Abstract
Objective
This study aims to explore the influence of dyadic coping (DC) on the quality of life (QoL) of spousal caregivers for patients with cervical cancer and to investigate the mediating role of self-efficacy in this relationship.
Methods
A convenience sample of 206 spouses of cervical cancer patients from five hospitals in Jiangsu Province, China, was included in the study. The participants completed three instruments: the 12-item Short-Form Health Survey, the General Self-Efficacy Scale, and the Dyadic Coping Inventory. Structural Equation Modeling (SEM) was used to analyze the mediating effect of self-efficacy in the DC and QoL relationship.
Results
The study found a positive correlation between self-efficacy and DC. Self-efficacy partially mediated the impact of DC on QoL, accounting for 16% of the total effect. Self-efficacy played a mediating role in facilitating the indirect positive effects of DC on QoL.
Conclusions
Spousal caregivers of cervical cancer patients frequently experience a relatively low QoL. The results suggest that interventions aimed at enhancing DC among spousal caregivers should incorporate strategies to improve self-efficacy, given its mediating role in the positive relationship between DC and QoL.
Keywords: Cervical cancer, Dyadic coping, Self-efficacy, Quality of life, Spousal caregiver, Mediating effect
Introduction
Cervical cancer is the fourth most prevalent female malignancy worldwide and is a major global health concern.1 The most recent global cancer statistics have shown that China was the country with the second highest incidence of cervical cancer in the world in 2020, with nearly 110,000 women newly diagnosed with the disease,2 and the average patient's age is decreasing.3 However, despite the increase in cancer cases, the survival rate has been rising steadily due to medical and technological advancements.4 Spouses are the main supporters and caregivers of patients with cervical cancer,5 and the diagnosis and treatment of the disease puts patients and their spouses under tremendous stress. This stress directly affects the quality of life (QoL) of the spousal caregiver.6, 7, 8
QoL is a multidimensional, dynamic health construct that includes physical, psychological, social, and spiritual dimensions9 and provides a comprehensive reflection of health.10 Cancer-related studies have shown11, 12, 13 that partners of oncology patients not only have a poorer QoL, but the QoL of the patients and their spouses can also influence each other’s. Previous studies have shown that spouses of gynecologic cancer patients not only have to maintain their marriages, take care of their families, secure their financial resources, and bear high treatment costs14 but also face problems such as changes in their wives' femininity, early menopause, and sexual dysfunction caused by treatment15 and focused on bearing multiple burdens, with depression, anxiety, and other problems that are sometimes worse than those of cancer patients.14 Over time, these burdens have a tendency to exhaust their emotional and psychological capacities, rendering them more vulnerable to severe distress16 and maladaptive coping mechanisms. Consequently, this process ultimately diminishes their QoL17 and can even precipitate marital crises and disrupt familial harmony. The study revealed that when the role demands of caring for cancer patients exceed the coping capacity of spousal caregivers, caregivers experience physical, psychological, social, and financial stress, which results in caregiving load and adversely affects the QoL of patients and their spousal caregivers.17
These results have led to cancer being recognized as a “we disease.”18 Scholars19 have begun to consider the cancer patients and their spouses as a dyadic whole, focusing on the characteristics of the coping behaviors of both spouses during the coping process of the chronic illness, the impact of coping styles on the psychological well-being of both spouses, and the prognosis of the patient's progression of the disease, i.e., the dyadic coping (DC). DC refers to the joint responses and strategies of both partners in an intimate relationship when confronted with a dyadic stressful event during an illness.20 According to Bodenmann et al.,21 the Systemic Transactional Model DC includes both positive and negative dimensions. Positive DC forms benefit both partners and their relationship and include supportive, delegated, and common DC. Negative DC forms include hostile, ambivalent, and superficial efforts to assist the stressed partner.22 Studies have found that more positive DC styles are associated with higher relationship satisfaction, healthy couples' behavior, higher relationship quality, and higher QoL.23 The DC of both patients with hematologic neoplasms and their life partners affects the partners' subsequent psychological and physical QoL.24 Ştefănuţ et al.25 highlighted that DC of oncology patients and their spouse caregivers has a significant influence on the couple's QoL and that positive DC provided by patients and reported by the caregivers had the effect of improving caregivers' QoL.
In cancer coping, self-efficacy refers to the internal forces that motivate individuals to respond to stressors rather than avoid them.26 DC in couples affects the self-efficacy of cancer patients and their caregivers. The DC scores of young- and middle-aged couples facing cancer were significantly associated with self-efficacy.27 The communal coping and adjustment model posits that DC will alter people's living environment, thereby influencing their internal motivations to deal with stress, such as self-efficacy.28 The study revealed this occurs as a result of behavior change and stress response, both of which are important in providing care for people with cancer.29 A person's self-efficacy reflects the extent to which an individual realizes his or her potential and can increase it through learning.30 When caregivers have strong self-efficacy, they are more capable of overcoming a variety of difficulties and psychological strains, quickly adjusting their emotions, and taking the initiative to use social resources to provide their patients the best care possible.31 Previous study have found a positive correlation between caregiver self-efficacy and QoL:32 cancer caregivers with higher self-efficacy can better perform their caregiving tasks and provide higher-quality care, improving patients' QoL.30 Multiple intervention studies have shown that improving the self-efficacy of spouse caregivers significantly improves their physical and psychological health outcomes.32,33 Therefore, self-efficacy may play a mediating role between DC and the QoL of spouse caregivers of patients with cervical cancer.
This study is based on the Systemic Transactional Model21 and focuses on the relationships between QoL, self-efficacy, and DC. It is hypothesized that spouse caregivers who used a more positive DC strategy would also report a higher QoL and greater self-efficacy. Similarly, DC would impact QoL directly and indirectly through self-efficacy. Therefore, the present study explores the current status of DC, self-efficacy, and QoL among spouses of patients with cervical cancer and identifies the mechanisms by which DC affects QoL through self-efficacy. The findings may serve as a theoretical basis for developing targeted nursing interventions for caregivers of spouses of patients with cervical cancer.
Methods
Participants
Researchers recruited spouse caregivers of patients with cervical cancer for this cross-sectional study while accompanying cervical cancer patients to in-patient oncology and gynecology departments in five tertiary hospitals in Jiangsu Province, China. Patients with cervical cancer were hospitalized due to receiving treatments such as surgery or radiotherapy or chemotherapy. The inclusion criteria of spouse caregivers of cervical cancer patients included the following: (1) age over 18, (2) being currently married or in common-law relationship with a patient with cervical cancer, (3) taking care of a patient with cervical cancer on a daily basis with no pay, (4) no history of serious mental or cognitive impairment, (5) no terminal illness such as cancer or advanced heart diseases, and 6) being fluent in Chinese. The sample size was estimated based on the requirements of structural equation modeling (SEM) testing, where 10 respondents per estimated parameter are sufficient.34 The total number of the variances, regression coefficients, and exogenous variables is equal to the number of parameters. The number of parameters of this study was 18 (8 errors, 7 loadings, and 3 path coefficients). Based on the suggestion, 180 individuals should be selected. The target number of individuals considering a 20% nonresponse or drop-out rate was 216. Finally, data for 206 caregivers were included in the analysis record. The attrition rate was 4.6%.
