Abstract
Objective: Patient-centered information management may overcome barriers that impede high-quality, safe care in the emergency department (ED). The utility of parents' report of medication data via a multimedia, touch screen interface, the asthma kiosk, was investigated. Our specific aims were (1) to estimate the validity of parents' electronically entered medication history for asthma and (2) to compare the parents' kiosk entries regarding medications to the documentation of ED physicians and nurses.
Methods: We enrolled a cohort of parents to use the asthma kiosk and tested the validity of this communication channel for medication data specific to pediatric asthma. Parents' data provided via the kiosk during the ED encounter and the documentation of ED nurses and physicians were compared with a telephone-based interview with the parent after discharge that reviewed all asthma-specific medications physically present in the home. Treating clinicians in the ED were blinded to the parents' kiosk entries.
Results: Sixty-six parents were enrolled and 49 of 66 (74.2%) completed the gold standard interview. When analyzed at the level of individual medications, the validity of parental report was 81% for medication name, 79% for route of delivery, 66% for the form of the medication, and 60% for dose. Parents' report improved on the validity of documentation by physicians across all medication details save for medication name. Parents' report was more valid than nursing documentation at triage for all medication details.
Conclusion: Parents can provide an independent source of medication data that improves on current documentation for key variables that impact quality and safety in emergency asthma care.
Complete and accurate knowledge of a patient's history is essential to safe and effective health care delivery. Information systems such as computerized provider order entry, which improve the quality of delivered care, depend on the electronic availability of valid data in key domains such as medication history and allergy history. Initial capture of data elements in these domains must occur through human effort at discovery and documentation. No evidence-based consensus exists for how best to populate critical domains of knowledge and validate the capture of patient-specific data at the point of entry for a patient in a health care environment.
The emergency department (ED) represents an archetype of a health care setting at risk of gaps in quality and safety as defined by the Committee on Data Standards of the Institute of Medicine: multiple providers involved in the care of individual patients, high acuity, a setting prone to distractions from noise and crowding, need for rapid decision-making, and communication barriers.1,2 The ED functions as an important safety net and site of care for large numbers of patients.2 In particular, ED visits for patients with asthma are considered a sentinel event and an opportunity for intervention to improve disease management.3 National guidelines for pediatric asthma require that a patient's symptoms and current medication regimen be evaluated to establish whether optimal chronic control has been achieved.4 Previous research in ED-based pediatric asthma care demonstrates important gaps in quality of history taking.5
A novel patient-centered technology, the asthma kiosk, was recently developed for parents' use in the pediatric ED to provide relevant data concerning childhood asthma.6 This multimedia, touch screen kiosk provides an electronic method to capture parents' knowledge regarding their child's asthma symptoms, current medications, and home care needs and environmental risks. Patient-centered information management holds the promise of addressing several ED-centric barriers that impede high-quality, safe care.7,8
The utility of this novel, parent-driven communication channel in providing valid medication data is the subject of this report. Our major aims were (1) to estimate the validity of parents' electronically entered medication history for asthma and (2) to compare the parents' kiosk entries regarding medications with the documentation of ED physicians and nurses.
Materials and Methods
We enrolled a cohort of parents to test the validity of a novel technology, the asthma kiosk, for the electronic capture of medication data specific to pediatric asthma. The pediatric ED of Children's Hospital Boston, an urban tertiary care setting, served as the study site. The research protocol was approved by the Committee on Clinical Investigation (Protocol # 02-05-056).
Selection of Participants
Parents and/or adult guardians of children between the ages of 1 and 12 years who had a chief complaint related to the respiratory system were identified on presentation to the ED. Eligibility criteria for the parent-child dyad included (1) a history of asthma for the child, (2) verbal report of child taking at least one medication for asthma, (3) primary language of English or Spanish. Parent-child dyad were considered ineligible if the above conditions were not met or if the child's triage status was emergent.
Parents were approached and screened by a bilingual research assistant after the completion of nursing triage in one of several areas of the ED: the waiting room, the triage area, or a treatment room.
Protocol for Enrolled Parents in the ED
Enrolled parents completed a stepwise protocol. All aspects of the protocol were completed while the parent and child were in the ED with the exception of the gold standard assessment of current medications as detailed below.
