ABSTRACT
Background: Although trauma exposure is universally prevalent, the ways in which individuals respond to potentially traumatic events vary. Between-country differences have been identified as affecting the development and manifestation of transdiagnostic psychological symptoms, but it remains unclear how stress and trauma-related transdiagnostic symptoms and risk patterns differ based on geographic region.
Objective: To explore whether there are distinct classes of stress and trauma-related transdiagnostic symptoms and to determine predictors of class membership in a global sample.
Method: Participants (N = 8675) from 115 different countries were recruited online between 2020–2022 and completed the Global Psychotrauma Screen, which assesses stress and trauma exposure, related symptoms, and risk factors. A latent class analysis (LCA) was used to identify classes of stress and trauma-related symptoms per world region (African States, Asia-Pacific States, Eastern European States, Latin American and Caribbean States, Western European and Other States, and North America) and the total sample. Likelihood of class membership was assessed based on demographics, characteristics of the potentially traumatic event, and potential risk factors across the world regions.
Results: Similar class compositions were observed across regions. A joint latent class analysis identified three classes that differed by symptom severity (i.e. high, moderate, low). Multinomial logistic regression analyses revealed several factors that conferred greater risk for experiencing higher levels of symptoms, including geographic region, gender, and lack of social support, among others.
Conclusions: Stress and trauma-related symptoms seem to be similarly transdiagnostic across the world, supporting the value of a transdiagnostic assessment.
KEYWORDS: Trauma, latent class analysis, transdiagnostic symptoms, cross-country comparison, risk factors
HIGHLIGHTS
A latent class analysis of transdiagnostic stress and trauma-related symptoms in a global sample showed high, medium, and low symptom classes.
Class compositions were similar across global geographic regions.
Several factors were associated with high symptom class membership globally, including gender, geographic region, and lack of social support.
Abstract
Antecedentes: aunque la exposición al trauma es universalmente prevalente, las formas en que los individuos responden a eventos potencialmente traumáticos varían. Se ha identificado que las diferencias entre países afectan el desarrollo y la manifestación de los síntomas psicológicos transdiagnósticos, pero permanece sin esclarecer cómo los síntomas transdiagnósticos y patrones de riesgo relacionados con el estrés y el trauma difieren según la región geográfica.
Objetivo: explorar si existen distintas clases de síntomas transdiagnósticos relacionados con el estrés y el trauma y determinar predictores de pertenencia a una clase en una muestra global.
Método: Participantes (N = 8.675) de 115 países diferentes fueron reclutados en línea entre 2020 y 2022 y completaron la Evaluación Global de Psicotrauma, que evalúa la exposición al estrés y al trauma, los síntomas relacionados y los factores de riesgo. Se utilizó un análisis de clases latentes (LCA) para identificar clases de síntomas relacionados con el estrés y el trauma por región del mundo (Estados de África, Estados de Asia y el Pacífico, Estados de Europa del Este, Estados de América Latina y el Caribe, Estados de Europa Occidental y otros, y América del Norte) y la muestra total. La probabilidad de pertenecer a una clase se evaluó en función de la demografía, las características del evento potencialmente traumático y los posibles factores de riesgo en todas las regiones del mundo.
Resultados: Se observaron composiciones de clases similares en todas las regiones. Un análisis conjunto de clases latentes identificó tres clases que diferían según la gravedad de los síntomas (es decir, alta, moderada, baja). Los análisis de regresión logística multinomial revelaron varios factores que conferían un mayor riesgo de experimentar niveles más altos de síntomas, incluida la región geográfica, el género y la falta de apoyo social, entre otros.
Conclusiones: Los síntomas relacionados con el estrés y el trauma parecen ser igualmente transdiagnósticos en todo el mundo, lo que respalda el valor de una evaluación transdiagnóstica.
PALABRAS CLAVE: Trauma, análisis de clases latentes, síntomas transdiagnósticos, comparación entre países, factores de riesgo
1. Introduction
Trauma exposure is common in all parts of the world, with 70% of people estimated to experience one or more potentially traumatic events (PTEs) in their lifetime (Benjet et al., 2016). Although trauma exposure is universally prevalent, the ways in which individuals respond to PTEs vary by symptom severity and type. Many trauma-exposed individuals do not experience persistent trauma-related symptoms, whereas some experience symptoms that contribute to ongoing psychological distress, functional impairment, and medical issues such as cardiovascular disease (Kessler et al., 2017; Lowe et al., 2021; Møller et al., 2021). Stress and trauma-related reactions are often transdiagnostic, meaning they can span multiple psychological disorders such as depression, anxiety, or substance abuse (Hogg et al., 2023; Sunderland et al., 2016). As such, examining stress and trauma-related reactions at the symptom level is crucial to better understand, assess, and treat transdiagnostic consequences of trauma exposure (Levin-Aspenson et al., 2021).
Previous studies have identified notable cultural, cross-national, and cross-regional differences in exposure to particular trauma types and to chronic and cumulative stressors, as well as in trauma-related symptom severity (Bromet et al., 2017; Cruz-Gonzalez et al., 2023; Ford et al., 2015). These differences have been explained not only by differences in traditions, beliefs, values, and socialization, but also by cross-national and cross-regional disparities in socioeconomic indicators, healthcare resources, education, gender and sexual orientation attitudes, and legal rights (Ford et al., 2015; Krueger et al., 2003; Nochaiwong et al., 2021). Not only do type and severity significantly differ but also the phenomenology of trauma reactions and symptom manifestations significantly differ across the world (Beller, 2023; Heim et al., 2022; Krueger et al., 2003; Nochaiwong et al., 2021; Rasmussen et al., 2014). For example, in some cultures, people may be more likely to present with somatic complaints, whereas in others specific PTSD symptoms, such as dissociation, may be more likely (Hinton & Lewis-Fernández, 2011; Marques et al., 2011). Thus, it is suggested to use a research approach that focuses on exploring global similarities and variations in trauma manifestations by emphasizing symptomatic heterogeneity and the transdiagnostic nature of trauma across the world (Heim et al., 2022; Rasmussen et al., 2014).
One way to investigate complex structures underlying the range of reactions to stress and trauma exposure is through Latent Class Analysis (LCA). In contrast to the variable-centered approach, e.g. Confirmatory Factor Analysis (CFA), which focuses on homogeneous patterns of associations between variables, LCA, a person-centered approach, identifies unobserved homogeneous subgroups of individuals characterized by particular combinations of symptoms endorsement (Nylund-Gibson & Choi, 2018). These approaches are complementary, as CFA tests if the transdiagnostic symptoms load on a certain factor, while LCA explores if one class of individuals tends to endorse some symptoms more than others. Previous studies used LCA to identify classes of symptom presentations with disorders like (complex) PTSD (Campbell et al., 2020; Deen et al., 2022; Elklit et al., 2014; Spikol et al., 2022). Resulting classes were distinguished by severity (e.g. a low and a high symptom class) or subgroups of symptoms (e.g. with versus without dissociative symptoms). While previous studies have applied CFA to define factors of transdiagnostic symptoms following trauma exposure (e.g. Frewen et al., 2021; Rossi et al., 2021; Salimi et al., 2023), only a few studies have explored patterns of transdiagnostic symptoms on a person-centered level (Boelen et al., 2022; Contractor et al., 2017).