Measures
General information questionnaire
A general information questionnaire collected information regarding age, marital status, education level, occupational status, place of residence, monthly income, knowledge of the human papillomavirus vaccine (HPV), and perceptions of the government's free cervical cancer-screening service. The aforementioned information was filled in by spousal caregivers, whereas clinical information on patients with cervical cancer, such as menopausal status (permanent cessation of menstruation), cancer stage, type of pathology, and therapy was obtained from medical records.
Dyadic coping
The Dyadic Coping Inventory35 was used to evaluate the specific dimensions of DC. It was adapted to Chinese,36 with 37 items and 6 subscales: stress communication (8 items), common dyadic coping (5 items), supportive dyadic coping (10 items), delegated dyadic coping (4 items), negative dyadic coping (8 items), and evaluation of dyadic coping (2 items). The response format for all the questions was a five-point Likert-type scale ranging from “(1) very little” to “(5) very much.” The DC dimensions are classified as either positive or negative.37 A positive DC style aims to maintain or restore individual well-being, while a negative one consists of activities characterized by a negative connotation. Score from all items except the “coping evaluation” subscale (items: 36 and 37) were summed to calculate the “dyadic coping” score which ranges from 37 to 175, with higher scores indicating more supportive behaviors.36 The cut-off scores established in the Dyadic Coping Inventory were determined by prior research, with a score of < 111 denoting below-average support, a score of 111–145 indicating normal level, and a score of > 145 exhibiting above-average support.38 In this study, the internal consistency of the total score was α = 0.890 and ranged from 0.903 to 0.977 on the 5 subscales discussed.
Self-efficacy
The General Self-Efficacy Scale was used to evaluate caregivers' general sense of self-efficacy.39 It is a 10-item Likert scale, where 1 = not at all true and 4 = completely true, and these were accumulated to obtain a total score of 10–40. The higher the score, the better the self-efficacy. Internally, the scale is consistent. In our sample, the alpha coefficient of Cronbach was 0.976.
Quality of life
The 12-item Short-Form Health Survey (SF-12),40 derived from the 36-item Short-Form Health Survey (SF-36), was utilized to evaluate the QoL among the participants. There are 12 items on the SF-12, with 8 subscales: physical functioning, role limitations due to physical problems, bodily pain, general health, vitality, social functioning, role limitations due to emotional problems, and perceived mental health. There are two summary scales: physical component score (PCS) and mental component score (MCS). The SF-12 has been administered to diverse populations (18 years and older) in China, and its psychometric properties are acceptable.41 In this study, QoL scores were transformed into T-scores using normative data from the general population in Jiangsu Province.42 The T-scores for PCS, MCS, and the eight subscales were below 50, indicating low QoL. There were 0.864 Cronbach's alpha coefficients for the full scale and 0.751 and 0.851 for the PCS and MCS subscales, respectively.
Data collection procedure
The original authors granted permission to utilize the standard instruments in the survey. Support from hospital management was obtained prior to data collection, participants were informed of the purpose and significance of the study, and consent was obtained from spousal caregivers of cervical cancer patients. The data collection was conducted in Jiangsu from December 2021 to September 2022. A convenience sampling method was used to select spouse caregivers of patients who were newly diagnosed with cervical cancer and hospitalized for treatment, before receiving treatment (surgery, radiotherapy, or chemotherapy). The researcher used standardized instruction to explain the precautions and requirements for completing the questionnaire and instructed the spouse caregivers to scan the QR code with their cell phones and complete the online questionnaire independently. The questionnaire was online, and participants were not allowed to submit until the last question was answered to complete the questionnaire. Therefore, there were no missing values in this study. Participants who answered the questions too quickly (less than 2 min) or too long (more than 20 min) were excluded from the study. If the spouses could not fill in the questionnaire themselves due to limitations in eyesight or literacy, the researcher helped to fill in the questionnaire by interview. The entire survey lasted approximately 5–15 min, and all participants were provided with small gifts.
Data analysis
The data were analyzed with SPSS Version 25.0 and Mplus 8.3. Normality was determined by analyzing skew and kurtosis using ±2 for skew and ±7 for kurtosis as cut-off scores.43 The SF-12 mean subscale scores (± standard deviation [SD]) in this study were converted to T-scores according to normative data from Jiangsu Province, China.42 The internal consistency, construct reliability, and convergent validity for each instrument were evaluated through confirmatory factor analysis. The common method bias was identified using Harman's single-factor test. The caregivers' demographic and patients' disease-related characteristics were analyzed using frequencies, percentages, means, and SDs. DC, self-efficacy, and QoL were analyzed using means and SDs. Differences in DC, self-efficacy, and QoL according to the demographic and cervical cancer patients' disease-related characteristics of the caregivers were analyzed using t tests, and one-way analysis of variance. On this basis, significant variables were controlled, and a partial correlation analysis was performed to examine the correlations among DC, self-efficacy, and QoL. The hypothesized model was examined with SEM. QoL was treated as the dependent variable, DC was treated as the independent variable, and self-efficacy was regarded as the mediating variable. A maximum-likelihood estimation structural model path analysis was carried out to verify the hypothesized relationships. The standardized root mean square residual (SRMR), chi-square test, the Tucker–Lewis index, the comparative fit index (CFI), and the root mean square error of approximation (RMSEA) were utilized to assess model fit. The bootstrapping approach was applied to examine the effects of the research model. A P-value of < 0.05 was considered significant.
Ethical consideration
This study, which involved human participants, was reviewed and approved by The Ethics Committee for Human Research at Burapha University and all study procedures were approved (IRB No. IRB3-067/2565). Informed written consent was also obtained from each participant before the study.
Results
Demographic and clinical characteristics
More than half of the 206 spousal caregivers were middle-aged (58.7%) and were married for > 20 years (56.3%). Most spousal caregivers had at least a junior high school diploma (69.5%) and low family income (< 5000 renminbi per month) (77.2%). The majority of the patients with cervical cancer were postmenopausal (72.8%), had cancer stage II or below (74.3%), had squamous cell carcinoma (78.6%), and were treated with surgery, radiotherapy, and chemotherapy (44.6%). The characteristics of the participants are shown in Table 1.
Table 1.
