Introduction
Psoriasis is a chronic inflammatory skin condition characterized by red, itchy, scaly patches that affects approximately 2% of the global population and has a significant effect on the patient’s quality of life [1]. Exploring epidemiological trends and relevant risk factors for psoriasis is vital to effectively reduce the global burden of the disease by directing efforts toward countries with the highest prevalence. This study aims to characterize trends in global rates of psoriasis and their associations with relevant risk factors.
Methods
We obtained global psoriasis data from the University of Washington Institute for Health Metrics and Evaluation Global Burden of Disease (GBD) Database and sorted it by age-standardized incidence, prevalence, and years lost to disability (YLD) rates per 100,000 people from 1990 to 2019 [2]. We further filtered these metrics by the four world regions (Asia, Africa, America, and Europe), sociodemographic index (SDI) quintiles, and the 204 countries/territories listed in the GBD database. Country-level indicator data was extracted from the World Health Organization Global Health Observatory database for possible associations with psoriasis [3]. Linear regression analyses were conducted between risk factors and incidence, prevalence, and YLD rates of psoriasis.
Ethical Considerations
This paper was conducted using publicly available databases. Therefore, no ethics approval was required.
Results
The global age-standardized prevalence rate of psoriasis per 100,000 people in 1990 was 660 (95% CI 637-681). It decreased to 504 (95% CI 487-519) in 2019. Across the world regions, psoriasis prevalence, incidence, and YLD were highest in Europe and lowest in Africa (Figure 1). Psoriasis prevalence rates were higher in the highest quintile of SDI (1990: 1256; 2019: 1073) than in the lowest quintile of SDI (1990: 338, 2019: 301) from 1990 to 2019. Similar trends were found for incidence and YLD rates.
Figure 1.
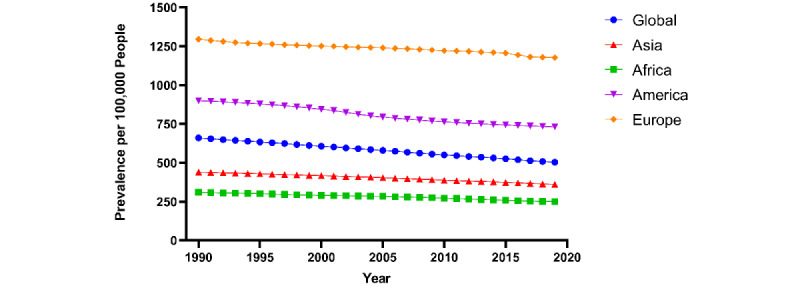
Global age-standardized prevalence rates of psoriasis per 100,000 people by Global Burden of Disease World Region.
Psoriasis incidence rates were positively associated with overweight prevalence (R2=0.36), mean cholesterol (R2=0.21), mental hospital admissions (R2=0.25), medical doctors (R2=0.50), and psychiatrists in the mental health sector (R2=0.58) while being negatively associated with air pollution mortality rates (R2=0.40; Table 1). Similar trends were noted for risk factor associations with psoriasis prevalence and YLD rates (P<.001).
Table 1.
Linear regression analyses of risk factors associated with incidence, prevalence, and years lost to disability (YLD) rates of psoriasis.
| Risk factors and Y value | Association | Countries, n | R 2 | P value | |||||||
| Overweight prevalence (BMI ≥25, age-standardized estimate; %) | 182 |
|
|
||||||||
|
|
Incidence of psoriasis | Positive |
|
0.26 | <.001 | ||||||
|
|
Prevalence of psoriasis | Positive |
|
0.22 | <.001 | ||||||
|
|
YLDs of psoriasis | Positive |
|
0.19 | <.001 | ||||||
| Mean total cholesterol (age-standardized estimate) | 184 |
|
|
||||||||
|
|
Incidence of psoriasis | Positive |
|
0.31 | <.001 | ||||||
|
|
Prevalence of psoriasis | Positive |
|
0.26 | <.001 | ||||||
|
|
YLDs of psoriasis | Positive |
|
0.23 | <.001 | ||||||
| Mortality rate attributed to household and ambient air pollution per 100,000 population (age-standardized) | 182 |
|
|
||||||||
|
|
Incidence of psoriasis | Negative |
|
0.40 | <.001 | ||||||
|
|
Prevalence of psoriasis | Negative |
|
0.35 | <.001 | ||||||
|
|
YLDs of psoriasis | Negative |
|
N/Aa | <.001 | ||||||
| Mental hospital admissions per 100,000 population | 98 |
|
|
||||||||
|
|
Incidence of psoriasis | Positive |
|
0.25 | <.001 | ||||||
|
|
Prevalence of psoriasis | Positive |
|
0.21 | <.001 | ||||||
|
|
YLDs of psoriasis | Positive |
|
0.17 | <.001 | ||||||
| Medical doctors per 100,000 population | 184 |
|
|
||||||||
|
|
Incidence of psoriasis | Positive |
|
0.50 | <.001 | ||||||
|
|
Prevalence of psoriasis | Positive |
|
0.44 | <.001 | ||||||
|
|
YLDs of psoriasis | Positive |
|
0.41 | <.001 | ||||||
| Psychiatrists working in mental health sector (per 100,000 population) | 102 |
|
|
||||||||
|
|
Incidence of psoriasis | Positive |
|
0.58 | <.001 | ||||||
|
|
Prevalence of psoriasis | Positive |
|
0.56 | <.001 | ||||||
|
|
YLDs of psoriasis | Positive |
|
0.53 | <.001 | ||||||
aN/A: not applicable.