As aforementioned, the development, severity, and persistence of trauma-related symptoms are affected by certain personal as well as social risk and protective factors. In a recent umbrella review of systematic reviews and meta-analyses (Tortella-Feliu et al., 2019), risk factors included (but were not limited to) exposure to childhood trauma, being female, coming from a lower socioeconomic background, type of trauma, and having a history of mental illness (Chiu et al., 2011; Kessler et al., 2017). Research has found, however, that social support and psychological resilience may mitigate risk for trauma-related symptoms (Iacoviello & Charney, 2014). To our knowledge, no study has assessed the association between these established risk and protective factors and a wide range of transdiagnostic reactions after trauma in an extensive global sample. To identify subgroups at risk for developing certain symptoms after experiencing PTEs, it is important to investigate whether specific factors are associated with a certain class membership (i.e. a certain subgroup identified by LCA).
Separately, taking a transdiagnostic perspective could provide better understanding of the impact of trauma exposure and the variety of stress and trauma-related symptoms. Furthermore, given the cross-cultural differences in symptom manifestations, it is possible that the composition of classes of symptom presentations after trauma differs across geographic regions. This notion is supported by a recent study that found that the meaning and nature of symptom classes differed between military personnel in the United States (US) and India (Contractor et al., 2020). This study's results indicated that a four-class solution was optimal in India as well as US samples. In both samples, the classes differed quantitatively in terms of severity of the symptoms; however, in the US sample the classes also differed qualitatively, indicating not only differing severity but also different symptom types between the four classes. Whether the class composition of transdiagnostic reactions after PTEs indeed differs across geographical regions worldwide warrants further research. Moreover, understanding cross-regional differences and similarities in stress and trauma-related reactions can help to develop targeted prevention and intervention strategies.
The primary aim of this paper was to explore whether there were distinct classes of stress and trauma-related transdiagnostic symptoms within a large and diverse geographic sample. First, we explored whether the composition of classes differed per geographic region (i.e. assessed whether visual inspection indicated configural non-invariance) using LCA. Considering potential cross-cultural differences in responses to PTEs, we wanted to explore whether geographic regions were associated with different class compositions. If different class compositions were found, we would perform a LCA for each geographic region. Otherwise, we would perform one LCA across all regions. Our second aim was to assess whether these classes differed in demographics, characteristics of the PTEs, and potential risk factors. We had no a priori hypotheses as these relied heavily on the class structures that we had yet to identify.
2. Method
2.1. Participants and procedures
Participants were recruited worldwide by collaborators in the field of traumatic stress studies and via social media to complete an online survey presented on the Global Collaboration on Traumatic Stress webpage (https://www.global-psychotrauma.net/gps). To participate in the study, participants were required to be at least 16 years old and to acknowledge and accept the terms of the survey: that the data was anonymous, that it would be stored on a secure server for at least 15 years, and that only group-averaged results would be published. Participation was voluntary and no remuneration was provided. The Medical Ethical Review Committee of the Academic Medical Center Amsterdam reviewed the study proposal and exempted it from formal ethical review (W19_481 # 19.556).
Data were collected from 25 April 2020 to 3 October 2022. In total, 8836 participants from 115 countries participated in the survey. At the time of recruitment, the questionnaire was available in 21 languages, which participants could select using a dropdown menu. Only those participants for whom country information was available were included in this study (n excluded = 161). The final sample consisted of 8675 participants.
2.2. Measures
Demographics. Demographic information was collected from participants including gender, age, and country of residence. Response options for gender were female, male, and other (herein referred to as woman, man, and gender nonbinary respectively).
The Global Psychotrauma Screen (GPS). The GPS (Olff et al., 2020, 2021) is a transdiagnostic screening tool that captures a range of reactions to PTEs across nine symptom domains: PTSD, disturbances in self-organization, anxiety, depression, sleep problems, self-harm, dissociation, other problems (physical, emotional, or social), and substance abuse. The self-report measure captures an index traumatic event or severe stressor, followed by 17 stress and trauma-related symptoms, and five risk factors. For the index event, participants were asked about timing, frequency, mode of exposure (happened to yourself or someone else), and the type of event (physical violence, sexual violence, emotional abuse, serious injury, sudden death of a loved one, perpetrating harm). For the latter two items, participants had the option to select more than one response option (e.g. a combination of emotional abuse and physical violence). We considered events that involved physical violence, sexual violence, serious injury, life threatening event, sudden death, or perpetrating harm as events that met Criterion A for PTSD in the DSM-5 (American Psychiatric Association, 2013). Participants responded to the 17 stress and trauma-related symptoms (e.g. having nightmares, feeling worthless, intentionally hurting oneself) based on their experiences in the past month. Of the five questions that capture risk factors, two assess experiences in the past month (other stressful events, lack of social support) and three assess lifetime experiences (childhood trauma, history of mental illness, lack of resilience). The symptoms and risk factors are scored dichotomously (Yes/No).
Although more psychometric testing of the GPS is encouraged, there is strong initial support for the psychometric validity of the GPS as administered in English, Japanese and Persian (Frewen et al., 2021; Oe et al., 2020; Salimi et al., 2023). Cronbach’s alpha for the 17 GPS symptom items in the current sample was 0.89.
Geographic Region. For this analysis, we categorized participants into groups based on the United Nations (UN) regional groups of member states (United Nations, 2022): (1) African States, (2) Asia-Pacific States, (3) Eastern European States, (4) Latin American and Caribbean States, and (5) Western European and Other States. Due to large sample sizes, we did not include the US and Canada in the ‘Western European and Other States’ group as suggested by the UN (2022), but broke them into their own group, (6) ‘North America’. For countries that did not fall under any of the UN groupings (e.g. Jersey), we assigned them to one of the six groups based on their geographical proximity to the nearest UN region.
2.3. Data analysis
Pearson’s χ2 tests and one-way analyses of variance (ANOVA) were conducted to examine global differences in event type and event-conditional transdiagnostic symptom load.
Six LCAs, one for each UN region, were conducted to explore empirically driven typologies (i.e. classes) characterized by different patterns of transdiagnostic reactions. Models included 17 stress and trauma-related symptoms measured as binary indicators. Models with one to six classes were considered for all regions based on model fit statistics, parsimony, and theoretical interpretability (Weller et al., 2020). Fit statistics used for model selection included the Akaike information criterion (AIC), Bayesian information criterion (BIC), and sample size adjusted BIC, for which lower values suggest better fit. We also used the Vuong-Lo-Mendell-Rubin adjusted likelihood ratio test (LMR) and bootstrapped likelihood ratio test (bLRT). These tests compare the fit of k to k-1 classes, with a statistically significant p-value indicating a better fit for k classes. Entropy values, which reflect classification accuracy of the model, were calculated. Higher values indicate higher accuracy in class assignment, with values greater than 0.80 indicating good, and 1 indicating perfect class assignment (Nylund-Gibson & Choi, 2018).