The demographic characteristics of spousal caregivers and clinical data of the patients with cervical cancer (N = 206).
| Characteristics | Participants (n = 206) |
|---|---|
| Spousal caregivers'characteristics | |
| Age (years), n (%) | |
| ≤ 40 | 55 (26.7) |
| 40–59 | 121 (58.7) |
| ≥ 60 | 30 (14.6) |
| Marital status, n (%) | |
| Married within 10 years | 36 (17.5) |
| Married within 10–20 years | 54 (26.2) |
| Married for over 20 years | 116 (56.3) |
| Education level, n (%) | |
| Elementary school or less | 63 (30.6) |
| Junior high school | 92 (44.7) |
| High school or more | 51 (24.8) |
| Occupation, n (%) | |
| Retired | 16 (7.8) |
| Employed | 175 (85.0) |
| Unemployed | 15 (7.3) |
| Residence, n (%) | |
| Rural | 93 (45.1) |
| Town | 46 (22.3) |
| County | 35 (17.0) |
| City | 32 (15.5) |
| Monthly income (renminbi [US $]), n (%) | |
| ≤ 3000 (410.8) | 92 (44.7) |
| 3000–5000 (410.18–684.80) | 67 (32.5) |
| ≥ 5000 (684.80) | 47 (22.8) |
| Awareness of human papillomavirus vaccine | |
| Yes | 52 (25.2) |
| No | 154 (74.8) |
| Perceptions of the government's free cervical cancer screening service | |
| Do not know at all | 96 (46.6) |
| Know some | 78 (37.9) |
| Know | 32 (15.5) |
|
Patients'characteristics Patients with menopausal status |
|
| Yes | 150 (72.8) |
| No | 56 (27.2) |
| Stage of cervical cancer, n (%) | |
| Precancerous lesion | 29 (14.1) |
| Stage I | 47 (22.8) |
| Stage II | 77 (37.4) |
| Stage III | 43 (20.9) |
| Stage IV | 10 (4.9) |
| Pathological type | |
| Precancerous lesion | 29 (14.1) |
| Squamous cell carcinoma | 162 (78.6) |
| Adenocarcinoma | 15 (7.3) |
| Therapy method | |
| Non-surgical treatment | 57 (27.7) |
| Surgery + radiotherapy + chemotherapy | 92 (44.7) |
| Surgical treatment | 57 (27.7) |
Dyadic coping, self-efficacy, and quality of life of spousal caregivers
The descriptive statistics of the components included in the model are listed in Table 2, including DC, self-efficacy, and QoL. The Harman’s single-factor test result revealed that eight factors with characteristic roots greater than one could be extracted from the unrotated solution and that the variance contribution rate of the first factor was not greater than 40% (31.28%), indicating that the common method bias was not severe.44 Throughout the variables, the skewness values varied from −1.90 to 0.96, and the kurtosis values from −0.70 to 2.41, indicating a relatively normal distribution. The T-scores of the PCS, MCS, as well as the eight subscales were below 50, indicating scores below the average (Table 2). The total DC score was divided into three levels according to the cutoff of 27.7% of the participants (n = 57) scored below the average level, 65.0% (n = 134) scored at the normal level, and 7.3% (n = 15) scored above the average level.
Table 2.
Descriptive characteristics of spousal caregivers for dyadic coping, self-efficacy, and quality of life.
| Variable | Rating, mean (SD) | T-scores, mean (SD) | Sk | Ku |
|---|---|---|---|---|
| Dyadic coping | ||||
| SC | 29.65 (7.31) | / | −0.67 | 0.43 |
| CDC | 18.09 (4.60) | / | −0.49 | 0.03 |
| SDC | 37.33 (9.66) | / | −0.81 | 0.49 |
| DDC | 15.11 (3.44) | / | −0.40 | 0.05 |
| NDC | 18.13 (11.28) | / | 0.96 | −0.54 |
| EDC | 7.52 (1.93) | / | −0.81 | 0.67 |
| Total | 118.31 (18.88) | / | −0.15 | 0.55 |
| Self-efficacy | 26.91 (7.29) | / | 0.12 | −0.45 |
| Quality of lifea | ||||
| PCS | 80.77 (22.97) | 45.80 (13.12) | −0.92 | 0.22 |
| PF | 85.07 (28.98) | 47.03 (15.58) | −1.90 | 2.41 |
| RP | 82.83 (28.10) | 46.29 (15.88) | −1.65 | 1.79 |
| BP | 84.96 (25.14) | 46.70 (14.70) | −1.53 | 1.32 |
| GH | 70.25 (31.59) | 43.20 (18.92) | −0.80 | −0.70 |
| MCS | 73.19 (19.58) | 44.42 (8.24) | −1.02 | 0.17 |
| VT | 69.90 (29.08) | 45.32 (13.10) | −0.98 | 0.27 |
| SF | 73.42 (31.92) | 48.74 (2.13) | −1.02 | 0.00 |
| RE | 78.22 (26.47) | 42.57 (16.54) | −1.22 | 0.91 |
| MH | 71.24 (20.20) | 41.07 (12.39) | −0.59 | 0.28 |
| Total | 76.98 (18.72) | 45.11 (9.50) | −0.92 | 0.22 |
SD, standard deviation; Sk, skewness; Ku, kurtosis; SC, stress communication; CDC, common dyadic coping; SDC, supportive dyadic coping; DDC, delegated dyadic coping; NDC, negative dyadic coping; EDC, evaluation of dyadic coping, PCS, physical component score; PF, physical functioning; RP, role limitations due to physical problems; BP, bodily pain; GH, general health; MCS, mental component score; VT, vitality; SF, social functioning; RE, role limitations due to emotional problems; MH, perceived mental health.
Transformed into T-scores based on the normative data from the general population in Jiangsu Province.
Preliminary correlation analyses
In Supplementary Table S1 of the supplementary materials, the one-way multivariate analysis' findings are presented. Education level, occupation, place of residence, monthly income, and awareness of the HPV, perceptions of the government's free cervical cancer–screening service were significantly related with DC, self-efficacy, and QoL scores. The caregivers with a high school diploma or higher, living in the city, aware of the HPV, and high income had the highest QoL, while clinical information on patients with cervical cancer did not correlate with caregiver’s QoL. These significant variables were included in the partial correlation as control variables. Statistically significant partial correlation was shown between the dependent and independent variables. DC was positively correlated with self-efficacy (r = 0.289, P < 0.001) and QoL (r = 0.241, P < 0.001). There is a positive correlation between self-efficacy and QoL (r = 0.312, P < 0.001) (Table 3).
Table 3.