Parents independently entered information about their child using the asthma kiosk (▶). The mean time to completion was 11.4 minutes. The asthma kiosk is a multimedia, bilingual, touch screen interface designed to capture asthma-related history from parents of children with asthma.6 The module on current medications leads parents through a detailed report of asthma-specific medications including name, route of delivery, form of medication, dose, and frequency of use. A summary screen gives the parent an opportunity to review the information entered for a specific medication and to endorse it as correct before entering data on the next medication. Screen shots of the interface are available as an online data supplement at www.jamia.org. Parents' data from the kiosk were not shared with physicians and nurses providing care for children whose parents enrolled in the study.
Figure 1.

Mobile kiosk.
After use of the kiosk, parents completed a paper-based survey that elicited demographic information, previous experience with technology, and self-efficacy for asthma care. Study subjects completed the paper-based survey in the language that they used while interacting with the kiosk. Parents were given a $10 coupon for use at a nearby food establishment as compensation for their time and effort.
Gold Standard Assessment of Medication History
A bilingual research assistant blinded to parents' kiosk entries completed a structured telephone interview with parents after the ED visit where enrollment occurred. This interview was conducted with the parent who used the asthma kiosk. To ensure that the gold standard included current medications physically present at home, parents were asked to gather all asthma medicines in the house that they used for the child in question and have the medications in hand during the interview.9 To ensure that the parent reviewed medications in use as of the ED visit in question, the parent was told “I would like to talk about just the medicines that (child_name) was taking at the time of the emergency room visit.” Asthma medications prescribed at the time of the ED visit or prescribed in the days subsequent to the ED visit were considered not to be part of the child's current medication list at the time of the ED visit and were excluded from analysis.
For each medication, the parent was asked to report the name, route of use, form (concentration), dose, and frequency as recorded on the label supplied by the pharmacy. Additional data recorded included manufacturer, physical appearance of the medication, and parents' report of any dose of medication and/or frequency of use that varied from that written on the prescription label.
Classes of chronic medications that were considered “asthma specific” by the gold standard assessment included β2 agonists, corticosteroids (oral and inhaled), leukotriene inhibitors, and mast cell stabilizers. The telephone interviewer attempted to contact parents beginning on day 3 after the ED visit, making repeated calls until successful or until 7 days had passed after the date of enrollment.
Triage Nurse and Physician Documentation in the Emergency Department
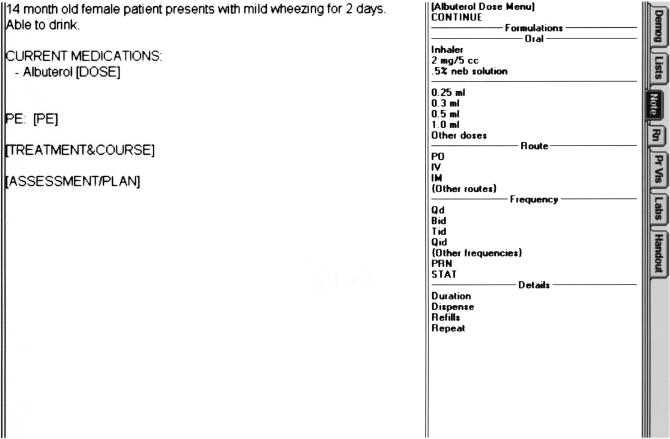
Triage nurses in the ED of the study site currently document asthma-specific medications on a paper form whose format prompts a detailed record (▶). ED physicians chart using a template-based EMR system (EM Station, VitalWorks, Ridgefield, CT) (▶). Physicians can choose to follow the template to record medications for a patient or type in free text.
Figure 2.
Asthma template used by triage nurse to document medication history.
Figure 3.
Example of medication template used by emergency department physician.
Medical Record Abstraction
A trained reviewer blinded to gold standard data and parents' kiosk responses surveyed nursing and physician ED records for documentation of medications used to treat the child at home. Using a structured form, the abstractor noted all attributes of medications that were documented in the medical record. Medications given by the primary care doctor or by EMS providers to stabilize the child's acute condition before arrival in the ED were not considered to represent current or “at home” medications for the purposes of this study. Ten percent of the records were re-abstracted by a second reviewer to confirm the accuracy of the data abstraction.
Outcome Measures
The primary outcome for this project was the point estimate of valid report of asthma-specific medications from three sources (parent, physician, and nurse). The unit of analysis was considered to be an individual medication. Report of a specific medication was considered valid if it matched details of that medication as determined by the gold standard interview (GSI). This definition of validity encompassed both the accuracy and completeness of a given attribute of a medication. Although theoretically correlated to the report of the medication name, subattributes of medication (route of delivery, form, and dose) were considered as distinct elements during primary analysis.
