Abstract
Objective
To evaluate the effects of yoga on health-related outcomes [i.e., physical function, mental health, and overall quality of life (QOL)] of cancer survivors via a systematic review and meta-analysis of randomized controlled trials (RCTs) over the past 5 years across cancer types.
Methods
An updated systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. RCTs published from January 1, 2018, to February 23, 2023, were searched in five English databases (PubMed, The Cochrane Library, ISI, PsycINFO, and CINAHL), three Chinese databases (Wan Fang, China National Knowledge Infrastructure, and Chinese Biomedical Literature Database), and three English clinical trials registry platforms (International Clinical Trials Registry Platform, ClinicalTrials.gov, and EU Clinical Trials Register).
Results
A total of 34 RCTs were included in this updated review. Yoga benefited the physical function, mental health, and overall QOL of cancer survivors. The effect size of yoga for most physical and mental health-related outcomes was relatively small, but that for the QOL was generally large. The impact of yoga on the QOL of cancer survivors ranged from moderate to high.
Conclusions
Yoga has health benefits for cancer survivors and could therefore be used as an optional supportive intervention for cancer-related symptom management.
Keywords: Yoga, Cancer survivors, Symptom management, Health-related outcomes, Systematic review, Meta-analysis
Introduction
Although cancer is a leading cause of death globally, advances in cancer treatment continue to improve survival rates.1 The overall 5-year relative survival rate for all types of cancer combined is 68%,1 resulting in a steady increase in the number of cancer survivors. After active cancer treatment, cancer survivors often experience numerous adverse disease- and treatment-related outcomes, including pain, fatigue, insomnia, anxiety, and depression, which substantially affect their quality of life (QOL).2,3 Evidence suggests that yoga effectively reduces some physical and psycho-emotional symptoms and improves the QOL of cancer survivors.4,5
Yoga was originally developed in Indian philosophy approximately 4000 years ago and has become a popular exercise for promoting physical and mental well-being in the general population.5,6 It is practiced as a mind–body therapy or an exercise that involves a combination of spiritual practices, physical activities, breathing, and meditation.5,6 Yoga practitioners focus their minds on specific postures with inner awareness and a meditative focus. The health benefits of yoga include improvements not only in physical function but also in mental health.4,5 The mechanism proposed to explain the health benefits of yoga involves a decrease in dysregulation within the sympathetic nervous system and the hypothalamic–pituitary–adrenal axis through the body's stress response.7, 8, 9 Yoga can enhance the activity of the parasympathetic nervous system and consequently reduce the level of the stress hormone cortisol.10 This effect helps restore the existing autonomic nervous system imbalance and reduce the allostatic load within stress response systems to recover optimal homeostasis among yoga practitioners.8,10 Hence, cancer survivors are recommended to undertake yoga as a regular exercise for improving their health.11,12
Although a number of systematic reviews summarizing the available evidence on the effects of yoga among cancer survivors exist, most randomized controlled trials (RCTs) on yoga included in a recently published systematic review were conducted in or before 2019.5,13, 14, 15, 16 The results showed that there is still a lack of strong evidence on the benefits of yoga on symptoms (e.g., pain), physical functions (e.g., exercise capacity), and physiological changes (e.g., immune responses) in cancer survivors.13, 14, 15, 16 In recent years, more research has further explored these benefits of yoga in more types of cancer survivors. An updated systematic review and meta-analysis are needed to combine previous and current evidence from comprehensive evaluations of yoga for cancer.
Therefore, this study aimed to evaluate the effects of yoga on health-related outcomes including physical function, mental health, and overall QOL of cancer survivors through an updated systematic review and meta-analysis of RCTs over the past 5 years across cancer types.
Methods
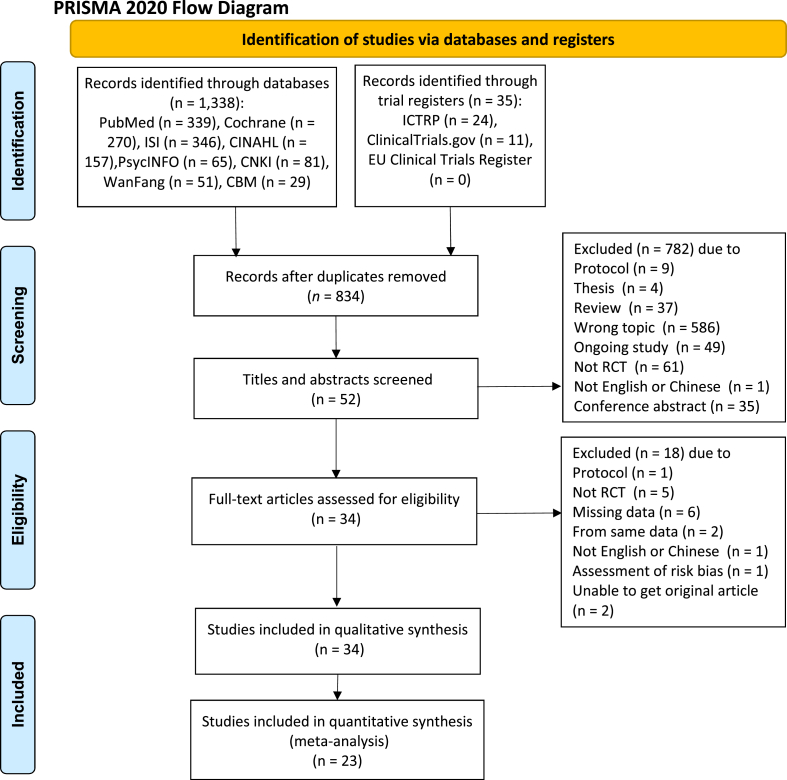
This study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).17 The PRISMA flow diagram of study selection is shown in Fig. 1.
Fig. 1.
Flow diagram of study selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomized controlled trial.
Search strategy
Parallel electronic searches for RCTs on yoga in adults with cancer published from January 1, 2018, to February 23, 2023, were conducted in five English databases (PubMed, The Cochrane Library, ISI, PsycINFO, and CINAHL), three English clinical trials registry platforms (International Clinical Trials Registry Platform, ClinicalTrials.gov, and EU Clinical Trials Register), and three Chinese databases (Wan Fang, China National Knowledge Infrastructure, and Chinese Biomedical Literature Database). The keywords and terms used in various combinations during the search included “neoplasms∗,” “cancer∗,” “tumor∗,” “malignan∗,” “carcino∗,” “lymphoma∗,” “adenocarcinoma∗,” and “yoga.” The detailed search strategy or search history is shown in Appendix 1.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) participants: adult (age > 18 years) survivors of any type of cancer; (2) group: at least two: experimental (yoga) group, which received any type of yoga as an intervention or yoga plus other combined intervention, and control group, which received usual care or the same intervention as the combined intervention in the yoga group; (3) primary outcomes: physical function (e.g., exercise capacity), biological indicators [e.g., serum anti-inflammatory factor tumor necrosis factor-α (TNF-α) level], cancer-related symptoms (e.g., pain, sleep disturbances, and fatigue), and mental health-related outcomes (e.g., anxiety and depression); secondary outcome: overall QOL; (4) design: RCT; and (5) publication language: English or Chinese. The exclusion criteria were duplicate publications, study protocols, theses, reviews, ongoing studies, and conference abstracts.
Data extraction and quality assessment
The following data were independently extracted from eligible studies by two reviewers (NN and RH) in accordance with the eligibility criteria: author/s, publication year, cancer type, sample size, intervention-related information, physical and mental health-related outcomes assessed, and assessment time. The risk of bias was judged by two reviewers (NN and JZ) using the Cochrane Collaboration's tool for risk of bias assessment.18 The Joanna Briggs Institute (JBI) Levels of Evidence and Grades of Recommendation tool was used to assess the quality of evidence. In the JBI evidence grading system, the evidence level is divided into five levels from high to low: level 1 to level 5.19 Any discrepancy was resolved through discussion with a third author (JZ or YZ).