Partial correlations among dyadic coping, self-efficacy, and quality of life while controlling for the effect of sociodemographic variables.
| Variables | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. DC | 1 | |||||||||
| 2. SC | 0.836∗∗∗ | 1 | ||||||||
| 3. SDC | 0.805∗∗∗ | 0.810∗∗∗ | 1 | |||||||
| 4. DDC | 0.827∗∗∗ | 0.799∗∗∗ | 0.831∗∗∗ | 1 | ||||||
| 5. CDC | 0.752∗∗∗ | 0.782∗∗∗ | 0.795∗∗∗ | 0.773∗∗∗ | 1 | |||||
| 6. NDC | −0.115 | −0.499∗∗∗ | −0.602∗∗∗ | −0.460∗∗∗ | −0.564∗∗∗ | 1 | ||||
| 7. SE | 0.289∗∗∗ | 0.307∗∗∗ | 0.407∗∗∗ | 0.400∗∗∗ | 0.418∗∗∗ | −0.351∗∗∗ | 1 | |||
| 8. QoL | 0.241∗∗∗ | 0.204∗∗ | 0.296∗∗∗ | 0.286∗∗∗ | 0.314∗∗∗ | −0.194∗∗ | 0.312∗∗∗ | 1 | ||
| 9. PCS | 0.269∗∗∗ | 0.210∗∗ | 0.293∗∗∗ | 0.274∗∗∗ | 0.296∗∗∗ | −0.138∗ | 0.313∗∗∗ | 0.930∗∗∗ | 1 | |
| 10. MCS | 0.125 | 0.135 | 0.213∗∗ | 0.221∗∗ | 0.248∗∗∗ | −0.224∗∗∗ | 0.218∗∗ | 0.812∗∗∗ | 0.541∗∗∗ | 1 |
Adjusted: education level, Occupation, Residence, income, awareness of human papillomavirus vaccine and learn about the government's free “Cervical and Breast Cancer Screening Service” for women.
DC, dyadic coping; SC, stress communication; SDC, supportive dyadic coping; DDC, delegated dyadic coping; CDC, common dyadic coping; NDC, negative dyadic coping; SE, self-efficacy; QoL, quality of life; PCS, physical component score; MCS, mental component score.
∗∗∗P < 0.001, ∗∗P < 0.01, ∗P < 0.05.
Measurement model analysis
This study presented two variables: DC and QoL; according to Table 4, the factor-loading parameters in the DC matrix (−0.608–0.930) and QoL matrix (0.672–0.833) were significant (P < 0.01). Each latent variable's construct reliability ranged between 0.726 and 0.865, exceeding the 0.7 threshold value45 and demonstrating excellent internal consistency. Moreover, the average variance extracted value for each concept was also higher than 0.5,46 showing sufficient convergence validity. In addition, the square roots of the average variance extracted coefficients (0.721, 0.573) were appreciably better than the squared correlation coefficient between both the constructs (r = 0.285), indicating satisfactory discriminant validity.
Table 4.
The confirmatory factor analysis of the measurement model.
| Latent variable | Measured variable | β | Β | C.R. | SMC | CR | AVE |
|---|---|---|---|---|---|---|---|
| Dyadic coping | SC CDC |
1 1.001 |
0.888 0.881 |
21.499∗∗ |
0.789 0.776 |
0.865 | 0.721 |
| SDC | 1.108 | 0.930 | 23.315∗∗ | 0.865 | |||
| DDC | 0.953 | 0.897 | 18.284∗∗ | 0.805 | |||
| NDC | −1.058 | −0.608 | −9.040∗∗ | 0.370 | |||
| Quality of life | PCS | 1 | 0.833 | 0.694 | 0.726 | 0.573 | |
| MCS | 0.506 | 0.672 | 4.073∗∗ | 0.452 |
B, unstandardized coefficients; β, standardized coefficients; C.R., critical ratio; SMC, squared multiple correlations; CR, construct reliability; AVE, average variance extracted; PCS, physical component score; MCS, mental component score; SC, stress communication; SDC, supportive dyadic coping; DDC, delegated dyadic coping; CDC, common dyadic coping; NDC, negative dyadic coping.
∗∗P < 0.01.
Structural model analysis
After synthesizing the aforementioned results, a SEM was constructed with DC as the predictor variable, self-efficacy as the mediator variable, and QoL as the outcome variable, which was tested and corrected by using the modification index. The following were evaluated as acceptance criteria:47 a chi-square to df ratio (χ2/df) < 3.0, TLI, and CFI values ≥ 0.90, SRMR values ≤ 0.05, and RMSEA value ≤ 0.08. This study's analysis data of the structural model suggested that χ2 = 44.512, df = 18, χ2/df = 2.473, TLI = 0.959, CFI = 0.974, SRMR = 0.031, and RMSEA = 0.085. The fitting indexes showed that the model was realistic and had a high degree of fitting.
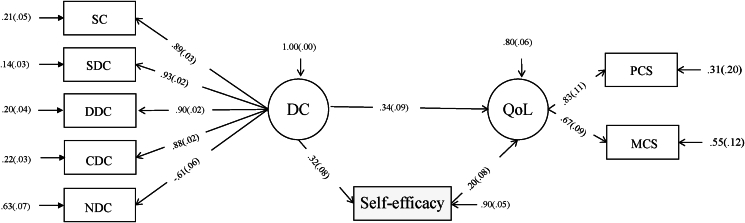
As shown in Table 5 and Fig. 1, the path coefficients are positive for all variables. Ninety percent of the variation in self-efficacy and 80% of the variation in QoL were explained by the model. The results for the direct effects of DC on self-efficacy (β = 0.324, P < 0.01), the direct effects of self-efficacy on QoL (β = 0.202, P < 0.01), and the direct effects of DC on QoL (β = 0.339, P < 0.01) were all positive and statistically significant. Moreover, DC indirectly positively affected QoL through self-efficacy (β = 0.065, P < 0.01), indicating a partial mediating effect on QoL through self-efficacy.
Table 5.
Path coefficient of self-efficacy on the relationship of dyadic coping and quality of life.
| Structural path | Path analysis coefficient |
Bootstrapping 95% CI |
|||||
|---|---|---|---|---|---|---|---|
| B | β | S.E. | C.R. | Lower | Upper | P | |
| Total effects | |||||||
| Dyadic coping → quality of life | 5.462 | 0.405 | 1.154 | 4.732 | 3.797 | 7.630 | < 0.001 |
| Direct effects | |||||||
| Dyadic coping → quality of life | 4.580 | 0.339 | 1.230 | 3.723 | 2.819 | 6.851 | < 0.001 |
| Self-efficacy → quality of life | 4.115 | 0.202 | 1.774 | 2.319 | 1.125 | 6.384 | 0.020 |
| Dyadic coping → self-efficacy | 0.214 | 0.324 | 0.057 | 3.767 | 0.131 | 0.311 | < 0.001 |
| Indirect effects | |||||||
| Dyadic coping → self-efficacy → quality of life | 0.882 | 0.065 | 0.433 | 2.037 | 0.305 | 1.750 | 0.042 |
B, unstandardized coefficients; β, standardized coefficients; S.E., standard error; C.R., critical ratio; CI, confidence interval.
Fig. 1.
Structural model predicted self-efficacy in the relationship of dyadic coping, and quality of life. DC, dyadic coping; SC, stress communication; SDC, supportive dyadic coping; DDC, delegated dyadic coping; CDC, common dyadic coping; NDC, negative dyadic coping; QoL, quality of life; PCS, physical component score; MCS, mental component score.