Primary Data Analysis
Point estimates were reported as proportions and as percentages with 95% confidence intervals (CIs). We compared the validity for different reporters (parent, nurse, and physician) and used the lack of overlap for 95% CIs as a measure of significant difference between reporters.
Microsoft Access (Microsoft Corporation, Redmond, WA) was used as the database for this work. SAS 8.0 (SAS Institute, Cary, NC) was used for all analyses.
Results
A total of 182 parents of children between ages 1 and 12 years presenting to the ED with a respiratory complaint were screened between May 2003 and September 2003. Of those screened, 105 (57.7%) parents were eligible. Sixty-six of 105 eligible parents (62.8%) were enrolled in the study. Of the 39 parents who were eligible but not enrolled, 11 (28.2%) refused to participate and 28 (71.8%) were missed. One parent of the enrolled cohort of 66 parents did not use the asthma kiosk after informed consent was obtained.
The GSI was completed with 49 of 66 parents (74%). Parents' data from use of the asthma kiosk was available for 40 of these 49 parents (82%). Physicians' documentation was reviewed for 47 of 49 records (96%); two patients had left before being seen by a physician. Triage nurses' documentation was examined for 47 of 49 records (96%); two records were not able to be located.
▶ compares the demographic and personal attributes of the 40 parents with data from both the kiosk and the GSI versus the original cohort of 65 parents who used the kiosk.
Table 1.
Comparison of Initial Cohort to Subset Available for Analysis*
| Descriptive Variable | Cohort of 40 parents, No. (%) | Cohort of 65 parents, No. (%) |
|---|---|---|
| Comfortable/very comfortable with ATM | 36/39 (92) | 57/63 (91) |
| Used ATM in last month | 33/40 (83) | 53/65 (82) |
| High school education or less | 15/40 (38) | 24/64 (38) |
| Self-report of race as black | 19/39 (49) | 32/63 (51) |
| Self-report of “more than one race” | 04/39 (10) | 07/63 (11) |
| Self-report of ethnicity as Latino | 05/40 (13) | 11/64 (17) |
ATM = automated teller machine.
Certain denominators ≠ 40 (analyzed cohort) or ≠ 65 (enrolled cohort) due to missing data.
Parental Cohort
Data for the 40 parents who had kiosk data available were compared with data gathered by the GSI. According to the GSI, a total of 99 asthma-specific medications could have been reported across the 40 patient visits, with the absolute number reported per child ranging from one to four. Data from the asthma kiosk demonstrated that seven medications noted on GSI were missing from the parental report kiosk and 15 medications were reported by the parent but not discovered during the GSI. The overall percentage of validity of parents' report for medication names specific to asthma was 81%.
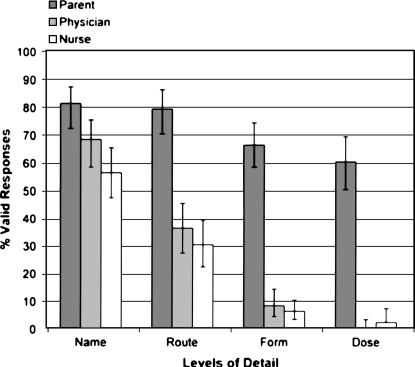
▶ outlines the validity of parents' electronically captured information and how inaccuracy and missing data affect the overall validity across four levels of detail: medication name, route of delivery, form of medication, and dose of medication.
Table 2.
Validity of Parents as Source of Asthma-Specific Medication Data*
| Level of Detail | Number Valid, No. (%, 95 CI) | Number inaccurate, No. (%, 95 CI) | Number missing, No. (%, 95 CI) |
|---|---|---|---|
| Medication name | 92 (81, 72–87) | 15 (13, 8–21) | 7 (6, 2–12) |
| Route of delivery | 90 (79, 70–86) | 17 (15, 9–23) | 7 (6, 2–12) |
| Form | 75 (66, 56–74) | 30 (26, 18–35) | 9 (8, 4–14) |
| Dose | 68 (60, 50–69) | 35 (31, 22–40) | 11 (10, 5–17) |
CI = confidence interval.
Analyzed as level of individual medications, total N = 114 for each attribute.
Comparison with Emergency Department Physicians and Nurses
The validity of parents' report on medications was compared with the documentation of physicians and nurses in the ED record. ▶ demonstrates important variation in the validity of data from each reporter. The validity of medication name reported by the parents using the kiosk was 81% (95% CI 72%–87%) compared with the validity of physician's documentation of medication names at 68% (95% CI 58%–75%). Parental report significantly improved on the validity of triage nurses' documentation at all levels of detail.
