Abstract
Haemophagocytic lymphohistiocytosis secondary to Histoplasma infection is rare and almost always occurs in immunocompromised hosts. We report a 32-year-old immunocompetent man presenting with a nonspecific febrile illness found to have disseminated histoplasmosis and associated haemophagocytic lymphohistiocytosis. The diagnosis was confirmed on histopathological examination and PCR of liver and bone marrow biopsies. He was successfully treated with steroids, intravenous immunoglobulin and itraconazole.
Keywords: Haemophagocytosis, Histoplasma capsulatum, Disseminated histoplasmosis
1. Introduction
Haemophagocytic lymphohistiocytosis (HLH) is a rare syndrome where immune dysregulation results in systemic inflammation and end organ damage [1]. Most cases occur in children with an underlying genetic defect. In adults, HLH is commonly instigated by an illness such as infection, malignancy or autoimmune disease [2]. Histoplasmosis is an infection caused by Histoplasma capsulatum, a thermally dimorphic fungus found in soil as well as bat and bird droppings [3]. Histoplasmosis is a rare cause of HLH, mostly seen in people living with HIV [4]. We report a case of HLH secondary to disseminated histoplasmosis in an immunocompetent man successfully treated with steroids, intravenous immunoglobulin (IVIG) and itraconazole.
2. Case presentation
A 32-year-old immunocompetent male presented to hospital (day 0) with a 3-week history of fever, myalgia and non-productive cough. There was associated anorexia and 9 kg of weight loss. He had no significant past medical history or regular medications. He was born in Indonesia and migrated to Australia 18 months prior. He had returned from a trip to Indonesia 3 weeks earlier, having stayed on a rural property that kept chickens though he had no direct contact with them or other animals.
On examination, his temperature was 39 °C, blood pressure 112/85 mmHg and pulse 86 beats per minute. There was hepatosplenomegaly but no lymphadenopathy or rash and the chest was clear to auscultation. Initial investigations showed white cell count of 2.4 x109/L, haemoglobin of 91 g/L (microcytic, hypochromic) and platelets of 55 x109/L. Alkaline phosphatase was 182 U/L, gamma-glutamyl transferase 260 U/L, alanine transaminase 97 U/L, aspartate transaminase 96 U/L with a total bilirubin of 16 μmol/L. Ferritin was 2661 g/L and triglycerides were 2.5 mmol/L. Blood, urine and stool cultures were negative. Testing for hepatitis A, B, C and HIV were negative. Empirical antibiotic therapy (ampicillin, gentamicin and metronidazole) was commenced on day 0 and then ceased on day +1.
Computed tomography of the chest and abdomen showed multifocal consolidation of the lungs and hepatosplenomegaly. Positron emission tomography demonstrated increased uptake in the bone marrow, spleen and paracaval and aortocaval lymph nodes. Bone marrow biopsy demonstrated mildly hypercellular marrow with increased megakaryopoiesis without haemophagocytosis. Methenamine silver staining revealed intracellular yeast suggestive of H.capsulatum, however no fungi were isolated from culture of bone marrow and panfungal polymerase chain reaction (PCR) was unsuccessful.
The patient deteriorated with ongoing fever and progressive pancytopaenia (total white cell count of 1.5 x109/L, haemoglobin of 87 g/L and platelets of 60 x109/L). Prednisolone 50 mg daily was commenced on day 10 as the differential diagnoses were vasculitis or HLH. Natural killer (NK) cell degranulation function was reduced. Bronchoalveolar lavage was performed, cultures for bacteria, fungi and mycobacteria were negative.
The immunology and clinical genetics teams were consulted to investigate for underlying immunodeficiency. Immunoglobulins, lymphocyte subsets and anti-interferon gamma antibodies were unremarkable.