To verify the indirect effects of the dependent variable via mediators, bias-corrected percentile bootstrapping was performed on a sample of 5000 at a 95% confidence interval. The results in Table 5 confirmed the existence of significant direct and indirect effects of self-efficacy between DC and QoL, and the lower- and upper-level confidence intervals did not include zero. The mediating effect of self-efficacy accounted for 16.0% of the total effect (0.065/0.405).
Discussion
This study investigated the DC, self-efficacy, and QoL of spouses caring for cervical cancer patients. In addition, a mediator model using self-efficacy as a mediator was used to assess the internal mechanism of DC in predicting QoL. There was a 16% variance in QoL that could be attributed to this mediation model.
Spousal caregivers of cervical cancer patients had poor quality of life
In this study, the physical component score (45.80 ± 13.12) and mental component score (44.42 ± 8.24) of the QoL of the spouse caregiver were significantly lower than those reported in previous literature regarding the QoL of people in general who are 40 or older in Jiangsu Province.42 According to a previous study, there is a mutual impact on QoL of cancer patients and their family caregivers.48 It is anticipated that cancer patients’ daily lives and of those who care for them will be significantly disrupted.49 Moreover, it has been reported that family caregivers are involved in every step of cancer care and management and that they need to spend time, money, and physical strength navigating through the complex process of cancer care. This caregiving stress may have a detrimental effect on their physical and mental health.50 Thus, for spousal caregivers, taking care of cervical patients can be burdensome, resulting in a lower QoL. This study also found that the mental component of QoL of the spouse caregiver was relatively low, which may be linked to their psychological burden. Caregiving-related stress can deplete spousal caregivers' emotional and psychological reserves.51,52 In addition, participants in this study with less than an elementary school education, rural residence, low income, and ignorance of the HPV had lower QoL, and previous study also found that the QoL of caregivers was significantly correlated with monthly household income.53
Spousal caregivers of cervical cancer patients had a relatively low self-efficacy
Self-efficacy plays an important role in cancer patients and their caregivers' QoL, especially improving benefit-finding and relieving anxiety and/or depression in dyads of cancer patients and family caregiver.54 In the current study, the self-efficacy score of 206 spousal caregivers was (26.91 ± 7.29), which was lower than the norm (28.63 ± 6.18) of the scale.55 Researchers have found that Chinese cultures endorse a more traditional concept of gender roles than western cultures.56 It might be related to Confucian social ethics, which emphasizes the subordination of wives to their husbands, one of the Five Cardinal Relationships.57,58 Therefore, women are much more likely to consistently assume their domestic roles in China. However, caring for a cervical cancer patient is potentially extremely stressful for their spouses, who were thrust into a caregiving role unprepared. In this situation, spouses often feel helpless and emotionally overwhelmed—unable to assist themselves or their wives with the diagnosis.59 In addition, in this study, self-efficacy was connected to factors such as level of education, monthly income, occupation, place of residence, and awareness of HPV, and the high financial, psychological, and physical demands of caregiving during the care process may be related with low self-efficacy of spousal caregivers of patients with cervical cancer. Patients recover at a higher rate and have more faith in their ability to recover from disease when their caregivers are more confident.60 It is recommended that clinical medical staff actively implement effective interventions such as knowledge and sensitivity about the coping strategies to improve spousal caregivers’ self-efficacy and assist spousal caregivers of cervical cancer patients to deal with the disease.
The overall level of dyadic coping among spousal caregivers of cervical cancer patients was normal
This study found that the overall level of DC among spousal caregivers of cervical cancer patients was normal, which might help them face illness management for patients with cervical cancer. Cervical cancer patients experience several physical, psychological, social, and spiritual changes due to the disease. These adjustments may cause stress for the patients, who may need to work together with their spouses to manage the stress, leading to DC patterns.61 DC is how couples communicate and react to stress in one another to stabilize their marriages. According to research, patients and caregivers are interdependent, and jointly managing illness-related issues results in better QoL and coping with cancer outcomes.62 In a large population-based study, dyadic interventions tended to have a greater impact on improving relationships between couples and their communication and reducing psychological distress.63 According to a recent meta-analysis,64 DC correlates significantly with emotional functioning, as well as with the perception of relationship quality by couples, common dyadic coping, supportive dyadic coping, and delegated dyadic coping may strengthen marital relationships, reduce couples' pressure, and promote psychological health. Our research found that DC of spousal caregivers of patients with cervical cancer was favorably connected with QoL. Therefore, nursing staff should implement interventions to enhance DC to enhance both QoL and relationship quality in couples. Patients and their spouses can use positive DC to maintain or re-establish internal stability, fostering an environment of increased trust, support, and cohesion that will improve their wellbeing, both physical and psychological.65,66 For example, couples should be urged to concentrate on the positive sides of their care partnership to enhance the QoL, and cervical cancer patients and their spousal caregivers can practice positive DC by receiving instructions, appreciation, informational support, and tangible support from nursing staff.67
Self-efficacy partially mediated the relationship between quality of life and dyadic coping
This study developed a mediating model of DC in predicting QoL using self-efficacy as a mediator. The mediating effect of self-efficacy accounted for 16.0% of the total effect. The relationship between a caregiver and care receiver is unique compared to other social relationships. Because the recipient of care depends on the caregiver, the link between self-efficacy and QoL is inherently unbalanced and may be impacted by various sociocultural influences. This study discovered that self-efficacy partially mediates between DC and QoL. The self-efficacy of spousal caregivers was positively correlated with QoL. Self-efficacy is a kind of belief that one may achieve desired results through independent action, utilizing one's abilities and skills. People with a high level of self-efficacy are more certain of their ability to carry out plans of action and are more likely to achieve their goals.68 Therefore, self-efficacy was crucial in promoting positive health outcomes and healthy behavior.69 Several studies have reported that self-efficacy is correlated with QoL in cancer.70,71 The current findings discovered that self-efficacy plays a mediating role between DC and QoL, that is, DC can not only directly affect QoL but also affect spousal caregivers' self-efficacy, thereby affecting QoL. Clinically, acknowledging the existence of such relationships aids in improving the QoL of spousal caregivers of patients with cervical cancer. Healthcare professionals should take action to promote the self-efficacy and DC of partners of cervical cancer patients.
Strength and limitation
This research is the first to investigate DC, self-efficacy, and QoL in spousal caregivers of cervical cancer patients in China and to examine the mediating function of self-efficacy between DC and QoL. The limitation was that no cervical cancer patients were involved. Future research might take a examine at how a couple's self-efficacy affects the relationship between DC and QoL. Our research findings highlight the importance of additional investigation into the interactions between DC-care recipient factors. To have a better understanding of how caregiver self-efficacy influences their QoL, longitudinal research would be useful for examining how caregiver self-efficacy affects the QoL of spousal caregivers over time.