Data analysis
Review Manager version 5.4 (Cochrane Collaboration) was used to generate pooled estimates of the effect size.20 Standardized mean differences (SMDs) and mean differences (MDs) with their corresponding 95% confidence intervals (CIs) were used for comparisons. SMDs of < 0.4, 0.4–0.7, and > 0.7 reflect small, moderate, and large effect sizes, respectively.20 Heterogeneity among the trials was assessed using the Higgins I2 statistic and Q test. I2 values of ≥ 50% and P values of < 0.1 were considered to indicate high heterogeneity of evidence, and the random-effects model was used to evaluate the effects of the intervention conservatively. Conversely, I2 values of < 50% and P values of > 0.1 were considered to indicate low-to-moderate heterogeneity, and the fixed-effects model was used. A sensitivity analysis was conducted to explore the potential sources of heterogeneity. P values of < 0.05 were considered statistically significant. Potential publication bias was not evaluated, as fewer than 10 studies were included in the meta-analysis. Individual study results that could not be pooled in the meta-analysis were summarized qualitatively.
Results
A total of 1373 records were identified through electronic searches. After exclusion of duplicates, 834 records remained. A preliminary screening of titles and abstracts was then conducted in accordance with the inclusion and exclusion criteria, yielding 52 remaining records. After further evaluation of the full-text articles, 34 studies were finally included (Fig. 1).
Characteristics of the included studies and levels of evidence
A total of 2552 cancer survivors were included in this review. The sample size of each study varied from 20 to 358 participants. The duration of the interventions ranged from 5 days to 48 weeks. Table 1 shows the characteristics of the included studies. The JBI evidence grading system was used to assess the level of evidence. Overall, the level of evidence among the studies was relatively high. Table 2 details the levels of evidence.
Table 1.
Characteristics of included studies.
| Author, year | Participants |
Intervention |
Measurements | Main outcomes | Assessment time | ||
|---|---|---|---|---|---|---|---|
| Cancer type | Sample size | YG | CG | ||||
| Jain et al, 2023 | Breast cancer | YG: 42 CG: 40 |
Yoga, 30 min/session, 5 days/week, 48 weeks | Usual care | EORTC QLQ-C30; Serum cytokines and oxidative stress markers | Yoga significantly improved QOL (P < 0.001) and reduced IFN-γ, TNF-α and MDA levels (P < 0.05). | Baseline, 16, 32, and 48 weeks |
| Lu et al, 2023 | Lung cancer | YG: 36 CG: 34 |
Yoga breathing exercises, 20 min/session, twice a day, 9–14 days | Usual care | BS; 6MWT; HADS; Thoracic closed drainage time | Significant difference for dyspnea and anxiety (P < 0.05) were found in yoga group when compared to the control group. | Admission, the day before surgery, and discharge |
| Zhang et al, 2023 | Lung cancer | YG: 40 CG: 40 |
Yoga, 30 min/session, 2 days/week, 8 weeks | Usual care | PSS; SAS; SDS; PPQ | Yoga group reported lower PSS, SAS and SDS scores and higher PPQ scores than control group (P < 0.05). | Baseline, 8 weeks |
| Greaney et al, 2022 | Breast cancer | YG: 13 CG: 13 |
Yoga, 30 min/session, 3 times/week, the end of treatment (12–20 weeks) | Usual care | Weight change; FACT-G; Serum cytokines | Control group increased weight while yoga group lost weight (P < 0.05). There was no significance in QOL, TNF-α and CRP between two groups. | Baseline and the end of treatment |
| Kaushik et al, 2022 | Prostate cancer | YG: 12 CG: 14 |
Yoga, 60 min/session, 2 times/week, 12 weeks (6 weeks preoperatively and postoperatively) | Usual care | FACT-G; FACT-P; FACIT-F; EPIC; Serum cytokines and immune cell levels | Yoga significantly increased Fc receptor III and IFN-γ expression and decreased G-CSF and MCP-1 levels (P < 0.05). | Baseline (6 weeks preoperatively), immediately before surgery, and 6 weeks postoperatively |
| Knoerl et al, 2022 | Breast, gastrointestinal, and gynecological cancer | YG: 23 CG: 14 |
Yoga, 45 min/session, 8 weeks | Usual care | BPI; PROMIS (pain interference, sleep-related impairment, anxiety, fatigue, depression and physical function); QLQ-CIPN20 | When compared to control group, yoga showed significant improvements in fatigue and depression (P < 0.05). | Baseline, 8 weeks |
| Liu et al, 2022 | Breast cancer | YG: 68 CG: 68 |
Yoga, 90 min/week, 8 weeks | Usual care | HADS; PFS; BPI; FACT-B | Significant difference for anxiety, depression and QOL were reported in yoga group when compared to the control group (P < 0.05). | Baseline, 8 and 20 weeks |
| Naderi et al, 2022 | Breast cancer | YG: 10 CG: 10 |
Yoga plus a high dose of vitamin D, 60–90 min/session, 2 times/week, 12 weeks | A high dose of vitamin D | Height, weight, and body fat measurements; Handgrip strength tests; EORTC QLQ-C30; Serum cytokines | Yoga group demonstrated significant improvements in body fat percentage, handgrip strength and QOL (P < 0.05). The level of IL-10 was increased, while IL-6 expression level declined in yoga group. | Baseline, 12 weeks |
| Sohl et al, 2022 | Gastrointestinal cancer | YG: 23 CG: 21 |
Yoga, four 30 min sessions, practice daily, 14 weeks | Usual care | PROMIS (fatigue, depression, sleep disturbances); PSS; Serum cytokines | Yoga found a larger reduction in fatigue, depression and sleep disturbances than control group. Serum IL-6, sTNF-R1 levels were lower than control group. | Baseline, 8, 10 and 14 weeks |
| Xing et al, 2022 | Cervical cancer | YG: 46 CG: 46 |
Yoga plus Clean intermittent catheterization, 8 weeks | Clean intermittent catheterization | Bladder function assessment; QLICP-CE | Significant difference for recovery time of self-urination, duration of indwelling catheter, residual urine volume, bladder neck mobility and QLICP-CE (P < 0.0001) were reported in yoga group when compared to control group. | Baseline, 8 weeks |
| Carson et al, 2021 | Breast cancer | YG: 30 CG: 18 |
Yoga, 15–30 min/day, 5–6 times/week, 8 weeks | Usual care | Self-made pain scale | There were no different treatment effects between 2 groups. More practice durations were related to the lower pain within yoga group. | Baseline, daily assessment on alternate weeks |
| D'Cunha et al, 2021 | Cervical cancer | YG: 24 CG: 24 |
Yoga, 23 min/session, 5 times/week, 5 weeks | Usual care | Self-made stress scale | Yoga revealed less stress than the control groups (P < 0.001). | Baseline, 5 weeks |
| Eyigör et al, 2021 | Breast cancer | YG: 15 CG: 16 |
Yoga, 60 min/session, 2 times/week, 10 weeks | Usual care | Phase angle; EORTC QLQ-C30; Arm volume; BMI | The comparisons between the 2 groups showed no significant differences. | Baseline, 10 weeks |
| Khedmati et al, 2021 | Breast cancer | YG: 10 CG: 10 |
Yoga plus a high dose of vitamin D, 60–90 min/session, 2 times/week, 12 weeks | A high dose of vitamin D | RWT; Shoulder flexibility; BAI; Serum cytokines | Yoga group found significant improvements in RWT, shoulder flexibility and anxiety (P < 0.05). The expression of blood leukocyte P53 and Bcl2 level was higher than control group (P < 0.05). | Baseline, 12 weeks |
| Zetzl et al, 2021 | Unlimited type | YG: 69 CG: 67 |
Yoga, 60 min/session, 1 times/week, 8 weeks | Usual care | EORTC QLQ-FA12; PHQ-9; EORTC QLQ-C15-PAL | When compared to control group, yoga revealed significant improvements in fatigue, depression and QOL (P < 0.05). | Baseline, 10 weeks |
| Zhi et al, 2021 | Breast and gynecological cancer | YG: 21 CG: 20 |
Yoga, 60 min/session, every day, 8 weeks | Usual care | HADS; BFI; ISI; TES | Yoga relieved anxiety significantly when compared to control group (P < 0.05). | Baseline, 4, 8 and 12 weeks |
| Chen et al, 2021 | Unlimited type | YG: 57 CG: 61 |