To assess for configural invariance, we examined the structure and distribution of classes across regions. Whether configural invariance was present was based on our qualitative assessment of the structure and distribution of classes per region. If configural invariance was found, the data would be pooled and a final LCA would be performed to explore different patterns of transdiagnostic symptoms in the full sample. Again, models with one to six classes were considered based on model fit statistics, and selection of the optimally fitting model was based on model fit statistics, parsimony, and theoretical interpretability. LCA analyses were conducted in MPlus 8.
Following class identification, we assigned participants to the class for which the posterior probability was the highest. Assignment to the highest membership probability should be appraised against potential classification error, which depends on the entropy value. To identify predictors of observed class membership, we conducted a logistic multinomial regression model simultaneously including demographics and previously identified risk factors from the literature. For inclusion in the regression model, all categorical variables were coded in a way that allowed for meaningful interpretation. For UN region, effect coding with deviation from the unweighted grand mean was used, and all other categorical variables were dummy coded. Alpha levels of < .05 were considered to be significant. Models were estimated in R version 4.0.3.
We imputed missing data for trauma type, timing of the event (how long ago), and trauma frequency. There was no missing data for the GPS symptoms and risk factors. Missing data on the imputed variables were minimal (1.4–4.8%), except for trauma frequency of the index event (single versus multiple; 16.5% missing). Missing data were imputed with random forests using R package missForest (Stekhoven, 2022). Imputation was successful with a normalized root mean squared error (NRMSE) of 0.31 and a proportion of falsely classified entries (PFC) of 0.05 (Stekhoven & Buhlmann, 2012). Our analyses on predictors of class membership as well as global differences in event-type and event-conditional transdiagnostic symptom load were based on the imputed dataset. The data and code for all analyses can be found in the OSF repository: https://osf.io/c6u3m/
3. Results
3.1. Sample characteristics
Our final sample consisted of N = 8675 participants. Participants’ age ranged between 16 and 105 years old (M = 38.1, SD = 14.1) and the majority were women (75.0%). Most respondents came from Western European and Other States (30.3%), with the least coming from African States (3.4%). The demographics and frequencies of risk factors of our sample can be found in Table 1.
Table 1.
Demographics and risk factors of the study sample.
| Variables | N = 8675a | |||
|---|---|---|---|---|
| n | % | |||
| Age (years) | Mean | 38.1 | ||
| SD | 14.1 | |||
| Gender | Men | 2077 | 23.9 | |
| Women | 6506 | 75.0 | ||
| Nonbinary | 92 | 1.1 | ||
| UN region | African States | 293 | 3.4 | |
| Asia-Pacific States | 1733 | 20.0 | ||
| Eastern European States | 1575 | 18.2 | ||
| Latin American and Caribbean States | 956 | 11.0 | ||
| Western European and Other States | 2631 | 30.3 | ||
| North America | 1487 | 17.1 | ||
| Risk factors | Other stressful events | 5544 | 63.9 | |
| Lack of social support | 3749 | 43.2 | ||
| Childhood trauma | 4728 | 54.5 | ||
| History of mental illness | 3282 | 37.8 | ||
| Lack of resilience | 1824 | 21.0 | ||
Note. aInformation reported based on raw data. No data was missing for these variables.
A majority of the index events met the DSM-5 A-Criterion for PTSD (69.8%). Approximately one third of our sample experienced an index event that happened multiple times. Additional characteristics of the index events experienced by the participants can be found in Table 2. In line with current best practices to more systematically consider the role of sex and gender in health services research and care (Heidari et al., 2016), we provide detailed information about demographics, trauma characteristics, and risk factors disaggregated by gender in Supplement 1. Notable differences in sexual and physical violence exposure by gender were found, with non-binary participants most likely and men least likely to endorse exposure.
Table 2.
Characteristics of the index event.
| N = 8675a | |||
|---|---|---|---|
| n | % | ||
| Meeting DSM-5 PTSD A-criterion | Yes | 6053 | 69.8 |
| No | 2413 | 27.8 | |
| Trauma onset > one year ago | Yes | 4812 | 55.5 |
| No | 3450 | 39.7 | |
| Multiple experiences of index event | Yes | 3007 | 34.7 |
| (vs. single event) | No | 4240 | 48.9 |
| Characteristics of index eventb | Physical violence | ||
| Happened to self | 1712 | 19.7 | |
| Happened to someone else | 1362 | 15.7 | |
| Sexual violence | |||
| Happened to self | 1397 | 16.1 | |
| Happened to someone else | 675 | 7.8 | |
| Emotional abuse | |||
| Happened to self | 3468 | 40.0 | |
| Happened to someone else | 1196 | 13.8 | |
| Serious injury | |||
| Happened to self | 998 | 11.5 | |
| Happened to someone else | 1020 | 11.8 | |
| Life threatening | |||
| Happened to self | 1784 | 20.6 | |
| Happened to someone else | 1819 | 21.0 | |
| Causing harm to someone else | 323 | 3.7 | |
| Sudden death | 1838 | 21.2 | |
Note. aInformation reported based on raw data. Percentages of the yes/no items that do not add up to 100 indicate missing data. Information on characteristics of the index event was missing in 1.4% to 2.1% of cases. bMultiple answers were possible.
Examinations of event type by region showed that participants from North America reported significantly higher rates of sexual violence than participants from all other regions (40% vs. 12–22%) and that the same was true for multiple experiences of the index event (60% vs. 27–39%). Participants from Eastern European states, on the other hand, reported significantly lower shares of events involving sexual violence (12% vs. 21–40%) or life threat (31% vs. 37–41%) compared to all other regions. Cross-regional examinations of symptom distributions furthermore suggested small to moderate effect size differences (Cohen’s d = 0.19–0.69) in event-type conditional transdiagnostic symptom load: For all three categories examined (i.e. sexual violence-related symptoms, symptoms related to multiple experiences of the event, and life threat-related symptoms) participants from North America reported higher transdiagnostic symptom scores than participants from most of the remaining regions. Detailed information on regional differences in event type and symptom distributions is provided in Supplement 2.
3.2. Latent class analyses
In all regions, we considered the absolute value of each fit statistic, which did not converge on a single solution in any region (see OSF repository for latent class fit model statistics by UN region). In all models, the BIC only improved marginally after 3 classes. Compared to the 3-class model, the 4-class model also showed an additional, redundant class that lacked a unique interpretation. We therefore selected a 3-class model for all regions. Our qualitative assessment of the structure and distribution of classes in each region suggested it likely there was configural invariance.
In a next step we hence carried out one LCA on the full sample. Table 3 presents the goodness-of-fit indices for the latent class models from the full sample analysis (one to six classes). Again, the BIC only improved marginally after 3 classes, and the 4-class model showed an additional, redundant class that lacked a unique interpretation. Additionally, the 3-class model had better classification quality (0.83), which is ideal when assigning individuals according to their highest class probability.
Table 3.
