Key Clinical Message
Root resection is performed to create a maintainable furcation area in teeth with advanced periodontitis. However, the long‐term feasibility of this treatment remains controversial. We present a case in which distal root resection in a maxillary molar successfully preserved the form and function of the dentition for approximately 14 years.
Keywords: furcation defect, long‐term, molar teeth, periodontitis, prognosis
1. INTRODUCTION
Periodontal diseases are a group of inflammatory processes that affect the tooth‐supporting structures, which, if left untreated, can progress and cause bone loss, thereby impairing the survival of the teeth. 1 , 2 , 3 Maxillary molars are the most commonly lost teeth, followed by the mandibular molars. 4 , 5
Treatment of periodontal disease focuses mainly on arresting disease progression and preserving the form and function of the dentition involved. Managing periodontal disease around multirooted teeth is challenging for periodontists because of the complex anatomy of the tooth furcation area, which favors plaque accumulation and hinders personal and professional cleaning attempts. The furcation is defined as the anatomic area of a multirooted tooth in which the roots diverge, and pathologic resorption of the bone in this region is known as “furcation involvement.” 6
Furcation involvement is associated with a poor prognosis and higher tendency for tooth loss 4 due to the complex anatomy 7 , 8 , 9 and difficulty in maintaining oral hygiene, performing periodontal debridement, 10 , 11 , 12 , 13 and periodontal maintenance. 5 Several treatment options have been proposed to manage furcation involvement by cleaning the area and rendering it more cleansable. Treatment options vary according to the degree of furcation involvement and patient‐ and clinician‐related factors and include simple debridement of the defect using either closed or surgical approaches; furcation plasty/osseous plasty; regenerative approaches involving guided tissue regeneration around the furcation; and respective approaches involving tunneling, 14 root resection/amputation, or hemisection. In case of failure of these options, tooth extraction is necessary.
Root amputation and hemisection are the least desired approaches by both patients and clinicians because of the assumption of inferior results compared with other therapies, such as dental implants. However, this assumption is contrary to the findings in several studies that reported high success rates when these procedures were performed correctly on properly selected patients. Herein, we present the 14‐year follow‐up of a maxillary right first molar (tooth #16) in which root amputation was performed and explain how this procedure saved the tooth during cancer treatment.
1.1. Case history
A 33‐year‐old woman was referred to our periodontal department by a prosthodontist for surgical crown lengthening of the endodontically treated tooth #16. The patient was medically fit and did not smoke. Clinical examination revealed fair oral hygiene with calculus deposition over the mandibular anterior teeth. Periodontal evaluation revealed a localized deep periodontal pocket with a probing depth (PD) of 6–7 mm distal to tooth #16 and distal grade 2 furcation involvement. 15 In addition, a periodontal pocket with a PD of 4–5 mm and grade 1 furcation involvement distal to tooth #26, 2 mm gingival recession around tooth #46 with lingual grade 2 furcation involvement, gingival recession on the lingual of the mandibular anterior teeth, and buccal of tooth #34 Recession type two (RT 2), 16 and short anterior crowns were observed. The patient had class 1 molar and canine relationships on both sides according to Angle's classification (Figure 1).
FIGURE 1.