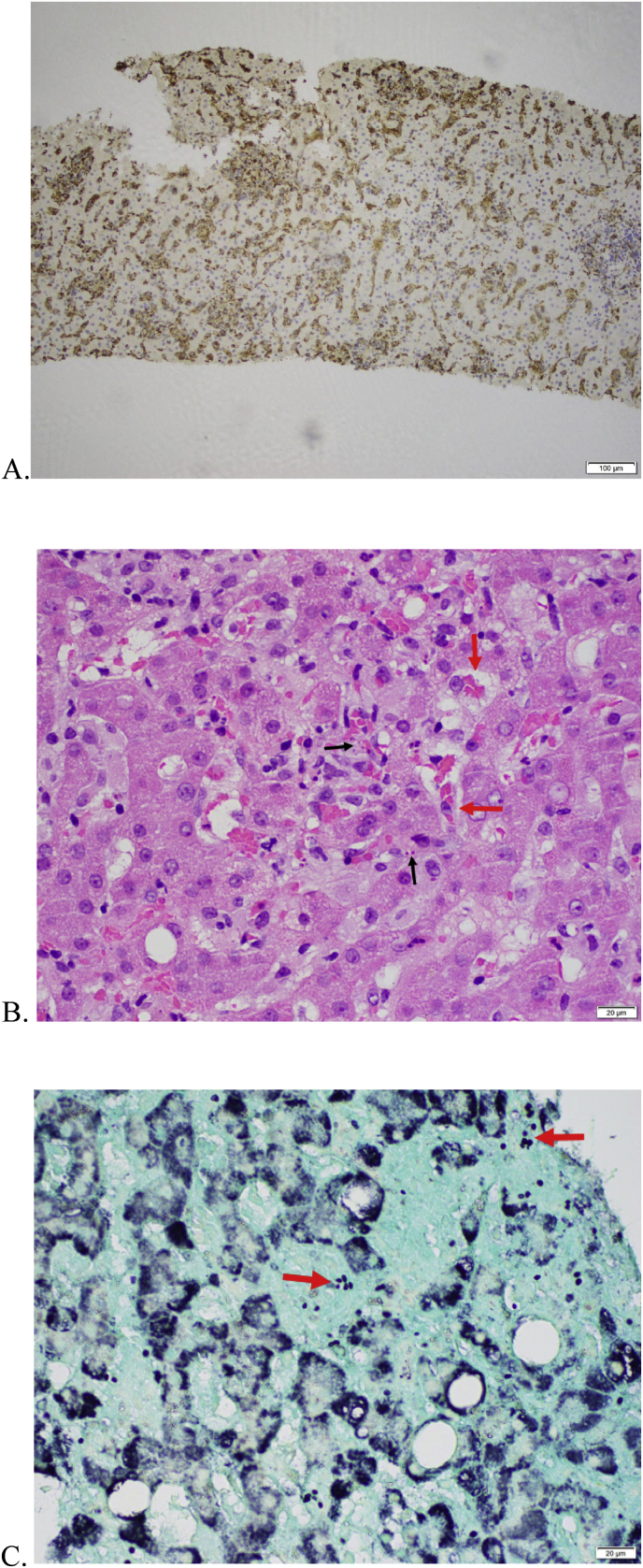
Liver biopsy demonstrated sinusoidal infiltration by histiocytes with evidence of haemophagocytosis. Silver staining again showed numerous fungi (Fig. 1). Another bone marrow aspirate was performed and H.capsulatum DNA was detected by PCR despite negative culture. H.capsulatum serology was also positive. The patient was treated with SUBA-itraconazole 200mg twice a day, IVIG 1g/kg/day for 2 days and prednisolone. His fevers resolved by day 7 of itraconazole and by 3 weeks he was asymptomatic. He was discharged on day +28 on the itraconazole and prednisolone which was able to be weaned over the next month. After 3 months of follow up he had remained well and decided to return to Indonesia with the plan to complete 12 months of itraconazole therapy.
Fig. 1.
Histopathology of the liver biopsy. (A) CD68 immunohistochemistry highlighting prominent sinusoidal infiltrate of histiocytes in the liver, 100x. (B) Haematoxylin and eosin stain showing histiocytes in liver sinusoids and haemophagocytosis (red arrows) and small round bodies suspicious for fungi (black arrows), 400x. (C) Methenamine silver stain showing fungi consistent with Histoplasma spp.(arrows), 400x. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
Our case is unusual for the development of HLH secondary to disseminated histoplasmosis in an immunocompetent patient without known risk factors and successful treatment with itraconazole without amphotericin induction.
Histoplasmosis primarily develops after inhalation of H.capsulatum spores which are then engulfed by pulmonary macrophages and multiply. In healthy individuals, cell mediated immunity develops and macrophages are activated to kill the fungus. The majority of pulmonary infections are asymptomatic [5]. Haematogenous spread of H.capsulatum results in disseminated infection, commonly affecting the spleen, liver, bone marrow and lymph nodes [3]. Patients with impaired cell mediated immunity, particularly people living with HIV and a CD4 count <200/μL, are at increased risk of disseminated histoplasmosis [5]. Other immunocompromised states including corticosteroid use and solid organ transplant are also risk factors.
Disseminated histoplasmosis in immunocompetent hosts is uncommon and usually associated with exposure to a large inoculum [3]. Cave exploration and outdoor activities have been reported as risk factors for disseminated infection in immunocompetent travellers [6]. We were unable to identify any immunocompromise or high risk exposures in our patient although he likely acquired the infection during his trip to Indonesia where seroprevalence is high [7].
