of age had significantly lower odds (OR = 0.70, 95% CI = 0.61 to 0.82) of reporting psychological financial hardship. Both male and female cancer survivors had significantly increased odds of reporting material (Figure 2) and behavioral financial hardship (Figure 4), but not psychological financial hardship (Figure 3).
Figure 3.
Estimated association between history of cancer and psychological financial hardship overall and by age, sex, race and ethnicity, residential region, health insurance coverage, and disease burden.
Figure 4.
Estimated association between history of cancer and behavioral financial hardship, stratified by age, sex, race and ethnicity, residential region, health insurance coverage, and disease burden.
Cancer survivors of all racial and ethnic groups had significantly increased odds of reporting behavioral (Figure 4) and material financial hardship (Figure 2, except the Black group). For psychological financial hardship, increased odds were significant only in Hispanic (OR = 1.28, 95% CI = 1.07 to 1.52) and other racial or ethnic (OR = 1.62, 95% CI = 1.01 to 2.60) young adult cancer survivors (Figure 3).
Young adult cancer survivors from the Northeast or West region had significantly higher odds of reporting material (Figure 2) and behavioral financial hardship (Figure 4) but not psychological financial hardship (Figure 3). In contrast, cancer survivors residing in the Midwest or South region were more likely to report psychological financial hardship, with an estimated OR = 1.21 (95% CI = 1.02 to 1.45) and OR = 1.13 (95% CI = 1.03 to 1.25), respectively (Figure 3). They also had increased odds of reporting behavioral financial hardship (Figure 4).
Compared with their counterparts, young adult cancer survivors, regardless of their insurance coverage and disease burden, had significantly higher odds of reporting behavioral financial hardship, particularly for those uninsured and those who had multiple chronic diseases (Figure 4).
Discussion
Using nationally representative NHIS data from 2015 to 2022, we conducted a matching analysis to examine the association between cancer history and medical financial hardship, measured in the material, psychological, and behavioral domains, by comparing young adult cancer survivors with their matched counterparts with no history of cancer. We found that having a cancer history was significantly associated with financial hardship in the material and behavioral domains. Compared with their matched controls, young adult cancer survivors had higher odds of reporting financial hardship in the material and behavioral domains. They were also more likely to report financial hardship in multiple domains. The magnitude and direction of our findings are in line with a recent study using the 2014 to 2016 NHIS data for cancer survivors of all ages as well as for the age group of 18- to 49-year-olds (5). These findings suggest an opportunity for the health-care team to initiate cost-related discussions proactively and assist patients with financial challenges associated with their cancer treatment and care.
We did not find a significant association between a history of cancer and psychological financial hardship. This null finding is congruent with a recent study by Lu et al. (10) that focused on adult survivors with a cancer diagnosis when they were adolescents or young adults, in contrast to an earlier study by Zheng et al. (5). The lack of statistically significant associations does not preclude the existence of such an association. There are notable differences between the study by Zheng et al. and ours. In the work by Zheng and colleagues, psychological financial hardship was measured by both worries about medical bills for normal care and care for accidents or being sick, while only a question on worries about medical bills for accidents or being sick was available in the NHIS in later years. In addition to the differences in how psychological financial hardship was defined, other possible explanations of different findings include the study time window (eg, 2013-2016 vs 2015-2022) and analytic sample (eg, adults of all ages vs young adults 18-39 years of age). Moreover, depending on whether the survey design was accounted for in the analysis, the findings may be inferred to the target population or limited to the analytic sample. In our study, we incorporated the survey design elements in the regression analysis for the matched sample of young adult cancer survivors, which allowed us to draw inferences at the national population level. Nevertheless, to further evaluate the relative impact of a history of cancer on different domains of financial hardship, particularly on the psychological domain, additional evidence, with comprehensive measures of cancer survivors’ perception of worry and detailed information about their personal finances, family support, insurance status, and cancer-related treatments, duration, and costs, is needed.
We also found that the impact of a history of cancer on young adult cancer survivors’ financial hardship varied by several sociodemographic and health factors. For example, compared with their counterparts, cancer survivors with no insurance coverage or who have multiple chronic diseases were more than likely to experience behavioral financial hardship. Also, Hispanic and other racial and ethnic young adult cancer survivors were more likely to report psychological financial hardship than non-Hispanic White young adult cancer survivors in addition of the other 2 domains. This finding may be explained by differences in their health insurance status, where the proportion of those who were uninsured was 18.8% in the Hispanic group and 14.4% in the other racial and ethnic group compared with 10.5% among those in the non-Hispanic White group in our study. Our results suggest that targeted interventions to improve health insurance coverage and access to health care among Hispanic and those in the other racial and ethnic young adult cancer survivors may reduce their financial burden resulting from medical bills and related stress and concerns.