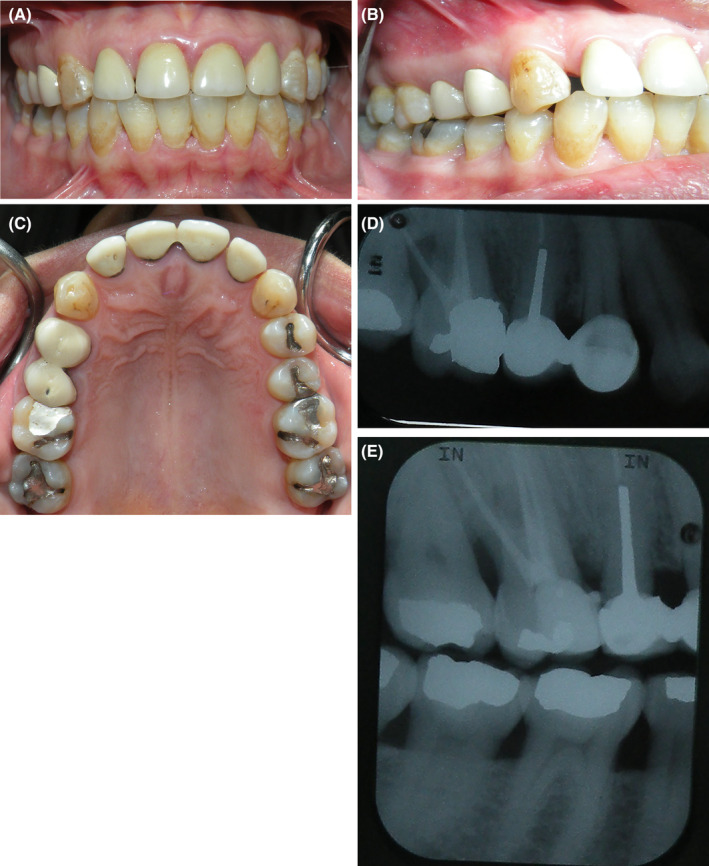
Pre‐treatment photos showing #16. (A) Frontal view, (B) lateral view, (C) Occlusal view, (D) Periapical radiograph, and (E) bitewing radiographs.
2. DIFFERENTIAL DIAGNOSIS AND INVESTIGATIONS
Endodontic‐induced bone loss as well as the possibility of traumatic occlusion were considered. However, further investigations and consultations have ruled out those factors.
2.1. Periodontal diagnosis
The patient was diagnosed with periodontitis stage 3 grade B with a molar incisor pattern 17 (formerly localized aggressive periodontitis), 18 with recession type two (RT 2) 16 on the lingual of teeth #33–43 and buccal of tooth #34, as well as altered passive eruption of the maxillary incisors.
3. TREATMENT
Phase 1 therapy, including oral hygiene instructions, scaling, and root planing, was performed, and combination antibiotic therapy consisting of 500 mg amoxicillin and 500 mg metronidazole orally was administered three times a day for a week. During the reevaluation, a significant improvement in patient's oral hygiene and bleeding index was noticed, however, with very little improvement distal to #16. Thus, periodontal surgical therapy was initiated after reevaluation. The patient underwent open flap debridement around teeth #26 and #46, connective tissue grafting around tooth #34, and anterior esthetic crown lengthening.
Tooth #16 was previously endodontically treated, and flap reflection revealed that the vertical defect involved more than two‐thirds of the distal root with deep grade 2 furcation involvement. Therefore, distal root amputation was performed to maintain the tooth while eliminating the pocket and furcation area, rendering the area accessible for maintenance using oral hygiene measures. (Figure 2).
FIGURE 2.
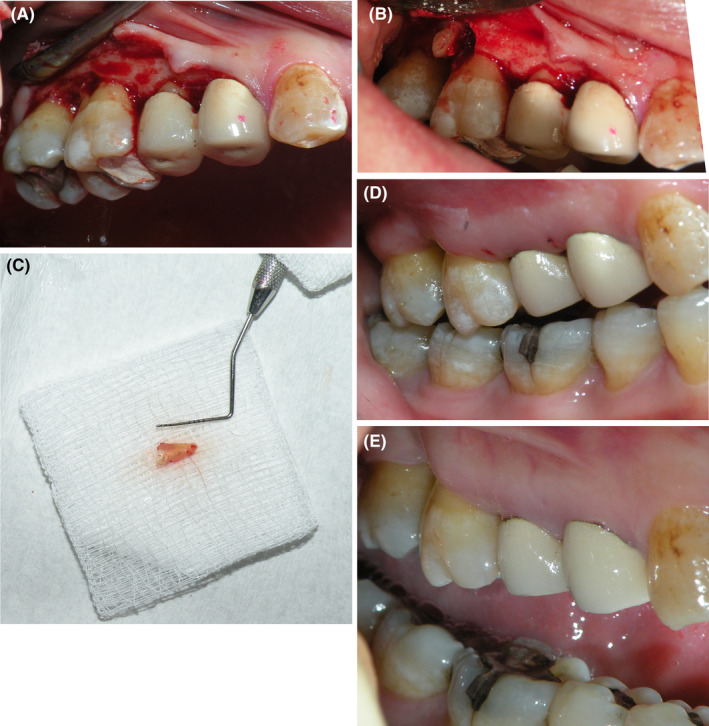
Surgical root amputation. (A): Flap reflection, (B) Distal root amputation, (C) the resected Root (D) 1‐week follow up after suture removal, and (E) 3‐months follow‐up.