Yoga, 20 min/session, 3 to 6 times/week, 8 weeks | Usual care | NRS; FACT-G; PSQI | Yoga group significantly improved QOL, sleep quality (P < 0.05), and reduced fatigue (P < 0.01) when compared to control group. | Baseline, 8 weeks |
| Bao et al, 2020 | Breast and gynecological cancer | YG: 21 CG: 20 |
Yoga, 60 min/session, every day, 8 weeks | Usual care | NRS (pain, numbness, and tingling); FACT/GOG-Ntx subscale; Functional reach test; Chair to stand; Number of falls; 4-Meter walk speed | Yoga group found significant improvements in pain, neurotoxicity, functional reach test and chair to stand test when compared to control group (P < 0.05). | Baseline, 4, 8 and 12 weeks |
| Prakash et al, 2020 | Breast cancer | YG: 48 CG: 52 |
Yoga, 2 times/day, 15 weeks | Usual care | EORTC QLQ-C30 | Yoga revealed significant advantages on increasing QOL (P < 0.05). | Baseline, 3, 6, 9, 12 and 15 weeks |
| Li et al, 2020 | Lung cancer | YG: 70 CG: 69 |
Yoga breathing exercises, 16 min/session, every day, 4 weeks | Usual care | EORTC QLQ-C30; 6MWT; SpO2; Pulse; BS | Significant improvements of 6MWT were reported in yoga when compared to control group (P < 0.05). | Baseline, 4 weeks |
| Yang et al, 2020 | Unlimited type | YG: 57 CG: 57 |
Yogic meditation, 30 min/session, twice a day, 1 week | Usual care | BPI | Yoga relieved pain symptom significantly when compared to control group (P < 0.05). | Baseline, 1 week |
| Huberty et al, 2019 | Myeloproliferative neoplasm | YG: 27 CG: 21 |
Yoga, 60 min/week, 12 weeks | Usual care | SAF; PROMIS (anxiety, depression, pain, sleep disturbance, sexual function, global health, and quality of life); Serum cytokines | Yoga showed small effects on anxiety, sleep and pain, and a moderate effect on depression. TNF-α in yoga group was found a decline from baseline to 12 weeks. | Baseline, 7, 12, and 16 weeks |
| Kothari et al, 2019 | Unlimited type | YG: 50 CG: 50 |
Yoga plus standard antiemetic therapy, 60 min/session, 5 days | Standard antiemetic therapy | Nausea and vomiting | Yoga reduced vomiting significantly when compared to control group (P < 0.05). | 3 days post- chemotherapy |
| Lin et al, 2019 | Unlimited type | YG: 177 CG: 181 |
Yoga, 75 min/session, 2 days/week, 4 weeks | Usual care | MFSI; PSQI | Significant improvements of fatigue and sleep were observed in yoga when compared to control (P < 0.01). | Baseline, 4 weeks |
| Milbury et al, 2019 | Glioma | YG: 10 CG: 10 |
Yoga, 45 min/session, 2 or 3 times/week, through radiotherapy | Usual care | MDASI-BT; CES-D; BFI; SF-36 | Yoga performed significant effects on improving cancer-related symptoms, depression and mental QOL when compared to control group. | Baseline, the last day of radiotherapy |
| Milbury et al, 2019 | Lung or esophageal cancer | YG: 13 CG: 13 |
Yoga, 60 min/session, 2 or 3 times/week, 6 weeks | Usual care | SF-36; CES-D; 6MWT | Yoga performed significant effects on improving 6MWT and QOL when compared to control group. | Baseline, the last day of radiotherapy, 12 weeks |
| Porter et al, 2019 | Breast cancer | YG: 35 CG: 20 |
Yoga, 120 min/week, 8 weeks | Usual care | BPI; BFI; PSQI; HADS; FFMQ; 6MWT | Modest improvements of fatigue, anxiety, depression and 6MWT were found in yoga group when compared to control group. | Baseline, 8, 12 and 24 weeks |
| Barassi et al, 2018 | Lung cancer | YG: 16 CG: 16 |
yoga breathing, 10 min/session, 30 times/day, 1 week | Usual care | Pulmonary and cardiocirculatory parameter | Yoga revealed significant advantages on improving heart rate and SpO2 when compared to control group (P < 0.05). | Baseline, 1 week |
| Chaoul et al, 2018 | Breast cancer | YG: 74 CG: 85 |
Yoga, 75–90 min/session, 4 sessions during chemotherapy, 3 booster sessions through follow up | Usual care | PSQI; BFI; Objective sleep parameter | Yoga found fewer sleep disturbances than control group after 1 week treatment (P < 0.05). | Baseline, 1 week, 3, 6, 12 months |
| Eyigor et al, 2018 | Breast cancer | YG: 22 CG: 14 |
Yoga, 60 min/session, 2 times/week, 10 weeks | Usual care | VAS; EORTC QLQ-C30; BDI; 6MWT | No significant differences were observed between the 2 groups. The improvements of pain in shoulder and arm were found within yoga group. | Baseline, 10 weeks |
| Hardoerfer et al, 2018 | Unlimited type | YG: 37 CG: 33 |
Yoga, 60 min/session, 1 times/week, 8 weeks | Usual care | GAD; PHQ-2; EORTC QLQ-FA | Yoga reduced anxiety significantly when compared to control group (P < 0.05). | Baseline, 8 weeks |
| Jong et al, 2018 | Breast cancer | YG: 47 CG: 36 |
Yoga, 75 min/session, 1 times/week, 12 weeks | Usual care | MFSI; FQL; EORTC QLQ-C30; EORTC QLQ-BR; HADS; IES | No significant differences were observed between the 2 groups. In sub-scale of EORTC QLQ-C30, yoga reported less nausea and vomiting than control group at 24 weeks. | Baseline, 12 and 24 weeks |
| Taylor et al, 2018 | Breast cancer | YG: 14 CG: 12 |
Yoga, 75 min/session, 1 times/week, 8 weeks | Usual care | BFI; ISI; CES-D; PSS | Yoga reduced depression significantly when compared to control group (P < 0.01). | Baseline, 8 weeks |
| Winters-Stone et al, 2018 | Breast cancer | YG: 47 CG: 43 |
Yoga, 30 min/session, 3 times/week, 8 weeks | Usual care | POMS-B; IPAQ-short; Physical activity stage assessment instrument | Significant improvements of fatigue, physical activity and exercise readiness were observed in yoga when compared to control group (P < 0.05). | Baseline, 4 and 8 weeks |
YG, Yoga group; CG, Control group; EORTC QLQ-C30, European organization for research and treatment of cancer quality of life questionnaire-core 30; QOL, Quality of life; IFN-γ, Interferon-γ; TNF-α, , Tumor necrosis factor-α; MDA, Malondialdehyde; BS, Borg scale; 6MWT, 6-min walk test; HADS, Hospital anxiety and depression scale; PSS, Perceived stress scale; SAS, Self-rating anxiety scale; SDS, Self-rating depression scale; PPQ, Psychological capital questionnaire; FACT-G, Functional assessment of cancer therapy-general; FACT-P, Functional assessment of cancer therapy-prostate cancer; FACIT-F, Functional assessment of chronic illness therapy-fatigue questionnaire; EPIC, Expanded prostate index composite questionnaire; G-CSF, Granulocyte colony stimulating factor; MCP-1, Monocyte chemoattractant protein-1; PROMIS, Patient-reported outcome measurement information system; BPI, Brief pain inventory; QLQ-CIPN20, Quality of life questionnaire-chemotherapy induced peripheral neuropathy; PFS, Piper fatigue scale; FACT-B, Functional assessment of cancer therapy-breast cancer; IL-10, Interleukin-10; IL-6, Interleukin-6; QLICP-CE, Quality of life instruments for cancer patients-cervical cancer; BMI, Body mass index; RWT, Rockport walk test; BAI, Beck anxiety inventory; EORTC QLQ-FA, European organization for research and treatment of cancer quality of life questionnaire-fatigue; PHQ, Patient Health Questionnaire; EORTC QLQ-C15-PAL, European organization for research and treatment of cancer quality of life questionnaire-core 15 - palliative cancer; BFI, Brief fatigue inventory; ISI, Insomnia severity index; TES, Treatment expectancy scale; NRS, Numerical rating scale; PSQI, Pittsburgh sleep quality index; FACT/GOG-Ntx, Functional assessment of cancer therapy/gynecologic oncology group-neurotoxicity; SAF, Symptom assessment form; MFSI, Multidimensional fatigue symptom inventory; MDASI-BT, MD Anderson symptom inventory-brain tumor module; CES-D, Center for epidemiological studies-depression measure; SF-36, Medical outcomes study 36-item short-form survey; FFMQ, Five facet mindfulness questionnaire; VAS, Visual analogue scale; BDI, Beck Depression Inventory; GAD, General anxiety disorder; FQL, Fatigue Quality List; EORTC QLQ-BR, European organization for research and treatment of cancer quality of life questionnaire-breast cancer; IES, Impact of events scale; POMS-B, Profile of mood states-brief version; IPAQ-short, International physical activity questionnaire-shortform.