Figure 4.
Validity of medication report by type of reporter and level of detail. Error bars represent 95% confidence intervals.
Two major threats to the validity of medication data were analyzed: inaccuracy and lack of documentation. Parents, nurses, and physicians did not vary significantly in the accuracy of the medication data provided. The percentage of individual medication reports provided by parents that had inaccurate medication names (13%, 95% CI 8%–21%) did not significantly differ from that of physicians (11%, 95% CI 6%–18%) or nurses (7%, 95% CI 3%–13%). However, parents' electronic report using the asthma kiosk to provide medication names limited the quantity of missing or undocumented data. Parents provided significantly less incomplete information (6%, 95% CI 2%–12%) compared with physicians (22%, 95% CI 15–30) or nurses (36%, 95% CI 28–45).
Secondary Analyses
Medications were grouped at the level of the parent reporter and the validity of parents' report was evaluated. Nineteen of 40 parents (48%) reported all medication names correctly and completely with no false positives. Seventeen of 40 parents (42%) reported all medication names and routes in a valid manner. Only ten of 40 parents (25%) provided valid data for all medications at the level of name, route, and form.
We investigated the kiosk's value as a “stand-alone” data source for asthma medications. A minority of parents (eight of 40 [20%, with lower 95% CI of 9%]) reported valid data on all asthma-specific medications used by their children at all levels of detail. Of note, validity of documentation by physicians and nurses as stand-alone data sources performed at a significantly lower level than did parental report. No physician or nurse documentation demonstrated complete and accurate medication data across all levels of detail (0/47, 0% with upper 95% CI of 6%).
Missing data were examined across type of medications for all reporters. Of seven medications missing in parents' report, four of seven (57%) were β2 agonists, two of seven (29%) were controllers, and one of seven (14%) was an oral systemic corticosteroid. Of 27 medications missing in physicians' reports, 18 of 27 (67%) were β2 agonists, eight of 27 (30%) were controllers, and one of 27 (4%) was an oral systemic corticosteroid. Of 45 medications missing in triage nurses' documentation, 25 of 45 (56%) were β2 agonists, 19 of 45 (42%) were controllers, and one of 45 (2%) was an oral systemic corticosteroid.
Discussion
Safe and effective medical care demands a complete and accurate assessment of a patient's current medications. We present evidence of serious gaps in data capture and documentation for the asthma-specific medication history based on the standard practice of ED physicians and nurses. Parents' independent report of current medications using a multimedia touch screen kiosk improves on the current documentation of clinical ED providers, despite its limitations as a stand-alone source of historical data.
The asthma kiosk promotes an active and structured role for parents as informants to the clinical care process in the ED. It produces patient-specific medication data in electronic form that could populate centralized knowledge management system. Strategies for improvement in health care must recognize all available resources and stakeholders who can contribute to better performance.10 Parents' provision of medication data using the asthma kiosk generates a more complete list of medications including relevant details such as route, form, and dose than does routine documentation of clinical providers. This finding leads to an important question for data system redesign: Should the ideal data discovery and documentation process begin with a patient-created template subject to review and annotation by health care personnel? This “in-series” approach to data gathering would promote the best “up front” capture of data for completeness and preserves the important audit function that a trained health care provider can contribute to the data validation process.10
The ED record functions as an important template of information for subsequent inpatient or outpatient care. Information on medications as documented by physicians and nurses demonstrates significant amounts of missing as well as inaccurate data. Missing data are not restricted to medications with little consequence to the management of asthma—between 30% and 40% of controller medications were not documented in the ED chart. If the template is assumed correct and complete when in fact it is flawed, the gaps in data quality may lead to incorrect decisions and medication errors by the health personnel who subsequently treat the patient. If the initial template is assumed to be flawed and “not trustworthy,” multiple health personnel may re-ask medication-specific questions, increasing the time and effort costs for both data discovery and the validation of acquired data. The consequences of uncertainty regarding the validity of previously acquired data and the repercussions for clinicians' assumptions regarding data as “true” or “false” deserve scrutiny. Our work represents a first step in evaluating the characteristics of critical data provided by patients, physicians, and nurses (hereafter called clinical stakeholders) in the iterative exchange of medical information. This essential measurement of “who provides what data best” will assist the implementation of medication reconciliation strategies mandated by the Joint Commission on Accreditation of Health Care Organizations (JCAHO). A JCAHO National Patient Safety Goal for 2006 requires hospitals to institute a robust process for reconciling medications across the entire continuum of hospital care, from intake through discharge.11
Our investigation reinforces the interdependence of patients and health care providers in pursuit of goals related to medication safety.12 We have demonstrated that one single health data reporter cannot be relied on to provide complete and accurate data in the ED setting and that the knowledge captured from parents via the computer can improve documentation of data on medications for name, route, form, and dose of medications. Such granular capture of information is important, especially for diseases such as asthma in which the effectiveness of treatment relies in part on how a medication is given and what form of a medication is used. If a nurse or physician documents that a child takes fluticasone propionate (Flovent) for asthma but provides no other details, the resulting “gap” in data leaves unanswered questions that affect important clinical decisions. If the child's chronic symptoms are poorly controlled, should a higher concentration of Flovent be used? Similarly, if symptoms are not well controlled, is the frequency of use appropriate? If the route of delivery for Flovent is a metered dose inhaler, is the child using a spacer device to deliver the drug most effectively? Parents who used the asthma kiosk successfully bridged this gap in data quality by providing improved documentation of medications across route, form, and dose.