Subsequent prosthodontic evaluation revealed that the tooth was subjected to low occlusal forces, the access cavity was small with minimal loss of tooth structure, precluding the need for tooth crowning.
4. FOLLOW‐UP
The patient was followed up every 4–6 months for around 10 years. During this period, her overall periodontal condition was stable, and routine maintenance was performed. Although few incidents of disease exacerbation with PDs of approximately 4–5 mm around the molars occurred, local nonsurgical measures were sufficient for their management (Figure 3). During that period, the patient developed type 2 diabetes mellitus and hypertension. Towards the end of the ninth year after surgery, the patient was diagnosed with breast cancer for which she underwent respective surgery and received hormonal treatment and bisphosphonate injections. The patient could not adhere to the periodontal maintenance program during this period and missed multiple appointments. Consequently, her oral hygiene reduced, and the periodontal status began to deteriorate. Probing depth (PD) around tooth #16 increased and arresting disease progression was difficult. Around 4 years later, the patient finished her breast cancer treatment and resumed her dental visits; PD around tooth #16 had significantly increased up to 9 mm, and surgical intervention was necessary. Cone‐beam radiographic evaluation revealed bone loss around the tooth, and extraction and implant placement were planned (Figure 4). However, the tooth was in function and had successfully preserved the space for approximately 14 years.
FIGURE 3.
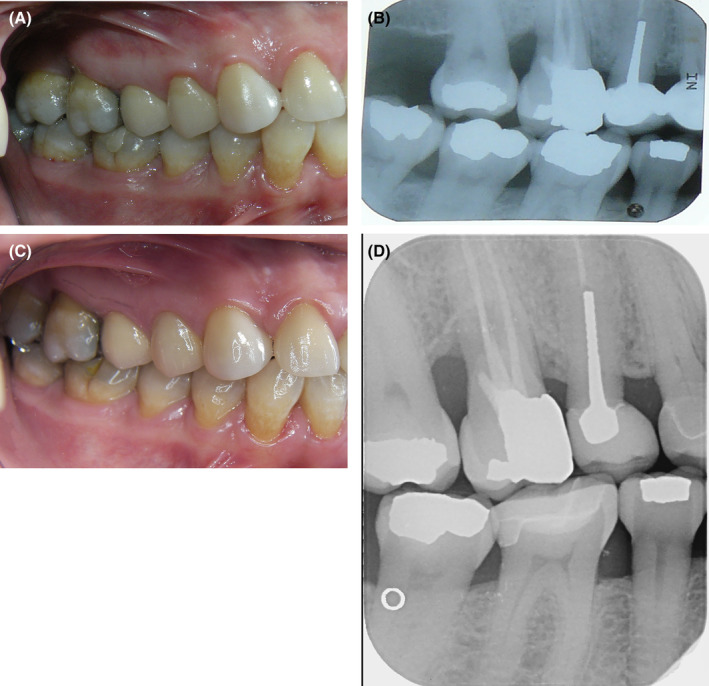
Follow‐up of the procedure after (A) 1‐year clinical view, (B) 1‐year Radiographs, (C) 6‐years clinical view, and (D) 10‐years bitewing radiograph.
FIGURE 4.