HLH in adults is usually secondary to another condition, most commonly haematological malignancies and viral infections [1,2]. Histoplasmosis is the most common fungal infection associated with HLH [2], primarily occurring in patients with HIV, but has been reported with solid organ transplantation, haematological malignancy and other immunosuppressed states [4,8]. Histoplasmosis causing HLH is rare in immunocompetent patients with only 11 other cases published [[9], [10], [11], [12], [13], [14], [15], [16], [17], [18]].
HLH is difficult to recognise due to the non-specific presentation, including fevers, lymphadenopathy and hepatosplenomegaly, often overlapping with histoplasmosis [8]. Diagnostic criteria from the HLH-2004 trial are used although not validated in adults (Table 1) [19]. If left untreated, HLH can rapidly progress to multi-organ failure [2]. Early initiation of treatment should be considered for unwell patients in whom there is a reasonable degree of suspicion.
Table 1.
HLH-2004 diagnostic criteria.
|
A molecular diagnosis consistent with HLH OR At least five of the following Fever Splenomegaly Peripheral blood cytopenias (affecting at least 2 of the 3 cell lineages)
Haemophagocytosis in bone marrow, spleen or lymph nodes Low or absent NK cell activity Ferritin >500mg/L Soluble CD25 > 2400U/ml |
High-quality evidence to guide treatment decisions in adults with HLH is lacking. Treatment of the underlying cause of secondary HLH is important to remove the trigger for ongoing immune activation [2]. In some cases this alone may be sufficient to control HLH. The HLH-2004 treatment protocol is widely used and includes corticosteroids, etoposide and ciclosporin, aiming to treat the abnormal immune response [19]. Other treatments, such as IVIG, are sometimes added. While these protocols have increased survival in paediatric populations, their efficacy in adults, especially those with secondary HLH is less clear due to the heterogeneous nature of the adult HLH population.
Treatment of histoplasmosis depends on severity of infection. Guidelines from the Infectious Disease Society of America recommend at least 12 months treatment in disseminated histoplasmosis depending on the patient's immune status [20]. For mild to moderate disease, therapy with itraconazole is recommended while for moderately severe to severe disease, they recommend liposomal amphotericin B for 1–2 weeks before transitioning to itraconazole. Our patient was treated with itraconazole alone without preceding amphotericin as his presentation was thought to be primarily due to HLH rather than severe histoplasmosis. In a review of 65 cases of histoplasmosis-associated HLH, 23 received some HLH specific treatment [8]. 48 were given amphotericin as initial antifungal therapy and 5 others received an azole alone, of whom only one was treated with itraconazole.
The prognosis of HLH in adults is poor with a reported mortality rate of 41% [2]. HLH secondary to malignancy or unknown cause is associated with worse outcomes. Mortality in histoplasmosis-associated HLH has been reported as 31% overall and 37% in patients with HIV [8]. Although only small numbers, mortality in immunocompetent patients appears low with all but one having survived [9].
This case highlights that HLH secondary to disseminated histoplasmosis should be considered in patients with prolonged febrile illness, hepatosplenomegaly and abnormal liver tests, even in immunocompetent patients. Prompt diagnosis and initiation of treatment is important to prevent mortality. Treatment of the underlying infection is important and does not necessarily require initial amphotericin. The optimal treatment of secondary HLH is uncertain and requires further research.
Ethical form
This was an unfunded study. The authors have obtained written and signed consent to publish the case report from the patient.
CRediT author statement
Mallory Morton: Writing- Original Draft.
Vinay Vanguru: Writing- Review and Editing.
Joo-Shik Shin: Writing- Review and Editing.
Amrita Ronnachit: Writing- Review and Editing.
Declaration of competing interest
There are none.