Conclusions
The findings of this research add to the knowledge system by demonstrating the significance of self-efficacy in DC and relationships with QoL for spousal caregivers of patients with cervical cancer. The results revealed that spousal caregivers had poor levels of self-efficacy and QoL. Given that self-efficacy mediates relationships, the importance of spousal caregiver self-efficacy in enhancing their physical and mental health should be emphasized in the intervention process. Nurses should assist spousal caregivers in adjusting to their new roles. Moreover, nursing staff should try to implement dyadic-level interventions by concentrating on husbands and wives and assisting them in cooperatively sharing responsibility for disease management.
CRediT author statement
CW: Conceptualization, Data curation, Investigation, Writing – Original draft preparation. CW: Conceptualization, Methodology, Supervision, Writing – Reviewing and Editing. PH: Software, Data curation.
All authors were granted complete access to all the data in the study, with the corresponding author bearing the final responsibility for the decision to submit for publication. The corresponding author affirms that all listed authors fulfill the authorship criteria and that no others meeting the criteria have been omitted.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
This work was supported by Ministry of Science and Technology of China “One Belt, One Road” Innovation Talent Exchange Program for Foreign Experts (Grant No. DL2022014005L), and Jiangsu Higher Education Institution Innovative Research Team for Science and Technology (2023). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Ethics statement
This study which involved human participants was reviewed and approved by The Ethics Committee for Human Research at the Burapha University and all study procedures were approved (IRB No. IRB3-067/2565).
Data availability statement
Access to the datasets that were used and analyzed for this research on a reasonable request.
Declaration of Generative AI and AI-assisted technologies in the writing process
No AI tools/services were used during the preparation of this work.
Acknowledgments
Spousal caregivers of cervical cancer patients who participated in the study, as well as the hospital staff members who assisted in the data collection are all acknowledged by the authors for their assistance.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.apjon.2023.100354.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
References
- 1.Guo M., Xu J., Du J. Trends in cervical cancer mortality in China from 1989 to 2018: an age-period-cohort study and Joinpoint analysis. BMC Publ Health. 2021;21(1):1329. doi: 10.1186/s12889-021-11401-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H., Ferlay J., Siegel R.L., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Li X., Zheng R., Li X., et al. Trends of incidence rate and age at diagnosis for cervical cancer in China, from 2000 to 2014. Chin J Cancer Res. Dec 2017;29(6):477–486. doi: 10.21147/j.issn.1000-9604.2017.06.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) 2018. International agency for Research on cancer.http://gco.iarc.fr/today/home Accessed 11-14. [Google Scholar]
- 5.Li Q., Chiang V.C., Xu X., Xu Y., Loke A.Y. The experiences of Chinese couples living with cancer: a focus group study. Cancer Nurs. Sep-Oct 2015;38(5):383–394. doi: 10.1097/ncc.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 6.Stenberg U., Ruland C.M., Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho Oncol. Oct 2010;19(10):1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 7.Ketcher D., Trettevik R., Vadaparampil S.T., Heyman R.E., Ellington L., Reblin M. Caring for a spouse with advanced cancer: similarities and differences for male and female caregivers. J Behav Med. Oct 2020;43(5):817–828. doi: 10.1007/s10865-019-00128-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An Y., Fu G., Yuan G. Quality of life in patients with breast cancer: the influence of family caregiver's burden and the mediation of patient's anxiety and depression. J Nerv Ment Dis. Nov 2019;207(11):921–926. doi: 10.1097/nmd.0000000000001040. [DOI] [PubMed] [Google Scholar]
- 9.Sibeoni J., Picard C., Orri M., et al. Patients' quality of life during active cancer treatment: a qualitative study. BMC Cancer. Oct 4 2018;18(1):951. doi: 10.1186/s12885-018-4868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung Y.B., Neo S.H.S., Teo I., et al. Development and evaluation of a quality of life measurement scale in English and Chinese for family caregivers of patients with advanced cancers. Health Qual Life Outcome. Feb 14 2019;17(1):35. doi: 10.1186/s12955-019-1108-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janda M., Neale R.E., Klein K., et al. Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatology. Mar-Apr 2017;17(2):321–327. doi: 10.1016/j.pan.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Boehmer U., Stokes J.E., Bazzi A.R., Clark M.A. Dyadic quality of life among heterosexual and sexual minority breast cancer survivors and their caregivers. Support Care Cancer. Jun 2020;28(6):2769–2778. doi: 10.1007/s00520-019-05148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bodschwinna D., Ernst J., Mehnert-Theuerkauf A., Gündel H., Weissflog G., Hönig K. Dyadic coping and social support: various types of support in hematooncological patients and their spouses-Associations with psychological distress. Psycho Oncol. Jul 2021;30(7):1041–1050. doi: 10.1002/pon.5631. [DOI] [PubMed] [Google Scholar]
- 14.Teskereci G., Kulakaç O. Life experiences of caregivers of women with gynaecological cancer: a mixed-methods systematic review. Eur J Cancer Care. Jan 2018;27(1) doi: 10.1111/ecc.12456. [DOI] [PubMed] [Google Scholar]
- 15.Facchin F., Buggio L., Vercellini P., Frassineti A., Beltrami S., Saita E. Quality of intimate relationships, dyadic coping, and psychological health in women with endometriosis: results from an online survey. J Psychosom Res. Jul 2021;146 doi: 10.1016/j.jpsychores.2021.110502. [DOI] [PubMed] [Google Scholar]
- 16.Üzar-Özçeti N.Y., Dursun S. Quality of life, caregiver burden, and resilience among the family caregivers of cancer survivors. Eur J Oncol Nurs. Oct 2020;48 doi: 10.1016/j.ejon.2020.101832. [DOI] [PubMed] [Google Scholar]
- 17.Li Y., Wang K., Yin Y., Li Y., Li S. Relationships between family resilience, breast cancer survivors' individual resilience, and caregiver burden: a cross-sectional study. Int J Nurs Stud. Dec 2018;88:79–84. doi: 10.1016/j.ijnurstu.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 18.Kayser K., Watson L.E., Andrade J.T. Cancer as a “we-disease”: examining the process of coping from a relational perspective. Fam Syst Health. 2007;25(4):404–418. doi: 10.1037/1091-7527.25.4.404. [DOI] [Google Scholar]