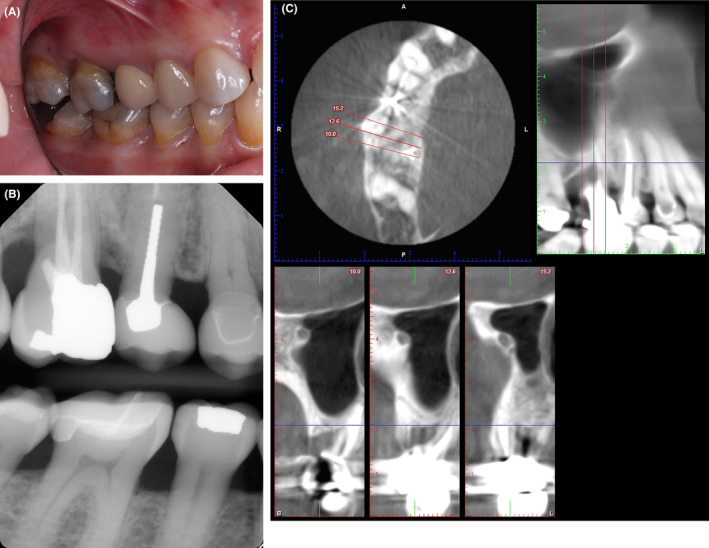
(A) 14 years clinical view, (B) 14 years bitewing radiograph, and (C) 14 years Cone beam computed tomography for the indicated tooth.
5. DISCUSSION WITH MINI REVIEW OF THE LITERATURE
Furcation involvement is a major factor hindering the prognosis of molar teeth because of the difficulty in maintaining an area free from dental plaque. Root resection and/or amputation is a possible strategy for managing this situation by creating an area that is more accessible for oral hygiene measures. Several previous studies have evaluated the long‐term success of this procedure. 19 , 20 , 21 , 22 , 23 , 24 , 25 Table 1 summarizes some of the studies available in the literature with their main findings.
TABLE 1.
Studies evaluating long‐term failure rates of root amputation.
| Author | Follow‐up period range in years (average) | No. of teeth | Overall percentage of teeth lost/failed |
|---|---|---|---|
| Bergenholtz, 1972 24 | 2–11 | 45 | 6 |
| Klavan, 1975 23 | 1–7 (3) | 34 | 2.9 |
| Hamp and Nyman 14 | 5 | 87 | 0 |
| Langer et al., 1981 22 | 10 | 100 | 38 |
| Erpenstein, 1983 25 | 1–7 (2.9) | 34 | 8.8 |
| Buhler, 1988, 20 | 10 | 28 | 32 |
| Newel 1991 26 | 0.5–7 | 70 | 30 |
| Basten 1996 27 | 2–23 (11.5) | 49 | 8 |
| Blomlof et al 1997 28 | 3–10 (5.8) | 146 | 22 |
| Carnevale 1998 29 | 10 | 175 | 7 |
| Hou 1999 30 | 5–13 (6.7 ± 1.9) | 85 | 0 |
| Park et al 2009 31 | 10 | 342 | 29.8 |
| Lee et al 2012 32 | 10 | 149 | 59.7 |
| Derks 2018 33 | 4–30 (14.7 ± 6.8) | 90 | 33.3 |
| Alassadi 2020 34 | 1–16.8 (5 ± 4.3) | 85 | 44.7% |
| AlSayed 2020 35 | 1–15 (9.62 ± 3.08) | 130 | 43.1% |
The success rate ranged from 100% 14 , 30 to 40% 32 ; however, a systematic review published in 2009 reported the survival rate to range between 62%–100% over an observation period of 15–13 years. 36 A more recent systematic review published during 2020 indicated an overall survival rate of 38%–94.4%, which is similar to that of scaling, root planing, and open flap debridement. 37 The difference in success rates between studies can be attributed to several factors, including the criteria for case selection, type of final restoration, follow‐up duration, and criteria for defining success. 38
Derks et al. 33 evaluated the long‐term survival rates of root‐resected teeth over approximately 30 years. They reported a cumulative survival rate of 90.6% for the first 10 years, which decreased considerably thereafter, with a median survival duration of 20 years after root resection.