Handling Editor: Dr Adilia Warris
References
- 1.Allen C.E., McClain K.L. Pathophysiology and epidemiology of hemophagocytic lymphohistiocytosis. Hematology. 2015 Dec 5;2015(1):177–182. doi: 10.1182/asheducation-2015.1.177. [DOI] [PubMed] [Google Scholar]
- 2.Ramos-Casals M., Brito-Zerón P., López-Guillermo A., Khamashta M.A., Bosch X. Adult haemophagocytic syndrome. Lancet. 2014 Apr;383(9927):1503–1516. doi: 10.1016/S0140-6736(13)61048-X. [DOI] [PubMed] [Google Scholar]
- 3.Wheat L.J., Azar M.M., Bahr N.C., Spec A., Relich R.F., Hage C. Histoplasmosis. Infect. Dis. Clin. 2016 Mar;30(1):207–227. doi: 10.1016/j.idc.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Townsend J.L., Shanbhag S., Hancock J., Bowman K., Nijhawan A.E. Histoplasmosis-induced hemophagocytic syndrome: a case series and review of the literature. Open Forum Infect. Dis. 2015 Apr 1;2(2):ofv055. doi: 10.1093/ofid/ofv055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mittal J., Ponce M.G., Gendlina I., Nosanchuk J.D. In: Fungal Physiology and Immunopathogenesis [Internet] Rodrigues M.L., editor. Springer International Publishing; Cham: 2018. Histoplasma capsulatum: mechanisms for pathogenesis; pp. 157–191.http://link.springer.com/10.1007/82_2018_114 [cited 2022 Aug 2] [Google Scholar]
- 6.Staffolani S., Buonfrate D., Angheben A., Gobbi F., Giorli G., Guerriero M., et al. Acute histoplasmosis in immunocompetent travelers: a systematic review of literature. BMC Infect. Dis. 2018 Dec;18(1):673. doi: 10.1186/s12879-018-3476-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker J., Setianingrum F., Wahyuningsih R., Denning D.W. Mapping histoplasmosis in south east asia – implications for diagnosis in AIDS. Emerg. Microb. Infect. 2019 Jan 1;8(1):1139–1145. doi: 10.1080/22221751.2019.1644539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jabr R., El Atrouni W., Male H.J., Hammoud K.A. Histoplasmosis-associated hemophagocytic lymphohistiocytosis: a review of the literature. Can. J. Infect Dis. Med. Microbiol. 2019;2019:1–8. doi: 10.1155/2019/7107326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bohra T.S., Shaikh H., Prabhudesai P. Fungal infection causing a diagnostic dilemma. Asian J Med Case Rep. 2021;3(1):13–18. [Google Scholar]
- 10.Chen H., Yuan Q., Hu H., Wang J., Yu M., Yang Q., et al. Hemophagocytic lymphohistiocytosis secondary to disseminated histoplasmosis in HIV seronegative patients: a case report and review of the literature. Front. Cell. Infect. Microbiol. 2022 Jun 16;12 doi: 10.3389/fcimb.2022.847950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De D., Nath U.K. Disseminated histoplasmosis in immunocompetent individuals- not a SO rare entity. Mediterr J Hematol Infect Dis. 2015 Apr 19;7 doi: 10.4084/MJHID.2015.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dousa K.M., De la Hoz A., Church E., Onger T., Perez F., Saade E. Progressive and disseminated histoplasma infection and hemophagocytic lymphohistiocytosis in an immunocompetent adult. Clin Case Rep. 2019 May;7(5):913–916. doi: 10.1002/ccr3.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferguson-Paul K., Mangum S., Porter A., Leventaki V., Campbell P., Wolf J. Hemophagocytic lymphohistiocytosis and progressive disseminated histoplasmosis. Emerg. Infect. Dis. 2016 Jun;22(6):1119–1121. doi: 10.3201/eid2206.151682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta N., Vinod K.S., Mittal A., Ajay Kumar A.P., Kumar A., Wig N. Histoplasmosis, heart failure, hemolysis and haemophagocytic lymphohistiocytosis. Pan Afr Med J [Internet] 2019;32 doi: 10.11604/pamj.2019.32.43.14954. http://www.panafrican-med-journal.com/content/article/32/43/full/ [cited 2022 May 8]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saluja S., null Sunita, Bhasin S., Gupta D.K., Gupta B., Kataria S.P. Disseminated histoplasmosis with reactive haemophagocytosis presenting as PUO in an immunocompetent host. J. Assoc. Phys. India. 2005 Oct;53:906–907. [PubMed] [Google Scholar]
- 16.Sonavane A.D.. Disseminated Histoplasmosis with Haemophagocytic Lymphohistiocytosis in an Immunocompetent Host. J Clin Diagn Res. 2016;10(13):OD03–05. doi: 10.7860/JCDR/2016/15839.7337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song D., Wang J., Wang Z. Hemophagocytic lymphohistiocytosis secondary to disseminated histoplasmosis in an immunocompetent patient. Infect Dis Now. 2021 May;51(3):308–309. doi: 10.1016/j.medmal.2020.09.019. [DOI] [PubMed] [Google Scholar]
- 18.Xiong X feng, li Fan L., Kang M., Wei J., Cheng D yun. Disseminated histoplasmosis: a rare clinical phenotype with difficult diagnosis: disseminated histoplasmosis in China. Respirol Case Rep. 2017 May;5(3) doi: 10.1002/rcr2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henter J.I., Horne A., Aricó M., Egeler R.M., Filipovich A.H., Imashuku S., et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr. Blood Cancer. 2007 Feb;48(2):124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 20.Wheat L.J., Freifeld A.G., Kleiman M.B., Baddley J.W., McKinsey D.S., Loyd J.E., et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the infectious diseases society of America. Clin. Infect. Dis. 2007 Oct 1;45(7):807–825. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]