Fit indices for 1–6 class solutions (full sample).
| Model | LL | AIC | BIC | sBIC | LMR | bLRT | Entropy |
|---|---|---|---|---|---|---|---|
| 1 class | −94443.144 | 188920.289 | 189040.448 | 188986.425 | – | – | – |
| 2 class | −79434.664 | 158939.329 | 159186.716 | 159075.492 | 0.000 | 0.000 | 0.886 |
| 3 class | −76788.214 | 153682.428 | 154057.043 | 153888.618 | 0.000 | 0.000 | 0.825 |
| 4 class | −76066.215 | 152274.431 | 152776.273 | 152550.648 | 0.000 | 0.000 | 0.785 |
| 5 class | −75814.680 | 151807.360 | 152436.430 | 152153.604 | 0.010 | 0.000 | 0.739 |
| 6 class | −75605.007 | 151424.013 | 152180.311 | 151840.284 | 0.000 | 0.000 | 0.702 |
Note. LL = Loglikelihood; AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; sBIC = sample size adjusted BIC; LMR = Vuong-Lo-Mendell-Rubin adjusted likelihood ratio test; bLRT = bootstrapped likelihood ratio test.
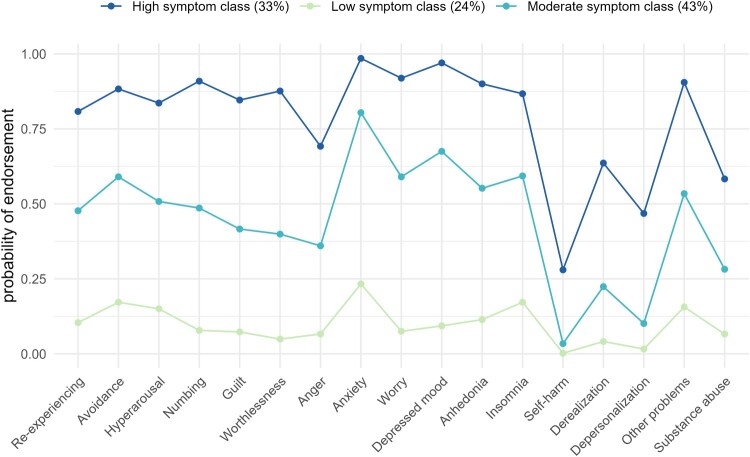
We did not find qualitatively different classes, but classes differed on symptom severity levels. Figure 1 shows the item probability rates per class. The first class consisted of 2102 respondents (24.2%) and was characterized by a generally low profile of symptom endorsement (‘low symptom class’). The second class consisted of 3739 respondents (43.1%) and was characterized by a moderate chance of endorsement on most symptoms (‘moderate symptom class’). Chances of symptom endorsement in this class were all higher than in the ‘low symptom class’. The third class, consisting of 2834 respondents (32.7%), was characterized by a high chance of endorsement on most symptoms (‘high symptom class’). Chances of symptom endorsement were higher across all symptoms compared to the ‘moderate symptom class’. Overall, the self-harm and depersonalization symptoms were least endorsed across all classes, whereas anxiety symptoms were the most endorsed. A descriptive overview of demographics, trauma characteristics, and risk factors by class membership is presented in Supplement 3.
Figure 1.
Estimated probabilities of endorsement for the 3-class-solution.
3.3. Predictors of class membership
The results of the multinomial regression analyses are presented in Table 4, including odds ratios (ORs), confidence intervals, and p-values. Significant contrasts are highlighted below. Compared to the low symptom class, women and gender nonbinary participants demonstrated higher odds of belonging to the high symptom class (ORs = 1.63, 3.34, respectively). Similarly, participants whose index event fulfilled DSM-5 PTSD Criterion A, occurred multiple times, or happened within the past year (ORs = 1.31, 4.89, 1.85, respectively) showed elevated odds of membership in the high versus low symptom class. Regarding geographic location, the likelihood of membership in the high symptom class, compared to low class, was higher for participants from Latin American and Caribbean States (OR = 1.23) as well as North America (OR = 1.38). In contrast, the likelihood of membership in the high symptom class, compared to the low symptom class, was lower for participants from Asia-Pacific States (OR = 0.71) and Eastern European States (OR = 0.80). Older age was also associated with lower likelihood of being in the high symptom class (OR = 0.98). All GPS risk factors (other stressful events, lack of social support, history of mental illness, childhood trauma, lack of resilience) were predictive of membership in the high versus low symptom class (ORs = 7.52, 6.52, 4.06, 2.27, 1.93, respectively).
Table 4.
Predictors of class membership.
| High vs. low (reference) | High vs. moderate (reference) | Moderate vs. low (reference) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | ||||||||||
| OR | Lower | Upper | p | OR | Lower | Upper | p | OR | Lower | Upper | p | |
| Gender: Womena | 1.63 | 1.37 | 1.93 | <.001 | 1.05 | 0.91 | 1.21 | .508 | 1.55 | 1.36 | 1.77 | <.001 |
| Gender: Nonbinaryb | 3.34 | 1.31 | 8.49 | .011 | 1.93 | 1.12 | 3.32 | .018 | 1.73 | 0.70 | 4.28 | .233 |
| Age | 0.98 | 0.97 | 0.98 | <.001 | 0.98 | 0.98 | 0.99 | <.001 | 0.99 | 0.99 | 1.00 | .003 |
| African Statesc | 1.11 | 0.80 | 1.54 | .533 | 1.31 | 1.03 | 1.67 | .025 | 0.85 | 0.63 | 1.13 | .260 |
| Asia-Pacific Statesc | 0.71 | 0.60 | 0.84 | .000 | 0.85 | 0.75 | 0.97 | .017 | 0.84 | 0.73 | 0.96 | .011 |
| Eastern European Statesc | 0.80 | 0.68 | 0.95 | .011 | 0.89 | 0.78 | 1.01 | .069 | 0.91 | 0.79 | 1.04 | .166 |
| Latin American and Caribbean States c | 1.23 | 1.01 | 1.51 | .043 | 0.98 | 0.84 | 1.15 | .841 | 1.25 | 1.06 | 1.49 | .009 |
| Western European and Other Statesc | 0.92 | 0.80 | 1.06 | .249 | 0.99 | 0.89 | 1.11 | .876 | 0.93 | 0.82 | 1.04 | .213 |
| North Americac | 1.38 | 1.13 | 1.69 | .001 | 1.03 | 0.91 | 1.17 | .616 | 1.34 | 1.12 | 1.60 | .002 |
| PTSD criterion A1d | 1.31 | 1.11 | 1.54 | .002 | 1.17 | 1.02 | 1.33 | .020 | 1.12 | 0.98 | 1.28 | .096 |
| Multiple experiences of index evente | 4.89 | 4.14 | 5.78 | <.001 | 2.15 | 1.92 | 2.41 | <.001 | 2.27 | 1.96 | 2.64 | <.001 |
| Index event happened in the past yearf | 1.85 | 1.58 | 2.16 | <.001 | 1.05 | 0.93 | 1.18 | .471 | 1.77 | 1.55 | 2.01 | <.001 |
| Other stressful eventsg | 7.52 | 6.40 | 8.84 | <.001 | 2.24 | 1.96 | 2.57 | <.001 | 3.35 | 2.97 | 3.79 | <.001 |
| Lack of social supportg | 6.52 | 5.54 | 7.68 | <.001 | 2.41 | 2.15 | 2.70 | <.001 | 2.71 | 2.34 | 3.12 | <.001 |
| Childhood traumag | 2.27 | 1.94 | 2.65 | <.001 | 1.65 | 1.46 | 1.86 | <.001 | 1.37 | 1.21 | 1.56 | <.001 |
| History of mental illnessg | 4.06 | 3.41 | 4.83 | <.001 | 2.35 | 2.08 | 2.65 | <.001 | 1.73 | 1.48 | 2.02 | <.001 |
| Lack of resilienceg | 1.93 | 1.60 | 2.32 | <.001 | 1.73 | 1.51 | 1.99 | <.001 | 1.11 | 0.95 | 1.30 | .192 |
Note. Predictors were included in the model simultaneously. a0: man, 1: woman; b0: man,1: nonbinary; cCoding for UN region: deviation from unweighted grand mean; d0: PTSD criterion A not fulfilled, 1: PTSD criterion A fulfilled; e0: index event was single event, 1: index event happened multiple times; f0: index event happened more than a year ago, 1: index event happened in the past year; g0: risk factor not present, 1: risk factor present.