Our results also show that cancer survivors in the South and Midwest were more likely to report psychological financial hardship. Material financial hardship has been demonstrated to be associated with a lack of health insurance coverage (26,37), which may further perpetuate psychological financial hardship and increase the worry about medical bills. It is noteworthy that the uninsured rates in our study sample were 3.5% and 8.1% for the Northeast and West, respectively, while the rates were 14.9% and 16.6% for the Midwest and South, respectively. The Patient Protection and Affordable Care Act (ACA), enacted in 2010, attempted to reduce the size of the uninsured population through a continuum of affordable coverage provisions (38). One of the ACA’s provisions was to allow young adults to remain in their parent’s private health insurance plans as dependents until they reach age 26 years. Medicaid expansion under the ACA has been shown to be associated with improved health insurance coverage and overall survival among young adults with cancer (39,40). It may also mitigate the financial hardship younger cancer survivors fact. The adoption of Medicaid expansion to cover poor and near-poor individuals with incomes up to 138% of the federal poverty level, however, is a state-level decision. Among the 11 states that have not expanded Medicaid for these populations, 10 were in the South and Midwest (41). Understanding the impact of these ACA provisions on medical financial hardship among young adult cancer survivors, particularly by state and region of residence, would be an important topic for future research.
Our study has some limitations. First, answers to questions in the NHIS were self-reported, which is subject to recall bias (42). Second, due to the cross-sectional nature of NHIS design, we were unable to identify the exact time order of the experience of financial hardship and cancer diagnosis, particularly when they were reported in the same year, and were thus unable to establish a causal relationship between cancer history and financial hardship. Third, considering the consistency of survey questions over the study years, psychological financial hardship was measured only by the respondents’ worry about medical bills if they should get sick or have an accident but not about normal care. Finally, we did not examine the impact of financial hardship by cancer types due to concerns about sample size; also, the NHIS lacks detailed information about cancer diagnoses, such as disease stage, duration of illness, and treatment history, and health condition. We considered comorbidities in the matching process, however, which may ameliorate some of the concerns about the lack of detailed cancer information.
Compared with their counterparts with no history of cancer, young adult cancer survivors 18 to 39 years of age had an elevated risk of experiencing medical financial hardship, particularly material and behavioral financial hardships. The patterns of material, psychological, and behavioral medical financial hardship vary by age, sex, race and ethnicity, and residential region. Our study highlights the importance of studying this age group of cancer survivors specifically. Findings also suggest that interventions that reduce medical financial hardship in young adult cancer survivors should focus on improving health insurance coverage and specific risk groups.
Supplementary Material
Acknowledgements
The authors thank Seth D. Goldfarb for proofreading and editing the manuscript. The authors also thank Dr Chen Yang for validating the statistical analyses. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Lihua Li, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; Institute for Health Care Delivery Science, Icahn School of Medicine at Mount Sinai, New York, NY, USA; The Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA; Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Donglan Zhang, Division of Health Services Research, Department of Foundations of Medicine, NYU Long Island School of Medicine, Mineola, NY, USA.
Yan Li, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, China.
Mayuri Jain, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; Institute for Health Care Delivery Science, Icahn School of Medicine at Mount Sinai, New York, NY, USA; The Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Xingyu Lin, Department of Statistical and Actuarial Sciences, University of Western Ontario, London, ON, Canada.
Rebecca Hu, Department of Molecular and Cellular Biology, University of California, Berkeley, Berkeley, CA, USA.
Junxiu Liu, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Janani Thapa, Department of Health Policy and Management, College of Public Health, University of Georgia, Athens, GA, USA.
Lan Mu, Department of Geography, University of Georgia, Athens, GA, USA.
Zhuo Chen, Department of Health Policy and Management, College of Public Health, University of Georgia, Athens, GA, USA.
Bian Liu, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; Institute for Translational Epidemiology, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
José A Pagán, Department of Public Health Policy and Management, School of Global Public Health, New York University, New York, NY, USA.
Data availability
The NHIS data are publicly available and can be found at the website of the Centers for Disease Control and Prevention (https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm).
Author contributions
Lihua Li, PhD (Conceptualization; Methodology; Project administration; Writing—original draft; Writing—review & editing), Donglan Zhang, PhD (Conceptualization; Funding acquisition; Investigation; Methodology; Writing—review & editing), Yan Li, PhD (Conceptualization; Funding acquisition; Methodology; Writing—review & editing), Mayuri Jain, MPH (Data curation; Formal analysis; Visualization), Xingyu Lin, BSc (Data curation; Validation), Rebecca Hu, PhD (Project administration; Writing—review & editing), Junxiu Liu, PhD (Writing—review & editing), Janani R. Thapa, PhD (Writing—review & editing), Lan Mu, PhD (Visualization; Writing—review & editing), Zhuo Chen, PhD (Writing—review & editing), Bian Liu, PhD (Conceptualization; Writing—review & editing), José A. Pagán, PhD (Conceptualization; Resources; Writing—review & editing).