Owing to the importance of proper case selection and careful performance of the procedure for improving the overall survival rate, several authors have attempted to define the essential criteria for determining procedural success.
Newel attributed failures to residual root fragments and furcation lips and ledges that were not properly identified and managed during surgery, 26 while Carnevale et al. 29 considered osseous recontouring and apical repositioning of the flap essential for procedural success.
Mjzoob and Kon stressed the importance of careful evaluation of the procedure and proper planning for subsequent restorations because only 8% of root‐resected molars have favorable periodontal support postoperatively. 39
Park reported that teeth with >50% residual supporting bone had higher survival rates. 31 In contrast, Lee et al. reported an increased risk for procedural failure in teeth with mobility ≥ grade 2 before root resection and removal of the supporting bone. 32 Persistent mobility of any degree after phase‐one therapy and the involvement of two or more proximal surfaces were considered contraindications by Klavan et al. 23
Rasperini presented a decision tree wherein root amputation/resection was indicated only for cases with grade 3 furcation involvement with the vertical component of the furcation not exceeding the middle third of the root and attachment loss limited to only one root. 40
The choice between maintaining a tooth with root amputation or replacing it with a dental implant is debatable. Fugazzotto et al. 41 compared the success rates of root‐resected molars to those of dental implants placed in the molar region and found success rates ranging between 95.2% and 100% over 15 years of observation, with cumulative success rates of 96.8% for root‐resected molars and 97% for implants. Zafiropoulos et al. 42 reported a complication rate of 32.1% in root‐resected molars compared to 11.1% in implants in the molar region over approximately 4 years. Similarly, Kinsel et al. 43 reported a 15.9% failure rate for root‐resected molars compared to 3.6% for single implants.
Higher failure rates for implants in the maxillary molar region are attributed to the bone quality in that region. 44 Simonis et al. 45 reported complications in approximately 48.03% of implants. Therefore, all factors should be considered, and treatment options should be discussed with the restorative dentist and presented to the patient before finalization of the treatment plan.
In this case, root amputation successfully maintained the form and function of the dentition for more than 10 years. We believe that problems only started when the patient showed reduced compliance with maintenance visits. Even though, we think that this treatment gave the patient the chance to postpone bone grafting and dental implant placement for better timing. Placing implants earlier might have led to the development of peri‐implantitis owing to the difficulties associated with their maintenance.
6. CONCLUSION
We reported a case with long‐term follow‐up after root amputation. Root resection helped maintain the form and function of the dentition for more than 10 years, allowing for better timing for dental implant placement. This case highlights the importance of proper maintenance visits and patient compliance.
AUTHOR CONTRIBUTIONS
Sumaiah Ajlan: Conceptualization; methodology; project administration; resources; writing – original draft.
FUNDING INFORMATION
Non applicable.
CONFLICT OF INTEREST STATEMENT
No conflict of interest to declare.
ETHICS STATEMENT
The patient has signed a written informed consent in accordance with Journal's policy.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Ajlan SA. Maxillary root amputation: Case report with a 14‐year‐follow‐up and updated mini review. Clin Case Rep. 2024;12:e8553. doi: 10.1002/ccr3.8553
DATA AVAILABILITY STATEMENT
The data that supports this case are available with the corresponding author upon reasonable request.