Table 2.
Evidence certainty of outcomes.
| No. | Outcomes | Evidence certainty |
|---|---|---|
| 1 | Yoga on fatigue at 4, 8, 10 weeks after intervention | Level 1a |
| 2 | Yoga on fatigue at 16, 24 weeks after intervention | Level 1c |
| 3 | Yoga on anxiety at 8, 12 weeks after intervention | Level 1a |
| 4 | Yoga on anxiety before surgery and at discharge | Level 1c |
| 5 | Yoga on anxiety at 16, 24 weeks after intervention | Level 1c |
| 6 | Yoga on depression at 8, 10, 12 weeks after intervention | Level 1a |
| 7 | Yoga on depression at 16, 24 weeks after intervention | Level 1c |
| 8 | Yoga on pain at 12 weeks after intervention | Level 1a |
| 9 | Yoga on pain at 1, 16 weeks after intervention | Level 1c |
| 10 | Yoga on sleep at 4, 8, 12 weeks after intervention | Level 1a |
| 11 | Yoga on QOL at 8 weeks after intervention | Level 1a |
| 12 | Yoga on global health, function and symptom of EORTC QLQ-C30 at 12 weeks after intervention | Level 1a |
| 13 | Yoga on 6MWT at 4 weeks after intervention | Level 1c |
| 14 | Yoga on 6MWT at 12 weeks after intervention | Level 1a |
| 15 | Yoga on heart rate and SpO2 after 1 week of intervention | Level 1c |
| 16 | Yoga on body fat percentage, handgrip strength, Rockport walk test, shoulder flexibility, functional reach test and chair to stand test at 12 weeks after intervention | Level 1c |
| 17 | Yoga on serum TNF-α, IL-6, IFN-γ, G-CSF, MCP-1, MDA, IL-10, P53 and Bcl2 levels | Level 1c |
| 18 | Yoga on neurotoxicity, nausea and vomiting, cancer-related symptom, stress, psychological capital and urinary function of patients | Level 1c |
QOL, Quality of life; EORTC QLQ-C30, European organization for research and treatment of cancer quality of life questionnaire-core 30; 6MWT, 6-min walk test; TNF-α, Tumor necrosis factor-α; IL-6, Interleukin-6; IFN-γ, Interferon-γ; G-CSF, Granulocyte colony stimulating factor; MCP-1, Monocyte chemoattractant protein-1; MDA, Malondialdehyde.
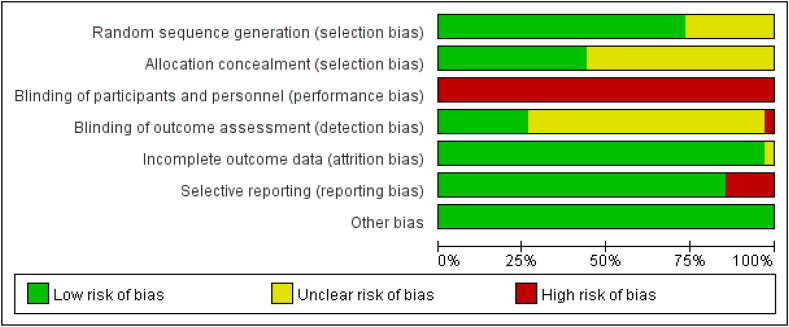
Methodological quality of the included studies
The evaluation of methodological quality revealed that all studies had a medium risk of bias. Owing to the nature of yoga, it was difficult to achieve blinding of patients and interveners. Therefore, all performance biases in the included studies were considered high risk. Furthermore, the sources of the risk of bias were associated with insufficient reports of randomization, allocation concealment, or evaluator blinding. Fig. 2 shows the results of the risk of bias assessment of the included studies.
Fig. 2.

(a) Risk of bias graph. (b) Risk of bias summary.
Effects of yoga on pain
Three studies21, 22, 23 reported the effects of yoga on pain 12 weeks after the intervention. The heterogeneity among these studies was high (P = 0.08, I2 = 61%), so a random-effects model was applied. The results showed no significant difference between the two groups (n = 144; SMD = −0.32; 95% CI = −0.86, 0.22) [Fig. 3(a)]. However, the sensitivity analysis suggested that the study by Porter et al23 had a large effect on the heterogeneity. No heterogeneity was observed when this study was removed (P = 0.46, I2 = 0%). There was a significant difference between the two groups (n = 89; SMD = −0.58; 95% CI = −1.01, −0.15; P = 0.008) [Fig. 3(b)]. The results were not stable, so the effects of yoga on pain among cancer survivors after 12 weeks of intervention must be verified by more studies. The results of three studies22,24,25 were reported qualitatively. Yang et al.24 observed that yoga relieved pain symptoms significantly after 1 week of intervention. For the long-term effects, Huberty et al.22 showed that yoga had moderate effects on reducing pain at 16 weeks. Carson et al.25 demonstrated that practice sessions of longer duration were related to lower daily pain levels within the yoga group.
Fig. 3.
(a) Mean changes of pain from baseline to 12 weeks after intervention; (b) Mean changes of pain from baseline to 12 weeks after intervention by sensitivity analysis.
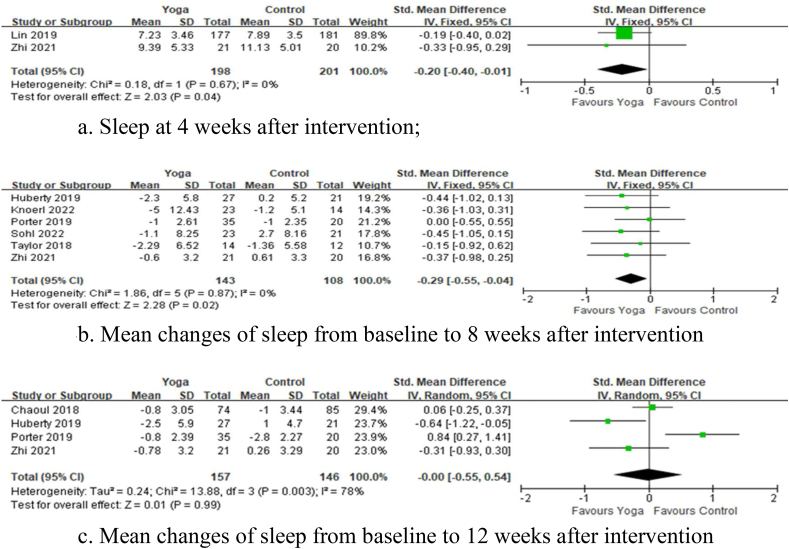
Effects of yoga on sleep quality
Two studies26,27 reported the effects of yoga on sleep 4 weeks after the intervention. No heterogeneity among these studies was found (P = 0.67, I2 = 0%). The results revealed that yoga significantly improved the sleep quality in cancer survivors 4 weeks after the intervention compared with the control intervention (n = 399; SMD = −0.2; 95% CI = −0.4, −0.01; P = 0.04) [Fig. 4(a)]. Six studies22,23,27, 28, 29, 30 reported the effects of yoga on sleep 8 weeks after the intervention. There was no heterogeneity among these studies (P = 0.87, I2 = 0%). The meta-analysis showed that yoga significantly improved sleep compared with the control intervention (n = 251; SMD = −0.29; 95% CI = −0.55, −0.04; P = 0.02) [Fig. 4(b)]. Four studies22,23,27,31 reported the effects of yoga on sleep 12 weeks after the intervention. The heterogeneity among these studies was high (P = 0.003, I2 = 78%), so a random-effects model was used. The results showed no significant difference between the two groups (n = 303; SMD = −0.00; 95% CI = −0.55, 0.54; P = 0.99) [Fig. 4(c)].
