Abstract
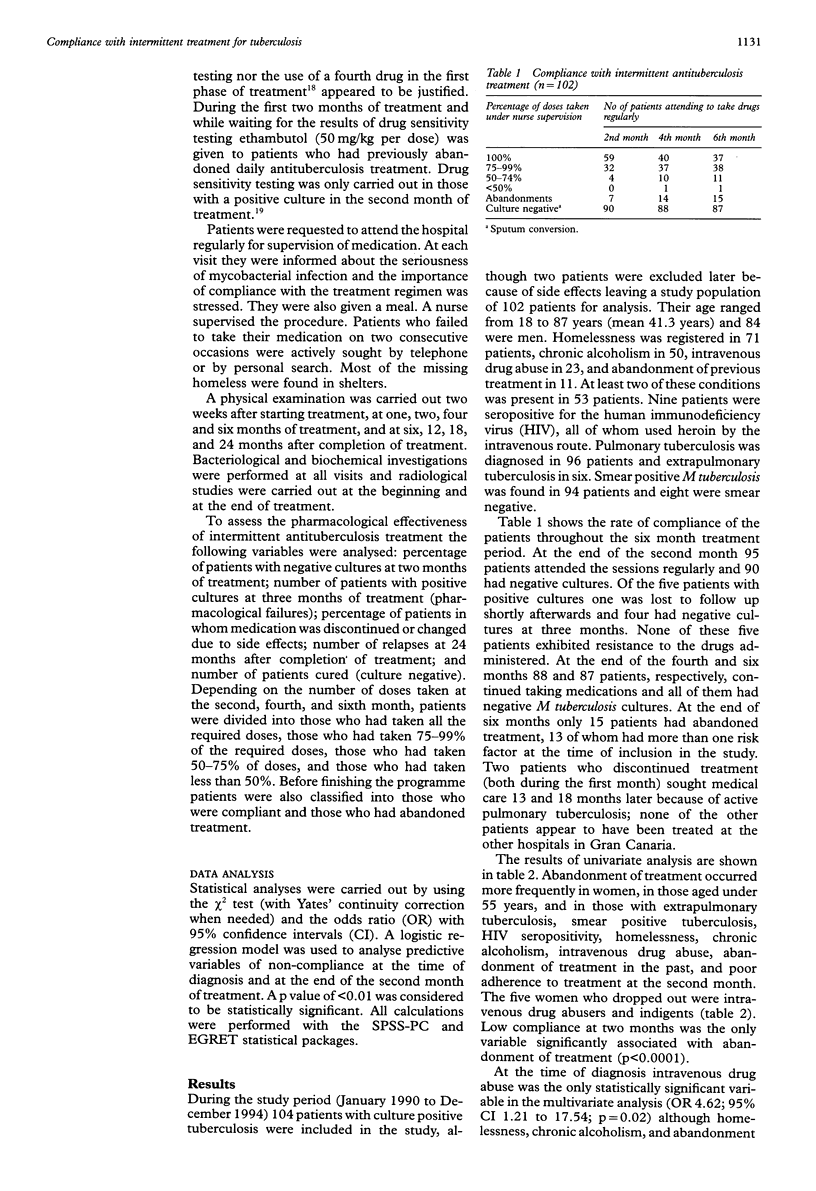
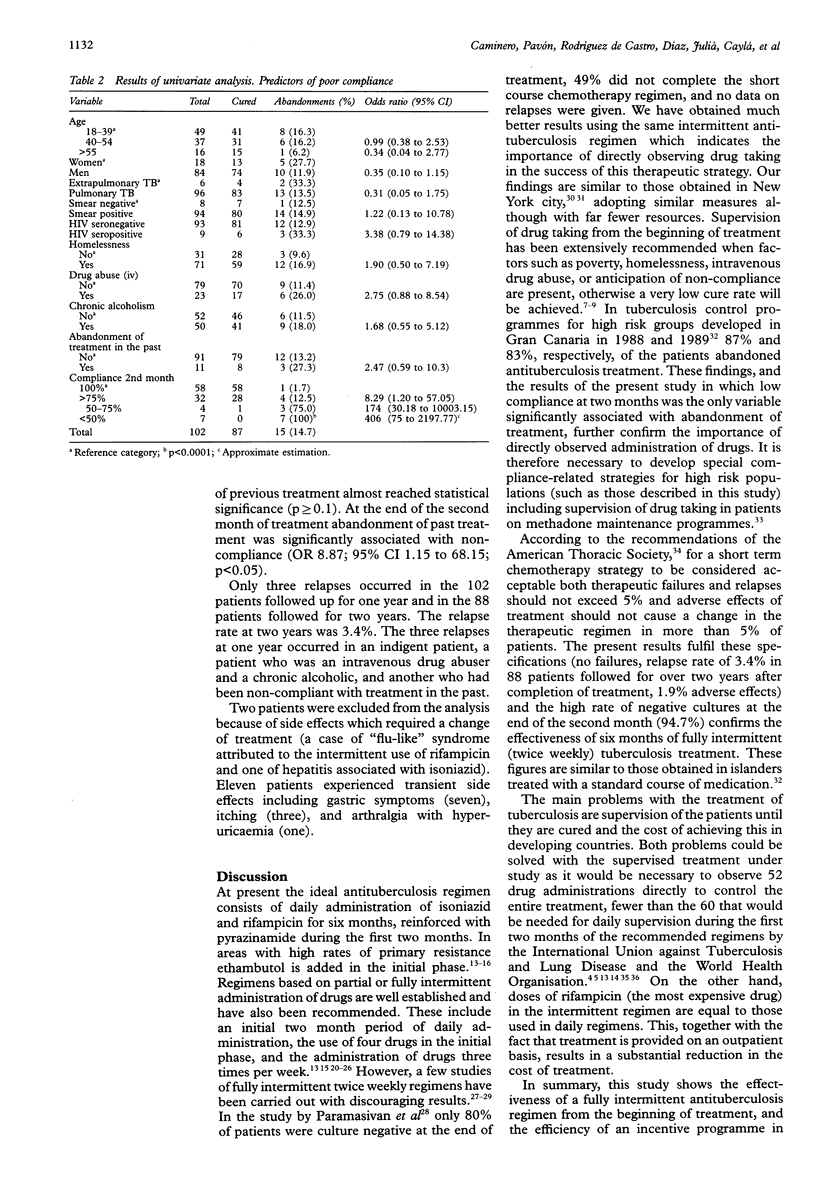
BACKGROUND: Although a priority for tuberculosis control is to achieve the maximum cure rate, compliance with chemotherapy in specific high risk groups (homeless, intravenous drug abusers, chronic alcoholics) is usually poor. METHODS: From January 1990 to December 1994 102 patients with tuberculosis (96 pulmonary, six extrapulmonary) who were poorly compliant with treatment were treated with a six month fully intermittent (twice weekly) directly observed regimen. They comprised 71 homeless subjects, 50 chronic alcoholics, 23 intravenous drug abusers, nine infected with HIV, and 11 who had previously abandoned a daily antituberculosis regimen; 53 had more than one of these risk factors. Treatment included isoniazid and rifampicin for six months and pyrazinamide during the first two months. Patients who failed to take their medication on two consecutive occasions were actively sought by telephone or by personal search. RESULTS: After two months of treatment 95 of the 102 patients had taken their medication regularly and 90 of them had negative cultures. Four of the remaining patients had negative cultures after three months. At the end of the six months 87 patients had completed treatment and were considered cured. Only 15 patients abandoned the treatment (13 of whom had more than one risk factor). Only three relapses occurred in the 102 patients at one year follow up and in the 88 patients followed for two years. Two patients required a change of treatment due to major side effects. Although intravenous drug abuse was the only predictor of non-compliance in the multivariate analysis, if the available variables in the second month of treatment were analysed, current poor compliance and abandonment of treatment in the past were found to be significantly associated with non-compliance. CONCLUSIONS: This study shows the efficacy of this intermittent regimen and the effectiveness of a directly observed treatment programme.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brudney K., Dobkin J. Resurgent tuberculosis in New York City. Human immunodeficiency virus, homelessness, and the decline of tuberculosis control programs. Am Rev Respir Dis. 1991 Oct;144(4):745–749. doi: 10.1164/ajrccm/144.4.745. [DOI] [PubMed] [Google Scholar]