Compared to the moderate symptom class, individuals identifying as gender nonbinary, reporting a PTSD Criterion A index event, and experiencing the index event multiple times demonstrated higher likelihoods of belonging to the high symptom class (ORs = 1.93, 1.17, 2.15, respectively). Being from African States was associated with a higher likelihood of being in the high symptom class compared to the moderate symptom class (OR = 1.31). In contrast, being from Asia-Pacific States was associated with a lower likelihood of membership in the high (versus moderate) symptom class (OR = 0.75). Older age was also associated with lower likelihood of being in the high symptom class (OR = 0.98). Again, other stressful events, childhood trauma, history of mental illness, lack of social support, and lack of resilience were predictive of membership in the high versus moderate symptom class (ORs = 2.24, 2.41, 1.65, 2.35, 1.73, respectively).
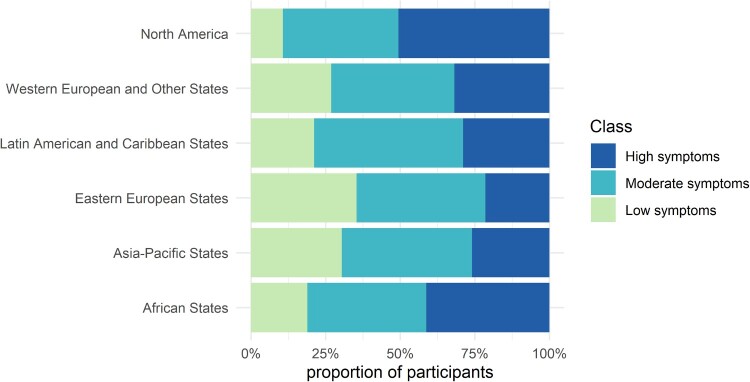
Compared to the low symptom class, the likelihood for membership in the moderate symptom class was higher for women, participants who experienced the index event multiple times, and those who experienced the index event in the past year (ORs = 1.55, 2.27, 1.77, respectively). The likelihood of membership in the moderate symptom class, compared to the low symptom class, was higher for participants from Latin American and Caribbean States (OR = 1.25), and North America (OR = 1.34). Again, participants from Asia-Pacific States demonstrated lower chances of being in the moderate symptom class compared to the low symptom class (OR = 0.84). Four of the GPS risk factors, (other stressful events, childhood trauma, history of mental illness, and lack of social support), were further predictive of membership in the moderate versus low symptom class (ORs = 3.35, 2.71, 1.37, 1.73, respectively). The likelihood for membership in the moderate symptom class (versus low symptom class) was again lower for older participants (OR = 0.99). Figure 2 shows a graphical representation of class membership by region.
Figure 2.
Class membership by region.
4. Discussion
The first aim of the current study was to identify latent classes of stress and trauma-related transdiagnostic symptoms using a person-centered approach in a global sample. We first explored whether compositions of transdiagnostic symptoms differed between six world regions, and found similar symptom severity class compositions across the geographic regions. In our full sample (N = 8675), the LCA identified three classes: 1) a high symptom class, 2) a moderate symptom class, and 3) a low symptom class. The second aim was to determine the predictors of class membership. Findings revealed several risk factors, including certain geographic regions, that were associated with more transdiagnostic symptoms following a PTE.
Our visual inspection did not show different class compositions across geographic regions. This could indicate that transdiagnostic symptoms manifestations after PTEs are similar across the world. This suggests that taking a transdiagnostic view when assessing reactions to stress and trauma is relevant for all parts of the world. An alternative explanation for this finding is that, due to methodological limitations, different countries were grouped into large geographical regions, creating regions that do not necessarily have a shared culture, language, economy, etc., which might be key drivers for cross-regional differences. As such, based on our data, it is difficult to draw firm conclusions about global differences in transdiagnostic symptom presentations following PTEs. To further investigate this topic, we recommend future studies to gather information on cultural background on a person-level, and/or assess cross-country differences (instead of regions).
Given the suggestion of configural invariance across geographical regions, LCA was applied to the total sample. Three classes distinguished by the severity of the symptoms were revealed. No qualitatively different classes were found (e.g. symptom-specific profiles), which is in contrast with previous findings (Boelen et al., 2022; Campbell et al., 2020; Contractor et al., 2020). Interestingly, these studies assessed diagnosis-specific symptoms (e.g. PTSD and depression only), and all found distinctive classes of PTSD, with or without depressive symptoms. While these prior studies used comprehensive diagnosis-specific questionnaires and/or clinical samples, the current study focused on the variety of responses to PTEs by a brief screening tool (GPS) in the general population. Our measure assessed each syndrome very briefly (mostly 1–2 items per syndrome) and with dichotomously (yes/no) scored items. Perhaps this less nuanced assessment made it more difficult to reveal distinctive patterns and reactions to PTEs. Notably, reactions to PTEs could be truly transdiagnostic, and could not fall within the symptom category of one specific disorder. This finding, which is suggested by the current results, should be examined in replication studies that address the above mentioned limitations by using transdiagnostic symptom measures that – at the same time – allow for a more detailed assessment of different syndromes.
Our study was the first to apply a person-centered approach to the GPS. Finding a three-class solution that differs by severity of symptoms is relatively common in psychiatric research, as diagnostic measures are often composed of covarying items that reflect overlapping approximations of related components and traits (Racz et al., 2023). This pattern is sometimes referred to as ‘salsa pattern’: It implies that the LCA has not revealed distinct heterogeneous classes per se but only gradients of severity (mild, medium, or hot salsa; Hallquist & Wright, 2014). Therefore, our findings may reflect spurious subgroups, but might also reflect conceptually meaningful classes of symptom severity. Previous studies applying a dimensional (variable-centered) approach to explore the GPS factor structure across different language versions showed either a three-factor (negative affectivity, core PTSD, and dissociative symptoms; Rossi et al., 2021; Salimi et al., 2023) or one-factor solution (Frewen et al., 2021). Thus, future research using a hybrid model, which integrates both approaches, is encouraged as it can further contribute to understanding stress and trauma-related transdiagnostic symptoms. However, analyzing risk factors using this approach (the second goal of our study), is currently not well developed. When applying this method, we might expect to find a one-factor solution with three severity levels, based on the current study findings and the CFA outcomes of the GPS.