REFERENCES
- 1. Bjorn AL, Hjort P. Bone loss of furcated mandibular molars. A longitudinal study. J Clin Periodontol. 1982;9(5):402‐408. doi: 10.1111/j.1600-051x.1982.tb02052.x [DOI] [PubMed] [Google Scholar]
- 2. Becker W, Berg L, Becker BE. Untreated periodontal disease: a longitudinal study. J Periodontol. 1979;50(5):234‐244. doi: 10.1902/jop.1979.50.5.234 [DOI] [PubMed] [Google Scholar]
- 3. Lindhe J, Okamoto H, Yoneyama T, Haffajee A, Socransky SS. Periodontal loser sites in untreated adult subjects. J Clin Periodontol. 1989;16(10):671‐678. doi: 10.1111/j.1600-051x.1989.tb01038.x [DOI] [PubMed] [Google Scholar]
- 4. Hirschfeld L, Wasserman B. A long‐term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49(5):225‐237. doi: 10.1902/jop.1978.49.5.225 [DOI] [PubMed] [Google Scholar]
- 5. McFall WT Jr. Tooth loss in 100 treated patients with periodontal disease. A long‐term study. J Periodontol. 1982;53(9):539‐549. doi: 10.1902/jop.1982.53.9.539 [DOI] [PubMed] [Google Scholar]
- 6. AAP . Glossary of Periodontal Terms. 4th ed. American academy of periodontology; 2001. [Google Scholar]
- 7. Bower RC. Furcation morphology relative to periodontal treatment. Furcation entrance architecture. J Periodontol. 1979;50(1):23‐27. doi: 10.1902/jop.1979.50.1.23 [DOI] [PubMed] [Google Scholar]
- 8. Bower RC. Furcation morphology relative to periodontal treatment. Furcation Root Surface Anatomy. J Periodontol. 1979;50(7):366‐374. doi: 10.1902/jop.1979.50.7.366 [DOI] [PubMed] [Google Scholar]
- 9. Svardstrom G, Wennstrom JL. Furcation topography of the maxillary and mandibular first molars. J Clin Periodontol. 1988;15(5):271‐275. doi: 10.1111/j.1600-051x.1988.tb01583.x [DOI] [PubMed] [Google Scholar]
- 10. Parashis AO, Anagnou‐Vareltzides A, Demetriou N. Calculus removal from multirooted teeth with and without surgical access. II. Comparison between external and furcation surfaces and effect of furcation entrance width. J Clin Periodontol. 1993;20(4):294‐298. doi: 10.1111/j.1600-051x.1993.tb00361.x [DOI] [PubMed] [Google Scholar]
- 11. Parashis AO, Anagnou‐Vareltzides A, Demetriou N. Calculus removal from multirooted teeth with and without surgical access. (I). Efficacy on external and furcation surfaces in relation to probing depth. J Clin Periodontol. 1993;20(1):63‐68. doi: 10.1111/j.1600-051x.1993.tb01762.x [DOI] [PubMed] [Google Scholar]
- 12. Matia JI, Bissada NF, Maybury JE, Ricchetti P. Efficiency of scaling of the molar furcation area with and without surgical access. Int J Periodontics Restorative Dent. 1986;6(6):24‐35. [PubMed] [Google Scholar]
- 13. Fleischer HC, Mellonig JT, Brayer WK, Gray JL, Barnett JD. Scaling and root planing efficacy in multirooted teeth. J Periodontol. 1989;60(7):402‐409. doi: 10.1902/jop.1989.60.7.402 [DOI] [PubMed] [Google Scholar]
- 14. Hamp SE, Nyman S, Lindhe J. Periodontal treatment of multirooted teeth. Results after 5 years. J Clin Periodontol. 1975;2(3):126‐135. doi: 10.1111/j.1600-051x.1975.tb01734.x [DOI] [PubMed] [Google Scholar]
- 15. Glickman I. Clinical periodontology. 2nd ed. W. B. Saunders; 1958. [Google Scholar]
- 16. Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol. 2011;38(7):661‐666. doi: 10.1111/j.1600-051X.2011.01732.x [DOI] [PubMed] [Google Scholar]