Fig. 4.
(a) Sleep at 4 weeks after intervention; (b) Mean changes of sleep from baseline to 8 weeks after intervention; (c) Mean changes of sleep from baseline to 12 weeks after intervention.
Effects of yoga on fatigue
Three studies26,27,32 reported the effects of yoga on fatigue 4 weeks after the intervention. The heterogeneity was high among these studies (P = 0.05, I2 = 67%), so a random-effects model was applied. The results showed no significant difference between the two groups (n = 489; SMD = −0.09; 95% CI = −0.49, 0.3; P = 0.64) [Fig. 5(a)]. However, the sensitivity analysis suggested that the study by Zhi et al.27 had a large effect on the heterogeneity. No heterogeneity was observed when this study was removed (P = 0.62, I2 = 0%). There was a significant difference between the two groups (n = 448; SMD = −0.29; 95% CI = −0.48, −0.11; P = 0.002). The meta-analysis results were unstable, indicating the need for further exploration.
Fig. 5.
(a) Fatigue at 4 weeks after intervention; (b) Mean changes of fatigue from baseline to 8 weeks after intervention; (c) Fatigue at 10 weeks after intervention.
Nine studies22,23,27, 28, 29, 30,32, 33, 34 reported the effects of yoga on fatigue 8 weeks after the intervention. The heterogeneity among these studies was low (P = 0.28, I2 = 18%). The results showed no significant difference between the two groups (n = 547; SMD = −0.06; 95% CI = −0.23, 0.11; P = 0.48) [Fig. 5(b)]. Two studies29,35 reported the effects of yoga on fatigue 10 weeks after the intervention. No heterogeneity was detected among these studies (P = 0.78, I2 = 0%). The results indicated that yoga significantly improved fatigue in cancer survivors 10 weeks after the intervention (n = 180; SMD = −0.63; 95% CI = −0.93, −0.33; P < 0.01) [Fig. 5(c)]. The results of two studies22,23 could not be pooled, so a qualitative description was adopted. For the long-term effects, Huberty et al.22 found that yoga was more effective in reducing fatigue than the control intervention at 16 weeks, and Porter et al.23 confirmed this positive effect at 24 weeks.
Effects of yoga on exercise capacity
Three studies23,36,37 reported the effects of yoga on the 6-min walk test (6MWT) distance 12 weeks after the intervention. The heterogeneity among these studies was high (P = 0.05, I2 = 66%), so a random-effects model was used. The results showed no significant difference between the two groups (n = 117; MD = 6.31; 95% CI = −42.99, 55.61; P = 0.80) [Fig. 6(a)]. The results of five studies21,38, 39, 40, 41 were reported qualitatively. Barassi et al.38 found that yoga significantly improved the heart rate and SpO2 after 1 week of intervention compared with the control intervention. Li et al.39 observed that yoga significantly improved the 6MWT distance 4 weeks after the intervention. Some studies demonstrated the physical benefits of yoga 12 weeks after the intervention. Naderi et al.40 showed the advantages of yoga in improving body fat percentage and handgrip strength. Khedmati et al.41 reported that patients in the yoga group performed better on the Rockport walk test and shoulder flexibility test. Bao et al.21 found significant effects on the functional reach test and chair–stand test results.
Fig. 6.
(a) Mean changes of 6MWT from baseline to 12 weeks after intervention.
Effects of yoga on serum cytokine level
Owing to insufficient data for the pooled analysis, only descriptive analyses were performed. Five studies22,29,40,42,43 reported the relationship between the serum level of the anti-inflammatory factor TNF-α and yoga. Jain et al.42 found that the decline in the TNF-α level in the yoga group was better than that in the control group at 48 weeks of follow-up. Huberty et al.22 showed a significant decrease in the TNF-α level within the yoga group at 12 weeks of follow-up. However, Greaney et al.,43 Naderi et al.,40 and Sohl et al.29 reported non-significant changes. For the serum level of the anti-inflammatory factor interleukin (IL)-6, Naderi et al.,40 Huberty et al.,22 and Sohl et al.29 all found a significant decline in the yoga group. For the serum level of interferon-γ, Jain et al.42 showed a significant decrease in the yoga group, but Kaushik et al.44 noted the opposite. In addition, the yoga group showed significant increases in the serum granulocyte colony-stimulating factor,44 monocyte chemotactic protein-1,44 and malondialdehyde levels,42 and significant decreases in the serum IL-10,40 anti-apoptotic gene P53,41 and anti-apoptotic gene Bcl2 levels.41
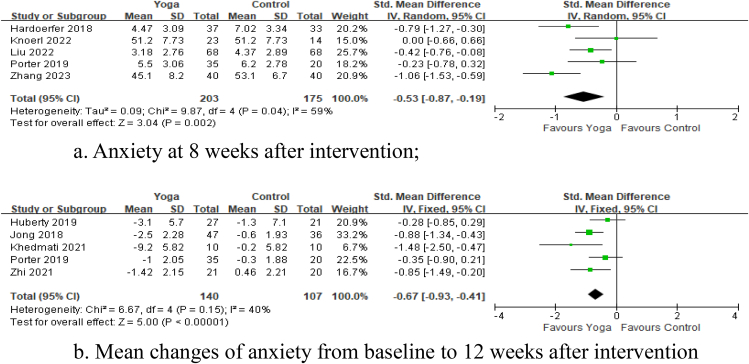
Effects of yoga on anxiety
Five studies23,28,33,34,45 reported the effects of yoga on anxiety 8 weeks after the intervention. The heterogeneity was high among these studies (P = 0.04, I2 = 59%), so a random-effects model was applied. The results showed that yoga significantly improved anxiety in cancer survivors 8 weeks after the intervention (n = 378; SMD = −0.53; 95% CI = −0.87, −0.19; P = 0.002) [Fig. 7(a)]. Five studies22,23,27,41,46 reported the effects of yoga on anxiety 12 weeks after the intervention. The heterogeneity among these studies was low (P = 0.15, I2 = 40%). The meta-analysis revealed that yoga significantly reduced anxiety compared with the control intervention (n = 247; SMD = −0.67; 95% CI = −0.93, −0.41; P < 0.01) [Fig. 7(b)]. Three studies22,23,47 were reported qualitatively. Lu et al.47 found that yoga breathing training after admission and at discharge significantly improved anxiety among lung cancer survivors. Concerning long-term effects, Huberty et al.22 found that yoga had small effects on reducing anxiety at 16 weeks. Porter et al.23 discovered that yoga yielded modest improvements in anxiety at 24 weeks.
Fig. 7.
(a) Anxiety at 8 weeks after intervention; (b) Mean changes of anxiety from baseline to 12 weeks after intervention.