The current study found that endorsement of previously identified risk factors (other stressful events, childhood trauma, history of mental illness, lack of social support, lack of resilience; Olff et al., 2020) was associated with membership in the respectively higher symptom classes. In line with previous research (Brewin et al., 2000), experiencing other stressful events recently and having a lack of social support were especially strong predictors of higher symptom class membership. The findings suggest that these risk factors relate not only to PTSD symptoms, but also to a range of transdiagnostic symptoms.
Several other demographic and trauma characteristics conferred greater risk for high symptom class membership. For example, geographic region emerged as a significant predictor of class membership, such that participants from North America and Latin American and Caribbean States were more likely to belong to the high versus low symptom class. Conversely, participants from Asia-Pacific States were more likely to belong to the low versus high symptom class. Interestingly, participants from North America reported both greater transdiagnostic symptom load after sexual violence exposure compared to other regions, as well as higher rates of events involving sexual violence. This double effect (greater response as well as higher frequency) may explain why those participants are also more likely to belong to a higher symptom class. Current findings may reflect a number of phenomena, including the ‘vulnerability paradox,’ in which higher rates of trauma-related sequelae are found in less vulnerable countries (Dückers et al., 2016). Widespread social stigmatization and discrimination of those with psychiatric conditions discourage symptom reporting in some regions, particularly Asian countries (Lauber & Rössler, 2007), or differences in cultural values in relation to self-concept and socialization characteristics in the different regions may furthermore impact symptom reporting (Markus & Kitayama, 1991).
However, cross-cultural differences in symptom manifestation and expression also deserve consideration. Namely, current conceptualizations of psychiatric concerns are heavily influenced by Western culture, meaning it is possible that available assessment measures, including the GPS, do not adequately capture nuanced differences in symptoms and culturally-specific manifestations of trauma across the globe (Heim et al., 2022; Rasmussen et al., 2014). Taken together, cross-cultural differences in stress and trauma-related transdiagnostic symptom manifestations and reporting point to the importance of using cross-culturally valid and accessible transdiagnostic symptom measures to inform prevention and treatment efforts, as well as to contribute to development of globally applicable nosology of mental disorders (Heim et al., 2022).
Women and gender nonbinary participants were more likely to belong to the high versus low and moderate symptom class. These results align with previous research indicating that women experience worse outcomes after trauma exposure than men (Kessler et al., 2017). Further, an index event that met Criterion A for PTSD in the DSM-5 (exposure to actual or threatened death, serious injury, or sexual violence; American Psychiatric Association, 2013) predicted high versus low and moderate symptom class membership. Of note, whether an index event met PTSD Criterion A did not discriminate between the moderate and low symptom class, supporting the notion that non-Criterion A events also contributed to notable mental health symptoms (Holmes et al., 2016). Lastly, in line with previous literature (Ogle et al., 2013), experiencing the index event multiple times was associated with greater symptom severity. An important avenue for future research is to address intersectionality and how this relates to the development of transdiagnostic health outcomes. Intersectionality refers to the interaction of two (or more) marginalized identities that contribute to multiple systems of disadvantage (Crenshaw, 2015). An individual’s social identities were not measured in the current study, except for gender. We encourage future studies to capture additional sociodemographic information to better understand transdiagnostic reactions among participants who may be more vulnerable to poor mental health outcomes.
4.1. Strengths and limitations
The study’s large sample size and participants’ diversity of countries and languages represent major strengths of the current study and make it one of the largest extant studies of exploring transdiagnostic symptoms. The following study limitations should be noted. Although the GPS is available in 21 different languages, its psychometric properties have only been assessed in English, Japanese, Persian, and Brazilian Portuguese; thus, further research is needed to confirm the validity of the measure in the additional languages. Selection bias may have influenced current findings, as participants were recruited online and via social media through connections to traumatic stress societies. It is likely that those with limited internet access or technological proficiency were less likely to participate, limiting generalizability. In addition, because data were collected online via a self-report survey, responses could not be verified for accuracy. Shortcomings that come with an online survey, however, may be balanced by greater disclosure of sensitive information. Lastly, although the sample was large overall, the sample size discrepancies in represented countries required meaningful grouping before statistical analysis; the UN regional groups were ultimately chosen as the most appropriate for the available data. These groups are based on geographical proximity, which limits the possibility of focusing on cross-cultural differences as these regions, in most cases, represent culturally very heterogeneous groups. This also might have mitigated the between-regional variations in the phenomenology of symptoms observed in the presented study. However, the UN uses these regional groups as a proxy indicator of country development that is connected to disparities in risk and protective factors associated with differences in exposure to various PTEs and vulnerability to trauma. Future work should focus on cross-cultural differences in more detail. In this regard, it is also important to consider multifaceted contextual influences. The results of this study must, for instance, be interpreted in light of the global Covid-19 pandemic during time of data collection. Considering global and, maybe even more important, regional impactful events and conflicts is crucial when conducting and interpreting research on global differences in stress and trauma-related reactions.
5. Conclusions
We explored whether there were distinct classes of transdiagnostic stress and trauma-related symptoms across geographic regions using an extensive worldwide sample. Symptom presentations appear to be similar (i.e. severity based) across six UN regions, but the extent to which symptom severity is expressed appears to differ. Future research with more distinct cultural and/or regional groupings is necessary to explain country and cultural differences in symptom manifestations after stress or trauma. In addition, researchers may consider administering the GPS to participants in person or through non-internet-based mediums to capture participants who might not otherwise access the measure and to potentially decrease selection bias. Our results found that lack of social support is a strong predictor for membership in the high symptom class, thus highlighting an important area of intervention for people exposed to stress or trauma. We encourage clinicians who provide care to trauma-exposed individuals to assess stress and trauma-related symptoms transdiagnostically, as symptoms like depression, anxiety, substance abuse, anger, or self-harm may be overlooked if only PTSD is assessed and vice versa.
Supplementary Material
Acknowledgements
This study was made possible by the Paper in a Day (PIAD) initiative as part of the International Society of Traumatic Stress Studies’ 38th Annual Meeting (9–12 November 2022, Atlanta, Georgia). We thank the conference organizing committee, and in particular Dr. Joanne Mouthaan and Dr. Sierra Elizabeth Carter for making PIAD possible; the Department of Psychology at Georgia State University for granting us their space and resources; and the Trauma Data Institute (TDI) for their PIAD sponsorship.
This PIAD project is part of the Global Collaboration on Traumatic Stress, a worldwide network of researchers and clinicians working together on traumatic stress topics of global importance. This study would not be possible without the work of Dr. Miranda Olff and her team for the Global Psychotrauma Screen. We thank them for granting us access to the data.
Funding Statement
Stephanie Haering’s time is supported by a PhD scholarship from ‘Stiftung der Deutschen Wirtschaft’. Christine Bourey’s time is supported by the United States’ National Institute of Mental Health training grant T32MH103210 and T32MH013043.