- 17. Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and Peri‐implant diseases and conditions. J Periodontol. 2018;89(Suppl 1):S173‐S182. doi: 10.1002/JPER.17-0721 [DOI] [PubMed] [Google Scholar]
- 18. Albandar JM. Aggressive periodontitis: case definition and diagnostic criteria. Periodontol 2000. 2000;65(1):13‐26. doi: 10.1111/prd.12014 [DOI] [PubMed] [Google Scholar]
- 19. Carnevale G, Pontoriero R, Hurzeler MB. Management of furcation involvement. Periodontol 2000. 1995;9:69‐89. doi: 10.1111/j.1600-0757.1995.tb00057.x [DOI] [PubMed] [Google Scholar]
- 20. Buhler H. Evaluation of root‐resected teeth. Results after 10 years. J Periodontol. 1988;59(12):805‐810. doi: 10.1902/jop.1988.59.12.805 [DOI] [PubMed] [Google Scholar]
- 21. Carnevale G, Di Febo G, Tonelli MP, Marin C, Fuzzi M. A retrospective analysis of the periodontal‐prosthetic treatment of molars with interradicular lesions. Int J Periodontics Restorative Dent. 1991;11(3):189‐205. [PubMed] [Google Scholar]
- 22. Langer B, Stein SD, Wagenberg B. An evaluation of root resections. A ten‐year study. J Periodontol. 1981;52(12):719‐722. doi: 10.1902/jop.1981.52.12.719 [DOI] [PubMed] [Google Scholar]
- 23. Klavan B. Clinical observations following root amputation in maxillary molar teeth. J Periodontol. 1975;46(1):1‐5. doi: 10.1902/jop.1975.46.1.1 [DOI] [PubMed] [Google Scholar]
- 24. Bergenholtz A. Radectomy of multirooted teeth. J Am Dent Assoc. 1972;85(4):870‐875. doi: 10.14219/jada.archive.1972.0445 [DOI] [PubMed] [Google Scholar]
- 25. Erpenstein H. A 3‐year study of hemisectioned molars. J Clin Periodontol. 1983;10(1):1‐10. doi: 10.1111/j.1600-051x.1983.tb01262.x [DOI] [PubMed] [Google Scholar]
- 26. Newell DH. The role of the prosthodontist in restoring root‐resected molars: a study of 70 molar root resections. J Prosthet Dent. 1991;65(1):7‐15. doi: 10.1016/0022-3913(91)90039-y [DOI] [PubMed] [Google Scholar]
- 27. Basten CH, Ammons WF Jr, Persson R. Long‐term evaluation of root‐resected molars: a retrospective study. Int J Periodontics Restorative Dent. 1996;16(3):206‐219. [PubMed] [Google Scholar]
- 28. Blomlof L, Jansson L, Appelgren R, Ehnevid H, Lindskog S. Prognosis and mortality of root‐resected molars. Int J Periodontics Restorative Dent. 1997;17(2):190‐201. [PubMed] [Google Scholar]
- 29. Carnevale G, Pontoriero R, di Febo G. Long‐term effects of root‐resective therapy in furcation‐involved molars. A 10‐year longitudinal study. J Clin Periodontol. 1998;25(3):209‐214. doi: 10.1111/j.1600-051x.1998.tb02430.x [DOI] [PubMed] [Google Scholar]
- 30. Hou GL, Tsai CC, Weisgold AS. Treatment of molar furcation involvement using root separation and a crown and sleeve‐coping telescopic denture. A longitudinal study. J Periodontol. 1999;70(9):1098‐1109. doi: 10.1902/jop.1999.70.9.1098 [DOI] [PubMed] [Google Scholar]
- 31. Park SY, Shin SY, Yang SM, Kye SB. Factors influencing the outcome of root‐resection therapy in molars: a 10‐year retrospective study. J Periodontol. 2009;80(1):32‐40. doi: 10.1902/jop.2009.080316 [DOI] [PubMed] [Google Scholar]
- 32. Lee KL, Corbet EF, Leung WK. Survival of molar teeth after resective periodontal therapy – a retrospective study. J Clin Periodontol. 2012;39(9):850‐860. doi: 10.1111/j.1600-051X.2012.01918.x [DOI] [PubMed] [Google Scholar]