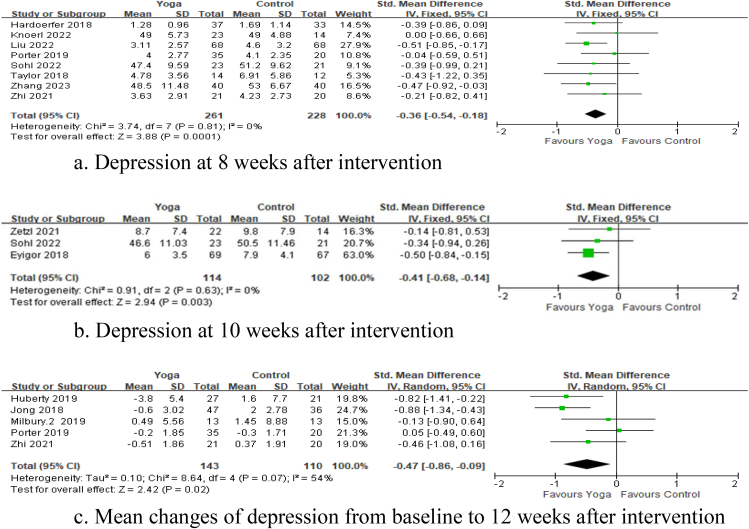
Effects of yoga on depression
Eight studies23,27, 28, 29, 30,33,34,45 reported the effects of yoga on depression 8 weeks after the intervention. There was no heterogeneity among these studies (P = 0.81, I2 = 0%). The meta-analysis showed that yoga significantly reduced depression compared with the control intervention (n = 489; SMD = −0.36; 95% CI = −0.54, −0.18; P < 0.01) [Fig. 8(a)]. Three studies29,35,36 reported the effects of yoga on depression 10 weeks after the intervention. No heterogeneity among these studies was found (P = 0.63, I2 = 0%). There was a significant difference between the two groups (n = 216; SMD = −0.41; 95% CI = −0.68, −0.14; P < 0.01), which indicated that yoga significantly improved depression in cancer survivors 10 weeks after the intervention [Fig. 8(b)]. Five studies22,23,27,37,46 reported the effects of yoga on depression 12 weeks after the intervention. The heterogeneity was high among these studies (P = 0.07, I2 = 54%), so a random-effects model was applied. The results revealed that yoga significantly reduced depression in cancer survivors 12 weeks after the intervention compared with the control intervention (n = 253; SMD = −0.47; 95% CI = −0.86, −0.09; P = 0.02) [Fig. 8(c)]. The results of two studies22,23 were reported qualitatively. For the long-term effects, Huberty et al.22 showed that yoga had moderate effects on reducing depression at 16 weeks. Porter et al.23 discovered that yoga yielded improvements in depression at 24 weeks compared with the control intervention.
Fig. 8.
(a) Depression at 8 weeks after intervention; (b) Depression at 10 weeks after intervention; (c) Mean changes of depression from baseline to 12 weeks after intervention.
Effects of yoga on QOL
Four studies34,35,48,49 reported the effects of yoga on the QOL 8 weeks after the intervention. These studies showed high heterogeneity (P = 0.006, I2 = 76%), so a random-effects model was used. The meta-analysis showed that yoga significantly improved the QOL compared with the control intervention (n = 482; SMD = 0.65; 95% CI = 0.27, 1.02; P = 0.001) [Fig. 9(a)]. Five studies36,40,46,50,51 reported the effects of yoga on the global health subdomain of the EORTC QLQ-C30 12 weeks after the intervention. The heterogeneity among these studies was low (P = 0.29, I2 = 20%). Yoga had significant advantages in improving global health (n = 270; MD = 9.58; 95% CI = 6.27, 12.89; P < 0.01) [Fig. 9(b)]. Three studies36,40,50 reported the effects of yoga on the functional subdomain of the EORTC QLQ-C30 12 weeks after the intervention. The heterogeneity was high among these studies (P = 0.005, I2 = 81%). No significant difference was found between the two groups (n = 87; MD = 6.96; 95% CI = −5.99, 19.91; P = 0.29) [Fig. 9(c)].
Fig. 9.
(a) QOL at 8 weeks after intervention; (b) Mean changes of global health subdomain of EORTC QLQ-C30 from baseline to 12 weeks after intervention; (c) Mean changes of functional subdomain of EORTC QLQ-C30 from baseline to 12 weeks after intervention; (d) Mean changes of symptom subdomain of EORTC QLQ-C30 from baseline to 12 weeks after intervention.
Three studies36,40,50 reported the effects of yoga on the symptom subdomain of the EORTC QLQ-C30 12 weeks after the intervention. These studies showed high heterogeneity (P < 0.1, I2 = 93%). No significant differences were found between two of the groups (n = 87; MD = −3.36; 95% CI = −20.97, 14.25; P = 0.71) [Fig. 9(d)]. However, the sensitivity analysis suggested that the study by Naderi et al.40 had a large effect on the heterogeneity. No heterogeneity was observed when this study was removed (P = 0.91, I2 = 0%). The pooled analysis of the remaining studies suggested that yoga had advantages over the control intervention in reducing symptoms (n = 67; MD = 6.61; 95% CI = 1.37, 11.84; P = 0.01). The meta-analysis results were unstable, indicating the need for further studies.
Others
Finally, the results of seven studies21,45,46,49,52, 53, 54 could not be included in the meta-analysis because the analysis focused on particular outcomes for which the available number of studies was insufficient. Bao et al.21 found that the yoga group performed better in reducing neurotoxicity at 12 weeks of follow-up. Kothari et al.52 found that the yoga group reported less nausea and vomiting than did the control group 3 days after chemotherapy; this positive effect was also demonstrated by Jong et al.46 at 24 weeks of follow-up. Additionally, the yoga group demonstrated significant improvements in cancer-related symptoms,53 stress,54 yoga capital,45 and urinary function49 compared with the control group.
Discussion
This updated systematic review and meta-analysis included 34 recent RCTs to determine the effects of yoga on cancer survivors. Consistent with previous reports,13, 14, 15, 16 the findings of this study suggested that yoga improved physical function, mental health, and overall QOL. However, for physical function, there is still a lack of strong evidence on the benefits of yoga on exercise capacity. Further research is needed on this topic. For mental health, previous studies13,16 reported the effects of yoga on reducing anxiety and depression in the short term.
Consistent with most previous studies,13 this updated review showed a moderate-to-high impact of yoga on the overall QOL of cancer survivors in the short term. For cancer-related symptoms, the updated review found that the effects of yoga on pain and fatigue were not consistent, indicating the need for more exploratory studies. In addition, Cramer et al.5 reported that yoga reduced sleep disturbances in the short term, which was also confirmed in this review. Overall, the methodological quality of the studies showed a moderate-to-low risk of bias. Owing to the nature of the study interventions, it was difficult to achieve blinding of participants and interveners. Some included studies lacked clear descriptions of the procedures of randomization and allocation concealment,27,36,39,42,45 resulting in potential selection bias. Accordingly, further rigorous and high-quality RCTs are needed to confirm the effects of yoga on health-related outcomes of cancer survivors.
In traditional Chinese medicine, it is believed that the pathogenesis of cancer is closely linked to imbalances in the body, including pathogenic disorders and positive bodily states. When mood fluctuates, the liver controls the free flow of Qi; Qi stagnation leads to phlegm and blood stasis, eventually producing a congealed mass. Conversely, the spleen is the source of Qi and blood generation. When patients ruminate, their diet may become irregular, causing damage to the spleen; since Qi and blood are not easily generated, a deficiency of Qi and blood gradually results. The loss of healthy Qi results in the invasion of evil Qi, causing the onset of cancers.7, 8, 9, 10 Within this traditional framework, the significant reductions in symptoms of anxiety and depression and the improvements in mood achieved suggest that yoga enhances the generation of healthy Qi while dispelling evil Qi. In addition, yoga improves physical and mental health- and QOL-related outcomes, which may be attributed to neuroendocrine regulation. Yoga may also enhance the immune function of cancer survivors by interrupting the inflammatory process and reducing the activity of T-cells and NK cells.42,55
Limitations
While the effect sizes of yoga for the QOL were generally large, the effect sizes for most physical and mental health-related outcomes were relatively small among the studies included in this review. This finding may be attributed to the heterogeneity of cancer survivors. Future exploration of the moderators of yoga's physical and mental health benefits for cancer survivors should utilize large samples. In addition, some studies included in this updated systematic review and meta-analysis evaluated multiple health-related outcomes, which can potentially lead to underestimation of the benefits of yoga. Finally, this updated study included articles published in Chinese or English only, and given yoga's Indian roots, some important articles may have been excluded.
Implications for practice
Despite the abovementioned limitations, the findings of this updated systematic review and meta-analysis have the following important implications. Yoga benefits the physical and mental health-related outcomes and overall QOL of cancer survivors and could therefore be used as an optional supportive intervention for people with cancer. Since most participants in the included studies were current cancer survivors and short-term cancer survivors, future research should explore yoga's health benefits for long-term cancer survivors. Cognitive impairment is a crucial problem for cancer survivors.56 Future research should also examine the effects of yoga on the cognitive function of long-term survivors. Because most studies included in this updated study lacked allocation concealment with a short-term follow-up assessment of study outcomes, more rigorous RCTs are needed to assess the longer-term effects of yoga and enhance the health benefits for people with cancer.