Electronic strategies to support patient safety such as computerized provider order entry (CPOE) require, in part, an accurate and complete report of current medications to allow assessment of risks posed by new medication orders and risks inherent in existing drug regimens. Knowledge regarding recently completed drug regimens is also critical to efforts to ensure safe and correct prescribing. Our investigation suggests that current ED triage nurse documentation would not be sufficient to populate this critical database at the front end of emergency care. We have shown that parents can participate in this front-end information capture, providing a data stream that could be incorporated into a knowledge repository that supports safe delivery of medications. Previous reports of patient-driven electronic solutions to data capture have largely focused on report of symptoms and health risk factors.13,14,15,16,17 To our knowledge, this report on the validity of parents' electronic documentation of data for the critical domain of medications represents the first evidence for patients as an integral part an informatics-based solution to medication safety.
The process of creating medication lists for use during ED care should not rely solely on patient report. Existing records within the institution or from external sources such as health plans or pharmacy networks can supply additional information about a patient's medication regimen before the ED visit.18 The accuracy and completeness of these data collected across multiple external sources have not been comprehensively evaluated to date. One study of adult patients who reviewed a paper printout of existing medication data from an institutional electronic record noted that patients provided new information to the existing record in 15 of 80 (19%) cases.19 Best practice in electronic collaborative information management for medication data should incorporate existing data, facilitate review and editing by the patient, and permit the patient's provider to have input in creating the “current” and most valid record.
The evidence from this investigation is limited by several important factors. The size of the recruited cohort is small and does not allow formal analysis of predictors of invalid data entry. As a single institution study, the results reflect the practice patterns of a specific group of ED physicians and nurses and institution-specific methods of documentation. Not all parents completed the follow-up interview to establish the gold standard, and it is possible that parents who did not complete follow-up may differ in important aspects. However, based on the demographic data available, no clear differences between the original study cohort and those who completed follow-up are apparent. The GSI considers the parents' physical possession of a medication at home to represent a current medication at the time of the ED visit. As such, we may not detect a medication that was current at the time of the ED visit but (1) was prescribed for a short duration of three to five days or (2) was replaced by a new prescription with the previous medication discarded. Our evaluation of physicians and nurses was based on documentation, not on audiotaped interviews of their interactions with parents. As such, physicians or nurses may have collected information but simply not have recorded it. Other institutions that use electronic charting vehicles wherein a physician or nurse receives prompts from the system to collect all levels of medication detail may achieve higher levels of validity than we present in this work. Finally, we cannot address the impact of the order of interviews conducted between nurse-parent, doctor-parent, and parent-computer. Workflow constraints in the ED and human subject concerns did not allow randomization of when the triage nurse and/or the treating physician conducted their interviews with the parent-child dyad.
This report on the validity of parents' electronic provision of medication data cannot address critical issues that will influence generalizability and technology adoption. These include but are not limited to (1) operational updates and maintenance of the kiosks themselves, (2) review and updates to ensure that medication content displayed to parents reflects currently available formulations, and (3) how variation in work flow across care settings will affect the presentation of patient-produced data for providers' review and use during clinical care.