- 33. Derks H, Westheide D, Pfefferle T, Eickholz P, Dannewitz B. Retention of molars after root‐resective therapy: a retrospective evaluation of up to 30 years. Clin Oral Investig. 2018;22(3):1327‐1335. doi: 10.1007/s00784-017-2220-1 [DOI] [PubMed] [Google Scholar]
- 34. Alassadi M, Qazi M, Ravida A, Siqueira R, Garaicoa‐Pazmino C, Wang HL. Outcomes of root resection therapy up to 16.8 years: a retrospective study in an academic setting. J Periodontol. 2020;91(4):493‐500. doi: 10.1002/JPER.19-0033 [DOI] [PubMed] [Google Scholar]
- 35. El Sayed N, Cosgarea R, Rahim S, Giess N, Krisam J, Kim TS. Patient‐, tooth‐, and dentist‐related factors influencing long‐term tooth retention after resective therapy in an academic setting‐a retrospective study. Clin Oral Investig. 2020;24(7):2341‐2349. doi: 10.1007/s00784-019-03091-9 [DOI] [PubMed] [Google Scholar]
- 36. Huynh‐Ba G, Kuonen P, Hofer D, Schmid J, Lang NP, Salvi GE. The effect of periodontal therapy on the survival rate and incidence of complications of multirooted teeth with furcation involvement after an observation period of at least 5 years: a systematic review. J Clin Periodontol. 2009;36(2):164‐176. doi: 10.1111/j.1600-051X.2008.01358.x [DOI] [PubMed] [Google Scholar]
- 37. Dommisch H, Walter C, Dannewitz B, Eickholz P. Resective surgery for the treatment of furcation involvement: a systematic review. J Clin Periodontol. 2020;47(Suppl 22):375‐391. doi: 10.1111/jcpe.13241 [DOI] [PubMed] [Google Scholar]
- 38. Kasaj A. Root resective procedures vs implant therapy in the management of furcation‐involved molars. Quintessence Int. 2014;45(6):521‐529. doi: 10.3290/j.qi.a31806 [DOI] [PubMed] [Google Scholar]
- 39. Majzoub Z, Kon S. Tooth morphology following root resection procedures in maxillary first molars. J Periodontol. 1992;63(4):290‐296. doi: 10.1902/jop.1992.63.4.290 [DOI] [PubMed] [Google Scholar]
- 40. Rasperini G, Majzoub J, Tavelli L, et al. Management of Furcation‐Involved Molars: recommendation for treatment and regeneration. Int J Periodontics Restorative Dent. 2020;40(4):e137‐e146. doi: 10.11607/prd.4341 [DOI] [PubMed] [Google Scholar]
- 41. Fugazzotto PA. A comparison of the success of root resected molars and molar position implants in function in a private practice: results of up to 15‐plus years. J Periodontol. 2001;72(8):1113‐1123. doi: 10.1902/jop.2001.72.8.1113 [DOI] [PubMed] [Google Scholar]
- 42. Zafiropoulos GG, Hoffmann O, Kasaj A, Willershausen B, Deli G, Tatakis DN. Mandibular molar root resection versus implant therapy: a retrospective nonrandomized study. J Oral Implantol. 2009;35(2):52‐62. doi: 10.1563/1548-1336-35.2.52 [DOI] [PubMed] [Google Scholar]
- 43. Kinsel RP, Lamb RE, Ho D. The treatment dilemma of the furcated molar: root resection versus single‐tooth implant restoration. A literature review. Int J Oral Maxillofac Implants. 1998;13(3):322‐332. [PubMed] [Google Scholar]
- 44. Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5‐year analysis. J Periodontol. 1991;62(1):2‐4. doi: 10.1902/jop.1991.62.1.2 [DOI] [PubMed] [Google Scholar]
- 45. Simonis P, Dufour T, Tenenbaum H. Long‐term implant survival and success: a 10‐16‐year follow‐up of non‐submerged dental implants. Clin Oral Implants Res. 2010;21(7):772‐777. doi: 10.1111/j.1600-0501.2010.01912.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that supports this case are available with the corresponding author upon reasonable request.