Open Scholarship

This article has earned the Center for Open Science badge for Open Data. The data are openly accessible at https://osf.io/c6u3m/
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability
The data, code, and analyses for this study are publicly available at https://osf.io/c6u3m/
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Beller, J. (2023). Morbidity profiles in Europe and Israel: International comparisons from 20 countries using biopsychosocial indicators of health via latent class analysis. Journal of Public Health, 31(8), 1329–1337. 10.1007/s10389-021-01673-0 [DOI] [Google Scholar]
- Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., Girolamo, G. d., Florescu, S., Gureje, O., Huang, Y., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelen, P. A., Eisma, M. C., Keijser, J. d., & Lenferink, L. I. M. (2022). Traumatic stress, depression, and non-bereavement grief following non-fatal traffic accidents: Symptom patterns and correlates. PLoS One, 17(2), Article e0264497. 10.1371/journal.pone.0264497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. 10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Bromet, E. J., Atwoli, L., Kawakami, N., Navarro-Mateu, F., Piotrowski, P., King, A. J., Aguilar-Gaxiola, S., Alonso, J., Bunting, B., Demyttenaere, K., Florescu, S., de Girolamo, G., Gluzman, S., Haro, J. M., de Jonge, P., Karam, E. G., Lee, S., Kovess-Masfety, V., Medina-Mora, M. E., … Kessler, R. C. (2017). Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. Psychological Medicine, 47(2), 227–241. 10.1017/S0033291716002026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, S. B., Trachik, B., Goldberg, S., & Simpson, T. L. (2020). Identifying PTSD symptom typologies: A latent class analysis. Psychiatry Research, 285, Article 112779. 10.1016/j.psychres.2020.112779 [DOI] [PubMed] [Google Scholar]
- Chiu, K. B., deRoon-Cassini, T. A., & Brasel, K. J. (2011). Factors identifying risk for psychological distress in the civilian trauma population: Psychological distress in civilian trauma. Academic Emergency Medicine, 18(11), 1156–1160. 10.1111/j.1553-2712.2011.01206.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor, A. A., Roley-Roberts, M. E., Lagdon, S., & Armour, C. (2017). Heterogeneity in patterns of DSM-5 posttraumatic stress disorder and depression symptoms: Latent profile analyses. Journal of Affective Disorders, 212, 17–24. 10.1016/j.jad.2017.01.029 [DOI] [PubMed] [Google Scholar]
- Contractor, A. A., Weiss, N. H., Schick, M. R., Natesan Batley, P., Forkus, S. R., & Sharma, R. (2020). Comparison of latent typologies of posttraumatic stress disorder and depression symptoms across military personnel from India and the US. Journal of Anxiety Disorders, 70, Article 102195. 10.1016/j.janxdis.2020.102195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw, K. (2015). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989(1), https://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8. [Google Scholar]
- Cruz-Gonzalez, M., Alegría, M., Palmieri, P. A., Spain, D. A., Barlow, M. R., Shieh, L., Williams, M., Srirangam, P., & Carlson, E. B. (2023). Racial/ethnic differences in acute and longer-term posttraumatic symptoms following traumatic injury or illness. Psychological Medicine, 53(11), 5099–5108. 10.1017/S0033291722002112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deen, A., Biedermann, S. V., Lotzin, A., Krüger-Gottschalk, A., Dyer, A., Knaevelsrud, C., Rau, H., Schellong, J., Ehring, T., & Schäfer, I. (2022). The dissociative subtype of PTSD in trauma-exposed individuals: A latent class analysis and examination of clinical covariates. European Journal of Psychotraumatology, 13(1), Article 2031591. 10.1080/20008198.2022.2031591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dückers, M. L. A., Alisic, E., & Brewin, C. R. (2016). A vulnerability paradox in the cross-national prevalence of post-traumatic stress disorder. British Journal of Psychiatry, 209(4), 300–305. 10.1192/bjp.bp.115.176628 [DOI] [PubMed] [Google Scholar]
- Elklit, A., Hyland, P., & Shevlin, M. (2014). Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology, 5(1), Article 24221. 10.3402/ejpt.v5.24221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford, J. D., Grasso, D. J., Elhai, J. D., & Courtois, C. A. (2015). Social, cultural, and other diversity issues in the traumatic stress field. In Posttraumatic stress disorder (s. 503–546). Elsevier. 10.1016/B978-0-12-801288-8.00011-X. [DOI] [Google Scholar]
- Frewen, P., McPhail, I., Schnyder, U., Oe, M., & Olff, M. (2021). Global Psychotrauma Screen (GPS): psychometric properties in two internet-based studies. European Journal of Psychotraumatology, 12(1), Article 1881725. 10.1080/20008198.2021.1881725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallquist, M. N., & Wright, A. G. C. (2014). Mixture modeling methods for the assessment of normal and abnormal personality, part I: Cross-sectional models. Journal of Personality Assessment, 96(3), 256–268. 10.1080/00223891.2013.845201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidari, S., Babor, T. F., De Castro, P., Tort, S., & Curno, M. (2016). Sex and gender equity in research: Rationale for the SAGER guidelines and recommended use. Research Integrity and Peer Review, 1(1), 2. 10.1186/s41073-016-0007-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heim, E., Karatzias, T., & Maercker, A. (2022). Cultural concepts of distress and complex PTSD: Future directions for research and treatment. Clinical Psychology Review, 93, Article 102143. 10.1016/j.cpr.2022.102143 [DOI] [PubMed] [Google Scholar]
- Hinton, D. E., & Lewis-Fernández, R. (2011). The cross-cultural validity of posttraumatic stress disorder: Implications for DSM-5. Depression and Anxiety, 28(9), 783–801. 10.1002/da.20753 [DOI] [PubMed] [Google Scholar]
- Hogg, B., Gardoki-Souto, I., Valiente-Gómez, A., Rosa, A. R., Fortea, L., Radua, J., Amann, B. L., & Moreno-Alcázar, A. (2023). Psychological trauma as a transdiagnostic risk factor for mental disorder: An umbrella meta-analysis. European Archives of Psychiatry and Clinical Neuroscience, 273(2), 397–410. 10.1007/s00406-022-01495-5 [DOI] [PubMed] [Google Scholar]
- Holmes, S. C., Facemire, V. C., & DaFonseca, A. M. (2016). Expanding criterion A for posttraumatic stress disorder: Considering the deleterious impact of oppression. Traumatology, 22(4), 314–321. 10.1037/trm0000104 [DOI] [Google Scholar]
- Iacoviello, B. M., & Charney, D. S. (2014). Psychosocial facets of resilience: Implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. European Journal of Psychotraumatology, 5(1), Article 23970. 10.3402/ejpt.v5.23970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., Degenhardt, L., de Girolamo, G., Dinolova, R. V., Ferry, F., Florescu, S., Gureje, O., Haro, J. M., Huang, Y., Karam, E. G., Kawakami, N., Lee, S., Lepine, J.-P., Levinson, D., … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), Article 1353383. 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger, R. F., Chentsova-Dutton, Y. E., Markon, K. E., Goldberg, D., & Ormel, J. (2003). A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology, 112(3), 437–447. 10.1037/0021-843X.112.3.437 [DOI] [PubMed] [Google Scholar]