Funding
This work was supported by a grant from the National Institute on Minority Health and Health Disparities at the National Institutes of Health (1R01MD013886) and a grant from the National Heart, Lung, and Blood Institute at the National Institutes of Health (R01HL141427).
Conflicts of interest
None reported.
References
- 1. Yabroff KR, Zhao J, Han X, Zheng Z.. Prevalence and correlates of medical financial hardship in the USA. J Gen Intern Med. 2019;34(8):1494-1502. doi: 10.1007/s11606-019-05002-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cohen RA, Kirzinger WK.. Financial burden of medical care: a family perspective. NCHS Data Brief. 2014;(142):1-8. [PubMed] [Google Scholar]
- 3. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR.. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109(2):djw205. doi: 10.1093/jnci/djw205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Odahowski CL, Zahnd WE, Zgodic A, et al. Financial hardship among rural cancer survivors: an analysis of the Medical Expenditure Panel Survey. Prev Med. 2019;129S:105881. doi: 10.1016/j.ypmed.2019.105881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zheng Z, Jemal A, Han X, et al. Medical financial hardship among cancer survivors in the United States. Cancer. 2019;125(10):1737-1747. doi: 10.1002/cncr.31913 [DOI] [PubMed] [Google Scholar]
- 6. Su M, Lao J, Zhang N, et al. Financial hardship in Chinese cancer survivors. Cancer. 2020;126(14):3312-3321. doi: 10.1002/cncr.32943 [DOI] [PubMed] [Google Scholar]
- 7. Khera N, Zhang N, Hilal T, et al. Association of health insurance literacy with financial hardship in patients with cancer. JAMA Netw Open. 2022;5(7):e2223141. doi: 10.1001/jamanetworkopen.2022.23141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith GL, Banegas MP, Acquati C, et al. Navigating financial toxicity in patients with cancer: a multidisciplinary management approach. CA Cancer J Clin. 2022;72(5):437-453. doi: 10.3322/caac.21730 [DOI] [PubMed] [Google Scholar]
- 9. Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR.. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(2):308-317. doi: 10.1158/1055-9965.EPI-19-0460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lu AD, Zheng Z, Han X, et al. Medical financial hardship in survivors of adolescent and young adult cancer in the United States. J Natl Cancer Inst. 2021;113(8):997-1004. doi: 10.1093/jnci/djab013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gordon LG, Merollini KMD, Lowe A, Chan RJ.. A systematic review of financial toxicity among cancer survivors: we can't pay the co-pay. Patient. 2017;10(3):295-309. doi: 10.1007/s40271-016-0204-x [DOI] [PubMed] [Google Scholar]
- 12. Kent EE, Forsythe LP, Yabroff KR, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710-3717. doi: 10.1002/cncr.28262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Banegas MP, Yabroff KR, O'Keeffe-Rosetti MC, et al. Medical care costs associated with cancer in integrated delivery systems. J Natl Compr Canc Netw. 2018;16(4):402-410. doi: 10.6004/jnccn.2017.7065 [DOI] [PubMed] [Google Scholar]
- 14. Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34(9):980-986. doi: 10.1200/JClinOncol.2015.64.6620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yabroff KR, Han X, Song W, et al. Association of medical financial hardship and mortality among cancer survivors in the United States. J Natl Cancer Inst. 2022;114(6):863-870. doi: 10.1093/jnci/djac044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kirchhoff AC, Krull KR, Ness KK, et al. Occupational outcomes of adult childhood cancer survivors: a report from the childhood cancer survivor study. Cancer. 2011;117(13):3033-3044. doi: 10.1002/cncr.25867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mols F, Tomalin B, Pearce A, Kaambwa B, Koczwara B.. Financial toxicity and employment status in cancer survivors. a systematic literature review. Support Care Cancer. 2020;28(12):5693-5708. doi: 10.1007/s00520-020-05719-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guy GP Jr, Berkowitz Z, Ekwueme DU, Rim SH, Yabroff KR.. Annual economic burden of productivity losses among adult survivors of childhood cancers. Pediatrics. 2016;138(suppl 1):S15-S21. doi: 10.1542/peds.2015-4268D [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stone DS, Ganz PA, Pavlish C, Robbins WA.. Young adult cancer survivors and work: a systematic review. J Cancer Surviv. 2017;11(6):765-781. doi: 10.1007/s11764-017-0614-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wengenroth L, Sommer G, Schindler M, et al. ; Swiss Paediatric Oncology Group (SPOG). Income in adult survivors of childhood cancer. PLoS One. 2016;11(5):e0155546. doi: 10.1371/journal.pone.0155546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zajacova A, Dowd JB, Schoeni RF, Wallace RB.. Employment and income losses among cancer survivors: Estimates from a national longitudinal survey of American families. Cancer. 2015;121(24):4425-4432. doi: 10.1002/cncr.29510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bleyer A, Barr R.. Cancer in young adults 20 to 39 years of age: overview. Semin Oncol. 2009;36(3):194-206. doi: 10.1053/j.seminoncol.2009.03.003 [DOI] [PubMed] [Google Scholar]