- 19.Meier F., Cairo Notari S., Bodenmann G., Revenson T.A., Favez N. We are in this together - aren't we? Congruence of common dyadic coping and psychological distress of couples facing breast cancer. Psycho Oncol. Dec 2019;28(12):2374–2381. doi: 10.1002/pon.5238. [DOI] [PubMed] [Google Scholar]
- 20.Huiying A., Changying C., Panpan W., Shuainan L., Xiaojing H. Research progress of dyadic coping in cancer patients and their spouse. Chinese Nursing Management. 2019;19(7):1064–1069. doi: 10.3969/j.issn.1672-1756.2019.07.022. [DOI] [Google Scholar]
- 21.Bodenmann G., Falconier M., Randall A.K. In: Encyclopedia of Couple and Family Therapy. Lebow J., Chambers A., Breunlin D.C., editors. Springer International Publishing; 2017. Systemic-transactional model of dyadic coping; pp. 1–7. [Google Scholar]
- 22.Falconier M.K., Kuhn R. Dyadic coping in couples: a conceptual integration and a review of the empirical literature. Front Psychol. 2019;10:571. doi: 10.3389/fpsyg.2019.00571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Revenson T.A., Kayser K.E., Bodenmann G.E. American Psychological Association; 2005. Couples Coping with Stress: Emerging Perspectives on Dyadic Coping. xvi, 209-xvi, 209. [Google Scholar]
- 24.Ernst J., Hinz A., Niederwieser D., et al. Dyadic coping of patients with hematologic malignancies and their partners and its relation to quality of life - a longitudinal study. Leuk Lymphoma. Mar 2017;58(3):655–665. doi: 10.1080/10428194.2016.1194983. [DOI] [PubMed] [Google Scholar]
- 25.Ştefănuţ A.M., Vintilă M., Bădău L.M., et al. Perception of disease, dyadic coping, and the quality of life of oncology patients in the active treatment phase and their life partners: an approach based on the actor-partner interdependence model. Front Psychol. 2023;14 doi: 10.3389/fpsyg.2023.1069767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karademas E.C., Simos P., Pat-Horenczyk R., et al. The interplay between trait resilience and coping self-efficacy in patients with breast cancer: an international study. J Clin Psychol Med Settings. Mar 2023;30(1):119–128. doi: 10.1007/s10880-022-09872-x. [DOI] [PubMed] [Google Scholar]
- 27.An H., Chen C., Du R., Cheng C., Wang P., Dong S. Self-efficacy, psychological distress, and marital quality in young and middle-aged couples facing lymphoma: the mediating effect of dyadic coping. Psycho Oncol. Sep 2021;30(9):1492–1501. doi: 10.1002/pon.5711. [DOI] [PubMed] [Google Scholar]
- 28.Helgeson V.S., Jakubiak B.K., Van Vleet M., Zajdel M. Communal coping and adjustment to chronic illness: theory update and evidence. Pers Soc Psychol Rev. May 2018;22(2):170–195. doi: 10.1177/1088868317735767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Leary A. Self-efficacy and health: behavioral and stress-physiological mediation. Cognit Ther Res. 1992;16(2):229–245. doi: 10.1007/BF01173490. [DOI] [Google Scholar]
- 30.Bei-bei L., Wei-li W., Yu Z. Relation among post-traumatic growth, coping styles and self-efficacy of the primary caregivers of cancer patients. Chinese General Practice. 2016;19:5. [Google Scholar]
- 31.Jun W.-H., Cha K.-S., Lee K.-L. The mediating effect of depression on the relationship between social support, spirituality and burnout in family members of patients with cancer. Int J Environ Res Publ Health. 2021;18(4):1727. doi: 10.3390/ijerph18041727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomas Hebdon M.C., Coombs L.A., Reed P., Crane T.E., Badger T.A. Self-efficacy in caregivers of adults diagnosed with cancer: an integrative review. Eur J Oncol Nurs. Jun 2021;52 doi: 10.1016/j.ejon.2021.101933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Q., Xu Y., Zhou H., Loke A.Y. A couple-based complex intervention for Chinese spousal caregivers and their partners with advanced cancer: an intervention study. Psycho Oncol. Nov 2015;24(11):1423–1431. doi: 10.1002/pon.3809. [DOI] [PubMed] [Google Scholar]
- 34.Hair J.F. 7th ed. Pearson Education; Upper Saddle River, N.J.: 2010. Multivariate Data Analysis: A Global Perspective. [Google Scholar]
- 35.Bodenmann G., Arista L.J., Walsh K.J., Randall A.K. In: Encyclopedia of Couple and Family Therapy. Lebow J., Chambers A., Breunlin D.C., editors. Springer International Publishing; 2018. Dyadic coping inventory; pp. 1–5. [Google Scholar]
- 36.Xu F., Hilpert P., Randall A.K., Li Q., Bodenmann G. Validation of the Dyadic Coping Inventory with Chinese couples: factorial structure, measurement invariance, and construct validity. Psychol Assess. Aug 2016;28(8):e127–e140. doi: 10.1037/pas0000329. [DOI] [PubMed] [Google Scholar]
- 37.Randall A.K., Hilpert P., Jimenez-Arista L.E., Walsh K.J., Bodenmann G. Dyadic coping in the U.S.: psychometric properties and validity for use of the English version of the dyadic coping inventory. Curr Psychol. 2016;35(4):570–582. doi: 10.1007/s12144-015-9323-0. [DOI] [Google Scholar]
- 38.Tang N., Jia Y., Zhao Q., et al. Influencing factors of dyadic coping among infertile women: a path analysis. Original research. Front Psychiatr. 2022;13 doi: 10.3389/fpsyt.2022.830039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang J.X., Schwarzer R. Measuring optimistic self-beliefs: a Chinese adaptation of the general self-efficacy scale. Psychologia: Int J Psychol Orient. 1995;38(3):174–181. [Google Scholar]
- 40.Ware J., Jr., Kosinski M., Keller S.D. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. Mar 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Li L., Wang H., Shen Y. Development and psychometric tests of a Chinese version of the SF-36 health survey scales. Zhonghua Yufang Yixue Zazhi. Mar 2002;36(2):109–113. [PubMed] [Google Scholar]
- 42.Yanan W., Jinyi Z., Jian S., et al. Reliability,validity and standard model of the quality of life scale for residents aged 40 and over in 6 counties and districts in Jiangsu. South China J Prev Med. Dec 2021;47:1401–1404+1409. [Google Scholar]
- 43.Muthen B., Kaplan D. A comparison of some methodologies for the factor analysis of non-normal Likert variables: a note on the size of the model. Br J Math Stat Psychol. 1992;45(1):19–30. doi: 10.1111/j.2044-8317.1992.tb00975.x. [DOI] [Google Scholar]
- 44.Podsakoff P.M., Organ D.W. Self-reports in organizational research: problems and prospects. J Manag. 1986;12(4):531–544. doi: 10.1177/014920638601200408. [DOI] [Google Scholar]
- 45.Peterson R.A., Kim Y., Choi B. A meta-analysis of construct reliability indices and measurement model fit metrics. Methodology. 2020;16(3):208–223. doi: 10.5964/meth.2797. [DOI] [Google Scholar]