- Lauber, C., & Rössler, W. (2007). Stigma towards people with mental illness in developing countries in Asia. International Review of Psychiatry, 19(2), 157–178. 10.1080/09540260701278903 [DOI] [PubMed] [Google Scholar]
- Levin-Aspenson, H. F., Watson, D., Ellickson-Larew, S., Stanton, K., & Stasik-O’Brien, S. M. (2021). Beyond distress and fear: Differential psychopathology correlates of PTSD symptom clusters. Journal of Affective Disorders, 284, 9–17. 10.1016/j.jad.2021.01.090 [DOI] [PubMed] [Google Scholar]
- Lowe, S. R., Ratanatharathorn, A., Lai, B. S., van der Mei, W., Barbano, A. C., Bryant, R. A., Delahanty, D. L., Matsuoka, Y. J., Olff, M., Schnyder, U., Laska, E., Koenen, K. C., Shalev, A. Y., & Kessler, R. C. (2021). Posttraumatic stress disorder symptom trajectories within the first year following emergency department admissions: Pooled results from the international consortium to predict PTSD. Psychological Medicine, 51(7), 1129–1139. 10.1017/S0033291719004008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markus, H. R., & Kitayama, S. (1991). Culture and the self: Implications for cognition, emotion, and motivation. Psychological Review, 98(2), 224–253. 10.1037/0033-295X.98.2.224 [DOI] [Google Scholar]
- Marques, L., Robinaugh, D. J., LeBlanc, N. J., & Hinton, D. (2011). Cross-cultural variations in the prevalence and presentation of anxiety disorders. Expert Review of Neurotherapeutics, 11(2), 313–322. 10.1586/ern.10.122 [DOI] [PubMed] [Google Scholar]
- Møller, L., Meisner, M. W., Søgaard, U., Elklit, A., & Simonsen, E. (2021). Assessment of personality functioning in ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder. Personality Disorders: Theory, Research, and Treatment, 12(5), 466–474. 10.1037/per0000491 [DOI] [PubMed] [Google Scholar]
- Nochaiwong, S., Ruengorn, C., Thavorn, K., Hutton, B., Awiphan, R., Phosuya, C., Ruanta, Y., Wongpakaran, N., & Wongpakaran, T. (2021). Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Scientific Reports, 11(1), Article 10173. 10.1038/s41598-021-89700-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund-Gibson, K., & Choi, A. Y. (2018). Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science, 4(4), 440–461. 10.1037/tps0000176 [DOI] [Google Scholar]
- Oe, M., Kobayashi, Y., Ishida, T., Chiba, H., Matsuoka, M., Kakuma, T., Frewen, P., & Olff, M. (2020). Screening for psychotrauma related symptoms: Japanese translation and pilot testing of the Global Psychotrauma Screen. European Journal of Psychotraumatology, 11(1), Article 1810893. 10.1080/20008198.2020.1810893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle, C. M., Rubin, D. C., Berntsen, D., & Siegler, I. C. (2013). The frequency and impact of exposure to potentially traumatic events over the life course. Clinical Psychological Science, 1(4), 426–434. 10.1177/2167702613485076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff, M., Bakker, A., Frewen, P., Aakvaag, H., Ajdukovic, D., Brewer, D., Elmore Borbon, D. L., Cloitre, M., Hyland, P., Kassam-Adams, N., Knefel, M., Lanza, J. A., Lueger-Schuster, B., Nickerson, A., Oe, M., Pfaltz, M. C., Salgado, C., Seedat, S., Wagner, A., & Schnyder, U. (2020). Screening for consequences of trauma – an update on the global collaboration on traumatic stress. European Journal of Psychotraumatology, 11(1), Article 1752504. 10.1080/20008198.2020.1752504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff, M., Primasari, I., Qing, Y., Coimbra, B. M., Hovnanyan, A., Grace, E., Williamson, R. E., Hoeboer, C. M., & the GPS-CCC Consortium . (2021). Mental health responses to COVID-19 around the world. European Journal of Psychotraumatology, 12(1), Article 1929754. 10.1080/20008198.2021.1929754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racz, S. J., McMahon, R. J., Gudmundsen, G., McCauley, E., & Vander Stoep, A. (2023). Latent classes of oppositional defiant disorder in adolescence and prediction to later psychopathology. Development and Psychopathology, 35(2), 730–748. 10.1017/S0954579421001875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen, A., Keatley, E., & Joscelyne, A. (2014). Posttraumatic stress in emergency settings outside North America and Europe: A review of the emic literature. Social Science & Medicine, 109, 44–54. 10.1016/j.socscimed.2014.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R., Socci, V., Talevi, D., Niolu, C., Pacitti, F., Di Marco, A., Rossi, A., Siracusano, A., Di Lorenzo, G., & Olff, M. (2021). Trauma-spectrum symptoms among the Italian general population in the time of the COVID-19 outbreak. European Journal of Psychotraumatology, 12(1), Article 1855888. 10.1080/20008198.2020.1855888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salimi, Y., Hoeboer, C., Motevalli Haghi, S. A., Williamson, R. E., Rahimi, M. D., Rajabi-Gilan, N., Almasi, A., & Olff, M. (2023). Trauma and its consequences in Iran: Cross-cultural adaption and validation of the Global Psychotrauma Screen in a representative sample. BMC Psychiatry, 23(1), 65. 10.1186/s12888-023-04564-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spikol, E., Robinson, M., McGlinchey, E., Ross, J., & Armour, C. (2022). Exploring complex-PTSD comorbidity in trauma-exposed Northern Ireland veterans. European Journal of Psychotraumatology, 13(1), Article 2046953. 10.1080/20008198.2022.2046953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stekhoven, D. J. (2022). missForest: Nonparametric Missing Value Imputation using Random Forest [R]. https://cran.r-project.org/package=missForest.
- Stekhoven, D. J., & Buhlmann, P. (2012). Missforest—Non-parametric missing value imputation for mixed-type data. Bioinformatics, 28(1), 112–118. 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- Sunderland, M., Carragher, N., Chapman, C., Mills, K., Teesson, M., Lockwood, E., Forbes, D., & Slade, T. (2016). The shared and specific relationships between exposure to potentially traumatic events and transdiagnostic dimensions of psychopathology. Journal of Anxiety Disorders, 38, 102–109. 10.1016/j.janxdis.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Tortella-Feliu, M., Fullana, M. A., Pérez-Vigil, A., Torres, X., Chamorro, J., Littarelli, S. A., Solanes, A., Ramella-Cravaro, V., Vilar, A., González-Parra, J. A., Andero, R., Reichenberg, A., Mataix-Cols, D., Vieta, E., Fusar-Poli, P., Ioannidis, J. P. A., Stein, M. B., Radua, J., & Fernández De La Cruz, L. (2019). Risk factors for posttraumatic stress disorder: An umbrella review of systematic reviews and meta-analyses. Neuroscience & Biobehavioral Reviews, 107, 154–165. 10.1016/j.neubiorev.2019.09.013 [DOI] [PubMed] [Google Scholar]
- United Nations . (2022). Regional groups of Member States. United Nations, Department for General Assembly and Conference Management. Retrieved November 9, 2022 from https://www.un.org/dgacm/en/content/regional-groups.
- Weller, B. E., Bowen, N. K., & Faubert, S. J. (2020). Latent class analysis: A guide to best practice. Journal of Black Psychology, 46(4), 287–311. 10.1177/0095798420930932 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data, code, and analyses for this study are publicly available at https://osf.io/c6u3m/