- Caminero Luna J. A. Medidas básicas para el control de la tuberculosis en una comunidad. Med Clin (Barc) 1994 Jan 22;102(2):67–73. [PubMed] [Google Scholar]
- Consenso nacional para el control de la tuberculosis en España. Grupo de Trabajo sobre Tuberculosis. Med Clin (Barc) 1992 Jan 11;98(1):24–31. [PubMed] [Google Scholar]
- Datta M., Radhamani M. P., Selvaraj R., Paramasivan C. N., Gopalan B. N., Sudeendra C. R., Prabhakar R. Critical assessment of smear-positive pulmonary tuberculosis patients after chemotherapy under the district tuberculosis programme. Tuber Lung Dis. 1993 Jun;74(3):180–186. doi: 10.1016/0962-8479(93)90008-L. [DOI] [PubMed] [Google Scholar]
- Enarson D. A. Principles of IUATLD collaborative tuberculosis progammes. Bull Int Union Tuberc Lung Dis. 1991 Dec;66(4):195–200. [PubMed] [Google Scholar]
- Ferrer X., Kirschbaum A., Toro J., Jadue J., Muñoz M., Espinoza A. Adherencia al tratamiento de la tuberculosis del adulto en Santiago, Chile. Bol Oficina Sanit Panam. 1991 Nov;111(5):423–431. [PubMed] [Google Scholar]
- Frieden T. R., Fujiwara P. I., Washko R. M., Hamburg M. A. Tuberculosis in New York City--turning the tide. N Engl J Med. 1995 Jul 27;333(4):229–233. doi: 10.1056/NEJM199507273330406. [DOI] [PubMed] [Google Scholar]
- Jindani A., Aber V. R., Edwards E. A., Mitchison D. A. The early bactericidal activity of drugs in patients with pulmonary tuberculosis. Am Rev Respir Dis. 1980 Jun;121(6):939–949. doi: 10.1164/arrd.1980.121.6.939. [DOI] [PubMed] [Google Scholar]
- Mitchison D. A. Basic mechanisms of chemotherapy. Chest. 1979 Dec;76(6 Suppl):771–781. doi: 10.1378/chest.76.6_supplement.771. [DOI] [PubMed] [Google Scholar]
- Nyangulu D. S. The point of view of a high prevalence country: Malawi. Bull Int Union Tuberc Lung Dis. 1991 Dec;66(4):173–174. [PubMed] [Google Scholar]
- Paramasivan C. N., Chandrasekaran V., Santha T., Sudarsanam N. M., Prabhakar R. Bacteriological investigations for short-course chemotherapy under the tuberculosis programme in two districts of India. Tuber Lung Dis. 1993 Feb;74(1):23–27. doi: 10.1016/0962-8479(93)90064-5. [DOI] [PubMed] [Google Scholar]
- Salomao M. A. The National Tuberculosis Control Programme in Mozambique, 1985-1990. Bull Int Union Tuberc Lung Dis. 1991 Dec;66(4):175–178. [PubMed] [Google Scholar]