Conclusion
We present preliminary evidence of the validity of parents' independent report of detailed medication data. This patient-derived data stream improved on nurses' and physicians' documentation in an ED setting. Patient safety in emergency medicine requires careful evaluation of current practices regarding documentation of medication history and the recognition of how all clinical stakeholders can contribute to improved capture and communication of these critical data. Our investigation establishes how a patient-centered technology, the asthma kiosk, may address gaps in data quality. Our work demonstrates that patients can truly be coproducers of quality and assist in improving the delivery of safe and effective care.20
Supplementary Material
Portions of this manuscript were presented in abstract form at the Pediatrics Academic Societies Meeting, May 2004, San Francisco, CA.
Supported by grant K08 HS11660-02 to Dr. Stephen Porter from the Agency for Healthcare Research and Quality and by a grant from the Charles H. Hood Foundation, Boston, MA.
The authors thank Dr. Zhaohui Cai and Ms. Sandra Lopez for their worthy efforts in the development and testing of the asthma kiosk.
References
- 1.Committee on Data Standards for Patient Safety. Patient safety—achieving a new standard of care. Institute of Medicine. Washington, DC: National Academies Press, 2004. p 1–66.
- 2.Burstin H. “Crossing the quality chasm” in emergency medicine. Acad Emerg Med. 2002;9:1074–7. [DOI] [PubMed] [Google Scholar]
- 3.Weiss KB. Measuring success in the treatment of children in the emergency department setting: process versus outcomes? Ambul Pediatr. 2002;2:301–5. [DOI] [PubMed] [Google Scholar]
- 4.National Heart, Blood, and Lung Institute. Expert Panel Report 2: guidelines for the management of asthma. Publication 97-4051. Bethesda, MD: National Institutes of Health, 1997.
- 5.Crain EF, Mortimer KM, Bauman LJ, et al. Pediatric asthma care in the emergency department: measuring the quality of history-taking and discharge planning. J Asthma. 1999;36:129–38. [DOI] [PubMed] [Google Scholar]
- 6.Porter SC, Cai Z, Gribbons W, et al. The asthma kiosk: a patient-centered technology for collaborative decision support in the emergency department. J Am Med Inform Assoc. 2004;11:458–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teich JM. Information systems support for emergency medicine. Ann Emerg Med. 1998;31:304–7. [DOI] [PubMed] [Google Scholar]
- 8.Knopp R, Rosenzweig S, Bernstein E, Totten V. Physician-patient communication in the emergency department, part 1. Acad Emerg Med. 1996;3:1065–9. [DOI] [PubMed] [Google Scholar]
- 9.Korthuis PT, Asch S, Mancewicz M, et al. Measuring medication: do interviews agree with medical record and pharmacy data? Med Care. 2002;40:1270–82. [DOI] [PubMed] [Google Scholar]
- 10.Elson RB, Faughnan JG, Connelly DP. An industrial process view of information delivery to support clinical decision making: implication and systems design and process measures. J Am Med Inform Assoc. 1997;4:266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joint Commission on Accreditation of Healthcare Organizations. 2005 critical access hospitals patient safety goals. Available from: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_cah.htm.
- 12.Porter SC, Mandl KD. Data quality and the electronic medical record: a role for direct parental data entry. Proc AMIA Symp. 1999;1/2:354–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Kim MI, Johnson KB. Personal health records: evaluation of functionality and utility. J Am Med Inform Assoc. 2002;9:171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams CA, Templin T. Usability of a computer-assisted interview system for the unaided self-entry of patient data in an urban rheumatology clinic. J Am Med Inform Assoc. 2004;11:249–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bachman JW. The patient-computer interview: a neglected tool that can aid the clinician. Mayo Clin Proc. 2003;78:67–78. [DOI] [PubMed] [Google Scholar]
- 16.Berthelsen CL, Stilley KR. Automated personal health inventory for dentistry: a pilot study. J Am Dent Assoc. 2000;131:59–66. [DOI] [PubMed] [Google Scholar]
- 17.Paperny DM, Hedberg VA. Computer-assisted health counselor visits: a low cost model for comprehensive adolescent preventive services. Arch Pediatr Adolesc Med. 1999;153:63–7. [DOI] [PubMed] [Google Scholar]
- 18.Massachusetts Health Data Consortium. The MedsInfo ED Project. Available from: http://www.mahealthdata.org/ma-share/projects/medsinfo.html.
- 19.Kuperman GJ, Sussman A, Schneider LI, Fiskio JM, Bates DW. Towards improving the accuracy of the clinical database: allowing outpatients to review their computerized data. Proc AMIA Symp. 1998:220–4. [PMC free article] [PubMed]
- 20.Kaplan B, Brennan PF. Consumer informatics supporting patients as co-producers of quality. J Am Med Inform Assoc. 2001;8:309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.