Conclusions
This updated systematic review and meta-analysis offers available evidence on the effects of yoga on the physical function, mental health, and QOL of cancer survivors. Since most included studies employed relatively small sample sizes, more large-scale, multi-center, high-quality RCTs are needed to further verify yoga's health benefits for cancer survivors.
CRedit author statement
Niu Niu: Conceptualization, Formal analysis, Writing original draft. Ruirui Huang: Conceptualization, Formal analysis, Writing original draft. Junwen Zhao: Conceptualization, Methodology, Writing – Review & Editing. Yingchun Zeng: Conceptualization, Formal analysis, Writing – Review & Editing. All authors were granted complete access to all the data in the study, with the corresponding author bearing the final responsibility for the decision to submit for publication. The corresponding author affirms that all listed authors fulfill the authorship criteria and that no others meeting the criteria have been omitted.
Declaration of competing interest
The authors declare no conflict of interest. The corresponding author, Dr. Yingchun Zeng, is a member of the editorial board of the Asia-Pacific Journal of Oncology Nursing. The article underwent the journal's standard review procedures, with peer review conducted independently of Dr. Zeng and their research groups.
Funding
This study was funded by the National Natural Science Foundation of China (Grant No. 72004039) for Dr Zeng. The funder had no role in the conduct of the research. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Ethics statement
Not required.
Data availability statement
The data that support the findings of this review are available on request from the first author.
Declaration of Generative AI and AI-assisted technologies in the writing process
No AI tools/services were used during the preparation of this work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.apjon.2023.100316.
Contributor Information
Junwen Zhao, Email: 596830447@qq.com.
Yingchun Zeng, Email: chloezengyc@hotmail.co.uk.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Siegel R.L., Miller K.D., Wagle N.S., et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48. doi: 10.3322/caac.21763. [DOI] [PubMed] [Google Scholar]
- 2.Campbell K.L., Winters-Stone K.M., Wiskemann J., et al. Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc. 2019;51(11):2375–2390. doi: 10.1249/MSS.0000000000002116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han C.J., Yang G.S., Syrjala K. Symptom experiences in colorectal cancer survivors after cancer treatments: a systematic review and meta-analysis. Cancer Nurs. 2020;43(3):E132–E158. doi: 10.1097/NCC.0000000000000785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buffart L.M., van Uffelen J.G., Riphagen, et al. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2012;12:559. doi: 10.1186/1471-2407-12-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cramer H., Lauche R., Klose P., et al. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1(1):CD010802. doi: 10.1002/14651858.CD010802.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feuerstein G. Hohm Press; Prescott: 1998. The Yoga Tradition. [Google Scholar]
- 7.Carroll B.J., Iranmanesh A., Keenan D.M., et al. Pathophysiology of hypercortisolism in depression: pituitary and adrenal responses to low glucocorticoid feedback. Acta Psychiatr Scand. 2012;125(6):478–491. doi: 10.1111/j.1600-0447.2011.01821.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Streeter C.C., Gerbarg P.L., Saper R.B., et al. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78(5):571–579. doi: 10.1016/j.mehy.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Gosain R., Gage-Bouchard E., Ambrosone C., et al. Stress reduction strategies in breast cancer: review of pharmacologic and non-pharmacologic based strategies. Semin Immunopathol. 2020;42(6):719–734. doi: 10.1007/s00281-020-00815-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eda N., Ito H., Akama T. Beneficial Effects of yoga stretching on salivary stress hormones and parasympathetic nerve activity. J Sports Sci Med. 2020;19(4):695–702. [PMC free article] [PubMed] [Google Scholar]
- 11.Gothe N.P., Erlenbach E. Feasibility of a yoga, aerobic and stretching-toning exercise program for adult cancer survivors: the STAYFit trial. J Cancer Surviv. 2022;16(5):1107–1116. doi: 10.1007/s11764-021-01101-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nejat N., Rahbarian A., Mehrabi F., et al. Complementary and alternative medicine application in cancer patients in Iran. J Cancer Res Clin Oncol. 2023;149(6):2271–2277. doi: 10.1007/s00432-022-04317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casuso-Holgado M.J., Heredia-Rizo A.M., Gonzalez-Garcia P., et al. Mind-body practices for cancer-related symptoms management: an overview of systematic reviews including one hundred twenty-nine meta-analyses. Support Care Cancer. 2022;30(12):10335–10357. doi: 10.1007/s00520-022-07426-3. [DOI] [PubMed] [Google Scholar]
- 14.Selvan P., Hriso C., Mitchell J., et al. Systematic review of yoga for symptom management during conventional treatment of breast cancer patients. Compl Ther Clin Pract. 2022;48 doi: 10.1016/j.ctcp.2022.101581. [DOI] [PubMed] [Google Scholar]
- 15.Song J., Wang T., Wang Y., et al. The Effectiveness of yoga on cancer-related fatigue: a systematic review and meta-Analysis. Oncol Nurs Forum. 2021;48(2):207–228. doi: 10.1188/21.ONF.207-228. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez M., Pascoe M.C., Yang G., et al. Yoga for depression and anxiety symptoms in people with cancer: a systematic review and meta-analysis. Psycho Oncol. 2021;30(8):1196–1208. doi: 10.1002/pon.5671. [DOI] [PubMed] [Google Scholar]
- 17.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88 doi: 10.1136/bmj.n71. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J.P.T., Altman D.G., Gotzsche P.C., et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party . The Joanna Briggs Institute; 2014. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation.https://joannabriggs.org/sites/default/files/2019-05/JBI%20Levels%20of%20Evidence%20Supporting%20Documents-v2.pdf; 2014. [Google Scholar]
- 20.Higgins J.P.T., Thomas J., Chandler J., et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. John Wiley & Sons; Chichester, UK: 2019. [Google Scholar]
- 21.Bao T., Zhi I., Baser R., et al. Yoga for chemotherapy-induced peripheral neuropathy and fall risk: a randomized controlled trial. JNCI Cancer Spectr. 2020;4:a48. doi: 10.1093/jncics/pkaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huberty J., Eckert R., Dueck A., et al. Online yoga in myeloproliferative neoplasm patients: results of a randomized pilot trial to inform future research. BMC Compl Alternative Med. 2019;19:1–12. doi: 10.1186/s12906-019-2530-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Porter L.S., Carson J.W., Olsen M., et al. Feasibility of a mindful yoga program for women with metastatic breast cancer: results of a randomized pilot study. Support Care Cancer. 2019;27:4307–4316. doi: 10.1007/s00520-019-04710-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang P.P., Chen L.M., Huang L.H. A study on the impact of yoga voice meditation on pain treatment in patients with advanced malignant tumors. Nurs Rehabil. 2020;19:52–55. doi: 10.3969/j.issn.1671-9875.2020.12.014. [In Chinese)] [DOI] [Google Scholar]