- 46.Fornell C., Larcker D.F. Evaluating structural equation models with unobservable variables and measurement error. J Market Res. 1981;18(1):39–50. doi: 10.1177/002224378101800104. [DOI] [Google Scholar]
- 47.Hu L-t, Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 48.Lin Y., Hu C., Xu Y., Zhao J., Li Q. The mutual impact and moderating factors of quality of life between advanced cancer patients and their family caregivers. Support Care Cancer. 2020;28(11):5251–5262. doi: 10.1007/s00520-020-05351-x. [DOI] [PubMed] [Google Scholar]
- 49.Kamau R.K., Osoti A.O., Njuguna E.M. Effect of diagnosis and treatment of inoperable cervical cancer on quality of life among women receiving radiotherapy at Kenyatta National Hospital. East Afr Med J. Jan 2007;84(1):24–30. doi: 10.4314/eamj.v84i1.9487. [DOI] [PubMed] [Google Scholar]
- 50.ZaH Saimaldaher, Wazqar D.Y. Relationships between caregiving stress, mental health and physical health in family caregivers of adult patients with cancer: implications for nursing practice. Scand J Caring Sci. 2020;34(4):889–898. doi: 10.1111/scs.12795. [DOI] [PubMed] [Google Scholar]
- 51.Clarijs M.E., Oemrawsingh A., Bröker M.E.E., Verhoef C., Lingsma H., Koppert L.B. Quality of life of caregivers of breast cancer patients: a cross-sectional evaluation. Health Qual Life Outcome. Feb 19 2022;20(1):29. doi: 10.1186/s12955-022-01930-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tang S.T., Hsieh C.H., Chiang M.C., et al. Impact of high self-perceived burden to others with preferences for end-of-life care and its determinants for terminally ill cancer patients: a prospective cohort study. Psycho Oncol. Jan 2017;26(1):102–108. doi: 10.1002/pon.4107. [DOI] [PubMed] [Google Scholar]
- 53.Lu L., Pan B., Sun W., Cheng L., Chi T., Wang L. Quality of life and related factors among cancer caregivers in China. Psychiatr Clin Neurosci. Oct 2010;64(5):505–513. doi: 10.1111/j.1440-1819.2010.02131.x. [DOI] [PubMed] [Google Scholar]
- 54.Cao Q., Gong J., Chen M., Lin Y., Li Q. The dyadic effects of self-efficacy on quality of life in advanced cancer patient and family caregiver dyads: the mediating role of benefit finding, anxiety, and depression. Journal of Oncology. 2022;2022 doi: 10.1155/2022/3073358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schwarzer R., Born A. Optimistic self-beliefs: assessment of general perceived self-efficacy in thirteen cultures. World Psychology. 1997;3(1-2):177–190. [Google Scholar]
- 56.Hu Y., Scott J. Family and gender values in China: generational, geographic, and gender differences. J Fam Issues. 2014;37(9):1267–1293. doi: 10.1177/0192513X14528710. [DOI] [Google Scholar]
- 57.Han Q. An overview of Traditional Chinese family ethics. Quarterly Journal of Chinese Studies. 2012;1(1):85–99. [Google Scholar]
- 58.Woods P.R., Lamond D.A. What would confucius do? – Confucian ethics and self-regulation in management. J Bus Ethics. 2011;102(4):669–683. doi: 10.1007/s10551-011-0838-5. [DOI] [Google Scholar]
- 59.Lewis F.M., Griffith K.A., Wu K.-C., Shands M.E., Zahlis E.H. Helping Us Heal: telephone versus in-person marital communication and support counseling for spouse caregivers of wives with breast cancer. Support Care Cancer. 2022;30(1):793–803. doi: 10.1007/s00520-021-06439-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Molloy G.J., Johnston M., Johnston D.W., et al. Spousal caregiver confidence and recovery from ambulatory activity limitations in stroke survivors. Health Psychol. Mar 2008;27(2):286–290. doi: 10.1037/0278-6133.27.2.286. [DOI] [PubMed] [Google Scholar]
- 61.Vellone E., Chung M.L., Cocchieri A., Rocco G., Alvaro R., Riegel B. Effects of self-care on quality of life in adults with heart failure and their spousal caregivers: testing dyadic dynamics using the actor-partner interdependence model. J Fam Nurs. Feb 2014;20(1):120–141. doi: 10.1177/1074840713510205. [DOI] [PubMed] [Google Scholar]
- 62.Chen H.L., Annie Kao T.-S., Reuille K.M., Northouse L. FOCUS Program: treating patients with cancer and family caregivers as a unit of care. Clin J Oncol Nurs. 2021;25(3):E17–E25. doi: 10.1188/21.CJON.E17-E25. [DOI] [PubMed] [Google Scholar]
- 63.Juan W., Jin Z. The mediating effect of self-efficacy between social support and benefit finding among caregivers of hospitalized patients with cancer. Chinese General Practice. 2020;6(1):5–9. [Google Scholar]
- 64.Chen M., Gong J., Cao Q., Luo X., Li J., Li Q. A literature review of the relationship between dyadic coping and dyadic outcomes in cancer couples. Eur J Oncol Nurs. 2021;54 doi: 10.1016/j.ejon.2021.102035. [DOI] [PubMed] [Google Scholar]
- 65.Brandão T., Brites R., Hipólito J., Pires M., Nunes O. Dyadic coping, marital adjustment and quality of life in couples during pregnancy: an actor-partner approach. J Reprod Infant Psychol. Feb 2020;38(1):49–59. doi: 10.1080/02646838.2019.1578950. [DOI] [PubMed] [Google Scholar]
- 66.Shi G., Shi T., Liu Y., Cai Y. Relationships between dyadic coping, intimate relationship and post-traumatic growth in patients with breast cancer: a cross-sectional study. J Adv Nurs. Dec 2021;77(12):4733–4742. doi: 10.1111/jan.14946. [DOI] [PubMed] [Google Scholar]
- 67.Juwitasari Harini R., Rosyad A.A. Husband support mediates the association between self-efficacy and cervical cancer screening among women in the rural area of Indonesia. Asia Pac J Oncol Nurs. Sep-Oct 2021;8(5):560–564. doi: 10.4103/apjon.apjon-2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chirico A., Lucidi F., Merluzzi T., et al. A meta-analytic review of the relationship of cancer coping self-efficacy with distress and quality of life. Oncotarget. May 30 2017;8(22):36800–36811. doi: 10.18632/oncotarget.15758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chin C.H., Tseng L.M., Chao T.C., Wang T.J., Wu S.F., Liang S.Y. Self-care as a mediator between symptom-management self-efficacy and quality of life in women with breast cancer. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Choi Y.Y., Rha S.Y., Park J.S., Song S.K., Lee J. Cancer coping self-efficacy, symptoms and their relationship with quality of life among cancer survivors. Eur J Oncol Nurs. 2023;66 doi: 10.1016/j.ejon.2023.102373. [DOI] [PubMed] [Google Scholar]
- 71.Liu K.-L., Chuang C.-K., Pang S.-T., et al. Emotional state and cancer-related self-efficacy as affecting resilience and quality of life in kidney cancer patients: a cross-sectional study. Support Care Cancer. 2022;30(3):2263–2271. doi: 10.1007/s00520-021-06644-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Access to the datasets that were used and analyzed for this research on a reasonable request.