Discussion
There are a few reasons why global psoriasis prevalence consistently decreased since 1990. Psoriasis may go into remission, decreasing the duration of the disease and ultimately its prevalence, especially in older individuals. Additionally, comorbidities and adverse health behaviors may lead to increased mortality rates among individuals with psoriasis, resulting in decreased prevalence rates [4]. However, a significant global disease burden remains. Europe has the highest incidence, while Africa has the lowest. These findings were consistent with a prior study on the epidemiology of psoriasis [5]. Factors that were characteristic of wealthier countries such as high SDI, high overweight prevalence, higher mean cholesterol, and lower air pollution mortality rates were found to be associated with higher psoriasis incidence, prevalence, and YLD. Despite greater access to medical resources, high psoriasis prevalence in the highest SDI countries remains. Strong positive associations between psoriasis rates and medical doctors per 100,000 population and psychiatrists per 100,000 population further highlight this trend, underscoring the burden of psoriasis in areas more densely populated with medical professionals. Additionally, psoriasis rates are associated with mental hospital indications, indicating possible psychiatric comorbidities among patients with psoriasis. Solutions must be tailored to more complex causes of psoriasis, such as the gut-brain-skin axis’ role in skin disorders, smoking exposure, alcohol intake, specific medications, and even genetic causes [6].
Limitations of this study include underreporting in some sub-Saharan regions and potentially inaccurate modeling algorithms by the GBD website. Additionally, there may potentially be an ecological fallacy as the populations analyzed in this study may not be representative of the individual members. This study provides a unique and recent perspective on the epidemiological trends of psoriasis. To effectively reduce the burden of psoriasis in these countries, more research on the complex environmental and genetic risk factors of psoriasis should be conducted.
Abbreviations
- GBD
Global Burden of Disease
- SDI
sociodemographic index
- YLD
years lost to disability
Footnotes
Conflicts of Interest: TS serves as an editorial board member-at-large for JMIR Dermatology. All other authors report no conflicts of interest. TS receives fellowship funding from Pfizer (grant 25B1519; principal investigator: Stanca Birlea) and the National Institutes of Health (grant 2T32AR00741136A1; principal investigator: Dennis Roop).
References
- 1.Christophers E. Psoriasis--epidemiology and clinical spectrum. Clin Exp Dermatol. 2001 Jun;26(4):314–20. doi: 10.1046/j.1365-2230.2001.00832.x.ced832 [DOI] [PubMed] [Google Scholar]
- 2.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct 17;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(20)30925-9 .S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Global Health Observatory. World Health Organization. [2021-08-13]. https://www.who.int/data/gho .
- 4.Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevalence and treatment of psoriasis in the United Kingdom: a population-based study. Arch Dermatol. 2005 Dec;141(12):1537–41. doi: 10.1001/archderm.141.12.1537.141/12/1537 [DOI] [PubMed] [Google Scholar]
- 5.Mehrmal S, Uppal P, Nedley N, Giesey RL, Delost GR. The global, regional, and national burden of psoriasis in 195 countries and territories, 1990 to 2017: a systematic analysis from the Global Burden of Disease Study 2017. J Am Acad Dermatol. 2021 Jan;84(1):46–52. doi: 10.1016/j.jaad.2020.04.139.S0190-9622(20)30760-X [DOI] [PubMed] [Google Scholar]
- 6.Arck P, Handjiski B, Hagen E, Pincus M, Bruenahl C, Bienenstock J, Paus R. Is there a 'gut-brain-skin axis'? Exp Dermatol. 2010 May;19(5):401–5. doi: 10.1111/j.1600-0625.2009.01060.x.EXD1060 [DOI] [PubMed] [Google Scholar]