- 25.Carsn J.W., Carson K.M., Olsen M., et al. Yoga practice predicts improvements in day-to-day pain in women with metastatic breast cancer. J Pain Symptom Manag. 2021;61:1227–1233. doi: 10.1016/j.jpainsymman.2020.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin P.J., Kleckner I.R., Loh K.P., et al. Influence of yoga on cancer-related fatigue and on mediational relationships between changes in sleep and cancer-related fatigue: a nationwide, multicenter randomized controlled trial of yoga in cancer survivors. Integr Cancer Ther. 2019;18:1–11. doi: 10.1177/1534735419855134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhi W.I., Baser R.E., Zhi L.M., et al. Yoga for cancer survivors with chemotherapy-induced peripheral neuropathy: health-related quality of life outcomes. Cancer Med. 2021;10:5456–5465. doi: 10.1002/cam4.4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knoerl R., Giobbie-Hurder A., Berfield J., et al. Yoga for chronic chemotherapy-induced peripheral neuropathy pain: a pilot, randomized controlled trial. J Cancer Surviv. 2022;16:882–891. doi: 10.1007/s11764-021-01081-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sohl S.J., Tooze J.A., Johnson E.N., et al. A randomized controlled pilot study of yoga skills training versus an attention control delivered during chemotherapy administration. J Pain Symptom Manag. 2022;63:23–32. doi: 10.1016/j.jpainsymman.2021.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor T.R., Barrow J., Makambi K., et al. A restorative yoga intervention for African-American breast cancer survivors: a pilot study. J Racial Ethn Health Disparities. 2018;5:62–72. doi: 10.1007/s40615-017-0342-4. [DOI] [PubMed] [Google Scholar]
- 31.Chaoul A., Milbury K., Spelman A., et al. Randomized trial of Tibetan yoga in patients with breast cancer undergoing chemotherapy. Cancer. 2018;124:36–45. doi: 10.1002/cncr.30938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winters-Stone K.M., Moe E.L., Perry C.K., et al. Enhancing an oncologist's recommendation to exercise to manage fatigue levels in breast cancer patients: a randomized controlled trial. Support Care Cancer. 2018;26:905–912. doi: 10.1007/s00520-017-3909-z. [DOI] [PubMed] [Google Scholar]
- 33.Hardoerfer K., Jentschke E. Effect of yoga therapy on symptoms of anxiety in cancer patients. Oncol Res Treat. 2018;41:526–532. doi: 10.1159/000488989. [DOI] [PubMed] [Google Scholar]
- 34.Liu W., Liu J., Ma L., et al. Effect of mindfulness yoga on anxiety and depression in early breast cancer patients received adjuvant chemotherapy: a randomized clinical trial. J Cancer Res Clin Oncol. 2022;148:2549–2560. doi: 10.1007/s00432-022-04167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zetzl T., Renner A., Pittig A., et al. Yoga effectively reduces fatigue and symptoms of depression in patients with different types of cancer. Support Care Cancer. 2021;29:2973–2982. doi: 10.1007/s00520-020-05794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eyigor S., Uslu R., Apaydın S., et al. Can yoga have any effect on shoulder and arm pain and quality of life in patients with breast cancer? a randomized, controlled, single-blind trial. Compl Ther Clin Pract. 2018;32:40–45. doi: 10.1016/j.ctcp.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 37.Milbury K., Liao Z., Shannon V., et al. Dyadic yoga program for patients undergoing thoracic radiotherapy and their family caregivers: results of a pilot randomized controlled trial. Psycho Oncol. 2019;28:615–621. doi: 10.1002/pon.4991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barassi G., Bellomo R.G., Di Iulio A., et al. Preoperative rehabilitation in lung cancer patients: yoga approach. Adv Exp Med Biol. 2018;1096:19–29. doi: 10.1007/5584_2018_186. [DOI] [PubMed] [Google Scholar]
- 39.Li Y.D., Li Y.M., Zeng F.Y., et al. A study on the application of yoga breathing exercise in lung rehabilitation of postoperative lung cancer patients. Nurs Interg Tradit Chin Western Med. 2020;6:265–269. [In Chinese)] [Google Scholar]
- 40.Naderi M., Kordestani H., Sahebi Z., et al. Serum and gene expression profile of cytokines following combination of yoga training and vitamin D supplementation in breast cancer survivors: a randomized controlled trial. BMC Wom Health. 2022;22:90. doi: 10.1186/s12905-022-01671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khedmati Z.V., Javadi M., Amani-Shalamzari S., et al. The high dose of vitamin D supplementation combined with yoga training improve the leukocytes cell survival-related gene expression in breast cancer survivors. Nutr Metab. 2021;18:80. doi: 10.1186/s12986-021-00607-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jain M., Mishra A., Yadav V., et al. Long-term yogic intervention improves symptomatic scale and quality of life by reducing inflammatory cytokines and oxidative stress in breast cancer patients undergoing chemotherapy and/or radiotherapy: a randomized control study. Cureus. 2023;15 doi: 10.7759/cureus.33427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greaney S.K., Amin N., Prudner B.C., et al. Yoga therapy during chemotherapy for early-stage and locally advanced breast Cancer. Integr Cancer Ther. 2022;21:1–12. doi: 10.1177/15347354221137285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaushik D., Shah P.K., Mukherjee N., et al. Effects of yoga in men with prostate cancer on quality of life and immune response: a pilot randomized controlled trial. Prostate Cancer Prostatic Dis. 2022;25:531–538. doi: 10.1038/s41391-021-00470-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang L.Y., Li Q.F., Xu R., et al. Effect of laughter yoga on stress perception in patients undergoing chemotherapy for non-small cell lung cancer. J Nurs Sci. 2023;38:94–99. doi: 10.3870/j.issn.1001-4152.2023.03.094. [In Chinese)] [DOI] [Google Scholar]
- 46.Jong M.C., Boers I., Schouten V.D.V.A., et al. A randomized study of yoga for fatigue and quality of life in women with breast cancer undergoing (Neo) adjuvant chemotherapy. J Alternative Compl Med. 2018;24:942–953. doi: 10.1089/acm.2018.0191. [DOI] [PubMed] [Google Scholar]
- 47.Lu H.B., Ma R.C., Yin Y.Y., et al. Clinical indicators of effects of yoga breathing exercises on patients with lung cancer after surgical resection: a randomized controlled trial. Cancer Nurs. 2023 doi: 10.1097/NCC.0000000000001208. [DOI] [PubMed] [Google Scholar]
- 48.Chen P.J., Lin J.F., Yang M. Effect of yoga on quality of life, cancer-related fatigue and sleep quality of cancer patients undergoing chemotherapy. Chin Evid-based Nurs. 2021;7:423–426. doi: 10.12102/j.issn.2095-8668.2021.03.031. [In Chinese)] [DOI] [Google Scholar]
- 49.Xing J. Effect of pelvic floor muscle Yoga training combined with clean intermittent catheterization on bladder function in patients after radical cervical cancer surgery. Reflex Therapy Rehabil Med. 2022;3:91–94. [In Chinese)] [Google Scholar]
- 50.Eyigör S., Apaydin S., Yesil H., et al. Effects of yoga on phase angle and quality of life in patients with breast cancer: a randomized, single-blind, controlled trial. Complement Med Res. 2021;28:523–532. doi: 10.1159/000515494. [DOI] [PubMed] [Google Scholar]
- 51.Prakash K., Saini S.K., Pugazhendi S. Effectiveness of yoga on quality of life of breast cancer patients undergoing chemotherapy: a randomized clinical controlled study. Indian J Palliat Care. 2020;26:323–331. doi: 10.4103/IJPC.IJPC_192_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kothari T.O., Jakhar S.L., Bothra D., et al. Prospective randomized trial of standard antiemetic therapy with yoga versus standard antiemetic therapy alone for highly emetogenic chemotherapy-induced nausea and vomiting in South Asian population. J Cancer Res Therapeut. 2019;15:1120–1123. doi: 10.4103/jcrt.JCRT_860_16. [DOI] [PubMed] [Google Scholar]
- 53.Milbury K., Li J., Weathers S.P., et al. Pilot randomized, controlled trial of a dyadic yoga program for glioma patients undergoing radiotherapy and their family caregivers. Neurooncol Pract. 2019;6:311–320. doi: 10.1093/nop/npy052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.D'Cunha R., B P., D'Souza O.L., et al. Effectiveness of yoga nidra in mitigating stress in women undergoing curative radiotherapy for cervical cancer. Mid East J Cancer. 2021;12:117–127. doi: 10.30476/mejc.2020.82648.1093. [DOI] [Google Scholar]
- 55.Rao R.M., Vadiraja H.S., Nagaratna R., et al. Effect of yoga on sleep quality and neuroendocrine immune response in metastatic breast cancer patients. Indian J Palliat Care. 2017;23(3):253–260. doi: 10.4103/IJPC.IJPC_102_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wefel J.S., Kesler S.R., Noll K.R., et al. Clinical characteristics, pathophysiology, and management of noncentral nervous system cancer-related cognitive impairment in adults. CA Cancer J Clin. 2015;65(2):123–138. doi: 10.3322/caac.21258. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this review are available on request from the first author.