- 23. Mitby PA, Robison LL, Whitton JA, et al. ; Childhood Cancer Survivor Study Steering Committee. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. 2003;97(4):1115-1126. doi: 10.1002/cncr.11117 [DOI] [PubMed] [Google Scholar]
- 24. Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30(19):2393-2400. doi: 10.1200/JClinOncol.2011.39.6333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ekwueme DU, Zhao J, Rim SH, et al. Annual out-of-pocket expenditures and financial hardship among cancer survivors aged 18–64 years–United States, 2011–2016. Morb Mort Weekly Rep. 2019;68(22):494-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yabroff KR, Dowling EC, Guy GP Jr, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259-267. doi: 10.1200/JClinOncol.2015.62.0468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zheng Z, Han X, Zhao J, et al. Financial hardship, healthcare utilization, and health among U.S. cancer survivors. Am J Prev Med. 2020;59(1):68-78. doi: 10.1016/j.amepre.2020.02.016 [DOI] [PubMed] [Google Scholar]
- 28. Meernik C, Kirchhoff AC, Anderson C, et al. Material and psychological financial hardship related to employment disruption among female adolescent and young adult cancer survivors. Cancer. 2021;127(1):137-148. doi: 10.1002/cncr.33190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bellizzi KM, Smith A, Schmidt S, et al. ; Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) Study Collaborative Group. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer. 2012;118(20):5155-5162. doi: 10.1002/cncr.27512 [DOI] [PubMed] [Google Scholar]
- 30. Centers for Disease Control and Prevention. National Health Interview Survey, Survey Description. 2015. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2015/srvydesc.pdf
- 31. Tucker-Seeley RD, Thorpe RJ.. Material-psychosocial-behavioral aspects of financial hardship: a conceptual model for cancer prevention. Gerontologist. 2019;59(suppl 1):S88-S93. doi: 10.1093/geront/gnz033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yabroff KR, Bradley C, Shih YT.. Understanding financial hardship among cancer survivors in the United States: strategies for prevention and mitigation. J Clin Oncol. 2020;38(4):292-301. doi: 10.1200/JClinOncol.19.01564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zheng Z, Han X, Guy GP Jr., et al. Do cancer survivors change their prescription drug use for financial reasons? Findings from a nationally representative sample in the United States. Cancer. 2017;123(8):1453-1463. doi: 10.1002/cncr.30560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399-424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cepeda MS, Boston R, Farrar JT, Strom BL.. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158(3):280-287. doi: 10.1093/aje/kwg115 [DOI] [PubMed] [Google Scholar]
- 36. Austin PC, Jembere N, Chiu M.. Propensity score matching and complex surveys. Stat Methods Med Res. 2018;27(4):1240-1257. doi: 10.1177/0962280216658920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Huang IC, Bhakta N, Brinkman TM, et al. Determinants and consequences of financial hardship among adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort study. J Natl Cancer Inst. 2019;111(2):189-200. doi: 10.1093/jnci/djy120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. U.S. Department of Health and Human Services. Compilation of Patient Protection and Affordable Care Act. 2010. 2010. https://housedocs.house.gov/energycommerce/ppacacon.pdf
- 39. Nogueira LM, Chawla N, Han X, Jemal A, Yabroff KR.. Patterns of coverage gains among young adult cancer patients following the affordable care act. JNCI Cancer Spectr. 2019;3(1):pkz001. doi: 10.1093/jncics/pkz001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ji X, Shi KS, Mertens AC, et al. Survival in young adults with cancer is associated with Medicaid expansion through the affordable care act. J Clin Oncol. 2023;41(10):1909-1920. doi: 10.1200/JClinOncol.22.01742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kaiser Family Foundation. Status of State Medicaid Expansion Decisions: Interactive Map. KFF.https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Accessed December 21, 2022.
- 42. Althubaiti A. Information bias in health research: Definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211-217. doi: 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The NHIS data are publicly available and can be found at the website of the Centers for Disease Control and Prevention (https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm).